Abstract
Objectives:
To elucidate the effects of the intravaginal ring, oral contraceptive pill (OCP), and spermicide plus condom on women’s sexual experiences through an in-depth understanding of the physical characteristics of these contraceptive methods.
Method:
We conducted qualitative in-depth interviews with women (aged 18–45 years) who used up to three contraceptive methods (intravaginal ring, OCP, and spermicide plus condom). Women completed in-depth interviews after each 3-month use period. We used a summarized matrix framework and thematic content analysis to explore how each method affected participants’ sexual experiences.
Results:
Sixteen women completed interviews, yielding 33 transcripts. Women reported physical effects on their sexual experiences while using the intravaginal ring and spermicide plus condom. The OCP was often discussed as lacking these physical effects. Discussion themes included product administration (e.g., navigating intravaginal ring removal) and physical product awareness (e.g., spermicide as a lubricant). From these experiences, women often altered and individualized their use and subsequent opinions of the contraceptive method.
Conclusions:
The range of contraceptive effects on women’s sexual experiences shape their use and opinions of the product, leading to either increased motivation and consistent use or poor adherence and discontinuation. Awareness of these individualized experiences can help providers better understand and guide their patients towards successful contraceptive use.
Precis:
The physical characteristics of contraceptive methods can affect the sexual experiences of women and their partners, shaping their subsequent opinions of each method.
INTRODUCTION
Significant strides have been made in the inclusion of sexual pleasure within the realm of family planning,1 but much is still unknown about women’s sexual experiences in the context of their contraceptive use. As sexual experience is important in shaping women’s contraceptive use,2 fully understanding a woman’s contraceptive decisions ultimately requires understanding contraceptive effects on sexual experience and pleasure.
Current literature focuses on hormonally derived effects (e.g., change in libido) of contraception on sexual experience. As a popular method, the oral contraceptive pill is well studied, but existing research presents a spectrum of hormonal effects on sexual arousal, frequency, and satisfaction.3–7 Other hormonal methods, such as the intravaginal ring8–9 are similarly researched under a lens of hormonal effects, but are significantly less studied. Of the nonhormonal methods, male condoms’ effects on sexual experience are best understood. A significant number of users dislike male condoms due to issues surrounding sexual pleasure, intimacy, lack of spontaneity, and physical comfort.10–13 The effects of other nonhormonal methods, like spermicide, on sexual experience are rarely discussed in the literature, perhaps due to their overall low use rate among women.14
Few studies comprehensively consider hormonal contraceptives’ non-hormonal effectss on sexual experiences; in addition, few studies explore effects of non-hormonal methods beyond condoms, with rare exceptions.9,11,15 Understanding contraceptive needs and experiences requires discussion on a greater variety of methods and consideration of each method as an entire product, rather than just a hormone. The objective of this analysis was to explore user perspectives when using three contraceptive products (the intravaginal ring, spermicide plus condom, and oral contraceptive pill) through qualitative, in-depth analyses of women’s individual sexual experiences. The current study adds to the literature by considering the physical effects of these contraceptive methods on participants’ sexual lives and resulting opinions, choices, and use.
METHODS
Project WISH (Women’s Input on Sexual Health) was a longitudinal prospective study utilizing a mixed-method integrative design, capturing data on users’ sensory experiences of sexual lubricants and contraceptives and the meaning derived from those experiences. This analysis focused on the qualitative data gathered from the contraceptive arm, which explored women’s experiences with an intravaginal ring (etonogestrel (0.120mg/day) and ethinyl estradiol (0.015mg/day) vaginal ring), spermicide plus condom (spermicidal gel containing 4% non-oxynol-9 with condom to improve efficacy), and OCP (triphasic ethinyl estradiol (0.035mg) and norgestimate (0.180/0.215/0.250mg) pill).
We recruited participants through call-lists from previous studies, flyers, advertisements on the internet and through social media, outpatient clinics, healthcare provider referral, community-based organizations, and word-of-mouth. Women received a description of the study by phone or in-person: those interested completed a prescreening questionnaire (e.g., age, self-reported need for contraception). If initially eligible, participants then completed a clinical screening visit. Eligibility criteria were 18 to 45 years of age, in good general health, not pregnant and without intention to become pregnant during the study, HIV-negative or unknown HIV status, reported vaginal sex with a male in the past month, and medical clearance for hormonal contraceptive use. Written informed consent was obtained as per appropriate guidelines. The study was approved by the institutional review board at The Miriam Hospital.
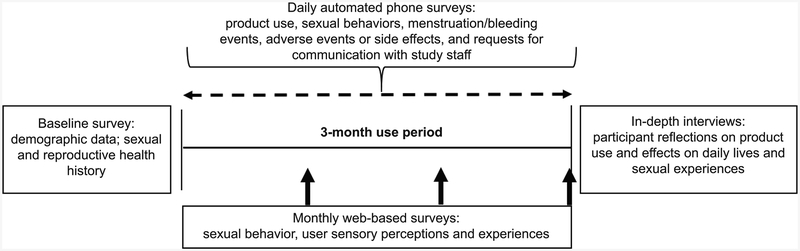
Women enrolled in one of two study designs. In protocol v.1, participants enrolled for 9 months and used one method (intravaginal ring, spermicide plus condom, OCP) per 3-month use period. Order of product use was assigned randomly. In protocol v.2, participants enrolled for 6 months. The first method, used for a 3-month period, was randomly assigned. Then, women had the option of 1) continuing with the first method for the second 3-month period or 2) being randomly assigned to a different method for the final 3-month period. Allowing women this option in protocol v.2 added to the overall study’s ability to understand women’s contraceptive choices, offering a different perspective from the random assignment in protocol v.1. At the beginning of each use period, study staff oriented all participants to proper product use and provided a 3-month supply. In addition, all participants were provided with condoms and counseled on their use in preventing sexually transmitted infections. Using condoms with the spermicidal gel was required in the study in order to improve contraceptive efficacy; participants employed their own perception of STI risk in their decisions to use or not use study-provided (or their own) condoms with the OCP and intravaginal ring. Participants completed a baseline survey at the clinical screening visit. Then, for each 3-month use period, participants completed daily automated phone surveys, monthly web surveys, and in-depth interviews (Figure 1). Participants were compensated for their time to complete research activities over a 6- to 9-month study period ($25 for baseline survey; $1/day for phone survey completion; $25/monthly survey; $50/IDI; $25 for final product evaluation survey) and received contraceptive methods at no cost.
Figure 1.
Data collection and descriptions of surveys and interviews.
In-depth interviews were semi-structured and aimed to establish an understanding of the relationship between salient physical product characteristics and participants’ use and experiences with their contraceptive methods, both in their daily lives and, specifically, during sexual experiences. Calendars displaying product use, sexual behavior, and menstrual data from the daily phone surveys also facilitated contextualization of the discussion. In-depth interviews were audio-recorded and transcribed verbatim.
Prior to data reduction into framework matrices, all analysts were trained to a common coding structure using clear, objective descriptions and examples. Using a summary matrix framework, two researchers independently extracted and summarized the transcripts into matrices representing specific constructs (e.g., sensory experiences). Subsequently, the two researchers met and consensus regarding summarized data was reached. If consensus could not be reached, a third, trained analyst was available to offer insight. Themes derived reflected both the original intent of the in-depth interviews and data as it emerged from the discussions. The first author further reduced data from matrices related to participants’ sexual experiences with the assigned contraceptive methods. These data explored themes regarding product administration and physical product awareness for all three methods, as well as individual experiences unique to each product.
RESULTS
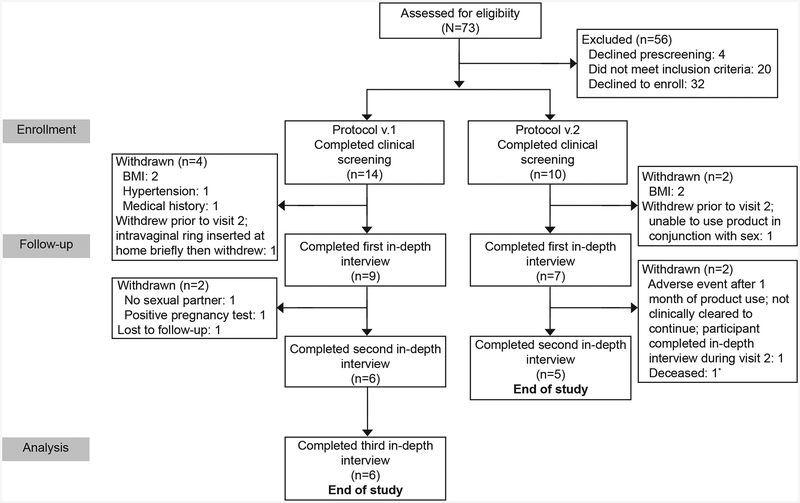
Twenty-four women were enrolled for the contraceptive condition (Figure 2). The final sample consisted of 16 women who used up to three contraceptive methods. Table 1 provides selected demographics and reproductive history. Though 5 women did not complete the full study protocol, these participants each completed 1 in-depth interview, which remained in the final dataset. Thus, the contraceptive arm consists of data from 33 IDI transcripts, representing the experiences of each participant with each contraceptive method used. In total, 10 women used the OCP, 12 women used the intravaginal ring, and 7 used the spermicide plus condom for 3 months. Illustrative quotations are uniquely attributed to each participant by age and contraceptive method used immediately prior to enrolling in this study (e.g. 23y, OCP); where more than one quote has the same age and contraceptive method but is a different participant “[A]” and “[B]” are used to distinguish them.
Figure 2.
Flow diagram of participant selection and study. BMI, body mass index. *Unrelated.
Table 1:
Selected demographic characteristics and reproductive history (n=16)
| Characteristic | Value |
|---|---|
| Age | 27 (20–34) |
| Hispanic/Latina Ethnicity | 4 (25%) |
| Race* | |
| Black | 2 (13%) |
| White | 8 (50%) |
| Asian | 1 (6%) |
| American Indian/Alaska Native | 3 (19%) |
| Other† | 1 (6%) |
| Financial Situation | |
| Comfortable, with “extras” | 6 (38%) |
| Enough to pay bills without cutting | 7 (44%) |
| Enough to pay bills, but cutting back | 1 (6%) |
| Not enough to pay bills | 2 (13%) |
| Health Insurance Coverage | |
| Employer-Sponsored | 5 (31%) |
| Direct from Insurance Company | 1 (6%) |
| Government-Sponsored | 5 (31%) |
| Parent’s insurance | 1 (6%) |
| None | 4 (25%) |
| Highest Educational Level | |
| Some high school | 1 (6%) |
| High school diploma/GED | 2 (13%) |
| Some college | 5 (31%) |
| College degree | 6 (38%) |
| Graduate/professional degree | 2 (13%) |
| Sexual History | |
| Vaginal Sex, # of Males in Past Month | 1.06 (1–2) |
| Vaginal Sex Frequency | |
| Less than once per week | 2 (13%) |
| 1–2 times per week | 4 (25%) |
| 3–4 times per week | 7 (44%) |
| 5–6 times per week | 3 (19%) |
| Contraceptive History – Ever Used | |
| Male Condoms | 16 (100%) |
| Spermicides (not on condom) | 1 (6%) |
| Non-Hormonal Intrauterine Device | 3 (19%) |
| Hormonal Contraception | 11 (69%) |
| Oral Contraceptive Pills | 11 (69%) |
| Patch | 2 (13%) |
| Ring | 4 (25%) |
| Injection | 4 (25%) |
| Hormonal Intrauterine Device | 2 (13%) |
| Emergency Contraception | 9 (56%) |
| In last 12 months | 3 (19%) |
| Current Contraceptive Method Use‡ | 10 (63%) |
| Male condoms | 7 (44%) |
| Hormonal Contraception | 5 (31%) |
| Oral Contraceptive Pills | 1 (4%) |
| Patch | 1 (4%) |
| Intravaginal Ring | 1 (4%) |
| Withdrawal | 1 (4%) |
| No current contraceptive method | 1 (4%) |
Data are mean (range) or n (%).
Participants were able to choose more than one race (n=6).
Other includes Cape Verdean (n=1).
Participants were able to choose more than one current contraceptive method (n=4): along with the male condom, one used the patch, one used the intravaginal ring, one used withdrawal method, and one used the oral contraceptive pill.
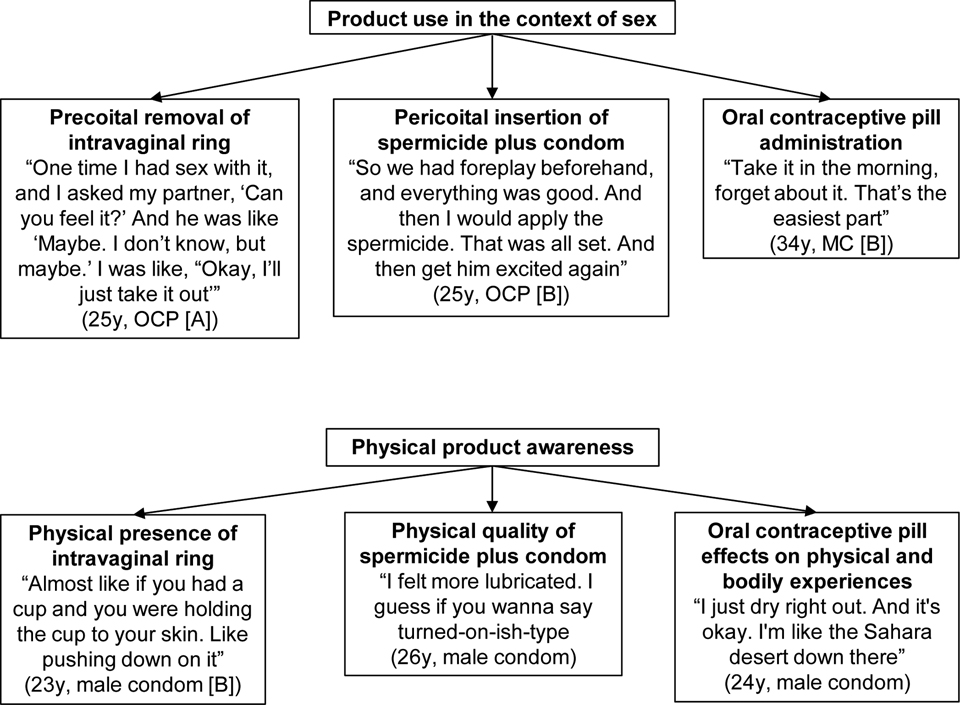
Though each contraceptive method was varied in use demands and product characteristics, we identified two salient themes that united all three products: product use and physical product awareness (Figure 3). Within the theme of product use, participants centered their decision-making processes on peri-coital removal of the intravaginal ring and pre-coital insertion for the spermicide plus condom. For the OCP, pill administration provided an interesting contrast to the intravaginal ring and spermicide plus condom experiences. Within the theme of product awareness, each contraceptive method led to a unique “felt” experience, from the physical presence of the intravaginal ring during vaginal intercourse (sex) to the lubricating quality of spermicide. The OCP lacked a physical presence in the vagina, but still had indirect effects on the “felt” sexual experience.
Figure 3.
Representation of overarching themes as organized for each contraceptive method. Illustrative quotes are attributed to each participant by their age and contraceptive method used before the study: [A] and [B] are used to distinguish individuals with the same characteristics and correspond accordingly to their quotes in the text. OCP, oral contraceptive pill, y, years.
Product Use in the Context of Sex
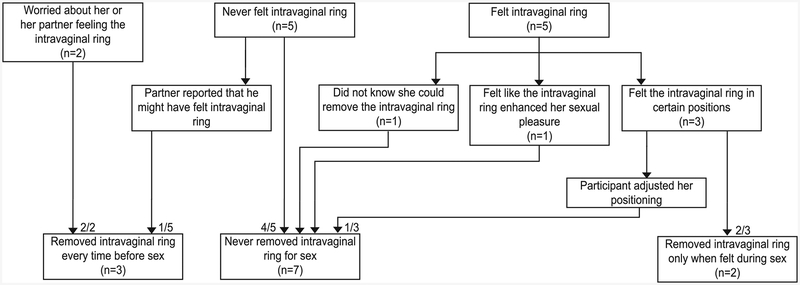
Decisions regarding intravaginal ring removal in the context of sex varied across participants: Figure 4 illustrates contributing reasons for, and timing of, intravaginal ring removal. Of the seven who never removed the intravaginal ring, some expressed concerns about intravaginal ring efficacy, reporting concern about inadequate protection overall or worrying they would forget to reinsert the intravaginal ring after sex:
I wanted to use it like you’re supposed to, so that’s what I was worried about. For pills, you’re supposed to take it at a certain time. And if you don’t, it’s less effective. I was worried that, even though you can take the ring out for a certain amount of time—if it’s out, or if it falls out—does it lose its effectiveness?
(29y, male condom (MC) and patch)
and
I never take it out because I don’t wanna worry about forgetting to put it back in. Like, you take it out, you leave it on the nightstand, then six hours later, you’re like, ‘oh, no!’ I don’t wanna deal with that.
(26y, OCP [B])
Figure 4.
Flow diagram describing the range of reasons behind participants’ decisions and timing surrounding intravaginal ring removal (n=12).
Several participants removed the intravaginal ring for sex at least once, citing actual or anticipated partner experience as a concern:
I thought that I would probably be able to feel it. And that my boyfriend would be able to feel it, and I guess the comfort is the reason why I took it out
(25y, no contraception)
and
It just wasn’t really going well. I tried to readjust it five or six times… Basically at that point I was frustrated and I was like, I’m just done. Take it out.
(23y, MC [B])
A few participants described the effect of intravaginal ring removal in the context of sex. For those who normally use the bathroom before sex, ring removal in the bathroom did not affect regular sexual experience. Others reported that intravaginal ring removal was somewhat awkward:
…You have to take this thing out of your vagina now. And you’re in the middle of having sex. It’s like okay, stop, take this, and then all right, let’s have sex again.
(25y, OCP [B])
Finally, one participant felt that ring removal was an additional step, which obstructed her desire for spontaneous sex. Also, intravaginal ring reinsertion after sex was painful, further decreasing her likelihood of having sex. She states:
Mentally, knowing that if I wanted to have sex, having to take it out and then put it back in was a minus sign in my head. So then that just made me less likely to have sex…
(25y, no contraception)
Behaviors associated with spermicide insertion varied with each participant, effecting subsequent sexual experiences. All participants who used spermicide plus condom discussed the location of spermicide insertion (approximately half each in the bathroom or bedroom). For two participants, going to the bathroom before intercourse was a normal occurrence; therefore, spermicide insertion in the bathroom did not feel like an interruption. For another, this was not her typical routine; therefore, spermicide insertion was both awkward and interrupted her sexual experience:
Things would start happening, and I’d be like, ‘Hold on, I gotta run to the bathroom.’ It sucked. It felt like it … killed the moment, a little bit. Cuz we’re in the middle of passion. And then I’m like, ‘Oh, you needa wait…two minutes. Just give me two minutes.’
(26y, OCP [A])
Participants inserting spermicide in the bedroom in their partners’ presence reported varying levels of comfort with this. Some participants were not bothered by their partners witnessing spermicide insertion, but others considered spermicide insertion similar to tampon insertion, which they would not do in front of their partners:
I wouldn’t feel comfortable inserting it in front of him. Like, he knows, but you wouldn’t put a tampon in front of your boyfriend. That’s weird.
(23y, MC [A])
Almost all participants discussed spermicide plus condom use as an interruption in their overall sexual experience. Half felt spermicide plus condom disrupted the mood:
We’re used to being able to [claps hands]—have sex, whenever, and not have to stop and worry about extra things, and that’s the reason why we never used the diaphragm or anything like that. Because it was just that extra step that we didn’t wanna have to take.
(26y, OCP [A])
Conversely, some women who acknowledged that spermicide use was an extra step weighed the inconvenience against motivators to use, such as increasing sexual pleasure, pregnancy prevention, or lack of hormonal side effects, as illustrated here:
It was an extra step, definitely, but I think because sex felt really great with it, it was fine
(25y, no contraception)
and
It’s definitely more time-consuming than just having a patch on your arm, but then again, there’s so many benefits with the hormone issue and all the other stuff that you miss. So it was definitely that factor. And if you’re a person that the hormones and the birth control really affects you, this is God-sent.
(26y, MC)
Most participants discussed their opinions around “fit” of spermicide plus condom as part of their usual sexual routine. Two participants felt that the spermicide plus condom did not fit well as it hindered spontaneous sex and disrupted their normal sexual routine. Remaining participants noted that the spermicide plus condom did fit well because of ease of spermicide use or natural incorporation in their previously set routines. One woman elaborates:
I think that I’ve been using something already for so long that…I don’t think of it as a nuisance or an additional step. I just think—oh, I’m just using something different this time.
(34y, MC [A])
Many participants experienced no change in their sexual routine while using OCPs. Compared to previous study products, two participants noted a lack of interruption with OCP use:
I liked that I didn’t have to take anything out or do any preparation. So that was nice. …Or stop in the middle of whatever and think about taking care of that.
(25y, no contraception)
Though the OCP was not associated with a direct physical effect on sex, a few women discussed mental awareness of OCP use during sex. One woman felt the OCP was mentally freeing. Other women reported ruminating, wondering whether they had taken the OCP that day:
If I was having sex, I’d be like ‘oh, my god, did I take it today, did I take it today?’ It’d be one of those fleeting thoughts…
(23y, MC [B])
Physical Awareness and the Felt Experience
The physical presence of the intravaginal ring during sex affected both participants’ and partners’ sexual experiences. Of the ten participants who experienced sex with the intravaginal ring inserted, half stated that they could not feel the ring during sex, while half felt the ring and elaborated on their sensory experiences and responses:
It didn’t feel like pain. It just felt not normal. I could feel that it was there
(34, MC)
and
The ring kinda made it feel a little better. The sensation. Every time he stroked his penis in and out, it felt better. I don’t know why, but it did.
(20y, MC and OCP)
Three participants were more physically aware of the ring in specific sexual positions:
Especially when I was on top, I could feel it a little bit more. I felt like it was hitting my cervix a little bit, which is very uncomfortable.
(25y, OCP [B])
Four expended mental effort around the sensation of the ring during sex, though two did not report physically feeling the ring. One woman states:
I think I was concentrating on the ring. That’s what I was really worried about, so that’s how I spent my time, worrying about the ring.
(29y, MC and patch).
Both physically and mentally, some participants reported less awareness with continued intravaginal ring use, as illustrated here:
I guess my body got used to it—cuz it’s been six months, so now it just feels natural. I guess it’s like… a part of sex.
(20y, MC and OCP).
All participants discussed their partner’s sexual experience with ring use. Both participants who always removed the intravaginal ring before sex cited concerns about partner sensation as a reason for preemptive ring removal. Of the remaining women, some reported that their partners did not feel the ring. However, a few worried about their partners feeling the intravaginal ring and the resulting consequences, such as mood disruption or even partner pressure to remove the intravaginal ring, as elaborated here:
I was worried about that, at first, because it’s a little awkward to know that something’s inside of you, and that your boyfriend could possibly feel it. Not like he would care or anything, it’s just weird. You don’t want him to be like, ‘well, I can feel that,’ cuz then the mood just got killed.
(23y, MC [A])
According to several participants, their partners did feel the ring, and most were not affected. Others were less neutral. One partner told the participant that the sensation of the ring was sometimes “too much” (25y, OCP [B]), and another partner reportedly did not enjoy feeling the ring but did not request intravaginal ring removal:
I don’t think it was hurting him, but he was aware that it was there. I don’t think he loved it, either. Cuz he said, ‘Oh, you could feel this.’ And the tone…
(34y, MC [A])
The spermicide’s physical presence affected both participants’ and partners’ experiences of lubrication and led to alterations in sexual activity. Most participants felt more lubricated with spermicide use. Over half perceived the spermicide’s lubricity as facilitating initial penetration, as illustrated here:
It definitely made it easier, and sometimes without it, when he first puts it in, it’d be a little bit uncomfortable for me…But, with the [spermicide], there wasn’t any type of discomfort. Cuz he just was able to slide in easier.
(26y, OCP [A])
Three participants regularly used lubricated condoms or sexual lubricant previously: two did not notice a sensory difference in initial penetration, while one denied any overall increase in lubrication. She states:
It felt no different from him using any other lubricant or condoms that we were already using previously, so it wasn’t a change, didn’t feel like anything different.
(34y, MC [A])
With increased lubrication, one participant no longer felt sore after sex, noting that sex was more enjoyable. She elaborates:
I guess it felt really comfortable and, like a lubricant, and after sex—I felt not sore, like it was fine, just went on with my day.
(25y, no contraception)
Most participants also had opinions on spermicide volume. While one participant found that the amount of spermicide was excessive, most considered it appropriate and similar to their physiologic vaginal lubrication, as illustrated here:
I just thought that it just blended in with your natural stuff going on there… Something like a spermicide is great because it just kinda disappears.
(23y, MC [A])
Participants also discussed their partners’ opinions on lubrication with spermicide use. The majority reported partners noticing increased wetness with spermicide. Per participant report, some partners accurately attributed the increased wetness to spermicide use, while others did not:
The first time, he was surprised. [Laughter] I think he thought that I was a lot more turned on than I was.
(26y, OCP [A])
For two participants’ partners, increased lubrication led to either increased or decreased sensation during sex, as illustrated here:
Since it was wetter, it’s easier to have sex, especially on his end because he can feel more at that point
(23y, MC [A])
and
Because of the condom and losing some sensitivity with that and then the lubricant also made him lose some sensitivity cuz it was very slippery…he had to have a certain position where he could get the most out of it and where it felt the best…The spermicide, there was a lot less friction. So, he had to create that friction…
(25y, OCP [B])
In reaction to the physical presence of spermicide, some participants changed their oral sex practices, either hesitating or refusing to receive oral sex. One participant felt that requesting oral sex would be “mean” (25y, OCP [B]) to her partner due to the spermicide volume, and one participant worried about partner safety, describing spermicide as a chemical (26y, MC). Others were more concerned with partner awareness of the product itself; one woman states:
…I just thought it was weird. I guess it’s just the thought of you thinking that it might come out—and then he’ll notice that.
(23y, MC [A]).
Though the OCP was not present in the vagina, participants described the effects the OCP had on their physical experiences. Approximately half of the participants discussed their natural lubrication while using the pill. Four women reported less lubrication while on the pill, while one woman reported no change, and another reported slightly increased lubrication after some difficulty with initial penetration. She describes:
…At first it’s a little difficult. I don’t know, I’m not excessively dry or anything, but I did notice that once we’re in the movement, it flows more freely.
(34y, MC [B]).
Decreased lubrication did not bother two participants as they considered it relative to lubrication associated with intravaginal ring or spermicide use. For two others, decreased lubrication with the OCP did effect both their and their partners’ sensory experiences. Both participants reported that their partners associated dryness with sexual desire: one partner attributed dryness with decreased sexual arousal, while another partner felt personal sexual inadequacy, as illustrated here:
He said that you wanna have sex, but you don’t seem excited. You don’t seem to be into it as much as sometimes you are…you just stay a little dryer.
(25y, OCP [B])
and
…Well, you’re not enjoying it, so what am I doing wrong?
(per 24y, MC)
One participant reported painful sex from vaginal dryness, but noted that both lubrication and arousal increased as the study continued; she states:
I maybe get a little, little, little bit wet, and it’s not even enough to call it damp. For the most part, it’s still painful for me…It’s still pleasurable, but not as much. I have to lube down there before then.
(24y, MC)
DISCUSSION
Physical characteristics of each contraceptive method led to a range of physical and psychosocial sexual experiences across participants. Though each product was unique, participants also described overarching, uniting themes of product administration and product physical quality. Particularly with intravaginal products, the physical characteristics affected participants’ sexual experiences either directly, through sensation and product awareness, or indirectly, through the effect of product administration on their sexual routine and overall sexual experience. OCP use offered contrasting discussion on its lack of physical presence and administration in conjunction with sex.
Many participants were uncomfortable being physically aware of their contraceptive method during sex; this was especially true of the intravaginal ring. Participants’ sensation of the intravaginal ring during sex, or pre-coital concern of intravaginal ring awareness, often led to ring removal. Other studies have also reported a negative effect of intravaginal ring awareness on sexual experiences.8,11 However, physical awareness of the intravaginal ring did not universally negatively affect sexual experiences; in fact, one participant felt increased sexual pleasure due to intravaginal ring awareness. Additionally, the spermicide positively effected some users’ sexual experiences through its dual effect as a lubricant, which can increase sexual pleasure,16–17 and participants in this study were able to use effective contraception while minimizing painful experiences such as initial penetration. Importantly, rather than solely considering physical products as potential barriers in sexual sensation, they can also act as sexual enhancers. Though contraceptive users and providers often emphasize and pursue the absence of effect of contraceptive methods on sexual pleasure and experience, both reduction of negative effects of contraception on sexual experiences and promotion of the contraceptive method’s potential in enhancing a woman’s sexual pleasure should be critically considered.
The contraceptives’ effect on partners’ sexual pleasure and comfort subsequently affected women’s sexual experiences. For some, concern over partner experience led to a change in sexual behavior, such as ring removal, refusal to receive oral sex when using spermicide, or altering sexual positions. Participants sometimes gave these concerns more weight than their own felt experience or even their partners’ stated opinions, supporting findings that women’s sexual pleasure is connected to their concern for partner pleasure.2,8
When discussing new products, participants valued a method that did not disrupt their sexual mood or routine. Consistent with other studies,2 many women desired a sexual routine involving the fewest steps to maintain a natural sense of spontaneity. However, some participants already had steps in their sexual routine (e.g., using the restroom beforehand) that facilitated product use requiring peri-coital tasks (e.g., intravaginal ring removal, spermicide plus condom insertion). Though the intravaginal ring and spermicide plus condom have additional product use demands, their actual effect on, and fit within, participants’ sexual routines were dependent on the user’s pre-established sexual routine. The ability to have spontaneous sex is a positive quality associated with OCPs and other methods where use does not co-occur with sex, but for some women, the positive effects (e.g. lubrication) of methods with greater peri-coital user demand were more important.
Contraceptive effects on sexual experience also modulated the way participants used their contraceptive method with respect to stated instructions. These changes ranged from deviations from ideal product use to minimal use or discontinuation. Given the importance of sexual pleasure in contraceptive satisfaction and continuation,2,3,7 variations in product use behaviors are important to consider because both incorrect product use and discontinuation increase the risk of unwanted pregnancy.18 Notably, these findings also describe how contraceptive users are able to individualize their method use while maintaining product efficacy, thus taking control of a method’s ability to “fit” within their sexual routine.19 Providers should consider the different effects contraceptive methods could have on their patients’ lives and offer guidance in handling those obstacles while maintaining product efficacy, in order to facilitate tailored contraceptive use and continuation.
Study strengths include the depth of understanding offered by qualitative data, which showcases voices of the very people experiencing these products and highlights issues that individual women find important to their own adherence to contraception. Limitations include potential bias in the participant population due to possible barriers in completing the study, such as the intensive nature of study activities, the study’s long duration, and the need to switch contraceptive methods. The study aimed to minimize sampling bias through inclusion of in-depth interviews from participants who did not complete all 3 contraceptive methods in the study; while inclusion of these data could effect comparative analyses, the current analysis did not rely on the longitudinal experiences participants had with their contraceptive methods. The data here is not necessarily generalizable to the overall population of contraceptive users, either in products studied or participant demographics, including sexual and reproductive history. Finally, this article did not explore non-binary identities in either the literature review or patient population. Though binary terms like ‘women’ and ‘men’ were used, the authors recognize the importance of considering transgender and non-binary identities in conversations on sexual pleasure and contraceptive use.
This study demonstrates the importance of considering physical effectss of contraceptive methods on sexual experiences and emphasizes the need to expand our discussion of contraception beyond hormonal methods and effects. With a better understanding of the multitude of effects contraception can have on users’ sexual experiences, providers can be better equipped to guide their patients in choosing a contraceptive method that maintains product efficacy while supporting user satisfaction and self-determination in sexual health.
Supplementary Material
Acknowledgements:
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), award K24HD062645 (Guthrie, KM: PI).
The authors thank the participants for their time and contributions to Project WISH.
Presented, in part, at the Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists, Nashville, Tennessee, May 3–6, 2019.
REFERENCES
- 1.Higgins JA and Hirsch JS, The Pleasure Deficit: Revisiting the “Sexuality Connection” in Reproductive Health. Perspectives on Sexual and Reproductive Health, 2007. 39(4): p. 240–247. [DOI] [PubMed] [Google Scholar]
- 2.Higgins JA and Hirsch JS, Pleasure, Power, and Inequality: Incorporating Sexuality Into Research on Contraceptive Use. American Journal of Public Health, 2008. 98(10): p. 1803–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanders SA, et al. , A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception, 2001. 64(1): p. 51–8. [DOI] [PubMed] [Google Scholar]
- 4.Smith NK, Jozkowski KN, and Sanders SA, Hormonal Contraception and Female Pain, Orgasm and Sexual Pleasure. The Journal of Sexual Medicine, 2014. 11(2): p. 462–470. [DOI] [PubMed] [Google Scholar]
- 5.Caruso S, et al. , Conventional vs. extended-cycle oral contraceptives on the quality of sexual life: comparison between two regimens containing 3 mg drospirenone and 20 microg ethinyl estradiol. J Sex Med, 2011. 8(5): p. 1478–85. [DOI] [PubMed] [Google Scholar]
- 6.Skrzypulec V and Drosdzol A, Evaluation of the quality of life and sexual functioning of women using a 30-microg ethinyloestradiol and 3-mg drospirenone combined oral contraceptive. Eur J Contracept Reprod Health Care, 2008. 13(1): p. 49–57. [DOI] [PubMed] [Google Scholar]
- 7.Sabatini R and Cagiano R, Comparison profiles of cycle control, side effects and sexual satisfaction of three hormonal contraceptives. Contraception, 2006. 74(3): p. 220–223. [DOI] [PubMed] [Google Scholar]
- 8.Gracia CR, et al. , Sexual function in first-time contraceptive ring and contraceptive patch users. Fertil Steril, 2010. 93(1): p. 21–8. [DOI] [PubMed] [Google Scholar]
- 9.Guida M, et al. , Sexual life impact evaluation of different hormonal contraceptives on the basis of their methods of administration. Arch Gynecol Obstet, 2014. 290(6): p. 1239–47. [DOI] [PubMed] [Google Scholar]
- 10.Bolton M, McKay A, and Schneider M, Relational influences on condom use discontinuation: A qualitative study of young adult women in dating relationships. Canadian Journal of Human Sexuality, 2010. 19(3): p. 91–104. [Google Scholar]
- 11.Fennell J, “And Isn’t that the point?”: pleasure and contraceptive decisions. Contraception, 2014. 89(4): p. 264–70. [DOI] [PubMed] [Google Scholar]
- 12.Free C, Ogden J, and Lee R, Young women’s contraception use as a contextual and dynamic behaviour: A qualitative study. Psychology & Health, 2005. 20(5): p. 673–690. [Google Scholar]
- 13.Higgins JA, et al. , Relationships between condoms, hormonal methods, and sexual pleasure and satisfaction: an exploratory analysis from the Womens Well-Being and Sexuality Study. Sexual Health, 2008. 5(4): p. 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Batar I, State-of-the-art of non-hormonal methods of contraception: II. Chemical barrier contraceptives. Eur J Contracept Reprod Health Care, 2010. 15(2): p. 89–95. [DOI] [PubMed] [Google Scholar]
- 15.Vonderheide S.g. and Mosher DL, Should I Put in my Diaphragm? Journal of Psychology & Human Sexuality, 1988. 1(1): p. 97–111. [Google Scholar]
- 16.Herbenick D, et al. , Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: a prospective daily diary study. J Sex Med, 2011. 8(1): p. 202–12. [DOI] [PubMed] [Google Scholar]
- 17.Jozkowski KN, et al. , Women’s perceptions about lubricant use and vaginal wetness during sexual activities. J Sex Med, 2013. 10(2): p. 484–92. [DOI] [PubMed] [Google Scholar]
- 18.Finer LB and Henshaw SK, Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health, 2006. 38(2): p. 90–6. [DOI] [PubMed] [Google Scholar]
- 19.Caruso S, et al. , Quality of sexual life of women using the contraceptive vaginal ring in extended cycles: preliminary report. Eur J Contracept Reprod Health Care, 2014. 19(4): p. 307–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.