Abstract
Background
Individuals are thought to compensate for femoral anteversion by altering hip rotation. However, the relationship between hip rotation in a neutral position (i.e. static rotation) and dynamic hip rotation is poorly understood, as is the relationship between anteversion and hip rotation.
Research Objective
Herein, anteversion and in-vivo hip rotation during standing, walking, and pivoting were measured in eleven asymptomatic, morphologically normal, young adults using three-dimensional computed tomography models and dual fluoroscopy.
Methods
Using correlation analyses, we: 1) determined the relationship between hip rotation in the static position to that measured during dynamic activities, and 2) evaluated the association between femoral anteversion and hip rotation during dynamic activities. Hip rotation was calculated while standing (static-rotation), throughout gait, as a mean during gait (mean gait rotation), and as a mean (mid-pivot rotation), maximum (max-rotation) and minimum (min-rotation) during pivoting.
Results
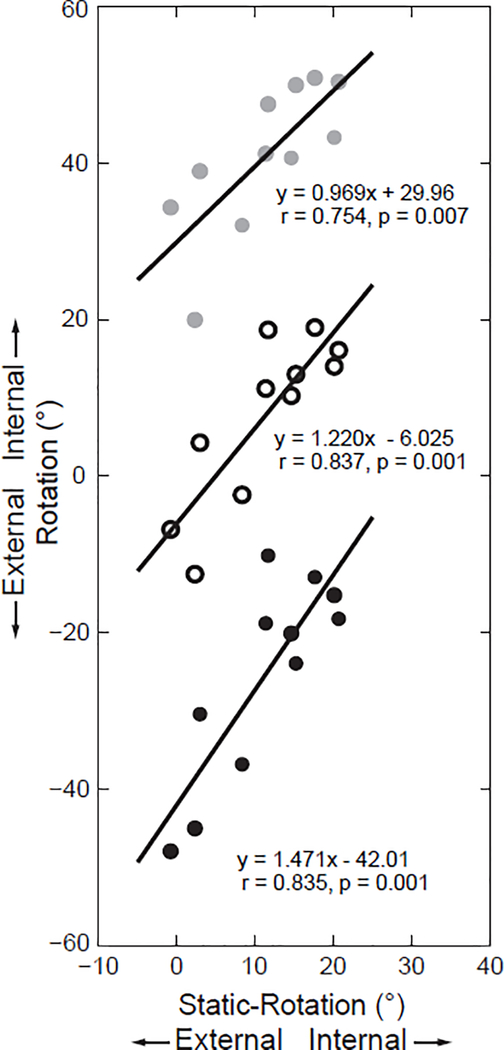
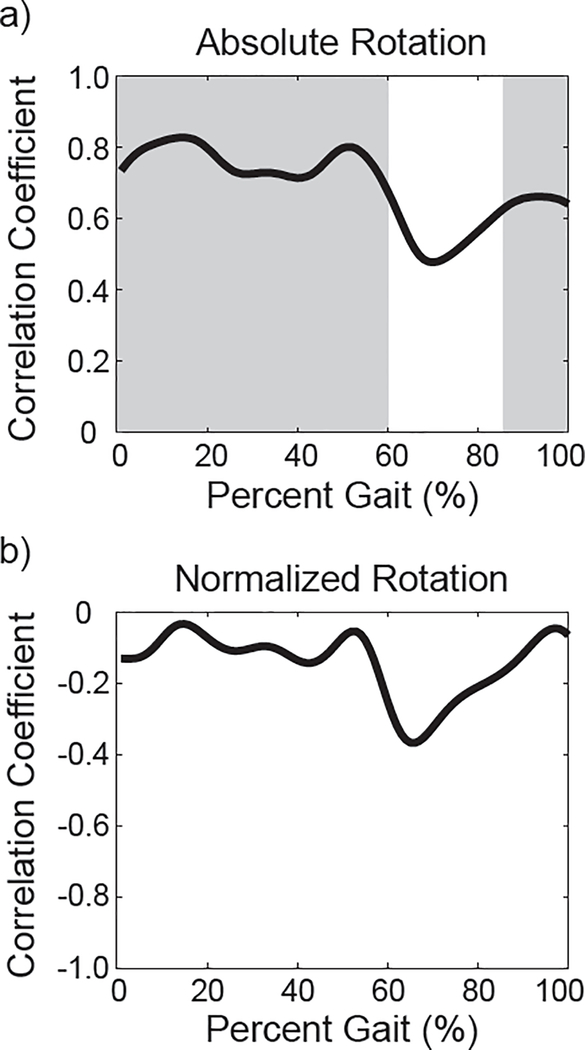
Static-rotation (mean±standard deviation; 11.3°±7.3°) and mean gait rotation (7.8°±4.7°) were positively correlated (r=0.679, p=0.022). Likewise, static-rotation was strongly correlated with mid-pivot rotation (r=0.837, p=0.001), max-rotation (r=0.754, p=0.007), and min-rotation (r=0.835, p=0.001). Strong positive correlations were found between anteversion and hip internal rotation during all of the stance phase (0–60% gait) and during mid- and terminal-swing (86–100% gait) (all r>0.607, p<0.05).
Conclusions
Our results suggest that the static position may be used cautiously to express the neutral rotational position of the femur for dynamic movements. Further, our results indicate that femoral anteversion is compensated for by altering hip rotation. As such, both anteversion and hip rotation may be important to consider when diagnosing hip pathology and planning for surgical procedures.
Keywords: functional anteversion, proximal femoral rotation, hip motion, dynamic imaging, hip kinematics
1. Introduction
Femoral anteversion describes the angle between the proximal femoral neck and distal femoral condyles [1] and is an important metric used to describe femoral anatomy. Computer simulations have used femoral anteversion to estimate the point at which the femur will impinge with the acetabulum in both normal and diseased hips [2–4]. Femoral anteversion, however, only describes an anatomic parameter of the femur, yet it is believed to affect hip kinematics, especially hip rotation about the axial plane [5]. To this end, investigators have used proximal femoral rotation (previously termed ‘functional femoral anteversion’ in [6–8]) (Fig. 1a), which may be more clinically relevant than anteversion alone, as it considers both femoral anteversion and hip function (i.e. rotation). Prior to the study of pathological patients, it is first necessary to define proximal femoral rotation angles in morphologically normal, asymptomatic subjects.
Figure 1:
Measurement of hip rotation (distal femoral rotation) and the anatomical landmarks used to define the femur and pelvis coordinate systems. (a) Hip rotation (angle A) measures the angle between the transverse axis of the pelvis (solid black line, recreated near the femoral condyles for clarity) and the posterior condylar line (orange dotted line). Proximal femoral rotation (angle B) is the angle between the transverse axis of the pelvis and the femoral neck (green dotted line). Proximal femoral rotation is a measurement of femoral anteversion (angle between the orange and green dotted lines) that is offset by hip rotation (distal femoral rotation). (b) To define the pelvis coordinate system, landmarks of the bilateral anterior superior iliac spines (ASIS, cyan) and the bilateral posterior superior iliac spines (PSIS, black) were identified. The pelvic plane (white plane shown on the anterior and lateral views) intersected the two ASIS landmarks and the mid-point of the PSIS (blue) landmarks, while the medial-lateral axis passed through the two ASIS landmarks (dotted black line shown on the anterior view). (c) To define the femur coordinate system, landmarks of the most posterior point on the proximal femur (magenta) and each femoral condyle (yellow) were identified. The table top plane (solid black line shown on the lateral view) intersected these three landmarks. (d) Landmarks of the femoral head center (light green) and center of the knee (orange) were identified. The head center was projected onto the table top plane (dark green). The superior-inferior axis of the femur (dotted black line shown on the posterior view) passed through the knee center and the projection of the head center.
Recently, hip rotation in supine and standing (i.e. static position) was measured in patients with hip osteoarthritis before and after total hip arthroplasty (THA) to evaluate the effects of surgery on the neutral position of the hip [6–8]. In one such study, hip rotation varied widely between subjects, with a range greater than 60° in supine, and was correlated with femoral anteversion [8]. These results suggest that individuals may compensate dynamically for femoral anteversion. However, hip rotation during dynamic activities has not been evaluated relative to hip rotation in static positions (i.e. supine or standing). Quantifying static and dynamic hip rotation and establishing the relationship with femoral anteversion in asymptomatic control subjects could provide valuable baseline data for refining pre-operative planning and computer simulations aimed at improving functional outcomes in pathological patients.
Motion capture methods that use reflective skin markers have been used to measure hip rotation during dynamic activities. However, skin motion artifact (i.e. movement of soft tissue relative to the underlying bones) may lead to substantial errors when estimating the location of the hip joint center and calculating hip kinematics, especially when evaluating hip rotation, where errors may exceed 21° [9, 10]. To this end, we have used dual fluoroscopy (DF) and model-based tracking (MBT) [11] to quantify in-vivo hip joint kinematics to sub-degree error [12] for a static (standing) position [13] and during dynamic activities [9, 13–16]. The advantage of DF is that bone motion is imaged directly, eliminating errors caused by soft tissue artifact.
The objectives of this study were to use DF, MBT, and measurements of 3D CT models to: 1) determine the relationship between hip rotation in the static position and during dynamic activities, and 2) evaluate the association between femoral anteversion and hip rotation during dynamic activities. In addition, we measured proximal femoral rotation during static and dynamic activities. We hypothesized that: 1) subjects with more internal hip rotation in the static position would have increased internal hip rotation during dynamic activities, and 2) subjects with increased anteversion would also have more internal hip rotation during dynamic activities (i.e. less proximal femoral rotation compared to femoral anteversion).
2. Methods
2.1. Recruitment, computed tomography imaging, 3D surface reconstruction
Eighteen subjects signed informed consent prior to participation in this Institutional Review Board approved study (University of Utah, IRB 51053). Only subjects free from pain and prior surgery of the lower limb or back were considered. All subjects were screened for deformities, including acetabular dysplasia and femoroacetabular impingement, using an anteroposterior film. Seven subjects with radiographic deformities were excluded. Eleven subjects (six males) participated and were analyzed with DF and MBT as part of previous research published by our group [9, 13, 15, 16]. The mean±standard deviation age, height, and body mass index was 23±2years, 173±10cm, and 21±2kg/m2, respectively.
CT arthrography scans were obtained for each subject (128-slice SOMATOM Definition, Siemens Healthcare, Munich, Bavaria, Germany). The scan included the entire pelvis and proximal femur (1mm slices, 120kVp, 200–400mAs) and distal femur (3mm slices, 120kVP, 150mAs) [9, 13, 15, 16]. Three-dimensional surface reconstructions of the pelvis and femur were obtained from semi-automatic segmentation of the CT images (Amira, v6.0.1, Visage Imaging, San Diego, CA, USA) [9, 12–16].
2.2. Activities
One static (standing) and three dynamic activities were completed on a dual-belt instrumented treadmill (Bertec Corporation, Columbus, OH, USA), including level walk at a self-selected over-ground walking speed, internal rotation, and external rotation [9, 13, 15, 16]. For the static trial, subjects were instructed to stand upright with their feet hip-width apart and pointed forward, but the position of their feet was not strictly enforced by research personnel. The internal and external rotation activities were performed to end range of motion with both feet on the ground, while angular changes were permitted at the ankle and knee joints. The order of the dynamic activities was randomized. One trial of the static activity and two trials of the dynamic activities were collected.
2.3. Dual fluoroscopy and model-based tracking
Details of the custom DF system and MBT used herein have been previously reported and validated to errors less than 0.5mm and 0.6° [12]. Briefly, two pairs of fluoroscopes were arranged around the instrumented treadmill such that the combined field of view contained the hip joint of interest. To balance imaging of each side, the right hip was imaged in six subjects. Fluoroscope images were acquired at 100Hz. For each dynamic activity, the trial with the greatest range of motion and/or highest quality fluoroscopy images (determined qualitatively by NMF) was selected and analyzed with MBT. Using MBT, digitally reconstructed radiographs from the CT images of the pelvis and femur were semi-automatically aligned with the DF images to calculate the spatial position of each bone [11].
2.4. Definition of landmarks, coordinate systems, anatomical planes
Three-dimensional CT reconstructions of the pelvis and femur were imported into MATLAB (v. 7.10, The MathWorks, Natick, MA, USA) and PostView (v.1.9.0, The University of Utah, Salt Lake City, UT, USA) to define landmarks of pelvic and femoral anatomy necessary to identify bone coordinate systems [12]. For the pelvis, the coordinates recommended by the International Society of Biomechanics (ISB) were used (Fig. 1b) [17]. The medial-lateral axis was defined as the vector through the nodes representing each anterior superior iliac spine (ASIS), while the transverse plane contained this vector and the mid-point of the two posterior superior iliac spine (PSIS) landmarks. For the femur, the table top plane [1] was defined as the plane through the most posterior point of the proximal femur (i.e. greater trochanter) and the most posterior point of each femoral condyle (Fig. 1c). The superior-inferior axis of the table top plane was defined as the vector connecting the femoral head center and the center of the knee (Fig. 1d). This axis was projected onto the table top plane to ensure an orthogonal coordinate system. Importantly, the use of the table top plane provided a direct comparison between hip rotation and femoral anteversion, as both used the posterior condylar line as the distal reference [1–3, 6–8, 18–20]. However, for consistency with ISB recommendations, the femoral coordinate system was also defined using the center of the femoral head and the medial and lateral epicondyles, and results relative to this coordinate system were included as supplemental material. Landmark coordinates were output from MBT for each activity and used to calculate hip angles.
2.5. Measurement of hip rotation and femoral anteversion
Femoral anteversion was measured as the angle between the femoral neck and the posterior condylar line [1–3, 6–8, 18–22]. Hip rotation (i.e. distal femoral rotation) was measured as the angle between the medial-lateral axis of the pelvis and the posterior condylar line, and was set positive for internal rotation (Fig. 1a). Proximal femoral rotation was measured as the angle between the medial-lateral axis of the pelvis and the femoral neck, which could also be calculated by subtracting hip rotation from femoral anteversion. Surface nodes representing the femoral neck were fit to a cylinder using MATLAB to establish the neck axis used to measure anteversion and proximal femoral rotation [23].
2.6. Data analysis and statistics
Hip rotation was measured in the static position (static-rotation), at each time point of the gait cycle, and at the end range of motion of the pivots. A single gait cycle, defined as heel-strike to heel-strike of the ipsilateral foot, was analyzed and data were normalized to 0–100% gait. Data for the internal and external rotation activities were considered together such that the maximum internal and external rotation occurred during the internal rotation pivot (max-rotation) and external rotation pivot (min-rotation), respectively. Proximal femoral rotation at each point was also calculated.
Several correlation analyses were conducted to determine the relationship between static-rotation and hip rotation measured dynamically. To evaluate with respect to range of motion, static-rotation was correlated with the max- and min-rotation from the pivot activity. The mean hip rotation during the gait cycle (mean gait rotation) and the mean of the max- and min-rotation during pivoting (mid-pivot rotation) were correlated with static-rotation to better assess the neutral position of dynamic activities.
Correlation was then evaluated for femoral anteversion with static-rotation, mean gait rotation, max-rotation, min-rotation, mid-pivot rotation, and the rotation at each time point of the normalized gait cycle to determine whether a relationship existed between anteversion and joint kinematics. Finally, this evaluation was repeated for normalized rotation during gait, which was calculated as a relative measure from the static position, to determine the effects of considering the static position as the absolute neutral orientation (as is sometimes performed in kinematic analyses).
Upon confirming a normal distribution using a Kolmogorov-Smirnov test, hip rotation angles were expressed as mean±standard deviation. The mean and 95% confidence interval were plotted for hip rotation during gait. Correlations were assessed using the Pearson correlation coefficient. Values of p<0.05 were considered significant. For the purpose of interpreting the correlation coefficient, r=0.00–0.19 was regarded as very weak, 0.20–0.39 as weak, 0.40–0.59 as moderate, 0.60–0.79 as strong, and 0.80–1.00 as very strong. All statistical analyses were performed with SPSS statistical software (v.22, IBM, Armonk, NY, USA).
3. Results
3.1. Relationship between static-rotation and hip rotation in dynamic activities
When averaged across subjects, the range of hip rotation during gait was 2.8° to 11.8° and was largest during the loading phase and mid stance (maximum at 13% gait) and smallest toward the end of stance (minimum at 56% gait) for both the coordinate system based on the table top plane (Fig. 2a) and the ISB femur coordinates (Fig. S1a). A strong correlation was found between static-rotation and the mean gait rotation (Table 1) for both the coordinate system based on the table top plane (Fig. 2b) and the ISB femur coordinates (Fig. S1b). For the pivots, static-rotation was strongly to very strongly correlated with the max-rotation, min-rotation, and mid-pivot rotation (Table 1) for both the coordinate system based on the table top plane (Fig. 3) and the ISB femur coordinates (Fig. S2). The rotation angles using ISB femur coordinates were within 9° of those using the table top plane for all observed activities.
Figure 2:
Hip rotation measured during gait (a) and the relationship between the mean hip rotation during gait and as measured during standing (b). Hip rotation was averaged across subjects over the time-normalized gait cycle (a), and indicated that hip rotation (solid black line) was maximized at 13% gait and minimized at 56% gait (vertical dotted lines). The 95% confidence interval of hip rotation is shown (gray lines). The mean gait rotation was positively correlated with hip rotation in static (static-rotation) (b).
Table 1.
Summary of hip rotation and proximal femoral rotation measured during static and dynamic activities, and correlation coefficients with p-values found when associating hip rotation with static-rotation and femoral anteversion.
| Hip rotation | Proximal femoral rotation | Hip rotation correlated with static-rotation | Hip rotation correlated with anteversion | |
|---|---|---|---|---|
| Static-rotation | 11.3°±7.3° | 4.4°±5.6° | NA | r=0.672 p=0.024 |
| Mean gait rotation | 7.8°±4.7° | 7.9°±3.8° | r=0.679 p=0.022 |
r=0.800 p=0.003 |
| Mid-pivot rotation | 7.7°±10.7° | 8.0°±8.7° | r=0.837 p=0.001 |
r=0.583 (NS) |
| Max-rotation | 40.9°±9.4° | −25.2°±8.2° | r=0.754 p=0.007 |
r=0.513 (NS) |
| Min-rotation | −25.4°±12.9° | 41.1°±10.5° | r=0.835 p=0.001 |
r=0.589 (NS) |
| Range of rotation | 66.3°±7.4° | 66.3°±7.4° | r=0.497 (NS) |
r=−0.375 (NS) |
Data expressed as mean ± standard deviation. NA: not applicable; NS: not significant.
Figure 3:
Correlation plots indicating the strength of the relationship between hip rotation measured during standing (static-rotation) and hip rotation measured during pivoting. The maximum rotation (max-rotation) occurred during internal rotation pivot (top, solid gray circles). The minimum rotation (min-rotation) occurred during external rotation (bottom, solid black circles). The correlation between the average of the max- and min-rotation (mid-pivot rotation) and static-rotation is also shown (middle, open circles).
3.2. Proximal femoral rotation and the association between femoral anteversion and hip rotation
Femoral anteversion was 15.7°±6.3°, and was strongly correlated with static-rotation and very strongly correlated with the mean gait rotation (Table 1). The deviation of proximal femoral rotation tended to be smaller than hip rotation and femoral anteversion (Table 1). In the analysis of femoral anteversion and rotation, a strong to very strong positive correlation was apparent during all of the stance phase (0–60% gait) and during mid- and terminal-swing (86–100% gait) (all r>0.607, p<0.05) for the coordinate system based on the table top plane (Fig. 4a). However, no significant correlations were observed when the rotation was normalized as the angular change from the static position for the coordinate system based on the table top plane (Fig. 4b).
Figure 4:
Plots of the correlation coefficient between anteversion and hip rotation over the time-normalized gait cycle as measured (a) and when normalized to the hip rotation measured during standing (b). Hip rotation and anteversion were significantly and strongly correlated during all of stance and during mid- and terminal-swing, as indicated in the regions where a gray background is present (a). However, when hip rotation was normalized based on the rotation measured during standing, no significant correlations were found between hip rotation and anteversion, as indicated by an absence of the gray background (b).
4. Discussion
In this study we determined: 1) the relationship between hip rotation in the static position and during dynamic activities, and 2) the association between femoral anteversion and hip rotation during dynamic activities. The strong positive correlations of static-rotation with hip rotation during dynamic activities support our hypothesis that hips that are internally rotated in the static position are also internally rotated during dynamic activities. Additionally, the positive correlation between femoral anteversion and static-rotation agrees with previous findings that subjects with increased anteversion have increased internal hip rotation when standing [7]. Interestingly, significant correlations between anteversion and rotation during gait were eliminated when rotation was expressed as a relative measure from the static position. This is an important finding, as it indicates that kinematic differences across subjects and groups could be concealed when equivalent neutral positions are assumed. Collectively, our results suggest that proximal femoral rotation, which considers both anatomy and subject-specific hip rotation, may be a good metric to use when interpreting joint kinematics derived from computer simulations, skin marker motion analysis, or for the purpose of pre-operative planning for surgeries that could alter femoral version.
Our results could improve simulation-based research. For example, many computer simulation studies have relied on femoral anteversion to represent proximal femoral rotation by defining the neutral position from the table top plane and assigning hip rotation to 0°, thereby ignoring the subject-specific neutral position of the femur [2, 3]. This assumption likely skews range of motion measurements as our findings suggest that hip rotation is not 0° in a neutral orientation for either static or dynamic activities. Specifically, we found hip rotation to be 11.3° during standing, a mean of 7.8° during gait, and a mean of 7.7° between the internal and external pivot activities (Table 1). Additionally, the standard deviations of these measurements (7.3°, 4.7°, and 10.7°, for standing, gait, and pivots, respectively) suggest that the vast majority of individuals will not have a hip rotation of 0°. To avoid errors in evaluating range of motion and making comparisons between subjects and across groups, we recommend that static hip rotation be measured on a subject-specific basis.
To our knowledge, our study is the first to report the association between anteversion and hip rotation during dynamic movements in asymptomatic subjects with morphologically normal hips. Previous studies have reported increased internal hip rotation during gait for persons with increased femoral anteversion [5, 24, 25]. However, our results are not directly comparable as previous research studied patients with anatomic deformities of the hip [5]. The positive correlations between femoral anteversion and hip rotation observed herein suggest that increased femoral anteversion may lead to compensatory motion at the hip. This conclusion is further supported by previous research that employed computer simulations [26], which suggested that increased hip internal rotation may help stabilize the hip during dynamic motions in persons with increased anteversion. Hip stabilization, created by the co-contraction of the internal and external hip rotators, may position the lateral greater trochanter in a more neutral orientation. In support of this, we found strong positive correlations between anteversion and hip rotation during the stance phase of gait (Fig. 4a). Furthermore, the gluteus medius has been reported to play a vital role in hip stabilization during this portion of gait [27, 28]. We believe contraction of the gluteus medius during hip stabilization causes internal femur rotation due to its attachment on the anterior greater trochanter, thus neutralizing proximal femoral rotation. However, future studies should investigate muscle activations and associated properties in relation to femoral anteversion to better quantify the role anteversion plays in dynamic hip motion.
The strong to very strong correlations between anteversion and hip rotation could have implications for pre-operative planning of THA. Modular stems [29] are frequently used in hips with excessive femoral anteversion as a means to decrease anteversion. However, based on the results of the current study, and the previously published finding that internal rotation increases following THA [6–8], this practice may not be as effective as has been proposed. For example, our results indirectly suggest that one risk of trying to reduce excessive anteversion is that proximal femoral rotation will be altered as well, possibly leading to impingement or dislocation. Accordingly, we recommend that proximal femoral rotation be evaluated prior to adjusting femoral version.
The advantage of using CT, DF, and MBT for this study was that both the 3D anatomy (e.g. femoral anteversion) and hip kinematics could be measured accurately [12]. However, there were limitations. First, the number of the subjects was relatively small, which required strong correlations to reach statistical significance. Nevertheless, one of the purposes of this study was to provide valuable baseline data from asymptomatic control subjects, and with significant findings, we feel the small sample size was sufficient. Second, relationships between static-rotation and rotation during dynamic activities were only assessed for gait and rotational pivots. Our goal was to evaluate an activity common to daily life (walking) and one performed primarily in the axial plane (pivoting). Future studies should examine other activities with larger and more complex motion. Third, observed motions may have affected the measured hip rotation. Specifically, verbal instructions were provided on how to perform each activity; since foot positions were not physically enforced, we believe the observed motions reflect a neutral position for each subject. Additionally, rotation of other lower extremity joints (i.e. knee and ankle) could affect hip rotation. However, our methods were consistent with simulation studies and pre-operative planning which often excludes the other joints. Finally, subjects were exposed to ionizing radiation; the estimated maximum amount received was 10.72mSv, which amounts to 21% of the annual exposure limit for a radiation worker. Detailed information regarding radiation exposure for this study is provided in [9].
In conclusion, static-rotation was strongly correlated with rotation measured during dynamic activities, which indicated that the static position may be used cautiously to express the neutral rotational position of the femur for dynamic movements. Furthermore, hip rotation was positively correlated with femoral anteversion in both the static position and during gait, which indicated femoral anteversion is compensated for by altering hip rotation. As such, we believe proximal femoral rotation, which considers both anteversion and hip rotation, should be considered when interpreting hip kinematics, especially when planning for surgical procedures that alter femoral anteversion.
Supplementary Material
Figure S-1: Hip rotation measured during gait (a) and the relationship between the mean hip rotation during gait and as measured during standing (b). Angles are measured using the coordinates recommended by the International Society of Biomechanics. Hip rotation was averaged across subjects over the time-normalized gait cycle (a), and indicated that hip rotation (solid black line) was maximized at 13% gait and minimized at 56% gait (vertical dotted lines). The 95% confidence interval of hip rotation is shown (gray lines). The mean gait rotation was positively correlated with hip rotation in static (static-rotation) (b).
Figure S-2: Correlation plots indicating the strength of the relationship between hip rotation measured during standing (static-rotation) and hip rotation measured during pivoting. Angles are measured using the coordinates recommended by the International Society of Biomechanics. The maximum rotation (max-rotation) occurred during internal rotation pivot (top, solid gray circles). The minimum rotation (min-rotation) occurred during external rotation (bottom, solid black circles). The correlation between the average of the max- and min-rotation (mid-pivot rotation) and static-rotation is also shown (middle, open circles).
Acknowledgments
Financial support was provided by the National Institutes of Health (NIH) (R21-AR063844, R21-AR069773, F32-AR067075, S10-RR026565), the LS Peery Discovery Program in Musculoskeletal Restoration, the Nakatomi Foundation, and the Nakatani Foundation for Advancement of Measuring Technologies in Biomedical Engineering. The research content herein is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other foundations.
5. References
- [1].Kingsley PC, Olmsted KL, A study to determine the angle of anteversion of the neck of the femur, The Journal of bone and joint surgery. American volume 30a (1948) 745–751. [PubMed] [Google Scholar]
- [2].Nakahara I, Takao M, Sakai T, Nishii T, Yoshikawa H, Sugano N, Gender differences in 3D morphology and bony impingement of human hips, Journal of orthopaedic research : official publication of the Orthopaedic Research Society 29 (2011) 333–339. [DOI] [PubMed] [Google Scholar]
- [3].Nakahara I, Takao M, Sakai T, Miki H, Nishii T, Sugano N, Three-dimensional morphology and bony range of movement in hip joints in patients with hip dysplasia, The bone & joint journal 96-b (2014) 580–589. [DOI] [PubMed] [Google Scholar]
- [4].Widmer KH, Zurfluh B, Compliant positioning of total hip components for optimal range of motion, Journal of orthopaedic research : official publication of the Orthopaedic Research Society 22 (2004) 815–821. [DOI] [PubMed] [Google Scholar]
- [5].Radler C, Kranzl A, Manner HM, Hoglinger M, Ganger R, Grill F, Torsional profile versus gait analysis: consistency between the anatomic torsion and the resulting gait pattern in patients with rotational malalignment of the lower extremity, Gait & posture 32 (2010) 405–410. [DOI] [PubMed] [Google Scholar]
- [6].Uemura K, Takao M, Hamada H, Sakai T, Sugano N, Change in axial rotation of the femur in the resting supine position following total hip arthroplasty, Artificial Organs (2017). doi: 10.1111/aor.12998. [DOI] [PubMed] [Google Scholar]
- [7].Uemura K, Takao M, Otake Y, Koyama K, Yokota F, Hamada H, et al. , Can Anatomic Measurements of Stem Anteversion Angle Be Considered as the Functional Anteversion Angle?, The Journal of arthroplasty (2017). doi: 10.1016/j.arth.2017.09.027. [DOI] [PubMed] [Google Scholar]
- [8].Uemura K, Takao M, Sakai T, Nishii T, Sugano N, The Validity of Using the Posterior Condylar Line as a Rotational Reference for the Femur, The Journal of arthroplasty 31 (2016) 302–306. [DOI] [PubMed] [Google Scholar]
- [9].Fiorentino NM, Atkins PR, Kutschke MJ, Goebel JM, Foreman KB, Anderson AE, Soft tissue artifact causes significant errors in the calculation of joint angles and range of motion at the hip, Gait & posture 55 (2017) 184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Leardini A, Chiari L, Della Croce U, Cappozzo A, Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation, Gait & posture 21 (2005) 212–225. [DOI] [PubMed] [Google Scholar]
- [11].Bey MJ, Zauel R, Brock SK, Tashman S, Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics, Journal of biomechanical engineering 128 (2006) 604–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kapron AL, Aoki SK, Peters CL, Maas SA, Bey MJ, Zauel R, et al. , Accuracy and feasibility of dual fluoroscopy and model-based tracking to quantify in vivo hip kinematics during clinical exams, Journal of applied biomechanics 30 (2014) 461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Fiorentino NM, Kutschke MJ, Atkins PR, Foreman KB, Kapron AL, Anderson AE, Accuracy of Functional and Predictive Methods to Calculate the Hip Joint Center in Young Non-pathologic Asymptomatic Adults with Dual Fluoroscopy as a Reference Standard, Annals of biomedical engineering 44 (2016) 2168–2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kapron AL, Aoki SK, Peters CL, Anderson AE, In-vivo hip arthrokinematics during supine clinical exams: Application to the study of femoroacetabular impingement, Journal of biomechanics 48 (2015) 2879–2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fiorentino NM, Atkins PR, Kutschke MJ, Foreman KB, Anderson AE, In-vivo quantification of dynamic hip joint center errors and soft tissue artifact, Gait & posture 50 (2016) 246–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Atkins PR, Fiorentino NM, Aoki SK, Peters CL, Maak TG, Anderson AE, In Vivo Measurements of the Ischiofemoral Space in Recreationally Active Participants During Dynamic Activities: A High-Speed Dual Fluoroscopy Study, The American journal of sports medicine (2017) 363546517712990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, et al. , ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of Biomechanics, Journal of biomechanics 35 (2002) 543–548. [DOI] [PubMed] [Google Scholar]
- [18].Gose S, Sakai T, Shibata T, Murase T, Yoshikawa H, Sugamoto K, Morphometric analysis of the femur in cerebral palsy: 3-dimensional CT study, Journal of pediatric orthopedics 30 (2010) 568–574. [DOI] [PubMed] [Google Scholar]
- [19].Sugano N, Noble PC, Kamaric E, A comparison of alternative methods of measuring femoral anteversion, Journal of computer assisted tomography 22 (1998) 610–614. [DOI] [PubMed] [Google Scholar]
- [20].Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS, The morphology of the femur in developmental dysplasia of the hip, The Journal of bone and joint surgery. British volume 80 (1998) 711–719. [DOI] [PubMed] [Google Scholar]
- [21].Lausten GS, Jorgensen F, Boesen J, Measurement of anteversion of the femoral neck. Ultrasound and computerised tomography compared, The Journal of bone and joint surgery. British volume 71 (1989) 237–239. [DOI] [PubMed] [Google Scholar]
- [22].Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT, Femoral anteversion, The Journal of bone and joint surgery. American volume 69 (1987) 1169–1176. [PubMed] [Google Scholar]
- [23].Casciaro ME, Ritacco LE, Milano F, Risk M, Craiem D, Angle estimation of human femora in a three-dimensional virtual environment, Conference proceedings: ... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference 2010 (2010) 3946–3949. [DOI] [PubMed] [Google Scholar]
- [24].Lee KM, Chung CY, Sung KH, Kim TW, Lee SY, Park MS, Femoral anteversion and tibial torsion only explain 25% of variance in regression analysis of foot progression angle in children with diplegic cerebral palsy, Journal of neuroengineering and rehabilitation 10 (2013) 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Simon AL Jr., Presedo A, Ilharreborde B, Mallet C, Mazda K, Pennecot GF, Can turned inward patella predict an excess of femoral anteversion during gait in spastic diplegic children?, Journal of pediatric orthopedics 34 (2014) 405–410. [DOI] [PubMed] [Google Scholar]
- [26].Arnold AS, Komattu AV, Delp SL, Internal rotation gait: a compensatory mechanism to restore abduction capacity decreased by bone deformity, Developmental medicine and child neurology 39 (1997) 40–44. [DOI] [PubMed] [Google Scholar]
- [27].Kumagai M, Shiba N, Higuchi F, Nishimura H, Inoue A, Functional evaluation of hip abductor muscles with use of magnetic resonance imaging, Journal of orthopaedic research : official publication of the Orthopaedic Research Society 15 (1997) 888–893. [DOI] [PubMed] [Google Scholar]
- [28].Bervet K, Bessette M, Godet L, Cretual A, KeR-EGI, a new index of gait quantification based on electromyography, Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology 23 (2013) 930–937. [DOI] [PubMed] [Google Scholar]
- [29].Khanuja HS, Vakil JJ, Goddard MS, Mont MA, Cementless femoral fixation in total hip arthroplasty, The Journal of bone and joint surgery. American volume 93 (2011) 500–509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S-1: Hip rotation measured during gait (a) and the relationship between the mean hip rotation during gait and as measured during standing (b). Angles are measured using the coordinates recommended by the International Society of Biomechanics. Hip rotation was averaged across subjects over the time-normalized gait cycle (a), and indicated that hip rotation (solid black line) was maximized at 13% gait and minimized at 56% gait (vertical dotted lines). The 95% confidence interval of hip rotation is shown (gray lines). The mean gait rotation was positively correlated with hip rotation in static (static-rotation) (b).
Figure S-2: Correlation plots indicating the strength of the relationship between hip rotation measured during standing (static-rotation) and hip rotation measured during pivoting. Angles are measured using the coordinates recommended by the International Society of Biomechanics. The maximum rotation (max-rotation) occurred during internal rotation pivot (top, solid gray circles). The minimum rotation (min-rotation) occurred during external rotation (bottom, solid black circles). The correlation between the average of the max- and min-rotation (mid-pivot rotation) and static-rotation is also shown (middle, open circles).