Abstract
Objectives:
Advance care planning (ACP) is important to ensure that nursing home (NH) residents receive care concordant with their goals. Video interventions have been developed to improve the process of ACP. Yet, little is known about which NH characteristics are associated with implementation of ACP video interventions in clinical practice. Our objective was to examine nursing home (NH)-level characteristics associated with the implementation of an ACP video intervention as part of the Pragmatic trial of Video Education in Nursing Homes (PROVEN) trial.
Design:
Cross-sectional study of NHs in PROVEN.
Setting and Participants:
119 NHs randomized to receive the ACP video intervention.
Measurements:
The outcomes were the proportion of short (< 100 days) and long-stay (≥100 days) nursing home (NH) residents who were: i. offered to watch a video and ii. shown a video, aggregated to the NH-level, measured using electronic forms of video offers. The association between outcomes and NH facility characteristics (e.g. staffing, resident acuity) and participation in other aspects of the PROVEN trial (e.g., monthly check-in calls), were estimated using multivariate linear regression models. NH characteristics were measured using data from Online Survey Certification and Reporting data, Long-term Care: Facts on Care in the US and NH Compare.
Results:
Offer-rates were 69% (SD: 28) for short-stay and 56% (SD: 20) for long-stay residents. Show-rates were 19% (SD: 21) for short-stay and 17% (SD: 17) for long-stay residents. After adjusting for NH characteristics, compared to 1-star NHs, higher star-rated NHs had higher offer-rates. Champions’ participation in check-in calls were positively associated with both outcomes for long-stay residents.
Conclusions/Implications:
Lower quality NHs seem unable to integrate a novel ACP video education program into routine care processes. Ongoing support for and engagement with NH staff to Champion the intervention throughout implementation is important for success of a pragmatic trial within NHs.
Keywords: advance care planning, nursing home, pragmatic trial, decision aids, shared decision making
Brief Summary:
Research from the Pragmatic trial of Video Education in Nursing Homes finds engaging staff throughout the intervention implementation is important for success of a pragmatic trial within nursing homes.
BACKGROUND
Advance care planning (ACP) is a process that supports individuals in defining their future goals and preferences for medical treatment at the end-of-life (EOL) and to discuss these goals with their family and health-care providers.1 ACP is particularly important for nursing home (NH) residents, who often receive unnecessary care and experience burdensome transitions at the EOL.2 Additionally, all federally funded NHs are required by the 1990 Patient Self-Determination Act to ascertain residents’ preferences towards EOL care.3 More recently in January 2016, the Centers for Medicare and Medicaid Services (CMS) began further incentivizing health professionals to engage in ACP by reimbursing clinicians for having ACP-related conversations with their patients, regardless of the patients setting.4
The Pragmatic trial of Video Education in Nursing Homes (PROVEN) is a pragmatic randomized clinical trial designed to test the efficacy of an ACP video education program. PROVEN is being conducted in 360 NHs (119 intervention facilities and 241 control facilities) that are part of two large for-profit NH healthcare systems (NH system 1 and 2).5 Each facility had at least one ACP Champion, often a social worker (53%) but also nurses (27%) and other management roles (20%), charged with the intervention implementation. Through a structured training session, Champions were instructed to offer the video using tablets that were provided to the NH at the beginning of the study, within the first week of admission for newly admitted residents and every 6 months for long-stay residents (> 100 days), in conjunction with regularly scheduled care planning sessions. Residents and/or their families offered the opportunity to see the video could agree or decline and all offers and actual showing of the video was to be documented on a special record integrated into the facility EMR. When a resident was cognitively impaired, the Champions were instructed to show the video to the resident’s family. Additionally, Champions could give family members a web link to view their video on their own time. More information on the study protocol can be found elsewhere.5
Two years into the 4-year PROVEN trial, adherence monitoring revealed that there is substantial variation in offer and show rates across the intervention facilities. This study examines the relationship between NH characteristics and these rates among short- and long-stay residents. We hypothesize different types of NH characteristics, such as structural characteristics, resident composition and NH quality, may be associated with adherence rates.6–15
METHODS
Data sources
The PROVEN trial commenced intervention implementation in NHs on March 1, 2016 and is scheduled to be completed in May, 2019. This report leverages data collected from the start of the implementation period, up to March 2018. These data include intervention Champion turnover rates, video status reports (VSR) information, and check-in call attendance. Data from the VSR reports were sent by the NH to the trial’s data coordinating center on a monthly basis. Corporate partners reported turnover in the Champion position directly to the research team. Check-in call date of whether and to whom attendance was recorded with internal project tracking system.
Secondary data for this study come from three sources: Online Survey, Certification and Reporting (OSCAR) data; Long-term Care: Facts on Care in the US (LTC FoCUS); and Nursing Home Compare. OSCAR, which contains information from the NH annual survey and re-certification process, was used to capture pre-intervention (2015) facility characteristics. OSCAR data is collected through onsite evaluations by state survey agencies every 12 to 15 months. This data is maintained by CMS for regulatory purposes and has been used in previous studies to measure facility characteristics such as staffing (e.g. number of full time social workers) and clinical measures (e.g. number of residents with documented signs of depression).16–19 LTCFocUS is a product of Shaping Long Term Care in America Project at Brown University funded in part by the National Institute on Aging (1P01AG027296), which incorporates data from the Minimum Data Set (MDS), OSCAR, area resource file and residential history file, was also used to capture NH characteristics in the pre-period. Nursing Home Compare is a publicly reported dataset of quality measures including regulatory penalties and star ratings from CMS that incorporate data from MDS and Medicare claims (2016).20
Variables
Outcome
The numerators for calculating the offer-rate are the number of short-stay residents offered a video within 14 days of admission and the number of long-stay residents who were ever offered a video during their NH stay, per the VSR. The numerators for show-rate are the number of short-stay residents shown the video within 14 days of admission and the number of long-stay residents who were ever shown the video. For short-stay residents, the denominator is the unique number of individuals newly admitted, cumulatively between NH study start date and March 15, 2018. For long-stay residents, the total number of residents in the NH for 90 out of 100 or more consecutive days at any time from March 2016 through March 2018. Outcomes are reported as percentages.
Independent Variables
Independent variables were categorized to represent the level of engagement of Champions in PROVEN, NH organization, resident composition and quality characteristics: Champion turnover, check-in attendance, NH system (NH System 1 had 98 NHs and NH system 2 (ref.) had 21), social workers per 100 beds, bed size, cognitive impairment, age, admissions per bed, occupancy %, Medicaid %, hospitalizations, star rating, and penalties.
A recent review of ACP interventions in the NH setting found having strong administration support facilitated successful implementation.14Implementation science research evidence has found that sharing best practices and practice concerns among intervention facilities can enhance stakeholder buy-in and enthusiasm for the intervention.15 Furthermore, the Agile Implementation model includes several components that can encourage sustainable implementation including localizing the solution and providing performance feedback.21 NH systems are complex health care organizations so the ability to localize the feedback to each specific NH with a continuous feedback cycle is known to foster greater success of implementation.21 PROVEN has incorporated many of these best practices into the implementation process. Corporate program leaders and research team members held joint monthly check-in calls with each facilities’ Champion(s) to review the offer- and show- rates at their facility and resolve problem-solve any difficulties with the implementation. Prior to June 2017, these monthly conference calls involved groups of champions from multiple facilities. Since these calls were held monthly it was an opportunity for a performance feedback loop to be integrated into the implementation. From June 2017 onward, monthly check-in conference calls were conducted on a 1:1 basis with each individual facilities’ Champions based on their availability. This change allowed feedback to become more localized as each facility has its own unique ecosystem for implementing the ACP videos.21 For example, one NH has a strong relationship with a particular hospice provider and offers the hospice video during an information session for the residents. Additionally, one Champion was struggling to engage their team so they started bringing the tablets to morning huddles to increase awareness of the video. Check-in call attendance was measured as a count of persons from each facility that attended any phone calls through April 2018 (e.g., if 1 Champion from 1 facility attended 6 meetings, the count for that facility would be 6; if 2 Champions from 1 facility attended 3 meetings, the count for that facility would also be 6). If other persons helping with the intervention, other than the Champion, attended the calls they were also included in this measure.
Given the length of the trial and rate of turnover in the industry,22 we also tested the effect of turnover in the Champion role, most of which were filled by social workers.10 Each NH began the trial with 1 or 2 Champions. Champion turnover was measured as the number of changes in the champion position (e.g., a Champion turnover value of 0 means there was no turnover; a value of 2 means there were two changes in the Champion position).
Another recent systematic review of successful ACP in long-term care settings identified one precondition for success was sufficient resources, time available for ACP and incorporation of ACP into standard practice.23 As the Champions are mostly social workers, their availability, given the many other pressing responsibilities they have, is an important factor that may affect implementation.7 The numbers of social workers in the NH could also affect availability, so the larger NHs may have more qualified social workers able to offer and show the ACP video to residents.24, 25 Additionally, the more NH admissions, building on the “practice makes perfect” perspective, the more opportunities for the intervention to become incorporated into standard admission process and thus the video will be more likely to be offered to short-stay residents.26 Admissions per bed is a measure of whether the NH has more short-stay or long-stay residents. NHs with higher admissions per bed can be considered more focused on post-acute residents.
Residents who are more cognitively impaired are less likely to engage in ACP themselves, and thus require facility staff to discuss the issues with family members.27–30 We hypothesize facilities with a larger proportion of residents who are severely cognitively impaired may have a lower video show rate.31 In addition, younger residents may not view ACP as a necessary conversation to engage in when they are still healthy so proportion of residents under 65 may be negatively associated with video show rates.32 Resident composition characteristics include NH-level aggregate measures of age and cognitive impairment from LTC FocUS. Resident cognitive status was quantified using the Cognitive Function Scale (range, 1–4 1= cognitively intact, 2=mildly impaired, 3=moderately impaired, 4=severely impaired).31 In these analyses we categorized the proportion of residents in the facility in three groups: those who were cognitively intact, have mild and moderate impairment, or severe impairment. Age was calculated as the proportion of residents in the facility 65 or younger versus over 65.
Pre-intervention NH quality is an important factor as NHs that are high performers on other aspects of quality may be more likely to take on an intervention. NHs with poor quality may be penalized and having higher hospitalization rates may adversely affect receiving referrals from local hospitals so more time will be focused elsewhere.33–35 In addition, lower occupancy rates and having a higher proportion of Medicaid residents have been associated with poorer NH quality.36, 37 CMS star ratings provide a simplified global measure of quality for consumer use to help facilitate comparison between nursing homes.38 Overall CMS star ratings are measured on a scale of 1 to 5 and are a composite of individual rankings of health inspections, quality indicators, and staffing (excluding social workers). Indicator variables were created for NH with 1-star, 2–3 stars and 4–5 star ratings, as we do not hypothesize a linear relationship between these rankings and the offer or show rates.38 Penalties are recorded in Nursing Home Compare as fines and payment denials. An indicator was created measuring whether a facility had any penalty in 2016. From LTC FocUS we use a measure of hospitalizations as the number of all hospital transfers per person-year.39
Statistical Analyses
The distribution of the outcome variables and descriptive statistics are presented for all measured variables. Correlations between NH characteristics were calculated to understand the relationship between them. Multivariate linear regression was used including all NH characteristics included in table 1 to test the hypothesized association between NH characteristics and the offer- and show-rates. The outcome measures are bounded between 0 and 1 so we used the logit-transformation to adjust for the non-normal distribution. Separate models were run for outcomes in short-stay and long-stay residents. Variance inflation factors were computed to check for multicollinearity between the facility characteristics. All analyses are conducted using Stata (c) 14.0 SE.40 The University Institutional Review Board approved the study by expedited review.
Table 1.
Descriptive Statistics of Nursing Homes
| Both Systems (N=119) Mean (SD) | |
|---|---|
| Outcome: Offer-rate | |
| Short-stay residents | 68.9 (28.2) |
| Long-stay residents | 56.4 (20.4) |
| Outcome: Show-rate | |
| Short-stay residents | 18.7 (20.7) |
| Long-stay residents | 17.1 (16.3) |
| PROVEN Engagement | |
| Champion Turnover | 1.8 (1.4) |
| Check-in call attendance | 6.4 (4.5) |
| Structural characteristics | |
| Total Social Workers/100 beds | 1.3 (0.1) |
| Bed size 120+, N (%) | 64.0 (53.8) |
| Resident composition | |
| % intact (CFS=1) | 34.1 (9.7) |
| % mild/moderate (CFS=2,3 ) | 53.0 (10.1) |
| % severe (CFS=4) | 12.9 (7.8) |
| % Under 65 | 16.2 (10.6) |
| Admissions per bed | 2.4 (1.1) |
| Quality | |
| Occupancy % | 88.0 (9.6) |
| Medicaid % | 70.7 (11.9) |
| Hospitalizations per person-year (2015) | 1.2 (0.4) |
| Overall Star Rating, N (%) | |
| 1 star | 21.0 (17.7) |
| 2/3 | 57.0 (47.9) |
| 4/5 star | 41.0 (34.5) |
| Any Penalty, N (%) | 19.0 (16.0) |
Notes: Means and standard deviations (SD) of the facility characteristics measured at the NH level. Offer-rate is the number of residents offered the ACP video of the total residents within each subgroup (short-stay/long-stay). Show-rate is the number of residents shown the ACP video of those offered. Champion turnover is a measure of previous people in the ACP Champion position at the NH. Check-in call attendance is a measure of the number of calls and people from a NH that participated in conference calls throughout the study period. Occupancy % is a measure of the number of beds filled out of total beds at the time of survey. Medicaid % is the total number of residents where Medicaid was the primary payer out of the total residents at the time of survey. Hospitalizations per person-year is a measure of hospitalizations measured by the Minimum Data Set divided by person-time for each NH. Cognitive function scale (CFS). Overall CMS 5-star rating from quarter 1, 2016. Any penalty is any recorded payment denial or fine from CMS in 2016.
RESULTS
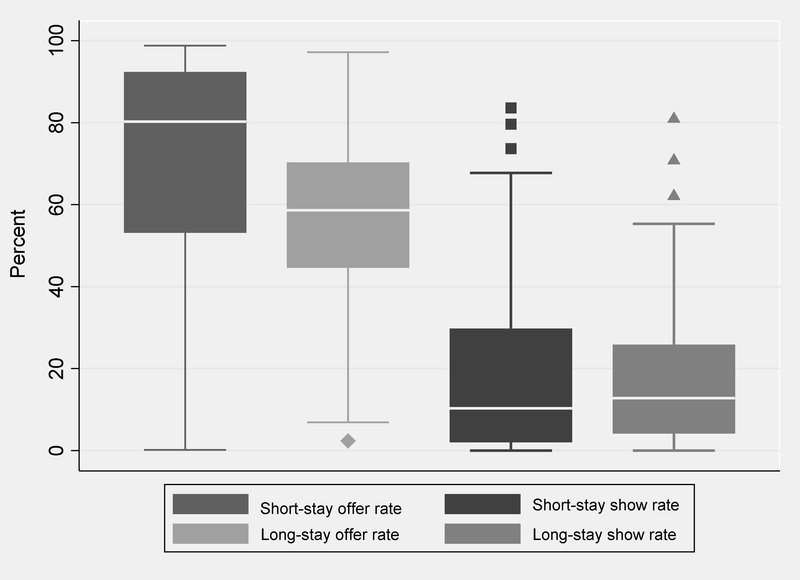
The offer-rate for short-stay and long-stay residents varied widely across NHs from 0 to 100%, with a median of 80% (Interquartile range (IQR) 53%−92%) and 58% (IQR 44%−70%) respectively (Figure 1). Show-rates varied from 0% to 83%, with a median of 10% (IQR 2%−30%) and 13% (IQR 4%−26%) for short-stay and long-stay residents respectively.
Figure 1.
Distribution of cumulative offer and show rate among short-stay and long-stay residents from March 2016 through March 2018
On average, NHs had 6.4 (SD: 4.5) people attending in check-in calls during the study period (Table 1). A high proportion of residents had some cognitive impairment, 53% mild or moderate impairment and 13% severe impairment. NHs had an average occupancy rate of 88% and Medicaid was the primary payer for 70% of residents. About half of the facilities were rated 2- and 3-stars. 19% of facilities had had a financial penalty in the prior year.
The correlation matrix between NH characteristics revealed that the majority of the characteristics are weakly correlated with each other, but some were moderately correlated (Supplemental Table 1). Occupancy rate was moderately negatively (−0.28) correlated with Champion turnover. Admissions per bed was positively correlated with social workers per 100 beds (0.49) and hospitalizations per person-year (0.41). Social workers per 100 beds was positively correlated with the percent of cognitively intact residents (0.33) and negatively correlated with percent of Medicaid recipients (−0.40).
After controlling for facility characteristics included in table 1 in the multivariable regression analyses, NH system 1 had higher offer rates for both short- and long-stay residents (Table 2). Variance inflation factors were all under 5 for all variables included in the models.41 Compared to 1-star facilities, higher rated facilities were associated with higher offer rates. Check-in call attendance was positively associated with the offer- and show-rate for long-stay residents. Otherwise, there were no consistent facility characteristics that were associated with engagement in the PROVEN ACP intervention.
Table 2.
Multivariable regression results
| Offer-rate | Show-rate | |||
|---|---|---|---|---|
| Short-stay | Long-stay | Short-stay | Long-stay | |
| Variable | Coefficient [95% CI] | Coefficient [95% CI] | Coefficient [95% CI] | Coefficient [95% CI] |
| PROVEN Engagement | ||||
| Champion turnover | −0.19 [−0.44,0.076] | −0.06 [−0.23,0.09] | 0.05 [−0.32,0.42] | 0.06 [−0.29,0.40] |
| Check-in call attendance | 0.08 [−0.01,0.16] | 0.08** [0.03,0.14] | 0.09 [−0.03,0.21] | 0.14* [0.03,0.26] |
| Structural characteristics | ||||
| NH system 1 (ref=NH system 2) | 2.00** [0.81,3.19] | 0.96* [0.22,1.69] | −0.33 [−2.05,1.40] | −0.54 [−2.16,1.07] |
| Total Social Workers/100 beds | 0.34 [−0.33,1.01] | 0.002 [−0.41,0.41] | 0.27 [−0.70,1.24] | 0.11 [−0.81,1.03] |
| Bed size 120+ | 0.15 [−0.51,0.81] | −0.01 [−0.42,0.39] | −0.13 [−1.09,0.83] | 0.41 [−0.48,1.30] |
| Resident composition | ||||
| % intact (CFS=1) | Ref. | Ref. | Ref. | Ref. |
| % mild/moderate (CFS=2,3 ) | 0.02 [−0.02,0.06] | 0.01 [−0.01,0.04] | 0.01 [−0.05,0.07] | −0.01 [−0.06,0.04] |
| % severe (CFS=4) | 0.01 [−0.04,0.07] | 0.01 [−0.03,0.04] | 0.02 [−0.07,0.10] | −0.02 [−0.09,0.05] |
| % Under 65 | 0.03 [−0.01,0.07] | 0.02 [−0.01,0.04] | −0.01 [−0.07,0.05] | −0.001 [−0.06,0.05] |
| Admissions per bed | 0.03 [−0.49,0.56] | 0.07 [−0.25,0.39] | −0.26 [−1.02,0.49] | −0.19 [−0.90,1.66] |
| Quality | ||||
| Occupancy % | −0.03 [−0.07,0.01] | −0.01 [−0.03,0.02] | −0.03 [−0.09,0.03] | −0.004 [−0.06,0.05] |
| Medicaid % | −0.02 [−0.06,0.02] | −0.01 [−0.03,0.02] | 0.04 [−0.02,0.10] | 0.02 [−0.04,0.07] |
| Hospitalizations per year (2015) | −0.22 [−1.36,0.91] | −0.07 [−0.77,0.63] | 0.10 [−1.55,1.75] | −0.31 [−1.85,1.23] |
| Overall Star Rating | ||||
| 1 star | Ref. | Ref. | Ref. | Ref. |
| 2/3 star | 1.74*** [0.76, 2.72] | 0.65* [0.05, 1.25] | 0.31 [−1.10, 1.73] | 0.33 [−0.99, 1.66] |
| 4/5 stars | 1.51** [0.42, 2.60] | 0.77* [0.10, 1.44] | 0.74 [−0.84, 2.33] | 0.52 [−0.96. 2.00] |
| Any Penalty | 0.19 [−0.73,1.11] | 0.33 [−0.23, 0.89] | 0.27 [−1.06,1.59] | 0.26 [−0.97,1.51] |
| N | 119 | 119 | 119 | 119 |
| R-squared | 0.33 | 0.22 | 0.26 | 0.18 |
Notes:
p < 0.05
p < 0.01
p < 0.001
Cognitive function scale (CFS); Overall star rating from quarter 1, 2016; Any penalty in 2016.
DISCUSSION
In this analysis of NH characteristics associated with ACP intervention implementation in a large pragmatic trial, we found that better quality facilities (rated above 1 star) were more likely to offer the ACP videos to residents. Champions engaged in ongoing communication and discussion with the research team were also more likely to offer and show the videos to long-stay residents. Otherwise, none of the structural characteristics we hypothesized would be related to intervention fidelity were.
Intervention engagement has been found to be a significant factor of other intervention implementation in NHs. For instance, an evaluation of INTERACT, a tool to reduce hospitalizations in the nursing home setting found that engaged NHs, as measured by a score assigned by the project coordinator who conducted calls with the NHs, had a much higher reduction in hospitalizations compared to the nursing homes rated as not engaged.42 Similarly, an evaluation of an intervention of telemedicine within the NH setting found stark differences between engaged and not engaged facilities in the changes in hospitalizations.43 Furthermore, in a study of pragmatic trials, Bertram et al. finds that communication strategies such as check-in calls are essential to ongoing engagement and success.44 Taken with the previous studies’ findings, the results of our study suggest that check-in calls may be a key ingredient to successful implementation of new quality improvement interventions in the NH setting. The check-in calls not only gave Champions an opportunity to connect over strategies of success but also localized feedback by allowing them to review their own offer and show rates. Although all Champions received their specific rates monthly compared to their system average, these check-in calls served as an additional reminder of offering and showing the ACP videos to residents in a non-threatening and friendly setting and an opportunity to focus on specific barriers that were a challenge to offering the videos to specific residents or groups of residents. The importance of ACP for long-stay residents was highlighted during these calls since long-stay residents are often more frail and with serious illness.45 This emphasis explains the significance of the positive association between check-in calls and the outcomes for long-stay residents but not for short-stay residents.
We found that higher rated NHs were more likely to offer the ACP video compared to 1-star rated facilities. The structure of the NH system has long been described as two-tiered,37 and several studies have found that these lower quality NHs are less likely to improve quality or implement change given the same level of resources.46, 47 If not given adequate support, pragmatic trials may increase disparities between NH residents. To support these residents, future pragmatic trials should consider investing more resources into implementation for the lower quality NHs or exclude them altogether. One resource that could be provided is additional support for staff, but this would require additional buy-in from the NH system. Anecdotal evidence ascertained through the 1:1 calls suggests that the intervention can be successful even in lower quality NHs, so long as they have a Champion with strong leadership skills and willingness to listen.
Although we had measures for many NH characteristics, there were unmeasured variables. We were unable to measure staff turnover and culture which could influence the success of implementing an intervention within the NH setting. Previous studies on quality improvement implementation have suggested that NHs which promote innovation and teamwork have been more successful, 8 while high staff turnover can lead to stress and higher workload for the remaining staff, leaving little time to devote for additional projects. 48 Omitting these variables likely adds noise to the NH system indicator, but also may add measurement error to the social worker staffing ratio which only captures staffing levels at one point in time. Further, simply a count of the number of Champion turnover does not take into consideration the quality or buy-in of such a Champion. Additionally, our measures of intervention offer- and show-rate is dependent upon the staff recording such actions in the electronic health record and thus there may be facility-level differences in the documentation of a “true” video offer and show. This would lead us to underestimate the true values of the outcome, however we believe this is non-differential across high and low performing NHs.
CONCLUSIONS/RELEVANCE
Our findings suggest that even ostensibly straightforward interventions that do not require extensive training, such as showing a video, must include the opportunity to provide feedback about the intervention along with close communication with staff. These results have implications for future pragmatic trials in the NH setting, because ongoing engagement between research and NH staff appears crucial for successful integration of interventions into routine clinical practice. Future research is needed to understand how to best engage NHs in implementation and encourage communication between NHs to share pragmatic strategies for improving clinical practice without the support of research staff.
Supplementary Material
ACKNOWLEDGEMENTS:
Funding sources: This work is supported by the National Institutes of Health (NIH) Common Fund, through a cooperative agreement (NIH-NIA UH3AG49619) from the Office of Strategic Coordination within the Office of the NIH Director. The views presented here are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Dr. Palmer is supported by NIH-NIA T32AG023480. Dr. Mitchell is supported by NIH-NIA K24AG033640.
Sponsor’s Role: Funding sources did not have any role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
CONFLICTS OF INTEREST: Dr. Mor is the Chair of the Independent Quality Committee at HCR ManorCare, a paid consultant to NaviHealth, Inc. and chair their Scientific Advisory Board, and the former Director at PointRight, Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. The Lancet Oncology 2017;18(9):e543–e551. [DOI] [PubMed] [Google Scholar]
- 2.Gozalo P, Teno JM, Mitchell SL, et al. End-of-life transitions among nursing home residents with cognitive issues. New England Journal of Medicine 2011;365(13):1212–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services; Office of the Assistant Secretary for Planning and Evalutaioin; Office of Disability, AaL-TCP. Advanced directives and advanced care planning: Report to Congress. 2008. [Google Scholar]
- 4.Centers for Medicare and Medicaid Services. CMS finalizes 2016 Medicare payment rules for physicians, hospitals & other providers. 2015. [Google Scholar]
- 5.Mor V, Volandes AE, Gutman R, et al. PRagmatic trial Of Video Education in Nursing homes: The design and rationale for a pragmatic cluster randomized trial in the nursing home setting. Clinical Trials 2017;14(2):140–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Intrator O, Castle NG, Mor V Facility Characteristics Associated With Hospitalization of Nursing Home Residents: Results of a National Study. Medical Care 1999;37(3):228–237. [DOI] [PubMed] [Google Scholar]
- 7.Castle NG, Engberg J Staff Turnover and Quality of Care in Nursing Homes. Medical Care 2005;43(6):616–626. [DOI] [PubMed] [Google Scholar]
- 8.Berlowitz DR, Young GJ, Hickey EC, et al. Quality improvement implementation in the nursing home. Health services research 2003;38(1p1):65–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmerman S, Gruber-Baldini AL, Hebel JR, et al. Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. Journal of the American Geriatrics Society 2002;50(12):1987–1995. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. The Milbank quarterly 2010;88(4):500–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahman AN, Schnelle JF. The nursing home culture-change movement: Recent past, present, and future directions for research. The Gerontologist 2008;48(2):142–148. [DOI] [PubMed] [Google Scholar]
- 12.Smith KM, Castle NG, Hyer K Implementation of quality assurance and performance improvement programs in nursing homes: A brief report. Journal of the American Medical Directors Association 2013;14(1):60–61. [DOI] [PubMed] [Google Scholar]
- 13.Banaszak-Holl J, Hines MA. Factors associated with nursing home staff turnover. The Gerontologist 1996;36(4):512–517. [DOI] [PubMed] [Google Scholar]
- 14.Flo E, Husebo B, Bruusgaard P, et al. A review of the implementation and research strategies of advance care planning in nursing homes. BMC geriatrics 2016;16(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagedorn H, Hogan M, Smith JL, et al. Lessons learned about implementing research evidence into clinical practice. Journal of General Internal Medicine 2006;21(S2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feng Z, Katz PR, Intrator O, et al. Physician and nurse staffing in nursing homes: The role and limitations of the Online Survey Certification and Reporting (OSCAR) system. Journal of the American Medical Directors Association 2005;6(1):27–33. [DOI] [PubMed] [Google Scholar]
- 17.Zhang NJ, Paek SC, Wan TT. Reliability estimates of clinical measures between Minimum Data Set and Online Survey Certification and Reporting data of US nursing homes. Medical care 2009:492–495. [DOI] [PubMed] [Google Scholar]
- 18.Konetzka RT, Yi D, Norton EC, et al. Effects of Medicare payment changes on nursing home staffing and deficiencies. Health services research 2004;39(3):463–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevenson DG, Grabowski DC. Sizing up the market for assisted living. Health Affairs 2010;29(1):35–43. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Medicare and Medicaid Services. Nursing Home Compare; 2017. https://data.medicare.gov/data/nursing-home-compare. Accessed 2018.
- 21.Boustani M, Alder CA, Solid CA. Agile Implementation: A Blueprint for Implementing Evidence-Based Healthcare Solutions. J Am Geriatr Soc 2018;66(7):1372–1376. [DOI] [PubMed] [Google Scholar]
- 22.Donoghue C Nursing home staff turnover and retention: An analysis of national level data. Journal of Applied Gerontology 2010;29(1):89–106. [Google Scholar]
- 23.Gilissen J, Pivodic L, Smets T, et al. Preconditions for successful advance care planning in nursing homes: A systematic review. International journal of nursing studies 2017;66:47–59. [DOI] [PubMed] [Google Scholar]
- 24.Bern-Klug M State variations in nursing home social worker qualifications. Journal of gerontological social work 2008;51(3–4):379–409. [DOI] [PubMed] [Google Scholar]
- 25.Wang C-W, Chan CLW, Chow AYM. Social workers’ involvement in advance care planning: a systematic narrative review. BMC Palliative Care 2018;17:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliver DP, Bickel-Swenson D, Zweig S, et al. Experience with implementation of a quality improvement project for the care of nursing home residents. Journal of nursing care quality 2009;24(2):100–104. [DOI] [PubMed] [Google Scholar]
- 27.Lamberg JL, Person CJ, Kiely DK, et al. Decisions to hospitalize nursing home residents dying with advanced dementia. Journal of the American Geriatrics Society 2005;53(8):1396–1401. [DOI] [PubMed] [Google Scholar]
- 28.van der Steen JT, van Soest-Poortvliet MC, Hallie-Heierman M, et al. Factors associated with initiation of advance care planning in dementia: a systematic review. Journal of Alzheimer’s Disease 2014;40(3):743–757. [DOI] [PubMed] [Google Scholar]
- 29.Volicer L, Cantor MD, Derse AR, et al. Advance Care Planning by Proxy for Residents of LongTerm Care Facilities Who Lack Decision-Making Capacity. Journal of the American Geriatrics Society 2002;50(4):761–767. [DOI] [PubMed] [Google Scholar]
- 30.Robinson L, Dickinson C, Rousseau N, et al. A systematic review of the effectiveness of advance care planning interventions for people with cognitive impairment and dementia. Age and Ageing 2012;41(2):263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas KS, Dosa D, Wysocki A, et al. The minimum data set 3.0 cognitive function scale. Medical care 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schickedanz AD, Schillinger D, Landefeld CS, et al. A Clinical Framework for Improving the Advance Care Planning Process: Start with Patients’ Self-Identified Barriers. Journal of the American Geriatrics Society 2009;57(1):31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harrington C, Tsoukalas T, Rudder C, et al. Variation in the use of federal and state civil money penalties for nursing homes. The Gerontologist 2008;48(5):679–691. [DOI] [PubMed] [Google Scholar]
- 34.Kane RL. Assuring quality in nursing home care. Journal of the American Geriatrics Society 1998;46(2):232–237. [DOI] [PubMed] [Google Scholar]
- 35.Grabowski DC, Stewart KA, Broderick SM, et al. Predictors of nursing home hospitalization: a review of the literature. Medical Care Research and Review 2008;65(1):3–39. [DOI] [PubMed] [Google Scholar]
- 36.Nyman JA. Excess demand, the percentage of Medicaid patients, and the quality of nursing home care. Journal of Human Resources 1988:76–92. [Google Scholar]
- 37.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. The Milbank Quarterly 2004;82(2):227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castle NG, Ferguson JC. What Is Nursing Home Quality and How Is It Measured? The Gerontologist 2010;50(4):426–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rahman M, Tyler D, Acquah JK, et al. Sensitivity and specificity of the Minimum Data Set 3.0 discharge data relative to Medicare claims. Journal of the American Medical Directors Association 2014;15(11):819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 41.Hair J, Anderson RE, Tatham R, et al. Multivariate data analysis. Saddle River. NJ: Prentice Hall; 1995. [Google Scholar]
- 42.Ouslander JG, Lamb G, Tappen R, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. Journal of the American Geriatrics Society 2011;59(4):745–753. [DOI] [PubMed] [Google Scholar]
- 43.Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for medicare. Health Affairs 2014;33(2):244–250. [DOI] [PubMed] [Google Scholar]
- 44.Bertram S, Graham D, Kurland M, et al. Communication is the key to success in pragmatic clinical trials in practice-based research networks (PBRNs). The Journal of the American Board of Family Medicine 2013;26(5):571–578. [DOI] [PubMed] [Google Scholar]
- 45.Fried TR, Mor V Frailty and hospitalization of long-term stay nursing home residents. Journal of the American Geriatrics Society 1997;45(3):265–269. [DOI] [PubMed] [Google Scholar]
- 46.Grabowski DC, Elliot A, Leitzell B, et al. Who are the innovators? Nursing homes implementing culture change. The Gerontologist 2014;54(Suppl_1):S65–S75. [DOI] [PubMed] [Google Scholar]
- 47.Werner RM, Kolstad JT, Stuart EA, et al. The effect of pay-for-performance in hospitals: lessons for quality improvement. Health Affairs 2011;30(4):690–698. [DOI] [PubMed] [Google Scholar]
- 48.Mentes JC, Tripp-Reimer T Barriers and facilitators in nursing home intervention research. Western Journal of Nursing Research 2002;24(8):918–936. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.