ABSTRACT
Background
Several studies have reported that dietary salt intake may be an independent risk factor for overweight/obesity, but results from previous studies are controversial, reflecting study limitations such as use of a single spot urine or dietary recall to estimate daily salt intake rather than 24-h urine collections, and population samples from only a single country or center.
Objective
The aim of this study was to use data from the International Study of Macro-/Micro-nutrients and Blood Pressure (INTERMAP Study) to explore the relation between dietary salt intake estimated from 2 timed 24-h urine collections and body mass index (BMI; in kg/m2) as well as prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States.
Methods
Data were from a cross-sectional study of 4680 men and women aged 40–59 y in Japan (n = 1145), China (n = 839), the United Kingdom (n = 501), and the United States (n = 2195). General linear models were used to obtain the regression coefficients (β) of salt intake associated with BMI. Multivariable logistic regression models were used to determine the ORs and 95% CIs of overweight/obesity associated with a 1-g/d higher dietary salt intake.
Results
After adjustment for potential confounding factors including energy intake, salt intake 1 g/d higher was associated with BMI higher by 0.28 in Japan, 0.10 in China, 0.42 in the United Kingdom, and 0.52 in the United States, all P values < 0.001. Salt intake 1 g/d higher was associated with odds of overweight/obesity 21% higher in Japan, 4% higher in China, 29% higher in the United Kingdom, and 24% higher in the United States, all P values < 0.05.
Conclusions
Salt intake is positively associated with BMI and the prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States. This association needs to be further confirmed in well-designed prospective studies with repeated dietary and BMI measurements.This trial was registered at clinicaltrials.gov as NCT00005271.
Keywords: salt intake, 24-h urine sodium, body mass index, obesity, cross-sectional study
Introduction
High salt intake has been widely reported to be associated with elevated blood pressure (BP) (1–3) and increased risk of cardiovascular diseases (4, 5). Over the last few years, several studies have reported that dietary salt intake was associated with overweight/obesity and put forward a hypothesis that salt intake may be an independent risk factor for overweight/obesity in adults (6–13), but results from previous studies are controversial (14, 15). Previous studies have limitations such as use of a single spot urine (15) or dietary recall (6, 12, 14) to estimate daily salt intake, which have been criticized for large bias in estimating individual salt intake (16–18). Multiple 24-h urine collections have been recommended as the most reliable method in this field (19). A possible explanation for a valid link between salt intake and overweight/obesity is that higher salt intake may result in more fluid intake and may thereby contribute to weight increase (20). In addition, increased consumption of processed calorie-dense foods may result in excessive sodium intake, thus energy intake may be important for the relation between salt intake and overweight/obesity. Unfortunately, lack of data on energy intake has weakened the meaning of data from some previous studies (7, 10). Only a few studies in adults used 24-h urine collection to estimate salt intake with adjustment for energy intake in multivariable models and found that the relation between salt intake and obesity may be independent from energy intake (8, 9, 11, 13). However, almost all those previous studies were carried out in a single country or center, leaving large limits on the generality of their conclusions. Therefore, the present study aims to use data from the International Study of Macro-/Micro-nutrients and Blood Pressure (INTERMAP Study) to explore the relation between dietary salt intake estimated from 2 timed 24-h urine collections and BMI as well as prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States.
Methods
Study population
Participants were from the INTERMAP international epidemiologic study on relations of dietary variables with BP, including 4680 men and women aged 40–59 y from 17 population samples in Japan (4 samples), China (3 samples), the United Kingdom (2 samples), and the United States (8 samples) (21). For each participant, data collection included 2 timed 24-h urine specimens, four 24-h dietary recalls, 8 BP measurements, and data on variables possibly confounding nutrient–BP relations. Interviewer-assisted questionnaires were used to obtain data on demographic and lifestyle factors, such as smoking and drinking status and physical activity. Field work was conducted from 1996 to 1999, with strict quality control procedures undertaken at the international, national, and local levels throughout the field surveys. Details about the study populations have been reported previously (21). The participant flowchart of the present observational study (NCT00005271) is shown in Supplemental Figure 1. Written informed consent was obtained from all participants.
Dietary data collection
Each participant attended the local research center 4 times: the first 2 visits were on consecutive days, then another such pair of visits followed with an interval of 3–6 wk. Four 24-h dietary recalls (2 pairs) were performed by trained certified interviewers using the in-depth multipass 24-h recall method (22). All foods, drinks, and dietary supplements consumed in the previous 24 h were recorded. Assessment tools such as real foods, food models, measuring devices, and photographs were used in the 4 countries to assist in accurate recording. Nutrient data were derived from country-specific food tables standardized and enhanced by the Nutrition Coordinating Center, University of Minnesota (23). Dietary quality control procedures indicated generally high data quality (22).
Urine collection
Two timed 24-h urine specimens were collected with an interval of 3–6 wk, each coinciding with a pair of 24-h dietary recalls. Collections started at the local research center on the first day of each visit and were completed there the next day. The start and end times were recorded as participants began and completed the collection at the research center. Also, participants reported any missing urine on a written form; in such cases the specimen was designated “incomplete” and the participant was asked to repeat the collection. Also, the collection was repeated if the collection time fell outside the range of 22–26 h, or the total volume of urine was <500 mL. Urine aliquots were stored frozen at −20°C and air-freighted frozen to the Central Laboratory (Leuven, Belgium) within 1 y, where urinary sodium, potassium, creatinine, and other variables were measured with rigorous internal and external quality control.
Definition of overweight/obesity
Height and weight without shoes or heavy clothing were measured at 2 visits and the BMI was calculated as kg/m2. In this study, based on the WHO cutoff criteria (24), we combined the definition of overweight or obesity as BMI ≥ 25 because the numbers of cases of obesity (defined as BMI ≥ 30) in Japan (n = 25) and China (n = 29) were very small.
Statistical analysis
Data are presented as mean ± SD for continuous variables and as n (percentage) for categorical variables. Salt intake is converted from the mean of the 2 timed 24-h urine sodium values (1 g salt is equivalent to 17.1 mmol sodium), used throughout the article as a continuous variable. We tested differences in baseline characteristics between different BMI status groups with t tests for continuous variables and with χ2 tests for categorical variables. General linear models were used to obtain the regression coefficients (β) of salt intake associated with BMI. We then used multivariable logistic regression models to determine the ORs and 95% CIs of overweight/obesity associated with a 1-g/d higher dietary salt intake. In multivariate models, we sequentially adjusted for age, gender, sample center, smoking status, drinking status, years of education, physical activity in leisure time, dietary fiber intake, and total energy intake. A 2-tailed P value <0.05 was considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute).
Results
The INTERMAP Study included 4680 participants from Japan (n = 1145), China (n = 839), the United Kingdom (n = 501), and the United States (n = 2195). The study was designed to include approximately equal numbers of men and women. The mean ± SD age of the study participants was 49.2 ± 5.5 y. The characteristics of the study sample according to BMI status across the 4 countries are shown in Table 1. Overall, those participants who were overweight/obese were more likely to be men, older, consumed more calories, and were less physically active. Overweight/obese participants had higher salt intake than those with normal BMI in all 4 countries.
TABLE 1.
Characteristics of the study population according to BMI status1
| Japan | China | United Kingdom | United States | All | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <25 | ≥25 | <25 | ≥25 | <25 | ≥25 | <25 | ≥25 | <25 | ≥25 | |
| n | 839 | 306 | 625 | 214 | 152 | 349 | 620 | 1575 | 2236 | 2444 |
| Male | 399 (47.6) | 175 (57.2)** | 349 (55.8) | 67 (31.3)** | 60 (39.5) | 206 (59.0)** | 226 (36.5) | 877 (55.7)** | 1034 (46.2) | 1325 (54.2)** |
| Age, y | 49.2 ± 5.3 | 49.9 ± 5.3* | 49.2 ± 5.9 | 48.3 ± 5.4 | 47.3 ± 5.5 | 49.9 ± 5.5** | 48.8 ± 5.3 | 49.3 ± 5.4* | 48.9 ± 5.5 | 49.4 ± 5.4** |
| Education, y | 12.0 ± 2.0 | 12.1 ± 2.2 | 5.5 ± 2.9 | 5.2 ± 2.8 | 13.1 ± 3.0 | 12.5 ± 3.1 | 15.5 ± 2.9 | 14.8 ± 3.1** | 11.2 ± 4.6 | 13.3 ± 4.0** |
| Smoking status | ||||||||||
| Current | 249 (29.7) | 97 (31.7)* | 254 (40.6) | 51 (23.8)** | 26 (17.1) | 61 (17.5) | 102 (16.5) | 267 (17.0)** | 631 (28.2) | 476 (19.5)** |
| Former | 103 (12.3) | 54 (17.7) | 50 (8.0) | 19 (8.9) | 35 (23.0) | 112 (32.1) | 159 (25.7) | 518 (32.9) | 347 (15.5) | 703 (28.8) |
| Never | 487 (58.1) | 155 (50.7) | 321 (51.4) | 144 (67.3) | 91 (59.9) | 176 (50.4) | 359 (57.9) | 790 (50.2) | 1258 (56.3) | 1265 (51.8) |
| Current alcohol | 759 (90.5) | 280 (91.5) | 305 (48.8) | 77 (36.0)** | 141 (92.8) | 303 (86.8) | 447 (72.1) | 1086 (69.0) | 1652 (73.9) | 1746 (71.4) |
| drinkers | ||||||||||
| Physical activity in leisure time | ||||||||||
| A lot | 231 (27.5) | 57 (18.6)** | 105 (16.8) | 13 (6.1)** | 15 (9.9) | 23 (6.6)* | 76 (12.3) | 127 (8.1)** | 427 (19.1) | 220 (9.0)** |
| Moderate | 269 (32.1) | 120 (39.2) | 237 (37.9) | 77 (36.0) | 77 (50.7) | 148 (42.4) | 349 (56.3) | 801 (50.9) | 932 (41.7) | 1146 (46.9) |
| Little or none | 339 (40.4) | 129 (42.2) | 283 (45.3) | 124 (57.9) | 60 (39.5) | 178 (51.0) | 195 (31.5) | 647 (41.1) | 877 (39.2) | 1078 (44.1) |
| Energy intake, kcal/d | 2012 ± 435 | 2112 ± 478** | 2033 ± 588 | 2051 ± 546 | 2166 ± 631 | 2169 ± 633 | 2058 ± 638 | 2317 ± 708** | 2041 ± 555 | 2247 ± 667** |
| Total fiber intake, g/d | 15.5 ± 4.8 | 16.0 ± 4.8 | 27.9 ± 9.4 | 29.2 ± 9.7 | 25.3 ± 8.9 | 25.6 ± 9.4 | 19.2 ± 8.3 | 19.1 ± 7.7 | 20.6 ± 9.2 | 20.5 ± 8.7 |
| Salt intake,2 g/d | 11.1 ± 3.0 | 13.1 ± 3.6** | 12.7 ± 6.0 | 15.1 ± 5.2** | 7.3 ± 2.3 | 9.0 ± 3.0** | 7.9 ± 2.6 | 10.1 ± 3.6** | 10.4 ± 4.4 | 10.8 ± 4.1** |
Values are mean ± SD or n (%) unless otherwise indicated. BMI in kg/m2. We tested differences in baseline characteristics between different BMI status groups with t tests for continuous variables and with χ2 tests for categorical variables.*P < 0.05, **P < 0.01.
Calculated with a mean of 2 timed 24-h urine sodium values.
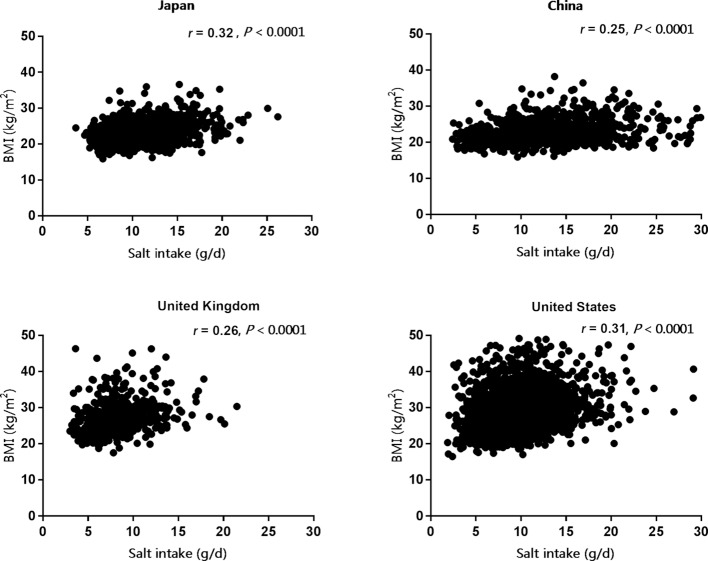
The scatterplots of salt intake against BMI in Japan, China, the United Kingdom, and the United States are presented in Figure 1. The regression coefficients (β) of salt intake associated with BMI are shown in Table 2. The mean ± SD daily salt intake in Japan, China, the United Kingdom, and the United States was 11.6 ± 3.3, 13.3 ± 5.9, 8.5 ± 2.9, and 9.5 ± 3.5 g, respectively. The mean ± SD BMI in these 4 countries was 23.4 ± 2.9, 23.1 ± 3.4, 27.5 ± 4.6, and 28.9 ± 5.9, respectively. After adjustment for several potential confounding factors including daily total energy intake, salt intake 1 g/d higher was associated with BMI 0.28 higher in Japan, 0.10 higher in China, 0.42 higher in the United Kingdom, and 0.52 higher in the United States, all P values < 0.001.
FIGURE 1.
Scatterplots of salt intake vs. BMI in Japan, China, the United Kingdom, and the United States. r was calculated by correlation analysis.
TABLE 2.
Regression coefficients (β) and 95% CIs of salt intake associated with BMI1
| Model 12 | Model 23 | Model 34 | ||||||
|---|---|---|---|---|---|---|---|---|
| Salt intake, g/d | BMI, kg/m2 | β (95% CI) | P value | β (95% CI) | P value | β (95% CI) | P value | |
| Japan | 11.6 ± 3.3 | 23.4 ± 2.9 | 0.28 (0.23, 0.33) | <0.0001 | 0.28 (0.23, 0.33) | <0.0001 | 0.28 (0.23, 0.34) | <0.0001 |
| China | 13.3 ± 5.9 | 23.1 ± 3.4 | 0.11 (0.06, 0.16) | <0.0001 | 0.11 (0.06, 0.15) | <0.0001 | 0.10 (0.05, 0.14) | 0.0001 |
| United | 8.5 ± 2.9 | 27.5 ± 4.6 | 0.40 (0.25, 0.55) | <0.0001 | 0.41 (0.27, 0.56) | <0.0001 | 0.42 (0.27, 0.56) | <0.0001 |
| Kingdom | ||||||||
| United States | 9.5 ± 3.5 | 28.9 ± 5.9 | 0.57 (0.50, 0.64) | <0.0001 | 0.53 (0.46, 0.60) | <0.0001 | 0.52 (0.45, 0.59) | <0.0001 |
| All | 10.6 ± 4.2 | 26.4 ± 5.5 | 0.36 (0.32, 0.40) | <0.0001 | 0.35 (0.31, 0.38) | <0.0001 | 0.34 (0.30, 0.38) | <0.0001 |
Values are mean ± SD unless otherwise indicated. β (95% CI) was calculated by general linear models.
Model 1 adjusted for age, gender, and sample center.
Model 2 further adjusted for smoking status, drinking status, years of education, and physical activity in leisure time.
Model 3 further adjusted for total energy intake and dietary fiber intake.
Table 3 shows the prevalence of overweight/obesity and the relation between salt intake and the prevalence of overweight/obesity in the 4 countries. The prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States was 26.7%, 25.5%, 69.7%, and 71.8%, respectively. Multivariable logistic regression models showed a positive relation between salt intake and the prevalence of overweight/obesity after adjustment for age, gender, sample center, smoking status, drinking status, years of education, and physical activity in leisure time. This relation persisted when we further adjusted for total energy intake. Salt intake 1 g/d higher was associated with odds of overweight/obesity 21% higher in Japan, 4% higher in China, 29% higher in the United Kingdom, and 24% higher in the United States, all P values < 0.05.
TABLE 3.
ORs (95% CIs) of salt intake in relation to overweight/obesity1
| Overweight/obesity,n (%) | Model 12 | Model 23 | Model 34 | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||
| Japan | 306 (26.7) | 1.21 (1.15, 1.26) | <0.0001 | 1.21 (1.16, 1.27) | <0.0001 | 1.21 (1.16, 1.27) | <0.0001 |
| China | 214 (25.5) | 1.06 (1.02, 1.09) | 0.0028 | 1.05 (1.02, 1.09) | 0.0041 | 1.04 (1.00, 1.08) | 0.0332 |
| United Kingdom | 349 (69.7) | 1.24 (1.13, 1.36) | <0.0001 | 1.26 (1.15, 1.39) | <0.0001 | 1.29 (1.17, 1.42) | <0.0001 |
| United States | 1575 (71.8) | 1.25 (1.20, 1.30) | <0.0001 | 1.24 (1.19, 1.29) | <0.0001 | 1.24 (1.19, 1.29) | <0.0001 |
| All | 2444 (52.2) | 1.16 (1.14, 1.19) | <0.0001 | 1.16 (1.14, 1.18) | <0.0001 | 1.16 (1.13, 1.18) | <0.0001 |
Overweight/obesity was defined as BMI ≥ 25 kg/m2. OR (95% CI) was calculated by logistic regression models.
Model 1 adjusted for age, gender, and sample center.
Model 2 further adjusted for smoking status, drinking status, years of education, and physical activity in leisure time.
Model 3 further adjusted for total energy intake and dietary fiber intake.
As a sensitivity analysis, we excluded 628 participants who reported the use of any special diet for medical, weight-loss, or other purposes, of which 76 were in Japan, 45 in China, 106 in the United Kingdom, and 401 in the United States. The associations between dietary salt intake and BMI as well as the ORs of overweight/obesity were somewhat attenuated in some countries but remained significant in all these 4 countries (see Supplemental Tables 1 and 2).
Discussion
In this international multicenter population study, we found a consistently significant association between dietary salt intake and BMI as well as the odds of overweight/obesity in Japan, China, the United Kingdom, and the United States, with adjustment for potential confounding factors including total energy intake. These findings have both important clinical and public health implications in that reducing salt intake, in addition to lowering BP, may also lower BMI and the prevalence of overweight/obesity, and thereby reduce the risk of main cardiovascular diseases.
Our results are consistent with those of several previous studies, although most of these had methodological problems, namely the use of either spot urine (15) or dietary recall methods (6, 12, 14) to estimate individual salt intake rather than 24-h urine collections. Energy intake is the most important confounding factor for the link between salt intake and overweight/obesity because high salt intake may stimulate thirst and appetite and lead to more energy intake (20), and some previous studies did not include total energy intake in their analysis (7, 10). Only a few studies in adults used 24-h urine collection to estimate salt intake and adjusted for energy intake in multivariable models. A study based on the UK National Diet and Nutrition Survey rolling program including 785 adults reported that a 1-g/d higher salt intake was associated with 26% higher odds of overweight or obesity (OR: 1.26; 95% CI: 1.16, 1.37) after adjusting for several potential confounding factors including energy intake (8), a finding similar to our results from the UK sample. We found that 1-g/d higher salt was associated with 29% (OR: 1.29; 95% CI: 1.17, 1.42) higher odds of overweight/obesity in the United Kingdom. A cross-sectional study of 1043 Japanese women aged 18–22 y found that the 24-h urine-derived sodium intake was associated with higher odds of obesity; the adjusted OR (95% CI) of the highest quartile was 2.49 (1.15, 5.42) compared with the lowest quartile of sodium intake (9). A study analyzed cross-sectional data of 640 healthy adults from South Korea and found a positive association between higher sodium intake as assessed by 24-h urinary sodium excretion and obesity independent of energy intake (11). A cross-sectional study based on data from a sample of 730 participants aged 20–69 y found that a 1000-mg/d higher sodium excretion was significantly associated with a 3.8-higher BMI (95% CI: 2.8, 4.8), adjusted for covariates. Compared with participants in the lowest quartile of sodium excretion, the adjusted prevalence ratio in the highest quartile was 1.93 (95% CI: 1.69, 2.20) for overweight/obesity (13). A longitudinal population study that enrolled 215 Danish participants found a significant association of 24-h sodium excretion with body fat and fat-free mass, but the power of this study was limited owing to the small sample size (25).
The mechanisms underlying the salt intake relation to obesity remain unclear. A possible explanation is that higher salt intake is associated with excessive energy intake, but our results along with the considerable previous evidence indicate that there may be a direct link between dietary salt intake and overweight/obesity independent of energy intake. This association remained significant when we excluded participants with any special diet during the study or stratified by energy intake (Supplemental Table 3) as sensitivity analyses. Recent experimental research in mice showed that high intake of salt activates the aldose reductase–fructokinase pathway in the liver and hypothalamus, leading to endogenous fructose production with the development of leptin resistance causing obesity (26). Other studies showed that a high-salt diet enhanced adipocyte insulin sensitivity for glucose uptake and the insulin-induced glucose metabolism, promoting adipocyte hypertrophy and increasing the mass of white adipose tissue and leptin production in rats (27, 28). Results from a human study also showed that a high-salt diet increased fasting ghrelin, which regulates appetite, glucose homeostasis, and fat deposition, and may be a novel underlying mechanism of obesity (29).
As far as we know, the present study is the first to explore the association between dietary salt intake and overweight/obesity in multicountry populations with a large sample size. Our study used 2 timed 24-h urine collections to estimate salt intake and 4 in-depth multipass 24-h dietary recalls for estimating daily dietary intake. Strict quality control procedures for both urine collections and dietary recalls added data reliability in our study. Several limitations in our study also need to be addressed. First, energy intake in our study was derived from 24-h dietary recalls but not more accurate methods such as the doubly labeled water method. Previous studies have demonstrated a bias toward underestimation when using 24-h dietary recalls for estimating total energy intake, especially among those that are obese (30–32). Nevertheless, there were no essential changes in the association between salt intake and BMI when we excluded 945 participants who were obese as a sensitivity analysis (Supplemental Table 4). Second, 2 urinary measurements may not be reflective of long-term dietary habits, but similar results were found for each urinary measurement compared with the combined exposure measurement analysis (Supplemental Tables 5 and 6). Third, the cross-sectional study design makes it impossible to conclude that there were causal relations between salt intake and overweight/obesity because the time sequence of exposure factors and outcomes is not clear; long-term prospective cohort analysis with repeated dietary and BMI measurements may provide clearer answers.
In conclusion, findings from the INTERMAP Study indicate that dietary salt intake is positively associated with BMI and the prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States, and this relation was independent of total energy intake. This association needs to be further confirmed in well-designed prospective studies with repeated dietary and BMI measurements.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—JS, LVH, MLD, ARD, KM, NO, YW, HU, PE, and L Zhao: were involved in the design and conduct of the INTERMAP Study; L Zhou, JS, QC, and L Zhao: designed the present study; L Zhou: performed the data analysis and drafted the manuscript; and all authors: read and approved the final manuscript. PE is a member of Consensus Action on Salt and Health and a member of the Agency for Healthcare Research and Quality Systematic Review on the Effects of Dietary Sodium and Potassium Intake on Health sponsored by the US NIH and US CDC. YW and PE are members of World Action on Salt and Health. None of the other authors reported a conflict of interest related to the study.
Notes
The INTERMAP Study is supported by the National Heart, Lung, and Blood Institute, NIH grants R01-HL50490 and R01-HL84228; by Ministry of Education, Science, Sports, and Culture (Japan) grant 090357003; by a project grant from West Midlands National Health Service Research and Development (United Kingdom); and by Chest, Heart, and Stroke Association (Northern Ireland, United Kingdom) grant R2019EPH.
All authors take responsibility for the reliability and freedom from bias of the data presented and their interpretation. The funding sources had no role in the design, analysis, or writing of this article.
Supplemental Figure 1 and Supplemental Tables 1–6 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
References
- 1. Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M; Intersalt Cooperative Research Group. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. BMJ. 1996;312:1249–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 3. Stamler J, Chan Q, Daviglus ML, Dyer AR, Van Horn L, Garside DB, Miura K, Wu Y, Ueshima H, Zhao L et al.. Relation of dietary sodium (salt) to blood pressure and its possible modulation by other dietary factors: the INTERMAP study. Hypertension. 2018;71:631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Song HJ, Cho YG, Lee HJ. Dietary sodium intake and prevalence of overweight in adults. Metabolism. 2013;62:703–8. [DOI] [PubMed] [Google Scholar]
- 7. Yi SS, Kansagra SM. Associations of sodium intake with obesity, body mass index, waist circumference, and weight. Am J Prev Med. 2014;46:e53–5. [DOI] [PubMed] [Google Scholar]
- 8. Ma Y, He FJ, MacGregor GA. High salt intake: independent risk factor for obesity?. Hypertension. 2015;66:843–9. [DOI] [PubMed] [Google Scholar]
- 9. Murakami K, Livingstone MB, Sasaki S, Uenishi K. Ability of self-reported estimates of dietary sodium, potassium and protein to detect an association with general and abdominal obesity: comparison with the estimates derived from 24 h urinary excretion. Br J Nutr. 2015;113:1308–18. [DOI] [PubMed] [Google Scholar]
- 10. Ge Z, Zhang J, Chen X, Yan L, Guo X, Lu Z, Xu A, Ma J. Are 24 h urinary sodium excretion and sodium:potassium independently associated with obesity in Chinese adults?. Public Health Nutr. 2016;19:1074–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nam GE, Kim SM, Choi MK, Heo YR, Hyun TS, Lyu ES, Oh SY, Park HR, Ro HK, Han K et al.. Association between 24-h urinary sodium excretion and obesity in Korean adults: a multicenter study. Nutrition. 2017;41:113–19. [DOI] [PubMed] [Google Scholar]
- 12. Elfassy T, Mossavar-Rahmani Y, Van Horn L, Gellman M, Sotres-Alvarez D, Schneiderman N, Daviglus M, Beasley JM, Llabre MM, Shaw PA et al.. Associations of sodium and potassium with obesity measures among diverse US Hispanic/Latino adults: results from the Hispanic Community Health Study/Study of Latinos. Obesity (Silver Spring). 2018;26:442–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhao L, Cogswell ME, Yang Q, Zhang Z, Onufrak S, Jackson SL, Chen T-C, Loria CM, Wang C-Y, Wright JD et al.. Association of usual 24-h sodium excretion with measures of adiposity among adults in the United States: NHANES, 2014. Am J Clin Nutr. 2019;109:139–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lampure A, Castetbon K, Deglaire A, Schlich P, Peneau S, Hercberg S, Mejean C. Associations between liking for fat, sweet or salt and obesity risk in French adults: a prospective cohort study. Int J Behav Nutr Phys Act. 2016;13:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oh SW, Koo HS, Han KH, Han SY, Chin HJ. Associations of sodium intake with obesity, metabolic disorder, and albuminuria according to age. PLoS One. 2017;12:e0188770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhou L, Tian Y, Fu JJ, Jiang YY, Bai YM, Zhang ZH, Hu XH, Lian HW, Guo M, Yang ZX et al.. Validation of spot urine in predicting 24-h sodium excretion at the individual level. Am J Clin Nutr. 2017;105:1291–6. [DOI] [PubMed] [Google Scholar]
- 17. Mercado CI, Cogswell ME, Valderrama AL, Wang CY, Loria CM, Moshfegh AJ, Rhodes DG, Carriquiry AL. Difference between 24-h diet recall and urine excretion for assessing population sodium and potassium intake in adults aged 18–39 y. Am J Clin Nutr. 2015;101:376–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wen X, Zhou L, Stamler J, Chan Q, Van Horn L, Daviglus ML, Dyer AR, Elliott P, Ueshima H, Miura K et al.. Agreement between 24-h dietary recalls and 24-h urine collections for estimating sodium intake in China, Japan, UK, USA: the International Study of Macro- and Micro-nutrients and Blood Pressure. J Hypertens. 2019;37:814–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cogswell ME, Mugavero K, Bowman BA, Frieden TR. Dietary sodium and cardiovascular disease risk—measurement matters. N Engl J Med. 2016;375:580–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity?. Hypertension. 2008;51:629–34. [DOI] [PubMed] [Google Scholar]
- 21. Stamler J, Elliott P, Dennis B, Dyer AR, Kesteloot H, Liu K, Ueshima H, Zhou BF. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary). J Hum Hypertens. 2003;17:591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dennis B, Stamler J, Buzzard M, Conway R, Elliott P, Moag-Stahlberg A, Okayama A, Okuda N, Robertson C, Robinson F et al.. INTERMAP: the dietary data—process and quality control. J Hum Hypertens. 2003;17:609–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schakel SF, Dennis BH, Wold AC, Conway R, Zhao L, Okuda N, Okayama A, Moag-Stahlberg A, Robertson C, Van Heel N et al.. Enhancing data on nutrient composition of foods eaten by participants in the INTERMAP Study in China, Japan, the United Kingdom and the United States. J Food Compos Anal. 2003;16:395–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- 25. Larsen SC, Angquist L, Sorensen TI, Heitmann BL. 24 h urinary sodium excretion and subsequent change in weight, waist circumference and body composition. PLoS One. 2013;8:e69689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lanaspa MA, Kuwabara M, Andres-Hernando A, Li N, Cicerchi C, Jensen T, Orlicky DJ, Roncal-Jimenez CA, Ishimoto T, Nakagawa T et al.. High salt intake causes leptin resistance and obesity in mice by stimulating endogenous fructose production and metabolism. Proc Natl Acad Sci USA. 2018;115:3138–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fonseca-Alaniz MH, Takada J, Andreotti S, de Campos TB, Campaña AB, Borges-Silva CN, Lima FB. High sodium intake enhances insulin-stimulated glucose uptake in rat epididymal adipose tissue. Obesity (Silver Spring). 2008;16:1186–92. [DOI] [PubMed] [Google Scholar]
- 28. Fonseca-Alaniz MH, Brito LC, Borges-Silva CN, Takada J, Andreotti S, Lima FB. High dietary sodium intake increases white adipose tissue mass and plasma leptin in rats. Obesity (Silver Spring). 2007;15:2200–8. [DOI] [PubMed] [Google Scholar]
- 29. Zhang Y, Li F, Liu FQ, Chu C, Wang Y, Wang D, Guo TS, Wang JK, Guan GC, Ren KY et al.. Elevation of fasting ghrelin in healthy human subjects consuming a high-salt diet: a novel mechanism of obesity?. Nutrients. 2016;8:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Heitmann BL, Lissner L. Dietary underreporting by obese individuals—is it specific or non-specific?. BMJ. 1995;311:986–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goris AH, Westerterp-Plantenga MS, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr. 2000;71:130–4. [DOI] [PubMed] [Google Scholar]
- 32. Hise ME, Sullivan DK, Jacobsen DJ, Johnson SL, Donnelly JE. Validation of energy intake measurements determined from observer-recorded food records and recall methods compared with the doubly labeled water method in overweight and obese individuals. Am J Clin Nutr. 2002;75:263–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.