Abstract
Vascular complications in forms of venous and arterial thrombi are common scenario in antiphospholipid syndrome with raised titer of antibodies. Here we describe an 18 years old female who was admitted with right parotid swelling due to external carotid artery thrombi within gland parenchyma in antiphospholipid syndrome, with past history of right lower leg arterial occlusion and digital gangrene.
Introduction
Antiphospholipid antibody syndrome (APS) is an autoimmune disorder where vascular thrombosis, pregnancy morbidities and the antiphospholipid antibodies in plasma like lupus anticoagulant (LA), anticardiolipin antibodies and anti-β2 glycoprotein-I (β2GPI) antibodies are characteristic [1]. Venous thrombosis is the most common systemic manifestation of APS, but arterial thrombosis is not uncommon.
With this knowledge, here we want to cite a rare presentation of vascular manifestation of APS in a young female.
CASE REPORT
An 18-year-old female patient presented with pain in the right parotid region for the past 30 days prior to admission and swelling over the same side for the past 15 days. Pain was dull in nature and was gradually increasing along with the swelling, compelling the patient unable to open her mouth. Swelling persisted, it is not associated with food intake. There was mild fever in association, without any chill and rigor. There was no history of increased salivation, dryness of the mouth, throbbing sensation, facial deviation, loss of consciousness or weight loss.
During her 9th month of pregnancy, 2 months ago, she suffered from pain in the right lower limb and there was a blackish discoloration of the right little toe. Peripheral angiogram showed a cut in the right popliteal artery with collateral development and low flow down the vessel (Fig. 1). Thrombectomy was done to release the obstruction. No investigation was available for evaluation. Lower uterine cesarean section was done 15 days prior to onset of present symptoms, and that was uneventful. There was no history of previous pregnancy loss. Her family history and drug or diet history did not give any clue toward diagnosis.
Figure 1.

Peripheral angiogram showing the right popliteal artery occlusion and collaterals.
On examination, her pulse was 80 beats per minute, regular and well palpable except right sided arteria dorsalis pedis, and posterior tibial artery pulsations were feeble. The right arm blood pressure was 112/60 mm Hg, and the left arm blood pressure was 110/64 mm Hg. Ankle-Brachial Pressure Index was 0.6. A 4 × 5 cm hard tender swelling was felt at the angle of mandible, everting the ear lobule (Fig. 2). There was no pulsation or bruit over the swelling, no superficial ulceration or sinus, no facial palsy on the same side and no tonsillar deviation on oral examination. Pus didn’t come on compression over the swelling. Cervical lymph nodes were not palpable. Right lower limb was cold and tender at the feet and showed dry gangrene at the little toe (Fig. 3) and scar marks of previous thrombectomy. Other general and systemic examinations were unremarkable.
Figure 2.

Swelling in the right parotid region.
Figure 3.

Right little toe gangrene.
Her complete blood count, liver and renal function tests, serum electrolytes, coagulation profile, fasting lipid profile and routine urine were all within reference ranges, and ICTC status was negative. Right parotid ultrasound revealed pseudo aneurysm arising from terminal part of external carotid artery with multilayered thrombus within. Contrast computed tomography (CT) of face (Fig. 4) showed a hypo-dense area within right parotid gland, which was suggestive of pseudo aneurysm of external carotid artery, and that time also a repeat Doppler study was done for confirmation. Magnetic resonance imaging (MRI) with MR angiography (Fig. 5) of face revealed a well-defined, well-marginated oval shaped (16 × 17 × 18 mm) lesion in the parenchyma of right parotid gland, which was hyper-intense in both T1- and T2-weighted images with surrounding hypo-intense rim, and there is a suggestion of communication with the external carotid artery and its branches at the medial aspect. Ultrasound Doppler of the right lower limb artery showed diffuse luminal narrowing of below-knee arteries. Venous Doppler of right lower limb and ultrasound whole abdomen were not evident of any abnormality.
Figure 4.
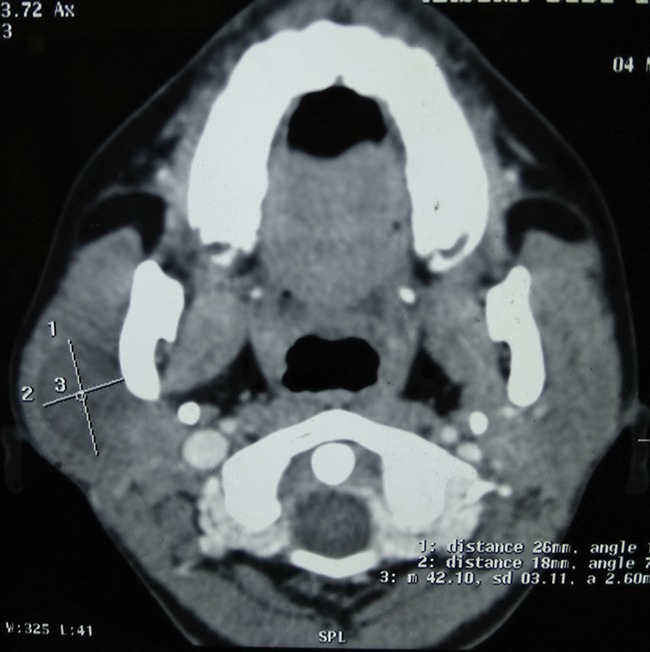
Contrast CT of the face showing a hypo-dense area in the right parotid region.
Figure 5.
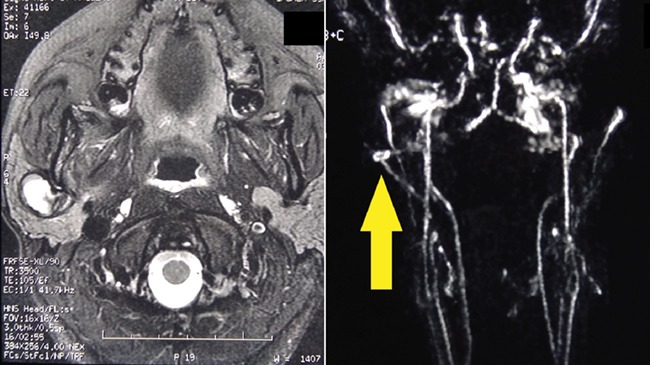
MRI and MRA of the face showing hyper-intense lesion in parotid gland and connection with right external carotid artery.
Her ANA was negative up to (1:160) dilution in Hep-20-10 indirect immunofluorescence; CRP, dsDNA and ANCA were negative; Anti β2 glycoprotein IgG was measured with ELISA in EUROIMMUN kit; the normal value was < 20 RU/ml, which came 73.2 RU/ml for the patient; and anti-cardiolipin IgM, IgG and LA were negative.
Diagnosis of primary antiphospholipid syndrome was considered according to Revised Sapporo classification criteria. Treatment was started with un-fractioned heparin and warfarin with monitoring of International Normalized Ratio (INR) with target between 2 and 3 (dose was adjusted accordingly). Later, heparin was omitted and treatment continued with warfarin only. After 12 weeks of initial investigation Anti β2 Glycoprotein was repeated with ELISA in EUROIMMUN kit and showed persistent high titer of IgG—22.4 RU/ml.
Discussion
The patient was diagnosed with primary antiphospholipid syndrome according to the Revised Sapporo classification criteria, where at least one clinical symptom and at least one positive laboratory test on two occasions in 12 weeks apart are required for diagnosis [2]. Here she had arterial thrombosis and persistently positive anti-β2 glycoprotein. As per international consensus statement 2006, anti-β2 glycoprotein assay is newly added in the criteria, and its positivity is classified as IIc APS [2].
Antiphospholipid syndrome presenting with unilateral parotid swelling due to external carotid artery thrombus was unique, and as we went through previous literature, involvements of internal carotid artery, even bilateral, were documented in association with APS. Alpert et al. [3] showed occlusion of extracranial part of internal carotid artery. Marques et al. [4] documented left internal carotid artery thrombus in a 48-year-old female who presented with stoke. But we did not find any such case of external carotid artery involvement within parenchyma of parotid, causing unilateral gland swelling. Mahale et al. [5] reported a case of right-sided internal carotid artery thrombus with right lower limb deep vein thrombosis in a 38-year-old female who had a history of 2nd trimester pregnancy loss and was later diagnosed as APS, and Anand et al. [6] cited a 39-year-old female patient with stroke due to bilateral involvement of the same in relation with APS. Etiologies of parotid swelling can be divided as infectious, non-infectious, benign and malignant. Now, infectious causes were unlikely in the question of unilaterality and other examination findings and laboratory reports. Malignant growth without facial nerve involvement is not common [7]. Thus, these two possibilities were kept down the list. Surgeons opined for a fine needle aspiration biopsy to ascertain the etiology, but the initial ultrasound report defied that. The dilemma was arisen regarding the cause, as the ultrasound finding and clinical look were contradictory. Also, in the CT scan, there was no contrast uptake within the lesion and that was going against the source of the swelling from a vessel. Radiological help in higher orders had been sought for a firm diagnosis. Lastly, MRI and MRA showed lesion within the parenchyma of right parotid gland and communication with ipsilateral external carotid artery, suggestive of a thrombosed aneurysm or pseudoaneurysm. No contrast uptake in CT scan can be explained by the blockage of the feeding vessel with thrombus.
After 6 months of follow-up, swelling and pain of the parotid region and right lower limb are both resolved as target INR was reached with warfarin.
Therefore, a proper evaluation of a parotid swelling should be done as it may be from its content instead of the gland parenchyma, especially when suggestion of vascular complication is present in APS. Unawareness may cost invasive hazards.
ACKNOWLEDGEMENTS
We are thankful to Dr Parasar Ghosh, Professor, Department of Rheumatology, Institute of Post Graduate Medical Education and Research, S.S.K.M. Hospital, Kolkata, and Dr Samiran Samanta, Department of Radiodiagnosis, Institute of Post Graduate Medical Education and Research, S.S.K.M. Hospital, Kolkata, West Bengal, India, for their immense help.
Conflict Of interest statement
None declared.
Funding
None.
Ethical Approval
Not required for this case.
Consent
Proper informed consent taken from the patient.
Guarantor
Rajdeep Basu (corresponding author) and Omkarr De Hazra (second author).
References
- 1. Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. J Autoimmun 2014;48–49:20–5doi: 10.1016/j.jaut.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 2. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 2006;4:295–306. [DOI] [PubMed] [Google Scholar]
- 3. Alpert JN, White M, Perusquia E. Lupus anticoagulant associated with extracranial internal carotid artery occlusion. Stroke 1990;21:1759–60. [PubMed] [Google Scholar]
- 4. Marques MA, Murad FF, Ristow AV, et al. Acute carotid occlusion and stroke due to antiphospholipid antibody syndrome: case report and literature review. Int Angiol 2010;29:380–4. [PubMed] [Google Scholar]
- 5. Mahale RR, Mehta A, Rangasetty S. Simultaneous occurrence of deep vein thrombosis and carotid artery thrombosis in antiphospholipid antibody syndrome. J Neurosci Rural Pract 2017;8:320–1doi:10.4103/0976-3147.203827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anand P, Mann SK, Fischbein NJ, Lansberg MG. Bilateral internal carotid artery occlusion associated with the antiphospholipid antibody syndrome. Case Rep Neurol 2014;6:50–4doi:10.1159/000360473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wierzbicka M, Kopeć T, Szyfter W, Kereiakes T, Bem G. The presence of facial nerve weakness on diagnosis of a parotid gland malignant process. Eur Arch Otorhinolaryngol 2011;269:1177–82. [DOI] [PMC free article] [PubMed] [Google Scholar]


