Highlights
-
•
Alexithymia is more closely related to suicide ideation than to suicide behaviour.
-
•
The subcomponents of difficulty identifying and describing feelings are more closely related to suicide ideation and behaviour than the subcomponent of externally oriented thinking.
-
•
The relationship between alexithymia and suicide ideation appears robust when controlling for confounding variables, though the relationship between suicide behaviour and alexithymia is not so robust.
-
•
Future research should aim to examine causality in this relationship through using longitudinal designs.
Keywords: Suicide, Alexithymia, Depression, Meta-analysis
Abstract
Background
Alexithymia reflects a difficulty with identifying and expressing emotions. This experience has been proposed as having an association with suicide ideation and behaviour. This review aimed to synthesise the evidence to establish the bivariate and multivariate relationships between alexithymia, and its subcomponents, with suicide ideation and behaviour.
Methods
Search terms related to alexithymia and suicide ideation and behaviour were searched across nine prominent databases in May 2018. Studies were eligible for inclusion if they reported original empirical quantitative findings from adult samples, used a validated measure of alexithymia, and any measure of suicide ideation or behaviour.
Results
Thirty-four studies were eligible for inclusion in this review. The review found a large effect size for the relationship between alexithymia and suicide ideation (r = 0.54, 95% CI= 0.40–0.65) and a small effect size for the relationship between alexithymia and suicide behaviour (r = 0.25, 95% CI = 0.16–0.34).
Limitations
A high level of heterogeneity was found in the meta-analysis meaning that results should be interpreted with caution.
Conclusion
A positive association was found between alexithymia and suicide ideation and, to a lesser extent, behaviour across a range of clinical and general population samples. This review has potentially important clinical implications, and promotes the need for suicide prevention to focus on emotion regulation skills.
1. Introduction
Globally, approximately 800,000 people die by suicide every year (WHO, 2014). Suicide is the most common cause of death for men aged 20–49 years in England and Wales (Office for National Statistics, 2016) and it is estimated that one person in fifteen has made a suicide attempt at some point in their life (McManus et al., 2016). Further to this, lifetime prevalence of suicide ideation in Europe is estimated at 5.6% (Hardt et al., 2015). Suicide ideation has been found to be related to emotional distress (Vilhjálmsson et al., 1998), and more severe psychopathological symptoms (Reinherz et al., 2006). It has therefore been advocated that suicide ideation be considered as a key clinical outcome in its own right (Tarrier et al., 2008).
Suicidality is operationalised in this review as comprising three main factors; suicide ideation, suicide behaviour and suicide risk. In this review, suicide ideation refers to thoughts, plans and wishes to end life through suicide either alongside or separate from attempting suicide (Beck et al., 1972). Suicide behaviour encompasses a wide range of self-inflicted behaviours which could potentially end a person's life. This may include but is not limited to; self-harm behaviours, suicide attempts, completed suicides and expressing suicidal plans (Silverman et al., 2007). In this review, suicide behaviour specifically refers to suicide attempts only; other aspects of suicide behaviour mentioned above are unfortunately beyond the scope of this review. Finally, in this review, suicide risk reflects a composite measure of various risk factors previously found to be associated with those who have attempted suicide compared to those who have not (Plutchik et al., 1989).
Research investigating causes of suicide should consider factors that predict suicide ideation, and those that may explain the transition from suicide ideation to suicide behaviour (Klonsky and May 2015). This is supported by findings that the correlates of suicide ideation and behaviour could be markedly different. For instance, a recent meta-analysis suggested that whilst factors such as depression and hopelessness distinguished people experiencing suicide ideation from people who had never experienced suicidality, these same factors did not distinguish between those experiencing suicide ideation and those who acted on these thoughts (May and Klonsky, 2016). It is therefore important that research exploring the clinical correlates of suicide aims to look specifically at correlates of suicide ideation and suicide behaviour separately.
It has been frequently observed that a common antecedent to suicidal thoughts and behaviours is the experience of unmanageable emotional distress (Dour et al., 2011, Shneidman, 1998). Furthermore, individuals who experience greater difficulty in regulating high levels of emotional distress are more likely to die by suicide (Pisani et al., 2013). It has therefore been suggested that emotional dysregulation may have a considerable impact on suicidal thoughts and behaviours. Emotion dysregulation has been defined as a multidimensional construct involving maladaptive ways of responding to emotions, regardless of their intensity (Gratz and Tull, 2010). Evidence has now been found for a relationship between suicidal thoughts and behaviours and emotional under-regulation strategies, such as rumination (Morrison and O'connor, 2008), as well as emotional over-regulation strategies, such as emotional avoidance (Najmi et al., 2007).
Related to emotion dysregulation is the concept of alexithymia, defined as the inability to identify or express emotions (Sifneos, 1973). Whilst originally perceived to be a personality trait, it has since been defined as a form of emotion regulation (Salminen et al., 2006, Taylor, 2000). Since its inception in the field of psychosomatics, alexithymia has been described as having five main components: i) a difficulty in identifying one's emotions ii) a difficulty in describing self-feelings verbally iii) a reduction or incapability to experience emotions iv) an externally orientated cognitive style and v) poor capacity for fantasising or symbolic thought (Taylor and Bagby, 2000). Alexithymia is most commonly measured using the Toronto Alexithymia Scale (Bagby et al., 1994), which comprises three main factors. Difficulty identifying feelings (DIF) assesses a person's ability to recognise their emotions, difficulty describing feelings (DDF) assesses a person's ability to communicate their emotions to others, and externally oriented thinking (EOT) assesses a person's tendency to focus their attention externally.
One concept that may link alexithymia to suicide ideation and behaviour is depression. Indeed, depressed patients have been found to experience a greater severity of alexithymia than individuals with other psychiatric disorders (Bankier et al., 2001, Leweke et al., 2012). Several studies have found a relationship between alexithymia and depression with a recent meta-analysis finding that alexithymia severity scores were moderately correlated to scores of depression severity in a range of clinical and general population samples (r = 0.46; Li et al., 2015). Given the close relationship between depression and suicide behaviour (Blackmore et al., 2008), it therefore seems plausible that depression might play a role in the posited relationship between alexithymia and suicidal thoughts and behaviours. Indeed it has been found that depression mediates the relationship between alexithymia and suicide risk (DeBerardis et al., 2017).
In addition to alexithymia impacting on suicidal thoughts and behaviours via depression, this relationship has also been found to exist independently of depression (e.g. Kim et al., 2016). It has been suggested that individuals with alexithymia may experience emotional information as overwhelming and confusing, which can lead to feelings of helplessness (Foran and O'Leary, 2013). Furthermore, effective emotion regulation is centred on both the ability to identify one's feelings (emotional clarity) alongside the ability to respond and recover from negative emotions (access to effective strategies; (Gratz and Roemer, 2004)). Thus, for individuals with poor emotional clarity, it is more difficult to progress to effectively regulate these emotions. Conversely, individuals experiencing alexithymia frequently utilise maladaptive coping strategies, such as social isolation, behavioural disengagement and emotional inhibition (Velasco et al., 2001). It is therefore hypothesised that individuals experiencing alexithymia may become motivated towards suicide ideation and behaviour due to an impaired / limited awareness of alternate ways of coping with the unnameable feelings they are experiencing.
1.1. Aims of the study
A range of studies have now linked alexithymia with suicide ideation and behaviour, however, there has been no synthesis of the research to date which examines this relationship. There are therefore several unanswered questions about this relationship, including whether particular features of alexithymia are specifically related to suicide ideation and behaviour, and whether alexithymia is more closely related to the development of suicide ideation or behaviour. Further to this, it is unclear whether specific mechanisms play a role in the facilitation of suicidal thoughts and behaviours in those who are experiencing alexithymia. The current systematic review therefore aims to synthesise the evidence on the relationship between alexithymia and suicide ideation and/or behaviour and to compare the relationships between alexithymia and suicide ideation / behaviour. Specifically, it was hypothesised that:
-
1
There will be a relationship between alexithymia, and its subcomponents, with suicidal ideation in adults
-
2
There will be a relationship between alexithymia, and its subcomponents, with suicidal behaviour in adults
2. Materials and methods
A protocol for the current systematic review can be found on the CRD Prospero website (ref: CRD42017069076)
2.1. Search strategy
The review was conducted and reported as per the Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). The following databases were searched for eligible studies: PsycINFO, EMBASE, MEDLINE, PubMed, Web of Science ASSIA, Sociological Abstracts, CINAHL, ComDisDome and Cochrane Trials Library.
The first search term related to alexithymia and was “alexithymi*”. This search term was specific to the concept of alexithymia, due to the review focussing only on the relationship between alexithymia and suicide ideation and behaviour, as opposed to similar but broader constructs such as emotion dysregulation.
The alexithymia search term was linked with the Boolean operator ‘AND’ to a set of search terms that related to suicide ideation and behaviour: “suicid*” OR “parasuicid*” OR “suicid* ideation” OR hopeless* OR “self-harm*” OR “deliberate self-harm*” OR “DSH” OR “attempt* suicide” OR “overdos*” OR “self-injur*” OR “self-destruct*” OR “self-inflict*” OR “self-mutilat*” OR “self-poison*” OR “self-immolat*” OR automutilat* OR “auto-mutilat*” OR “self-cut*” OR “auto-destruct*” OR “non-suicidal self injur*” OR “NSSI”. Given the difficulties in differentiating between self-harm and suicidal behaviour, the suicide search terms were purposefully broad to include papers that may report both on suicide behaviour and self-harm. These search terms were used in initial screening searches, and were found to elicit all eligible studies.
Full database searches were conducted in May 2018, with no limit on the year of published studies to be included in the review. To ensure the search was as inclusive as possible, including the grey literature, ‘citation chaining’ was performed, whereby the ‘cited-by’ function in Google Scholar was used to identify any eligible studies that had cited studies included in the review, and the reference lists of included studies were screened to identify any studies that the search terms had not identified. Despite critiques that Google Scholar may contain inadequacies (Vine, 2006), Google Scholar has been found to be of sound utility in its search functions, in fact often returning unique citations (Falagas et al., 2008).
2.2. Eligibility criteria
The following criteria were used to identify eligible studies:
-
1
An empirical study in English language
-
2
Included a validated measure of alexithymia (validated measures had to have at least one other study published on the psychometric properties of the scale)
-
3
Included any measure of suicide ideation or behaviour
-
4
Reported on the relationship between alexithymia and suicide ideation or behaviour
-
5
Studies in which at least two thirds of the sample were aged sixteen or over (deciphered either from the age range, or where this information was not available, from calculating the mean age minus one standard deviation)
Samples aged sixteen years or under were excluded in the present review on the theoretical basis that emotions and concurrent emotion regulation strategies are not fully formed at this young age (Zeman et al., 2006), and thus alexithymia may not be an appropriate concept for this age group. Further to this, there is an empirical issue in the measurement of alexithymia in this age group, as it has been noted that the Toronto Alexithymia Scale has not yet been validated with this age group and in fact demonstrated poor internal consistency with younger age groups (Parker et al., 2010).
Studies were excluded on the following basis:
-
1
Did not report original findings (e.g. reviews, book chapters, clinical guidelines, conference abstracts, letters, case studies, study protocols)
-
2
Use of qualitative methods only
2.3. Study selection and risk of bias
The first author screened the search results at title and abstract level against the identified eligibility criteria. In addition, an independent researcher screened 20% to provide a measure of the reliability of the screening process. The two researchers had an agreement rate of 97%, (Cohen's Kappa = 0.92, p<.001). The first author then screened eligible results at full study level, with an independent researcher also screening 20%. The two researchers had an agreement rate of 95% (Cohen's Kappa = 0.87, p<.001). Any disagreements that could not be resolved through consensus were discussed with a third reviewer (DP).
The first author then extracted data using a pre-piloted data extraction form. The data extraction form was piloted with three eligible studies. The data extraction form elicited the following information from each study: title, authors, year of publication, country, funding sources, conflicts of interest, research aims, research design, measures used, analyses conducted, number of participants, participant response rate, sample characteristics and demographics, results of analysis.
A revised version of the AXIS tool (Downes et al., 2016) was utilised to assess risk of bias for all cross-sectional studies included in the review. An additional question was added for case-control studies (“Are cases clearly defined and differentiated from controls?”). In addition, an independent researcher assessed risk of bias in twenty percent of full studies to provide a measure of reliability of this assessment process and there was good agreement between the two raters.
2.4. Synthesis of results
Meta-analyses of standardised mean differences and correlations were performed using the MetaXL v5.3 (Barendregt and Doi, 2010) add-in for Microsoft Office Excel. The effect size used in the meta-analyses was the correlation coefficient. The Fisher's Z transformation was applied to correlation coefficients to stabilize their variance prior to inclusion within the meta-analysis (Borenstein et al., 2011). The results were then converted back into correlation coefficients to aid interpretation. The standard error for these effect sizes was calculated from the sample size (see equations in Borenstein et al., 2011). Where correlation coefficients were not available, Cohen's D scores were calculated to ascertain the effect size of mean differences. The Cohen's D score was then converted into a correlation coefficient.
Meta-analyses were performed using a random-effects model due to expected differences between studies in the definition and measurement of suicide ideation and behaviour. The I2 statistic was calculated to estimate inconsistency, as this statistic estimates the proportion of variance explained by heterogeneity (Higgins and Thompson, 2002). According to Higgins and Thompson (2002), an I2 value of over 75% indicates high heterogeneity. Heterogeneity was addressed by examining possible outliers via visual inspection of forest plots, and where appropriate, using post-hoc sensitivity analysis to remove these outliers.
Effect sizes of the relationship between alexithymia and suicide ideation / behaviour were compared by contrasting effect sizes and their precision using Cohen's (Cohen, 1988) framework of effect sizes as a guideline. Formal decision rules were not deemed appropriate due to the differences in effect sizes needing to be considered within the wider context of study characteristics and methodological quality.
3. Results
Authors of papers which reported on the relationship between alexithymia and suicide ideation or behaviour but did not report a statistical analysis were contacted to provide the statistical analysis of this relationship. A total of fourteen authors were contacted. Ten authors did not reply, three replied explaining they were unable to provide the analysis and one replied supplying the analysis requested, rendering this paper eligible for inclusion (Meaney et al., 2016).
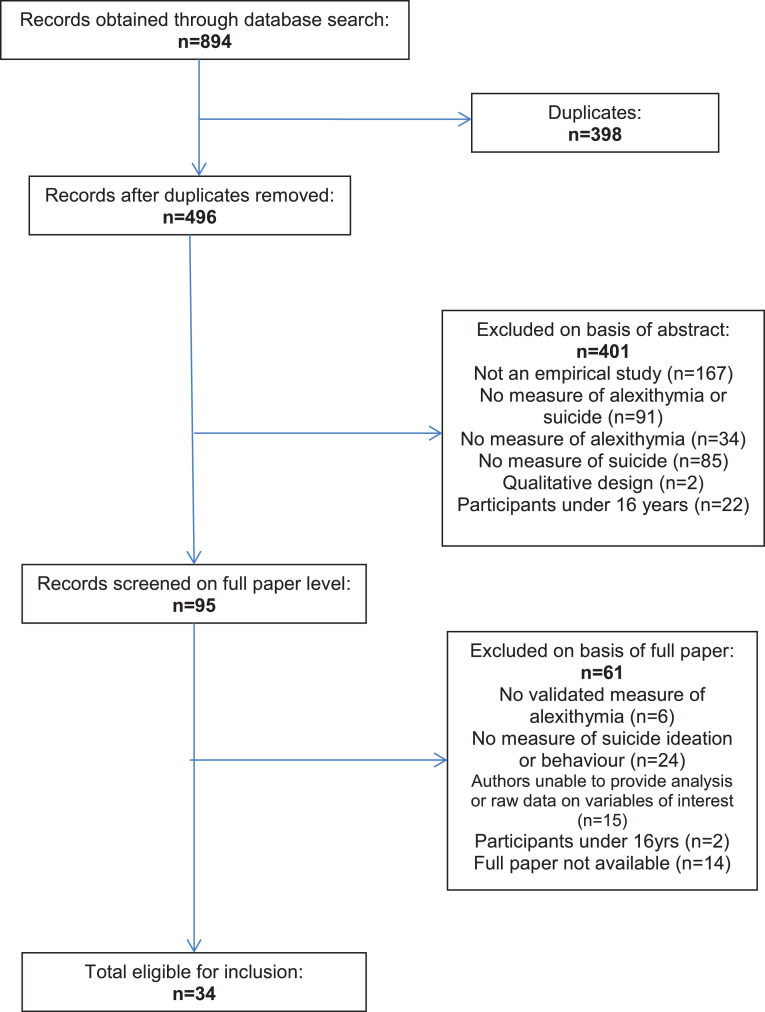
A flowchart of each stage of the database search was produced, with the search returning a total of 894 studies (Fig. 1).
Fig. 1.
PRISMA flow diagram of systematic search.
3.1. Study characteristics
A total of 34 studies were included in the review which incorporated data from 10,104 participants. Table 1 summarises the characteristics of included studies in the review. Eleven studies assessed the relationship between alexithymia and suicide ideation, twelve the relationship between alexithymia and suicide behaviour, eight the relationship between alexithymia and both suicide ideation and behaviour and three the relationship between alexithymia and suicide risk.
Table 1.
Characteristics of included studies.
| Authors and year | Country | Research design | N | Sample characteristics | Age (mean, SD) | Gender - male N (%) | Alexithymia measure | Suicide ideation measure | Suicide behaviour measure | Suicide risk measure |
|---|---|---|---|---|---|---|---|---|---|---|
| Carano et al. (2012) | Italy | Cross-sectional | 80 | Binge eating disorder outpatients | 39.5 (8.2) | 38 (48%) | TAS-20 | SSI | History taking – lifetime attempt | |
| Chang et al. (2016) | Taiwan | Case-control | 1077 | Suicide attempt / threat patients, controls | 39.0 (16.4) | 446 (41%) | TAS-20 | BSRS | Clinical records – lifetime attempt | |
| De Berardis, Campanella, et al. (2013) | Italy | Cross-sectional | 72 | Panic disorder outpatients | 25.3 (3.3) | 37 (51%) | TAS-20 | SSI | ||
| De Berardis, Conti, et al. (2013) | Italy | Cross-sectional | 30 | Non-affective psychosis patients | 25.9 (6.0) | 13 (43%) | TAS-20 | SSI | ||
| De Berardis et al. (2008) | Italy | Cross-sectional | 145 | Major depression outpatients | 28,5 (5.7) | 69 (48%) | TAS-20 | SSI | ||
| De Berardis et al. (2017) | Italy | Cross-sectional | 70 | GAD outpatients | 28.2 (5.3) | 34 (49%) | TAS-20 | SSI | ||
| De Berardis et al. (2015) | Italy | Cross-sectional | 104 | OCD outpatients | 32.1 (8.0) | 52 (50%) | TAS-20 | SSI | ||
| De Berardis et al. (2014) | Italy | Case-control | 79 | OCD outpatients, controls | 28.7 (8.0) | 43 (54%) | TAS-20 | SSI | ||
| Evren and Evren (2006) | Turkey | Cross-sectional | 154 | Substance dependent patients | 31.9 (11.7) | 154 (100%) | TAS-20 | CANQ – lifetime attempt | ||
| Evren et al. (2009) | Turkey | Cross-sectional | 159 | Substance dependent patients | 36.9 (8.4) | 159 (100%) | TAS-20 | CANQ – lifetime attempt | ||
| Ghorbani et al. (2017) | Iran | Case-control | 305 | Alcoholic outpatients, controls | 33.4 (10.3) | 214 (70%) | TAS-20 | SSI | History taking – lifetime attempt | |
| Gulec et al. (2014) | Turkey | Case-control | 144 | Conversion disorder patients, controls | Not reported (age range 18–64) | 29 (20%) | TAS-20 | Clinical records – lifetime attempt | ||
| Hamilton (2003) | USA | Cross-sectional | 103 | Undergraduate students | 20.6 | 22 (21%) | TAS-26 | SPS | ||
| Haviland et al. (1988) | USA | Cross-sectional | 125 | Substance dependent in-patients | 40.8 (11.2) | 125 (100%) | TAS-26 | History taking – lifetime attempt | ||
| Hintikka et al. (2004) | Finland | Longitudinal | 1563 | General population | 45.1 (10.5) | 649 (42%) | TAS-20 | BDI item 9 | ||
| Huang et al. (2016) | Taiwan | Case-control | 455 | Maladjusted soldiers, controls | 21.9 (4.5) | 429 (95%) | TAS-20 | BSRS | ||
| Iancu et al. (2001) | Israel | Case-control | 66 | Panic disorder outpatients, controls | 44.3 (11.7) | 26 (40%) | TAS-26 | SRS | ||
| Iancu et al. (1999) | Israel | Case-control | 60 | Major depression patients, controls | 35 (15.7) | 30 (50%) | TAS-26 | Clinical records – hospitalised for suicide attempt | ||
| Izci et al. (2015) | Turkey | Case-control | 149 | Depression patients, controls | 41.4 (12.6) | 59 (59%) | TAS-20 | SfSI | History taking - lifetime attempt | |
| Kampfer et al. (2016) | Germany | Cross-sectional | 155 | Somatoform disorder patients | 42.2 (15.7) | 66 (43%) | TAS-20 | History taking – lifetime attempt | ||
| Kim et al. (2016) | Korea | Cross-sectional | 81 | OCD patients | 28.9 (7.6) | 50 (62%) | TAS-20 | SSI | History taking – lifetime attempt | |
| Kusevic et al. (2015) | Croatia | Cross-sectional | 127 | War veterans with PTSD | 48.1 (6.6) | 127 (100%) | TAS-20 | History taking – lifetime attempt | ||
| Laget et al. (2006) | Switzerland | Case-control | 570 | Suicide attempt patients, controls | 27 (8.5) | 225 (40%) | TAS-20 | Hospitalised suicide attempt patients | ||
| Lester (1991) | USA | Cross-sectional | 127 | Undergraduate students | 21.3 (3.9) | 54 (43%) | TAS-26 | BDI item 9 | History taking – lifetime attempt | |
| Levi et al. (2008) | Israel | Case-control | 173 | Suicide attempt patients, controls | 37.5 (14.3) | 86 (50%) | TAS-20 | Hospitalised suicide attempt patients | ||
| Links et al. (2012) | Canada | Longitudinal | 120 | Psychiatric ward discharged patients | 37.5 (11.1) | 63 (53%) | TAS-20 | SSI | PHI – attempts in the past year | |
| Loas et al. (2016) | France | Cross-sectional | 122 | Inpatients with mood or anxiety disorder | 44.6 (13.5) | 33 (27%) | TAS-20 | BDI item 9 | ||
| Loftis (2014) | USA | Cross-sectional | 550 | Undergraduate students | 20.5 (3.6) | 272 (50%) | TAS-20 | SBQ-R | ||
| Meaney et al. (2016) | Australia | Cross-sectional | 2261 | Undergraduate students | 24.8 (8.1) | 619 (27%) | TAS-20 | BSL-supplement – attempts in past week | ||
| Na et al. (2013) | Korea | Case-control | 276 | Adjustment disorder soldiers, controls | 20.9 (1.4) | 276 (100%) | TAS-20 | Clinical records – attempts since joining armed forces | ||
| Rogers (2015) | USA | Cross-sectional | 99 | Psychiatric inpatients | 40.6 (12.0) | 0 (0%) | TAS-20 | SADS – attempts in past 6 months | ||
| Sakuraba et al. (2005) | Japan | Case-control | 164 | Alcoholic patients, controls | 53.9 (7.7) | 164 (100%) | TAS-26 | SSI | ||
| Sayar et al. (2003) | Turkey | Case-control | 160 | Suicide attempt patients, controls | 25.0 (8.3) | 26 (23%) | TAS-26 | ZSDS item 19 | History taking – lifetime attempt | |
| Wood et al. (2010) | UK | Case-control | 179 | Traumatic brain injury patients, controls | 28.2 (15.0) | 118 (66%) | TAS-20 | BDI item 9 |
BDI = Beck Depression Inventory, BSL-supplement = Borderline Symptom List-supplement: Items for assessing behaviour, BSRS = Brief Symptom Rating Scale, CANQ = Childhood Abuse and Neglect Questionnaire, ISS = Intent Score Scale, LRS = Lethality Rating Scale, PHI = Parasuicide History Inventory, SADS = Schedule of Affective Disorders for Schizophrenia Suicide Module, SBQ-R = Suicide Behaviours Questionnaire-Revised, SfSI = Scale for Suicide Ideation, SIS = Suicide Intent Scale, SLS = Suicide Lethality Scale, SPS = Suicide Probability Scale, SRS = Suicide Risk Scale, SSI = Scale of Suicidal Ideation, TAS = Toronto Alexithymia Scale, ZSDS = Zung Self-rating Depression Scale.
Of the 34 studies, 31 were published studies in peer-review journals and three were dissertation theses. Included studies utilised a range of designs; eighteen were cross-sectional studies, fourteen case control and two longitudinal. Included studies took place in a variety of countries worldwide; seven in Italy, five in Turkey, five in USA, three in Israel, two in Taiwan and Korea and one in Finland, Iran, Germany, Croatia, Switzerland, Canada, France, Australia, Japan and the UK. The majority of included studies (70%) were conducted within the past 10 years. Most included studies (85%) sampled clinical populations, with just 5 of the included studies sampling students or general population.
3.2. Measures used
All studies used a version of the Toronto Alexithymia Scale (TAS) to assess alexithymia. Four studies used the original TAS-26 scale (Taylor et al., 1985) and the more recent TAS-20 scale (Bagby et al., 1994) was used in the remaining studies.
Included studies used a variety of measures of suicide ideation. The majority of studies (k = 11) used the Scale for Suicide Ideation (Beck et al., 1979). Five studies used suicide ideation items from scales of depression including Beck Depression Inventory (Beck et al., 1996) and Zung Self-Report Depression Scale (Zung, 1965). The remaining studies utilised the brief symptom rating scale (k = 2) (Lee et al., 2003) or the Scale for Suicide Ideation (k = 1) (Linehan and Nielsen, 1981). Each of these scales assesses recent suicide ideation, asking for responses ranging from today up to the past two weeks.
Similarly, a variety of measures were utilised to report suicide behaviour. The majority of studies (k = 16) used a bespoke self-report question to measure number of suicide behaviours. An example of such a question is: “In your lifetime, did you ever make a suicide attempt?” (Carano et al., 2012). The time range that suicide behaviours were measured across varied, though most studies asked about lifetime suicide attempts (see Table 1).
Finally, three studies took an aggregate measure of suicide ideation and suicide behaviour, which it was not possible to separate for analysis purposes. These studies are therefore included in the review, in the exploration of the association between alexithymia and suicide ‘risk’. Hamilton (2003) used the Suicide Probability Scale (Cull and Gill, 1989), Iancu et al. (2001) used the Suicide Risk Scale (Plutchik et al., 1989) and Loftis (2014) used the Suicide Behaviours Questionnaire Revised (Osman et al., 2001).
3.3. Risk of bias and heterogeneity
The results of the quality assessment using the adapted AXIS tool showed that all studies were of good quality. Despite this, there were some common areas for which it was difficult to assess for risk of bias, due to studies not routinely reporting information. For instance, only two included studies gave information about non-responders, meaning this data bias could not be accounted for in the present review and may therefore affect the validity of the results. Furthermore, none of the included studies gave a justification for the sample size. This, again, may affect the validity of the results in this review, given that ten studies included a sample size of fewer than 100 participants. This may mean that studies in this review were underpowered, which can often lead to Type 2 errors. Out of the 34 included studies in this review, only eight studies explicitly addressed and categorised non-responders. This may mean that the studies included in this review are inherently biased in their samples. However, the majority of studies included in the review did use a selection process which was likely to select participant's representative of the target population, so this may go some way to alleviating this risk of bias.
All 34 studies identified clear aims and objectives, used study designs appropriate for the aims, clearly identified the target populations, measured risk factors and outcomes appropriate to the aims of the study, using instruments that have been trialled, piloted or published previously, discussed limitations of their study, and gave justified conclusions by the results.
According to Higgins and Thompson's (2002) cut-off points, heterogeneity levels were high in the majority of analyses completed (Table 2), supporting the decision to use a random-effects model. It is important to note that due to high levels of inconsistency, the 95% confidence intervals are likely to be more informative than relying only upon point-estimates of effect sizes.
Table 2.
Heterogeneity of meta-analyses.
| Analysis | Number of studies | I2 value |
|---|---|---|
| Suicide ideation and alexithymia | 15 | 95% |
| Suicide behaviour and alexithymia | 16 | 85% |
| Suicide ideation and difficulty identifying feelings | 6 | 79% |
| Suicide ideation and difficulty describing feelings | 5 | 90% |
| Suicide ideation and externally oriented thinking | 5 | 89% |
| Suicide behaviour and difficulty identifying feelings | 8 | 65% |
| Suicide behaviour and difficulty describing feelings | 8 | 58% |
| Suicide behaviour and externally oriented thinking | 8 | 63% |
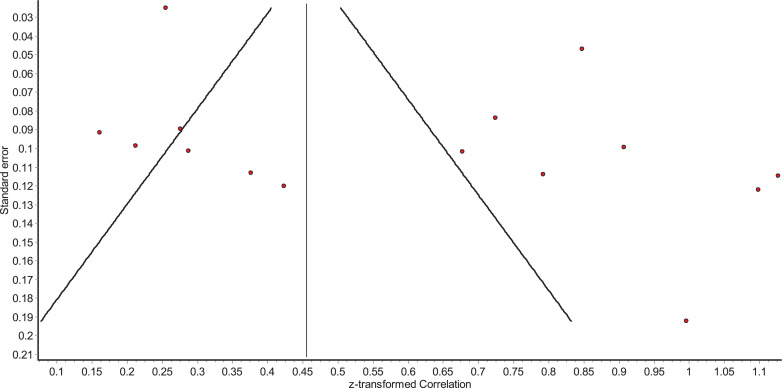
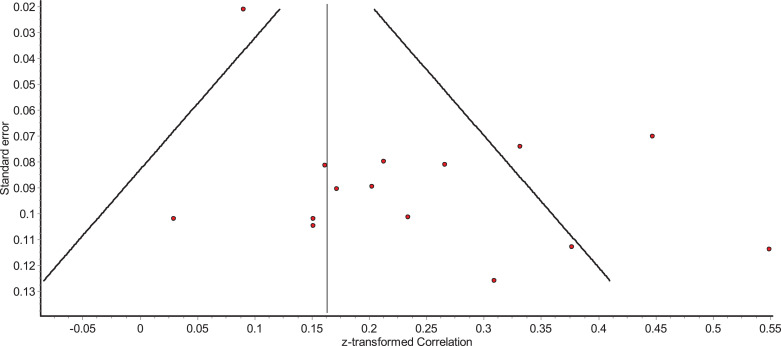
For those analyses where more than ten studies were included in the analysis, funnel plots were inspected to identify the possibility of publication bias. All funnel plots appeared asymmetric, though this may have occurred due to the high levels of heterogeneity, potentially caused by differences in study populations (Sterne et al., 2011). An Egger's test of publication bias supported the notion that there was no publication bias in studies that investigated the relationship between alexithymia and suicide ideation (β=3.76, SE=1.87, p=.065). For studies that investigated the relationship between alexithymia and suicide behaviour, Egger's test revealed a possibility of publication bias (β=2.15, SE=0.78, p=.016). However, it is important to note that there are only fifteen studies included in each Egger's test which can result in individual studies having an inflated effect on the test. The reader is therefore referred to the funnel plots (Figs. 2 and 3).
Fig. 2.
Funnel plot of relationship between alexithymia and suicide ideation.
Fig. 3.
Funnel plot of relationship between alexithymia and suicide behaviour.
3.4. The relationship between suicide ideation and alexithymia
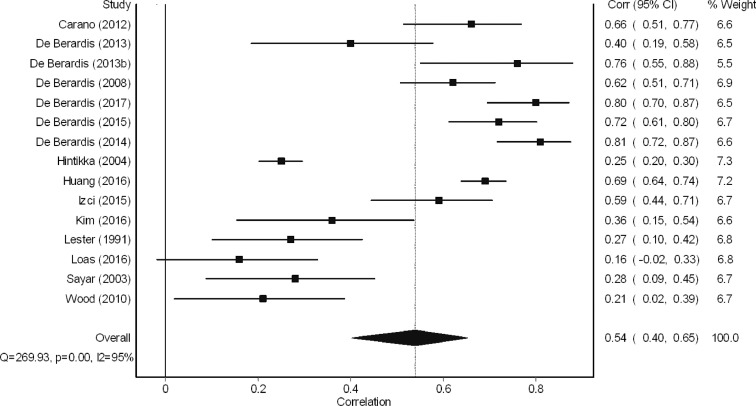
3.4.1. Suicide ideation and alexithymia: bivariate relationship
A total of 16 studies examined the bivariate relationship between alexithymia and suicide ideation. The meta-analysis revealed a ‘large’ effect size (Cohen, 1988) in the relationship between alexithymia and suicide ideation (r = 0.54, 95% CI = 0.40–0.65, Fig. 4). When considering study design, it was found that effect sizes were marginally larger for studies using a between-groups case-control design (difference in alexithymia scores; Cohen's D = 1.30, 95% CI =0.50–2.10, k = 4. Difference in suicide ideation scores; Cohen's D = 1.95, 95% CI = 1.44–2.46, k = 6) than for studies using a within-group cross-sectional design correlation design studies (r = 0.34, 95% CI =0.18–0.48, k = 5). This is likely due to the fact that between-groups design studies often maximise the difference through comparing a group with particularly high scores on a particular trait to a group with particularly low scores on a particular trait. The difference in these groups is therefore often more pronounced than searching for a correlation between variables within one sample. The 95% confidence intervals were much larger for the effect sizes computed for between-group design studies than for within-group design studies, suggesting the within-group studies had a wider range in findings than those which utilised correlation techniques.
Fig. 4.
Meta-analysis of relationship between alexithymia and suicide ideation.
As can be seen in Fig. 4, of the nine studies that yielded a ‘large’ effect size, six of these studies were conducted by the same research team in Italy (De Berardis and colleagues). Post-hoc sensitivity analysis was conducted to investigate further the potential effect this group of results may have had upon this meta-analysis. When the findings of all studies conducted by DeBerardis et al. were removed, the effect size of the relationship between alexithymia and suicide ideation was smaller, although still moderate (r = 0.41, 95% CI = 0.25–0.55). The inconsistency I2 values of this analysis remained the same (I2 = 95%).This group of six studies appear no different to the other studies included in the meta-analysis in relation to their risk of bias as reported using the AXIS quality assessment tool (Downes et al., 2016).
It is notable that those studies which used a validated measure of suicide ideation yielded larger effect sizes than the five studies which opted for specific items from validated scales of depression symptoms (Hintikka et al., 2004, Lester, 1991, Loas et al., 2016, Sayar et al., 2003, Wood et al., 2010).
In addition to the data included in the meta-analysis, three studies (Carano et al., 2012, De Berardis et al., 2015, Hintikka et al., 2004) also reported on the mean difference in prevalence of suicide ideation between those who were experiencing alexithymia and those who were not. The odds ratios ranged from 4.59 (95% CI=3.11–6.78) to 94.67 (95% CI=21.96–408.09), indicating a 4 to 95-fold increase in risk of suicide ideation for those experiencing alexithymia. These figures are likely inflated as a result of issues of data separation, and so the more extreme values are unlikely to be robust. Nonetheless, these figures suggest that those who experience alexithymia are more likely to experience concomitant suicide ideation.
Finally, one study assessed the longitudinal relationship between alexithymia and suicide ideation. Links et al. (2012) found that alexithymia did not significantly predict suicide ideation measured post discharge from hospital (OR=1.02, CI=0.99–1.05, p=.1809) nor did alexithymia predict change in suicide ideation scores between baseline and one-month follow-up (B = 0.12, p=.227). There is therefore currently no evidence that alexithymia is associated with suicide ideation over time.
3.4.2. Suicide ideation and alexithymia: multivariate relationship
A total of seven studies examined the multivariate relationship between alexithymia and suicide ideation (see Table 3). The most common confounding variables included in analyses were age (k = 4), gender (k = 4) and depression severity (k = 4). As can be seen in Table 3 it appears that the relationship between alexithymia and suicide ideation is robust when accounting for various demographic and clinical variables. The exception to this is the study conducted by Wood et al. (2010); when depression, hopelessness and worthlessness were controlled for, the relationship between alexithymia and suicide ideation was no longer significant. This study found that only worthlessness made a unique significant contribution to the model, with patients who reported worthlessness being 91% more likely to report suicide ideation than those who did not report feelings of worthlessness.
Table 3.
Multivariate associations between alexithymia and suicide ideation.
| Study | Bivariate association | Multivariate association | Control variables |
|---|---|---|---|
| Chang et al. (2016) | – | Standardised B = 0.15⁎⁎⁎ | Demographic variables, parental bonding, personality characteristics, mental disorder |
| De Berardis (2008) | r = 0.62* | r = 0.75⁎⁎⁎ | Demographic variables |
| De Berardis (2017) | r = 0.80* | r = 0.72⁎⁎⁎ | Demographic variables |
| Hamilton (2003) | r = 0.53⁎⁎⁎ | R2 change = 0.06⁎⁎ | Anxiety |
| Hintikka et al. (2004) | OR: 1.06 (95% CI = 1.05–1.08)* | OR: 1.03 (95% CI = 1.01–1.05)* | Demographic variables, psychosocial and economic risk factors, depression |
| Kim et al. (2016) | r = 0.36⁎⁎⁎ | r = 0.31⁎⁎ | Depression |
| Wood et al. (2010) | Unstandardized B = 0.35* | Unstandardized B = 0.02† | Depression, hopelessness, worthlessness |
*p<.05.
**p<.01.
***p<.001.
Non significant.
A meta-regression was conducted using the Knapp–Hartung variance estimator (Harbord and Higgins, 2008) to explore characteristics which might account for the high degree of inconsistency across studies. The results of this meta-regression should be interpreted with caution since they were planned post-hoc and meta-regression is prone to Type 1 error (Higgins and Thompson, 2004). Specifically, age (25 years and under, K = 5 vs. over 25 years, K = 10) and geographic location (Eastern, K = 4 vs. Western, K = 11) were explored as potential moderators. Neither age (β= 0.72, 95% CI = −0.35–0.49, p= .714) nor geographic location (β=0.68, 95% CI = −0.37–0.51, p=.743) were significant moderators in the relationship between alexithymia and suicide ideation. Moreover, neither moderator explained much of the between-study variance with I2 values still remaining high (age=94.4%, geographic location=93.9%).
3.4.3. Suicide ideation and alexithymia subscales
Twelve studies assessed the relationship between subscales of TAS-20 and suicide ideation and a further two studies assessed the bivariate relationship between subscales of TAS-26 and suicide ideation (see Table 4).
Table 4.
Suicide ideation and alexithymia subscales: Bivariate and multivariate relationships.
| Study | Alexithymia measure | DIF bivariate relationship | DIF multivariate relationship | DDF bivariate relationship | DDF multivariate relationship | EOT bivariate relationship | EOT multivariate relationship | Control variables |
|---|---|---|---|---|---|---|---|---|
| Carano et al. (2012) | TAS-20 | – | Standardised B = 0.54* | – | Standardised B = 0.21* | – | Non-significant – no values given† | Depression |
| De Berardis (2008) | TAS-20 | – | pr=0.72⁎⁎⁎ | – | pr=0.64⁎⁎⁎ | – | pr=0.20† | Demographic variables |
| De Berardis (2013) | TAS-20 | – | Standardised B = 0.31⁎⁎ | – | Non-significant – no values given† | – | Non-significant – no values given† | Demographic variables, panic disorder, depression, laboratory variables, TAS-20 subscales |
| De Berardis (2014) | TAS-20 | – | Standardised B = 0.54* | – | Non-significant – no values given† | – | Non-significant – no values given† | Demographic variables, OCD, depression, laboratory variables, TAS-20 subscales |
| De Berardis (2015) | TAS-20 | – | Standardised B = 0.29⁎⁎⁎ | – | Non-significant – no values given† | – | Non-significant – no values given† | Demographic variables, OCD, depression, responsibility attitudes, TAS-20 subscales |
| De Berardis (2017) | TAS-20 | – | pr=0.70⁎⁎⁎ | – | pr=0.53⁎⁎⁎ | – | pr=0.58⁎⁎⁎ | Demographic variables |
| Ghorbani et al. (2017) | TAS-20 | r = 0.42⁎⁎⁎ | pr=0.12† | r = 0.53⁎⁎⁎ | pr=0.29⁎⁎⁎ | r = 0.58⁎⁎⁎ | pr=0.42⁎⁎⁎ | Depression, alcohol dependence severity |
| Huang et al. (2016) | TAS-20 | d = 1.03* | Standardised B = 0.03⁎⁎ | d = 1.64* | – | d = 0.79* | – | Demographic variables, adverse life events, personality traits, suicidality factors |
| Izci et al. (2015) | TAS-20 | r = 0.64⁎⁎⁎ | – | r = 0.41⁎⁎⁎ | – | r = 0.09† | – | – |
| Loas et al. (2016) | TAS-20 | r = 0.19* | Standardised B= −0.23* | r = 0.28* | Standardised B = 0.23⁎⁎ | r = 0.00† | Non-significant – no values given† | Demographic variables, depression, anhedonia, TAS-20 subscales, laboratory variables |
| Sakuraba et al. (2005) | TAS-26 | Significant – no values given⁎⁎⁎ | – | Significant – no values given⁎⁎⁎ | – | Non-significant – no values given† | – | – |
| Sayar et al. (2003) | TAS-26 | r = 0.44⁎⁎⁎ | – | Non-significant – no values given† | – | Non-significant – no values given† | – | – |
| Wood et al. (2010) | TAS-20 | d = 0.47* | – | d = 0.39* | – | d = 0.24† | – | – |
EOT=Externally Oriented Thinking; DDF=Difficulty Describing Feelings; DIF=Difficulty Identifying Feelings; OCD=Obsessive Compulsive Disorder; TAS-20=Toronto Alexithymia Scale.
p<.05.
p<.01.
p<.001.
Non-significant.
A meta-analysis of the bivariate relationship between difficulty identifying feelings (DIF) and suicide ideation revealed a ‘moderate’ relationship (r = 0.41, 95% CI= 0.29–0.51, k = 6). This effect size is smaller than that found for the bivariate relationship between total alexithymia scores and suicide ideation (r = 0.54). Significant cross-sectional relationships between DIF and suicide ideation largely remained when demographic and clinical variables were accounted for.
A ‘moderate’ effect size was found in the meta-analysis of the relationship between difficulty describing feelings (DDF) and suicide ideation (r = 0.43, 95% CI = 0.24–0.59, k = 5). This effect size is again smaller than that found for the bivariate relationship between total alexithymia scores and suicide ideation (r = 0.54) but is very similar to that found for the relationship between DIF and suicide ideation (r = 0.41). Largely these findings remained significant when accounting for demographic and clinical variables.
The relationship between externally oriented thinking (EOT) and suicide ideation was found to have a ‘small’ effect size according to the meta-analysis (r = 0.28, 95% CI = 0.09–0.46, k = 5). This effect size is much smaller than those found between alexithymia total score (r = 0.54), DIF (r = 0.41) or DDF (r = 0.43) subscales and suicide ideation. Additionally, this relationship does not appear robust when accounting for clinical and demographic variables.
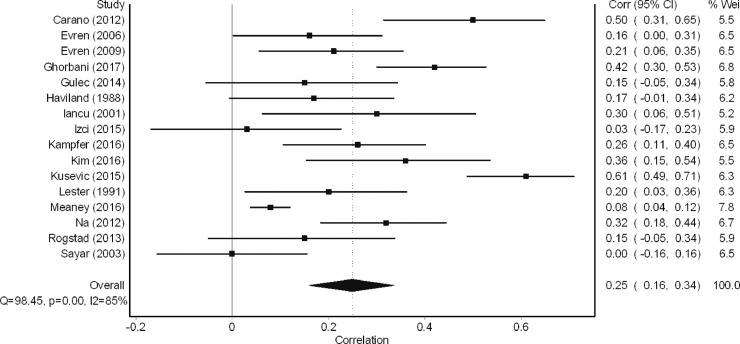
3.5. The relationship between suicide behaviour and alexithymia
3.5.1. Suicide behaviour and alexithymia: bivariate relationship
A total of 17 studies examined the bivariate relationship between alexithymia and suicide behaviour. Of these, 16 studies were eligible for inclusion in the meta-analysis. The meta-analysis revealed a small effect size in the relationship between alexithymia and suicide behaviour (r = 0.25, 95% CI = 0.16–0.34, k = 16, Fig. 5). When considering study designs, it was found that effect sizes were largest for between-group case-control studies (Difference in alexithymia scores; Cohen's D = 0.71, 95% CI =0.48–0.93. Difference in prevalence of suicide behaviours; OR=0.17, 95% CI=0.07–0.45). Effect sizes were considerably smaller for within-group cross-sectional studies (r = 0.11, 95% CI=0.04–0.17).
Fig. 5.
Meta-analysis of relationship between alexithymia and suicide behaviour.
In addition to the data included in the meta-analysis, one study (Links et al., 2012) utilised a longitudinal design to examine the relationship between alexithymia at baseline and suicide attempts occurring within six months of hospital discharge. Alexithymia was not found to be a significant univariate predictor of suicide attempts (OR=0.99, 95% CI=0.94–1.03, p=.552).
3.5.2. Suicide behaviour and alexithymia: multivariate relationship
A total of eight studies examined the multivariate relationship between alexithymia and suicide behaviour (see Table 5). The most common confounding variables included in analyses were depression severity (k = 4), age (k = 3), gender (k = 3) and marital status (k = 3). As can be seen in Table 5 control variables appears to have a mixed impact on this relationship, suggesting that the relationship between suicide behaviours and alexithymia is not robust, and instead may be accounted for by other factors.
Table 5.
Multivariate associations between alexithymia and suicide behaviour.
| Study | Bivariate association | Multivariate association | Control variables |
|---|---|---|---|
| Chang et al. (2016) | – | Standardised B = 0.14⁎⁎⁎ | Demographic variables, parental bonding, personality characteristics, mental disorder, suicide ideation |
| Gulec et al. (2014) | r = 0.15† | Non-significant – no values given† | Demographic variables, clinical variables, character variables, childhood maltreatment |
| Kim et al. (2016) | r = 0.36⁎⁎⁎ | Standardised B = 0.076⁎⁎ | Demographic variables, depression, OCD, perfectionism |
| Kusevic et al. (2015) | – | Odds ratio=2.87 (95% CI=1.18–7.0)* | Demographic variables |
| Levi et al. (2008) | – | Standardised B = 0.16* | Mental pain, depression, hopelessness, life events, schizoid, loneliness |
| Links et al. (2012) | – | Odds ratio=0.93 (95% CI=0.87–0.99)* | Demographic variables, suicidality variables, depression, impulsivity, problem solving, clinical variables, patient-care factors |
| Na et al. (2013) | r = 0.32* | Odds ratio=2.31 (95% CI=1.08–4.97)* | Cooperativeness |
p<.05.
p<.01.
p<.001.
Non-significant.
A meta-regression was conducted to explore whether age (25 years and under, K = 4 vs. over 25 years, K = 10) and geographic location (Eastern, K = 10 vs. Western location, K = 5) were potential moderators in the relationship between alexithymia and suicide behaviour. Neither age (β= 0.12, 95% CI = −0.07–0.30, p= .193) nor geographic location (β=0.05, 95% CI = −0.13–0.24, p=.524) were significant moderators in the relationship between alexithymia and suicide ideation. Moreover, neither moderator explained much of the between-study variance with I2 values still remaining high (age=67.7%, geographic location=75.9%).
3.5.3. Suicide behaviour and alexithymia subscales
Eight studies assessed the relationship between subscales of TAS-20 and suicide behaviour and a further one study assessed the relationship between subscales of TAS-26 and suicide behaviour (see Table 6).
Table 6.
Suicide behaviour and alexithymia subscales: Bivariate and multivariate relationships.
| Study | Alexithymia measure | DIF bivariate relationship | DIF multivariate relationship | DDF bivariate relationship | DDF multivariate relationship | EOT bivariate relationship | EOT multivariate relationship | Control variables |
|---|---|---|---|---|---|---|---|---|
| Evren (2006) | TAS-20 | d = 0.49* | – | d = 0.49* | – | d= - 0.11† | – | – |
| Ghorbani et al. (2017) | TAS-20 | – | Non-significant – no values given† | – | Non-significant – no values given† | – | Unstandardized B = 0.14⁎⁎⁎ | Demographic variables, alcohol dependency, depression, emotion regulation, TAS-20 subscales |
| Gulec et al. (2014) | TAS-20 | d = 0.37* | – | d = 0.37† | – | d= −0.33† | – | – |
| Izci et al. (2015) | TAS-20 | r = 0.06† | – | r = 0.04† | – | r = 0.04† | – | – |
| Loftis (2014) | TAS-20 | r = 0.28⁎⁎⁎ | – | r = 0.14⁎⁎⁎ | – | r = 0.07† | – | – |
| Meaney et al. (2016) | TAS-20 | r = 0.10⁎⁎⁎ | – | r = 0.08⁎⁎⁎ | – | r= −0.02† | – | – |
| Na (2013) | TAS-20 | d = 0.72* | OR=1.07 (95% CI=1.01–1.13)* | d = 0.72* | OR=1.20 (95% CI=1.09–1.32)⁎⁎⁎ | d = 0.36* | – | Cooperativeness |
| Rogers (2015) | TAS- 20 | r = 0.08* | – | r = 0.15† | – | r = 0.13† | – | – |
| Sayar et al. (2003) | TAS-26 | d = 0.17† | – | d = 0.09† | – | d= −0.32† | – | – |
EOT=Externally Oriented Thinking; DDF=Difficulty Describing Feelings; DIF=Difficulty Identifying Feelings; TAS-20=Toronto Alexithymia Scale.
⁎⁎p<.01.
p<.05.
p<.001.
Non-significant.
A meta-analysis revealed a ‘small’ effect size in the relationship between DIF and suicide behaviour (r = 0.16, 95% CI = 0.09–0.23, k = 8). This effect size is much smaller than that found for the bivariate relationship between alexithymia total score and suicide behaviour (r = 0.30). Furthermore, this effect size is much smaller than that found for the relationship between DIF and suicide ideation (r = 0.41). There are limited and mixed results on the impact that clinical and demographic variables have on this relationship.
There was also a ‘small’ effect size for the relationship between DDF and suicide behaviour (r = 0.15, 95% CI = 0.08–0.21, k = 8). This effect size is very similar to that found between DIF and suicide behaviour (r = 0.16), but is much smaller than the relationship found between DDF and suicide ideation (r = 0.43). There are mixed findings regarding the impact of clinical and demographic variables on this relationship.
Finally, the meta-analysis did not support the hypothesis of a bivariate relationship between EOT and suicide behaviour (r = 0.00, 95% CI = −0.07–0.08, k = 8). This effect size is much smaller than those found for the subscales of DIF and DDF with suicide behaviour (r = 0.16 and r = 0.11) and is also much smaller than the relationship between EOT and suicide ideation (r = 0.28). There is not enough data to assess the impact of clinical and demographic variables on this relationship.
3.6. The relationship between suicide risk and alexithymia
A total of three studies examined the relationship between alexithymia and suicide ‘risk’. All three studies found evidence to suggest that alexithymia is related to suicide risk. Iancu et al. (2001) found a moderate correlation between alexithymia and the suicide risk scale (r = 0.3, p<.05). Furthermore, Hamilton (2003) found a large correlation between alexithymia and the suicide probability scale (r = 0.53, p<.001). Finally, Loftis (2014) found that alexithymia significantly predicted suicide risk as measured by the suicide behaviours questionnaire revised (β = 0.21, p<.001). Specifically, Loftis (2014) found that alexithymia accounted for 4% of the variance in suicide risk. Furthermore, of the participants who classified as at risk for suicide, 64.4% of these scored above the cut-off point for alexithymia. Loftis also found that suicide risk was more closely related to difficulty identifying feelings (r = 0.28, p<.001) and difficulty describing feelings (r = 0.14, p<.001) than it was with externally oriented thinking (r= −0.07, p=.12).
3.7. Summary
Table 7 shows a summary of the bivariate relationships between alexithymia and suicide ideation and behaviour. The review found a large effect size for the relationship between alexithymia and severity of suicide ideation (r = 0.54, 95% CI=0.40–0.65). Furthermore, the review found moderate effect sizes for the relationship between difficulty identifying feelings (DIF, r = 0.41, 95% CI=0.29–0.51) and difficulty describing feelings (DDF, r = 0.43, 95% CI=0.24–0.59) subscales with suicide ideation. Finally, the review found small effect sizes for the relationship between alexithymia and suicide behaviour (r = 0.25, 95% CI=0.16–0.34), externally oriented thinking (EOT) and suicide ideation (r = 0.28, 95% CI=0.09–0.46), and also between suicide behaviour and DIF (r = 0.16, 95% CI=0.09–0.23) and DDF (r = 0.15, 95% CI=0.08–0.21) subscales. The review found no evidence for a relationship between EOT and suicide behaviour (r = 0.00, 95% CI=−0.07–0.08).
Table 7.
Summary of bivariate relationships with suicide ideation and suicide behaviour.
| Suicide ideation | Suicide behaviour | |||
|---|---|---|---|---|
| r | 95% CI | r | 95% CI | |
| Alexithymia (overall scores) | 0.54* | 0.40 - 0.65 | 0.25* | 0.16 - 0.34 |
| Difficulty identifying feelings | 0.41* | 0.29 – 0.51 | 0.16* | 0.09 - 0.23 |
| Difficulty describing feelings | 0.43* | 0.24 – 0.59 | 0.15* | 0.08 – 0.21 |
| Externally oriented thinking | 0.28* | 0.09 – 0.46 | 0.00 | −0.07 – 0.08 |
p<.05.
4. Discussion
4.1. Summary of results
The aim of this review was to (1) assess the relationship between alexithymia and its subcomponents and suicidal ideation in adults, (2) assess the relationship between alexithymia and its subcomponents and suicidal behaviour in adults and (3) compare the relationships between alexithymia and suicide ideation / behaviour.
This review found a large effect size in the meta-correlation between alexithymia and suicide ideation (0.54) and a medium effect size in the meta-correlation between alexithymia and suicide behaviour (0.25). These effect sizes echo research which has found existing risk factors for suicide ideation and behaviour such as psychotic disorders, substance use disorders and attention deficit hyperactivity disorder (Franklin et al., 2017). This therefore represents a need to better understand the nature of the relationship between alexithymia and suicide ideation and behaviour and may outline alexithymia as a new treatment target.
This review found a stronger relationship between alexithymia, and all subcomponents, with suicide ideation than with suicide behaviour. This study therefore supports the findings of May and Klonsky (2016) who assert that the risk factors for suicide ideation differ from those for suicide behaviour. This finding is in line with other research which has found that emotion dysregulation more broadly has been found to be more closely correlated with suicide ideation than suicide behaviour (Anestis et al., 2011, Zlotnick et al., 1997, 2003). Despite emotion dysregulation having a weaker relationship with suicide behaviour, there is nonetheless an association between emotion dysregulation and suicide behaviour. This has been explained by evidence that people who have difficulty regulating their emotions are only at greater risk of engaging in suicide behaviour if they have also engaged in repetitive self-injury (Law et al., 2015). This may explain the findings in the current review, especially given that several studies have found a relationship between alexithymia and non-suicidal self-injury (Norman and Borrill, 2015).
Further to this, this review found greater evidence for a relationship between suicide ideation and behaviour and the subscales of difficulty identifying feelings (DIF) and difficulty describing feelings (DDF) than with the externally oriented thinking (EOT) subscale. As discussed below, the impact of depression on the relationship between alexithymia and suicide ideation and behaviour is as yet unclear. However, in a recent meta-analysis, it was found that only the DIF and DDF components of alexithymia correlated with depression, and not the EOT component (Li et al., 2015). Assuming that depression has an impact on the relationship between alexithymia and suicide ideation and behaviour, this may help to explain the findings in this review that EOT was not as closely related to suicide ideation or behaviour as DIF and DDF subscales. Furthermore, the EOT component of the TAS-20 has frequently been found to have low internal consistency (Thorberg et al., 2010). This notion is supported by the fact that several studies have not been able to replicate the three factor structure of TAS-20 in a range of populations (Haviland, 1996, Müller et al., 2003, Zech et al., 1999).
The findings in this review regarding multivariate associations between alexithymia, subscales and suicide ideation and behaviour are somewhat unclear. This review found some evidence that demographic variables such as age, gender and location did not have any impact on the relationship between alexithymia and both suicide ideation and behaviour. Despite this, the review has highlighted inconsistencies in whether clinical variables, particularly depression, have an impact on the relationship between alexithymia and suicide ideation and behaviour or not.
To date, there has been much debate about the distinction between alexithymia and depression, with some even suggesting that subscales of alexithymia do no more than measure the pre-defined concept of depression (Cohen, 1989). This review found that the relationship between alexithymia and suicide ideation remained robust when depression was controlled for. However, when depression was controlled for in the relationship between alexithymia and suicide behaviour, the relationship did not appear as robust. Studies included in this review tended to measure a number of confounding variables, making it difficult to disentangle the specific impact of depression upon this relationship. Future research should aim to delineate the precise role of depression in the relationship between alexithymia and suicide ideation and behaviour.
4.2. Strengths, limitations and areas for future research
The present review involved a comprehensive search of the literature for evidence relating to the relationship between alexithymia and suicide ideation and behaviour. This review has also used meta-analyses to help synthesise the data and describe the current findings in the literature regarding the relationship between alexithymia and suicide ideation and behaviour. This review encompasses research from a variety of sources including peer-review journals and theses, which may go some way to alleviating a publication bias in the results.
Despite this, the review excluded studies that were not written in English which may limit the findings’ generalisability to non-Western cultures. However, the review does include several studies which originate from non-English speaking countries. Further, the review is limited in its exclusion of studies which examine child and adolescent samples. Future reviews could therefore focus on the relationship between alexithymia and suicide ideation and behaviour in child and adolescent populations.
Another limitation of the present review is the relatively high I2 levels of inconsistency within meta-analyses. This statistic is indicative of high levels of between-study variance, suggesting that differences in the design of studies may account for the differences in correlation coefficients. Despite relatively high levels of inconsistency, others have still advocated for the use of a meta-analysis, due to the approach being able to quantify and comment on levels of inconsistency (Ioannidis et al., 2008).
High levels of heterogeneity are particularly pertinent to studies examining the relationship between alexithymia and suicide behaviour, as the included measures of suicide behaviour varied considerably, with few studies utilising validated measures to assess suicide behaviour. Future research investigating the relationship between alexithymia and suicide ideation and behaviour should aim to utilise a validated measure of suicide ideation and/or behaviour, in order to ensure that measurement is accurate, reliable and valid.
In this review statistical testing of moderating effects of clinical variables were not possible due to there being small numbers in each subgroup, a limited number of studies included in the review, and due to such analysis being post-hoc in nature and therefore lending itself to a Type 1 error (Higgins and Thompson, 2004, Thompson and Higgins, 2002). Therefore important distinctions in the relationship between alexithymia and suicide ideation and behaviour may not have been discovered in the current study. Once a more substantial body of research in this area has been established, future reviews should aim to incorporate sub-group analysis into the design of the review, allowing for comparison of, for example, different clinical diagnoses.
The majority of studies included in this review included only one time point of data collection. However, in order to ascertain whether a causal relationship exists between alexithymia and suicide ideation and behaviour, temporality and directionality must be examined to decipher which phenomenon occurs first (Bradford, 1965). Future research should therefore aim to examine the prospective relationship between alexithymia and suicide ideation and behaviour. Furthermore, to establish a causal relationship between alexithymia and suicide ideation and behaviour, it is recommended that future research utilise experimental designs which aim to reduce alexithymia before assessing its impact on suicidal ideation and behaviour outcomes.
Finally, this review was inconclusive regarding which factors may facilitate or hinder the relationship between alexithymia and suicide ideation and behaviour. Future research should aim to control only for depression in the analysis of the relationship between alexithymia and suicide ideation and behaviour given the concept's strong overlap with both alexithymia and suicide ideation and behaviour. Furthermore, it is important for research to assess for self-harm as a possible mechanism through which alexithymia might lead to suicide behaviour.
4.3. Clinical implications
The implications of this study should be interpreted with caution due to the high levels of heterogeneity found in the review. Despite this, the present findings have several important implications for clinical practice. Firstly, this review has found that alexithymia is closely related to suicide ideation. This suggests that clinicians working with suicidal patients should attempt to screen patients for alexithymia. Alexithymia may often present with psychosomatic symptoms, so it is important for clinicians to be aware of and assess appropriately for alexithymia in suicidal patients (Taylor, 1984).
Screening for alexithymia is integral to ascertaining the best treatment option for patients. It has been frequently found that individuals who experience alexithymia may struggle to engage with talking therapies due to their lack of emotional insight (Grabe et al., 2008) which can subsequently lead to boredom for the psychotherapist, undermining the therapeutic relationship (Taylor, 1984) and also higher drop-out rates (Pierloot and Vinck, 1977). Despite this, it has been suggested that talking therapies provide a useful intervention for people with alexithymia, but only when therapy is tailored to tackle the specific needs that a person experiencing alexithymia may exhibit (Krystal, 1979). For instance, it has been suggested that people who struggle with emotional clarity may benefit from more skills-based therapies as opposed to therapies which are insight-oriented. Such behavioural therapies have been found to improve competency in identifying and describing feelings (Kennedy and Franklin, 2002).
Given that this review found a stronger association between the difficulty identifying and describing feelings components of alexithymia than the externally oriented thinking component, it is suggested that clinicians should aim to focus on these difficulties before the patient engages in talking therapy, in order to maximise effectiveness of talking therapy. There is some evidence to suggest that teaching elements of emotional intelligence may help to reduce severity of alexithymia (Amani et al., 2014). Engaging in educational material about emotional intelligence may therefore help reduce the severity of alexithymia in patients to enough of a degree to enable them to actively participate in and benefit from talking therapies.
This review has synthesised and analysed the results of 34 studies which have investigated the relationship between alexithymia and suicide ideation and behaviour. The review has found stronger evidence for a relationship between alexithymia and suicide ideation than with suicide behaviour. Further, the review found the difficulty identifying and describing feelings subcomponents of alexithymia were more closely linked with suicide ideation and behaviour than the subcomponent which relates to externally oriented thinking.
Acknowledgments
Acknowledgements
The authors wish to acknowledge and thank Mrs. Kamelia Harris and Miss Isabelle Butcher for their assistance with inter-rater reliability tasks.
Author statement
All authors were involved in the design and ongoing management of the study, and contributed to drafts of this report. LH, the principal investigator, prepared the protocol, conducted searches, extracted and analysed the data and took a lead on writing the manuscript. PT, DP, GH and JS provided feedback on the manuscript. PT advised on statistical aspects of the analysis.
Role of the funding source
This study was conducted as part of the first author's PhD funded by the Medical Research Council Doctoral Training Program (MRC-DTP) and the University of Manchester President's Doctoral Scholar Award. The funders had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the study for publication.
Conflict of interest
The authors have no conflicts of interest to declare.
References
- Amani M., Goodarzi M., Ahamadian H. Efficiency of training emotional intelligence on reducing Alexithymia syndrome in third grade male high school students. Int. Lett. Social Humanistic Sci. 2014;1:7–13. [Google Scholar]; Amani, M., Goodarzi, M., Ahamadian, H., 2014. Efficiency of training emotional intelligence on reducing Alexithymia syndrome in third grade male high school students. Int. Lett. Social Humanistic Sci.1, 7–13.
- Anestis M.D., Bagge C.L., Tull M.T., Joiner T.E. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. J. Psychiatric Res. 2011;45:603–611. doi: 10.1016/j.jpsychires.2010.10.013. [DOI] [PubMed] [Google Scholar]; Anestis, M.D., Bagge, C.L., Tull, M.T., Joiner, T.E., 2011. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. J. Psychiatric Res.45, 603–611. [DOI] [PubMed]
- Bagby R.M., Parker J.D., Taylor G.J. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. J. Psychosomatic Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]; Bagby, R.M., Parker, J.D., Taylor, G.J., 1994. The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. J. Psychosomatic Res.38, 23–32. [DOI] [PubMed]
- Bankier B., Aigner M., Bach M. Alexithymia in DSM-IV disorder: comparative evaluation of somatoform disorder, panic disorder, obsessive-compulsive disorder, and depression. Psychosomatics. 2001;42:235–240. doi: 10.1176/appi.psy.42.3.235. [DOI] [PubMed] [Google Scholar]; Bankier, B., Aigner, M., Bach, M., 2001. Alexithymia in DSM-IV disorder: comparative evaluation of somatoform disorder, panic disorder, obsessive-compulsive disorder, and depression. Psychosomatics42, 235–240. [DOI] [PubMed]
- Barendregt J., Doi S. EpiGear International Pty Ltd.; Australia: 2010. MetaXL User Guide: Version 1.0. Wilston. [Google Scholar]; Barendregt, J., Doi, S., 2010. MetaXL User Guide: Version 1.0. Wilston, Australia: EpiGear International Pty Ltd.
- Beck A., Davis J., Frederick C., Perlin S., Pokorny A., Schulman R., Seiden R., Wittlin B. Classification and nomenclature. Suicide prevention in the seventies. Resnick, HLP. 1972;1 30-37.27. [Google Scholar]; Beck, A., Davis, J., Frederick, C., Perlin, S., Pokorny, A., Schulman, R., Seiden, R., Wittlin, B., 1972. Classification and nomenclature. Suicide prevention in the seventies. Resnick, HLP, 1.30-37.27.
- Beck A.T., Kovacs M., Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J. Consulting Clinical Psychol. 1979;47:343. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]; Beck, A.T., Kovacs, M., Weissman, A., 1979. Assessment of suicidal intention: the Scale for Suicide Ideation. J. Consulting Clinical Psychol.47, 343. [DOI] [PubMed]
- Beck A.T., Steer R.A., Brown G.K. Beck depression inventory-II. San Antonio. 1996;78:490–498. [Google Scholar]; Beck, A.T., Steer, R.A., Brown, G.K., 1996. Beck depression inventory-II. San Antonio78, 490–498.
- Blackmore E.R., Munce S., Weller I., Zagorski B., Stansfeld S.A., Stewart D.E., Caine E.D., Conwell Y. Psychosocial and clinical correlates of suicidal acts: results from a national population survey. Br. J. Psychiatry. 2008;192:279–284. doi: 10.1192/bjp.bp.107.037382. [DOI] [PubMed] [Google Scholar]; Blackmore, E.R., Munce, S., Weller, I., Zagorski, B., Stansfeld, S.A., Stewart, D.E., Caine, E.D., Conwell, Y., 2008. Psychosocial and clinical correlates of suicidal acts: results from a national population survey. Br. J. Psychiatry192, 279–284. [DOI] [PubMed]
- Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. John Wiley & Sons; 2011. Introduction to Meta-Analysis. [Google Scholar]; Borenstein, M., Hedges, L.V., Higgins, J.P., Rothstein, H.R., 2011. Introduction to Meta-Analysis. John Wiley & Sons.
- Bradford A. Association or Causation? Proc. R. Soc. Med. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bradford, A., 1965. Association or Causation?Proc. R. Soc. Med.58, 295–300. [DOI] [PMC free article] [PubMed]
- Carano A., De Berardis D., Campanella D., Serroni N., Ferri F., Di Iorio G., Acciavatti T., Mancini L., Mariani G., Martinotti G., Moschetta F.S., Di Giannantonio M. Alexithymia and suicide ideation in a sample of patients with binge eating disorder. J. Psychiatric Pract. 2012;18:5–11. doi: 10.1097/01.pra.0000410982.08229.99. [DOI] [PubMed] [Google Scholar]; Carano, A., De Berardis, D., Campanella, D., Serroni, N., Ferri, F., Di Iorio, G., Acciavatti, T., Mancini, L., Mariani, G., Martinotti, G., Moschetta, F.S., Di Giannantonio, M., 2012. Alexithymia and suicide ideation in a sample of patients with binge eating disorder. J. Psychiatric Pract.18, 5–11. [DOI] [PubMed]
- Chang M.C., Lee M.B., Lee T.H., Lung F.W. Paternal and maternal bonding disparity in suicide. Neuropsychiatry. 2016;6:351–361. [Google Scholar]; Chang, M.C., Lee, M.B., Lee, T.H., Lung, F.W., 2016. Paternal and maternal bonding disparity in suicide. Neuropsychiatry6, 351–361.
- Cohen J. 2nd edn. Erlbaum Associates; Hillsdale: 1988. Statistical Power Analysis For the Behavioral Sciences. [Google Scholar]; Cohen, J., 1988. Statistical Power Analysis For the Behavioral Sciences2nd edn. Erlbaum Associates, Hillsdale.
- Cohen, K.R., 1989. A psychometric study of the concept alexithymia.
- Cull J.G., Gill W.S. Western Psychological Services; Los Angeles: 1989. Suicide Probability Scale (SPS) [Google Scholar]; Cull, J.G., Gill, W.S., 1989. Suicide Probability Scale (SPS). Los Angeles: Western Psychological Services.
- De Berardis D., Campanella D., Serroni N., Moschetta F.S., Di Emidio F., Conti C., Carano A., Acciavatti T., Di Iorio G., Martinotti G., Siracusano A., Di Giannantonio M. Alexithymia, suicide risk and serum lipid levels among adult outpatients with panic disorder. Compr. Psychiatry. 2013;54:517–522. doi: 10.1016/j.comppsych.2012.12.013. [DOI] [PubMed] [Google Scholar]; De Berardis, D., Campanella, D., Serroni, N., Moschetta, F.S., Di Emidio, F., Conti, C., Carano, A., Acciavatti, T., Di Iorio, G., Martinotti, G., Siracusano, A., Di Giannantonio, M., 2013a. Alexithymia, suicide risk and serum lipid levels among adult outpatients with panic disorder. Compr. Psychiatry54, 517–522. [DOI] [PubMed]
- De Berardis D., Conti C.M., Marini S., Serroni N., Moschetta F.S., Carano A., Valchera A., Iasevoli F., Fornaro M., Perna G., Di Iorio G., Martinotti G., Niolu C., Siracusano A., Di Giannantonio M. C-reactive protein level and its relationship with suicide risk and alexithymia among newly diagnosed, drug-naive patients with non-affective psychosis. Eur. J. Inflammation. 2013;11:215–221. [Google Scholar]; De Berardis, D., Conti, C.M., Marini, S., Serroni, N., Moschetta, F.S., Carano, A., Valchera, A., Iasevoli, F., Fornaro, M., Perna, G., Di Iorio, G., Martinotti, G., Niolu, C., Siracusano, A., Di Giannantonio, M., 2013b. C-reactive protein level and its relationship with suicide risk and alexithymia among newly diagnosed, drug-naive patients with non-affective psychosis. Eur. J. Inflammation11, 215–221.
- De Berardis D., Fornaro M., Orsolini L., Valchera A., Carano A., Vellante F., Perna G., Serafini G., Gonda X., Pompili M., Martinotti G., Di Giannantonio M. Alexithymia and suicide risk in psychiatric disorders: a mini-review. Front. Psychiatry. 2017;8:148. doi: 10.3389/fpsyt.2017.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]; De Berardis, D., Fornaro, M., Orsolini, L., Valchera, A., Carano, A., Vellante, F., Perna, G., Serafini, G., Gonda, X., Pompili, M., Martinotti, G., Di Giannantonio, M., 2017. Alexithymia and suicide risk in psychiatric disorders: aA mini-review. Front. Psychiatry8, 148. [DOI] [PMC free article] [PubMed]
- De Berardis D., Serroni N., Campanella D., Carano A., Gambi F., Valchera A., Conti C., Sepede G., Scali M., Fulcheri M., Salerno R.M., Ferro F.M. Alexithymia and its relationships with c-reactive protein and serum lipid levels among drug naive adult outpatients with major depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2008;32:1982–1986. doi: 10.1016/j.pnpbp.2008.09.022. [DOI] [PubMed] [Google Scholar]; De Berardis, D., Serroni, N., Campanella, D., Carano, A., Gambi, F., Valchera, A., Conti, C., Sepede, G., Scali, M., Fulcheri, M., Salerno, R.M., Ferro, F.M., 2008. Alexithymia and its relationships with c-reactive protein and serum lipid levels among drug naive adult outpatients with major depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry32, 1982–1986. [DOI] [PubMed]
- De Berardis D., Serroni N., Campanella D., Marini S., Rapini G., Valchera A., Iasevoli F., Mazza M., Fornaro M., Perna G., Di Iorio G., Martinotti G., Di Giannantonio M. Alexithymia, suicide ideation, C-Reactive Protein, and serum lipid levels among outpatients with generalized anxiety disorder. Arch. Suicide Res. 2017;21:100–112. doi: 10.1080/13811118.2015.1004485. [DOI] [PubMed] [Google Scholar]; De Berardis, D., Serroni, N., Campanella, D., Marini, S., Rapini, G., Valchera, A., Iasevoli, F., Mazza, M., Fornaro, M., Perna, G., Di Iorio, G., Martinotti, G., Di Giannantonio, M., 2017. Alexithymia, suicide ideation, C-Reactive Protein, and serum lipid levels among outpatients with generalized anxiety disorder. Arch. Suicide Res.21, 100–112. [DOI] [PubMed]
- De Berardis D., Serroni N., Campanella D., Rapini G., Olivieri L., Feliziani B., Carano A., Valchera A., Iasevoli F., Tomasetti C., Mazza M., Fomaro M., Perna G., Di Nicola M., Martinotti G., Di Giannantonio M. Alexithymia, responsibility attitudes and suicide ideation among outpatients with obsessive-compulsive disorder: an exploratory study. Compr. Psychiatry. 2015;58:82–87. doi: 10.1016/j.comppsych.2014.12.016. [DOI] [PubMed] [Google Scholar]; De Berardis, D., Serroni, N., Campanella, D., Rapini, G., Olivieri, L., Feliziani, B., Carano, A., Valchera, A., Iasevoli, F., Tomasetti, C., Mazza, M., Fomaro, M., Perna, G., Di Nicola, M., Martinotti, G., Di Giannantonio, M., 2015. Alexithymia, responsibility attitudes and suicide ideation among outpatients with obsessive-compulsive disorder: aAn exploratory study. Compr. Psychiatry58, 82–87. [DOI] [PubMed]
- De Berardis D., Serroni N., Marini S., Rapini G., Carano A., Valchera A., Iasevoli F., Mazza M., Signorelli M., Aguglia E., Perna G., Martinotti G., Varasano P.A., Pressanti G.L., Di Giannantonio M. Alexithymia, suicidal ideation, and serum lipid levels among drug-naive outpatients with obsessive-compulsive disorder. Revista Brasileira de Psiquiatria. 2014;36:125–130. doi: 10.1590/1516-4446-2013-1189. [DOI] [PubMed] [Google Scholar]; De Berardis, D., Serroni, N., Marini, S., Rapini, G., Carano, A., Valchera, A., Iasevoli, F., Mazza, M., Signorelli, M., Aguglia, E., Perna, G., Martinotti, G., Varasano, P.A., Pressanti, G.L., Di Giannantonio, M., 2014. Alexithymia, suicidal ideation, and serum lipid levels among drug-naive outpatients with obsessive-compulsive disorder. Revista Brasileira de Psiquiatria36, 125–130. [DOI] [PubMed]
- Dour H.J., Cha C.B., Nock M.K. Evidence for an emotion–cognition interaction in the statistical prediction of suicide attempts. Behav. Res. Therapy. 2011;49:294–298. doi: 10.1016/j.brat.2011.01.010. [DOI] [PubMed] [Google Scholar]; Dour, H.J., Cha, C.B., Nock, M.K., 2011. Evidence for an emotion–cognition interaction in the statistical prediction of suicide attempts. Behav. Res. Therapy49, 294–298. [DOI] [PubMed]
- Downes M.J., Brennan M.L., Williams H.C., Dean R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]; Downes, M.J., Brennan, M.L., Williams, H.C., Dean, R.S., 2016. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open6, e011458. [DOI] [PMC free article] [PubMed]
- Evren C., Evren B. The relationship of suicide attempt history with childhood abuse and neglect, alexithymia and temperament and character dimensions of personality in substance dependents. Nordic J. Psychiatry. 2006;60:263–269. doi: 10.1080/08039480600790051. [DOI] [PubMed] [Google Scholar]; Evren, C., Evren, B., 2006. The relationship of suicide attempt history with childhood abuse and neglect, alexithymia and temperament and character dimensions of personality in substance dependents. Nordic J. Psychiatry60, 263–269. [DOI] [PubMed]
- Evren C., Evren B., Dalbudak E., Ozcelik B., Oncu F. Childhood abuse and neglect as a risk factor for alexithymia in adult male substance dependent inpatients. J. Psychoact. Drugs. 2009;41:85–92. doi: 10.1080/02791072.2009.10400677. [DOI] [PubMed] [Google Scholar]; Evren, C., Evren, B., Dalbudak, E., Ozcelik, B., Oncu, F., 2009. Childhood abuse and neglect as a risk factor for alexithymia in adult male substance dependent inpatients. J. Psychoact. Drugs41, 85–92. [DOI] [PubMed]
- Falagas M.E., Pitsouni E.I., Malietzis G.A., Pappas G. Comparison of PubMed, Scopus, web of science, and Google scholar: strengths and weaknesses. FASEB J. 2008;22:338–342. doi: 10.1096/fj.07-9492LSF. [DOI] [PubMed] [Google Scholar]; Falagas, M.E., Pitsouni, E.I., Malietzis, G.A., Pappas, G., 2008. Comparison of PubMed, Scopus, web of science, and Google scholar: strengths and weaknesses. FASEB J.22, 338–342. [DOI] [PubMed]
- Foran H.M., O'Leary K.D. The role of relationships in understanding the alexithymia–depression link. Eur. J. Personality. 2013;27:470–480. [Google Scholar]; Foran, H.M., O'Leary, K.D., 2013. The role of relationships in understanding the alexithymia–depression link. Eur. J. Personality27, 470–480.
- Franklin J.C., Ribeiro J.D., Fox K.R., Bentley K.H., Kleiman E.M., Huang X., Musacchio K.M., Jaroszewski A.C., Chang B.P., Nock M.K. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psycholo. Bulletin. 2017;143:187. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]; Franklin, J.C., Ribeiro, J.D., Fox, K.R., Bentley, K.H., Kleiman, E.M., Huang, X., Musacchio, K.M., Jaroszewski, A.C., Chang, B.P., Nock, M.K., 2017. Risk factors for suicidal thoughts and behaviors: aA meta-analysis of 50 years of research. Psycholo. Bulletin143, 187. [DOI] [PubMed]
- Ghorbani F., Khosravani V., Sharifi Bastan F., Jamaati Ardakani R. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol-dependent outpatients. Psychiatry Res. 2017;252:223–230. doi: 10.1016/j.psychres.2017.03.005. [DOI] [PubMed] [Google Scholar]; Ghorbani, F., Khosravani, V., Sharifi Bastan, F., Jamaati Ardakani, R., 2017. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol-dependent outpatients. Psychiatry Res.252, 223–230. [DOI] [PubMed]
- Grabe H.J., Frommer J., Ankerhold A., Ulrich C., Gröger R., Franke G.H., Barnow S., Freyberger H.J., Spitzer C. Alexithymia and outcome in psychotherapy. Psychotherapy Psychosomatics. 2008;77:189–194. doi: 10.1159/000119739. [DOI] [PubMed] [Google Scholar]; Grabe, H.J., Frommer, J., Ankerhold, A., Ulrich, C., Gröger, R., Franke, G.H., Barnow, S., Freyberger, H.J., Spitzer, C., 2008. Alexithymia and outcome in psychotherapy. Psychotherapy Psychosomatics77, 189–194. [DOI] [PubMed]
- Gratz K.L., Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopatho. Behav. Assess. 2004;26:41–54. [Google Scholar]; Gratz, K.L., Roemer, L., 2004. Multidimensional assessment of emotion regulation and dysregulation: dDevelopment, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopatho. Behav. Assess.26, 41–54.
- Gratz K.L., Tull M.T. Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change. 2010. Emotion regulation as a mechanism of change in acceptance-and mindfulness-based treatments; pp. 107–133. [Google Scholar]; Gratz, K.L., Tull, M.T., 2010. Emotion regulation as a mechanism of change in acceptance-and mindfulness-based treatments. Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change, 107–133.
- Gulec M.Y., Ynanc L., Yanarta O., Uzer A., Gulec H. Predictors of suicide in patients with conversion disorder. Compr. Psychiatry. 2014;55:457–462. doi: 10.1016/j.comppsych.2013.10.009. [DOI] [PubMed] [Google Scholar]; Gulec, M.Y., Ynanc, L., Yanarta, O., Uzer, A., Gulec, H., 2014. Predictors of suicide in patients with conversion disorder. Compr. Psychiatry55, 457–462. [DOI] [PubMed]
- Hamilton D.M. Alexithymia, anxiety and suicide ideation among african american college students. Dissertation Abstracts Int. 2003;63:4904. [Google Scholar]; Hamilton, D.M., 2003. Alexithymia, anxiety and suicide ideation among african american college students. Dissertation Abstracts Int.63, 4904.
- Harbord R.M., Higgins J.P. Meta-regression in Stata. Stata J. 2008;8:493–519. [Google Scholar]; Harbord, R.M., Higgins, J.P., 2008. Meta-regression in Stata. Stata J.8, 493–519.
- Hardt J., Bernert S., Matschinger H., Angermeier M., Vilagut G., Bruffaerts R., De Girolamo G., De Graaf R., Haro J., Kovess V. Suicidality and its relationship with depression, alcohol disorders and childhood experiences of violence: results from the ESEMeD study. J. Affect. Disorders. 2015;175:168–174. doi: 10.1016/j.jad.2014.12.044. [DOI] [PubMed] [Google Scholar]; Hardt, J., Bernert, S., Matschinger, H., Angermeier, M., Vilagut, G., Bruffaerts, R., De Girolamo, G., De Graaf, R., Haro, J., Kovess, V., 2015. Suicidality and its relationship with depression, alcohol disorders and childhood experiences of violence: rResults from the ESEMeD study. J. Affect. Disorders175, 168–174. [DOI] [PubMed]
- Haviland M. Structure of the twenty-item Toronto Alexithymia Scale. J. Personality Assess. 1996;66:116–125. doi: 10.1207/s15327752jpa6601_9. [DOI] [PubMed] [Google Scholar]; Haviland, M., 1996. Structure of the twenty-item Toronto Alexithymia Scale. J. Personality Assess.66, 116–125. [DOI] [PubMed]
- Haviland M., MacMurray J.P., Cummings M.A. The relationship between alexithymia and depressive symptoms in a sample of newly abstinent alcoholic inpatients. Psychotherapy Psychosomatics. 1988;49:37–40. doi: 10.1159/000288065. [DOI] [PubMed] [Google Scholar]; Haviland, M., MacMurray, J.P., Cummings, M.A., 1988. The relationship between alexithymia and depressive symptoms in a sample of newly abstinent alcoholic inpatients. Psychotherapy Psychosomatics49, 37–40. [DOI] [PubMed]
- Higgins J., Thompson S.G. Quantifying heterogeneity in a meta‐analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]; Higgins, J., Thompson, S.G., 2002. Quantifying heterogeneity in a meta‐analysis. Stat. Med.21, 1539–1558. [DOI] [PubMed]
- Higgins J.P., Thompson S.G. Controlling the risk of spurious findings from meta‐regression. Stat. Med. 2004;23:1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]; Higgins, J.P., Thompson, S.G., 2004. Controlling the risk of spurious findings from meta‐regression. Stat. Med.23, 1663–1682. [DOI] [PubMed]
- Hintikka J., Honkalampi K., Koivumaa-Honkanen H., Antikainen R., Tanskanen A., Haatainen K., Viinamaki H. Alexithymia and suicidal ideation: a 12-month follow-up study in a general population. Compr. Psychiatry. 2004;45:340–345. doi: 10.1016/j.comppsych.2004.06.008. [DOI] [PubMed] [Google Scholar]; Hintikka, J., Honkalampi, K., Koivumaa-Honkanen, H., Antikainen, R., Tanskanen, A., Haatainen, K., Viinamaki, H., 2004. Alexithymia and suicidal ideation: aA 12-month follow-up study in a general population. Compr. Psychiatry45, 340–345. [DOI] [PubMed]
- Huang K.C., Tzeng D.S., Lin C.H., Chung W.C. Interpersonal-Psychological Theory, Alexithymia, and Personality Predict Suicide Ideation among Maladjusted Soldiers in Taiwan. Suicide Life-Threatening Behav. 2016 doi: 10.1111/sltb.12315. [DOI] [PubMed] [Google Scholar]; Huang, K.C., Tzeng, D.S., Lin, C.H., Chung, W.C., 2016. Interpersonal-Psychological Theory, Alexithymia, and Personality Predict Suicide Ideation among Maladjusted Soldiers in Taiwan. Suicide Life-Threatening Behav.. [DOI] [PubMed]
- Iancu I., Dannon P.N., Poreh A., Lepkifker E., Grunhaus L. Alexithymia and suicidality in panic disorder. Compr. Psychiatry. 2001;42:477–481. doi: 10.1053/comp.2001.27893. [DOI] [PubMed] [Google Scholar]; Iancu, I., Dannon, P.N., Poreh, A., Lepkifker, E., Grunhaus, L., 2001. Alexithymia and suicidality in panic disorder. Compr. Psychiatry42, 477–481. [DOI] [PubMed]
- Iancu I., Horesh N., Offer D., Dannon P.N., Lepkifker E., Kotler M. Alexithymia, affect intensity and emotional range in suicidal patients. Psychotherapy Psychosomatics. 1999;68:276–280. doi: 10.1159/000012344. [DOI] [PubMed] [Google Scholar]; Iancu, I., Horesh, N., Offer, D., Dannon, P.N., Lepkifker, E., Kotler, M., 1999. Alexithymia, affect intensity and emotional range in suicidal patients. Psychotherapy Psychosomatics68, 276–280. [DOI] [PubMed]
- Ioannidis J.P., Patsopoulos N.A., Rothstein H.R. Research methodology: reasons or excuses for avoiding meta-analysis in forest plots. BMJ. 2008;336:1413. doi: 10.1136/bmj.a117. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ioannidis, J.P., Patsopoulos, N.A., Rothstein, H.R., 2008. Research methodology: reasons or excuses for avoiding meta-analysis in forest plots. BMJ336, 1413. [DOI] [PMC free article] [PubMed]
- Izci F., Zincir S., Zincir S.B., Bilici R., Gica S, Iris Koc M.S., Goncu T., Terzi A., Semiz U.B. Suicide attempt, suicidal ideation and hopelessness levels in major depressive patients with and without alexithymia. Dusunen Adam: J. Psychiatry Neurol. Sci. 2015;28:27–33. [Google Scholar]; Izci, F., Zincir, S., Zincir, S.B., Bilici, R., Gica, S., Iris Koc, M.S., Goncu, T., Terzi, A., Semiz, U.B., 2015. Suicide attempt, suicidal ideation and hopelessness levels in major depressive patients with and without alexithymia. Dusunen Adam: J. Psychiatry Neurol. Sci.28, 27–33.
- Kampfer N., Staufenbiel S., Wegener I., Rambau S., Urbach A.S., Mucke M., Geiser F., Conrad R. Suicidality in patients with somatoform disorder-The speechless expression of anger? Psychiatry Res. 2016;246:485–491. doi: 10.1016/j.psychres.2016.10.022. [DOI] [PubMed] [Google Scholar]; Kampfer, N., Staufenbiel, S., Wegener, I., Rambau, S., Urbach, A.S., Mucke, M., Geiser, F., Conrad, R., 2016. Suicidality in patients with somatoform disorder-The speechless expression of anger?Psychiatry Res.246, 485–491. [DOI] [PubMed]
- Kennedy M., Franklin J. Skills-based treatment for alexithymia: an exploratory case series. Behav. Change. 2002;19:158–171. [Google Scholar]; Kennedy, M., Franklin, J., 2002. Skills-based treatment for alexithymia: aAn exploratory case series. Behav. Change19, 158–171.
- Kim H., Seo J., Namkoong K., Hwang E.H., Sohn S.Y., Kim S.J., Kang J.I. Alexithymia and perfectionism traits are associated with suicidal risk in patients with obsessive-compulsive disorder. J. Affect. Disorders. 2016;192:50–55. doi: 10.1016/j.jad.2015.12.018. [DOI] [PubMed] [Google Scholar]; Kim, H., Seo, J., Namkoong, K., Hwang, E.H., Sohn, S.Y., Kim, S.J., Kang, J.I., 2016. Alexithymia and perfectionism traits are associated with suicidal risk in patients with obsessive-compulsive disorder. J. Affect. Disorders192, 50–55. [DOI] [PubMed]
- Klonsky E.D., May A.M. The three-step theory (3ST): a new theory of suicide rooted in the “ideation-to-action” framework. Int. J. Cognitive Therapy. 2015;8:114–129. [Google Scholar]; Klonsky, E.D., May, A.M., 2015. The three-step theory (3ST): aA new theory of suicide rooted in the “ideation-to-action” framework. Int. J. Cognitive Therapy8, 114–129.
- Krystal H. Alexithymia and psychotherapy. Am. J. Psychotherapy. 1979;33:17–31. doi: 10.1176/appi.psychotherapy.1979.33.1.17. [DOI] [PubMed] [Google Scholar]; Krystal, H., 1979. Alexithymia and psychotherapy. Am. J. Psychotherapy33, 17–31. [DOI] [PubMed]
- Kusevic Z., Cusa B.V., Babic G., Marcinko D. Could alexithymia predict suicide attempts-A study of Croatian war veterans with post-traumatic stress disorder. Psychiatria Danubina. 2015;27:420–423. [PubMed] [Google Scholar]; Kusevic, Z., Cusa, B.V., Babic, G., Marcinko, D., 2015. Could alexithymia predict suicide attempts-A study of Croatian war veterans with post-traumatic stress disorder. Psychiatria Danubina27, 420–423. [PubMed]
- Laget J., Plancherel B., Stephan P., Bolognini M., Corcos M., Jeammet P., Halfon O. Personality and repeated suicide attempts in dependent adolescents and young adults. Crisis. 2006;27:164–171. doi: 10.1027/0227-5910.27.4. [DOI] [PubMed] [Google Scholar]; Laget, J., Plancherel, B., Stephan, P., Bolognini, M., Corcos, M., Jeammet, P., Halfon, O., 2006. Personality and repeated suicide attempts in dependent adolescents and young adults. Crisis27, 164–171. [DOI] [PubMed]
- Law K.C., Khazem L.R., Anestis M.D. The role of emotion dysregulation in suicide as considered through the ideation to action framework. Curr. Opinion Psychol. 2015;3:30–35. [Google Scholar]; Law, K.C., Khazem, L.R., Anestis, M.D., 2015. The role of emotion dysregulation in suicide as considered through the ideation to action framework. Curr. Opinion Psychol.3, 30–35.
- Lee M.-B., Liao S.-C., Lee Y.-J., Wu C.-H., Tseng M.-C., Gau S.-F., Rau C.-l. Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J. Formosan Med. Assoc. 2003;102:687–694. [PubMed] [Google Scholar]; Lee, M.-B., Liao, S.-C., Lee, Y.-J., Wu, C.-H., Tseng, M.-C., Gau, S.-F., Rau, C.-l., 2003. Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J. Formosan Med. Assoc.102, 687–694. [PubMed]
- Lester D. Alexithymia, depression, and suicidal preoccupation. Perceptual Motor Skills. 1991;72:1058. doi: 10.2466/pms.1991.72.3.1058. [DOI] [PubMed] [Google Scholar]; Lester, D., 1991. Alexithymia, depression, and suicidal preoccupation. Perceptual Motor Skills72, 1058. [DOI] [PubMed]
- Levi Y., Horesh N., Fischel T., Treves I., Or E., Apter A. Mental pain and its communication in medically serious suicide attempts: an “impossible situation”. J. Affective Disorders. 2008;111:244–250. doi: 10.1016/j.jad.2008.02.022. [DOI] [PubMed] [Google Scholar]; Levi, Y., Horesh, N., Fischel, T., Treves, I., Or, E., Apter, A., 2008. Mental pain and its communication in medically serious suicide attempts: aAn “impossible situation”. J. Affective Disorders111, 244–250. [DOI] [PubMed]
- Leweke F., Leichsenring F., Kruse J., Hermes S. Is alexithymia associated with specific mental disorders. Psychopathology. 2012;45:22–28. doi: 10.1159/000325170. [DOI] [PubMed] [Google Scholar]; Leweke, F., Leichsenring, F., Kruse, J., Hermes, S., 2012. Is alexithymia associated with specific mental disorders. Psychopathology45, 22–28. [DOI] [PubMed]
- Li S., Zhang B., Guo Y., Zhang J. The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and depression: a meta-analysis. Psychiatry Res. 2015;227:1–9. doi: 10.1016/j.psychres.2015.02.006. [DOI] [PubMed] [Google Scholar]; Li, S., Zhang, B., Guo, Y., Zhang, J., 2015. The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and depression: a meta-analysis. Psychiatry Res.227, 1–9. [DOI] [PubMed]
- Linehan M.M., Nielsen S.L. Assessment of suicide ideation and parasuicide: hopelessness and social desirability. J. Consulting Clinical Psychol. 1981;49:773. doi: 10.1037//0022-006x.49.5.773. [DOI] [PubMed] [Google Scholar]; Linehan, M.M., Nielsen, S.L., 1981. Assessment of suicide ideation and parasuicide: hHopelessness and social desirability. J. Consulting Clinical Psychol.49, 773. [DOI] [PubMed]
- Links P., Nisenbaum R., Ambreen M., Balderson K., Bergmans Y., Eynan R., Harder H., Cutcliffe J. Prospective study of risk factors for increased suicide ideation and behavior following recent discharge. General Hospital Psychiatry. 2012;34:88–97. doi: 10.1016/j.genhosppsych.2011.08.016. [DOI] [PubMed] [Google Scholar]; Links, P., Nisenbaum, R., Ambreen, M., Balderson, K., Bergmans, Y., Eynan, R., Harder, H., Cutcliffe, J., 2012. Prospective study of risk factors for increased suicide ideation and behavior following recent discharge. General Hospital Psychiatry34, 88–97. [DOI] [PubMed]
- Loas, G., Dalleau, E., Lecointe, H., Yon, V., 2016. Relationships between anhedonia, alexithymia, impulsivity, suicidal ideation, recent suicide attempt, C-reactive protein and serum lipid levels among 122 inpatients with mood or anxious disorders. Psychiatry Research 246, 296–302. [DOI] [PubMed]
- Loftis M.A. Dissertation Abstracts International: Section B: The Sciences and Engineering 75. 2014. Alexithymia, impulsivity, locus of control, and suicide risk in college students. No-Specified. [Google Scholar]; Loftis, M.A., 2014. Alexithymia, impulsivity, locus of control, and suicide risk in college students. Dissertation Abstracts International: Section B: The Sciences and Engineering 75, No Pagination Specified.
- May A.M., Klonsky E.D. What distinguishes suicide attempters from suicide ideators? Clinical Psychol. 2016;23:5–20. [Google Scholar]; May, A.M., Klonsky, E.D., 2016. What distinguishes suicide attempters from suicide ideators? A meta‐analysis of potential factors. Clinical Psychol.23, 5–20.
- McManus S., Bebbington P., Jenkins R., Brugha T. University of Leicester. NHS Digital; 2016. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014: a Survey Carried Out for NHS Digital by NatCen Social Research and the Department of Health Sciences. [Google Scholar]; McManus, S., Bebbington, P., Jenkins, R., Brugha, T., 2016. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014: a Survey Carried Out for NHS Digital by NatCen Social Research and the Department of Health Sciences, University of Leicester. NHS Digital.
- Meaney R., Hasking P., Reupert A. Borderline personality disorder symptoms in college students: the complex interplay between alexithymia, emotional dysregulation and rumination. PLoS ONE. 2016;11(6) doi: 10.1371/journal.pone.0157294. [DOI] [PMC free article] [PubMed] [Google Scholar]; Meaney, R., Hasking, P., Reupert, A., 2016. Borderline personality disorder symptoms in college students: tThe complex interplay between alexithymia, emotional dysregulation and rumination. PLoS ONE11 (6) (no pagination). [DOI] [PMC free article] [PubMed]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Internal Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]; Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G., 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Internal Med.151, 264–269. [PMC free article] [PubMed]
- Morrison R., O'connor R.C. A systematic review of the relationship between rumination and suicidality. Suicide Life-Threatening Behav. 2008;38:523–538. doi: 10.1521/suli.2008.38.5.523. [DOI] [PubMed] [Google Scholar]; Morrison, R., O'connor, R.C., 2008. A systematic review of the relationship between rumination and suicidality. Suicide Life-Threatening Behav.38, 523–538. [DOI] [PubMed]
- Müller J., Bühner M., Ellgring H. Is there a reliable factorial structure in the 20-item Toronto Alexithymia Scale?: a comparison of factor models in clinical and normal adult samples. J. Psychosomatic Res. 2003;55:561–568. doi: 10.1016/s0022-3999(03)00033-3. [DOI] [PubMed] [Google Scholar]; Müller, J., Bühner, M., Ellgring, H., 2003. Is there a reliable factorial structure in the 20-item Toronto Alexithymia Scale?: aA comparison of factor models in clinical and normal adult samples. J. Psychosomatic Res.55, 561–568. [DOI] [PubMed]
- Na K.S., Oh S.J., Jung H.Y., Irene Lee S., Kim Y.K., Han C., Ko Y.H., Paik J.W., Kim S.G. Alexithymia and low cooperativeness are associated with suicide attempts in male military personnel with adjustment disorder: a case-control study. Psychiatry Res. 2013;205:220–226. doi: 10.1016/j.psychres.2012.08.027. [DOI] [PubMed] [Google Scholar]; Na, K.S., Oh, S.J., Jung, H.Y., Irene Lee, S., Kim, Y.K., Han, C., Ko, Y.H., Paik, J.W., Kim, S.G., 2013. Alexithymia and low cooperativeness are associated with suicide attempts in male military personnel with adjustment disorder: aA case-control study. Psychiatry Res.205, 220–226. [DOI] [PubMed]
- Najmi S., Wegner D.M., Nock M.K. Thought suppression and self-injurious thoughts and behaviors. Behav. Res. Therapy. 2007;45:1957–1965. doi: 10.1016/j.brat.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]; Najmi, S., Wegner, D.M., Nock, M.K., 2007. Thought suppression and self-injurious thoughts and behaviors. Behav. Res. Therapy45, 1957–1965. [DOI] [PMC free article] [PubMed]
- Norman H., Borrill J. The relationship between self-harm and alexithymia. Scandinavian J. Psychol. 2015;56:405–419. doi: 10.1111/sjop.12217. [DOI] [PubMed] [Google Scholar]; Norman, H., Borrill, J., 2015. The relationship between self-harm and alexithymia. Scandinavian J. Psychol.56, 405–419. [DOI] [PubMed]
- Office for National Statistics . Office for National Statistics; London: 2016. Suicides in the UK: 2016 Registrations. [Google Scholar]; Office for National Statistics, 2016. Suicides in the UK: 2016 Registrations. Office for National Statistics, London.
- Osman A., Bagge C.L., Gutierrez P.M., Konick L.C., Kopper B.A., Barrios F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8:443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]; Osman, A., Bagge, C.L., Gutierrez, P.M., Konick, L.C., Kopper, B.A., Barrios, F.X., 2001. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment8, 443–454. [DOI] [PubMed]
- Parker J.D., Eastabrook J.M., Keefer K.V., Wood L.M. Can alexithymia be assessed in adolescents? Psychometric properties of the 20-item Toronto Alexithymia Scale in younger, middle, and older adolescents. Psychological Assessment. 2010;22:798. doi: 10.1037/a0020256. [DOI] [PubMed] [Google Scholar]; Parker, J.D., Eastabrook, J.M., Keefer, K.V., Wood, L.M., 2010. Can alexithymia be assessed in adolescents? Psychometric properties of the 20-item Toronto Alexithymia Scale in younger, middle, and older adolescents. Psychological Assessment22, 798. [DOI] [PubMed]
- Pierloot R., Vinck J. A pragmatic approach to the concept of alexithymia. Psychotherapy Psychosomatics. 1977;28:156–166. doi: 10.1159/000287058. [DOI] [PubMed] [Google Scholar]; Pierloot, R., Vinck, J., 1977. A pragmatic approach to the concept of alexithymia. Psychotherapy Psychosomatics28, 156–166. [DOI] [PubMed]
- Pisani A.R., Wyman P.A., Petrova M., Schmeelk-Cone K., Goldston D.B., Xia Y., Gould M.S. Emotion regulation difficulties, youth–adult relationships, and suicide attempts among high school students in underserved communities. J. Youth Adolescence. 2013;42:807–820. doi: 10.1007/s10964-012-9884-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Pisani, A.R., Wyman, P.A., Petrova, M., Schmeelk-Cone, K., Goldston, D.B., Xia, Y., Gould, M.S., 2013. Emotion regulation difficulties, youth–adult relationships, and suicide attempts among high school students in underserved communities. J. Youth Adolescence42, 807–820. [DOI] [PMC free article] [PubMed]
- Plutchik R., Van Praag H.M., Conte H.R. Correlates of suicide and violence risk: III. A two-stage model of countervailing forces. Psychiatry Res. 1989;28:215–225. doi: 10.1016/0165-1781(89)90048-6. [DOI] [PubMed] [Google Scholar]; Plutchik, R., Van Praag, H.M., Conte, H.R., 1989. Correlates of suicide and violence risk: III. A two-stage model of countervailing forces.Psychiatry Res.28, 215–225. [DOI] [PubMed]
- Reinherz H.Z., Tanner J.L., Berger S.R., Beardslee W.R., Fitzmaurice G.M. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. Am. J. Psychiatry. 2006;163:1226–1232. doi: 10.1176/ajp.2006.163.7.1226. [DOI] [PubMed] [Google Scholar]; Reinherz, H.Z., Tanner, J.L., Berger, S.R., Beardslee, W.R., Fitzmaurice, G.M., 2006. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. Am. J. Psychiatry163, 1226–1232. [DOI] [PubMed]
- Rogers R. Dissertation Abstracts International: Section B: The Sciences and Engineering 76. 2015. Female psychopathy predictors: cluster B traits and alexithymia. No-Specified. [Google Scholar]; Rogers, R., 2015. Female psychopathy predictors: cCluster B traits and alexithymia. Dissertation Abstracts International: Section B: The Sciences and Engineering 76, No Pagination Specified.
- Sakuraba S., Kubo M., Komoda T., Yamana J. Suicidal ideation and alexithymia in patients with alcoholism: a pilot study. Subst. Use Misuse. 2005;40:823–830. doi: 10.1081/ja-200030702. [DOI] [PubMed] [Google Scholar]; Sakuraba, S., Kubo, M., Komoda, T., Yamana, J., 2005. Suicidal ideation and alexithymia in patients with alcoholism: a pilot study. Subst. Use Misuse40, 823–830. [DOI] [PubMed]
- Salminen J., Saarijärvi S., Toikka T., Kauhanen J., Äärelä E. Alexithymia behaves as a personality trait over a 5-year period in Finnish general population. J. Psychosomatic Res. 2006;61:275–278. doi: 10.1016/j.jpsychores.2006.01.014. [DOI] [PubMed] [Google Scholar]; Salminen, J., Saarijärvi, S., Toikka, T., Kauhanen, J., Äärelä, E., 2006. Alexithymia behaves as a personality trait over a 5-year period in Finnish general population. J. Psychosomatic Res.61, 275–278. [DOI] [PubMed]
- Sayar K., Acar B., Ak I. Alexithymia and Suicidal Behavior. Israel J. Psychiatry Relat. Sci. 2003;40:165–173. [PubMed] [Google Scholar]; Sayar, K., Acar, B., Ak, I., 2003. Alexithymia and Suicidal Behavior. Israel J. Psychiatry Relat. Sci.40, 165–173. [PubMed]
- Shneidman E.S. Oxford University Press; USA: 1998. The Suicidal Mind. [Google Scholar]; Shneidman, E.S., 1998. The Suicidal Mind. Oxford University Press, USA.
- Sifneos P.E. The prevalence of ‘alexithymic'characteristics in psychosomatic patients. Psychotherapy Psychosomatics. 1973;22:255–262. doi: 10.1159/000286529. [DOI] [PubMed] [Google Scholar]; Sifneos, P.E., 1973. The prevalence of ‘alexithymic'characteristics in psychosomatic patients. Psychotherapy Psychosomatics22, 255–262. [DOI] [PubMed]
- Silverman M.M., Berman A.L., Sanddal N.D., O'carroll P.W., Jr Joiner. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors part 2: suicide‐related ideations, communications, and behaviors. Suicide Life Threatening Behav. 2007;37:264–277. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]; Silverman, M.M., Berman, A.L., Sanddal, N.D., O'carroll, P.W., Joiner Jr, T.E., 2007. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors part 2: suicide‐related ideations, communications, and behaviors. Suicide Life Threatening Behav.37, 264–277. [DOI] [PubMed]
- Sterne J.A., Sutton A.J., Ioannidis J.P., Terrin N., Jones D.R., Lau J., Carpenter J., Rücker G., Harbord R.M., Schmid C.H. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]; Sterne, J.A., Sutton, A.J., Ioannidis, J.P., Terrin, N., Jones, D.R., Lau, J., Carpenter, J., Rücker, G., Harbord, R.M., Schmid, C.H., 2011. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj343, d4002. [DOI] [PubMed]
- Tarrier N., Taylor K., Gooding P. Cognitive-behavioral interventions to reduce suicide behavior: a systematic review and meta-analysis. Behav. Modification. 2008;32:77–108. doi: 10.1177/0145445507304728. [DOI] [PubMed] [Google Scholar]; Tarrier, N., Taylor, K., Gooding, P., 2008. Cognitive-behavioral interventions to reduce suicide behavior: a systematic review and meta-analysis. Behav. Modification32, 77–108. [DOI] [PubMed]
- Taylor G.J. Alexithymia: concept, measurement, and implications for treatment. Am. J. Psychiatry. 1984 doi: 10.1176/ajp.141.6.725. [DOI] [PubMed] [Google Scholar]; Taylor, G.J., 1984. Alexithymia: concept, measurement, and implications for treatment. Am. J. Psychiatry. [DOI] [PubMed]
- Taylor G.J. Recent developments in alexithymia theory and research. Can. J. Psychiatry. 2000;45:134–142. doi: 10.1177/070674370004500203. [DOI] [PubMed] [Google Scholar]; Taylor, G.J., 2000. Recent developments in alexithymia theory and research. Can. J. Psychiatry45, 134–142. [DOI] [PubMed]
- Taylor, G.J., Bagby, R.M., 2000. An overview of the alexithymia construct.
- Taylor G.J., Ryan D., Bagby M. Toward the development of a new self-report alexithymia scale. Psychotherapy Psychosomatics. 1985;44:191–199. doi: 10.1159/000287912. [DOI] [PubMed] [Google Scholar]; Taylor, G.J., Ryan, D., Bagby, M., 1985. Toward the development of a new self-report alexithymia scale. Psychotherapy Psychosomatics44, 191–199. [DOI] [PubMed]
- Thompson S.G., Higgins J.P. How should meta‐regression analyses be undertaken and interpreted? Stat. Med. 2002;21:1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]; Thompson, S.G., Higgins, J.P., 2002. How should meta‐regression analyses be undertaken and interpreted? Statistics in medicine 21, 1559–1573. [DOI] [PubMed]
- Thorberg F.A., Young R.M., Sullivan K.A., Lyvers M., Connor J.P., Feeney G.F. A psychometric comparison of the Toronto Alexithymia Scale (TAS-20) and the Observer Alexithymia Scale (OAS) in an alcohol-dependent sample. Personality Individual Differences. 2010;49:119–123. [Google Scholar]; Thorberg, F.A., Young, R.M., Sullivan, K.A., Lyvers, M., Connor, J.P., Feeney, G.F., 2010. A psychometric comparison of the Toronto Alexithymia Scale (TAS-20) and the Observer Alexithymia Scale (OAS) in an alcohol-dependent sample. Personality Individual Differences49, 119–123. [DOI] [PubMed]
- Velasco C., Fernández I., Páez D. Boletín de Psicología; Spain: 2001. Alexitimia, afrontamiento, Compartir Social y Salud. [Google Scholar]; Velasco, C., Fernández, I., Páez, D., 2001. Alexitimia, afrontamiento, Compartir Social y Salud. Boletín de Psicología (Spain).
- Vilhjálmsson R., Sveinbjarnardottir E., Kristjansdottir G. Factors associated with suicide ideation in adults. Social Psychiatry Psychiatric Epidemiol. 1998;33:97–103. doi: 10.1007/s001270050028. [DOI] [PubMed] [Google Scholar]; Vilhjálmsson, R., Sveinbjarnardottir, E., Kristjansdottir, G., 1998. Factors associated with suicide ideation in adults. Social Psychiatry Psychiatric Epidemiol.33, 97–103. [DOI] [PubMed]
- Vine R. Google scholar. J. Med. Lib. Assoc. 2006;94:97. [Google Scholar]; Vine, R., 2006. Google scholar. J. Med. Lib. Assoc.94, 97.
- WHO, 2014. Preventing suicide: aA global imperative.
- Wood R.L.L., Williams C., Lewis R. Role of alexithymia in suicide ideation after traumatic brain injury. J. Int. Neuropsychol. Soc. 2010;16:1108–1114. doi: 10.1017/S1355617710001013. [DOI] [PubMed] [Google Scholar]; Wood, R.L.L., Williams, C., Lewis, R., 2010. Role of alexithymia in suicide ideation after traumatic brain injury. J. Int. Neuropsychol. Soc.16, 1108–1114. [DOI] [PubMed]
- Zech E., Luminet O., Rimé B., Wagner H. Alexithymia and its measurement: confirmatory factor analyses of the 20-item Toronto Alexithymia Scale and the Bermond-Vorst Alexithymia Questionnaire. Eur. J. Personality. 1999;13:511–532. [Google Scholar]; Zech, E., Luminet, O., Rimé, B., Wagner, H., 1999. Alexithymia and its measurement: confirmatory factor analyses of the 20-item Toronto Alexithymia Scale and the Bermond-Vorst Alexithymia Questionnaire. Eur. J. Personality13, 511–532.
- Zeman J., Cassano M., Perry-Parrish C., Stegall S. Emotion regulation in children and adolescents. J. Dev. Behav. Pediatrics. 2006;27:155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]; Zeman, J., Cassano, M., Perry-Parrish, C., Stegall, S., 2006. Emotion regulation in children and adolescents. J. Dev. Behav. Pediatrics27, 155–168. [DOI] [PubMed]
- Zlotnick C., Donaldson D., Spirito A., Pearlstein T. Affect regulation and suicide attempts in adolescent inpatients. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:793–798. doi: 10.1097/00004583-199706000-00016. [DOI] [PubMed] [Google Scholar]; Zlotnick, C., Donaldson, D., Spirito, A., Pearlstein, T., 1997. Affect regulation and suicide attempts in adolescent inpatients. J. Am. Acad. Child Adolesc. Psychiatry36, 793–798. [DOI] [PubMed]
- Zlotnick C., Wolfsdorf B.A., Johnson B., Spirito A. Impaired self-regulation and suicidal behavior among adolescent and young adult psychiatric inpatients. Arch. Suicide Res. 2003;7:149–157. [Google Scholar]; Zlotnick, C., Wolfsdorf, B.A., Johnson, B., Spirito, A., 2003. Impaired self-regulation and suicidal behavior among adolescent and young adult psychiatric inpatients. Arch. Suicide Res.7, 149–157.
- Zung W.W. A self-rating depression scale. Arch. Gen. Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]; Zung, W.W., 1965. A self-rating depression scale. Arch. Gen. Psychiatry12, 63–70. [DOI] [PubMed]