Abstract
Objectives:
Eighteen years ago, the Institute of Medicine estimated that medical errors in hospital were a major cause of mortality. Since that time reducing patient harm and improving the culture of patient safety have been national health care priorities. The study objective was to describe the current state of patient safety in pediatric acute care settings, and to assess whether modifiable features of organizations are associated with better safety culture.
Methods:
An observational cross-sectional study used 2015-2016 survey data on 177 hospitals in four U.S. states, including pediatric care in general hospitals and freestanding children’s hospitals. Pediatric registered nurses providing direct patient care assessed hospital safety and the clinical work environment. Safety was measured by items from the Agency for Healthcare Reseach and Quality’s Culture of Patient Safety survey. Hospital clinical work environment was measured by the National Quality Forum endorsed Practice Environment Scale.
Results:
A total of 1,875 pediatric nurses provided an assessment of safety in their hospitals. Sixty percent of pediatric nurses gave their hospitals less than an excellent grade on patient safety; significant variation across hospitals was observed. In the average hospital, 46% of nurses report that mistakes are held against them and 28% do not feel safe questioning authority regarding unsafe practices. Hospitals with better clinical work environments received better patient safety grades.
Conclusions:
The culture of patient safety varies across U.S. hospital pediatric settings. In better clinical work environments nurses report more positive safety culture and higher safety grades.
Through an analysis of clinician-reported safety, this study suggests that improving the clinical work environment may promote patient safety in the pediatric setting.
Introduction
Shortfalls in healthcare safety cause significant harm to patients and are associated with high costs.1,2 It has been 18 years since the Institute of Medicine’s landmark study To Err Is Human1 issued a challenge to hospitals to eliminate medical errors and improve patient safety.3–5 Hospitalized children are particularly vulnerable to serious harm in medical settings, with errors estimated to occur as frequently as 1 per 6.8 admissions.1 This paper provides an assessment of safety in today’s acute pediatric inpatient care settings, and examines whether an association between clinical practice environments of health professionals and a culture of patient safety exists.
Medication errors are the most frequent medical error identified in pediatrics6 and are ten times more likely to occur in children than in adults.7 Because of immature organ function and physiology, children may lack the capacity to buffer the harmful effects of medication errors.1 Clinical deterioration in children is also difficult to detect,8–10 and some children are unable or reluctant to report symptoms. A recent review of patient safety event prevalence in 5.7 million pediatric patient discharges identified a high occurrence of safety events, specifically in failure to rescue, postoperative sepsis, decubitus ulcers, postoperative respiratory failure, and obstetric trauma, creating an estimated >$1 billion in preventable costs.11 Distractions and interruptions, inadequate nurse to patient ratios, and multiple medications per patient contributed most to medications errors.6,7
The Agency for Healthcare Research and Quality (AHRQ), as part of the national commitment to improve patient safety1, developed survey-based measures12 of the culture of patient safety that embrace principles to reduce patient harm, such as near-miss reporting and blame-free error reporting, to improve communications among health professionals, and foster a commitment to learning from each mistake to eliminate future patient harm.
Concurrent with the emphasis on patient safety culture, a separate research literature developed documenting the important association of hospital work environments with better patient outcomes for both hospitalized adults and children. This line of research led to the adoption by the National Quality Forum of the Practice Environment Scale as a validated indicator of quality.13,14 The Practice Environment Scale measures staffing and resource adequacy, collaboration and respect between nurses and physicians, supportive and capable leadership, clinical excellence recognized and supported by hospital administration, clinician participation in hospital policy and administrative decisions, investment in staff education, and an institutional commitment to quality.15 In adult care, these organizational traits are associated with multiple clinical, patient, and organizational outcomes, including patient safety.16,17 Clinical work environment scores explained half of the variance in a study of patient safety climate in adult acute care settings.18
Limited evidence in pediatrics supports the relationship between the work environment and safety. An association between better work environments and higher ratings of safety was reported in neonatal intensive care units.5 Nursing care is missed less frequently in better pediatric hospital environments.19 Previous research has shown that nurse staffing and the work environment are better in freestanding children’s hospitals20 as compared to pediatric units in general hospitals. . No studies have linked the clincial work environment to patient safety in pediatrics. This study addresses this knowledge gap. This study had two purposes. The first was to describe the characteristics of pediatric nurses and hospitals with pediatric services, their clinical work environment, and associated safety outcomes. The second was to examine whether and to what extent hospitals with favorable work environments have higher patient safety ratings from pediatric nurses.
Methods
Design, Data, and Sample
This is a cross-sectional study in which nurse survey data are used to measure the key variables. This is a study about hospitals that uses nurses that work in those hospitals as informants about patient safety culture and other measures. Nurse reports have been demonstrated to be valid predictors of patient outcomes in prior research.5,21–26 Nurses were surveyed at their home addresses and asked to provide the name of their employer to construct hospital level measures of safety grade, culture of patient safety, and clinical work environment. Nurses were selected as informants because of their constancy in pediatric acute care settings, their proximity to patients, other staff, and physicians, and the direct impact of management decisions on their practices. While nurses are the participants in the research, the focus of the study is patient safety in hospitals, namely pediatric acute care settings, as detailed in previous publications.5,27 This design minimizes response bias at the hospital level, which is the major validity threat to studies of institutional performance.
A 30% random sample of licensed registered nurses in California, Florida, New Jersey and Pennsylvania were surveyed for the study Panel Study of Effects of Changes in Nursing on Patient Outcomes (NINR R01-NR014855). The study was led by Dr. Linda Aiken at the University of Pennsylvania School of Nursing Center for Health Outcomes and Policy Research. The purpose of the study was to collect information on nurse staffing, education, skill mix, work environment, and other organizational factors to study the relationships of such elements to patient outcomes across a large number of health care organizations, including hospitals. These four states were selected because they are among the largest in the country and account for over 20 percent of hospital admissions in the US. Using a modified Dillman28 approach, a 26.4% response rate was achieved. The total population of respondents included 59,972 nurses. While the response rate of the nurses was lower than desired the focus in the study design was to have enough randomly selected respondents in study hospitals to generate reliable estimates of the hospital level measures of interest. Nevertheless, a survey of a random subsample of 1,400 non-responders achieved an 87% response rate and when compared to the hospital level measures of interest in the primary survey results, no response bias in these measures was revealed.29 For this study on pediatric hospitals, responses from 1,875 registered nurses (RN’s) working in direct patient care in acute pediatric settings, including neonatal intensive care, pediatric intensive, care and general pediatrics were used. Responses from these acute care pediatric nurses allowed for the analysis of a total of 177 hospitals, including general acute hospitals with pediatric units and freestanding children’s hospitals. Institutional review board approval was granted by the University of Pennsylvania.
Measures
The hospital work environment was measured using the Practice Environment Scale of the Nursing Work Index (PES-NWI), a psychometrically valid measurement tool 15 endorsed by the National Quality Forum.30 The PES-NWI consists of 31 organizational traits associated with professional nursing practice. Five work environment domains are present: 1) Nurse Participation in Hospital Affairs, 2) Nursing Foundations for Quality of Care, 3) Nurse Manager Ability, Leadership, and Support of Nurses, 4) Staffing and Resource Adequacy and 5) Collegial Nurse-Physician Relations. Nurses are asked to what extent the traits are present in their current job and respond on a 4-point Likert scale.15 Nurse agreement that traits are present corresponds with higher scores. Reliability of aggregate scores was established by calculating intra-class correlation coefficients for each subscale and composite. The intraclass correlation coefficient ([1,k]) should be at least 0.6 in order to justify use of a composite score.31Values greater than 0.6 are consistent with sufficient reliability of the hospital mean. 31,32 We used responses from at least 3 nurses from each hospital. The intraclass correlation coefficient of each of the five subscales exceeded the minimum criterion. Hospitals were classified into better, mixed, and poor work environments corresponding to the top 25%, middle 50%, and bottom 25% of the composite score distribution.
The nurse survey includes selected items from the Agency for Healthcare Research and Quality Hospital Survey on Patient Safety Culture.33 Three categories, including safety climate, handoff communication, and actions related to safety were created from seven existing safety-indicator items. Nurses responded to statements such as, “staff feels free to question the decision or actions of those in authority” or “we are given feedback about changes put into place based on event reports.” Safety-related items are measured on a 5-point Likert scale from strongly agree to strongly disagree. Nurses were asked to provide an overall grade on patient safety in their current practice setting, ranging across five levels from “A” for excellent to “F” for failing. We calculated the percentage of nurses in each hospital that rated safety as B, C, D, or F, i.e., less than excellent. Then we collapsed safety grade to a dichotomous variable with grades of C, D, and F representing “poor” scores. Although technically C grades are defined as acceptable, we do not believe that the public would view a C as desirable for safety. We calculated the percentage of nurses in each hospital that rated safety as poor.
We control in our analysis for organizational characteristics of hospitals that may be associated with measures of safety as we are primarily interested in modifiable features of hospitals that may hold promise for improving safety. Hospital characteristics including bed size, teaching, and technology status were obtained from the 2015 American Hospital Association Annual Survey.34 These characteristics are used to describe the sample and are also used as controls in the regression model. Hospital bed size includes all hospital beds and is categorized into two levels 100-249 beds and greater than 250 beds. Teaching status was classified into the following three categories, major, minor and non-teaching based on the resident to bed ratio. High technology status refers to hospitals that perform pediatric heart surgery, the only pediatric specific high technology designation from the American Hospital Association Survey. Hospital type was classified as general hospitals with pediatric services and children’s hospitals based on the hospital’s pediatric-specific leadership structure and status as listed in the Children’s Hospital Association website in 2016.
The characteristics of the pediatric nurses and hospitals, the hospital safety outcomes, and the clinical work environment are described. The percentage of nurses reporting patient safety concerns across different work environment categories was calculated and graphed. Parameters in the data are symmetrically distributed, so means and standard deviation are reported. Linear regression models were used after model assumptions, linearity, independence, normality and equal variance, were satisfied. The hospital work environment was the primary predictor in a linear regression of the percentage of nurses who rated safety as poor. The regression controlled for hospital size, teaching status, and technology level.
Results
There was a total of 1,875 pediatric nurses in 177 hospitals. The typical hospital was large with a minor teaching status (Table 1). The average number of registered nurse respondents per hospital was 11 (range: 3 – 137). The majority of nurses (70%) had a Bachelor of Science degree in nursing (BSN) or higher. Almost half (48%) held a national specialty certification. The majority of pediatric nurses in this sample (61%) worked in intensive care units with 39% practicing on general medical and surgical pediatric units.
Table 1.
Characteristics of Sample Hospitals and Nurses
| Variable | n | No. (%) | Mean (SD) |
|---|---|---|---|
| Hospital characteristic | |||
| Bed Size | 174 | ||
| 100-249 beds | 25 (14.4) | ||
| ≥ 250 beds | 149 (85.6) | ||
| Teaching hospital | 170 | ||
| Major | 40 (23.4) | ||
| Minor | 76 (44.4) | ||
| Non | 54 (32) | ||
| High technology - Pediatric | 177 | 34(19%) | |
| Children’s hospital type | 177 | ||
| General | 159 (90) | ||
| Freestanding | 17 (9.6) | ||
| State | 177 | ||
| California | 79 (44.6) | ||
| Pennsylvania | 31 (17.5) | ||
| Florida | 43 (24.3) | ||
| New Jersey | 24 (13.6) | ||
| Nurse Characteristics | 1875 | ||
| Female | 1809 (96.7) | ||
| Age | 46 (12.3) | ||
| BSN or higher degree in nursing | 1866 | 1296 (69.5) | |
| Years of Experience | |||
| As an RN | 1869 | 20.1 (12.7) | |
| In present hospital | 1842 | 14.4 (10.9) | |
| National specialty certification | 1865 | 889 (47.7) | |
| Type of Unit | 1875 | ||
| General pediatric | 729 (39.0) | ||
| PICU | 240 (12.8) | ||
| NICU | 903 (48.2) |
Abbreviations: BSN Bachelor of Science in Nursing; PICU pediatric intensive care unit; NICU neonatal intensive care unit
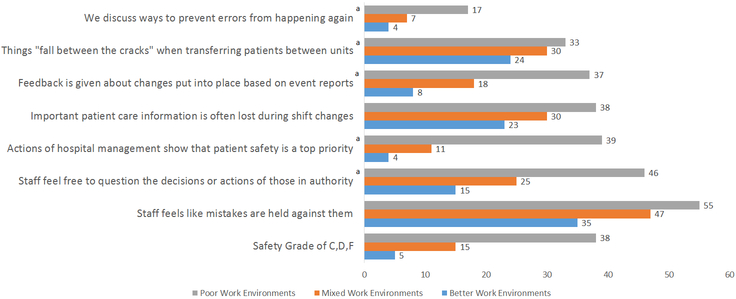
Sixty percent of pediatric nurses gave their hospitals less than an excellent grade on patient safety. Hospital-level descriptive statistics on the safety grade and safety culture measures are reported in Table 2. On average, 19 percent of pediatric nurses rated safety in their hospitals as poor (C, D, or F). Variation in poor safety ratings across hospitals is demonstrated in Figure 1. Thirty six percent or 63 hospitals had no nurses rating safety as poor and they are represented at the far left on the graph. Among hospitals that had poor safety ratings by any nurses, the percentage of nurses that rated their hospital poor ranged from approximately 20% to nearly 100%. The freestanding children’s hospitals are distributed throughout the range.
Table 2.
Pediatric Nurses’ Reports About Safety (N=177 hospitals)
| Mean(SD) | |
|---|---|
| Safety grade C, D, or F | 18.5% (21) |
| Safety Climate | |
| Staff feel free to question the decisions or actions of those in authority.a | 28.3% (24) |
| Staff feels like mistakes are held against them. | 45.8% (27) |
| Communication | |
| Important patient care information is often lost during shift changes. | 30.5% (22) |
| Things “fall between the cracks” when transferring patients from one unit to another.a | 29.3% (23) |
| Action | |
| In this unit, we discuss ways to prevent errors from happening again.a | 8.9% (15) |
| We are given feedback about changes put into place based on event reports.a | 20.8% (22) |
| The actions of hospital management show that patient safety is a top priority.a | 16.1% (21) |
Indicates the item is reverse coded such that agree and strongly agree are negative, that is, undesirable responses.
Figure 1. Percentage of Nurses by Hospital that Graded Safety as Poor.
Methods: This figure provides descriptive statistics on the percentage of hospital nurses (n=1875 nurses) in each hospital (n=177 hospitals) that graded safety as poor (i.e. a C, D, or F overall safety grade). Hospitals were categorized into children’s hospitals (blue bars), or general hospitals with pediatric services (grey bars). Results: Thirty six percent (n=63) of hospitals had zero pediatric nurses rating safety as poor, and 64% (n=114) had some percentage of nurses rating safety as poor. The variation was 20%-100% of nurses responding. Children’s hospitals are distributed throughout the range, with only one containing zero nurses reporting a poor safety grade.
Results for the safety item statements are presented in Table 2. In regards to safety climate, 28% of pediatric nurses reported not feeling free to question authority, and 46% felt that mistakes are held against them. Close to a third (31%) of nurses indicated that important care information is lost at shift changes, and a similar percentage (30%) agreed that things fall between the cracks when patients are transferred. Regarding the actions of leadership, only 9% reported that error prevention is not discussed in their unit. Less than one-fifth (16%) reported that hospital management’s actions show that safety is a not a priority. About one-fifth of nurses (21%) say they do not receive feedback about changes implemented based on event reports. Overall, reports of safety culture exhibited substantial variation across hospitals. The greatest variation was evident in “Staff feel like mistakes are held against them” and ““Staff feel free to question the decisions or actions of those in authority” and the least for “in this unit, we do not discuss ways to prevent errors from happening again.”
The clinical work environment composite and domain scores of acute inpatient pediatric care settings studied are presented in Table 3. The composite score for the PES-NWI across all pediatric settings studied was 3.00, equivalent to the response category “agree,” but ranged from 1.77 (disagree) to 4 (strongly agree). Hospitals in the bottom quartile of composite scores (worst clinical environments), representing 44 hospitals, had average PES-NWI scores of 2.55 score with the worst hospital scoring 1.77. The two domains with the lowest (worst) rating were leadership capability and nurse participation in hospital affairs. The highest rated domains were collegial relationships between physicians and nurses and hospital recognition of nursing’s contribution to quality care.
Table 3.
Work Environment of Pediatric Hospital Nurses: Mean Ratings for Practice Environment Scale of Nursing Work Index (PES-NWI) Composite and Subscales (N=177)
| Variable | Mean (SD) | Range Min – Max |
|
|---|---|---|---|
| PES-NWI composite | 3.00 (0.38) | 1.77 | 4 |
| Nurse Participation in Hospital Affairs | 2.85 (0.46) | 1.48 | 4 |
| Nursing Foundations for Quality of Care | 3.19 (0.34) | 2.03 | 4 |
| Nurse Manager Ability, Leadership, and Support of Nurses | 2.83 (0.5) | 1.44 | 4 |
| Staffing and Resource Adequacy | 2.88 (0.47) | 1.25 | 4 |
| Collegial Nurse-Physician Relations | 3.24 (0.38) | 1.56 | 4 |
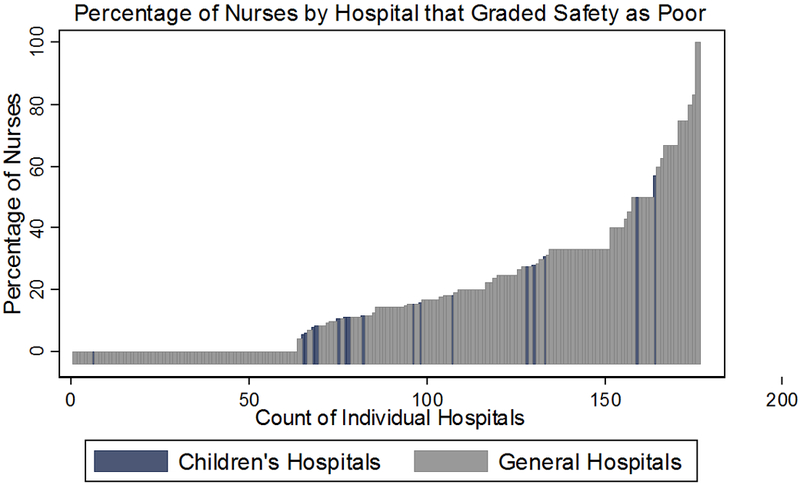
Significant variation was demonstrated in the patient safety measures across the clinical work environment categories (Figure 2). In hospitals rated as having poor clinical work environments 39% of nurses reported a poor safety grade. In contrast, only 5% of nurses in hospitals with the best clinical work environments reported poor safety grades. In hospitals rated by nurses as good on some clinical environment dimensions but not good on others, that is hospitals falling in the middle 50% of composite scores, 15% received poor patient safety scores. In the best work environments only 4% of nurses report that safety is not a priority by hospital leadership compared to 39% of nurses in poor work environments. This contrast is also evident in “staff feel that mistakes are held against them”; in the best work environments 15% of nurses report this concern, which increases to 46% in hospitals with poor work environments.
Figure 2. Percentage of Nurses Reporting Patient Safety by Work Environment Categories.
Methods: This figure presents pediatric nurse ratings (n=1875) of the specific PES-NWI survey items that relate to safety culture (n=7 statements, and the overall safety grade) and the quality of their clinical work environment. The work environment is categorized into poor, mixed, and best corresponding to the top 25%, middle 50%, and bottom 25% of the composite score distribution in the sample. Some items, (noted with an “a”) indicate that the statements were reverse coded such that agree and strongly agree are negative (undesirable) responses. Results: There was significant variation in safety culture responses across the work environment categories. In hospitals with better work environments, nurses are consistently more likely to report the presence of favorable safety-related actions in their workplace as compared with those in poor environments. The nurse responses to the individual safety culture-related statements follow the same general pattern as overall safety grade by work environment quality.
a Indicates the item is reverse recoded such that agree and strongly agree are negative, that is, undesirable responses
Table 4 further explores the association of clinical work environment with patient safety grade. The unadjusted linear regression and an adjusted model controlling for hospital characteristics yielded identical results; only the adjusted model results are reported in text. Hospitals with the best (top quartile) and mixed (middle 50%) work environments had significantly lower percentages of nurses who rated safety poorly. The coefficient for the top quartile hospitals of −34 (CI:−41.1- −26.9, p < 0.001) indicates that 34 percent fewer nurses in hospitals with better clinical work environments rated safety poorly than in the hospitals with poor work environments. In mixed work environments, 24 percent (CI: −29.5 - −17.2, p < 0.001) fewer nurses rated safety poorly compared with those in the hospitals with poor work environments.
Table 4.
Regression Results: The Percent of Nurses who graded Safety as Poora by Work Environment Category (n=177)
| Coefficient (95% CI) Unadjusted Model |
Coefficient (95% CI) Adjusted Modelb |
|
|---|---|---|
| Best Environments | −34.04c (−41.13 - −26.94) | −34.77c (−42.11- −27.42) |
| Mixed Environments | −23.36c (−29.50 - −17.21) | −24.03c (−30.48 - −17.58) |
| Poor Environments | reference | reference |
Poor is defined as ratings of fair, poor or failing
Adjusted model controls for hospital size, teaching status and technology status
p=0.000
Discussion
We determined that the work environment is significantly related to safety culture in pediatric care settings, which addresses a critical gap in our understanding of safety culture in pediatrics. Two previous studies have examined the relationship between the clinical work environment and how nurses grade the safety of their units or hospitals. In one study, nurses in U.S. and European hospitals with better work environments were half as likely to give their hospitals a poor or failing safety grade.35 Similarly, nurses in neonatal intensive care units with better work environments had lower odds of reporting a fair or poor grade for patient safety.5 Consistent with these previous results, our contemporary study further suggests that the improvements in the culture of patient safety recommended by the Institute of Medicine 18 years ago have not yet been fully realized in acute inpatient pediatric settings. According to the AHRQ, a “culture of patient safety” encompasses 4 key features; acknowledging inherent safety risks, establishing a blame-free environment where individuals can report errors, encouraging collaboration, and committing resources to address safety concerns.36 While several of our survey responses suggest that attention to children’s safety is occurring in hospitals, the survey responses describing a culture of patient safety vary greatly by hospital, with the work environment explaining much of the variation..
While there is room for improvement in all dimensions of patient safety culture in pediatric inpatient settings, deficits in two foundational principles of harm prevention are particularly troubling and need immediate attention. First, 46% of nurses report that mistakes are held against them in direct opposition to the “blame free” climate AHRQ suggests36 is necessary to prevent harm. Humans are fallible, and blaming individuals discourages timely reporting of errors and near misses so that interventions can be quickly implemented to minimize patient harm. “Just culture,” or the act of individuals reporting their own errors in an effort to facilitate learning by the system and others,37 is supported by AHRQ as a means to improve safety, and holding mistakes against individual clinicians reduces the chances of institutional learning about error prevention, a tenet of just culture. Second, more than a quarter of nurses (28%) do not feel free to question the decisions or actions of those in authority, a foundational requirement of safety in every sector, not only in health care.
Further, our study points to the need for a broader set of actions beyond the focus of most hospital safety initiatives. We find that the quality of clinical work environments, as defined by appropriate staffing, good doctor-nurse relations, effective clinical nurse managers, institutional managerial commitment to address problems in patient care, investments in continuing education of clinical staff, and evidence of an institutional commitment to patient safety and quality improvement, are associated with the extent to which hospitals have operationalized a culture of patient safety.36
Specifically, we show that hospital safety grade is significantly related to the quality of the overall clinical work environment in pediatrics. In the hospitals with the worst clinical work environments, 39% of nurses gave their clinical site a poor patient safety grade. In hospitals with poor work environments, significantly more nurses feel mistakes are held against them and do not feel empowered to question the decisions of those in authority. We also show safety-related communication is not what it should be. One-third of nurses report that important patient care information is lost both during shift changes and when patients are transferred between units.
Our results suggest that education about safety and attention to safety-related concerns is not enough to achieve a culture of patient safety. In other words, good clinical work environments may be a prerequisite for a culture of patient safety. Specific patient safety initiatives such as checklists, care bundles for prevention of central line infections, 38 and rapid response teams have likely been superimposed over dysfunctional clinical work environments, which may undermine the effectiveness of these interventions in actual practice. Our results suggest that broader attention to improving clinical work environments will also likely have a significant payoff in improving the culture of patient safety as well as gaining the full benefit of specific patient safety interventions shown to be effective under controlled conditions but currently not as effective under usual practice conditions.
The cross-sectional design does not determine a causal relationship between the work environment and safety grade. Our analysis accounted for hospital characteristics including size, technology and teaching status yet there is potential that important variables were omitted from the analysis. We used key informants to evaluate safety in hospitals rather than direct measures of safety on the basis of previous research showing that nurse reported quality is significantly associated with independent measures of patient outcomes.39,40
Conclusion
The development of a culture of patient safety in acute inpatient pediatric settings has not been uniformly achieved, and is seriously deficient in many institutions, risking harm to vulnerable children. Improvingclinical work environments in hospitals holds promise for achieving a culture of patient safety that increases the reliability of care and prevents harm.
What’s Known on This Subject
Safety events occur in hospitalized children as often as one event every seven admissions. Research has demonstrated that the work environment for clinicians is associated with better patient outcomes, but its association with pediatric patient safety is unclear.
What This Study Adds
Safety varies considerably across acute pediatric settings. Hospitals with poor work environments have poorer safety. Improving clinical work environments holds promise for achieving a culture of patient safety that increases the reliability of care and prevents harm to hospitalized children.
Acknowledgments
Funding Source: This study was supported by grants to the Center for Health Outcomes and Policy Research from the National Institute of Nursing Research (T32-NR-007104 and R01-NR-004513, L. Aiken, principal investigator) and from the Children’s Hospital of Philadelphia.
Abbreviations:
- PES-NWI
Practice Environment Scale of the Nursing Work Index
- AHRQ
The Agency for Healthcare Research and Quality
Footnotes
Financial Disclosure: All authors have indicated they have no financial relationships relevant to this article to disclose.
Conflict of Interest: All authors have indicated they have no potential conflicts of interest to disclose.
References:
- 1.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. (Kohn LT, Corrigan JM, Donaldson MS, eds.). Washington, DC: National Academies Press; 2000. doi: 10.17226/9728. [DOI] [PubMed] [Google Scholar]
- 2.Page A Keeping Patients Safe: Transforming the Work Environment of Nurses. (Page A, ed.). Washington, DC: National Academies Press; 2004. doi: 10.1016/S0140-6736(12)60171-8. [DOI] [PubMed] [Google Scholar]
- 3.Cox KS, Teasley SL, Lacey SR, Carroll CA, Sexton KA. Work Environment Perceptions of Pediatric Nurses. J Pediatr Nurs. 2007;22(1):9–14. doi: 10.1016/j.pedn.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Kotzer AM, Koepping DM, Leduc K. Perceived Nursing Work Environment of Acute Care Pediatric Nurses. Pediatr Nurs. 2006;32(4):327–332. [PubMed] [Google Scholar]
- 5.Lake ET, Hallowell SG, Kutney-Lee A, et al. Higher Quality of Care and Patient Safety Associated With Better NICU Work Environments. J Nurs Care Qual. 2016;31(1):24–32. doi: 10.1097/NCQ.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sears K, O’Brien-Pallas L, Stevens B, Murphy GT. The Relationship Between the Nursing Work Environment and the Occurrence of Reported Paediatric Medication Administration Errors: A Pan Canadian Study. J Pediatr Nurs. 2013;28(4):351–356. doi: 10.1016/j.pedn.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Stratton KM, Blegen MA, Pepper G, Vaughn T. Reporting of medication errors by pediatric nurses. J Pediatr Nurs. 2004;19(6):385–392. doi: 10.1016/j.pedn.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Duncan H, Hutchison J, Parshuram CS. The pediatric early warning system score: A severity of illness score to predict urgent medical need in hospitalized children. J Crit Care. 2006;21(3):271–278. doi: 10.1016/j.jcrc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit Care. 2009;13(4):R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.da Silva YS, Fiedor Hamilton M, Horvat C, et al. Evaluation of Electronic Medical Record Vital Sign Data Versus a Commercially Available Acuity Score in Predicting Need for Critical Intervention at a Tertiary Children’s Hospital. Pediatr Crit Care Med. 2015;16(7):644–651. doi: 10.1097/PCC.0000000000000444. [DOI] [PubMed] [Google Scholar]
- 11.Miller MR, Zhan C. Pediatric Patient Safety in Hospitals: A National Picture in 2000. Pediatrics. 2004;113(6):1741–1746. [DOI] [PubMed] [Google Scholar]
- 12.AHRQ. Hospital Survey on Patient Safety Culture User’s Guide. Rockville; 2016. [Google Scholar]
- 13.National Quality Forum. National voluntary consensus standards for nursing-sensitive care: An initial performance measure set—A consensus report. 2004. http://www.qualityforum.org/Projects/n-r/Nursing-Sensitive_Care_Initial_Measures/Nursing_Sensitive_Care__Initial_Measures.aspx.
- 14.National Quality Forum. Practice Environment Scale - Nursing Work Index (PES-NWI) (composite and five subscales). http://www.qualityforum.org/QPS/0206. Published 2017.
- 15.Lake ET. Development of the practice environment scale of the nursing work index. Res Nurs Heal. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 16.Warshawsky NE, Sullivan Havens D. Global use of the Practice Environment Scale of the Nursing Work Index. Nurs Res. 2012;60(1):17–31. doi: 10.1097/NNR.0b013e3181ffa79c.Global. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swiger PA, Patrician PA, Miltner RS, Raju D, Breckenridge-Sproat S, Loan LA. The Practice Environment Scale of the Nursing Work Index_ An updated review and recommendations for use. 2017. doi: 10.1016/j.ijnurstu.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Armstrong KJ., Laschinger H. Structural Empowerment, Magnet Hospital Characteristics, and Patient Safety Culture. J Nurs Care Qual. 2006;21(2):133–134. doi: 10.1097/00001786-200604000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Lake ET, De Cordova PB, Barton S, et al. Missed Nursing Care in Pediatrics. Hosp Pediatr. 2017;7(7):378–384. doi: 10.1542/hpeds.2016-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cimiotti JP, Barton SJ, Gorman KEC, Sloane DM, Aiken LH. Nurse Reports on Resource Adequacy in Hospitals that Care for Acutely Ill Children. J Healthc Qual. 2014;36(2):25–32. doi: 10.1111/j.1945-1474.2012.00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone PW, Mooney-Kane C, Larson EL, et al. Nurse Working Conditions and Patient Safety Outcomes. Med Care. 2007;45(6):571–578. [DOI] [PubMed] [Google Scholar]
- 22.McHugh MD, Rochman MF, Sloane DM, et al. Better Nurse Staffing and Nurse Work Environments Associated With Increased Survival of In-Hospital Cardiac Arrest Patients. Med Care. 2016;54(1):74–80. doi: 10.1097/MLR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lake ET, Shang J, Klaus S, Dunton NE. Patient falls: Association with hospital Magnet status and nursing unit staffing. Res Nurs Health. 2010;33(5):413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brooks Carthon JM, Lasater KB, Sloane DM, Kutney-Lee a. The quality of hospital work environments and missed nursing care is linked to heart failure readmissions: a cross-sectional study of US hospitals. BMJ Qual Saf. 2015;(February):255–263. doi: 10.1136/bmjqs-2014-003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lasater KB, McHugh MD. Nurse staffing and the work environment linked to readmissions among older adults following elective total hip and knee replacement. Int J Qual Health Care. 2016;28(February):mzw007-. doi: 10.1093/intqhc/mzw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brooks-Carthon JM, Lasater KB, Rearden J, Holland S, Sloane DM. Unmet Nursing Care Linked to Rehospitalizations Among Older Black AMI Patients: A Cross-Sectional Study of US Hospitals. Med Care. 2016;54(5):457–465. doi: 10.1097/MLR.0000000000000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aiken LH, Cimiotti JP, Sloane DM, Smith H, Flynn L, Neff D. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49(12):1047–1053. doi: 10.1016/j.ijnurstu.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dillman D Mail and Telephone Surveys: The Total Design Method. Wiley; 1978. https://proxy.library.upenn.edu/login?url=https://search.proquest.com/docview/38137983?accountid=14707. [Google Scholar]
- 29.Smith HL. Double Sample to Minimize Bias Due to Non- response in a Mail Survey Double Sample to Minimize Bias Due to Non-response in a Mail Survey. 2009. http://repository.upenn.edu/psc_working_papers.
- 30.National Quality Forum. Practice Environment Scale-Nursing Work Index PES-NWI Composite and Five Subscales.; 2015. http://www.qualityforum.org/QPS/0206.
- 31.Glick WH. Conceptualizing and Measuring Organizational and Psychological Climate: Pitfalls in. Source Acad Manag Rev. 1985;10(3):601–616. [Google Scholar]
- 32.Cicchetti DV Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. [Google Scholar]
- 33.Agency for Health Care Research and Quality. Hospital Survey on Patient Safety Culture. 2013:1–5. http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/hospital/index.html.
- 34.American Hospital Association. AHA Annual Survey Database FY 2015.; 2015.
- 35.Aiken LH, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344(March):e1717. doi: 10.1136/bmj.e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agency for Healthcare Research and Quality. Culture of Safety. PSNet. https://psnet.ahrq.gov/primers/primer/5/Culture-of-Safety. Published 2018.
- 37.Mark D Patient Safety and the “ Just Culture :” A Primer For Health Care Executives ; Medical Event Reporting System – Transfusion Medicine (MERS-TM). Natl Institutes Heal J. 2001;(April):3. [Google Scholar]
- 38.Kelly BD, Kutney-lee A, Lake ET, Aiken LH. The Critical Care Work Environment and Nurse-Reported Health-Care Associated Infections. Am J Crit Care. 2013;22(6):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McHugh MD, Stimpfel AW. Nurse reported quality of care: A measure of hospital quality. Res Nurs Heal. 2012;35(6):566–575. doi: 10.1002/nur.21503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smeds-Alenius L, Tishelman C, Lindqvist R, Runesdotter S, McHugh MD. RN assessments of excellent quality of care and patient safety are associated with significantly lower odds of 30-day inpatient mortality: A national cross-sectional study of acute-care hospitals. Int J Nurs Stud. 2016;61:117–124. doi: 10.1016/j.ijnurstu.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]