Abstract
Context:
There is an ever-increasing trend toward sports, fitness, and recreation activities, so the incidence of anterior cruciate ligament sports injuries has increased. Perhaps the greatest challenge for sports clinicians is to return the injured athlete back to his/her original sport at an even greater level of functional ability than preinjury. For this, rigorous and well-researched criteria are needed.
Evidence Acquisition:
Using medical subject headings and free-text words, an electronic search was conducted up to October 2018. Subject-specific search was based on the terms return to play and return to sport in combination with guidelines, criteria, and anterior cruciate ligament reconstruction.
Study Design:
Descriptive review.
Level of Evidence:
Level 2.
Results:
Five principal criteria were found, including psychological factors, performance/functional tests, strength tests, time, and modifiable and nonmodifiable risk factors.
Conclusion:
The psychological readiness of the player is a major factor in successful safe return to sport (SRTS) decision making. Although strength, performance, and functional tests presently form the mainstay of SRTS criteria, there exists very little scientific evidence for their validity. More protection should be provided to athletes with known risk factors. Movement quality is important, if not more important than the quantifiable measures. As a result of the significantly high rerupture rate in young individuals, delayed SRTS should be considered preferably beyond 9 months postsurgery.
Keywords: ACL reconstruction, return to sport criteria, clinical decision making
The 2016 physical activity participation report,32 which tracked sports, fitness, and recreation participation in the United States, revealed an increasing trend in the casual sports activity population, rising from 8.4% in 2010 to 12.8% in 2015. This represents a 52% increase over this 5-year period. As sports participation increases, so does the number of sports injuries.
Anterior cruciate ligament (ACL) injuries are frequent in sports, particularly in female athletes,20 and the injury rates continue to rise in men’s and women’s soccer. Every year, about 3% of amateur athletes injure their ACL.22 For elite athletes, this percentage is as high as 15%.22 Controlling for exposures, there were statistically significant increases in the average annual number of ACL injuries for men’s and women’s basketball, ice hockey, field hockey, football, and volleyball for the 2004-2005 through 2012-2013 playing seasons.2 Women continue to sustain ACL injuries at higher rates than men in the comparable sports of soccer, basketball, and lacrosse.2,34 Many of these athletes undergo ACL reconstruction. In the United States, for example, approximately 250,000 ACL reconstructions (ACLRs) are performed annually.11,24
This increase in sports activity has heightened the awareness of safe return to sport (SRTS), culminating in the first World Return to Sport Congress in Sports Physical Therapy in Bern, Switzerland, in 2015. Seventeen expert clinicians participated with an audience of over 800 clinicians from 65 countries. As a result of this meeting, a new consensus statement on return to play (RTP) or “return to sport” (RTS) was published.5 Included was a discussion on the definition of RTS and the proposition of a framework that incorporates the Strategic Assessment of Risk and Risk Tolerance (StARRT) step model (http://bjsm.bmj.com) as well as the biopsychosocial model with appropriate load management.
Successful SRTS may be defined as the ability to play a competitive match at the preinjury level.7,9 Although the optimal return to competition for most athletes requires the absence of functional limitations, some athletes continue to participate in functionally challenging activities, and even compete at a high level, despite major functional complaints.7 There are several studies that have identified RTS criteria post-ACLR.5,7,13,19,21,40 While there are several guidelines, there is limited evidence for parameters that influence or predict the final result of ACLR rehabilitation and RTP.41
In a recent study,19 patients performed a standardized test battery at 2 time periods after ACL reconstruction. Eighty-four percent (n = 79) were not ready to return to either recreational sports or competitive sports at 5.7 months. At 8 months, only 1 of the 95 patients was ready to return to competitive sports and 28 (30%) to recreational sports. Competing with inadequate preparation may increase the risk of secondary injury.47 Those who return to level 1 sports (pivot and contact sports) have a 4.68 times higher risk of knee reinjury than those who do not return to sporting activities.17 ACL rerupture may result in accelerated deterioration of knee function and progression of osteoarthritis.3,33
Post-ACLR rehabilitation should be a graded progression and should include interventions besides sports-specific training. This is imperative in the decision-making process. The RTS process will involve a prolonged time period and should involve careful observation. Blanchard and Glasgow,10 for example, have provided an exercise progression model during this process, commencing with hopping and progressing to forward motion activities, including hurdles and perturbation.
ACL rerupture rate has remained between 4.5% and 11%, but may be significantly higher, even up to 50% within the first postoperative year.20 This, despite the fact that current rehabilitation programs after ACLR are more aggressive than those utilized in the 1980s, emphasizing immediate weightbearing, range of motion, progressive muscular strengthening, proprioception, dynamic stability, and neuromuscular control drills.7,17
Although the incidence of reinjury is not as high as that of ankle sprains, for example, the severity of the reinjury creates a serious problem for the returning athlete.42,43 The rate of revision surgery has increased more than primary repairs.20,48 Among female participants undergoing reconstruction with autograft hamstring, a contralateral harvest predicted a more than 3 times higher 5-year risk of contralateral ACL reconstruction.4 It remains unclear whether this is a result of insufficient rehabilitation, RTS criteria, or simply the fact that athletes return too soon, therefore exposing themselves to a possible 50% reinjury rate within the first postoperative year.20 The athlete should only return back to sport safely, with the risk of reinjury approximating the risk for primary injury. However, in most cases, the athlete’s preinjury status is unknown.
Although this subject is broad, the aim is to provide highlights of the current researched criteria regarding SRTS after ACLR.
Method
Search Strategy
A computerized, bibliographic database search within the medical and rehabilitation literature was carried out. The following databases were searched from their inception to May 2018: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBase, CINAHL, and the Musculoskeletal Injuries Group’s specialized register. Subject-specific search was based on the terms return to play and return to sport in combination with guidelines, criteria, and anterior cruciate ligament reconstruction. The search was restricted to studies including humans only and those published in English. The reference list of relevant articles was also reviewed to find additional publications not identified in the formal search strategy.
Results
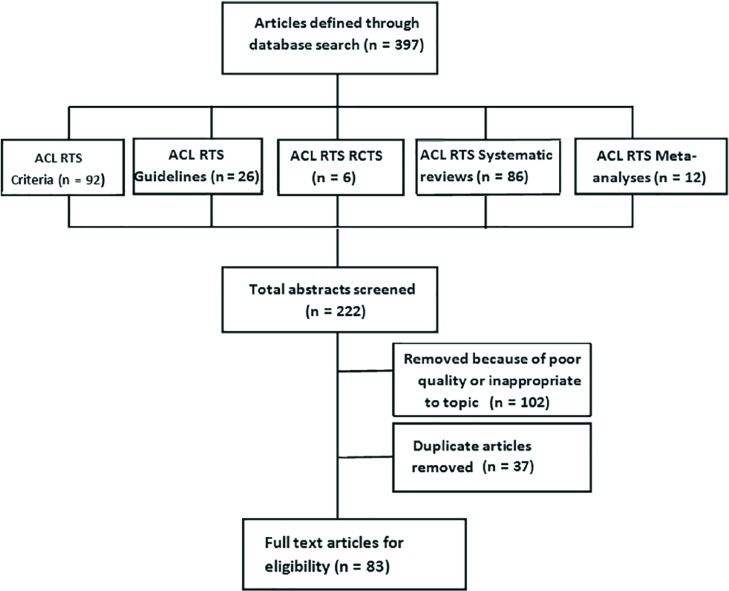
The results of the literature search are summarized in the flow diagram (Figure 1). The search led to 397 articles. Of these, 222 were related to ACL RTS criteria and guidelines. One hundred two articles were excluded as they were of poor research quality (level 4, 5, or foundational evidence) or they were not directly related to the topic. Once the 37 duplicates were removed, a total of 83 potential articles remained.
Figure 1.
Flowchart showing the anterior cruciate ligament (ACL) return to sport (RTS) literature search.
The results of the search revealed 5 main RTS criteria, all of which are purposely depicted as being interrelated (Figure 2).
Figure 2.
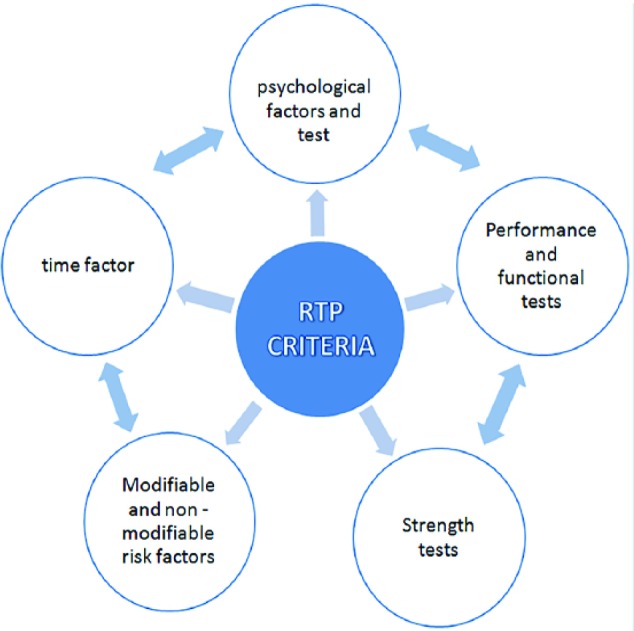
Categories related to return to play (RTP).
Discussion
Psychological Factors
Over the past few years, patient psychology has become a dominant issue relating to SRTS research. Psychological readiness of the player and kinesiophobia as identified in RTS and the whole rehabilitation process has recently received greater attention and is known to be associated with poorer outcomes.28,44
In fact, several studies showed that when athletes were asked about returning to their previous sporting activity, a high percentage expressed fear of new injury, repeated injury, and lack of trust in the knee.6 Indeed, in a study of RTS after ACL rupture, the main reasons patients did not RTS were not trusting the knee (28%), fear of a new injury (24%), and poor knee function (22%).7 Psychological readiness for RTS was the factor most strongly associated with returning to the preinjury activity. Athletes who were more psychologically ready to RTP were more likely to return to their preinjury level, RTP faster, and perceive superior performance on RTP.6 Psychological interventions during postoperative rehabilitation were capable of improving the rate of RTP.6 A high self-efficacy, a high internal locus of control, and a low level of fear were also associated with a higher chance of RTP.15,40
In a recent study, female patients had a more negative outlook and therefore potentially benefited more from interventions designed to facilitate a smooth transition back to sport.49 Physical and psychological readiness to return to sport were seen typically as not necessarily coinciding.6 In patients with elevated kinesiophobia, cognitive training may be needed before initiating movement retraining or other exercises to improve landing mechanics. Additional prospective studies are needed to assess if these relationships improve over time and determine the optimal time to intervene to reduce subsequent injury risk.28
Performance and Functional Tests
Most emphasis regarding RTP has traditionally been placed on the hop tests, which have become the mainstay of performance tests prior to returning the athlete to sport.27 Over the past few years, variations of classical hop tests have been added: the drop jump test, side hop test, and vertical hop test.12,17 The literature typically describes clinical assessments conducted in an organized and comprehensive manner at various periods during the rehabilitation process. This includes the battery of hop tests at 6, 8, and 10 months postoperatively.14,18,19 Although sparse evidence supports performance or functional tests,22 a battery of tests at discharge is a good tool for evaluating SRTS in ACLR patients.21 Athletes who did not meet the discharge criteria before returning to professional sport had a 4 times greater risk of sustaining an ACL graft rupture compared with those who met all 6 RTS criteria.21 Only 5.6% of patients who successfully passed RTS criteria before returning to level 1 sports suffered reinjuries compared with 37.5% who did not.17
More recently, attention has been placed not only on the ability of the injured athlete to perform these tests successfully but also on impairment-based measures and the quality of movement while performing these tests.22 Laboratory-based 3-dimensional (3D) motion capture systems are helpful in the evaluation of biomechanical risk factors.16 Functional tasks can accurately determine multiplanar and dimensional kinematics, including rotational forces across joints. However, 3D motion capture systems have limited application in the clinical setting.25 Electromagnetic sensors do not always relate well to the performance of functional tasks and are difficult to incorporate into preseason screenings.26,36 Although movement quality may affect the ACL (re)injury rate, there is a lack of focus on the evaluation and training of the quality of movement as a measurement of neuromuscular recovery.37 Qualitative scoring systems such as the Jump Landing System8 and Landing Error Scoring System29,30,39 have been developed, but it is still unclear how quality of movement plays a role in the occurrence of ACL reinjuries.1,8,9,23,33 There should be a gradual increase in sports-specific training without pain, effusion, or fear of reinjury. The restoration of impaired flexion-adduction moments may take more than 5 years, and it may take more than a year for normal gait patterns to be restored.31
The Limb Symmetry Index (LSI) has been widely utilized as a measurement of the readiness to RTS. Clinically accepted LSI values are usually >90%.14 This >90% rule is highly questionable because performance tests may be neither demanding nor sensitive enough to accurately identify differences between the injured and noninjured sides.2
The accepted criteria regarding muscle strength measurements include >90% strength results as opposed to the nonoperative side.14 Whether these values are enough to return the player to sport safely is unknown. Unfortunately, hamstring and quadriceps weakness continues up to 2 years and beyond surgery.17 It has therefore been suggested that muscle strength tests be conducted both preoperatively as well as 6, 8, and 10 months postoperatively.14,19 It may in fact not be individual muscle strength that is a factor as much as a decreased hamstring to quadriceps ratio.20
Time
The ACL reinjury rate was significantly reduced by 51% for each month RTS was delayed until 9 months after surgery, after which no further risk reduction was observed.17 Using this simple rule, it is possible to reduce the risk of second injury by 84%. This new information provides clear evidence that the RTS decision after ACLR should preferably be delayed from the current 4- to 6-month period, to at least 9 months postsurgery.19 Interestingly, when magnetic resonance imaging studies are examined, a high percentage of players still exhibit observable abnormalities after muscle injury.38 If the RTS decision is delayed after certain soft tissue injuries and these muscle abnormalities do not exist, the risk of further injury is reduced.38
Nonmodifiable and Modifiable Risk Factors
Although numerous risk factors may be modifiable, many are not. Those that are not may include a previous ipsilateral ACLR tear, age, and ethnicity.7 All these elements should be taken into account when returning the injured athlete to sport. In some cases, added protection should be considered, for example adding rehabilitation time before returning the adolescent player to sport.35 What is of most concern is the evidence of increasing incidence of ACLR in younger patients.23,35,49 This is a growing public health burden and has potential ramifications for long-term health outcomes. Although 96% of young athletes are able to RTS at the same skill level after ACLR, these individuals face a significantly increased risk of revision ACL surgery.49 Those aged younger than 20 years have a 6.3 times risk increase of rerupture as opposed to those older than 20 years, and as many as 35% of these younger patients have a second injury.45 Combined data indicate that nearly 1 in 4 young athletic patients who sustain an ACL injury and return to high-risk sport will go on to sustain another ACL injury at some point in their career, and they will likely sustain it early in the RTP period.45,46
Conclusion
The greatest challenge for sports clinicians is how to return the athlete back to his/her original sport at an even greater level of functional ability, thereby significantly reducing the possibility of reinjury. For the athlete, it may be a return to sustained participation in sport in the shortest possible time. For the athletic trainer, it may be the athlete’s performance level when returning to sport. For the clinician, the prevention of new or recurring injuries may be the ultimate goal of success.13 Good communication between clinicians is of great importance. Whatever the expectation, the RTS decision should preferably be made as a collaborative decision between all those involved. Therefore, close communication is of great importance.
The psychological readiness of the player is a major factor in successful RTS decision making. A high self-efficacy, a high internal locus of control, and a low level of fear are associated with a higher chance of RTP. Despite the wide usage of strength, performance, and functional tests as part of the RTS process, there is very little scientific evidence for their validity. There is preliminary evidence that a battery of tests at discharge is a good tool for evaluating SRTS in ACLR patients. As a result of the significantly high rerupture rate in young individuals, great emphasis must be placed on their delayed RTS, with recent evidence showing that the RTS decision after ACLR should be preferably delayed to at least 9 months postsurgery in all population groups.
Acknowledgments
The authors would like to thank Miss Elana Tiberi, BFA, and Miss Courtney Hersch for their editing assistance in preparing this article. The authors would like to thank Miss Megan Quinn for her assistance in the editing and reviewing of this article.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Aerts I, Cumps E, Verhagen E, et al. Efficacy of a 3 month training program on the jump-landing technique in jump-landing sports. Design of a cluster randomized controlled trial. BMC Musculoskelet Disord. 2010;11:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: national collegiate athletic association injury surveillance system data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26:518-523. [DOI] [PubMed] [Google Scholar]
- 3. Amoako AO, Pujalte GGA. Osteoarthritis in young, active, and athletic individuals. Clin Med Insights Arthritis Musculoskelet Disord. 2014;7:27-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Andernord D, Desai N, Björnsson H, Gillén S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction: a cohort study of 9061 patients with 5-year follow-up. Am J Sports Med. 2015;43:295-302. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in sports physical therapy, Bern. Br J Sports Med. 2016;50:853-864. [DOI] [PubMed] [Google Scholar]
- 6. Ardern CL, Taylor NF, Feller JA, Webster KE. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47:1120-1126. [DOI] [PubMed] [Google Scholar]
- 7. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [DOI] [PubMed] [Google Scholar]
- 8. Bell DR, Smith MD, Pennuto AP, Stiffler MR, Olson ME. Jump-landing mechanics after anterior cruciate ligament reconstruction: a landing-error scoring system study. J Athl Train. 2014;49:435-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bien DP, Dubuque TJ. Considerations for late stage ACL rehabilitation and return to sport to limit re-injury risk and maximize athletic performance. Int J Sports Phys Ther. 2015;10:256-271. [PMC free article] [PubMed] [Google Scholar]
- 10. Blanchard S, Glasgow P. A theoretical model to describe progressions and regressions for exercise rehabilitation. Phys Ther Sport. 2014;15:131-135. [DOI] [PubMed] [Google Scholar]
- 11. Buller LT, Best MB, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3:2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cesar GM, Tomasevicz CL, Burnfield JM. Frontal plane comparison between drop jump and vertical jump: implications for the assessment of ACL risk of injury. Sports Biomech. 2016; 15:440-449. [DOI] [PubMed] [Google Scholar]
- 13. Dijkstra HP, Pollock N, Chakraverty R, Ardern CL. Return to play in elite sport: a shared decision-making process. Br J Sports Med. 2016;51:419-420. [DOI] [PubMed] [Google Scholar]
- 14. Eitzen I, Moksnes H, Snyder-Mackler L, Engebretsen L, Risberg MA. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1517-1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:752-762. [DOI] [PubMed] [Google Scholar]
- 16. Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sport Exerc. 2007;39:2021-2028. [DOI] [PubMed] [Google Scholar]
- 17. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hatton AL, Crossley KM, Clark RA, Whitehead TS, Morris HG, Culvenor AG. Between-leg differences in challenging single-limb balance performance one year following anterior cruciate ligament reconstruction. Gait Posture. 2016;52:22-25. [DOI] [PubMed] [Google Scholar]
- 19. Hildebrandt C, Müller L, Zisch B, Huber R, Fink C, Raschner C. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part I: development of a new test battery. Knee Surg Sports Traumatol Arthrosc. 2015;23:1273-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36:1-8. [DOI] [PubMed] [Google Scholar]
- 21. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946-951. [DOI] [PubMed] [Google Scholar]
- 22. Mayer SW, Queen RM, Taylor D, et al. Functional testing differences in anterior cruciate ligament reconstruction patients released versus not released to return to sport. Am J Sports Med. 2015;43:1648-1655. [DOI] [PubMed] [Google Scholar]
- 23. McCarthy M, Dodwell E, Pan T, Green DW. Long-term follow-up of pediatric ACL reconstruction in New York State: high rates of subsequent ACL reconstruction. Orthop J Sports Med. 2015;3:2325967115S00129. [Google Scholar]
- 24. Moses B, Orchard J, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med. 2012;20:157-179. [DOI] [PubMed] [Google Scholar]
- 25. Munro A, Herrington L, Carolan M. Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. J Sport Rehabil. 2012;21:7-11. [DOI] [PubMed] [Google Scholar]
- 26. Nakagawa TH, Uehara Moriya ET, Maciel CD, Serrao FV. Test-retest reliability of three-dimensional kinematics using an electromagnetic tracking system during single-leg squat and stepping maneuver. Gait Posture. 2014;39:141-146. [DOI] [PubMed] [Google Scholar]
- 27. Neeter C, Gustavsson A, Thomeé P, Augustsson J, Thomeé R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:571-580. [DOI] [PubMed] [Google Scholar]
- 28. Noehren B, Kline P, Ireland ML, Johnson DL. Kinesiophobia is strongly associated with altered loading after an ACL reconstruction: implications for re-injury risk. Orthop J Sports Med. 2017;5(7)(suppl 6):2325967117S00323. [Google Scholar]
- 29. Padua DA, Boling MC, DiStefano LJ, Onate JA, Beutler AI, Marshall SW. Reliability of the landing error scoring system-real time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehabil. 2011;20:145-156. [DOI] [PubMed] [Google Scholar]
- 30. Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50:589-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Paulos L, Noyes FR, Grood E, Butler DL. Knee rehabilitation after anterior cruciate ligament reconstruction and repair. J Orthop Sports Phys Ther. 1991;13:60-70. [DOI] [PubMed] [Google Scholar]
- 32. Physical Activity Council. 2019. Physical Activity Council’s overview report on U.S. participation. http://www.physicalactivitycouncil.com/pdfs/current.pdf. Accessed February 11, 2019.
- 33. Paradowski PT, Englund M, Lohmander LS, Roos EM. The effect of patient characteristics on variability in pain and function over two years in early knee osteoarthritis. Health Qual Life Outcomes. 2005;3:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Saper M, Pearce S, Shung J, Zondervan R, Ostrander R, Andrews JR. Outcomes and return to sport after revision anterior cruciate ligament reconstruction in adolescent athletes. Orthop J Sports Med. 2018;6:2325967118764884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shurr S, Marshall A, Resch J, Saliba S. Two-dimensional video analysis is comparable to 3D motion capture in lower extremity movement assessment. Int J Sports Phys Ther. 2017;12:163-172. [PMC free article] [PubMed] [Google Scholar]
- 37. Sigward SM, Lin P, Pratt K. Knee loading asymmetries during gait and running in early rehabilitation following anterior cruciate ligament reconstruction: a longitudinal study. Clin Biomech (Bristol, Avon). 2016;32:249-254. [DOI] [PubMed] [Google Scholar]
- 38. Silder A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43:284-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40:521-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798-1805. [DOI] [PubMed] [Google Scholar]
- 41. van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506-1515. [DOI] [PubMed] [Google Scholar]
- 42. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279-2284. [DOI] [PubMed] [Google Scholar]
- 43. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827-2832. [DOI] [PubMed] [Google Scholar]
- 44. Webster KE, Nagelli CV, Timothy E, Hewett TE. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46:1545-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wierike SC, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2012;23:527-540. [DOI] [PubMed] [Google Scholar]
- 46. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42:153-171. [DOI] [PubMed] [Google Scholar]
- 48. Yabroudi MA, Björnsson H, Lynch AD, et al. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sports Med. 2016;4:2325967116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians. Med J Aust. 2018;208:354-358. [DOI] [PubMed] [Google Scholar]