Abstract
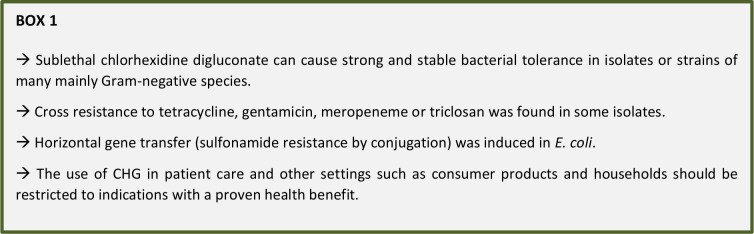
Chlorhexidine digluconate (CHG) is commonly used in healthcare, e.g. in skin antiseptics, antimicrobial soaps, alcohol-based hand rubs and oral or wound antiseptics. Aim of the literature review was to evaluate the potential of bacteria to adapt to low level CHG exposure. A maximum 4fold MIC increase to CHG was found after low level exposure in most of the 71 evaluated bacterial species. A strong adaptive mostly stable MIC change was described in strains or isolates of the healthcare-associated species E. coli, S. marcescens and P. aeruginosa (up to 500fold, 128fold or 32fold, respectively). The highest MIC values after adaptation were 2,048 mg/l (S. marcescens) and 1,024 mg/l (P. aeruginosa). A new resistance to tetracycline, gentamicin, meropeneme or triclosan was found in some adapted isolates. In E. coli horizontal gene transfer was induced (sulfonamide resistance by conjugation), pointing out an additional risk of sublethal CHG. The use of CHG in patient care - but also all other settings such as consumer products and households - should therefore be critically assessed and restricted to indications with a proven health benefit or justifiable public health benefits. Additional CHG has no health benefit when used in alcohol-based hand rubs and is not recommended by the WHO. For routine hand washing of soiled hands the use of plain soap is sufficient, CHG in soaps has no health benefit. In surgical hand antisepsis alcohol-based hand rubs should be preferred to CHG soaps. Implementation of these principles will help to reduce avoidable selection pressure.
Keywords: chlorhexidine digluconate, adaptation, resistance, cross-tolerance, low level exposure, MIC values
INTRODUCTION
Chlorhexidine digluconate (CHG) is a commonly used antiseptic agent in human healthcare and veterinary medicine, mainly used for hand hygiene (e.g. at 2% - 4% as the only active agent in antiseptic soaps or at 0.5% or 1% as an additional active agent in alcohol-based hand rubs), in alcohol-based skin antiseptics at 2% and in mouth rinse solutions at 0.12% - 0.2% [1]. The widespread CHG use in various types of applications has probably lead to an increase of acquired bacterial resistances, mainly in Gram-negative species such as Pseudomonas aeruginosa (minimal inhibitory concentration (MIC) of up to 800 mg/l), Serratia marcescens (MIC of up to 400 mg/l) or Klebsiella pneumoniae (MIC of up to 256 mg/l) [1]. In some types of applications such as skin antiseptics CHG has been shown to reduce healthcare associated infections, e.g. catheter-associated bloodstream infections [2]. Recent evidence also suggests a contribution to the prevention of surgical site infections [3] although the single effect of CHG for this application is still under controversial debate [4–6].
Its widespread use in hand hygiene by healthcare workers in many countries suggests to look specifically at all possible applications in this area. The WHO has published a recommendation on hand hygiene for healthcare in 2009 with the aim to reduce healthcare-associated infections [7]. Three types of applications can be distinguished. The use of alcohol-based hand rubs is recommended on clean hands in five specific clinical situations: before touching a patient, before clean or aseptic procedures, after body fluid exposure, after touching a patient and after touching patient surroundings [7, 8]. Hand washing with either plain soap or antiseptic soap and water is recommended for visibly soiled hands or in case of contamination with spore-forming bacteria such as Clostridium difficile [7]. The third type of application is in the surgical theater. Healthcare workers should decontaminate their hands prior to donning sterile surgical gloves with either alcohol-based hand rubs (surgical hand disinfection) or with antimicrobial soaps (surgical scrubbing) [7].
In the past years there is an increasing concern on the development of resistance not only to antibiotics but also to antiseptic agents which are essential to limit the spread of multidrug-resistant pathogens in healthcare [9, 10]. Some antiseptic agents are more likely than others to cause a bacterial tolerance or even resistance [11]. Aim of the review is therefore to evaluate the potential of CHG to cause an adaptive bacterial response during exposure to sublethal concentrations and to propose reasonable implications for the use of CHG in hand hygiene.
RESULTS
General remark
The magnitude of any adaptive response to CHG is expressed as an MIC change and assigned to one of the following three categories: No adaptive response (no MIC increase), weak adaptive response (MIC increase ≤ 4fold) and strong adaptive response (MIC increase > 4fold). For some bacterial species two or more studies were found resulting in data from various isolates or strains. That is why some bacterial species can be found in two or three categories depending on the results obtained with the various isolates or strains of the same species.
Adaptive bacterial response in Gram-negative species
No adaptive response was found in isolates or strains of 15 species (Acinetobacter baumannii, Aeromonas hydrophila, Campylobacter coli, Campylobacter jejuni, Chryseobacterium indologenes, Citrobacter spp., Cronobacter sakazakii, E. coli, K. pneumoniae, Moraxella osloensis, P. aeruginosa, Pseudomonas nitroreductans, Pseudomonas putida, Pseudoxanthomonas spp. and Sphingobacterium multivorum). Some isolates or strains of 12 species were able to express a weak adaptive response (MIC increase ≤ 4fold) such as A. xylosoxidans, A. jandaei, Chrysobacterium spp., E. cloacae, Enterobacter spp., E. coli, H. gallinarum, K. pneumoniae, P. aeruginosa, S. Typhimurium, Serratia spp. and S. maltophilia (Table 1).
TABLE 1:
Adaptive response of Gram-negative bacterial species to sublethal CHG exposure, adapted from [35].
| Species | Strain / isolate | Type of exposure | Increase in MIC | MICmax (mg/l) | Stability | Associated changes | Ref | |
|---|---|---|---|---|---|---|---|---|
| A. xylosoxidans | Domestic drain biofilm isolate MBRG 4.31 | 14 d at various concentrations | 2fold | 31.2 | No data | None reported | [36] | |
| A. baumannii | Strain MBRG15.1 from a domestic kitchen drain biofilm | 14 passages at various concentrations | None | 7.8 | Not applicable | None reported | [37] | |
| A. baylyi | Strain ADP1 | 30 min at 0.000001% | Protection from lethal CHG concentration (0.00007%) | No data | No data | More resistance to a lethal hydrogen peroxide concentration (300 mM) | [38] | |
| A. hydrophila | Domestic drain biofilm isolate MBRG 4.3 | 14 d at various concentrations | None | 15.6 | Not applicable | None reported | [36] | |
| A. jandaei | Domestic drain biofilm isolate MBRG 9.11 | 14 d at various concentrations | 2fold | 15.6 | No data | None reported | [36] | |
| A. proteolyticus | Domestic drain biofilm isolate MBRG 9.12 | 14 d at various concentrations | 16fold | 125 | No data | None reported | [36] | |
| B. fragilis | ATCC 25285 | 12 h at 0.06% | No data | No data | Not applicable | Induction of multiple antibiotic resistance*; 2.7fold – 6fold increase of 6 efflux pumps | [39] | |
| B. cenocepacia | 6 strains from clinical and environmental habitats | Up to 28 d at 15 mg/l | Survival | 100 | No data | No degradation of CHG | [40] | |
| B. cepacia | ATCC BAA-245 | 40 d at various concentrations | 8fold | 29 | Unstable for 14 d | Decrease biofilm formation | [41] | |
| B. cepacia complex | B. lata strain 383 | 5 min at 50 mg/l | No data | 700 | Not applicable | Reduced susceptibility** to ceftazidime (30 – 33 mm), ciprofloxacin (11 – 20 mm) and imipenem (15 – 21 mm; 2 of 4 experiments) and to meropenem (33 mm; 1 of 4 experiments); up-regulation of transporter and efflux pump genes | [42] | |
| C. coli | ATCC 33559 and a poultry isolate | Up to 15 passages with gradually higher concentrations | None | 0.031 | Not applicable | None described | [15] | |
| C. jejuni | NCTC 11168, ATCC 33560 and a poultry isolate | Up to 15 passages with gradually higher concentrations | None | 1 | Not applicable | None described | [15] | |
| C. indologenes | MRBG 4.29 (kitchen drain biofilm isolate) | 40 d at various concentrations | None | 7.3 | Not applicable | None described | [41] | |
| C. indologenes | Domestic drain biofilm isolate MBRG 9.15 | 14 d at various concentrations | None | 31.2 | Not applicable | None reported | [36] | |
| Chrysobacterium spp. | Domestic drain biofilm isolate MBRG 9.17 | 14 d at various concentrations | 2fold | 7.8 | No data | None reported | [36] | |
| Chrysobacterium spp. | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 5fold – 6fold | 30 | Unstable | Cross-adaptation* to benzalkoniumchloride (2fold - 100fold; 2 strains), triclosan (4fold; 1 strain) and didecyldimethyl- ammonium bromide (16fold; 1 strain); cross-resistance* to cefotaxime and ceftazidime (2 strains each), sulfamethoxazole, ampicillin and tetracycline (1 strain each) | [43] | |
| Citrobacter spp. | Domestic drain biofilm isolate MBRG 9.18 | 14 d at various concentrations | None | 1.9 | Not applicable | None reported | [36] | |
| C. sakazakii | Strain MBRG15.5 from a domestic kitchen drain biofilm | 14 passages at various concentrations | None | 7.8 | Not applicable | None reported | [37] | |
| E. cloacae | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 10fold – 16fold | 80 | Stable for 20 subcultures (1 strain) | Cross-adaptation* to benzalkoniumchloride (6fold; 2 strains), triclosan (6fold - 15fold; 2 strains) and didecyldimethylammonium bromide (6fold; 1 strain); cross-resistance* to imipenem, ceftazidime and sulfamethoxazole (2 strains each), cefotaxime and tetracycline (1 strain each) | [43] | |
| E. ludwigii | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 6fold – 8fold | 40 | Unstable | Cross-adaptation* to benzalkoniumchloride (6fold – 8fold; 2 strains), triclosan (8fold – 10fold; 2 strains) and didecyldimethylammonium bromide (4fold – 6fold; 2 strains); cross-resistance* to imipenem, ceftazidime and sulfamethoxazole (2 strains each) | [43] | |
| Enterobacter spp. | 6 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 4fold – 10fold | 80 | Stable for 20 subcultures (1 strain) | Cross-adaptation* to benzalkoniumchloride (3fold – 20fold; 6 strains), triclosan (4fold – 100fold; 6 strains) and didecyldimethylammonium bromide (4fold – 6fold; 3 strains); cross-resistance* to ceftazidime and imipenem (3 strains each), cefotaxime and sulfamethoxazole (2 strains each) | [43] | |
| E. coli | ATCC 25922 | 40 d at various concentrations | None | 7.3 | Not applicable | None described | [41] | |
| E. coli | NCIMB 8879 | 6 x 48 h at variable concentrations | None | 0.7 | Not applicable | None reported | [44] | |
| E. coli | ATCC 25922 and strain MBRG15.4 from a domestic kitchen drain biofilm | 14 passages at various concentrations | 1.5fold - 5fold | 11.7 | Stable for 14 d | None reported | [37] | |
| E. coli | NCIMB 8545 | 0.00005% for 30 s, 5 min and 24 h | ≤ 6fold | 39 | Unstable for 10 d | No increase of MBC; unstable resistance** to tobramycin | [45] | |
| E. coli | NCTC 8196 | 12 w at various concentrations | 32fold | No data | No data | None described | [46] | |
| E. coli | NCTC 12900 strain O157 | 6 passages at variable concentrations | Approx. 500fold | Approx. 500 | Stable for 30 d | Increased tolerance** to triclosan (15 mm) | [47] | |
| E. coli | CV601 | 24.4 µg/l for 3 h | No data | 4.9 | Not applicable | Induction of horizontal gene transfer (sulfonamide resistance by conjugation) | [48] | |
| H. gallinarum | Domestic drain biofilm isolate MBRG 4.27 | 14 d at various concentrations | 2fold | 31.2 | No data | None reported | [36] | |
| K. oxytoca | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 2fold – 8fold | 40 | Unstable | Cross-adaptation* to benzalkoniumchloride (60fold; 1 strain), triclosan (3fold – 8fold; 2 strains) and didecyldimethyl- ammonium bromide (6fold; 1 strain) | [43] | |
| K. pneumoniae | 7 “Murray isolates” from the pre-CHG era | Up to 5 w at various concentrations | None (5 isolates) | 4fold (2 isolates) | 256 | Stable for 10 d | None reported | [49] |
| K. pneumoniae | 7 modern isolates / strains | Up to 5 w at various concentrations | 4fold - 16fold | > 512 | Stable for 10 d | None reported | [49] | |
| K. pneumoniae | 6 clinical strains with a variety of antibiotic resistance markers | 6 passages of 2 days at various concentrations | 4fold – 16fold | 512 | Stable for 10 d | Cross-resistance*** to colistin (6 strains); no cross-adaptation to benzalkoniumchloride, octenidine, hexadecylpyridinium chloride | monohydrate and ethanol | [16] |
| K. pneumoniae | ATCC 13883 | 40 d at various concentrations | 6.9fold | 14.5 | Stable for 14 d | Increase biofilm formation | [41] | |
| Klebsiella spp. | Biocide-sensitive strain from organic foods | Several passages with gradually higher concentrations | 2fold | 30 | Unstable | Cross-adaptation* to benzalkoniumchloride (12fold) and triclosan (12fold); cross-resistance* to imipenem and ceftazidime | [43] | |
| M. osloensis | Strain MBRG15.3 from a domestic kitchen drain biofilm | 14 passages at various concentrations | None | 2.0 | Not applicable | None reported | [37] | |
| P. agglomerans | 5 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 5fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (30fold – 40fold; 5 strains), triclosan (8fold – 100fold; 5 strains) and didecyldimethylammonium bromide (4fold - 6fold; 2 strains); cross-resistance* to cefotaxime and ceftazidime (3 strains each), tetracycline and sulfamethoxazole (2 strains each) and imipenem (1 strain) | [43] | |
| P. ananatis | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 10fold – 50fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (20fold – 30fold; 2 strains), triclosan (60fold – 100fold; 2 strains) and didecyldimethylammonium bromide (6fold; 2 strains); cross-resistance* to cefotaxime (2 strains), sulfamethoxazole, imipenem, ceftazidime and tetracycline (1 strain each) | [43] | |
| Pantoea spp. | 3 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 5fold – 16fold | 80 | Unstable | Cross-adaptation* to benzalkoniumchloride (6fold – 60fold; 2 strains), triclosan (8fold; 3 strains) and didecyldimethylammonium bromide (4fold - 6fold; 3 strains); cross-resistance* to tetracycline (2 strains), ampicillin, ceftazidime, cefotaxime, sulfamethoxazole and imipenem (1 strain each) | [43] | |
| P. aeruginosa | 178 CHG sensitive strains | Exposure to CHG | None | 625 | Not applicable | None reported | [50] | |
| P. aeruginosa | ATCC 9027 | 40 d at various concentrations | 2fold | 14.5 | Unstable for 14 d | None described | [41] | |
| P. aeruginosa | ATCC 9027 | 14 passages at various concentrations | 4fold | 31.3 | Stable for 14 d | None reported | [37] | |
| P. aeruginosa | NCIMB 10421 | 6 x 48 h at variable concentrations | 7fold | 70 | Stable for 15 d | High MICs to BAC did not change in a relevant extent | [44] | |
| P. aeruginosa | NCTC 6749 | 12 w at various concentrations | 8fold – 32fold | 1,024 | Stable for 7 w | None described | [46] | |
| P. nitroreductans | Domestic drain biofilm isolate MBRG 4.6 | 14 d at various concentrations | None | 3.9 | Not applicable | None reported | [36] | |
| P. putida | Strain MBRG15.2 from a domestic kitchen drain biofilm | 14 passages at various concentrations | None | 7.8 | Not applicable | None reported | [37] | |
| Pseudomonas spp. | Domestic drain biofilm isolate MBRG 9.14 | 14 d at various concentrations | 16fold | 15.6 | No data | None reported | [36] | |
| Pseudoxanthomonas spp. | Domestic drain biofilm isolate MBRG 9.20 | 14 d at various concentrations | None | 0.97 | Not applicable | None reported | [36] | |
| Ralstonia spp. | Domestic drain biofilm isolate MBRG 4.13 | 14 d at various concentrations | 21fold | 167 | No data | None reported | [36] | |
| S. Virchow | Food isolate | 6 passages at variable concentrations | Approx. 120fold | Approx. 120 | Stable for 30 d | Increased tolerance** to triclosan (0 mm) | [47] | |
| Salmonella enterica serovar | Typhimurium | Strain SL1344 | 5 min at 0.1, 0.5, 1 and 4 mg/l | 13fold – 27fold | 800 | Unstable for 1 d | 3fold – 67fold increase of tolerance*** to BAC | [51] |
| Salmonella enterica serovar | Typhimurium | Strain 14028S | 5 min at 1 and 5 mg/l | 3fold – 33fold | 1,000 | Unstable for 1 d | 2.5fold – 20fold increase of tolerance*** to BAC | [51] |
| S. enteritidis | ATCC 13076 | 7 d of sublethal exposure | ≥ 10fold | > 50 | Unstable | None reported | [52] | |
| Salmonella spp. | 3 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 5fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (8fold – 30fold; 2 strains) and triclosan (4fold - 8fold; 3 strains) cross-resistance* to cefotaxime, nalidixic acid and imipenem (2 strains each), tetracycline and sulfamethoxazole (1 strain each) | [43] | |
| Salmonella spp. | 6 strains with higher MICs to biocidal products | 8 days at increasing concentrations | 50fold – 200fold (2 strains) | > 1,000 | “stable” | One strain with increased tolerance*** | to tetracycline (> 16 mg/l), chloramphenicol (8 mg/l) and nalidixic acid (16 mg/l) | [53] |
| S. marcescens | Strain GSU 86-828 | 7 d exposure to CHG-containing contact lens solutions | 8fold | 50 | No data | Increased adherence to polyethylene | [54] | |
| S. marcescens | ATCC 13880 | 40 d at various concentrations | 9.6fold | 116 | Stable for 14 d | Increase biofilm formation | [41] | |
| S. marcescens | Clinical isolate | 12 w at various concentrations | 32fold – 128fold | 2,048 | Stable for 7 w | None described | [46] | |
| Serratia spp. | Not described | 5 to 8 transfers | “resistance“ to CHG | No data | “stable” | None described | [55] | |
| S. multivorum | Domestic drain biofilm isolate MBRG 9.19 | 14 d at various concentrations | None | 15.6 | Not applicable | None reported | [36] | |
| S. maltophilia | Domestic drain biofilm isolate MBRG 9.13 | 14 d at various concentrations | 4fold | 62.5 | No data | None reported | [36] | |
| S. maltophilia | MRBG 4.17 (kitchen drain biofilm isolate) | 40 d at various concentrations | 6fold | 29 | Stable for 14 d | None described | [41] |
spiral gradient endpoint method;
disc diffusion method;
broth microdilution;
macrodilution method
A strong but unstable MIC change (> 4fold) was found in isolates or strains of four species (Burkholderia cepacia, E. coli, Salmonella enteritidis, Salmonella Typhimurium). A strong and stable MIC change (> 4fold) was described for isolates or strains of seven species (E. coli, K. pneumoniae, P. aeruginosa, Salmonella Virchow, Salmonella spp., S. marcescens, Stenotrophomonas maltophilia). In isolates or strains of six species (Acinetobacter baylyi, Acinetobacter proteolyticus, E. coli, Pseudomonas spp., Ralstonia spp., S. marcescens) the adaptive response was strong but its stability was not described.
Selected strains or isolates revealed substantial MIC changes: E. coli (up to 500fold), Salmonella spp. (up to 200fold), S. marcescens (up to 128fold), P. aeruginosa (up to 32fold), or A. proteolyticus, K. pneumoniae, and Pseudomonas spp. (all up to 16fold). The highest MIC values after adaptation were found in S. marcescens (2,048 mg/l), P. aeruginosa (1,024 mg/l), Salmonella spp. (> 1,000 mg/l), B. cepacia complex (700 mg/l), K. pneumoniae (> 512 mg/l) and E. coli (500 mg/l). Most maximum MIC values are above the proposed epidemiological cut-off value of 16–64 mg/l to determine CHG resistance in Gram-negative bacterial species [12].
Cross resistance to various antibiotics such as tetracycline, gentamicin or meropeneme was found in some isolates of Bacterioides fragilis, B. cepacia complex and Salmonella spp.. In addition, a lower susceptibility to other biocidal agents was described for E. coli and S. Virchow to triclosan, for A. baylyi to hydrogen peroxide and for S. Typhimurium to benzalkonium chloride (BAC).
Other adaptive changes include a significant up-regulation of efflux pump genes in B. fragilis and B. cepacia complex. Horizontal gene transfer (sulfonamide resistance by conjugation) was induced in E. coli. VanA-type vancomycin resistance gene expression was increased vanA Enterococcus faecium (≥ 10fold increase of vanHAX encoding). Enhanced biofilm formation was described for K. pneumoniae and S. marcescens, adherence to poly-ethylene was increased in S. marcescens. Biofilm formation was decreased in B. cepacia.
Adaptive bacterial response in Gram-positive species
No adaptive response was found in isolates or strains from 18 species (Bacillus cereus, Corynebacterium xerosis, Enterococcus saccharolyticus, Eubacterium spp., Methylobacterium phyllosphaerae, Micrococcus luteus, Staphylococcus aureus, Staphylococcus capitis, Staphylococcus caprae, Staphylococcus cohnii, Staphylococcus epidermidis, Staphylococcus haemolyticus, Staphylococcus hominis, Staphylococcus kloosii, Staphylococcus lugdenensis, Staphylococcus saprophyticus, Staphylococcus warneri and Streptococcus mutans).
Some isolates or strains of 12 species ware able to express a weak adaptive response (MIC increase ≤ 4fold) such as B. cereus, Corynebacterium pseudogenitalum, Corynebacterium renale group, Enterococcus casseliflavus, Enterococcus faecalis, E. faecium, M. luteus, S. aureus, S. capitis, S. haemolyticus, S. lugdenensis and S. warneri.
A strong but unstable MIC change (> 4fold) was found in isolates or strains of E. faecalis. A strong MIC change (> 4fold) was also described for isolates or strains of S. aureus which could be stable or of unknown stability.
The largest MIC increase was noticed in S. aureus (up to 16fold) and E. faecalis (up to 6.7fold) leading to MIC values as high as 24.2 mg/l in E. faecalis and 20 mg/l in S. aureus (Table 2). Some maximum MIC values are above the proposed epidemiological cut-off value (8 mg/l for S. aureus) and some below (64 mg/l for E. faecalis) to determine CHG resistance in Gram-positive bacterial species [12].
TABLE 2:
Adaptive response of Gram-positive bacterial species to sublethal CHG exposure, adapted from [35].
| Species | Strain / isolate | Type of exposure | Increase in MIC | MICmax (mg/l) | Stability | Associated changes | Ref |
|---|---|---|---|---|---|---|---|
| B. cereus | MRBG 4.21 (kitchen drain biofilm isolate) | 40 d at various concentrations | None | 14.5 | Not applicable | None described | [41] |
| B. cereus | Domestic drain biofilm isolate MBRG 4.21 | 14 d at various concentrations | None | 1.9 | Not applicable | None reported | [36] |
| B. cereus | 4 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 6fold – 16fold | 80 | Stable for 20 subcultures (1 strain) | Cross-adaptation* to benzalkoniumchloride (≥ 100fold; 3 strains), triclosan (4fold – 36fold; 3 strains) and didecyldimethylammonium bromide (6fold; 2 strains); cross-resistance* to imipenem (4 strains), sulfamethoxazole (2 strains), ampicillin and tetracycline (1 strain each) | [43] |
| B. licheniformis | 2 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 4fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (40fold - 75fold; 2 strains) and triclosan (8fold; 1 strain); cross-resistance* to imipenem (2 strains), cefotaxime and tetracycline (1 strain each) | [43] |
| B. subtilis | 2 strains and 3 derivates | 2 h at 0.00005% | No data | No data | Not applicable | No increase of transfer of the mobile genetic element Tn916, a conjugative transposon | [56] |
| Bacillus spp. | 4 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 4fold – 8fold | 40 | Unstable | Cross-adaptation* to benzalkoniumchloride (15fold – 100fold; 4 strains), triclosan (8fold; 4 strains) and didecyldimethylammonium bromide (4fold - 6fold; 2 strains); cross-resistance* to imipenem and sulfamethoxazole (4 strains each), cefotaxime and ceftazidime (1 strain each) | [43] |
| C. pseudogenitalum | Human skin isolate MBRG 9.24 | 14 d at various concentrations | 4fold | 3.9 | No data | None reported | [36] |
| C. renale group | Human skin isolate MBRG 9.13 | 14 d at various concentrations | 4fold | 31.2 | No data | None reported | [36] |
| C. xerosis | WIBG 1.2 (wound isolate) | 40 d at various concentrations | None | 3.6 | Not applicable | None described | [41] |
| E. casseliflavus | 3 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 8fold – 20fold | 100 | Stable for 20 subcultures (1 strain) | Cross-adaptation* to benzalkoniumchloride (30fold - 100fold; 4 strains), triclosan (> 100fold; 1 strain) and didecyldimethylammonium bromide (4fold - 6fold; 2 strains); cross-resistance* to imipenem (3 strains), cefotaxime and tetracycline (1 strain each) | [43] |
| E. durans | Biocide-sensitive strain from organic foods | Several passages with gradually higher concentrations | 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (≥ 100fold), triclosan (10fold) and didecyldimethylammonium bromide (16fold); cross-resistance* to imipenem and ampicillin | [43] |
| E. faecalis | 1 strain of unknown origin | 14 passages at various concentrations | 2fold | 7.8 | Stable for 14 d | None reported | [37] |
| E. faecalis | Strain SS497 | 10 passages at various concentrations | 3.7fold | 11 | Significant increase of surface hydrophobicity | No data | [57] |
| E. faecalis | WIBG 1.1 (wound isolate) | 40 d at various concentrations | 6.7fold | 24.2 | Unstable for 14 d | None described | [41] |
| E. faecalis | Biocide-sensitive strain from organic foods | Several passages with gradually higher concentrations | 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (80fold) and didecyldimethylammonium bromide (8fold); cross-resistance* to imipenem and ceftazidime | [43] |
| E. faecium | 9 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 2fold – 16fold | 80 | Stable for 20 subcultures (1 strain) | Cross-adaptation* to benzalkoniumchloride (10fold - 100fold; 9 strains), triclosan (4fold - 100fold; 6 strains) and didecyldimethylammonium bromide (4fold - 8fold; 7 strains); cross-resistance* to imipenem (9 strains), tetracycline (4 strains), ampicillin (2 strains) cefotaxime and ceftazidime (1 strain each) | [43] |
| E. faecium | VRE strain 410 (skin and soft tissue infection isolate) | 21 d at various concentrations | 4fold | 19.6 | No data | Subpolulation with reduced susceptibility* to daptomycin including significant alterations in membrane phospholipids | [58] |
| E. faecium | 3 vanA VRE strains | 15 min at MIC | No data | No data | Not applicable | ≥ 10fold increase of vanHAX encoding VanA-type vancomycin resistance and of liaXYZ associated with reduced daptomycin susceptibility; vanA upregulation was not strain or species specific; VRE was more susceptible to vancomycin in the presence of subinhibitory chlorhexidine | [59] |
| E. saccharolyticus | Domestic drain biofilm isolate MBRG 9.16 | 14 d at various concentrations | None | 1.9 | Not applicable | None reported | [36] |
| Enterococcus spp. | 6 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 2fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (30fold - 100fold; 6 strains), triclosan (4fold - 15fold; 5 strains) and didecyldimethylammonium bromide (4fold - 6fold; 4 strains); cross-resistance* to imipenem (6 strains), ceftazidime and sulfamethoxazole (5 strains each), cefotaxime (4 strains), tetracycline (3 strains) and ampicillin (2 strains) | [43] |
| Eubacterium spp. | Domestic drain biofilm isolate MBRG 4.14 | 14 d at various concentrations | None | 31.2 | Not applicable | None reported | [36] |
| M. phyllosphaerae | Domestic drain biofilm isolate MBRG 4.30 | 14 d at various concentrations | None | 15.6 | Not applicable | None reported | [36] |
| M. luteus | MRBG 9.25 (skin isolate) | 40 d at various concentrations | None | 3.6 | Not applicable | None described | [41] |
| S. aureus | ATCC 6538 | 40 d at various concentrations | None | 3.6 | Not applicable | None described | [41] |
| S. aureus | ATCC 6538 | 100 d at various concentrations | None | 0.6 | Not applicable | None described | [60] |
| S. aureus | NCTC 6571 plus 2 MRSA strains | Several passages with gradually higher concentrations | 1.3fold – 2fold | 1 | “unstable” | None described | [61] |
| S. aureus | NCIMB 9518 | 0.00005% for 30 s, 5 min and 24 h | 2fold – 5fold | 20 | Stable for 10 d | No increase of MBC | [45] |
| S. aureus | ATCC 6538 | 7 d of sublethal exposure | 2.5fold | 2.5 | Unstable for 10 d | None reported | [52] |
| S. aureus | 3 clinical MRSA strains | 10 passages at various concentrations | ≤ 4fold | 8 | No data | No change of PHMB susceptibility** | [62] |
| S. aureus | ATCC 6538 | 14 passages at various concentrations | 4fold | 7.8 | Unstable for 14 d | None reported | [37] |
| S. aureus | ATCC 25923 and 14 clinical isolates | 14 d at various sublethal concentrations | 4fold - 6fold (6 isolates) | 6.3 | No data | Increased tolerance* to ciprofloxacin (4fold - 64fold; 10 isolates), tetracycline (4fold - 512fold; all isolates), gentamicin (4fold - 512fold; 8 isolates), amikacin (16fold - 512fold; 11 isolates), cefepime (8fold - 64fold; 11 isolates) and meropeneme (8fold - 64fold; 9 isolates) | [63] |
| S. aureus | NCTC 4163 | 12 w at various concentrations | 16fold | No data | No data | None described | [46] |
| S. aureus | Strain SAU3 carrying plasmid pWG613 | 10 min at 0.00005% | No data | No data | Not applicable | No significant reduction of plasmid transfer frequency | [64] |
| S. capitis | MRBG 9.34 (skin isolate) | 40 d at various concentrations | 1.7fold | 6 | Stable for 14 d | None described | [41] |
| S. capitis | Human skin isolate MBRG 9.34 | 14 d at various concentrations | None | 7.8 | Not applicable | None reported | [36] |
| S. caprae | MRBG 9.3 (skin isolate) | 40 d at various concentrations | None | 3.6 | Not applicable | None described | [41] |
| S. caprae | Human skin isolate MBRG 9.30 | 14 d at various concentrations | None | 7.8 | No data | None reported | [36] |
| S. cohnii | Human skin isolate MBRG 9.31 | 14 d at various concentrations | None | 3.9 | Not applicable | None reported | [36] |
| S. epidermidis | MRBG 9.33 (skin isolate) | 40 d at various concentrations | None | 9.7 | Not applicable | None described | [41] |
| S. epidermidis | Human skin isolate M 9.33 | 14 d at various concentrations | None | 7.8 | Not applicable | None reported | [36] |
| S. epidermidis | CIP53124 | 1 d at various concentrations | No data | No data | Not applicable | Significant increase of biofilm formation at various sublethal concentrations | [65] |
| S. haemolyticus | Human skin isolate MBRG 9.35 | 14 d at various concentrations | None | 15.6 | Not applicable | None reported | [36] |
| S. haemolyticus | MRBG9.35 (skin isolate) | 40 d at various concentrations | 2.1fold | 3 | Unstable for 14 d | None described | [41] |
| S. hominis | Human skin isolate MBRG 9.37 | 14 d at various concentrations | None | 7.8 | Not applicable | None reported | [36] |
| S. kloosii | Human skin isolate MBRG 9.37 | 14 d at various concentrations | None | 7.8 | Not applicable | None reported | [36] |
| S. lugdunensis | Human skin isolate MBRG 9.36 | 14 d at various concentrations | None | 15.6 | Not applicable | None reported | [36] |
| S. lugdunensis | MRBG 9.36 (skin isolate) | 40 d at various concentrations | 4fold | 3.6 | Stable for 14 d | None described | [41] |
| S. saprophyticus | Human skin isolate MBRG 9.29 | 14 d at various concentrations | None | 3.9 | Not applicable | None reported | [36] |
| S. saprophyticus | 4 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 2fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (25fold - 100fold; 4 strains), triclosan (4fold - 8fold; 3 strains) and didecyldimethylammonium bromide (6fold - 12fold; 2 strains); cross-resistance* to ceftazidime (4 strains), imipenem, sulfamethoxazole and cefotaxime (2 strains each) and tetracycline (1 strain) | [43] |
| S. warneri | MRBG 9.27 (skin isolate) | 40 d at various concentrations | None | 29 | Not applicable | None described | [41] |
| S. warneri | Human skin isolate MBRG 9.27 | 14 d at various concentrations | 2fold | 15.6 | No data | None reported | [36] |
| S. xylosus | Biocide-sensitive strain from organic foods | Several passages with gradually higher concentrations | 4fold | 20 | Unstable | Cross-adaptation* to benzalkoniumchloride (> 100fold), triclosan (8fold) and didecyldimethylammonium bromide (20fold); cross-resistance* to ceftazidime, imipenem, sulfamethoxazole, cefotaxime and tetracycline | [43] |
| Staphylococcus spp. | 3 biocide-sensitive strains from organic foods | Several passages with gradually higher concentrations | 4fold – 10fold | 50 | Unstable | Cross-adaptation* to benzalkoniumchloride (4fold - 10fold; 3 strains), triclosan (8fold - 100fold; 3 strains) and didecyldimethylammonium bromide (6fold - 20fold; 3 strains); cross-resistance* to ceftazidime (1 strain) | [43] |
| S. mutans | Strain UA159 | 10 passages at various concentrations | None | 3 | Not applicable | None reported | [57] |
broth microdilution;
macrodilution method
Cross tolerance to various antibiotics such as tetracycline, gentamicin or meropeneme could be found in some isolates of S. aureus. In E. faecium (vancomycin-resistant enterococcus; VRE) a more than 10fold vanA up-regulation was detected as well as reduced daptomycin susceptibility. An increase in biofilm formation was described in S. epidermidis.
DISCUSSION
The strongest adaptation to low level CHG exposure was found in common nosocomial pathogens such as E. coli (up to 500fold MIC increase), S. marcescens (up to 128fold MIC increase), P. aeruginosa (up to 32fold MIC increase) and K. pneumoniae (up to 16fold MIC increase). After sublethal exposure the highest MIC values were also found in common nosocomial pathogens such as S. marcescens (2,048 mg/l), P. aeruginosa (1,024 mg/l), K. pneumoniae (> 512 mg/l) and E. coli (500 mg/l), It is probably no coincidence that these pathogens are among those species considered to have extreme or even pan resistance to antibiotics [13].
Low level CHG exposure also reduced the susceptibility to selected antibiotics in Burkholderia spp. or Salmonella spp. In Burkholderia spp. an up-regulation of transporter and efflux pump genes was found. Efflux pumps are often not agent-specific and may well result in resistance to other biocidal agents or antibiotics [1]. A quite alarming finding was that horizontal gene transfer was induced in E. coli by low level CHG exposure enabling the faster spread of resistance genes within the bacterial community.
Some mechanisms of the adaptive response have been described. Increased expression of efflux pumps is recognized as a mechanism of antibiotic and biocide resistance. The pumps may have limited or broad substrates, the so-called multiple drug resistance pumps [14]. The multiple antibiotic resistance (mar) locus and mar regulon in E. coli and other members of the enterobacteriaceae is a paradigm for a generalized response locus leading to increased expression of efflux pumps. One such pump, the AcrAB pump, extrudes biocides such as triclosan, chlorhexidine and quaternary ammonium compounds as well as multiple antibiotics [14]. In P. aeruginosa, a number of multidrug efflux pumps export a broad range of substrates [14]. In C. jejuni and C. coli active efflux was identified in adapted strains. In addition, the outer membrane protein profiles had changed, along with morphological changes [15]. In K. pneumoniae CHG adaptation was associated with mutations in the two-component regulator phoPQ and a putative Tet repressor gene (smvR) adjacent to the major facilitator superfamily (MFS) efflux pump gene, smvA [16]. And in Salmonella spp. a defense network was described that involved multiple cell targets including those associated with the synthesis and modification of the cell wall, the SOS response, virulence, and a shift in cellular metabolism toward anoxic pathways. In addition, results indicated that CHG tolerance was associated with more extensive modifications of the same cellular processes involved in this proposed network, as well as a divergent defense response involving the up-regulation of additional targets such as the flagellar apparatus and an altered cellular phosphate metabolism [17].
A major limitation of this review is that most of the data were obtained in laboratories under defined conditions. The findings are certainly suitable to describe the potential for adaptation to CHG. But it is less clear if or how the findings are transferred to the clinic. In 2002 Block et al. described that the MIC for CHG was higher among clinical isolates when more CHG was used for any type of application [18]. A similar correlation between CHG usage and MIC values was described in 2018 with S. aureus [19]. Lindford et al. described an outbreak by MDR A. baumannii in a burn unit. One of the measures to finally control the outbreak was to reduce moist low-concentration CHG dressings on burn wounds [20]. And yet the clinical impact of an elevated MIC value remains under controversial debate [21]. In hand hygiene it is known that a low bactericidal effect of CHG on the skin can only be achieved in the presence of small volumes of water, the water released by the skin as transepidermal water loss does not seem to be sufficient [22]. If the water realised by the skin is sufficient to allow adaptive changes of the bacterial species on the skin is currently not know. And yet, the triclosan tale strongly suggested that “a chemical that constantly stresses bacteria to adapt, and behaviour that promotes antibiotic resistance needs to be stopped immediately when the benefits are null” [10]. CHG is obviously such a chemical that constantly stresses bacteria to adapt. Even if the clinical impact of isolates or strains with elevated MIC values cannot finally be evaluated at the moment it seems justified restricting the use of CHG to applications where health benefits are associated with its use.
IMPLICATIONS FOR HAND HYGIENE
Alcohol-based hand rubs
In alcohol-based hand rubs with additional CHG used for hygienic hand disinfection there is no sound evidence for an additional effect of CHG in vitro [23]. There is also no evidence on the prevention of any type of healthcare-associated infection by the additional CHG in hand rubs. But there are obvious risks such as acquired bacterial resistance, anaphylactic reactions or skin irritation [24]. Its use in the immediate patient environment may therefore contribute to the selection pressure especially when the CHG concentration is sublethal [20]. Additional biocidal agents in alcohol-based hand rubs such as CHG are not recommended by the WHO [7].
The same applies to hand rubs used for surgical hand disinfection [24]. For surgical hand disinfection additional biocidal agents such as CHG are not recommended because they do not contribute to the prevention of surgical site infections [3, 25]. Replacing hand rubs with additional CHG by hand rubs without CHG will help to reduce avoidable CHG selection pressure. They should, however, have an equivalent efficacy, dermal tolerance and user acceptability [26].
Antimicrobial soaps
Another simple option to reduce CHG selection pressure is to ban CHG soaps in healthcare for regular hand washing. Based on the WHO recommendation for hand hygiene from 2009 hand washing is recommended to wash hands when they are visibly soiled. The use of plain soap, however, is adequate, there is no health benefit for antimicrobial soaps [7].
Another possible use of antimicrobial soaps is prior to surgery. Surgical scrubbing usually lasts for 6–10 min of scrubbing time and consumes between 5 and 20 l water per scrub [27–29]. Surgical scrub products may only be effective with additional post-scrub water-based CHG treatments of the hands which pose an additional contamination and selection pressure risk [30, 31]. Alcohol-based hand rubs with an appropriate concentration of alcohol(s) have a stronger effect on the resident hand flora, require typically 1.5 min for application, cause less skin irritation [32] and do not pose any selection pressure to bacterial species due to their volatility [33, 34].
CONCLUSION
Overall, the evidence on the adaptive potential of various pathogens to low level CHG exposure strongly suggests to critically review the use of CHG in patient care and to eliminate it in all applications where no health benefit has been shown or is realistically expectable.
METHODS
A systematic literature search was conducted via the National Library of Medicine (PubMed) and via ScienceDirect (only research articles) on 10th March 2018 and up-dated on 25th June 2018 using the term chlorhexidine in combination with low level exposure (17 hits PubMed, 5 hits ScienceDirect), adaptive response (6/24), sublethal (27/72), resistance and MIC (142/640), and resistant and MIC (116/648). In addition, studies deemed suitable for this review were also included. Publications were included and results were extracted from them when they provided original data on any type of adaptive response to the exposure of bacteria to sublethal concentrations of CHG, corresponding changes of MICs (CHG, antibiotics, and other biocidal agents), survival in CHG solutions, efflux pump activity, gene expression or biofilm formation. Articles were excluded when they described only data on fungi, outbreaks, pseudo-outbreaks or infections caused by contaminated CHG products or solutions, only biochemical changes, an adaptive effect with other chlorhexidine salts or when a CHG solution or product was used for disinfection during an outbreak but without being the suspected or proven source. Reviews were also excluded and screened for any original information within the scope of the review.
The susceptibility of isolates or strains to CHG is described as the minimum inhibitory concentration (MIC value). In most studies it was described as a single value and is presented as such unless stated otherwise. The magnitude of any adaptive response to CHG is expressed as an MIC change and assigned to one of the following three categories: no adaptive response (no MIC increase), weak adaptive response (MIC increase ≤ 4fold) and strong adaptive response (MIC increase > 4fold).
SUPPLEMENTAL MATERIAL
All supplemental data for this article are available online at http://www.microbialcell.com/researcharticles/2019a-kampf-microbial-cell/.
Abbreviations:
- BAC
– benzalkonium chloride,
- CHG
– chlorhexidine digluconate,
- MIC
– minimal inhibitory concentration,
- PHMB
– polyhexanide.
REFERENCES
- 1.Kampf G. Acquired resistance to chlorhexidine – is it time to establish an “antiseptic stewardship” initiative? J Hosp Infect. 2016;94(3):213–227. doi: 10.1016/j.jhin.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 2.O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad, Randolph AG, Rupp ME, Saint S. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2011;39(4 Suppl 1):S1–34. doi: 10.1016/j.ajic.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, Abbas M, Atema JJ, Gans S, van Rijen M, Boermeester MA, Egger M, Kluytmans J, Pittet D, Solomkin JS. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276–e287. doi: 10.1016/s1473-3099(16)30398-x. [DOI] [PubMed] [Google Scholar]
- 4.Allegranzi B, Egger M, Pittet D, Bischoff P, Nthumba P, Solomkin J. WHO's recommendation for surgical skin antisepsis is premature - Authors' reply. Lancet Infect Dis. 2017;17(10):1024–1025. doi: 10.1016/s1473-3099(17)30526-1. [DOI] [PubMed] [Google Scholar]
- 5.Maiwald M, Widmer AF. WHO's recommendation for surgical skin antisepsis is premature. Lancet Infect Dis. 2017;17(10):1023–1024. doi: 10.1016/s1473-3099(17)30448-6.. [DOI] [PubMed] [Google Scholar]
- 6.Maiwald M, Chan ES. The forgotten role of alcohol: a systematic review and meta-analysis of the clinical efficacy and perceived role of chlorhexidine in skin antisepsis. PLoS One. 2012;7(9):e44277. doi: 10.1371/journal.pone.0044277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. First Global Patient Safety Challenge Clean Care is Safer Care. WHO; Geneva: 2009. WHO guidelines on hand hygiene in health care. [PubMed] [Google Scholar]
- 8.Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. 'My five moments for hand hygiene': a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9–21. doi: 10.1016/j.jhin.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Halden RU, Lindeman AE, Aiello AE, Andrews D, Arnold WA, Fair P, Fuoco RE, Geer LA, Johnson PI, Lohmann R, McNeill K, Sacks VP, Schettler T, Weber R, Zoeller RT, Blum A. The Florence Statement on Triclosan and Triclocarban. Environmental Health Perspectives. 2017;125(6):064501. doi: 10.1289/ehp1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNamara PJ, Levy SB. Triclosan: an Instructive Tale. Antimicrob Agents Chemother. 2016;60(12):7015–7016. doi: 10.1128/aac.02105-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampf G. Springer International Publishing; Cham: 2018. Antiseptic Stewardship: Biocide Resistance and Clinical Implications. [Google Scholar]
- 12.Morrissey I, Oggioni MR, Knight D, Curiao T, Coque T, Kalkanci A, Martinez JL. Evaluation of epidemiological cut-off values indicates that biocide resistant subpopulations are uncommon in natural isolates of clinically-relevant microorganisms. PLoS One. 2014;9(1):e86669. doi: 10.1371/journal.pone.0086669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh TR, Toleman MA. The emergence of pan-resistant Gram-negative pathogens merits a rapid global political response. Journal of Antimicrobial Chemotherapy. 2012;67(1):1–3. doi: 10.1093/jac/dkr378. [DOI] [PubMed] [Google Scholar]
- 14.Levy SB. Active efflux, a common mechanism for biocide and antibiotic resistance. J Appl Microbiol. 2002;92(Suppl):65s–71s. doi: 10.1046/j.1365-2672.92.5s1.4.x. [DOI] [PubMed] [Google Scholar]
- 15.Mavri A, Smole Mozina S. Development of antimicrobial resistance in Campylobacter jejuni and Campylobacter coli adapted to biocides. International Journal of Food Microbiology. 2013;160(3):304–312. doi: 10.1016/j.ijfoodmicro.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Wand ME, Bock LJ, Bonney LC, Sutton JM. Mechanisms of Increased Resistance to Chlorhexidine and Cross-Resistance to Colistin following Exposure of Klebsiella pneumoniae Clinical Isolates to Chlorhexidine. Antimicrob Agents Chemother. 2017;61(1) doi: 10.1128/aac.01162-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Condell O, Power KA, Handler K, Finn S, Sheridan A, Sergeant K, Renaut J, Burgess CM, Hinton JC, Nally JE, Fanning S. Comparative analysis of Salmonella susceptibility and tolerance to the biocide chlorhexidine identifies a complex cellular defense network. Frontiers in Microbiology. 2014;5(373) doi: 10.3389/fmicb.2014.00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Block C, Furman M. Association between intensity of chlorhexidine use and microorganisms of reduced susceptibility in a hospital environment. J Hosp Infect. 2002;51(3):201–206. doi: 10.1053/jhin.2002.1246. [DOI] [PubMed] [Google Scholar]
- 19.Hardy K, Sunnucks K, Gil H, Shabir S, Trampari E, Hawkey P, Webber M. Increased Usage of Antiseptics Is Associated with Reduced Susceptibility in Clinical Isolates of Staphylococcus aureus. mBio. 2018;9(3) doi: 10.1128/mBio.00894-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindford A, Kiuru V, Anttila VJ, Vuola J. Successful Eradication of Multidrug Resistant Acinetobacter in the Helsinki Burn Centre. Journal of Burn Care & Research : official publication of the American Burn Association. 2015;36(6):595–601. doi: 10.1097/bcr.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 21.Cookson BD, Bolton MC, Platt JH. Chlorhexidine resistance in methicillin-resistant Staphylococcus aureus or just an elevated MIC? An in vitro and in vivo assessment. Antimicrob Agents Chemother. 1991;35(10):1997–2002. doi: 10.1128/aac.35.10.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutter JD, Angiulo K, Macinga DR. Measuring residual activity of topical antimicrobials: is the residual activity of chlorhexidine an artefact of laboratory methods? J Hosp Infect. 2014;88(2):113–115. doi: 10.1016/j.jhin.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Kampf G. What is left to justify the use of chlorhexidine in hand hygiene? J Hosp Infect. 2008;70(Suppl. 1):27–34. doi: 10.1016/S0195-6701(08)60008-0. [DOI] [PubMed] [Google Scholar]
- 24.Kampf G, Kramer A, Suchomel M. Lack of sustained efficacy for alcohol-based surgical hand rubs containing “residual active ingredients” according to EN 12791. Journal of Hospital Infection. 2017;95(2):163–168. doi: 10.1016/j.jhin.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 25.WHO. WHO; Geneva: 2016. Global guidelines for the prevention of surgical site infections. [PubMed] [Google Scholar]
- 26.Kampf G. Antiseptic Stewardship for Alcohol-Based Hand Rubs. In: Kampf G, editor. Antiseptic Stewardship: Biocide Resistance and Clinical Implications. Springer International Publishing; Cham: 2018. pp. 643–650. [Google Scholar]
- 27.Ahmed A. Surgical hand scrub: lots of water wasted. Annals of African Medicine. 2007;6(1):31–33. doi: 10.4103/1596-3519.55733. [DOI] [PubMed] [Google Scholar]
- 28.Petterwood J, Shridhar V. Water conservation in surgery: a comparison of two surgical scrub techniques demonstrating the amount of water saved using a 'taps on/taps off' technique. The Australian Journal of Rural Health. 2009;17(4):214–217. doi: 10.1111/j.1440-1584.2009.01074.x. [DOI] [PubMed] [Google Scholar]
- 29.Somner JEA, Stone N, Koukkoulli A, Scott KM, Field AR, Zygmunt J. Surgical scrubbing: can we clean up our carbon footprints by washing our hands? J Hosp Infect. 2008;70(3):212–215. doi: 10.1016/j.jhin.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Kampf G. Aqueous chlorhexidine for surgical hand disinfection? J Hosp Infect. 2018;98(4):378–379. doi: 10.1016/j.jhin.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 31.Herruzo R, Vizcaino MJ, Yela R. Surgical hand preparation with chlorhexidine soap or povidone iodine: new methods to increase immediate and residual effectiveness, and provide a safe alternative to alcohol solutions. J Hosp Infect. 2018;98(4):365–368. doi: 10.1016/j.jhin.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 32.Parienti JJ, Thibon P, Heller R, Le Roux Y, von Theobald P, Bensadoun H, Bouvet A, Lemarchand F, Le Coutour X. Hand-rubbing with an aqueous alcoholic solution vs traditional surgical hand-scrubbing and 30-day surgical site infection rates - a randomized equivalence study. JAMA. 2002;288(6):722–727. doi: 10.1001/jama.288.6.722. [DOI] [PubMed] [Google Scholar]
- 33.Widmer AF, Rotter M, Voss A, Nthumba P, Allegranzi B, Boyce J, Pittet D. Surgical hand preparation: state–of-the-art. J Hosp Infect. 2010;74(2):112–122. doi: 10.1016/j.jhin.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 34.Widmer AF. Surgical hand hygiene: scrub or rub? J Hosp Infect. 2013;83(suppl. 1):S35–S39. doi: 10.1016/S0195-6701(13)60008-0. [DOI] [PubMed] [Google Scholar]
- 35.Kampf G. Chlorhexidine Digluconate. In: Kampf G, editor. Antiseptic Stewardship: Biocide Resistance and Clinical Implications. Springer International Publishing; Cham: 2018. pp. 429–534. [Google Scholar]
- 36.Moore LE, Ledder RG, Gilbert P, McBain AJ. In vitro study of the effect of cationic biocides on bacterial population dynamics and susceptibility. Appl Environ Microbiol. 2008;74(15):4825–4834. doi: 10.1128/aem.00573-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cowley NL, Forbes S, Amezquita A, McClure P, Humphreys GJ, McBain AJ. Effects of Formulation on Microbicide Potency and Mitigation of the Development of Bacterial Insusceptibility. Appl Environ Microbiol. 2015;81(20):7330–7338. doi: 10.1128/aem.01985-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fuangthong M, Julotok M, Chintana W, Kuhn K, Rittiroongrad S, Vattanaviboon P, Mongkolsuk S. Exposure of Acinetobacter baylyi ADP1 to the biocide chlorhexidine leads to acquired resistance to the biocide itself and to oxidants. J Antimicrob Chemother. 2011;66(2):319–322. doi: 10.1093/jac/dkq435. [DOI] [PubMed] [Google Scholar]
- 39.Pumbwe L, Skilbeck CA, Wexler HM. Induction of multiple antibiotic resistance in Bacteroides fragilis by benzene and benzene-derived active compounds of commonly used analgesics, antiseptics and cleaning agents. J Antimicrob Chemother. 2007;60(6):1288–1297. doi: 10.1093/jac/dkm363. [DOI] [PubMed] [Google Scholar]
- 40.Ahn Y, Kim JM, Lee YJ, LiPuma J, Hussong D, Marasa B, Cerniglia C. Effects of Extended Storage of Chlorhexidine Gluconate and Benzalkonium Chloride Solutions on the Viability of Burkholderia cenocepacia. Journal of Microbiology and Biotechnology. 2017;27(12):2211–2220. doi: 10.4014/jmb.1706.06034. [DOI] [PubMed] [Google Scholar]
- 41.Forbes S, Dobson CB, Humphreys GJ, McBain AJ. Transient and sustained bacterial adaptation following repeated sublethal exposure to microbicides and a novel human antimicrobial peptide. Antimicrob Agents Chemother. 2014;58(10):5809–5817. doi: 10.1128/aac.03364-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knapp L, Rushton L, Stapleton H, Sass A, Stewart S, Amezquita A, McClure P, Mahenthiralingam E, Maillard JY. The effect of cationic microbicide exposure against Burkholderia cepacia complex (Bcc); the use of Burkholderia lata strain 383 as a model bacterium. J Appl Microbiol. 2013;115(5):1117–1126. doi: 10.1111/jam.12320. [DOI] [PubMed] [Google Scholar]
- 43.Gadea R, Glibota N, Perez Pulido R, Galvez A, Ortega E. Adaptation to Biocides Cetrimide and Chlorhexidine in Bacteria from Organic Foods: Association with Tolerance to Other Antimicrobials and Physical Stresses. Journal of Agricultural and Food Chemistry. 2017;65(8):1758–1770. doi: 10.1021/acs.jafc.6b04650. [DOI] [PubMed] [Google Scholar]
- 44.Thomas L, Maillard JY, Lambert RJ, Russell AD. Development of resistance to chlorhexidine diacetate in Pseudomonas aeruginosa and the effect of a “residual” concentration. J Hosp Infect. 2000;46(4):297–303. doi: 10.1053/jhin.2000.0851. [DOI] [PubMed] [Google Scholar]
- 45.Wesgate R, Grasha P, Maillard JY. Use of a predictive protocol to measure the antimicrobial resistance risks associated with biocidal product usage. Am J Infect Control. 2016;44(4):458–464. doi: 10.1016/j.ajic.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 46.Nicoletti G, Boghossian V, Gurevitch F, Borland R, Morgenroth P. The antimicrobial activity in vitro of chlorhexidine, a mixture of isothiazolinones ('Kathon' CG) and cetyl trimethyl ammonium bromide (CTAB). J Hosp Infect. 1993;23(2):87–111. doi: 10.1016/0195-6701(93)90014-q. [DOI] [PubMed] [Google Scholar]
- 47.Braoudaki M, Hilton AC. Adaptive resistance to biocides in Salmonella enterica and Escherichia coli O157 and cross-resistance to antimicrobial agents. J Clin Microbiol. 2004;42(1):73–78. doi: 10.1128/jcm.42.1.73-78.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jutkina J, Marathe NP, Flach CF, Larsson DGJ. Antibiotics and common antibacterial biocides stimulate horizontal transfer of resistance at low concentrations. The Science of the Total Environment. 2017;616-617:172–178. doi: 10.1016/j.scitotenv.2017.10.312. [DOI] [PubMed] [Google Scholar]
- 49.Bock LJ, Wand ME, Sutton JM. Varying activity of chlorhexidine-based disinfectants against Klebsiella pneumoniae clinical isolates and adapted strains. J Hosp Infect. 2016;93(1):42–48. doi: 10.1016/j.jhin.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 50.Kurihara T, Sugita M, Motai S, Kurashige S. [In vitro induction of chlorhexidine- and benzalkonium-resistance in clinically isolated Pseudomonas aeruginosa]. Kansenshogaku zasshi The Journal of the Japanese Association for Infectious Diseases. 1993;67(3):202–206. doi: 10.11150/kansenshogakuzasshi1970.67.202. [DOI] [PubMed] [Google Scholar]
- 51.Knapp L, Amezquita A, McClure P, Stewart S, Maillard JY. Development of a protocol for predicting bacterial resistance to microbicides. Appl Environ Microbiol. 2015;81(8):2652–2659. doi: 10.1128/aem.03843-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riazi S, Matthews KR. Failure of foodborne pathogens to develop resistance to sanitizers following repeated exposure to common sanitizers. Int Biodeter Biodegr. 2011;65(2):374–378. doi: 10.1016/j.ibiod.2010.12.001. [DOI] [Google Scholar]
- 53.Condell O, Iversen C, Cooney S, Power KA, Walsh C, Burgess C, Fanning S. Efficacy of biocides used in the modern food industry to control salmonella enterica, and links between biocide tolerance and resistance to clinically relevant antimicrobial compounds. Appl Environ Microbiol. 2012;78(9):3087–3097. doi: 10.1128/aem.07534-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gandhi PA, Sawant AD, Wilson LA, Ahearn DG. Adaption and growth of Serratia marcescens in contact lens disinfectant solutions containing chlorhexidine gluconate. Applied and Environmental Microbiology. 1993;59(1):183–188. doi: 10.1128/aem.59.1.183-188.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Prince HN, Nonemaker WS, Norgard RC, Prince DL. Drug resistance studies with topical antiseptics. Journal of Pharmaceutical Sciences. 1978;67(11):1629–1631. doi: 10.1002/jps.2600671134. [DOI] [PubMed] [Google Scholar]
- 56.Seier-Petersen MA, Jasni A, Aarestrup FM, Vigre H, Mullany P, Roberts AP, Agerso Y. Effect of subinhibitory concentrations of four commonly used biocides on the conjugative transfer of Tn916 in Bacillus subtilis. J Antimicrob Chemother. 2014;69(2):343–348. doi: 10.1093/jac/dkt370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kitagawa H, Izutani N, Kitagawa R, Maezono H, Yamaguchi M, Imazato S. Evolution of resistance to cationic biocides in Streptococcus mutans and Enterococcus faecalis. Journal of Dentistry. 2016;47:18–22. doi: 10.1016/j.jdent.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 58.Bhardwaj P, Hans A, Ruikar K, Guan Z, Palmer KL. Reduced Chlorhexidine and Daptomycin Susceptibility in Vancomycin-Resistant Enterococcus faecium after Serial Chlorhexidine Exposure. Antimicrob Agents Chemother. 2018;62(1) doi: 10.1128/aac.01235-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gadea R, Glibota N, Pérez Pulido R, Gálvez A, Ortega E. Effects of exposure to biocides on susceptibility to essential oils and chemical preservatives in bacteria from organic foods. Food Control. 2017;80(Supplement C):176–182. doi: 10.1016/j.foodcont.2017.05.002. [DOI] [Google Scholar]
- 60.Wiegand C, Abel M, Ruth P, Hipler UC. Analysis of the adaptation capacity of Staphylococcus aureus to commonly used antiseptics by microplate laser nephelometry. Skin Pharmacology and Physiology. 2012;25(6):288–297. doi: 10.1159/000341222. [DOI] [PubMed] [Google Scholar]
- 61.Suller MTE, Russell AD. Antibiotic and biocide resistance in methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococcus. J Hosp Infect. 1999;43(281-291) doi: 10.1016/s0195-6701(99)90424-3. [DOI] [PubMed] [Google Scholar]
- 62.Renzoni A, Von Dach E, Landelle C, Diene SM, Manzano C, Gonzales R, Abdelhady W, Randall CP, Bonetti EJ, Baud D, O'Neill AJ, Bayer A, Cherkaoui A, Schrenzel J, Harbarth S, Francois P. Impact of Exposure of Methicillin-Resistant Staphylococcus aureus to Polyhexanide In Vitro and In Vivo. Antimicrob Agents Chemother. 2017;61(10) doi: 10.1128/aac.00272-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu D, Lu R, Chen Y, Qiu J, Deng C, Tan Q. Study of cross-resistance mediated by antibiotics, chlorhexidine and Rhizoma coptidis in Staphylococcus aureus. Journal of Global Antimicrobial Resistance. 2016;7(61-66) doi: 10.1016/j.jgar.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 64.Pearce H, Messager S, Maillard JY. Effect of biocides commonly used in the hospital environment on the transfer of antibiotic-resistance genes in Staphylococcus aureus. J Hosp Infect. 1999;43(2):101–107. doi: 10.1053/jhin.1999.0250. [DOI] [PubMed] [Google Scholar]
- 65.Houari A, Di Martino P. Effect of chlorhexidine and benzalkonium chloride on bacterial biofilm formation. Lett Appl Microbiol. 2007;45(6):652–656. doi: 10.1111/j.1472-765X.2007.02249.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.