Abstract
Background
Autologous fat transfer in breast reconstruction has become increasingly important in breast reconstructive surgery. Although the indication to obtain fat, the various operative procedures, and the risks for the patient have been addressed in a large number of studies, detailed information on the everyday use of autologous lipotransfer in breast units in Germany is still lacking.
Methods
The objective of the study was to obtain primary data on the use of autologous lipotransfer to treat breast cancer patients in Germany and to determine measures for quality assurance in the daily practice. An online questionnaire concerning breast cancer and lipofilling was sent to specialists in gynecology and plastic surgery.
Results
Two-thirds of the specialists who responded to the questionnaire use autologous lipotransfer for breast reconstruction and did not report an increase of local recurrence following lipotransfer. There were only small differences between gynecologists and plastic surgeons regarding the procedure and indication for lipotransfer. The method is highly accepted by patients and physicians, and both gynecologists and plastic surgeons rated the improvement achieved through lipofilling as ‘high’.
Conclusions
The lack of randomized controlled data, especially in high-risk patients, demonstrates the necessity for a registry study on this topic. Our survey describes, in detail, the indications for lipofilling as well as its appropriate application in breast cancer patients in Germany and may thereby reduce the present therapeutic uncertainties.
Keywords: Lipofilling, Breast cancer, Autologous lipotransfer, Plastic-reconstructive surgery fat grafting
Introduction
Autologous fat transplantation has become increasingly important in breast reconstruction after (breast) surgery in breast cancer patients. It is mainly used for contour enhancements after breast conservation therapy (BCT) and heterologous or autologous breast reconstruction after mastectomy. Despite the increasing popularity of the procedure, the advantages and disadvantages have been discussed controversially. Autologous material has several advantages: Immunologic rejection reactions as seen with alloplastic and allogenic materials do not occur. The access to large volumes of fat tissue (depending on the existing amount of subcutaneous fat tissue), which can be obtained without causing significant donor site defects, and the minimal complication rate are additional advantages of this method. Fat tissue is metabolically active tissue consisting of a heterogeneous cell population: mature adipocytes, fibroblasts, blood vessels, and adipose-derived stromal cells (ASCs) [1, 2, 3]. Due to cell differentiation and the release of cytokines, fat tissue possesses unique regenerative qualities. Rohrich et al. [4] showed that the cell quality and the survival rate of the fat transplant are independent of the extraction site.
The extraction technique, however, may have an effect on the vitality and purity of the mature adipocytes and on the number of the transplanted adipose-derived regenerative cells (ADRCs) and may thereby play a decisive role in the success of autologous fat transplantation [5, 6].
The disadvantages of lipotransfer are the general risks of surgery, necrosis, infections [7, 8, 9, 10], cyst formation [11], or loss of the transplant [12, 13, 14, 15]. Whether or not transplantation of ASCs and ADRCs can influence the risk of recurrence has been questioned, and several studies have shown that there is an increase in tumor cell vitality and cell proliferation, as well as a decrease in apoptosis following lipotransfer [16, 17]. Sun et al. [18], on the other hand, found a downregulation of cell signals and an inhibition of tumor tissue proliferation. By contrast, Lohsiriwat et al. [19] published a retrospective study demonstrating an increase in local recurrence after lipotransfer in a subgroup (n = 9) with an elevated risk profile (poorly differentiated breast cancer, high Ki-67 proliferation index, unclear margin status), when primary resection of the tumor and lipofilling were less than 3 years apart. Interestingly, there were no local recurrences when the lipotransfer was performed more than 3 years after the primary breast cancer surgery. This agrees with 2 recent case-control studies that also did not demonstrate an increased risk for recurrence following autologous lipotransfer [20, 21].
These data show why the role of endocrine, paracrine, and autocrine activities of the transplanted fat tissues and the actual risk of recurrence remain unclear. Our literature search did not identify adequately powered randomized controlled trials on the topic of lipotransfer, and the existing publications have low levels of evidence and are statistically and methodologically biased. We consider it fundamental to further elucidate the field of indication for fat transplantation in breast reconstructive surgery.
Therefore, the objective of our retrospective survey was to obtain primary data regarding the use of lipofilling from specialists in medical societies and study groups who treat breast cancer patients in Germany on a daily basis and to identify difficulties or concerns regarding the indications for and limitations of lipofilling.
Material and Methods
Between December 2014 and December 2015, 360 specialists in breast centers were contacted via e-mail by the following medical societies: Nord-Ostdeutsche Gesellschaft für Gynäkologische Onkologie (NOGGO), Westdeutsche Studiengruppe (WSG), German Breast Group (GBG), Arbeitsgemeinschaft für ästhetische, plastische und wiederherstellende Operationsverfahren in der Gynäkologie (AWO Gyn) and Deutsche Gesellschaft der Plastischen, Rekonstruktiven und Ästhetischen Chirurgen (DGPRÄC). They were requested to respond retrospectively to an agreed-upon questionnaire concerning the use of lipotransfer for breast reconstruction in patients who had had breast cancer. The questionnaire was designed with our co-authors' expert advice. The questions in the online questionnaire could be answered with yes/no, as multiple choice, or by ranking. There was only 1 answer for some of the questions; for others, more than 1 answer could be given. A descriptive statistical presentation was chosen because of the limited number of cases.
Results
Baseline Data
The response rate to the questionnaire was 16.4%. 59 of the 360 contacted physicians responded to the survey, of which 42 were specialists in gynecology, 16 were specialists for plastic-reconstructive surgery, and 1 was a specialist in both areas. 35 of the 59 physicians (59.3%) use lipotransfer as a reconstructive procedure in breast cancer patients (gynecology (G): 44.2%; plastic surgery (PS): 100%). 86.4% of the physicians who use lipotransfer work at an oncologically certified center (G: 95.4%; PS: 64.2%) and 91.5% work at an interdisciplinary breast center (G: 100.0%; PS: 70.6%). During the monitored time, 16,671 breast cancer operations were performed in these centers and lipotransfer was offered to the patients in 927 cases (equally distributed between G and PS). On average, the participating specialists had been using lipotransfer in breast cancer patients for 5 years (G: 4 years; PS: 6 years).
Details Regarding the Procedure
There were no differences regarding the liposuction system (LipiVage® in 39.4%, Body-jet® in 39.4%, and Coleman in 36.4%), though gynecologists used the LipiVage system more often (61.1%) and plastic surgeons preferred the Body-jet (62.5%) and the Coleman system (50.0%). In 59.4%, the fat tissue was prepared by sedimentation, in 37.5% by filtration, and in 31.3% by centrifugation. In 22.9%, the fat tissue was injected under constant sonographic view (G: 31.9%; PS: 17.7%).
All physicians injected fat tissue subcutaneously (100%) followed by prepectoral injection in 60%, intramuscular injection in 40%, intraglandular injection in 14.3%, and subpectoral injection in 11.4%.
In 70.6%, the average amount of transferred fat tissue was 50-150 ml per procedure (G: 72.3%; PS: 40.0%). 25-50 ml were transferred in 17.7% (G: 33.3%; PS: 5.8%) and more than 150 ml in 14.7% (G: 0%; PS: 29.4%). Overall, the plastic surgeons tended to transfer greater volumes/a greater amount of fat than the gynecologists.
No survey participant reported a transfer below 25 ml. In 70.6%, the plastic surgeons transferred a volume of more than 100 ml, whereas in 72.3%, the gynecologist transferred a volume between 50 and 100 ml.
Indication and Limitations of the Procedure
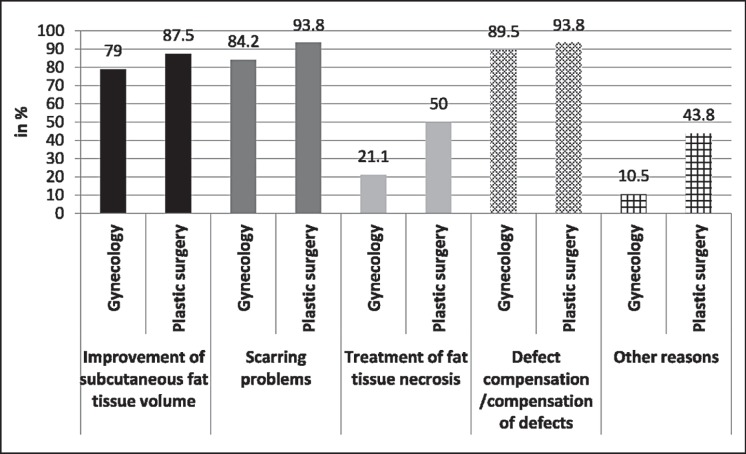
The majority of the respondents used lipotransfer for contour enhancements after mastectomy with implant-based breast reconstruction, autologous-based breast reconstruction and after BCT, and less often as the only method for breast reconstruction after mastectomy (table 1, fig. 1).
Table 1.
General information by the study participants regarding the use of lipotransfer in breast cancer patientsa
| 1 | 2 | 3 | 4 | 5 | Rating Average | |
|---|---|---|---|---|---|---|
| Only method after mastectomy | 6 | 7 | 5 | 8 | 8 | 3.15 |
| After mastectomy and implant reconstruction | 9 | 15 | 8 | 2 | 0 | 2.09 |
| After a breast-conserving operation without significant intraglandular volume reconstruction < 25% | 3 | 8 | 12 | 7 | 3 | 2.97 |
| After a breast-conserving operation with significant intraglandular volume reconstruction > 25% | 6 | 3 | 7 | 14 | 3 | 3.15 |
| Contour enhancement after autologous tissue reconstruction | 10 | 0 | 2 | 2 | 1 | 1.93 |
1 = Most frequent; 5 = least frequent.
Fig. 1.
Indications for lipotransfer differentiated according to the treating specialty.
Mammography was not seen as a contraindication after lipotransfer, when performed after complete healing of the wound. Common mammographic changes were the formation of oil cysts (70%), fatty tissue necroses (63.3%), and micro-calcifications (50%), and were mainly detected after intraglandular injection (93.3%), as compared to the other injection sites (0-6.7%). The fat graft survival rate was estimated to be 60.0%. There were no differences among the specialists regarding the above-mentioned points.
Of the participants, 35.3% applied for coverage of the costs for lipotransfer of the affected breast by a health insurance company (G: 31.6%; PS: 52.9%), whereas 51.5% applied for coverage of the costs for lipotransfer of the healthy breast to achieve symmetry (G: 29.4%; PS: 70.6%). We have no information on how often the health insurance companies actually covered the costs for lipotransfer. One-third of both gynecologists and plastic surgeons were concerned about an increased risk of local recurrence after lipotransfer. 63.2% of the gynecologists and 20% of the plastic surgeons performed lipotransfer irrespective of the tumor biology. However, the specification of the patients' BRCA status was not included in the questionnaire.
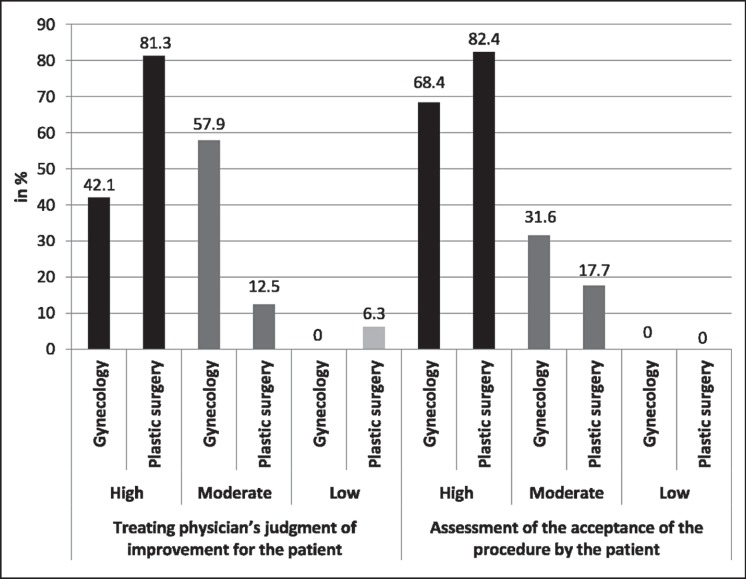
Rate of Satisfaction
The physicians rated the breast shape improvement through lipofilling as high in 61.8%, as intermediate in 35.3%, and as low in 2.9%. They estimated the level of acceptance by the patient to be high in 77.1% and intermediate in 22.9% (fig. 2).
Fig. 2.
Patients' and physicians' rate of satisfaction with the use of lipotransfer in breast cancer patients.
Discussion
In recent years, autologous fat transfer has become increasingly important in breast reconstruction after breast surgery due to cancer. This, however, has led to intense discussions regarding its advantages and disadvantages, especially concerning a potentially increased carcinogenic risk after lipotransfer [16, 17, 18, 21, 22].
In one of the largest observational studies on this subject, Kronowitz et al. [23] compared the rate of local recurrence in breast cancer patients with breast tissue removal and autologous lipotransfer for breast reconstruction (n = 1,000) and patients without lipotransfer (n = 670) after a median follow-up of 60 months between 1981 and 2014 in the USA. No differences were seen in the rate of local recurrence between the two patient groups. However, their analyses showed statistical and methodological bias and they did not provide adequate information on the patients' risk profile or BRCA status [24, 25].
Two-thirds of the specialists participating in our survey had no concerns regarding the induction of local recurrence after autologous lipotransfer, which agrees with the findings by Kronowitz et al. [23] as well as with several recent clinical studies showing no increase in the incidence of breast cancer in patients after autologous fat transfer [2, 23, 26, 27, 28, 29].
To our knowledge, there are no studies reporting a higher rate of recurrence in patients with a BRCA mutation. Nevertheless, the current guideline for autologous fat transplantation released by the German Society for Plastic Reconstruction, Dermatology and Gynecology recommends that autologous lipotransfer should only be performed in BRCA-positive women given a strict indication [30].
In our survey, the great majority of the participating physicians rated the improvement and the acceptance of lipotransfer by the patients as ‘high’. In their study, Harder et al. [31] describe the performance of autologous fat transfer with a morbidity rate below 1%. They refer to studies that describe a total of 2,254 autologous fat transfers with only 21 infections (<1%). These infections healed conservatively and did not require surgical intervention [25, 30, 31, 32]. However, the authors noted that the end points regarding complications after autologous fat transfer were defined differently in the studies, which made a direct comparison difficult [31].
Aside from the medical aspects, economic factors also play an important role in autologous breast reconstruction. Unfortunately, the health insurance companies in Germany do not generally cover the expenses for lipofilling, which could explain why only 35-51% of the participating specialists applied for the coverage of costs at all. (Unfortunately, we have no information on how often the health insurances actually covered the costs for lipotransfer.) Although lipofilling undoubtedly has a great benefit for the patient by achieving breast symmetry after breast cancer surgery and is well accepted by both patients and physicians, the health insurers are reluctant to cover the costs [32]. This problem must be addressed in the future, especially because lipofilling has gained such importance in breast reconstruction therapy.
The participants were asked to evaluate the basic benefits of the method as well as the patients' acceptance. The data show that the plastic surgeons rated both the cosmetic results and the patient acceptance more positively than the gynecologists. Evaluation of patient acceptance and satisfaction with lipofilling by the treating physicians has not been assessed in any international study and should play a relevant role in subsequent investigations.
The high acceptance shown by the participating centers regarding structured data collection (including follow-up data) indicates that the establishment of a national registry would be an important step. This would simplify analyses in the future and would allow reliable monitoring of patient safety. Inconsistent definitions of complication rates could be avoided; a predefined procedure to evaluate the rate of satisfaction by both patients and physicians and reliable data for the rate of recurrence after autologous fat transfer could be generated. The liposuction procedures and techniques should be evaluated and transmitted to the registry as well.
Our survey has a few limitations that must be discussed: The response rate to the questionnaire was low with only 16.4% and therefore cannot fully represent the use of autologous lipotransfer in Germany. In addition, the nature of surveys on a voluntary basis is that they lead to a positive selection as only centers experienced with the method tend to respond. Further, the low number of participating physicians did not allow detailed statistical calculations, so that the subgroup analyses were performed as descriptive analyses.
However, the data clearly show that autologous fat transplantation has been well accepted in breast reconstructive surgery both by gynecologists and plastic surgeons, resulting in an increase in patient satisfaction. In order to reduce therapeutic uncertainties in the use of autologous fat transplantation for breast cancer patients, additional basic research and extensive clinical studies should be performed, especially when a high risk of recurrence or a BRCA mutation is present. The establishment of a registry to collect clinically relevant data regarding lipofilling in breast cancer patients would greatly improve the clinical practice.
Conclusions
Our survey is the first to describe the indications and limitations of autologous fat transfer and to provide detailed information on its use in the daily practice in breast units and plastic reconstructive surgery departments in Germany. Autologous fat transfer is a well-established method to enhance the breast contour after BCT and after implant- or autologous-based breast reconstructive surgery. A search of the literature, as well as our own data, shows a lack of prospective, systematic studies concerning the reliability of this reconstructive procedure in breast cancer patients. The collection of high-quality prospective data with a representative long-term follow-up period in a national registry could help us identify methodological difficulties and limitations and determine the patients' rate of satisfaction and quality of life after the procedure. This should be addressed in future studies.
Disclosure Statement
The authors declare that they have no financial connections with any companies that may be of relevance for this article.
Acknowledgement
We would like to thank all colleagues who participated in the study and thereby contributed to improve the treatment for breast cancer patients.
References
- 1.Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- 2.Rigotti G, Marchi A, Sbarbati A. Adipose-derived mesenchymal stem cells: past, present, and future. Aesthetic Plast Surg. 2009;33:271–273. doi: 10.1007/s00266-009-9339-7. [DOI] [PubMed] [Google Scholar]
- 3.Pearl RA, Leedham SJ, Pacifico MD. The safety of autologous fat transfer in breast cancer: lessons from stem cell biology. J Plast Reconstr Aesthet Surg. 2012;65:283–288. doi: 10.1016/j.bjps.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rohrich R, Sorokin E, Brown S. In search of improved fat transfer viability: a quantitative analysis of the role of centrifugation and harvest site. Plast Reconstr Surg. 2004;113:391–395. doi: 10.1097/01.PRS.0000097293.56504.00. [DOI] [PubMed] [Google Scholar]
- 5.Gehmert S, Gehmert S, Hidayat M, Sultan M, Berner A, Klein S. Angiogenesis: the role of PDGF-BB on adipose-tissue derived stem cells (ASCs) Clin Hemorheol Microcirc. 2011;48:5–13. doi: 10.3233/CH-2011-1397. [DOI] [PubMed] [Google Scholar]
- 6.Conde-Green A, Baptista L, de Amorin N, de Oliveira E, da Silva K, Pedrosa CS. Effects of centrifugation on cell composition and viability of aspirated adipose tissue processed for transplantation. Aesthet Surg J. 2010;30:249–255. doi: 10.1177/1090820X10369512. [DOI] [PubMed] [Google Scholar]
- 7.Hang-Fu L, Marmolya G, Feiglin D. Liposuction fat-fillant implant for breast augmentation and reconstruction. Aesthetic Plast Surg. 1995;19:427–437. doi: 10.1007/BF00453876. [DOI] [PubMed] [Google Scholar]
- 8.Valdatta L, Thione A, Buoro M, Tuinder S. A case of life-threatening sepsis after breast augmentation by fat injection. Aesthetic Plast Surg. 2001;25:347–349. doi: 10.1007/s002660010147. [DOI] [PubMed] [Google Scholar]
- 9.Kuran I, Tumerdem B. A new simple method used to prepare fat for injection. Aesthetic Plast Surg. 2005;29:18–22. doi: 10.1007/s00266-004-0059-8. [DOI] [PubMed] [Google Scholar]
- 10.Niechajev I. Lip enhancement: surgical alternatives and histologic aspects. Plast Reconstr Surg. 2000;105:1173–1183. doi: 10.1097/00006534-200003000-00055. [DOI] [PubMed] [Google Scholar]
- 11.Juhl AA, Redsted S, Engberg Damsgaard T. Autologous fat grafting after breast conserving surgery: breast imaging changes and patient-reported outcome. J Plast Reconstr Aesthet Surg. 2018;71:1570–1576. doi: 10.1016/j.bjps.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Gutowski K. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg. 2009;124:272–280. doi: 10.1097/PRS.0b013e3181a09506. [DOI] [PubMed] [Google Scholar]
- 13.Coleman S. Lower lid deformity secondary to autogenous fat transfer: a cautionary tale. Aesthetic Plast Surg. 2008;32:415–417. doi: 10.1007/s00266-007-9007-8. [DOI] [PubMed] [Google Scholar]
- 14.Latoni J, Marshall D, Wolfe S. Overgrowth of fat autotransplanted for correction of localized steroid-induced atrophy. Plast Reconstr Surg. 2000;106:1566–1569. doi: 10.1097/00006534-200012000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Pulagam S, Poulton T, Mamounas E. Long-term clinical and radiologic results with autologous fat transplantation for breast augmentation: case reports and review of the literature. Breast J. 2006;12:63–65. doi: 10.1111/j.1075-122X.2006.00188.x. [DOI] [PubMed] [Google Scholar]
- 16.Hsu VM, Stransky CA, Bucky LP, Percec I. Fat grafting's past, present, and future: Why adipose tissue is emerging as a critical link to the advancement of regenerative medicine. Aesthet Surg J. 2012;32:892–899. doi: 10.1177/1090820X12455658. [DOI] [PubMed] [Google Scholar]
- 17.Zimmerlin L, Donnenberg AD, Rubin JP, Basse P, Landreneau RJ, Donnenberg VS. Regenerative therapy and cancer: in vitro and in vivo studies of the interaction between adipose-derived stem cells and breast cancer cells from clinical isolates. Tissue Eng Part A. 2011;17:93–106. doi: 10.1089/ten.tea.2010.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun B, Roh KH, Park JR, Lee SR, Park SB, Jung JW, Kang SK, Lee YS, Kang KS. Therapeutic potential of mesenchymal stromal cells in a mouse breast cancer metastasis model. Cytotherapy. 2009;11:289–298. doi: 10.1080/14653240902807026. [DOI] [PubMed] [Google Scholar]
- 19.Lohsiriwat V, Curigliano G, Rietjens M, Goldhirsch A, Petit JY. Autologous fat transplantation in patients with breast cancer: ‘silencing’ or ‘fueling’ cancer recurrence? Breast. 2011;20:351–357. doi: 10.1016/j.breast.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Silva-Vergara C, Fontdevila J, Weshahy O, Yuste M, Descarrega J, Grande L. Breast cancer recurrence is not increased with lipofilling reconstruction. Ann Plast Surg. 2017;79:243–248. doi: 10.1097/SAP.0000000000001106. [DOI] [PubMed] [Google Scholar]
- 21.Gale K, Rakha E, Ball G, Tan V, McCulley S, Macmillan R. A case controlled study of the oncological safety of fat grafting. Plast Reconstr Surg. 2015;135:1263–1275. doi: 10.1097/PRS.0000000000001151. [DOI] [PubMed] [Google Scholar]
- 22.Petit J, Rietjens M, Botteri E, et al. Evaluation of fat grafting safety in patients with intraepithelial neoplasia: a matched-cohort study. Ann Oncol. 2013;24:1479–1484. doi: 10.1093/annonc/mds660. [DOI] [PubMed] [Google Scholar]
- 23.Kronowitz S, Mandujano C, Liu J, et al. Lipofilling of the breast does not increase the risk of recurrence of breast cancer: a matched controlled study. Plast Reconstr Surg. 2016;137:385–393. doi: 10.1097/01.prs.0000475741.32563.50. [DOI] [PubMed] [Google Scholar]
- 24.Batista BN, Fraga MF, Sampaio MM, Barros AC. Lipofilling of the breast does not increase the risk of recurrence of breast cancer. Plast Reconstr Surg. 2016;138:1068e–1069e. doi: 10.1097/PRS.0000000000002794. [DOI] [PubMed] [Google Scholar]
- 25.Petit JY, Maisonneuve P. Lipofilling of the breast does not increase the risk of recurrence of breast cancer. Plast Reconstr Surg. 2016;138:937e–938e. doi: 10.1097/PRS.0000000000002707. [DOI] [PubMed] [Google Scholar]
- 26.Illouz Y, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009;33:706–715. doi: 10.1007/s00266-009-9377-1. [DOI] [PubMed] [Google Scholar]
- 27.Fraser J, Hedrick M, Cohen S. Oncologic risks of autologous fat grafting to the breast. Aesthet Surg J. 2011;31:68–75. doi: 10.1177/1090820X10390922. [DOI] [PubMed] [Google Scholar]
- 28.Khouri R, Rigotti G, Cardoso E, Khouri R, Biggs T. Megavolume autologous fat transfer: part I. Theory and principles. Plast Reconstr Surg. 2014;133:550–557. doi: 10.1097/01.prs.0000438044.06387.2a. [DOI] [PubMed] [Google Scholar]
- 29.Largo R, Tchang L, Mele V, Scherberich A, Harder Y, Wettstein R. Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67:437–448. doi: 10.1016/j.bjps.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 30.Deutsche Dermatologische Gesellschaft Deutsche Gesellschaft für Mund-Kiefer-und Gesichtschirurgie (DGMKG) Deutsche Gesellschaft für Gynäkologie und Geburtshilfe (DGGG) Leitlinie ‘Autologe Fetttransplantation’. 2015 www.dgpraec.de/wp-content/uploads/2018/03/S2k_Leitlinie_Fetttransplantation.pdf, (last accessed: April 11, 2018) [Google Scholar]
- 31.Harder Y, Allan AA, Eder M, Kovacs L, Schantz J, Machens H. Eigenfetttransfer zur Korrektur von erworbenen Konturdefekten und Volumenasymmetrien nach rekonstruktiven Brusteingriffen. Plastische Chirurgie. 2014:26–36. [Google Scholar]
- 32.Skillman J, Hardwicke J, Whisker L, England D. Attitudes of U.K. breast and plastic surgeons to lipomodelling in breast surgery. Breast. 2013;22:1200–1204. doi: 10.1016/j.breast.2013.08.005. [DOI] [PubMed] [Google Scholar]