Abstract
Alcoholic liver disease (ALD) refers to the damages to the liver and its functions due to alcohol overconsumption. It consists of fatty liver/steatosis, alcoholic hepatitis, steatohepatitis, chronic hepatitis with liver fibrosis or cirrhosis, and hepatocellular carcinoma. However, the mechanisms behind the pathogenesis of alcoholic liver disease are extremely complicated due to the involvement of immune cells, adipose tissues, and genetic diversity. Clinically, the diagnosis of ALD is not yet well developed. Therefore, the number of patients in advanced stages has increased due to the failure of proper early detection and treatment. At present, abstinence and nutritional therapy remain the conventional therapeutic interventions for ALD. Moreover, the therapies which target the TNF receptor superfamily, hormones, antioxidant signals, and MicroRNAs are used as treatments for ALD. In particular, mesenchymal stem cells (MSCs) are gaining attention as a potential therapeutic target of ALD. Therefore, in this review, we have summarized the current understandings of the pathogenesis and diagnosis of ALD. Moreover, we also discuss the various existing treatment strategies while focusing on promising therapeutic approaches for ALD.
Keywords: ALD, pathogenesis, diagnose, phytochemical, MSCs
1. Introduction
Alcoholic liver disease (ALD) is the second most common cause of total human death every year [1]. According to previous studies, ALD includes alcoholic fatty liver, alcoholic hepatitis, steatohepatitis, liver fibrosis, cirrhosis, and liver cancer [2]. Long-term excessive drinking can cause oxidative stress in the liver through the accumulation of reactive oxygen species (ROS) produced from alcohol metabolism [3]. It causes liver inflammation through the toxicity of lipopolysaccharides (LPS) and acetaldehyde. Moreover, the burden to the liver can be increased by other symptoms, such as chronic viral hepatitis and nonalcoholic fatty liver [4,5]. Fat accumulation in the liver, an early stage of ALD, is the only stage of ALD which can be completely reversible through abstinence without any drug intervention. Therefore, the diagnosis of early stage ALD and treatment with correct strategies is pivotal to treat ALD successfully if irreversible liver damage has not yet occurred [6].
Even though ALD has a profound impact on public health, the research progress of this field stands at a relatively low level. Furthermore, the pathogenesis of the disease remains unclear. To date, alcohol abstinence and nutrient supplements are considered the conventional treatment strategies for ALD in the clinic [7]. Therefore, the current researchers have focused on more therapeutic strategies, such as improving patient survival and prognosis, prevention of ALD and early diagnosis and targeted therapies [7]. As a result, the accumulating evidence has shown that the effects of non-toxic compounds extracted from natural food and herbal plants prevent ALD [8]. Especially, it has also shown the potential application of mesenchymal stem cells (MSCs)-based therapies for ALD treatment [9,10].
In this review paper, we summarized the recent studies on pathogenesis, underlying mechanisms, and diagnosis of ALD. In addition, we also summarized the possible therapeutic strategies to treat or prevent ALD.
2. Pathogenesis of ALD
2.1. Alcohol Metabolism
Alcohol, a polar molecular substance, is soluble in both water and lipid. After being consumed, it is absorbed into the blood circulation through the gastrointestinal tract. Generally, more than 95% of absorbed alcohol is metabolized by the liver, and a small amount is directly excreted through the lungs, urine, and sweat [11].
As shown in previous studies, there are three main metabolic systems which participate in the oxidative metabolism of alcohol into acetaldehyde. First is the hepatocyte cytoplasmic alcohol dehydrogenase (ADH) system, which oxidizes ethanol into acetaldehyde using nicotinamide adenine dinucleotide (NAD+) as a co-factor. ADH1, amongst the other isoenzymes of ADH, plays a main role in ethanol metabolism in the liver. Acetaldehyde, which is produced by ADH, is further oxidized to acetate by acetaldehyde dehydrogenase (ALDH) [12,13].
The second main metabolic system of alcohol is cytochrome P450 2E1 (CYP2E1) enzymes that convert chemical molecules into polar metabolites prior to excretion. CYP2E1 is considered to be the main component of this system. Under normal physiological conditions, CYP2E1 catalyzes the oxidization of a small amount of ethanol, such as 10%, into acetaldehyde. However, it is increased in chronic alcohol abuse conditions due to the induction of the expression of CYP2E1. The third metabolic system is the catalase endoplasmic reticulum (CAT) system, which is considered as the other main metabolic system that relies on NADPH for oxidative metabolism. This heme-containing catalase enzyme usually catalyzes the H2O2 removal but also is capable of catalyzing the oxidation of alcohol to acetaldehyde [14,15].
When the concentration of ethanol in blood and tissue fluid is low, it is mainly metabolized by the ADH pathway. However, when the concentration of ethanol is higher than 10 mol/L, the other two enzyme systems also begin to participate in ethanol metabolism [15].
2.2. The Spectrum of ALD
ALD comprises a broad spectrum of liver disorders ranging from simple alcoholic fatty liver/steatosis to severe lesion of liver injuries including steatohepatitis, fibrosis/cirrhosis, and hepatocellular carcinoma. These stages are classified based on the histology of the liver of patients [16]. Frequently, the pathologic processes are overlapped instead of being distinct disorder entities [17,18].
2.2.1. Alcoholic Fatty Liver (AFL)/Steatosis
Fatty liver, the earliest liver response to alcohol abuse, is generally able to revert completely by abstinence or maintained by the moderation in alcohol consumption. In this stage, fat vacuoles can be observed in liver tissue sections under the microscope [5]. According to previous studies, the over-consumption of alcohol increases the ratio of reduced nicotinamide adenine dinucleotide to oxidized nicotinamide adenine dinucleotide in hepatocytes. It results in AFL by disrupting the mitochondrial β-oxidation of fatty acids [5,19].
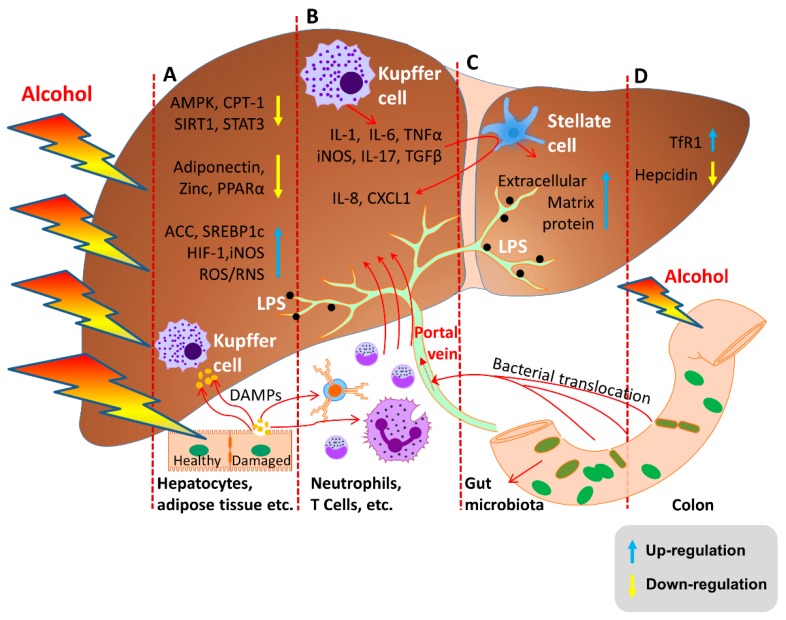
Moreover, recent studies have shown several underlying mechanisms which develop AFL through the direct or indirect regulation of lipid-metabolism associated factors. According to those studies, alcohol abuse increases sterol regulatory element-binding proteins c (SREBP-1c) expression and diminishes peroxisome proliferator-activated receptor alpha (PPAR-α) expression which leads the development of AFL via the induction of fatty acid synthesis and the inhibition of fatty acid β-oxidation. Furthermore, the consumption of alcohol subsequently induces Acetyl-CoA Carboxylase (ACC) activity and suppresses carnitine palmitoyltransferase I (CPT-1) activity via inhibiting AMP-activated protein kinase (AMPK) which develop AFL by increased fatty acid synthesis and reduced fatty acid β-oxidation. Furthermore, alcohol modulates many factors, such as the hypoxia-inducible Factor 1 (HIF-1) and inducible nitric oxide synthase (iNOS), which contribute to AFL development [5,15,20,21,22] (Figure 1).
Figure 1.
Molecular mechanisms of ALD. (A) Alcohol and its metabolites cause AFL by increasing ROS/RNS levels and the expression of ACC and SREBP1c. Additionally, via the reduced expression of AMPK-SIRT1, adiponectin, and zinc which activate PPARα. (B,C) Excessive alcohol consumption-enhanced permeability of the colon allows LPS to enter into the liver through the portal vein. The activated Kupffer cells release cytokines such as IL-1, IL-17, TGF-β, iNOS, and TNF-α which activates stellate cells and release IL-8 and CXCL1 in AH and ASH. Activated stellate cells also release the extracellular matrix which results in liver fibrosis. (D) Regulation of hepcidin, one of the main pathogenic factors in ALD.
After AFL develops, and if the person does not get treatment, fibrosis and cirrhosis may develop, followed by eventual liver failure [5].
2.2.2. Alcoholic Hepatitis (AH)
AH, a clinical syndrome of liver function decompensation, develops in patients with an ALD related background [23]. AH is not directly related to an alcohol dose. Therefore, only 10 to 35% of heavy drinkers develop AH. AH is associated with poor liver function and ductular formation. Furthermore, in previous studies, induced levels of LPS and impaired hepatocyte proliferation have been shown to be characteristics of AH [24,25] (Figure 1).
2.2.3. Alcoholic Steatohepatitis (ASH)
ASH is characterized by the hepatic injuries associated with steatosis. Most commonly, the hepatocyte ballooning can be identified as the frequent cellular injury of the ASH [26,27]. Studies have shown that alcohol and obesity can promote the development of steatohepatitis. The inflammatory environment produced in alcoholic liver subsequently leads to polymorph nuclear leukocyte infiltration, ROS formation, and hepatocyte damage. Finally, the damaged proteins are degraded by proteasome pathways which increase endoplasmic reticulum (ER) stress, alter autophagy, and promote hepatocyte injury. It also induces the development of hepatic inclusions that aggregate cytokeratin, which is known as the Mallory–Denk body [4,28].
When sterile inflammation (SI) occurs, damage-associated molecular patterns (DAMPs) can be released from damaged tissues. It can activate receptors on immune cells to promote the development of liver fibrosis and cancer [29] (Figure 1).
2.2.4. Alcoholic Liver Fibrosis/Cirrhosis
Heavy alcohol consumption is associated with the fibrosis progression in other types of liver diseases. The acetaldehyde produced by the oxidation of ethanol has a high toxicity and high activity which can destroy the microtubule structure of hepatocyte, causing microtubule dysfunction and further affecting the transportation of nutrients. Moreover, the formation of acetaldehyde-protein adducts further leads the protease inactivation of hepatocytes, abnormalities in DNA repair, damages in hepatocyte mitochondrial structure, oxygen utilization disorders, stimulation of collagen synthesis, and the accumulation of extracellular matrix proteins to form liver fibrosis and cirrhosis (Figure 1). Activation of the hepatic stellate cell (HSC) is the key step in the pathogenesis of alcoholic liver fibrosis (Figure 1). Dependent on these understandings; bone marrow cells (BMC), hematopoietic stem cells (HSC), and mesenchymal stem cells (MSC) have been used recently to develop cirrhosis treatment [30,31].
2.3. Molecular Mechanisms of ALD
During the last decade, significant effort has been made to understand the underlying molecular mechanisms of ALD which contribute to its pathogenesis [32]. According to previous studies, those mechanisms include direct hepatotoxicity, alcohol and its metabolites induced ROS production, the activation of innate immunity, and the production of pro-inflammatory cytokines [32,33,34].
2.3.1. Alcohol and Its Metabolites Damage the Liver
As a primary metabolite of alcohol, acetaldehyde has obvious toxic effects on liver by damaging the mitochondria and microtubules of hepatocytes. Generally, CYP2E1 is up-regulated in chronic alcohol abuse conditions and leads to converting more alcohol to acetaldehyde [35]. Acetaldehyde causes the dysfunction of mitochondrial fatty acid β-oxidation and hepatocyte secretion. Furthermore, it directly activates the transcription of SREBP-1c to promote the synthesis of fatty acids which results in fatty acid accumulation in hepatocytes [5] (Figure 1).
In chronic alcohol consumption, CYP2E1 enzyme is absolutely responsible for the excessive production of ROS, considered the second messenger in the cell. These produced ROS, such as hydrogen peroxide and superoxide ions, are associated with the pro-inflammatory profile of alcohol-mediated liver damages via recruiting immune cells and inducing pro-inflammatory cytokines circulation [35,36]. Moreover, in fatty liver disease, ROS-induced oxidative stress can inhibit the expression of energy metabolism signaling pathway-related proteins such as AMPK, Sirtuin 1 (SIRT1), and the transcription factor signal transducer and activator of transcription 3 (STAT3) [37] (Figure 1). It also down-regulates the levels of adiponectin and zinc that activates PPARα [5] (Figure 1), causing the peroxidation of hepatic membrane phospholipids, producing a large number of lipid free radicals, and promoting the expression of early growth response protein 1 (Egr-1), tumor necrosis factor alpha (TNF-α), adiponectin and acetyl-CoA carboxylase (ACC), which cause the accumulation of fat in liver [5].
2.3.2. Oxidative Stress and Lipid Peroxidation
In chronic alcohol abuse, alcohol increases the expression of CYP2E1 in liver, causing dysregulations in lipid peroxidation through ROS free radicals. Therefore, it leads to the dynamic imbalance of antioxidant systems which target the important antioxidant regulatory gene nuclear factor erythroid 2-related factor 2 (Nrf-2) in ALD [38]. It also damages other antioxidant genes which have important roles in ROS scavenging, such as superoxide dismutase (SOD), glutathione (GSH), catalase, peroxidase-1, metallothionein, and heme oxygenase (HO-1) [39,40]. Studies have shown that peroxiredoxin-1 and CYP2E1 located in the cytoplasmic side of the ER membrane can directly remove the ROS produced by the metabolism of alcohol. However, the expression of these antioxidant proteins is regulated by Nrf-2 or Thioredoxin (Trx) [41]. Therefore, the removal of ROS is dysregulated by damaged Nrf-2.
2.3.3. Endotoxin Enteric Leakage
Research has shown that chronic drinking can cause the imbalance of intestinal flora and intestinal toxin accumulation. Alcohol exposure causes the excessive proliferation of gram negative bacteria in the intestine. This growth results in the accumulation of endotoxin. Other than this, the metabolism of alcohol by gram negative bacteria and intestinal epithelial cells results in acetaldehyde accumulation, which increases the phosphorylation of tyrosine in tight and adherent junctions. It increases the permeability of the intestine to endotoxins, which in turn transfers these to the liver and this results in inflammatory changes in the liver and other organs [42].
Moreover, studies have also found that alcohol and metabolites stimulate the intestinal tract to produce a large number of nuclear transcription factors NF-κB and inducible nitric oxide synthase (iNOS), which increase the intercellular permeability by reacting with tubulin and activating intracellular non-specific protease C. This leads to cytoskeletal phosphorylation, the damage of the microtubule cytoskeleton, and cell conformational changes. It results in the disruption of intestinal barrier functions [42,43]. At the same time, toll-like receptor (TLR) mediates the synthesis and release of cytokines and induces the massive release of inflammatory factors, impairing antiviral infection and systemic immune regulation function. This induces the occurrence of “leak” in ALD patients which facilitates the entrance of endotoxin into the blood circulation [44] (Figure 1). Blood endotoxin can activate Kupffer and inflammatory cells, which inhibit macrophage phagocytosis and stimulate the proliferation of hepatic stellate cells (HSC) by releasing cytokines such as TNF-α, interleukin IL-1, IL-17, CXC chemokines, osteopontin, and inflammatory factors and free radicals [5] (Figure 1). IL-17 can also promote the recruitment of neutrophils by stimulating the production of IL-8 and (chemokine (C-X-C motif) ligand 1) CXCL1 by hepatic stellate cells (HSC) (Figure 1). These activated Kupffer cells and neutrophils release fibrosis-related factors, such as the transforming growth factor beta (TGF-β) and the platelet-derived growth factor [45].
2.3.4. Hepcidin Regulation
The research demonstrates that the iron deposition in liver is associated with ALD and more than 30% of patients with ALD suffer from iron metabolism disorders [46]. Recent studies have shown that even mild alcohol consumption induces the iron stores in the liver [46,47]. Therefore, it is common to observe iron overload in ALD patients. This is mediated by regulatory mechanisms and one of those underlying mechanisms is the alcohol-mediated down-regulation of hepcidin synthesis in liver [46] (Figure 1). Hepcidin plays a key role in iron homeostasis [48,49]. It is considered as the key regulator of iron circulation in mammals [50]. Alcohol down-regulates the expression of hepcidin by directly acting on it rather than regulating the status of the iron in cells [51].
Generally, the overload of iron increases the hepcidin synthesis in the liver as a response to the body’s iron level [48]. However, alcohol exposure down-regulates the expression of hepcidin in the liver despite an iron overload [51]. Therefore, a study has demonstrated that alcohol makes the synthesis of hepcidin insensitive to iron levels in the body [52]. Thus, alcohol has been reported to compromise the molecular mechanisms which protect the body from the damages by iron overload [52].
It is also well-known that iron and alcohol, individually, are capable of inducing oxidative stress and lipid peroxidation [53]. Therefore, both alcohol and alcohol-induced iron enhance the production of free radicals and pro-inflammatory cytokines [54,55]. Moreover, oxidative stress increases the level of transferrin receptor 1 (TfR1) which then promotes the intestinal iron absorption and body iron indices (Figure 1). Altogether, the increased iron absorption and deposition aggravates liver damage [46,56].
2.4. Apoptotic Signaling Pathway and Autophagy in ALD
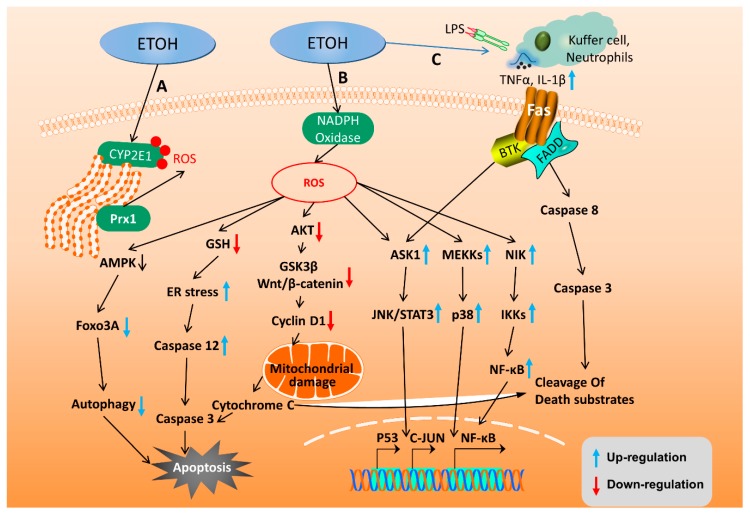
The apoptosis and autophagy of hepatocytes are pathological conditions that accompany ALD. Alcoholic liver toxicity and alcohol metabolism induce oxidative stress and inflammatory reactions which then cause hepatocyte apoptosis and accelerate the progression of liver diseases. Apoptosis induced by mitochondrial damages and ER stress caused by oxidative stress during ALD have been extensively studied. Accumulated ROS due to alcohol metabolism plays an important role in this mitochondria-dependent apoptosis. ROS accumulates in hepatocytes and inhibits the phosphorylation of alpha serine/threonine-protein kinase (AKT) [57], thereby down-regulating cycle G1 protein cyclin D1 through the inhibition of glycogen synthase kinase 3 beta (GSK3β)/Wnt/β-catenin signaling pathway activation in hepatocytes [58]. It causes the cell cycle arrest and activates mitochondria-dependent apoptosis. ROS can also directly activate apoptosis signal-regulating kinase 1 (ASK1) [59], nuclear factor kappa-light-chain-enhancer of activated B (NF-κB), and c-Jun N-terminal kinases (JNK)/P38 to induce mitochondrial-dependent apoptosis [60] (Figure 2).
Figure 2.
Molecular mechanisms of alcohol-induced apoptosis and autophagy in hepatocytes. (A,B) Intracellular ROS is produced through the alcohol metabolism via CYP2E1 and NADPH oxidase. These induced ROS level cause hepatocyte apoptosis through AMPK, GSH, AKT, JNK/STAT3, and NF-κB pathways. (C) Alcohol consumption activates Kupffer cells to release TNF-α AND IL-1β, which then activates the Fas ligand-dependent caspase pathway to induce hepatocyte apoptosis.
Moreover, the alcohol metabolism in the gut and liver change the microorganisms in the gut and induce the production of LPS, which in turn increases the inflammatory responses, causing liver inflammation and dysfunctions in lipid metabolism [61]. On the other hand, both ROS and LPS induce the production of TNF-α [62], promote the expression of pro-inflammatory factors IL-1β [7], induce apoptosis by ER stress, induce caspase cascade by activation of JNK/STAT3 and P53 [63], and cause Fas ligand-dependent apoptosis by recruit neutrophils [57] (Figure 2).
Autophagy is the self-destruction of apoptotic cells which degrades the damaged proteins and organelles by lysosomes [64]. Numerous studies have shown that autophagy has inhibitory effects on steatosis, inflammatory response, and hepatocyte apoptosis during ALD [65,66,67,68]. Moreover, research haa shown that various pathways, such as AMPK-Forkhead box O3 (FOXO3A) axis, sorting nexin 10 (SNX10)/chaperone, ALDH2, cannabinoid receptor 2 can induce autophagy to prevent alcoholic liver damage [61,69,70,71,72] (Figure 2).
2.5. Genetic Factors of ALD
According to previous reports, more than 95% of chronic alcoholics suffer from alcoholic fatty liver disease. However, only approximately 30% of patients develop severe stages and the potential protective mechanisms behind this are still unclear [73]. Previous studies have concluded that the consumption of different amounts of alcohol in various populations or the different expression levels of ALDH and CYP2E1 enzymes between individuals may result in this variation in disease progression. Recent case-control studies in the United States have shown that the single nucleotide rs738409 polymorphism in the Patatin-like phospholipase domain-containing protein 3 (PNPLA3) gene is closely related to the incidence of alcoholic liver [74]. Additionally, it was reported that single-nucleotide rs738409 polymorphisms are strongly associated with ALD in Han Chinese males [75]. In patients with advanced liver disease, PNPLA3 I148M variant primarily contributs to increase the risk of ALD development into HCC. It also causes a poor prognosis for liver transplantation [76]. Therefore, I148M may act as a genetic indicator for evaluating whether a patient is eligible for liver transplantation.
3. Early Diagnosis of ALD
3.1. Clinical Symptoms
Early manifestations of ALD in are fatty liver and mild hepatitis. The diagnosis of ALD requires the faithful reflection of patients on their history of chronic drinking to avoid difficulties in diagnosis. The presence of alcoholic liver can generally be judged according to common symptoms, such as fatigue, loss of appetite, bloating, nausea, vomiting, and obesity [77]. Clinically, the most common method to diagnose ALD is the liver function test. It takes the advantage of a 5 to 8 times higher aminotransferase level in blood samples of ALD patients compared to that in a healthy person. Generally, the aspartate transaminase (AST)/alanine transaminase (ALT) ratio can be used to detect ALD, as 70 to 80% of patients have twice the ratio of AST/ALT compared to a healthy person [78].
Gamma-glutamyltranspeptidase (GGT) is another sensitive index to diagnose fatty liver in cases of excessive alcoholism, as it combines the content of triglyceride and cholesterol in serum. However, these indicators cannot specifically diagnose whether liver damage is caused by obesity or alcohol-induced liver damage. Alcoholic liver and non-alcoholic fatty liver also have similar pathology ranges, ranging from simple fatty liver to steatohepatitis and cirrhosis. Therefore, the B-ultrasound test is needed to confirm the presence of fatty liver and the status can be further confirmed by CT test [6,79].
3.2. Imaging Examination
B-ultrasound is a commonly used technique in clinical diagnostics. It can prescribe three cases of abdominal ultrasound manifestations. The satisfaction of two of those indicates the diffuse fatty liver. First, is the diffuse enhancement of near field echo of the liver called “bright liver”. Normally, the bright liver echo is stronger than the kidney. Second, the manifestation of gradual echo attenuation in the liver far field. The third is characterized by significantly enhanced near-field echo, an obviously attenuated far field echo, and the tubular structure of the liver. An ultrasound diagnosis of alcoholic liver usually diagnoses the condition of the disease, effectively judges the degree of the disease, and improves the condition in time. Other advantages, such as the simple operation, not causing trauma to the patient, and high safety make the B-ultrasound widely promoted [80].
Computed tomography (CT) is used to diagnose the conditions that reduce the diffuse liver density. Usually, the ratio of CT values of the liver to spleen is reduced with the diffuse liver density in patients. According to studies, the liver/spleen CT ratio is ≤1.0 but >0.7 in mild conditions, ≤0.7 but >0.5 in moderate level conditions, and ≤0.5 in severe conditions [18,77].
The imaging examination is also used to reflect the distribution of liver fat infiltration, roughly determine the degree of diffuse fatty liver, and indicate the presence or absence of cirrhosis. However, it cannot distinguish the simple fatty liver and steatohepatitis separately. Also, it is difficult to detect liver cell steatosis lower than 33% in its grading. It also has to consider that the diffuse liver echo enhancement and density reduction can be seen in other chronic liver diseases [81].
3.3. Detection of Specific Biomarkers
Carbohydrate-deficient transferrin (CDT) is a highly specific biomarker for the detection of chronic alcohol abuse. It is the most ideal marker for judging drinking conditions. Generally, the content of alcohol metabolites in the urine 4–5 days after the last alcohol abuse is determined by CDT [82]. Especially during severe AH, it is a fundamental tool to define the severity of the disease and to differentiate AH from decompensated cirrhosis [78]. Another study found that when liver fibrosis or fatty liver is present in patients with alcoholic liver disease, the combination of CDT and other biochemical indicators (such as GGT, AST/ALT ratio) can further improve the accuracy of FibroTest and SteatoTest which is recommended by World Health Organization (WHO) for testing patients with metabolic conditions or who consume excessive amounts of alcohol [83].
Mass spectrometry-based metabolomics analysis is a rapid, non-invasive urine test to identify early stage alcohol-induced liver disease. This permits risk stratification and the treatment of high-risk individuals, before ALD leads to irreversible liver damage and death [84].
4. Current Therapies
Mild liver damage caused by alcoholism can be eliminated by long-term abstinence, which is currently the main treatment for ALD. However, treatments for alcoholics depend on the degree of alcohol consumption [8]. On the basis of previous studies, we have highlighted those available therapies and promising approaches to treat ALD patients.
4.1. Nutritional Therapy
Alcoholic liver patients often suffer from malnutrition caused by protein damage, which induces bacterial infections. Therefore, it is recommended to supply nutritional support for patients with mild AH by providing high protein, low-fat diets, and balancing the levels of vitamin B, C, K, and folic acid [85]. This nutrient supplement upgrades the conditions of patients as observed in previous studies through short-term diagnosis, such as liver function analysis and histological analysis. Patients with acute alcohol intoxication or high hepatic encephalopathy should protect the respiratory tract, and patients with severe AH usually need a referral rehabilitation program. According to clinical studies, the daily protein intake of ALD patients should be 1.5 g/kg of body weight. Furthermore, it is necessary to supply vitamin B often to patients with ALD and malnutrition, due to the potential risk of Wernicke encephalopathy [5].
4.2. Alcohol Withdrawal Therapies
Special alcohol withdrawal drugs are used clinically as adjuvant treatment to treat alcoholics who are addicted to alcohol consumption and who actively drink alcohol. Patients with liver transplantation treatment plans need to obtain liver transplantation qualification through long-term alcohol withdrawal. Disulfiram is an irreversible alcohol dehydrogenase inhibitor that is often used to treat alcoholism. However, it is not advised to use Disulfiram for advanced ALD patients, due to its potentially severe hepatotoxicity [73]. Acamprosate, a medication used along with counseling to treat alcohol dependence, is effective in preventing recurrence, but may have potential liver toxicity [86]. Baclofen, a gamma-aminobutyric acid B receptor agonist, has been found to be effective in maintaining a withdrawal, even in patients with cirrhosis. Additionally, the opioid antagonist naltrexone has been shown to reduce relapse, although its efficacy is moderate [87].
4.3. Hormone Related Therapies
Corticosteroids have been used to improve the nutritional status of AH patients. The anti-thyroid drug propylthiouracil also has been evaluated for the treatment of acute AH. However, the analysis of six clinical trials has shown that propylthiouracil does not affect survival time and is associated with adverse reactions [73]. Since ALD is associated with elevated levels of oxidative stress, antioxidants such as vitamin E and silymarin have been investigated and evaluated for the treatment of AH patients in previous studies. Unfortunately, the survival time of patients did not increase [5]. However, another study, which evaluated the potential benefits of the combination of N-acetylcysteine and corticosteroids, showed an increase in patient survival [5].
Losartan is considered a treatment to prevent the development of hepatic fibrosis and progression and regression of fibrosis stage [88,89]. Prednisolone, a steroid medication, is used to inhibit the inflammation of hepatocytes [4]. Although initial trials with oxandrolone showed positive results, it was not confirmed with further studies and no benefit was shown in a meta-analysis [90].
4.4. Liver Transplantation
Liver transplantation is the main choice for patients with advanced-stages of ALD. Liver transplantation has a better prognosis for patients with severe alcoholic hepatitis, who are not sensitive to drug treatments [7]. A physiologically functioning liver can be provided to patients with ALD by liver transplantation. Even though it increases the survival and quality of patient’s life, it does not eliminate the underlying alcoholism. Therefore, it may have a potential for relapse [91,92,93].
4.5. Targeted Therapies
In this section, we highlight the potential early therapeutic targets and provided promising therapeutic targets in various stages of ALD.
4.5.1. TNF Receptor Superfamily Target Therapies
Several clinical studies have been conducted on the effects of reagents, such as pentoxifylline or S-adenosyl-L-methionine, on AH patients that block TNF-α.
Pentoxifylline, a phosphodiesterase inhibitor that blocks the transcription of TNF-α, has successfully reduced mortality in patients with severe AH, which results in the decreased development of hepatorenal syndrome. Pentoxifylline can be used to treat patients with severe AH who are unable to administer glucocorticoids but it is not effective in the rescue of patients who are not responding to corticosteroids [73].
S-adenosyl-L-methionine (SAMe) is a methyl donor that has been shown to have antioxidant activity and prevents ALD by maintaining the mitochondrial function and further down-regulating TNF-α. Early clinical studies have shown that the use of SAMe can significantly reduce mortality in ALD patients. However, in another randomized controlled trial, there was no evidence to support the efficiency of SAMe in ALD therapy. Therefore, the therapeutic activity of this compound on ALD is yet to be determined. In addition, the clinical efficacy of SAMe as a treatment for ALD should be further established in large-scale research with the help of well-designed trials [73,94].
4.5.2. Antioxidant Signal Targeting Therapies
Activation of antioxidant genes such as Nrf-2, [38] NF-κB, superoxide dismutase, [95,96] catalase, glutathione, peroxidase-1, metallothionein, and peroxiredoxin-1 [97,98] is the targeted treatment for ALD caused by oxidative stress. Furthermore, the drugs inhibit CYP2E1, reduce reactive oxygen species, promote PPARα and activate SIRT1, AMPK, [99] HO-1, [100] and other pathways that can be used for the treatment of ALD.
4.5.3. Targeting the Inhibition of Hepatocyte Apoptosis
The whole process of acute and chronic ALD is accompanied with apoptosis. Clinical trials have shown that various caspase inhibitors can alleviate liver damage and fibrotic or nonalcoholic steatohepatitis in chronic hepatitis C virus (HCV) infected patients. Therefore, its use was suggested for ALD. Moreover, therapeutic, reversible and specific caspase high activity inhibitors are ideal drugs to treat ALD, as side effects can be avoided by inhibiting other cysteines. Caspase cascade can be activated by pathways such as mitochondrial-dependent, FAS/Fas ligand (FASl)-dependent [101] and endoplasmic reticulum pathways.
Also, the activation of upstream anti-apoptotic signaling such as SIRT/FOXO1 [62], PI3K/AKT, Wnt/β-catenin/FOXO3A [58,71] and the inhibition of pro-apoptotic protein P53/P21can inhibit alcohol hepatocyte apoptosis and alleviate liver damage. Furthermore, the regulation of anti-inflammatory signaling IL-10, IL-15 and pro-inflammatory factor IL-6/STAT3 also inhibit hepatocyte apoptosis [102,103]. Studies have also shown that mitogen-activated protein kinase (MAPK) family signaling proteins are highly expressed in ALD [60,104,105], which may serve as a target for inhibiting apoptosis of alcoholic hepatocytes.
4.5.4. MicroRNAs Targeted Therapies
MicroRNAs are a variety of biologically-regulated trimmers that are expressed in various cell types of gut-liver. These MicroRNAs participate in oxidative stress, inflammatory responses, lipid metabolism, and the activation of HSCs by regulating the transcription of target proteins. In the pathogenic process of alcoholic liver, the expression levels of miR-155, miR-132, and miR-182, are significantly up-regulated. However, the microRNAs such as miR-148a, miR-203, and miR122 are downregulated. Therefore, as shown in Table 1, the downregulation or overexpression of specific microRNAs can be used as therapeutic targets for ALD. Moreover, studies have shown that melatonin and intestinal probiotics prevent alcoholic liver by regulating microRNAs [106,107].
Table 1.
Involvement of MicroRNAs in ALD.
| MicroRNAs | Target | Dysregulation | References |
|---|---|---|---|
| miR-203 | Lipin1 | Decreased | [108] |
| miR-122 | Lipid metabolism: HMGCoA, ApoE, MTTP, PGC1a, HIF1A; Fibrosis: P4HA1; Hepatocellular cancer: Igf1R, ADAM10, cyclin G1, KLF6 | Decreased/Increased | [109,110,111] |
| miR-30e | UCP, ATP | Decreased | [112] |
| miR-19b | miR-17-92 | Decreased | [113] |
| miR-497 | Btg2, Yy1 | Decreased | [114] |
| miR-148a | FOXO1, TXNIP | Decreased | [115] |
| miR-217 | SIRT1/Lipin1 | Increased | [116] |
| miR-214 | GSR, CYP450 OR | Increased | [117] |
| miR-132 | Neuroimmune microRNAs | Increased | [111,118] |
| miR-155 | FABP4, LXRα, ACC1, LDLR | Increased | [109,111,118,119] |
| miR-29a; Let-7f; miR-340 | ASH | Increased | [120] |
| miR-17-92 | Fibrosis | Increased | [113] |
| miR-200a | ZER2 | Increased | [121] |
| miR-34a | SIRT1 | Increased | [122] |
4.6. Specific Treatment Options for AH
AH belongs to the severe ALD, a pathological stage in which patients have obvious symptoms of liver injury. Unlike alcoholic fatty liver, it requires alcohol abstinence and adjuvant drugs in addition to nutritional support. Furthermore, hospitalization is needed to prevent bacterial infection in severe cases. Many types of drugs have been used currently to manage alcoholic hepatitis patients in the clinic. However, the poor effect of these drugs remains a major challenge to overcome. Researchers are generally focused on studying the pathogenesis and therapeutic targets of AH. In addition, many pharmaceutical companies also are interested in drug development for AH. Therefore, here, we simply sorted out several potential treatment targets of AH.
The pro-inflammatory factor IL-6 is expressed in high levels in patients with AH. Therefore, inhibiting IL-6 is considered a potential target for the treatment of AH. However, a study has shown that IL-6-deficient mice are susceptible to AFL [123]. IL-1 is a multipotent immune regulator in vivo and may drive multiple spontaneous inflammations [124]. IL-1β accelerates the effect on production of neutrophil-associated adhesion factor E-selectin in Gao–Binge animal model [125]. IL-1R antagonists and IL-1β inhibitors can alleviate inflammasomes-dependent ASH [124]. IL-22 is a member of IL-10 cytokine family that controls bacterial infection by activation of STAT3 [126,127]. IL-22 can be used to treat ALD patients because of its antioxidant, anti-apoptotic, and anti-steatogenic, antibacterial, and proliferative effects [126,128]. In addition, IL-22 may be a good therapeutic target that overcomes the promotion of corticosteroid-mediated infection as the IL-22 receptor is expressed only on epithelial cells such as hepatocytes.
The CXC chemokine family includes ELR+ or ELR-. The members of ELR+ CXC family usually attract neutrophils and infiltrate the liver of ALD patients [129]. In AH patients, the expressions of CXCL1, CXCL2, and Chemokine (C-C motif) ligand 20 (CCL20) are increased in the liver [130,131,132] and CXCR1-CXCR5 are considered as the main receptors [133,134]. Moreover, the higher expression levels of IL-8, CXCL5, Gro-γ, and CXCL6 are associated with a worse prognosis of ALD [129]. Therefore, the agents that target CXC chemokines may be developed as therapeutic agents for AH.
The regulation of intestinal flora and attenuation of the LPS-TLR4 signaling pathway are considered as effective treatment strategies of ALD [135,136,137]. Previous studies have reported that intestinal probiotics can promote the expression of alcohol metabolism genes in the intestine. Additionally, it is capable of reducing the expression of TNF-α and TLR4 [138,139], increasing the production of IL-10, and preventing the dysregulation of intestinal microbiota through the addition of probiotics, [140] such as Lactobacillus rhamnosus GG, Akkermansia muciniphila, [141] Lactobacillus fermentum [142]. The addition of probiotics also can improve the intestinal permeability by regulating miRNA production and promoting intestinal occludin protein expression [107]. Rifaximin, a non-absorbable antibiotic that alters the intestinal microbiota, is known to be effective in the treatment of hepatic encephalopathy in clinical [5,78]. Inhibition of TLR4 signaling attenuates alcohol-induced liver injury and provides a therapeutic target for the treatment of alcoholic liver. According to studies, it is useful for the treatment of ALD by modifying TLR4 inhibitor or inhibiting LPS-induced TNF-α production.
Osteopontin is an extracellular matrix protein which is significantly up-regulated in ALD patients [143]. It promotes the pathogenesis of ALD by activating HSC. Therefore, the expression level of osteopontin positively relates with the severity of disease [144]. Early studies have shown that blocking osteopontin is effective in improving ALD [145]. However, it also reduces the production of TNF-α by binding LPS in the early stage of ALD [145]. The loss of osteopontin promotes the infiltration of neutrophils in the liver [146] and also leads to the transfer of hematopoietic stem cells into the liver and induces ALD by increasing iron content in liver [147]. Therefore, the mechanism of differential expression of osteopontin needs further study.
Endogenous cannabinoids mediate lipid metabolism and inflammatory responses in the liver and participate in ALD through the cannabinoid receptor (CB) 1 and cannabinoid receptor (CB) 2 regulatory signaling pathways [148]. Research has shown that CB1-deficient mice are resistant to alcoholic liver [149], and the pro-inflammatory response caused by CB1 can be negatively regulated by CB2 [150]. Moreover, it has shown that CB1 antagonists and CB2 agonists can protect alcohol-induced liver injury through different pathways [151,152]. However, the usage of CB1 antagonists has been limited in the treatment of liver diseases due to its neuropsychiatric side effects. Therefore, peripherally restricted CB1 antagonists have been actively explored recently. The inhibition of the liver CB1 receptor transcriptional regulator and estrogen-related receptor, has been reported to control alcohol-induced liver damages [153]. It may provide therapeutic benefits for ALD patients synergistically with CB2 agonists [69,152].
4.7. Pluripotent Mesenchymal Stem Cells for the Treatment of Liver Fibrosis
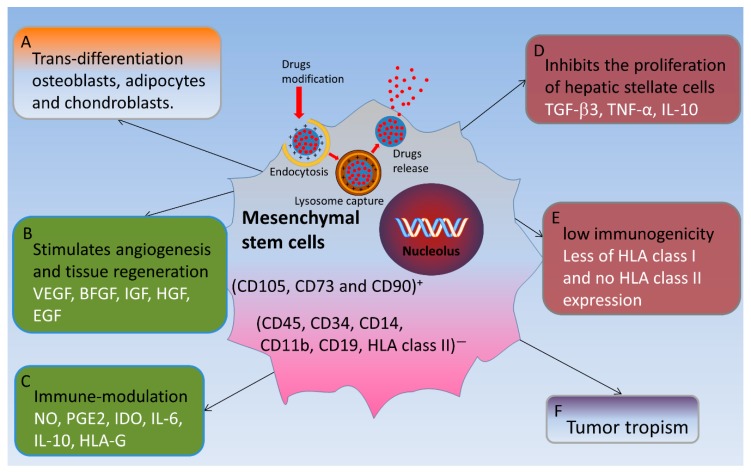
Liver fibrosis is the final stage of many chronic liver diseases. Once patients are diagnosed with alcoholic liver fibrosis/cirrhosis, alcohol withdrawal only can slow down the onset of the disease. According to previous studies, liver transplantation therapy remains the only treatment for alcoholic liver fibrosis. However, with the development of stem cell therapy research, the therapeutic potential of MSC, HSC, and BMC in liver regenerative medicine was compared. MSCs have low immunogenicity and tumor tropism in addition to properties such as cell proliferation, self-renewal, and self-differentiation. MSCs can inhibit the inflammatory response, reduce hepatocyte apoptosis, increase hepatocyte regeneration, reverse liver fibrosis, and enhance liver metabolism. Due to these characteristics, MSCs can alleviate the condition of liver fibrosis and cirrhosis. MSCs also carry and transform the chemotherapeutic drugs into the liver cancer site to release anti-cancer components and promote liver regeneration by escaping from immune surveillance system in the body [154]. Although MSC population is rare (<0.01% of monocytes present in the bone marrow), they can easily perform in vitro amplification. Therefore, MSCs are considered ideal candidates for cell therapy [9] (Figure 3).
Figure 3.
Possible interventions of mesenchymal stem cells in ALD. Interventions of MSCs consist of (A) trans-differentiation into parenchymal cells (B) induction of endogenous regeneration (C) modulation of inflammation and (D) decreased liver fibrosis via inhibiting the proliferation of hepatic stellate cells. (E,F) Specific characteristics of MSCs which facilitate the intervention of MSCs.
Few identification criteria have been reported for MSCs. First, it must be plastic-adhered when stored under standard culture conditions. Second, it must express CD105, CD73, and CD90, and be free from the expression of CD45, CD34, CD14, CD11b, CD19, and human leukocyte antigens surface molecules II. Third, it must have the ability of differentiation into osteoblasts, adipocytes, and chondroblasts under in vitro differentiation culture conditions [155,156] (Figure 3).
4.7.1. Functional with Low Immunogenicity and Inhibition of Inflammatory Responses
MSCs can be obtained from donors without serious complications, since MSCs express a small amount of Human leukocyte antigen (HLA) class I and do not express HLA class II molecules, which allows them to evade allogeneic immune response [157]. In addition, MSC transplantation has been tested, with promising results, in several clinical trials, and is a possible alternative approach for thetreatment of patients with liver diseases. MSCs can reduce collagen deposition in patients with alcoholic liver cirrhosis [158,159]. MSCs can directly inhibit the activity of CD8+ cytotoxic T lymphocytes by inhibiting their proliferation after antigen stimulation, and indirectly inhibit the activity of CD8+ cytotoxic T lymphocytes by increasing the relative proportion of CD4+T helper-2 (TH2) lymphocytes and CD4+ regulatory T lymphocytes. Since B lymphocyte activation is largely dependent on T cells, the effect of MSCs on T lymphocytes indirectly relates to the inhibition of B cell functions. In addition, MSCs also have a direct effect on B lymphocytes through cell-cell contact and the secretion of paracrine molecules [160] (Figure 2).
4.7.2. Tumor Tropism
The therapeutic potential of MSCs is also based on their inherent ability of being home to sites of inflammation after tissue injury. Damaged tissues release several molecules that interact with different receptors expressed by MSCs. It gives MSCs the ability to migrate through the endothelial cell layer and be attached and retained in ischemic tissue rather than in distal or intact tissues. Although the mechanisms driving this property are not fully understood, damaged tissues may express specific receptors or ligands that promote the transport, adhesion, and infiltration of MSCs to damaged sites, similar to white blood cells [161,162] (Figure 3).
4.7.3. Promotes the Proliferation and Regeneration of Hepatocytes
MSCs can differentiate into hepatocyte-like cells in vitro and in vivo and secrete a wide range of cytokines, including IL-10 which inhibits the apoptosis of hepatic parenchymal cells, vascular endothelial growth factor (VEGF), and basic fibroblast growth factor (BFGF), insulin-like growth factor (IGF), hepatocyte growth factor (HGF), epidermal growth factor (EGF), chemokines, transforming growth factor β3 (TGF-β3), and TNF-α [163,164]. These secretions inhibit the proliferation of hepatic stellate cells, reduce the inflammation and fibrosis of damaged tissues, improve impaired tissue, prevent parenchymal cell apoptosis, provide nutritive support for damaged tissues, and induce local precursor cell proliferation and differentiation by changing the microenvironment to stimulate angiogenesis and tissue regeneration [156]. In addition, MSCs can also express various soluble factors such as nitric oxide (NO), prostaglandin E2 (PGE2), indoleamine 2, 3-dioxygenase (IDO), IL-6, IL-10, and human leukocyte antigens G (HLA-G). These soluble factors regulate the proliferation and function of a variety of immune cells, and they have also been shown to induce regulatory T cells (Treg) [162,165] (Figure 3).
4.8. Research Studies on the Effects of Natural Plant Extractions for ALD
Treatment with natural plant extractions for ALD has gained attention, since an effective treatment for ALD is still limited. The low toxicity and easy absorption nature of herbal medicines and food extracts is advantageous in these treatments. In previous in vitro and in vivo studies, a variety of natural medicines and plant extracts have shown anti-oxidation and anti-inflammatory effects and the ability to regulate fat metabolism.
Researchers have found that food extracts such as garlic, betaine, anthocyanin, and resveratrol have protective effects on the alcoholic liver as shown in Table 2. Furthermore, they have found that herbal plant extracts have the effect of protecting the liver and clearing fat, as shown in Table 3. A large amount of active compounds were identified to prevent alcoholic liver from herbal plants such as Panax genus, salvia, Pueraria, astragalus, ginger, Silybum marianum, and licorice. Moreover, traditional Chinese medicine formula Zhi-Zi-Da-Huang, Qinggan Huoxue Recipe and Hugan Qingzhi tablet (HQT) have inhibitory effects on ALD and may be involved in multiple stages of ALD [166,167,168].
Table 2.
Active substances extracted from food to prevent alcoholic liver.
| Names | The Sources | Target | References |
|---|---|---|---|
| Resveratrol | Grapes, red wine, peanuts and berries. | HIF-1α, Oxidative stress | [169,170,171] |
| Diallyl trisulfide | Garlic | Nrf-2/HO-1, Steatosis | [172,173,174,175] |
| Anthocyanin | Purple potato, wild grape | Anti-inflammatory, Oxidative stress, Steatosis | [62,176,177,178,179] |
| Tomato powder | Tomato | CYP2E1 | [180] |
| Fisetin | Strawberry, apple, persimmon, lotus root, and onion | NOX4, Adiponectin, AMPK | [181] |
| Ginger-derived nanoparticles | Ginger | Nrf-2 | [182] |
| β-caryophyllene | Plant-derived food additive | Cannabinoid 2 receptors | [183] |
| lychee pulp phenolic | Lychee | Fatty acid β-oxidation, Hepatocyte apoptosis | [184] |
Table 3.
Active substances extracted from herbs for preventing alcoholic liver.
| Names | The Sources | Target | References |
|---|---|---|---|
| Ginsenosides | Ginseng | Steatosis, oxidative stress | [185,186,187] |
| Salvianolic acid | Salvia miltiorrhiza | SIRT1, P38, NF-κB | [188,189,190] |
| Puerarin | Pueraria lobata | PPARα, AMPK | [191,192,193] |
| Baicalin | Scutellaria baicalensis | Hedgehog Pathway, Oxidative stress, Inflammation | [194,195,196] |
| Curcumin | Curcuma longa | NF-κB, Nrf-2, Cytochrome c, Lipid peroxidation | [197,198,199] |
| Glycyrrhizic acid | Glycyrrhiza uralensis | Glutathione, TNF-α | [200,201,202] |
| Berberine | Coptis chinensis | PPARα, HNF4α | [203] |
| Ligustrazine | Ligusticum chuanxiong | Nrf-2, Hepatic steatosis | [204] |
| Honokiol and magnolol | Magnolia officinalis | AMPK/SREBP-1c, CB2 | [205,206] |
5. Conclusions and Future Directions
ALD is the leading cause of global advanced liver disease. Significant progress has been made in understanding the pathogenesis of animal models at the experimental level. Additionally, few therapeutic targets have been identified using transformation studies of human liver samples. However, the translation of basic research and translational research results into new therapies has been modest. Future efforts should be focused on identifying the main factors that contribute to the disease in patients with moderate and severe ALD to develop new therapies. For the terminal phase of ALD, the only effective treatment is liver transplantation [207]. However, it also still has several problems, including the lack of a donor source, immune rejection, and high surgical costs. However, the use of cell therapy is gaining attention, and mesenchymal stem cells (MSCs) appear to be promising cell types for the treatment of liver fibrosis. MSCs have a variety of differentiation capabilities allowing them to migrate directly into damaged tissues and differentiate into hepatocyte-like cells. In addition, MSCs release various growth factors and cytokines to increase hepatocyte regeneration, resolve liver fibrosis, and regulate inflammation and immune response [5].
Acknowledgments
Cooperative Research Program for Agriculture Science and Technology Development (PJ01316701) Rural Development Administration, Republic of Korea. NRF-2016R1A6A1A03012862.
Abbreviations
| ACC | Acetyl-CoA Carboxylase |
| ADH | Alcohol Dehydrogenase |
| AFL | Alcoholic Fatty Liver |
| AH | Alcoholic Hepatitis |
| AKT | Serine/threonine-protein kinase B |
| ALD | Alcoholic Liver Disease |
| ALDH | Acetaldehyde Dehydrogenase |
| ALT | Alanine Transaminase |
| AMPK | AMP-activated protein kinase |
| ApoE | Apolipoprotein E |
| ASK | Apoptosis Signal-regulating Kinase 1 |
| AST | Aspartate Transaminase |
| ATP | Adenosine Triphosphate |
| BFGF | Basic Fibroblast Growth Factor |
| BMC | Bone Marrow Cells |
| Btg2 | B-cell translocation gene 2 |
| CAT | Catalase Endoplasmic Reticulum |
| CB | Cannabinoid Receptor |
| CCL20 | Chemokine (C-C motif) Ligand 20 |
| CDT | Carbohydrate-Deficient Transferrin |
| CXCL | Chemokine (C-X-C motif) Ligand 1 |
| CYP2E1 | Cytochrome P450 2E1 |
| CYP450 OR | Cytochrome P450 oxidoreductase |
| DAMPs | Damage-Associated Molecular Patterns |
| EGF | Epidermal Growth Factor |
| Egr-1 | Early growth response protein 1 |
| ER | Endoplasmic Reticulum |
| FABP4 | Fatty Acid Binding Protein |
| FOXO3A | Forkhead box O3 |
| GGT | Gamma-Glutamyltranspeptidase |
| GSK3β | Glycogen Synthase Kinase 3 beta |
| GSR | Glutathione reductase |
| HCV | Hepatitis C Virus |
| HGF | Hepatocyte Growth Factor |
| HIF1α | Hypoxia-Inducible Factor 1-alpha |
| HLA | Human Leukocyte Antigen |
| HMGCoA | 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase |
| HO-1 | Heme Oxygenase |
| HSC | Hepatic Stellate Cell |
| IDO | Indoleamine 2,3-dioxygenase |
| IGF | Insulin-like Growth Factor |
| Igf1R | Insulin-like growth factor 1 receptor |
| IL | Interleukin |
| JNK | C-Jun N-terminal kinases |
| iNOS | Inducible nitric oxide synthase |
| KLF6 | Kruppel-Like Factor 6 |
| LDLR | Low-Density Lipoprotein Receptor |
| LPS | Lipopolysaccharides |
| LXRα | Liver X Receptor alpha |
| MAPK | Mitogen-Activated Protein Kinase |
| MSC | Mesenchymal Stem Cell |
| MTTP | Microsomal Triglyceride Transfer Protein |
| NAD | Nicotinamide Adenine Dinucleotide |
| NF-κB | Nuclear Factor kappa-light-chain-enhancer of activated B |
| Nrf-2 | Nuclear factor erythroid 2-related factor 2 |
| PGC1a | Peroxisome proliferator-activated receptor gamma coactivator 1-alpha |
| PGE2 | Prostaglandin E2 |
| PNPLA3 | Patatin like phospholipase domain containing protein 3 |
| PPARα | Peroxisome Proliferator-Activated Receptor alpha |
| P4HA1 | Prolyl 4-hydroxylase subunit alpha 1 |
| ROS | Reactive Oxygen Species |
| RNS | Reactive Nitrogen Species |
| SAMe | S-adenosyl-L-methionine |
| SIRT1 | Sirtuin 1 |
| SNX10 | Sorting Nexin 10 |
| STAT3 | Signal Transducer and Activator of Transcription 3 |
| TGF-β3 | Transforming Growth Factor beta 3 |
| TfR1 | Transferrin Receptor 1 |
| TLR4 | Toll-like Receptor 4 |
| TNF-α | Tumor Necrosis Factor alpha |
| Treg | Regulatory T cells |
| Trx | Thioredoxin |
| TXNIP | Thioredoxin Interacting Protein |
| UCP | Uncoupling Protein |
| VEGF | Vascular Endothelial Growth Factor |
| Yy1 | Yin Yang 1 |
| ZER2 | Zinc finger E-box binding homeobox 2 |
Author Contributions
Conceptualization, L.-Z.K., N.C., Y.-H.H., and T.K.; validation, T.K., D.K.J., and H.-N.S.; investigation, L.-Z.K., N.C., Y.-H.H., D.-H.L., J.-S.K., S.-U.K., T.-D.K., D.K.J., H.-N.S., and T.K.; writing—original draft preparation, L.-Z.K., N.C., Y.-H.H., and T.K.; writing—review and editing, T.K., D.K.J., and H.-N.S.; supervision, T.K., D.S.L., H.-N.S.; funding acquisition, T.K. and J.-S.K.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2017R1D1A1B03028188), KRIBB-OGM5201922, and KGM4251913 and by the grants from the KRIBB Research Initiative Program (KGM5161914).
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- 1.Poznyak V., Rekve D. Management of Substance Abuse Team, Global Status Report on Alcohol and Health 2018. World Health Organization; Geneva, Switzerland: 2018. [Google Scholar]
- 2.Dunn W., Shah V.H. Pathogenesis of Alcoholic Liver Disease. Clin. Liver Dis. 2016;20:445–456. doi: 10.1016/j.cld.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galicia-Moreno M., Gutierrez-Reyes G. The role of oxidative stress in the development of alcoholic liver disease. Rev. Gastroenterol. Mex. 2014;79:135–144. doi: 10.1016/j.rgmxen.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Altamirano J., Bataller R. Alcoholic liver disease: Pathogenesis and new targets for therapy. Nat. Rev. Gastroenterol. Hepatol. 2011;8:491–501. doi: 10.1038/nrgastro.2011.134. [DOI] [PubMed] [Google Scholar]
- 5.Gao B., Bataller R. Alcoholic liver disease: Pathogenesis and new therapeutic targets. Gastroenterology. 2011;141:1572–1585. doi: 10.1053/j.gastro.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abenavoli L., Masarone M., Federico A., Rosato V., Dallio M., Loguercio C., Persico M. Alcoholic Hepatitis: Pathogenesis, Diagnosis and Treatment. Rev. Recent Clin. Trials. 2016;11:159–166. doi: 10.2174/1574887111666160724183409. [DOI] [PubMed] [Google Scholar]
- 7.Orman E.S., Odena G., Bataller R. Alcoholic liver disease: Pathogenesis, management, and novel targets for therapy. J. Gastroenterol. Hepatol. 2013;28(Suppl. S1):77–84. doi: 10.1111/jgh.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim M.S., Ong M., Qu X. Optimal management for alcoholic liver disease: Conventional medications, natural therapy or combination? World J. Gastroenterol. 2016;22:8–23. doi: 10.3748/wjg.v22.i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ezquer F., Bruna F., Calligaris S., Conget P., Ezquer M. Multipotent mesenchymal stromal cells: A promising strategy to manage alcoholic liver disease. World J. Gastroenterol. 2016;22:24–36. doi: 10.3748/wjg.v22.i1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suk K.T., Yoon J.H., Kim M.Y., Kim C.W., Kim J.K., Park H., Hwang S.G., Kim D.J., Lee B.S., Lee S.H., et al. Transplantation with autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: Phase 2 trial. Hepatology. 2016;64:2185–2197. doi: 10.1002/hep.28693. [DOI] [PubMed] [Google Scholar]
- 11.Marshall W.J., Bangert S.K. Clinical biochemistry: Metabolic and clinical aspects. Churchill Livingstone; Edinburgh, NY, USA: 1995. [Google Scholar]
- 12.Eriksson C.J., Fukunaga T., Sarkola T., Chen W.J., Chen C.C., Ju J.M., Cheng A.T., Yamamoto H., Kohlenberg-Muller K., Kimura M., et al. Functional relevance of human adh polymorphism. Alcohol. Clin. Exp. Res. 2001;25(Suppl. S5):157S–163S. doi: 10.1111/j.1530-0277.2001.tb02391.x. [DOI] [PubMed] [Google Scholar]
- 13.Bosron W.F., Ehrig T., Li T.K. Genetic factors in alcohol metabolism and alcoholism. Semin. Liver Dis. 1993;13:126–135. doi: 10.1055/s-2007-1007344. [DOI] [PubMed] [Google Scholar]
- 14.Cederbaum A.I. Alcohol metabolism. Clin. Liver Dis. 2012;16:667–685. doi: 10.1016/j.cld.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ceni E., Mello T., Galli A. Pathogenesis of alcoholic liver disease: Role of oxidative metabolism. World J. Gastroenterol. 2014;20:17756–17772. doi: 10.3748/wjg.v20.i47.17756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teschke R. Alcoholic steatohepatitis (ASH) and alcoholic hepatitis (AH): Cascade of events, clinical aspects, and pharmacotherapy options. Expert Opin. Pharm. 2018;19:779–793. doi: 10.1080/14656566.2018.1465929. [DOI] [PubMed] [Google Scholar]
- 17.Chacko K.R., Reinus J. Spectrum of Alcoholic Liver Disease. Clin. Liver Dis. 2016;20:419–427. doi: 10.1016/j.cld.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Torruellas C., French S.W., Medici V. Diagnosis of alcoholic liver disease. World J. Gastroenterol. 2014;20:11684–11699. doi: 10.3748/wjg.v20.i33.11684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baraona E., Lieber C.S. Effects of ethanol on lipid metabolism. J. Lipid Res. 1979;20:289–315. [PubMed] [Google Scholar]
- 20.You M., Matsumoto M., Pacold C.M., Cho W.K., Crabb D.W. The role of AMP-activated protein kinase in the action of ethanol in the liver. Gastroenterology. 2004;127:1798–1808. doi: 10.1053/j.gastro.2004.09.049. [DOI] [PubMed] [Google Scholar]
- 21.You M., Fischer M., Deeg M.A., Crabb D.W. Ethanol induces fatty acid synthesis pathways by activation of sterol regulatory element-binding protein (SREBP) J. Biol. Chem. 2002;277:29342–29347. doi: 10.1074/jbc.M202411200. [DOI] [PubMed] [Google Scholar]
- 22.Galli A., Pinaire J., Fischer M., Dorris R., Crabb D.W. The transcriptional and DNA binding activity of peroxisome proliferator-activated receptor alpha is inhibited by ethanol metabolism. A novel mechanism for the development of ethanol-induced fatty liver. J. Biol. Chem. 2001;276:68–75. doi: 10.1074/jbc.M008791200. [DOI] [PubMed] [Google Scholar]
- 23.Aday A.W., Mitchell M.C., Casey L.C. Alcoholic hepatitis: Current trends in management. Curr. Opin. Gastroenterol. 2017;33:142–148. doi: 10.1097/MOG.0000000000000359. [DOI] [PubMed] [Google Scholar]
- 24.Odena G., Chen J., Lozano J.J., Altamirano J., Rodrigo-Torres D., Affo S., Morales-Ibanez O., Matsushita H., Zou J., Dumitru R., et al. LPS-TLR4 Pathway Mediates Ductular Cell Expansion in Alcoholic Hepatitis. Sci. Rep. 2016;6:35610. doi: 10.1038/srep35610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sancho-Bru P., Altamirano J., Rodrigo-Torres D., Coll M., Millan C., Jose Lozano J., Miquel R., Arroyo V., Caballeria J., Gines P., et al. Liver progenitor cell markers correlate with liver damage and predict short-term mortality in patients with alcoholic hepatitis. Hepatology. 2012;55:1931–1941. doi: 10.1002/hep.25614. [DOI] [PubMed] [Google Scholar]
- 26.Sakhuja P. Pathology of alcoholic liver disease, can it be differentiated from nonalcoholic steatohepatitis? World J. Gastroenterol. 2014;20:16474–16479. doi: 10.3748/wjg.v20.i44.16474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Celli R., Zhang X. Pathology of Alcoholic Liver Disease. J. Clin. Transl. Hepatol. 2014;2:103–109. doi: 10.14218/JCTH.2014.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mandrekar P., Bataller R., Tsukamoto H., Gao B. Alcoholic hepatitis: Translational approaches to develop targeted therapies. Hepatology. 2016;64:1343–1355. doi: 10.1002/hep.28530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mihm S. Danger-Associated Molecular Patterns (DAMPs): Molecular Triggers for Sterile Inflammation in the Liver. Int. J. Mol. Sci. 2018;19:3104. doi: 10.3390/ijms19103104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dumortier J., Dharancy S., Cannesson A., Lassailly G., Rolland B., Pruvot F.R., Boillot O., Faure S., Guillaud O., Rigole-Donnadieu H., et al. Recurrent alcoholic cirrhosis in severe alcoholic relapse after liver transplantation: A frequent and serious complication. Am. J. Gastroenterol. 2015;110:1160–1166. doi: 10.1038/ajg.2015.204. [DOI] [PubMed] [Google Scholar]
- 31.Gudowska M., Wojtowicz E., Cylwik B., Gruszewska E., Chrostek L. The Distribution of Liver Steatosis, Fibrosis, Steatohepatitis and Inflammation Activity in Alcoholics According to FibroMax Test. Adv. Clin. Exp. Med. 2015;24:823–827. doi: 10.17219/acem/28485. [DOI] [PubMed] [Google Scholar]
- 32.Miller A.M., Horiguchi N., Jeong W.I., Radaeva S., Gao B. Molecular mechanisms of alcoholic liver disease: Innate immunity and cytokines. Alcohol. Clin. Exp. Res. 2011;35:787–793. doi: 10.1111/j.1530-0277.2010.01399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breitkopf K., Nagy L.E., Beier J.I., Mueller S., Weng H., Dooley S. Current experimental perspectives on the clinical progression of alcoholic liver disease. Alcohol. Clin Exp Res. 2009;33:1647–1655. doi: 10.1111/j.1530-0277.2009.01015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rao R. Endotoxemia and gut barrier dysfunction in alcoholic liver disease. Hepatology. 2009;50:638–644. doi: 10.1002/hep.23009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seth D., Haber P.S., Syn W.K., Diehl A.M., Day C.P. Pathogenesis of alcohol-induced liver disease: Classical concepts and recent advances. J. Gastroenterol. Hepatol. 2011;26:1089–1105. doi: 10.1111/j.1440-1746.2011.06756.x. [DOI] [PubMed] [Google Scholar]
- 36.Parola M., Robino G. Oxidative stress-related molecules and liver fibrosis. J. Hepatol. 2001;35:297–306. doi: 10.1016/S0168-8278(01)00142-8. [DOI] [PubMed] [Google Scholar]
- 37.Seitz H.K., Bataller R., Cortez-Pinto H., Gao B., Gual A., Lackner C., Mathurin P., Mueller S., Szabo G., Tsukamoto H. Alcoholic liver disease. Nat. Rev. Dis. Primers. 2018;4:16. doi: 10.1038/s41572-018-0014-7. [DOI] [PubMed] [Google Scholar]
- 38.Zhao N., Guo F.F., Xie K.Q., Zeng T. Targeting Nrf-2 is a promising intervention approach for the prevention of ethanol-induced liver disease. Cell. Mol. Life Sci. 2018;75:3143–3157. doi: 10.1007/s00018-018-2852-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McClain C., Vatsalya V., Cave M. Role of Zinc in the Development/Progression of Alcoholic Liver Disease. Curr. Treat. Options. Gastroenterol. 2017;15:285–295. doi: 10.1007/s11938-017-0132-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han K.H., Hashimoto N., Fukushima M. Relationships among alcoholic liver disease, antioxidants, and antioxidant enzymes. World J. Gastroenterol. 2016;22:37–49. doi: 10.3748/wjg.v22.i1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pang C., Sheng Y.C., Jiang P., Wei H., Ji L.L. Chlorogenic acid prevents acetaminophen-induced liver injury: The involvement of CYP450 metabolic enzymes and some antioxidant signals. J. Zhejiang Univ. Sci. B. 2015;16:602–610. doi: 10.1631/jzus.B1400346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Purohit V., Bode J.C., Bode C., Brenner D.A., Choudhry M.A., Hamilton F., Kang Y.J., Keshavarzian A., Rao R., Sartor R.B., et al. Alcohol, intestinal bacterial growth, intestinal permeability to endotoxin, and medical consequences: Summary of a symposium. Alcohol. 2008;42:349–361. doi: 10.1016/j.alcohol.2008.03.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Groebner J.L., Tuma P.L. The Altered Hepatic Tubulin Code in Alcoholic Liver Disease. Biomolecules. 2015;5:2140–2159. doi: 10.3390/biom5032140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szabo G. Gut-liver axis in alcoholic liver disease. Gastroenterology. 2015;148:30–36. doi: 10.1053/j.gastro.2014.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma H.Y., Xu J., Liu X., Zhu Y., Gao B., Karin M., Tsukamoto H., Jeste D.V., Grant I., Roberts A.J., et al. The role of IL-17 signaling in regulation of the liver-brain axis and intestinal permeability in Alcoholic Liver Disease. Curr. Pathobiol. Rep. 2016;4:27–35. doi: 10.1007/s40139-016-0097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harrison-Findik D.D. Role of alcohol in the regulation of iron metabolism. World J. Gastroenterol. 2007;13:4925–4930. doi: 10.3748/wjg.v13.i37.4925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ioannou G.N., Dominitz J.A., Weiss N.S., Heagerty P.J., Kowdley K.V. The effect of alcohol consumption on the prevalence of iron overload, iron deficiency, and iron deficiency anemia. Gastroenterology. 2004;126:1293–1301. doi: 10.1053/j.gastro.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 48.Detivaud L., Nemeth E., Boudjema K., Turlin B., Troadec M.B., Leroyer P., Ropert M., Jacquelinet S., Courselaud B., Ganz T., et al. Hepcidin levels in humans are correlated with hepatic iron stores, hemoglobin levels, and hepatic function. Blood. 2005;106:746–748. doi: 10.1182/blood-2004-12-4855. [DOI] [PubMed] [Google Scholar]
- 49.Nemeth E., Tuttle M.S., Powelson J., Vaughn M.B., Donovan A., Ward D.M., Ganz T., Kaplan J. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–2093. doi: 10.1126/science.1104742. [DOI] [PubMed] [Google Scholar]
- 50.Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood. 2003;102:783–788. doi: 10.1182/blood-2003-03-0672. [DOI] [PubMed] [Google Scholar]
- 51.Harrison-Findik D.D., Schafer D., Klein E., Timchenko N.A., Kulaksiz H., Clemens D., Fein E., Andriopoulos B., Pantopoulos K., Gollan J. Alcohol metabolism-mediated oxidative stress down-regulates hepcidin transcription and leads to increased duodenal iron transporter expression. J. Biol. Chem. 2006;281:22974–22982. doi: 10.1074/jbc.M602098200. [DOI] [PubMed] [Google Scholar]
- 52.Harrison-Findik D.D., Klein E., Crist C., Evans J., Timchenko N., Gollan J. Iron-mediated regulation of liver hepcidin expression in rats and mice is abolished by alcohol. Hepatology. 2007;46:1979–1985. doi: 10.1002/hep.21895. [DOI] [PubMed] [Google Scholar]
- 53.Pietrangelo A. Iron, oxidative stress and liver fibrogenesis. J. Hepatol. 1998;28(Suppl. S1):8–13. doi: 10.1016/S0168-8278(98)80368-1. [DOI] [PubMed] [Google Scholar]
- 54.Valerio L.G., Parks T., Jr., Petersen D.R. Alcohol mediates increases in hepatic and serum nonheme iron stores in a rat model for alcohol-induced liver injury. Alcohol. Clin. Exp. Res. 1996;20:1352–1361. doi: 10.1111/j.1530-0277.1996.tb01134.x. [DOI] [PubMed] [Google Scholar]
- 55.Tsukamoto H., Horne W., Kamimura S., Niemela O., Parkkila S., Yla-Herttuala S., Brittenham G.M. Experimental liver cirrhosis induced by alcohol and iron. J. Clin. Invest. 1995;96:620–630. doi: 10.1172/JCI118077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Silva I., Rausch V., Seitz H.K., Mueller S. Does Hypoxia Cause Carcinogenic Iron Accumulation in Alcoholic Liver Disease (ALD)? Cancers (Basel) 2017;9:145. doi: 10.3390/cancers9110145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abdelmegeed M.A., Banerjee A., Jang S., Yoo S.H., Yun J.W., Gonzalez F.J., Keshavarzian A., Song B.J. CYP2E1 potentiates binge alcohol-induced gut leakiness, steatohepatitis, and apoptosis. Free Radic. Biol. Med. 2013;65:1238–1245. doi: 10.1016/j.freeradbiomed.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang C.K., Yu T., de la Monte S.M., Wands J.R., Derdak Z., Kim M. Restoration of Wnt/beta-catenin signaling attenuates alcoholic liver disease progression in a rat model. J. Hepatol. 2015;63:191–198. doi: 10.1016/j.jhep.2015.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ibusuki R., Uto H., Oda K., Ohshige A., Tabu K., Mawatari S., Kumagai K., Kanmura S., Tamai T., Moriuchi A., et al. Human neutrophil peptide-1 promotes alcohol-induced hepatic fibrosis and hepatocyte apoptosis. PLoS ONE. 2017;12:e0174913. doi: 10.1371/journal.pone.0174913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee Y.J., Shukla S.D. Histone H3 phosphorylation at serine 10 and serine 28 is mediated by p38 MAPK in rat hepatocytes exposed to ethanol and acetaldehyde. Eur. J. Pharm. 2007;573:29–38. doi: 10.1016/j.ejphar.2007.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kong X., Yang Y., Ren L., Shao T., Li F., Zhao C., Liu L., Zhang H., McClain C.J., Feng W. Activation of autophagy attenuates EtOH-LPS-induced hepatic steatosis and injury through MD2 associated TLR4 signaling. Sci. Rep. 2017;7:9292. doi: 10.1038/s41598-017-09045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu J., Zhou J., Wu Z., Wang X., Liu L., Yao C. Cyanidin 3-O-beta-Glucoside Ameliorates Ethanol-Induced Acute Liver Injury by Attenuating Oxidative Stress and Apoptosis: The Role of SIRT1/FOXO1 Signaling. Alcohol. Clin. Exp. Res. 2016;40:457–466. doi: 10.1111/acer.12982. [DOI] [PubMed] [Google Scholar]
- 63.Pani G., Fusco S., Colavitti R., Borrello S., Maggiano N., Cravero A.A., Farre S.M., Galeotti T., Koch O.R. Abrogation of hepatocyte apoptosis and early appearance of liver dysplasia in ethanol-fed p53-deficient mice. Biochem. Biophys. Res. Commun. 2004;325:97–100. doi: 10.1016/j.bbrc.2004.09.213. [DOI] [PubMed] [Google Scholar]
- 64.Chen G., Ke Z., Xu M., Liao M., Wang X., Qi Y., Zhang T., Frank J.A., Bower K.A., Shi X., et al. Autophagy is a protective response to ethanol neurotoxicity. Autophagy. 2012;8:1577–1589. doi: 10.4161/auto.21376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guo X., Cui R., Zhao J., Mo R., Peng L., Yan M. Corosolic acid protects hepatocytes against ethanol-induced damage by modulating mitogen-activated protein kinases and activating autophagy. Eur. J. Pharm. 2016;791:578–588. doi: 10.1016/j.ejphar.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 66.Lu Y., Cederbaum A.I. Autophagy Protects against CYP2E1/Chronic Ethanol-Induced Hepatotoxicity. Biomolecules. 2015;5:2659–2674. doi: 10.3390/biom5042659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ni H.M., Bhakta A., Wang S., Li Z., Manley S., Huang H., Copple B., Ding W.X. Role of hypoxia inducing factor-1beta in alcohol-induced autophagy, steatosis and liver injury in mice. PLoS ONE. 2014;9:e115849. doi: 10.1371/journal.pone.0115849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Song X., Yin S., Huo Y., Liang M., Fan L., Ye M., Hu H. Glycycoumarin ameliorates alcohol-induced hepatotoxicity via activation of Nrf2 and autophagy. Free Radic. Biol. Med. 2015;89:135–146. doi: 10.1016/j.freeradbiomed.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 69.Denaes T., Lodder J., Chobert M.N., Ruiz I., Pawlotsky J.M., Lotersztajn S., Teixeira-Clerc F. The Cannabinoid Receptor 2 Protects Against Alcoholic Liver Disease Via a Macrophage Autophagy-Dependent Pathway. Sci. Rep. 2016;6:28806. doi: 10.1038/srep28806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guo R., Xu X., Babcock S.A., Zhang Y., Ren J. Aldehyde dedydrogenase-2 plays a beneficial role in ameliorating chronic alcohol-induced hepatic steatosis and inflammation through regulation of autophagy. J. Hepatol. 2015;62:647–656. doi: 10.1016/j.jhep.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 71.Nepal S., Park P.H. Activation of autophagy by globular adiponectin attenuates ethanol-induced apoptosis in HepG2 cells: Involvement of AMPK/FoxO3A axis. Biochim. Biophys. Acta. 2013;1833:2111–2125. doi: 10.1016/j.bbamcr.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 72.You Y., Li W.Z., Zhang S., Hu B., Li Y.X., Li H.D., Tang H.H., Li Q.W., Guan Y.Y., Liu L.X., et al. SNX10 mediates alcohol-induced liver injury and steatosis by regulating the activation of chaperone-mediated autophagy. J. Hepatol. 2018;69:129–141. doi: 10.1016/j.jhep.2018.01.038. [DOI] [PubMed] [Google Scholar]
- 73.Stickel F., Datz C., Hampe J., Bataller R. Pathophysiology and Management of Alcoholic Liver Disease: Update 2016. Gut. Liver. 2017;11:173–188. doi: 10.5009/gnl16477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kolla B.P., Schneekloth T.D., Biernacka J., Shah V., Lazaridis K.N., Geske J., Karpyak V. PNPLA3 Association with Alcoholic Liver Disease in a Cohort of Heavy Drinkers. Alcohol Alcohol. 2018;53:357–360. doi: 10.1093/alcalc/agy007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang Y., Guo T., Yang F., Mao Y., Li L., Liu C., Sun Q., Li Y., Huang J. Single-nucleotide rs738409 polymorphisms in the PNPLA3 gene are strongly associated with alcoholic liver disease in Han Chinese males. Hepatol. Int. 2018;12:429–437. doi: 10.1007/s12072-018-9889-3. [DOI] [PubMed] [Google Scholar]
- 76.Friedrich K., Wannhoff A., Kattner S., Brune M., Hov J.R., Weiss K.H., Antoni C., Dollinger M., Neumann-Haefelin C., Seufferlein T., et al. PNPLA3 in end-stage liver disease: Alcohol consumption, hepatocellular carcinoma development; transplantation-free survival. J. Gastroenterol. Hepatol. 2014;29:1477–1484. doi: 10.1111/jgh.12540. [DOI] [PubMed] [Google Scholar]
- 77.Li Y.M., Fan J.G., Wang B.Y., Lu L.G., Shi J.P., Niu J.Q., Shen W. Chinese Association for the Study of Liver, D. Guidelines for the diagnosis and management of alcoholic liver disease: Update 2010: (published in Chin. Chin. J. Hepatol. 2010, 18, 167–170) J. Dig. Dis. 2011;12:45–50. doi: 10.1111/j.1751-2980.2010.00477.x. [DOI] [PubMed] [Google Scholar]
- 78.Singal A.K., Bataller R., Ahn J., Kamath P.S., Shah V.H. ACG Clinical Guideline: Alcoholic Liver Disease. Am. J. Gastroenterol. 2018;113:175–194. doi: 10.1038/ajg.2017.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sueyoshi S., Sawai S., Satoh M., Seimiya M., Sogawa K., Fukumura A., Tsutsumi M., Nomura F. Fractionation of gamma-glutamyltransferase in patients with nonalcoholic fatty liver disease and alcoholic liver disease. World J. Hepatol. 2016;8:1610–1616. doi: 10.4254/wjh.v8.i36.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Palmentieri B., de Sio I., La Mura V., Masarone M., Vecchione R., Bruno S., Torella R., Persico M. The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig. Liver Dis. 2006;38:485–489. doi: 10.1016/j.dld.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 81.Grandison G.A., Angulo P. Can NASH be diagnosed, graded, and staged noninvasively? Clin. Liver Dis. 2012;16:567–585. doi: 10.1016/j.cld.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kollmann D., Rasoul-Rockenschaub S., Steiner I., Freundorfer E., Gyori G.P., Silberhumer G., Soliman T., Berlakovich G.A. Good outcome after liver transplantation for ALD without a 6 months abstinence rule prior to transplantation including post-transplant CDT monitoring for alcohol relapse assessment-a retrospective study. Transpl. Int. 2016;29:559–567. doi: 10.1111/tri.12756. [DOI] [PubMed] [Google Scholar]
- 83.European Association for the Study of the Liver EASL clinical practical guidelines: Management of alcoholic liver disease. J. Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 84.Vasiliou V. Biological basis of alcohol-induced cancer. Springer Science+Business Media; New York, NY, USA: 2014. [Google Scholar]
- 85.Suk K.T., Kim M.Y., Baik S.K. Alcoholic liver disease: Treatment. World J. Gastroenterol. 2014;20:12934–12944. doi: 10.3748/wjg.v20.i36.12934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sidhu S.S., Goyal O., Kishore H., Sidhu S. New paradigms in management of alcoholic hepatitis: A review. Hepatol. Int. 2017;11:255–267. doi: 10.1007/s12072-017-9790-5. [DOI] [PubMed] [Google Scholar]
- 87.Morley K.C., Leung S., Baillie A., Haber P.S. The efficacy and biobehavioural basis of baclofen in the treatment of alcoholic liver disease (BacALD): Study protocol for a randomised controlled trial. Contemp. Clin. Trials. 2013;36:348–355. doi: 10.1016/j.cct.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 88.Salama Z.A., Sadek A., Abdelhady A.M., Darweesh S.K., Morsy S.A., Esmat G. Losartan may inhibit the progression of liver fibrosis in chronic HCV patients. Hepatobiliary Surg. Nutr. 2016;5:249–255. doi: 10.21037/hbsn.2016.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sookoian S., Fernandez M.A., Castano G. Effects of six months losartan administration on liver fibrosis in chronic hepatitis C patients: A pilot study. World J. Gastroenterol. 2005;11:7560–7563. doi: 10.3748/wjg.v11.i48.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rambaldi A., Iaquinto G., Gluud C. Anabolic-androgenic steroids for alcoholic liver disease: A Cochrane review. Am. J. Gastroenterol. 2002;97:1674–1681. doi: 10.1016/S0002-9270(02)04182-5. [DOI] [PubMed] [Google Scholar]
- 91.Marroni C.A., Fleck A.M., Fernandes S.A., Jr., Galant L.H., Mucenic M., de Mattos Meine M.H., Mariante-Neto G., Brandao A.B.M. Liver transplantation and alcoholic liver disease: History, controversies, and considerations. World J. Gastroenterol. 2018;24:2785–2805. doi: 10.3748/wjg.v24.i26.2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Iruzubieta P., Crespo J., Fabrega E. Long-term survival after liver transplantation for alcoholic liver disease. World J. Gastroenterol. 2013;19:9198–9208. doi: 10.3748/wjg.v19.i48.9198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rice J.P., Eickhoff J., Agni R., Ghufran A., Brahmbhatt R., Lucey M.R. Abusive drinking after liver transplantation is associated with allograft loss and advanced allograft fibrosis. Liver Transpl. 2013;19:1377–1386. doi: 10.1002/lt.23762. [DOI] [PubMed] [Google Scholar]
- 94.Testino G., Leone S., Ansaldi F., Borro P. Silymarin and S-adenosyl-L-methionine (SAMe): Two promising pharmacological agents in case of chronic alcoholic hepathopathy. A review and a point of view. Minerva. Gastroenterol. Dietol. 2013;59:341–356. [PubMed] [Google Scholar]
- 95.Kessova I.G., Cederbaum A.I. Mitochondrial alterations in livers of Sod1-/- mice fed alcohol. Free Radic. Biol. Med. 2007;42:1470–1480. doi: 10.1016/j.freeradbiomed.2007.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Assiri M.A., Roy S.R., Harris P.S., Ali H., Liang Y., Shearn C.T., Orlicky D.J., Roede J.R., Hirschey M.D., Backos D.S., et al. Chronic Ethanol Metabolism Inhibits Hepatic Mitochondrial Superoxide Dismutase via Lysine Acetylation. Alcohol. Clin. Exp. Res. 2017;41:1705–1714. doi: 10.1111/acer.13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chattopadhyay A., Pinkaew D., Doan H.Q., Jacob R.B., Verma S.K., Friedman H., Peterson A.C., Kuyumcu-Martinez M.N., McDougal O.M., Fujise K. Fortilin potentiates the peroxidase activity of Peroxiredoxin-1 and protects against alcohol-induced liver damage in mice. Sci. Rep. 2016;6:18701. doi: 10.1038/srep18701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bae S.H., Sung S.H., Cho E.J., Lee S.K., Lee H.E., Woo H.A., Yu D.Y., Kil I.S., Rhee S.G. Concerted action of sulfiredoxin and peroxiredoxin I protects against alcohol-induced oxidative injury in mouse liver. Hepatology. 2011;53:945–953. doi: 10.1002/hep.24104. [DOI] [PubMed] [Google Scholar]
- 99.Chen Y., Singh S., Matsumoto A., Manna S.K., Abdelmegeed M.A., Golla S., Murphy R.C., Dong H., Song B.J., Gonzalez F.J., et al. Chronic Glutathione Depletion Confers Protection against Alcohol-induced Steatosis: Implication for Redox Activation of AMP-activated Protein Kinase Pathway. Sci. Rep. 2016;6:29743. doi: 10.1038/srep29743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bakhautdin B., Das D., Mandal P., Roychowdhury S., Danner J., Bush K., Pollard K., Kaspar J.W., Li W., Salomon R.G., et al. Protective role of HO-1 and carbon monoxide in ethanol-induced hepatocyte cell death and liver injury in mice. J. Hepatol. 2014;61:1029–1037. doi: 10.1016/j.jhep.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang X., Cederbaum A.I. Acute ethanol pretreatment increases FAS-mediated liver injury in mice: Role of oxidative stress and CYP2E1-dependent and -independent pathways. Free Radic. Biol. Med. 2007;42:971–984. doi: 10.1016/j.freeradbiomed.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koteish A., Yang S., Lin H., Huang X., Diehl A.M. Chronic ethanol exposure potentiates lipopolysaccharide liver injury despite inhibiting Jun N-terminal kinase and caspase 3 activation. J. Biol. Chem. 2002;277:13037–13044. doi: 10.1074/jbc.M101632200. [DOI] [PubMed] [Google Scholar]
- 103.Miller A.M., Wang H., Park O., Horiguchi N., Lafdil F., Mukhopadhyay P., Moh A., Fu X.Y., Kunos G., Pacher P., et al. Anti-inflammatory and anti-apoptotic roles of endothelial cell STAT3 in alcoholic liver injury. Alcohol. Clin. Exp. Res. 2010;34:719–725. doi: 10.1111/j.1530-0277.2009.01141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hoek J.B., Pastorino J.G. Cellular signaling mechanisms in alcohol-induced liver damage. Semin. Liver Dis. 2004;24:257–272. doi: 10.1055/s-2004-832939. [DOI] [PubMed] [Google Scholar]
- 105.Lee Y.J., Shukla S.D. Pro- and anti-apoptotic roles of c-Jun N-terminal kinase (JNK) in ethanol and acetaldehyde exposed rat hepatocytes. Eur. J. Pharm. 2005;508:31–45. doi: 10.1016/j.ejphar.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 106.Hu S., Yin S., Jiang X., Huang D., Shen G. Melatonin protects against alcoholic liver injury by attenuating oxidative stress, inflammatory response, and apoptosis. Eur. J. Pharm. 2009;616:287–292. doi: 10.1016/j.ejphar.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 107.Zhao H., Zhao C., Dong Y., Zhang M., Wang Y., Li F., Li X., McClain C., Yang S., Feng W. Inhibition of miR122a by Lactobacillus rhamnosus GG culture supernatant increases intestinal occludin expression and protects mice from alcoholic liver disease. Toxicol. Lett. 2015;234:194–200. doi: 10.1016/j.toxlet.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 108.Cheng X.Y., Liu J.D., Lu X.Y., Yan X., Huang C., Meng X.M., Li J. miR-203 Inhibits Alcohol-Induced Hepatic Steatosis by Targeting Lipin1. Front. Pharm. 2018;9:275. doi: 10.3389/fphar.2018.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bala S., Petrasek J., Mundkur S., Catalano D., Levin I., Ward J., Alao H., Kodys K., Szabo G. Circulating microRNAs in exosomes indicate hepatocyte injury and inflammation in alcoholic, drug-induced, and inflammatory liver diseases. Hepatology. 2012;56:1946–1957. doi: 10.1002/hep.25873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Satishchandran A., Ambade A., Rao S., Hsueh Y.C., Iracheta-Vellve A., Tornai D., Lowe P., Gyongyosi B., Li J., Catalano D., et al. MicroRNA 122, Regulated by GRLH2, Protects Livers of Mice and Patients From Ethanol-Induced Liver Disease. Gastroenterology. 2018;154:238–252.e7. doi: 10.1053/j.gastro.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Szabo G., Satishchandran A. MicroRNAs in alcoholic liver disease. Semin. Liver Dis. 2015;35:36–42. doi: 10.1055/s-0034-1397347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jin X., Yu M.S., Huang Y., Xiang Z., Chen Y.P. MiR-30e-UCP2 pathway regulates alcoholic hepatitis progress by influencing ATP and hydrogen peroxide expression. Oncotarget. 2017;8:64294–64302. doi: 10.18632/oncotarget.19729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Brandon-Warner E., Feilen N.A., Culberson C.R., Field C.O., deLemos A.S., Russo M.W., Schrum L.W. Processing of miR17-92 Cluster in Hepatic Stellate Cells Promotes Hepatic Fibrogenesis During Alcohol-Induced Injury. Alcohol Clin. Exp. Res. 2016;40:1430–1442. doi: 10.1111/acer.13116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim Y.D., Hwang S.L., Lee E.J., Kim H.M., Chung M.J., Elfadl A.K., Lee S.E., Nedumaran B., Harris R.A., Jeong K.S. Melatonin ameliorates alcohol-induced bile acid synthesis by enhancing miR-497 expression. J. Pineal. Res. 2017;62:e12386. doi: 10.1111/jpi.12386. [DOI] [PubMed] [Google Scholar]
- 115.Heo M.J., Kim T.H., You J.S., Blaya D., Sancho-Bru P., Kim S.G. Alcohol dysregulates miR-148a in hepatocytes through FoxO1, facilitating pyroptosis via TXNIP overexpression. Gut. 2018;68:708–720. doi: 10.1136/gutjnl-2017-315123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yin H., Liang X., Jogasuria A., Davidson N.O., You M. miR-217 regulates ethanol-induced hepatic inflammation by disrupting sirtuin 1-lipin-1 signaling. Am. J. Pathol. 2015;185:1286–1296. doi: 10.1016/j.ajpath.2015.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dong X., Liu H., Chen F., Li D., Zhao Y. MiR-214 promotes the alcohol-induced oxidative stress via down-regulation of glutathione reductase and cytochrome P450 oxidoreductase in liver cells. Alcohol Clin. Exp. Res. 2014;38:68–77. doi: 10.1111/acer.12209. [DOI] [PubMed] [Google Scholar]
- 118.Bala S., Szabo G. MicroRNA Signature in Alcoholic Liver Disease. Int. J. Hepatol. 2012;2012:498232. doi: 10.1155/2012/498232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bala S., Csak T., Saha B., Zatsiorsky J., Kodys K., Catalano D., Satishchandran A., Szabo G. The pro-inflammatory effects of miR-155 promote liver fibrosis and alcohol-induced steatohepatitis. J. Hepatol. 2016;64:1378–1387. doi: 10.1016/j.jhep.2016.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Eguchi A., Lazaro R.G., Wang J., Kim J., Povero D., Willliams B., Ho S.B., Starkel P., Schnabl B., Ohno-Machado L., et al. Extracellular vesicles released by hepatocytes from gastric infusion model of alcoholic liver disease contain a MicroRNA barcode that can be detected in blood. Hepatology. 2017;65:475–490. doi: 10.1002/hep.28838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhao Y.X., Sun Y.Y., Huang A.L., Li X.F., Huang C., Ma T.T., Li J. MicroRNA-200a induces apoptosis by targeting ZEB2 in alcoholic liver disease. Cell Cycle. 2018;17:250–262. doi: 10.1080/15384101.2017.1417708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Iwagami Y., Zou J., Zhang H., Cao K., Ji C., Kim M., Huang C.K. Alcohol-mediated miR-34a modulates hepatocyte growth and apoptosis. J. Cell. Mol. Med. 2018;22:3897–3995. doi: 10.1111/jcmm.13681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.El-Assal O., Hong F., Kim W.H., Radaeva S., Gao B. IL-6-deficient mice are susceptible to ethanol-induced hepatic steatosis: IL-6 protects against ethanol-induced oxidative stress and mitochondrial permeability transition in the liver. Cell. Mol. Immunol. 2004;1:205–211. [PubMed] [Google Scholar]
- 124.Tilg H., Moschen A.R., Szabo G. Interleukin-1 and inflammasomes in alcoholic liver disease/acute alcoholic hepatitis and nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Hepatology. 2016;64:955–965. doi: 10.1002/hep.28456. [DOI] [PubMed] [Google Scholar]
- 125.Bertola A., Park O., Gao B. Chronic plus binge ethanol feeding synergistically induces neutrophil infiltration and liver injury in mice: A critical role for E-selectin. Hepatology. 2013;58:1814–1823. doi: 10.1002/hep.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ki S.H., Park O., Zheng M., Morales-Ibanez O., Kolls J.K., Bataller R., Gao B. Interleukin-22 treatment ameliorates alcoholic liver injury in a murine model of chronic-binge ethanol feeding: Role of signal transducer and activator of transcription 3. Hepatology. 2010;52:1291–1300. doi: 10.1002/hep.23837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Santiago-Lomeli M., Gomez-Quiroz L.E., Ortiz-Ortega V.M., Kershenobich D., Gutierrez-Ruiz M.C. Differential effect of interleukin-10 on hepatocyte apoptosis. Life Sci. 2005;76:2569–2579. doi: 10.1016/j.lfs.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 128.Ni Y.H., Huo L.J., Li T.T. Antioxidant axis Nrf2-keap1-ARE in inhibition of alcoholic liver fibrosis by IL-22. World J. Gastroenterol. 2017;23:2002–2011. doi: 10.3748/wjg.v23.i11.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dominguez M., Miquel R., Colmenero J., Moreno M., Garcia-Pagan J.C., Bosch J., Arroyo V., Gines P., Caballeria J., Bataller R. Hepatic expression of CXC chemokines predicts portal hypertension and survival in patients with alcoholic hepatitis. Gastroenterology. 2009;136:1639–1650. doi: 10.1053/j.gastro.2009.01.056. [DOI] [PubMed] [Google Scholar]
- 130.Affo S., Morales-Ibanez O., Rodrigo-Torres D., Altamirano J., Blaya D., Dapito D.H., Millan C., Coll M., Caviglia J.M., Arroyo V., et al. CCL20 mediates lipopolysaccharide induced liver injury and is a potential driver of inflammation and fibrosis in alcoholic hepatitis. Gut. 2014;63:1782–1792. doi: 10.1136/gutjnl-2013-306098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Degre D., Lemmers A., Gustot T., Ouziel R., Trepo E., Demetter P., Verset L., Quertinmont E., Vercruysse V., Le Moine O., et al. Hepatic expression of CCL2 in alcoholic liver disease is associated with disease severity and neutrophil infiltrates. Clin. Exp. Immunol. 2012;169:302–310. doi: 10.1111/j.1365-2249.2012.04609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Roh Y.S., Zhang B., Loomba R., Seki E. TLR2 and TLR9 contribute to alcohol-mediated liver injury through induction of CXCL1 and neutrophil infiltration. Am. J. Physiol. Gastrointest. Liver Physiol. 2015;309:G30–G41. doi: 10.1152/ajpgi.00031.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ambade A., Lowe P., Kodys K., Catalano D., Gyongyosi B., Cho Y., Iracheta Vellve A., Adejumo A., Saha B., Calenda C., et al. Pharmacological inhibition of CCR2/5 signaling prevents and reverses alcohol-induced liver damage, steatosis and inflammation in mice. Hepatology. 2018 doi: 10.1002/hep.30249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Karim S., Liaskou E., Hadley S., Youster J., Faint J., Adams D.H., Lalor P.F. An in vitro model of human acute ethanol exposure that incorporates CXCR3- and CXCR4-dependent recruitment of immune cells. Toxicol. Sci. 2013;132:131–141. doi: 10.1093/toxsci/kfs337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cassard A.M., Ciocan D. Microbiota, a key player in alcoholic liver disease. Clin. Mol. Hepatol. 2018;24:100–107. doi: 10.3350/cmh.2017.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hartmann P., Chen W.C., Schnabl B. The intestinal microbiome and the leaky gut as therapeutic targets in alcoholic liver disease. Front. Physiol. 2012;3:402. doi: 10.3389/fphys.2012.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hong M., Han D.H., Hong J., Kim D.J., Suk K.T. Are Probiotics Effective in Targeting Alcoholic Liver Diseases? Probiotics Antimicrob. Proteins. 2018 doi: 10.1007/s12602-018-9419-6. [DOI] [PubMed] [Google Scholar]
- 138.Chen R.C., Xu L.M., Du S.J., Huang S.S., Wu H., Dong J.J., Huang J.R., Wang X.D., Feng W.K., Chen Y.P. Lactobacillus rhamnosus GG supernatant promotes intestinal barrier function, balances Treg and TH17 cells and ameliorates hepatic injury in a mouse model of chronic-binge alcohol feeding. Toxicol. Lett. 2016;241:103–110. doi: 10.1016/j.toxlet.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 139.Hong M., Kim S.W., Han S.H., Kim D.J., Suk K.T., Kim Y.S., Kim M.J., Kim M.Y., Baik S.K., Ham Y.L. Probiotics (Lactobacillus rhamnosus R0011 and acidophilus R0052) reduce the expression of toll-like receptor 4 in mice with alcoholic liver disease. PLoS ONE. 2015;10:e0117451. doi: 10.1371/journal.pone.0117451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chiu W.C., Huang Y.L., Chen Y.L., Peng H.C., Liao W.H., Chuang H.L., Chen J.R., Yang S.C. Synbiotics reduce ethanol-induced hepatic steatosis and inflammation by improving intestinal permeability and microbiota in rats. Food Funct. 2015;6:1692–1700. doi: 10.1039/C5FO00104H. [DOI] [PubMed] [Google Scholar]
- 141.Grander C., Adolph T.E., Wieser V., Lowe P., Wrzosek L., Gyongyosi B., Ward D.V., Grabherr F., Gerner R.R., Pfister A., et al. Recovery of ethanol-induced Akkermansia muciniphila depletion ameliorates alcoholic liver disease. Gut. 2018;67:891–901. doi: 10.1136/gutjnl-2016-313432. [DOI] [PubMed] [Google Scholar]
- 142.Barone R., Rappa F., Macaluso F., Caruso Bavisotto C., Sangiorgi C., Di Paola G., Tomasello G., Di Felice V., Marciano V., Farina F., et al. Alcoholic Liver Disease: A Mouse Model Reveals Protection by Lactobacillus fermentum. Clin. Transl. Gastroenterol. 2016;7:e138. doi: 10.1038/ctg.2015.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Apte U.M., Banerjee A., McRee R., Wellberg E., Ramaiah S.K. Role of osteopontin in hepatic neutrophil infiltration during alcoholic steatohepatitis. Toxicol. Appl. Pharm. 2005;207:25–38. doi: 10.1016/j.taap.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 144.Seth D., Duly A., Kuo P.C., McCaughan G.W., Haber P.S. Osteopontin is an important mediator of alcoholic liver disease via hepatic stellate cell activation. World J. Gastroenterol. 2014;20:13088–13104. doi: 10.3748/wjg.v20.i36.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ge X., Leung T.M., Arriazu E., Lu Y., Urtasun R., Christensen B., Fiel M.I., Mochida S., Sorensen E.S., Nieto N. Osteopontin binding to lipopolysaccharide lowers tumor necrosis factor-alpha and prevents early alcohol-induced liver injury in mice. Hepatology. 2014;59:1600–1616. doi: 10.1002/hep.26931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lazaro R., Wu R., Lee S., Zhu N.L., Chen C.L., French S.W., Xu J., Machida K., Tsukamoto H. Osteopontin deficiency does not prevent but promotes alcoholic neutrophilic hepatitis in mice. Hepatology. 2015;61:129–140. doi: 10.1002/hep.27383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Magdaleno F., Ge X., Fey H., Lu Y., Gaskell H., Blajszczak C.C., Aloman C., Fiel M.I., Nieto N. Osteopontin deletion drives hematopoietic stem cell mobilization to the liver and increases hepatic iron contributing to alcoholic liver disease. Hepatol. Commun. 2018;2:84–98. doi: 10.1002/hep4.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Basu P.P., Aloysius M.M., Shah N.J., Brown R.S., Jr. Review article: The endocannabinoid system in liver disease, a potential therapeutic target. Aliment. Pharm. 2014;39:790–801. doi: 10.1111/apt.12673. [DOI] [PubMed] [Google Scholar]
- 149.Trebicka J., Racz I., Siegmund S.V., Cara E., Granzow M., Schierwagen R., Klein S., Wojtalla A., Hennenberg M., Huss S., et al. Role of cannabinoid receptors in alcoholic hepatic injury: Steatosis and fibrogenesis are increased in CB2 receptor-deficient mice and decreased in CB1 receptor knockouts. Liver Int. 2011;31:860–870. doi: 10.1111/j.1478-3231.2011.02496.x. [DOI] [PubMed] [Google Scholar]
- 150.Yang Y.Y., Lin H.C. Cross-regulation of cannabinoid CB(1) and CB(2) receptors governs hepatic steatosis. Liver Int. 2010;30:1397–1399. doi: 10.1111/j.1478-3231.2010.02352.x. [DOI] [PubMed] [Google Scholar]
- 151.Amato G.S., Manke A., Harris D.L., Wiethe R.W., Vasukuttan V., Snyder R.W., Lefever T.W., Cortes R., Zhang Y., Wang S., et al. Blocking Alcoholic Steatosis in Mice with a Peripherally Restricted Purine Antagonist of the Type 1 Cannabinoid Receptor. J. Med. Chem. 2018;61:4370–4385. doi: 10.1021/acs.jmedchem.7b01820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.De Gottardi A., Spahr L., Ravier-Dall’Antonia F., Hadengue A. Cannabinoid receptor 1 and 2 agonists increase lipid accumulation in hepatocytes. Liver Int. 2010;30:1482–1489. doi: 10.1111/j.1478-3231.2010.02298.x. [DOI] [PubMed] [Google Scholar]
- 153.Kim D.K., Kim Y.H., Jang H.H., Park J., Kim J.R., Koh M., Jeong W.I., Koo S.H., Park T.S., Yun C.H., et al. Estrogen-related receptor gamma controls hepatic CB1 receptor-mediated CYP2E1 expression and oxidative liver injury by alcohol. Gut. 2013;62:1044–1054. doi: 10.1136/gutjnl-2012-303347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wang S., Pacher P., De Lisle R.C., Huang H., Ding W.X. A Mechanistic Review of Cell Death in Alcohol-Induced Liver Injury. Alcohol Clin. Exp. Res. 2016;40:1215–1223. doi: 10.1111/acer.13078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wang H., Zhao T., Xu F., Li Y., Wu M., Zhu D., Cong X., Liu Y. How important is differentiation in the therapeutic effect of mesenchymal stromal cells in liver disease? Cytotherapy. 2014;16:309–318. doi: 10.1016/j.jcyt.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 156.Ji R., Zhang N., You N., Li Q., Liu W., Jiang N., Liu J., Zhang H., Wang D., Tao K., et al. The differentiation of MSCs into functional hepatocyte-like cells in a liver biomatrix scaffold and their transplantation into liver-fibrotic mice. Biomaterials. 2012;33:8995–9008. doi: 10.1016/j.biomaterials.2012.08.058. [DOI] [PubMed] [Google Scholar]
- 157.Le Blanc K., Ringden O. Mesenchymal stem cells: Properties and role in clinical bone marrow transplantation. Curr. Opin. Immunol. 2006;18:586–591. doi: 10.1016/j.coi.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 158.Mohamadnejad M., Namiri M., Bagheri M., Hashemi S.M., Ghanaati H., Zare Mehrjardi N., Kazemi Ashtiani S., Malekzadeh R., Baharvand H. Phase 1 human trial of autologous bone marrow-hematopoietic stem cell transplantation in patients with decompensated cirrhosis. World J. Gastroenterol. 2007;13:3359–3363. doi: 10.3748/wjg.v13.i24.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jang Y.O., Kim Y.J., Baik S.K., Kim M.Y., Eom Y.W., Cho M.Y., Park H.J., Park S.Y., Kim B.R., Kim J.W., et al. Histological improvement following administration of autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: A pilot study. Liver Int. 2014;34:33–41. doi: 10.1111/liv.12218. [DOI] [PubMed] [Google Scholar]
- 160.Puglisi M.A., Tesori V., Lattanzi W., Piscaglia A.C., Gasbarrini G.B., D’Ugo D.M., Gasbarrini A. Therapeutic implications of mesenchymal stem cells in liver injury. J. Biomed. Biotechnol. 2011;2011:860578. doi: 10.1155/2011/860578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Meier R.P., Muller Y.D., Morel P., Gonelle-Gispert C., Buhler L.H. Transplantation of mesenchymal stem cells for the treatment of liver diseases, is there enough evidence? Stem Cell Res. 2013;11:1348–1364. doi: 10.1016/j.scr.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 162.Seitz H.K., Mueller S. Established therapies and new therapeutic strategies in alcoholic liver disease. Z Gastroenterol. 2017;55:291–303. doi: 10.1055/s-0042-119454. [DOI] [PubMed] [Google Scholar]
- 163.Parekkadan B., van Poll D., Megeed Z., Kobayashi N., Tilles A.W., Berthiaume F., Yarmush M.L. Immunomodulation of activated hepatic stellate cells by mesenchymal stem cells. Biochem. Biophys. Res. Commun. 2007;363:247–252. doi: 10.1016/j.bbrc.2007.05.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Qin S., Jiang H., Su S., Wang D., Liang Z., Zhang J., Yang W. Inhibition of hepatic stellate cell proliferation by bone marrow mesenchymal stem cells via regulation of the cell cycle in rat. Exp. Med. 2012;4:375–380. doi: 10.3892/etm.2012.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Guo Y., Chen B., Chen L.J., Zhang C.F., Xiang C. Current status and future prospects of mesenchymal stem cell therapy for liver fibrosis. J. Zhejiang Univ. Sci. B. 2016;17:831–841. doi: 10.1631/jzus.B1600101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.An L., Lang Q., Shen W., Shi Q., Feng F. Dynamic metabolic profiling of urine biomarkers in rats with alcoholinduced liver damage following treatment with ZhiZiDaHuang decoction. Mol. Med. Rep. 2016;14:2093–2100. doi: 10.3892/mmr.2016.5494. [DOI] [PubMed] [Google Scholar]
- 167.Wu T., Liu T., Zhang L., Xing L.J., Zheng P.Y., Ji G. Chinese medicinal formula, Qinggan Huoxue Recipe protects rats from alcoholic liver disease via the lipopolysaccharide-Kupffer cell signal conduction pathway. Exp. Med. 2014;8:363–370. doi: 10.3892/etm.2014.1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yin J., Luo Y., Deng H., Qin S., Tang W., Zeng L., Zhou B. Hugan Qingzhi medication ameliorates hepatic steatosis by activating AMPK and PPARalpha pathways in L02 cells and HepG2 cells. J. Ethnopharmacol. 2014;154:229–239. doi: 10.1016/j.jep.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 169.Chen W.M., Shaw L.H., Chang P.J., Tung S.Y., Chang T.S., Shen C.H., Hsieh Y.Y., Wei K.L. Hepatoprotective effect of resveratrol against ethanol-induced oxidative stress through induction of superoxide dismutase in vivo and in vitro. Exp. Med. 2016;11:1231–1238. doi: 10.3892/etm.2016.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Liu L.Q., Fan Z.Q., Tang Y.F., Ke Z.J. The resveratrol attenuates ethanol-induced hepatocyte apoptosis via inhibiting ER-related caspase-12 activation and PDE activity in vitro. Alcohol. Clin. Exp. Res. 2014;38:683–693. doi: 10.1111/acer.12311. [DOI] [PubMed] [Google Scholar]
- 171.Ma Z., Zhang Y., Li Q., Xu M., Bai J., Wu S. Resveratrol improves alcoholic fatty liver disease by downregulating HIF-1alpha expression and mitochondrial ROS production. PLoS ONE. 2017;12:e0183426. doi: 10.1371/journal.pone.0183426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chen L.Y., Chen Q., Cheng Y.F., Jin H.H., Kong D.S., Zhang F., Wu L., Shao J.J., Zheng S.Z. Diallyl trisulfide attenuates ethanol-induced hepatic steatosis by inhibiting oxidative stress and apoptosis. Biomed. Pharm. 2016;79:35–43. doi: 10.1016/j.biopha.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 173.Chen L.Y., Chen Q., Zhu X.J., Kong D.S., Wu L., Shao J.J., Zheng S.Z. Diallyl trisulfide protects against ethanol-induced oxidative stress and apoptosis via a hydrogen sulfide-mediated mechanism. Int. Immunopharmacol. 2016;36:23–30. doi: 10.1016/j.intimp.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 174.Guan M.J., Zhao N., Xie K.Q., Zeng T. Hepatoprotective effects of garlic against ethanol-induced liver injury: A mini-review. Food Chem. Toxicol. 2018;111:467–473. doi: 10.1016/j.fct.2017.11.059. [DOI] [PubMed] [Google Scholar]
- 175.Zeng T., Zhang C.L., Song F.Y., Zhao X.L., Yu L.H., Zhu Z.P., Xie K.Q. The activation of HO-1/Nrf-2 contributes to the protective effects of diallyl disulfide (DADS) against ethanol-induced oxidative stress. Biochim. Biophys. Acta. 2013;1830:4848–4859. doi: 10.1016/j.bbagen.2013.06.028. [DOI] [PubMed] [Google Scholar]
- 176.Bak M.J., Truong V.L., Ko S.Y., Nguyen X.N., Ingkasupart P., Jun M., Shin J.Y., Jeong W.S. Antioxidant and Hepatoprotective Effects of Procyanidins from Wild Grape (Vitis amurensis) Seeds in Ethanol-Induced Cells and Rats. Int. J. Mol. Sci. 2016;17:758. doi: 10.3390/ijms17050758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Jiang Z., Chen C., Wang J., Xie W., Wang M., Li X., Zhang X. Purple potato (Solanum tuberosum L.) anthocyanins attenuate alcohol-induced hepatic injury by enhancing antioxidant defense. J. Nat. Med. 2016;70:45–53. doi: 10.1007/s11418-015-0935-3. [DOI] [PubMed] [Google Scholar]
- 178.Jiang Z., Chen C., Xie W., Wang M., Wang J., Zhang X. Anthocyanins attenuate alcohol-induced hepatic injury by inhibiting pro-inflammation signalling. Nat. Prod. Res. 2016;30:469–473. doi: 10.1080/14786419.2015.1020492. [DOI] [PubMed] [Google Scholar]
- 179.Wang Z., Su B., Fan S., Fei H., Zhao W. Protective effect of oligomeric proanthocyanidins against alcohol-induced liver steatosis and injury in mice. Biochem. Biophys. Res. Commun. 2015;458:757–762. doi: 10.1016/j.bbrc.2015.01.153. [DOI] [PubMed] [Google Scholar]
- 180.Stice C.P., Liu C., Aizawa K., Greenberg A.S., Ausman L.M., Wang X.D. Dietary tomato powder inhibits alcohol-induced hepatic injury by suppressing cytochrome p450 2E1 induction in rodent models. Arch. Biochem. Biophys. 2015;572:81–88. doi: 10.1016/j.abb.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sun Q., Zhang W., Zhong W., Sun X., Zhou Z. Dietary Fisetin Supplementation Protects Against Alcohol-Induced Liver Injury in Mice. Alcohol Clin. Exp. Res. 2016;40:2076–2084. doi: 10.1111/acer.13172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhuang X., Deng Z.B., Mu J., Zhang L., Yan J., Miller D., Feng W., McClain C.J., Zhang H.G. Ginger-derived nanoparticles protect against alcohol-induced liver damage. J. Extracell. Vesicles. 2015;4:28713. doi: 10.3402/jev.v4.28713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Varga Z.V., Matyas C., Erdelyi K., Cinar R., Nieri D., Chicca A., Nemeth B.T., Paloczi J., Lajtos T., Corey L., et al. beta-Caryophyllene protects against alcoholic steatohepatitis by attenuating inflammation and metabolic dysregulation in mice. Br. J. Pharm. 2018;175:320–334. doi: 10.1111/bph.13722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Xiao J., Zhang R., Huang F., Liu L., Deng Y., Ma Y., Wei Z., Tang X., Zhang Y., Zhang M. Lychee (Litchi chinensis Sonn.) Pulp Phenolic Extract Confers a Protective Activity against Alcoholic Liver Disease in Mice by Alleviating Mitochondrial Dysfunction. J. Agric. Food Chem. 2017;65:5000–5009. doi: 10.1021/acs.jafc.7b01844. [DOI] [PubMed] [Google Scholar]
- 185.Han J.Y., Lee S., Yang J.H., Kim S., Sim J., Kim M.G., Jeong T.C., Ku S.K., Cho I.J., Ki S.H. Korean Red Ginseng attenuates ethanol-induced steatosis and oxidative stress via AMPK/Sirt1 activation. J. Ginseng. Res. 2015;39:105–115. doi: 10.1016/j.jgr.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Hu C.F., Sun L.P., Yang Q.H., Lu D.X., Luo S. Ginsenosides from stems and leaves of ginseng prevent ethanol-induced lipid accumulation in human L02 hepatocytes. Chin. J. Integr. Med. 2017;23:438–444. doi: 10.1007/s11655-016-2617-8. [DOI] [PubMed] [Google Scholar]
- 187.Li Y.G., Ji D.F., Zhong S., Shi L.G., Hu G.Y., Chen S. Saponins from Panax japonicus protect against alcohol-induced hepatic injury in mice by up-regulating the expression of GPX3, SOD1 and SOD3. Alcohol Alcohol. 2010;45:320–331. doi: 10.1093/alcalc/agq034. [DOI] [PubMed] [Google Scholar]
- 188.Ding L., Wo L., Du Z., Tang L., Song Z., Dou X. Danshen protects against early-stage alcoholic liver disease in mice via inducing PPARalpha activation and subsequent 4-HNE degradation. PLoS ONE. 2017;12:e0186357. doi: 10.1371/journal.pone.0186357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Yue S., Hu B., Wang Z., Yue Z., Wang F., Zhao Y., Yang Z., Shen M. Salvia miltiorrhiza compounds protect the liver from acute injury by regulation of p38 and NFkappaB signaling in Kupffer cells. Pharm. Biol. 2014;52:1278–1285. doi: 10.3109/13880209.2014.889720. [DOI] [PubMed] [Google Scholar]
- 190.Zhang N., Hu Y., Ding C., Zeng W., Shan W., Fan H., Zhao Y., Shi X., Gao L., Xu T., et al. Salvianolic acid B protects against chronic alcoholic liver injury via SIRT1-mediated inhibition of CRP and ChREBP in rats. Toxicol. Lett. 2017;267:1–10. doi: 10.1016/j.toxlet.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 191.Kang O.H., Kim S.B., Mun S.H., Seo Y.S., Hwang H.C., Lee Y.M., Lee H.S., Kang D.G., Kwon D.Y. Puerarin ameliorates hepatic steatosis by activating the PPARalpha and AMPK signaling pathways in hepatocytes. Int. J. Mol. Med. 2015;35:803–809. doi: 10.3892/ijmm.2015.2074. [DOI] [PubMed] [Google Scholar]
- 192.Xiong Y., Yang Y., Yang J., Chai H., Li Y., Yang J., Jia Z., Wang Z. Tectoridin, an isoflavone glycoside from the flower of Pueraria lobata, prevents acute ethanol-induced liver steatosis in mice. Toxicology. 2010;276:64–72. doi: 10.1016/j.tox.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 193.Zhao Y.Z., Zhang L., Gupta P.K., Tian F.R., Mao K.L., Qiu K.Y., Yang W., Lv C.Z., Lu C.T. Using PG-Liposome-Based System to Enhance Puerarin Liver-Targeted Therapy for Alcohol-Induced Liver Disease. Aaps. Pharmscitech. 2016;17:1376–1382. doi: 10.1208/s12249-015-0427-5. [DOI] [PubMed] [Google Scholar]
- 194.Jin H., Lian N., Bian M., Zhang C., Chen X., Shao J., Wu L., Chen A., Guo Q., Zhang F., et al. Oroxylin A prevents alcohol-induced hepatic steatosis through inhibition of hypoxia inducible factor 1alpha. Chem. Biol. Interact. 2018;285:14–20. doi: 10.1016/j.cbi.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 195.Li H.D., Chen X., Yang Y., Huang H.M., Zhang L., Zhang X., Zhang L., Huang C., Meng X.M., Li J. Wogonin attenuates inflammation by activating PPAR-gamma in alcoholic liver disease. Int. Immunopharmacol. 2017;50:95–106. doi: 10.1016/j.intimp.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 196.Wang H., Zhang Y., Bai R., Wang M., Du S. Baicalin Attenuates Alcoholic Liver Injury through Modulation of Hepatic Oxidative Stress, Inflammation and Sonic Hedgehog Pathway in Rats. Cell. Physiol. Biochem. 2016;39:1129–1140. doi: 10.1159/000447820. [DOI] [PubMed] [Google Scholar]
- 197.Ghoneim A.I. Effects of curcumin on ethanol-induced hepatocyte necrosis and apoptosis: Implication of lipid peroxidation and cytochrome c. Naunyn. Schmiedebergs. Arch. Pharm. 2009;379:47–60. doi: 10.1007/s00210-008-0335-2. [DOI] [PubMed] [Google Scholar]
- 198.Lu C., Zhang F., Xu W., Wu X., Lian N., Jin H., Chen Q., Chen L., Shao J., Wu L., et al. Curcumin attenuates ethanol-induced hepatic steatosis through modulating Nrf2/FXR signaling in hepatocytes. Iubmb. Life. 2015;67:645–658. doi: 10.1002/iub.1409. [DOI] [PubMed] [Google Scholar]
- 199.Nanji A.A., Jokelainen K., Tipoe G.L., Rahemtulla A., Thomas P., Dannenberg A.J. Curcumin prevents alcohol-induced liver disease in rats by inhibiting the expression of NF-kappa B-dependent genes. Am. J. Physiol. Gastrointest. Liver Physiol. 2003;284:G321–G327. doi: 10.1152/ajpgi.00230.2002. [DOI] [PubMed] [Google Scholar]
- 200.Wang Y., Zhang Z., Wang X., Qi D., Qu A., Wang G. Amelioration of Ethanol-Induced Hepatitis by Magnesium Isoglycyrrhizinate through Inhibition of Neutrophil Cell Infiltration and Oxidative Damage. Mediat. Inflamm. 2017;2017:3526903. doi: 10.1155/2017/3526903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lu C., Xu W., Shao J., Zhang F., Chen A., Zheng S. Blockade of hedgehog pathway is required for the protective effects of magnesium isoglycyrrhizinate against ethanol-induced hepatocyte steatosis and apoptosis. Iubmb. Life. 2017;69:540–552. doi: 10.1002/iub.1639. [DOI] [PubMed] [Google Scholar]
- 202.Jung J.C., Lee Y.H., Kim S.H., Kim K.J., Kim K.M., Oh S., Jung Y.S. Hepatoprotective effect of licorice, the root of Glycyrrhiza uralensis Fischer, in alcohol-induced fatty liver disease. BMC Complement. Altern. Med. 2016;16:19. doi: 10.1186/s12906-016-0997-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhang P., Ma D., Wang Y., Zhang M., Qiang X., Liao M., Liu X., Wu H., Zhang Y. Berberine protects liver from ethanol-induced oxidative stress and steatosis in mice. Food Chem. Toxicol. 2014;74:225–232. doi: 10.1016/j.fct.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 204.Lu C., Xu W., Shao J., Zhang F., Chen A., Zheng S. Nrf2 Activation Is Required for Ligustrazine to Inhibit Hepatic Steatosis in Alcohol-Preferring Mice and Hepatocytes. Toxicol. Sci. 2017;155:432–443. doi: 10.1093/toxsci/kfw228. [DOI] [PubMed] [Google Scholar]
- 205.Patsenker E., Chicca A., Petrucci V., Moghadamrad S., de Gottardi A., Hampe J., Gertsch J., Semmo N., Stickel F. 4-O’-methylhonokiol protects from alcohol/carbon tetrachloride-induced liver injury in mice. J. Mol. Med. (Berl) 2017;95:1077–1089. doi: 10.1007/s00109-017-1556-y. [DOI] [PubMed] [Google Scholar]
- 206.Lee J.H., Jung J.Y., Jang E.J., Jegal K.H., Moon S.Y., Ku S.K., Kang S.H., Cho I.J., Park S.J., Lee J.R., et al. Combination of honokiol and magnolol inhibits hepatic steatosis through AMPK-SREBP-1 c pathway. Exp. Biol. Med. (Maywood) 2015;240:508–518. doi: 10.1177/1535370214547123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lucey M.R. Liver transplantation for alcoholic liver disease. Nat. Rev. Gastroenterol. Hepatol. 2014;11:300–307. doi: 10.1038/nrgastro.2013.247. [DOI] [PubMed] [Google Scholar]