Abstract
Objective:
To examine the modifying effects of social support on depressive symptoms and health-related quality of life (QoL) in patients receiving coping skills training (CST).
Methods:
We considered the modifying effects of social support in the COPE-HF (Coping Effectively with Heart Failure) clinical trial, which randomized 179 heart failure (HF) patients to either 4-months of CST or usual care enhanced by HF education (HFE). CST involved training in specific coping techniques while HFE involved education about HF self-management. Social support was assessed by the ENRICHD Social Support Inventory; QoL was assessed with the Kansas City Cardiomyopathy Questionnaire (KCCQ) and depression was assessed with the Beck Depression Inventory-II (BDI-II).
Results:
Linear regression models revealed a significant intervention group by baseline social support interaction for change in KCCQ total scores (P=0.006) and BDI-II scores (P<0.001). Participants with low social support assigned to the CST intervention showed large improvements in KCCQ scores (mean: 11.2, 95% CI: 5.7 to 16.8), while low social support patients assigned to the HFE controls showed no significant change (mean: −0.8, 95% CI: −7.2 to 5.6). Similarly, BDI-II scores in participants with low social support in the CST group showed large reductions (mean: −8.7, 95% CI: −11.3 to −6.1) compared to low social support HFE participants (mean: −3.0, 95% CI: −6.0 to −0.1).
Conclusions:
HF patients with low social support benefit substantially from telephone-based CST interventions. Targeting HF patients with low social support for behavioral interventions could prove to be a cost-effective strategy for improving QoL and reducing depression.
Keywords: Heart failure, Coping skills, Depression, Quality of Life, Social support
Heart failure (HF) is a chronic disease that results in high morbidity and mortality and impaired quality of life (QoL). More than 5.7 million adults are currently living with HF in the United States, and an estimated 870,000 new cases are diagnosed each year.(Mozaffarian et al., 2015) Improvements in the treatment of patients with heart disease can reduce mortality, but also produce an increased prevalence of HF in the general population. As the prevalence of HF increases, the ability to care for the growing population of patients with HF becomes more salient, and developing strategies to help patients cope with HF is now recognized as being critically important (Braunwald, 2015; McAlister, Stewart, Ferrua, & McMurray, 2004; Sears et al., 2013).
Pharmacological interventions to treat depression and improve QoL have proven to be of limited value. (Angermann et al., 2007; O’Connor et al., 2008; O’Connor et al., 2010) Alternative therapies, on the other hand, including exercise and cognitive behavior therapy (CBT), have shown some promise (Lavie, Menezes, De Schutter, Milani, & Blumenthal, 2016). For example, in the HF-ACTION trial, exercise training was associated with modest reductions in depression and improvements in QoL. (Blumenthal et al., 2012; Flynn et al., 2009) Freedland and colleagues (Freedland, Carney, Rich, Steinmeyer, & Rubin, 2015) provided up to 6-months of intensive, weekly 1-hour CBT sessions and four 20–30 minute relapse prevention telephone contacts between 6 and 12 months, delivered by experienced therapists. Results showed reduced depression and anxiety and improved QoL at 6- and 12-months post-randomization. Similarly, Sherwood et al. (Sherwood et al., 2017) recently reported that a 4-month, telephone-delivered CBT-based coping skills intervention produced improved QoL and better health outcomes in a sample of 179 patients with class II or III HF. Compared to a control group receiving usual care enhanced by HF education, the coping skills group demonstrated significantly larger improvements in health-related QoL and increased functional capacity.
In an effort to identify individual differences in response to the coping skills intervention, the present secondary analysis of the COPE-HF trial (Sherwood et al., 2017) examined the potential modifying effects of social support on the impact of Coping Skills Training (CST) on depressive symptoms and health-related QoL. Recent evidence suggests that lower social support is common among more disadvantaged HF patients(Nordgren & Soderlund, 2017), and that greater social support is associated with better self-care behaviors in HF patients (Gallagher, Luttik, & Jaarsma, 2011; Graven & Grant, 2014). We previously have shown that social support may modify the relationship between depression and mortality in post-myocardial patients.(Lett et al., 2007) Other studies have shown that social support modifies the effects of stress on depression in college students(Wang, Cai, Qian, & Peng, 2014) and several intervention studies have examined the modifying effects of social support in cancer patients.(Helgeson, 1992; Helgeson, Cohen, Schulz, & Yasko, 1999, 2000) In a group support intervention for survivors of breast cancer, a subgroup of women who lacked social support from their partners benefitted most from peer discussion group support and women who felt that they had adequate support from their social network did not benefit and actually deteriorated over time. The purpose of this secondary analysis of the COPE-HF trial was to determine if perceived social support modifies the effects of the CST intervention on QoL and depression in HF patients. We hypothesized, a priori, that HF patients with low social support would stand to gain the most from the CST intervention designed to enhance self-care health behaviors and improve coping to reduce distress.
Methods
Overall Design:
As previously reported,(Sherwood et al., 2011) COPE-HF (Coping Effectively With Heart Failure) was a single-site randomized clinical trial in which 179 men and women with New York Heart Association Class II or III HF for at least 3 months and left ventricular ejection fraction (LVEF) ≤40% were randomized to either CBT-based coping skills training (CST) or to usual care enhanced by HF education (HFE). Participants were enrolled between September 2009 and January 2014. Details of the study methodology and results have been previously published.(Sherwood et al., 2017) (Sherwood et al., 2011) Written informed consent was provided by each participant; the protocol was approved by the Institutional Review Board (IRB) at Duke University Medical Center and the University of North Carolina at Chapel Hill.
Procedures:
Participants were randomly assigned to one of two intervention arms: Coping Skills Training (CST) or HF Education (HFE) in 1:1 ratio. CST was delivered via telephone by a trained clinical psychologist. The intervention involved 16 weekly 30-minute individual phone calls. Motivational interviewing was used to enhance adherence to prescribed self-care health behaviors such as diet, physical activity, and medication adherence. CST included training in specific coping techniques such as relaxation training, cognitive restructuring, and problem solving that have been used in our previous work with cardiac and pulmonary patients(Blumenthal et al., 2006; Blumenthal et al., 1997; Blumenthal et al., 2016). The HFE intervention also involved 16 weekly individual phone calls of ≤30-minutes duration, delivered by a physician’s assistant/health educator, which focused on HF medical issues deemed important for HF self-management without teaching behavioral skills to improve coping.
Assessment of Quality of Life:
The Kansas City Cardiomyopathy Questionnaire (KCCQ) was used to measure health-related QoL. The KCCQ is a 23-item self-administered disease-specific questionnaire.(Green, Porter, Bresnahan, & Spertus, 2000) The KCCQ is scored from 0 to 100, with higher scores representing better health QoL. We handled missing values by using the standard scoring algorithms to assign the average of the completed items when at least half of the items were answered.
Assessment of Depression:
The Beck Depression Inventory-II (BDI-II) was used to assess depression(Beck, Steer, & Brown, 1996). The BDI-II is a 21-item self-report instrument in which each item corresponds to a specific category of symptoms and attitudes. It has been shown to be both a reliable and valid measure of depression severity (Beck, Steer, & Carbin, 1988) and has been used in a number of major RCTs of cardiac patients (Berkman et al., 2003; Davidson et al., 2010; Frasure-Smith et al., 1997).
Assessment of Social Support:
We used the ENRICHD Social Support Inventory to assess functional support.(Mitchell et al., 2003) The ESSI is a 5-item instrument that was developed specifically to screen post-myocardial infarction patients for low levels of perceived support as part of the inclusion criterion for the Enhancing Recovery in Coronary Heart Disease (ENRICHD) trial(The ENRICHD investigators, 2000). The standardized coefficient alpha for the ESSI is 0.87 (Mitchell et al., 2003) and the ESSI has been shown to correlate positively with other social support instruments and negatively with measures of depression (Kiropoulos et al., 2012; Vaglio et al., 2004). As noted by Gottleib and Bergen (Gottlieb & Bergen, 2010), its brevity and strong psychometric properties commend the ESSI as an excellent screening tool for perceived social support that could be used to determine who is likely to benefit most from interventions that augment support. Participants were considered to have low social support if they obtained a score of ≤18 and scored ≤ 3 on at least 2 items.
Statistical analysis:
Analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, North Carolina). Multiple imputation (PROC MI) was used to account for post-treatment KCCQ scores and BDI-II scores missing in their entirety using Markov chain Monte Carlo simulation methods and 50 imputations. To examine the potential moderating/modifying effect of social support on the treatment effects for QoL and depression, pre-randomization baseline to post-intervention change in KCCQ scores and change in BDI-II scores were the dependent variables in separate general linear models. Social support, Intervention group, an intervention group by social support interaction term, and a set of pre-specified covariates, including age, sex, race, marital status, obesity, etiology, brain natriuretic peptide (BNP) levels and baseline KCCQ/BDI-II scores were included in the model. To further examine the effects of social support on the QoL and depression, adjusted mean change in KCCQ total scores and BDI-II scores in patients with high and low social support were calculated for each intervention group, with adjustment for all covariates. Two-way interaction terms between social support and each of the demographic variables were examined to determine if the association of social support with QoL and depression were affected by any confounders. We also conducted a set of sensitivity analyses by excluding patients with incomplete KCCQ data (n=10) and BDI-II data (n=10) at follow-up, to address the robustness of our findings. Finally, in order to determine if the intervention group by social support interaction was influenced by marital status, we conducted a sensitivity analysis of whether marital status and social support together modified treatment improvements, or whether marital status by itself modified the effects of treatment. A two-sided p value < 0.05 was considered statistically significant and all analyses followed the intent-to-treat principle.
Results
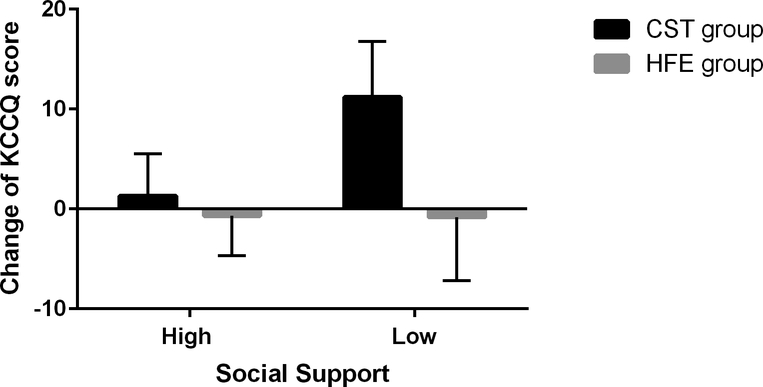
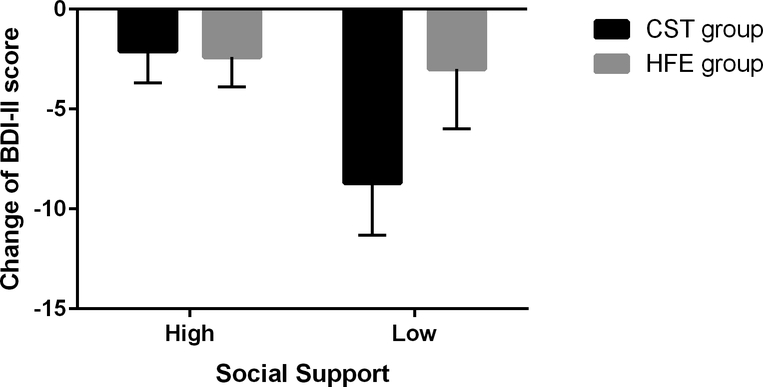
The primary results of the COPE-HF trial have been reported previously. A total of 179 patients were reported in the primary analysis; 81 patients completed the CST intervention and 89 patients completed the HFE intervention. CST participants completed an average of 14.5 (SD = 3.5) sessions and HFE participants completed an average of 15.7 (SD = 1.6) sessions. We observed no differences between patients with high and low social support on any demographic characteristic, except for marital status and ischemic cause (see Table 1). Neither marital status (P = .265) nor social support level (P = .710) was associated with intervention adherence. Results of the primary analysis revealed that the CST group exhibited significantly greater improvements in KCCQ total QoL score (P=0.009) and BDI-II score (P=0.027) compared with HFE; the CST group demonstrated an improvement of 8.3 points (95%CI: 5.0 to 11.5) compared to only 2.3 points (95% CI: −0.8 to 5.4) for HFE on the KCCQ and a reduction of 4.5 points (95%CI: −5.8 to −3.1) compared to 2.4 points (95% CI: −3.7 to −1.1) on the BDI-II for HFE controls (Sherwood et al., 2017). The interaction between baseline social support and treatment group revealed a significant intervention group by baseline social support interaction for change in KCCQ total scores (P=0.006) and BDI-II scores (P<0.001). Participants with low social support randomized to the CST intervention showed the largest improvements in KCCQ scores (Figure 1) and BDI-II scores (Figure 2) compared to the other groups. Adjusted mean change scores in the KCCQ and BDI-II, with adjusted mean differences for high and low social support by intervention group are shown in Table 2. Participants with low social support assigned to the CST intervention showed large improvements in KCCQ scores (mean: 11.2, 95% CI: 5.7 to 16.8), while low social support patients assigned to the HFE controls had no significant change (mean: −0.8, 95% CI: −7.2 to 5.6). Similarly, BDI-II scores in participants with low social support assigned to the CST group showed larger reductions (mean: −8.7, 95% CI: −11.3 to −6.1) compared to low social support HFE patients (mean: −3.0, 95% CI: −6.0 to −0.1). Comparison of patients with high social support assigned to the CST intervention and HFE controls revealed no differences in changes in KCCQ (P=0.482) or BDI-II (P=0.787). Sensitivity analyses found that results remained the same after patients with incomplete follow-up KCCQ and BDI-II data were removed from the analyses.
Table 1:
Baseline characteristics of 179 HF patients in the COPE-HF study
| Total | High social support | Low social support | p | |
|---|---|---|---|---|
| n=119 | n=60 | |||
| Age, years | 57.8 ± 11.5 | 58.3 ± 11.7 | 56.8 ± 11.2 | 0.414 |
| Men | 131 (73.2%) | 84 (70.6%) | 47 (78.3%) | 0.270 |
| Race: White | 96 (53.6%) | 67 (56.3%) | 29 (49.2%) | 0.368 |
| Married | 99 (55.3%) | 75 (63.0%) | 24 (40.0%) | 0.003 |
| Obesity | 99 (57.2%) | 63 (55.3%) | 36 (61.0%) | 0.468 |
| Ischemic cause | 72 (40.0%) | 54 (45.4%) | 18 (30.0%) | 0.048 |
| BNP* | 121.6 (52.9, 304.9) | 121.2 (53.1, 294.7) | 136.6 (50.0, 320.4) | 0.800 |
| Baseline KCCQ score | 62.1 ± 21.7 | 63.9 ± 21.6 | 58.5 ± 21.7 | 0.117 |
| Baseline BDI-II score | 13.9 ± 9.9 | 11.9 ± 9.0 | 17.9 ± 10.5 | <0.001 |
Note: Continuous variables are described as mean ± Standard Deviation or *Median (Q25, Q75) based on their distribution. Discrete variables are presented as n (%).
Figure 1:
Change in KCCQ scores in HF patients randomized to CST and HFE groups with different levels of social support. Note: n = 30 for CST low social support; n = 30 for HFE with low social support; n = 59 for CST with high support; n = 60 for HFE with high social support. SS= Social Support
Figure 2:
Change in BDI-II scores in HF patients randomized to CST and HFE groups with different levels of social support. Note: n = 30 for CST low social support; n = 30 for HFE with low social support; n = 59 for CST with high support; n = 60 for HFE with high social support. SS= Social Support
Table 2:
Change of KCCQ scores and BDI-II scores in HF patients randomized to CST and HFE group with high and low social support
| Baseline | Follow-up | Adjusted change from baseline | Adjusted difference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | SE | mean | SE | mean | 95%CI | mean | 95%CI | p | |||
| KCCQ | High social support | ||||||||||
| CST group | 59 | 67.1 | 2.8 | 68.7 | 23.5 | 1.3 | −3.0 to 5.5 | 2.0 | −3.5 to 7.4 | 0.482 | |
| HFE group | 60 | 60.7 | 2.8 | 61.1 | 22.7 | −0.7 | −4.7 to 3.3 | Ref | |||
| Low social support | |||||||||||
| CST group | 30 | 54.9 | 3.9 | 67.8 | 21.3 | 11.2 | 5.7 to 16.8 | 12.0 | 4.7 to 19.4 | 0.001 | |
| HFE group | 30 | 62.1 | 3.9 | 62.3 | 22.6 | −0.8 | −7.2 to 5.6 | Ref | |||
| BDI-II | High social support | ||||||||||
| CST group | 59 | 11.7 | 1.2 | 9.4 | 8.6 | −2.1 | −3.7 to −0.6 | 0.3 | −1.7 to 2.3 | 0.787 | |
| HFE group | 60 | 12.0 | 1.2 | 9.5 | 8.8 | −2.4 | −3.9 to −1.0 | Ref | |||
| Low social support | |||||||||||
| CST group | 30 | 19.2 | 1.9 | 10.4 | 7.9 | −8.7 | −11.3 to −6.1 | −5.7 | −9.1 to −2.3 | 0.001 | |
| HFE group | 30 | 16.6 | 1.9 | 14.7 | 12.1 | −3.0 | −6.0 to −0.1 | Ref | |||
Note: SE = standard error; CST = Coping Skills Training; HFE = Heart Failure Education
Interestingly, married participants reported greater social support compared to their unmarried counterparts (21.1± 4.4 v 17.5 ± 6.0, P < .001). However, the marital status by intervention group interaction was not significant for the KCCQ (P = 0.888) or the BDI-II (P = 0.845). Moreover, the 3-way marital status by social support by intervention group interaction also was not significant for the KCCQ (P= 0.572) and BDI-II (P = 0.603), indicating that low social support was not simply a surrogate marker for being unmarried.
Discussion
The COPE-HF trial was a successful, telephone-based CST intervention for HF patients, improving QoL and depression in HF patients. In this secondary analysis of data from the trial, social support was found to modify the effects of the intervention on QoL and depression symptom severity outcomes. The greater improvements in QoL and reductions in depression observed in the CST participants compared to HFE controls was largely attributable to the changes observed in the subset of participants who had low baseline levels of social support. Patients assigned to the CST condition who reported low social support prior to treatment were especially likely to benefit from the CST intervention. An 8-point increase in KCCQ score is considered clinically meaningful (Spertus et al., 2005), and low social support patients in the CST intervention experienced an average 13-point improvement (9.3 points adjusted), which is both statistically and clinically significant. Interestingly, the improvement in QoL observed in those patients with high social support was relatively small and non-significant, and was comparable to the minimal changes observed among participants in the HFE control group. Because the QoL of participants with high social support was high to begin with, it is possible that there was a ceiling effect in which there was little room for further improvement. The finding that the low social support participants assigned to HFE had no improvements in QoL suggests that merely providing social contact to those patients with low social support was not sufficient to improve their QoL. Teaching participants coping skills, in addition to providing support and attention, was needed to improve their QoL. Similarly, for depression, participants with low social support in the CST group achieved a 6.5-point reduction in BDI-II scores, compared to only 2.0 points among those with low social support assigned to the HFE control group.
Efforts to identify modifiers of psychosocial interventions, often in cancer patients, have generally found that patients with elevated levels of distress exhibit greater improvements compared to those with lower levels of distress or higher QoL,(Andersen et al., 2004; Carmack Taylor et al., 2007; Schneider et al., 2010) presumably because they have the most to gain from treatment. Results are not entirely consistent, however, as several studies have shown that better psychosocially adjusted patients benefit more from interventions (Doorenbos, Given, Given, & Verbitsky, 2006; Hosaka, Sugiyama, Tokuda, & Okuyama, 2000) or are at least provided some protection against depression.(Kissane et al., 2007) A meta-analysis by Schneider et al. examined whether the effects of psychosocial interventions on psychological distress in cancer patients are modified by pre-intervention distress levels.(Schneider et al., 2010) Results showed that baseline distress significantly modified intervention effects, explaining up to 50% of the between-study effect-size variance: effects on anxiety and depression were generally negligible when pre-intervention distress was low and the effects were pronounced when distress was high.
The evidence for social support, on the other hand, provides a more mixed picture. Several studies report that patients with low social support may experience greater benefit from psychosocial interventions.(Antoni et al., 2001; Scheier et al., 2007) In a RCT of men with early stage prostate cancer, Gilts et al.(Gilts, Parker, Pettaway, & Cohen, 2013) reported that men who reported low baseline social support and received two, 90-minute CBT-based stress management sessions prior to surgery had increased physical functioning one year after surgery compared to men with low social support in the standard care control group. However, the results did not employ an intent-to-treat analysis as only 89 men (56% of the sample) were included in the analysis. Also, changes in mental health QoL were not reported; physical functioning was the only outcome for which there were group differences one year after surgery. In contrast, a study of 277 patients with renal cell carcinoma randomized to either expressive writing or neutral writing conditions and followed at 1, 4, and 10 months, reported that expressive writing improved QoL outcomes for patients with high social support, but actually could be contraindicated for those with low social support.(Milbury et al., 2017) Patients who underwent expressive writing with low social support had greater sleep disturbance compared to neutral writing controls, suggesting that the provocation of negative affect in the absence of a supportive social network may be detrimental.
Few studies have examined potential modifiers of behavioral interventions in HF patients. In an analysis of treatment modifiers, Freedland et al. (Freedland et al., 2015) reported that none of the tests for effect modification were statistically significant, suggesting that efficacy of the intensive, in-person CBT sessions did not depend on sex, race, or use of non-study antidepressants. In the present study, we focused specifically on the potential modifying effects of social support on QoL among HF patients receiving telephone-delivered coping skills training. We were surprised to find that the low social support participants in the CST intervention demonstrated such a large improvement in QoL, while the high social support participants apparently experienced minimal benefit. It is possible that they reached a ceiling, and could not improve further. Alternatively, it has been suggested that patients with high social support may exhibit a paradoxical worsening of QoL with treatment, particularly as a result of interventions geared to encouraging social interactions.(Helgeson et al., 2000) However, this explanation is unlikely because the intervention was not delivered in a group context and patients received one-on-one counseling by telephone that was not designed specifically to promote interpersonal interactions, but rather was designed to enhance skills in self-care health behaviors and coping with daily stressors. Participants in the HF education control condition also received individualized attention and health information relevant to HF.
Limitations.
It is possible that because the CST intervention was delivered by a psychologist while HFE was delivered by a physician’s assistant, outcome differences attributed to the two interventions could have been affected by the differences in interventionists’ training and experience, as well as by the content of the interventions. However, a psychologist with specialized training and experience in the delivery of the CST intervention and a physician’s assistant with training in the medical management of HF were considered the best test of the differential effects of CST and HF education delivered by experienced health professionals. A more likely explanation for the intervention effects is that differences in the content and process of the interventions, rather than the personality or professional training of the interventionists, was responsible for the group differences.
Summary.
Results of this secondary analysis suggest that coping skills training for HF patients, delivered over the telephone, provides better improvements in health-related quality of life and greater reductions in depressive symptoms for those with low social support compared to those with high social support. This finding is an especially encouraging result in light of the negative findings of the SADHART-CHF and MOOD-HF antidepressant trials (Angermann et al., 2016; O’Connor et al., 2010), which showed that pharmacologic interventions were ineffective in improving QoL in HF patients. Furthermore, because HF patients often have significant physical and geographic barriers to receiving traditional mental health treatments, telehealth interventions such as the telephone-delivered CST employed in COPE-HF may be especially beneficial. Importantly, HF patients with low social support appear to benefit more substantially from treatment. Screening for low social support and then targeting those patients for more intensive psychosocial interventions could prove to be a worthwhile, cost-effective strategy for improving quality of life and reducing depressive symptoms in this vulnerable patient population.
Acknowledgments
Supported by Grant HL091920 from the National Heart, Lung and Blood Institute.
ACRONYMS
- BDI-II
Beck Depression Inventory-II
- CI
Confidence interval
- COPE-HF
Coping Effectively with Heart Failure
- CBT
Cognitive Behavior Therapy
- CST
Coping Skills Training
- ENRICHD
Enhancing Recovery in Coronary Heart Disease
- ESSI
ENRICHD Social Support Inventory
- HF
Heart failure
- HFE
Heart Failure Education
- KCCQ
Kansas City Cardiomyopathy Questionnaire
- QoL
Quality of Life
Footnotes
TRIAL REGISTRATION: Clinicaltrials.gov identifier: NCT00873418.
References
- Andersen BL, Farrar WB, Golden-Kreutz DM, Glaser R, Emery CF, Crespin TR, … Carson WE 3rd. (2004). Psychological, behavioral, and immune changes after a psychological intervention: a clinical trial. J Clin Oncol, 22(17), 3570–3580. doi: 10.1200/jco.2004.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angermann CE, Gelbrich G, Stork S, Fallgatter A, Deckert J, Faller H, & Ertl G (2007). Rationale and design of a randomised, controlled, multicenter trial investigating the effects of selective serotonin re-uptake inhibition on morbidity, mortality and mood in depressed heart failure patients (MOOD-HF). Eur J Heart Fail, 9(12), 1212–1222. doi: 10.1016/j.ejheart.2007.10.005 [DOI] [PubMed] [Google Scholar]
- Angermann CE, Gelbrich G, Stork S, Gunold H, Edelmann F, Wachter R, … Ertl G (2016). Effect of Escitalopram on All-Cause Mortality and Hospitalization in Patients With Heart Failure and Depression: The MOOD-HF Randomized Clinical Trial. Jama, 315(24), 2683–2693. doi: 10.1001/jama.2016.7635 [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, … Carver CS (2001). Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol, 20(1), 20–32. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical psychology review, 8(1), 77–100. [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, … Schneiderman N (2003). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Jama, 289(23), 3106–3116. doi: 10.1001/jama.289.23.3106 [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Keefe FJ, Davis RD, Lacaille RA, Carney RM, … Palmer SM (2006). Telephone-based coping skills training for patients awaiting lung transplantation. J Consult Clin Psychol, 74(3), 535–544. doi: 10.1037/0022-006x.74.3.535 [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, O’Connor C, Keteyian S, Landzberg J, Howlett J, … Whellan DJ (2012). Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA, 308(5), 465–474. doi: 10.1001/jama.2012.8720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, Coleman RE, … Morris JJ (1997). Stress management and exercise training in cardiac patients with myocardial ischemia. Effects on prognosis and evaluation of mechanisms. Arch Intern Med, 157(19), 2213–2223. [PubMed] [Google Scholar]
- Blumenthal JA, Sherwood A, Smith PJ, Watkins L, Mabe S, Kraus WE, … Hinderliter A (2016). Enhancing Cardiac Rehabilitation With Stress Management Training: A Randomized, Clinical Efficacy Trial. Circulation, 133(14), 1341–1350. doi: 10.1161/circulationaha.115.018926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braunwald E (2015). The war against heart failure: the Lancet lecture. Lancet, 385(9970), 812–824. doi: 10.1016/s0140-6736(14)61889-4 [DOI] [PubMed] [Google Scholar]
- Carmack Taylor CL, de Moor C, Basen-Engquist K, Smith MA, Dunn AL, Badr H, … Gritz ER (2007). Moderator analyses of participants in the Active for Life after cancer trial: implications for physical activity group intervention studies. Ann Behav Med, 33(1), 99–104. doi: 10.1207/s15324796abm3301_11 [DOI] [PubMed] [Google Scholar]
- Davidson KW, Rieckmann N, Clemow L, Schwartz JE, Shimbo D, Medina V, … Burg MM (2010). Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch Intern Med, 170(7), 600–608. doi: 10.1001/archinternmed.2010.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doorenbos A, Given B, Given C, & Verbitsky N (2006). Physical functioning: effect of behavioral intervention for symptoms among individuals with cancer. Nurs Res, 55(3), 161–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, … Weinfurt KP (2009). Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. Jama, 301(14), 1451–1459. doi: 10.1001/jama.2009.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Prince RH, Verrier P, Garber RA, Juneau M, … Bourassa MG (1997). Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet, 350(9076), 473–479. doi: 10.1016/s0140-6736(97)02142-9 [DOI] [PubMed] [Google Scholar]
- Freedland KE, Carney RM, Rich MW, Steinmeyer BC, & Rubin EH (2015). Cognitive Behavior Therapy for Depression and Self-Care in Heart Failure Patients: A Randomized Clinical Trial. JAMA Intern Med, 175(11), 1773–1782. doi: 10.1001/jamainternmed.2015.5220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher R, Luttik ML, & Jaarsma T (2011). Social support and self-care in heart failure. J Cardiovasc Nurs, 26(6), 439–445. doi: 10.1097/JCN.0b013e31820984e1 [DOI] [PubMed] [Google Scholar]
- Gilts CD, Parker PA, Pettaway CA, & Cohen L (2013). Psychosocial moderators of presurgical stress management for men undergoing radical prostatectomy. Health Psychol, 32(12), 1218–1226. doi: 10.1037/a0030189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb BH, & Bergen AE (2010). Social support concepts and measures. J Psychosom Res, 69(5), 511–520. doi: 10.1016/j.jpsychores.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Graven LJ, & Grant JS (2014). Social support and self-care behaviors in individuals with heart failure: an integrative review. Int J Nurs Stud, 51(2), 320–333. doi: 10.1016/j.ijnurstu.2013.06.013 [DOI] [PubMed] [Google Scholar]
- Green CP, Porter CB, Bresnahan DR, & Spertus JA (2000). Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol, 35(5), 1245–1255. [DOI] [PubMed] [Google Scholar]
- Helgeson VS (1992). Moderators of the relation between perceived control and adjustment to chronic illness. J Pers Soc Psychol, 63(4), 656–666. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S, Schulz R, & Yasko J (1999). Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatry, 56(4), 340–347. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S, Schulz R, & Yasko J (2000). Group support interventions for women with breast cancer: who benefits from what? Health Psychol, 19(2), 107–114. [DOI] [PubMed] [Google Scholar]
- Hosaka T, Sugiyama Y, Tokuda Y, & Okuyama T (2000). Persistent effects of a structured psychiatric intervention on breast cancer patients’ emotions. Psychiatry Clin Neurosci, 54(5), 559–563. doi: 10.1046/j.1440-1819.2000.00753.x [DOI] [PubMed] [Google Scholar]
- Kiropoulos LA, Meredith I, Tonkin A, Clarke D, Antonis P, & Plunkett J (2012). Psychometric properties of the cardiac depression scale in patients with coronary heart disease. BMC Psychiatry, 12, 216. doi: 10.1186/1471-244x-12-216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissane DW, Grabsch B, Clarke DM, Smith GC, Love AW, Bloch S, … Li Y (2007). Supportive-expressive group therapy for women with metastatic breast cancer: survival and psychosocial outcome from a randomized controlled trial. Psychooncology, 16(4), 277–286. doi: 10.1002/pon.1185 [DOI] [PubMed] [Google Scholar]
- Lavie CJ, Menezes AR, De Schutter A, Milani RV, & Blumenthal JA (2016). Impact of Cardiac Rehabilitation and Exercise Training on Psychological Risk Factors and Subsequent Prognosis in Patients With Cardiovascular Disease. Can J Cardiol, 32(10 Suppl 2), S365–s373. doi: 10.1016/j.cjca.2016.07.508 [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Catellier DJ, Carney RM, Berkman LF, … Schneiderman N (2007). Social support and prognosis in patients at increased psychosocial risk recovering from myocardial infarction. Health Psychol, 26(4), 418–427. doi: 10.1037/0278-6133.26.4.418 [DOI] [PubMed] [Google Scholar]
- McAlister FA, Stewart S, Ferrua S, & McMurray JJ (2004). Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol, 44(4), 810–819. doi: 10.1016/j.jacc.2004.05.055 [DOI] [PubMed] [Google Scholar]
- Milbury K, Lopez G, Spelman A, Wood C, Matin SF, Tannir NM, … Cohen L (2017). Examination of moderators of expressive writing in patients with renal cell carcinoma: the role of depression and social support. Psychooncology, 26(9), 1361–1368. doi: 10.1002/pon.4148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, … Berkman LF (2003). A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil, 23(6), 398–403. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, … Turner MB (2015). Heart disease and stroke statistics−-2015 update: a report from the American Heart Association. Circulation, 131(4), e29–322. doi: 10.1161/cir.0000000000000152 [DOI] [PubMed] [Google Scholar]
- Nordgren L, & Soderlund A (2017). Received and needed social support in relation to sociodemographic and socio-economic factors in a population of people on sick leave due to heart failure. ESC Heart Fail, 4(1), 46–55. doi: 10.1002/ehf2.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor CM, Jiang W, Kuchibhatla M, Mehta RH, Clary GL, Cuffe MS, … Krishnan RR (2008). Antidepressant use, depression, and survival in patients with heart failure. Arch Intern Med, 168(20), 2232–2237. doi: 10.1001/archinte.168.20.2232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, … Krishnan R (2010). Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol, 56(9), 692–699. doi: 10.1016/j.jacc.2010.03.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, Helgeson VS, Schulz R, Colvin S, Berga SL, Knapp J, & Gerszten K (2007). Moderators of interventions designed to enhance physical and psychological functioning among younger women with early-stage breast cancer. J Clin Oncol, 25(36), 5710–5714. doi: 10.1200/jco.2007.11.7093 [DOI] [PubMed] [Google Scholar]
- Schneider S, Moyer A, Knapp-Oliver S, Sohl S, Cannella D, & Targhetta V (2010). Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med, 33(1), 1–14. doi: 10.1007/s10865-009-9227-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears SF, Woodrow L, Cutitta K, Ford J, Shea JB, & Cahill J (2013). A patient’s guide to living confidently with chronic heart failure. Circulation, 127(13), e525–e528. [DOI] [PubMed] [Google Scholar]
- Sherwood A, Blumenthal JA, Koch GG, Hoffman BM, Watkins LL, Smith PJ, … Hinderliter AL (2017). Effects of Coping Skills Training on Quality of Life, Disease Biomarkers, and Clinical Outcomes in Patients With Heart Failure: A Randomized Clinical Trial. Circ Heart Fail, 10(1). doi: 10.1161/circheartfailure.116.003410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood A, O’Connor CM, Routledge FS, Hinderliter AL, Watkins LL, Babyak MA, … Blumenthal JA (2011). Coping effectively with heart failure (COPE-HF): design and rationale of a telephone-based coping skills intervention. J Card Fail, 17(3), 201–207. doi: 10.1016/j.cardfail.2010.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spertus J, Peterson E, Conard MW, Heidenreich PA, Krumholz HM, Jones P, … Rumsfeld JS (2005). Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J, 150(4), 707–715. doi: 10.1016/j.ahj.2004.12.010 [DOI] [PubMed] [Google Scholar]
- The ENRICHD investigators. (2000). Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J, 139(1 Pt 1), 1–9. [DOI] [PubMed] [Google Scholar]
- Vaglio J Jr., Conard M, Poston WS, O’Keefe J, Haddock CK, House J, & Spertus JA (2004). Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual Life Outcomes, 2, 24. doi: 10.1186/1477-7525-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Cai L, Qian J, & Peng J (2014). Social support moderates stress effects on depression. Int J Ment Health Syst, 8(1), 41. doi: 10.1186/1752-4458-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]