Abstract
Objective:
Pregnancy-induced nausea and vomiting are common maladies during early pregnancy and may be related to physical activity (PA). Our objective was to determine relations among work-related PA (work PA), leisure-time physical activity (LTPA), and nausea during the first trimester.
Study design:
Online or mailed surveys with questions on pregnancy-related nausea, work PA, and LTPA were completed by 70 women at 15 to 30 months postpartum. Women recalled nausea during the first trimester (none, ≤1 h/d, 2-3 h/d, 4-6 h/d, ≥6 h/d) as well as LTPA frequency, duration, and type. Women also recalled total working hours in their first trimester and percentage of time sitting, standing, and walking at work.
Results:
A total of 42 women (60%) were categorized as having high nausea (≥2 h/d). Mann-Whitney U tests showed that women with low nausea had significantly more MET minutes per week of LTPA (P = .05) and hours per week spent standing at work (P = .03). Logistic regression analyses showed standing for ≥20 h/wk at work was related to reduced odds of high nausea (adjusted odds ratio = 0.23; 95% CI = 0.06-0.96), whereas meeting LTPA guidelines was nonsignificantly related to reduced odds.
Conclusion:
These findings suggest an inverse relationship between first trimester PA and level of nausea. Further investigation is needed to determine the directionality of these relations.
Keywords: pregnant women, nausea, work physical activity, leisure-time physical activity
‘Whereas some pregnant women experience only minor levels of nausea and the occasional urge to vomit, others experience physically and psychologically debilitating symptoms.‘
Introduction
Pregnancy-induced nausea and vomiting are experienced by 75% to 80% of pregnant women,1,2 with the majority of cases resolving by the end of the first or early in the second trimester.2,3 Whereas some pregnant women experience only minor levels of nausea and the occasional urge to vomit, others experience physically and psychologically debilitating symptoms. Indeed, higher levels of nausea and vomiting during pregnancy may result in reduced health-related quality of life,4 an inability to complete daily activities or tasks,5 and possibly a negative impact on immediate family relationships.6 The most severe form of pregnancy-induced nausea, hyperemesis gravidarum, is experienced by 0.5% to 2% of pregnant women7,8 and is characterized by severe dehydration, electrolyte imbalance, and possible hospitalization. This condition can result in low weight gain, renal failure, jaundice, and depression for the expectant mother and early delivery, low birth weight, and low APGAR scores for the baby.9,10 Unfortunately, the underlying cause of nausea and vomiting during pregnancy is unknown, with the existing evidence indicating some combination of biological, psychological, and environmental factors.11
Depending on the level of severity, nausea and vomiting during pregnancy may impede the expectant mother’s ability to perform important health behaviors, such as leisure-time physical activity (LTPA). Pregnant women have previously reported nausea and vomiting as a barrier to LTPA, particularly during the first trimester.12-14 Owe et al15 sampled pregnant women from the population-based Norwegian Mother and Child Cohort and found those who experienced any nausea were 22% less likely to participate in regular exercise (as defined by frequency). However, neither exercise intensity nor severity of nausea were reported as a part of these investigations. The lay press has often suggested that regular PA may even reduce feelings of nausea during pregnancy, although this hypothesis has received very little consideration within the scientific literature. Findings from a single qualitative investigation have indicated that pregnant women’s perceived nausea may be reduced with outdoor activity as compared with gym-based exercise.16 It is evident that the relationship between pregnancy-induced nausea and LTPA lacks clarity at this time. Moreover, the relationship of nausea/vomiting to a pregnant woman’s occupation activity (work PA) has not been considered in previous research investigations. A more precise examination of these relationships could indicate the true impact of nausea and vomiting on women’s PA behaviors and, thereby, provide researchers and clinicians with information critical in developing effective early-pregnancy PA interventions. Therefore, the objective of this investigation was to determine the relationships for both LTPA and work-related PA with level of nausea among first-trimester pregnant women. We hypothesized that meeting the current LTPA guidelines would be related to lower levels of nausea. We also hypothesized that women who have lower levels of nausea would engage in more standing and walking at work.
Methods
Participants
This investigation is a part of the Physical Activity during Pregnancy and Offspring Size Study (PAPOS), which recruited 311 pregnant women from 9 prenatal care clinics in 2006.17 Women who were currently pregnant, at their first prenatal care visit, 18 to 50 years old, and proficient in English or Spanish were eligible. Of the original cohort, 298 provided contact information for follow-up and were contacted 15 to 30 months postpartum to complete a mailed or online survey containing questions with respect to LTPA, work PA, gestational weight gain, reproductive health, nausea level, and basic demographics. A total of 86 surveys were returned to study investigators (29% response rate), with 70 containing complete data (23% of potential participants). This study was approved by the Michigan State University Institutional Review Board, and women signed informed consent at both enrollment and follow-up.
Variables
The survey consisted of questions on various participant demographics, including race, education, income, relationship status, occupation, pregnancy history, smoking, and alcohol consumption. Participant anthropometric characteristics, including maternal weight, height, and gestational weight gain, were self-reported. These were used to determine whether participants met the Institute of Medicine weight gain guidelines for pregnant women.18 Participants were also asked to report their nausea-related treatment, specifically whether they used prescribed or nonprescribed medication as well as whether they required nausea-related hospitalization.
Pregnancy-induced nausea was assessed using questions derived from the Pregnancy Unique Quantification of Emesis Scale (PUQE), a scoring system used to assess the severity of nausea and vomiting symptoms among pregnant women.19 The PUQE scale has demonstrated excellent predictive validity among various clinical aspects of pregnancy-induced nausea, including women’s self-reported scores of well-being, emergency room visits, and ability to ingest multivitamins.20 Each participant was asked to recall how often she had feelings of nausea per day during the first trimester. Possible responses to this question were the following: not at all, ≤1, 2 to 3, 4 to 6, or ≥6 h/d. As a result of the distribution of responses in this investigation, first-trimester nausea was categorized as “high” (≥2 h/d) or “low” (≤1 h/d).
Survey questions with respect to LTPA and work PA were adapted slightly from the Modifiable Activity Questionnaire, which has been validated for pregnancy-related recall up to 6 years postpartum.21 Participants reported their LTPA by recalling frequency, duration, and type of LTPA participated in during a typical first-trimester week. MET minutes per week of LTPA was then calculated for each participant. Because of the nonparametric nature of the PA data, LTPA was categorized for each trimester as meeting guidelines22 (≥150 min/wk) or not (<150 min/wk). Participants were also asked to recall total working hours in their first trimester and percentage of time sitting, standing, and walking at work. This allowed for the hours per week of sitting, standing, and walking at work to be calculated. Each type of activity was categorized as low (<10 h/wk), moderate (10-20 h/wk), or high (>20 h/wk).
Statistical Analyses
Descriptive statistics (eg, frequencies, means, medians) were calculated for all variables of interest. Because variables were nonnormally distributed, Mann-Whitney U tests were performed to compare the distribution of continuous variables of LTPA and work PA between high- and low-nausea women. χ2 Analyses were used to compare the frequency of meeting LTPA guidelines and categories of work PA between high- and low-nausea women. Logistic regression analyses were then performed to determine how both LTPA and work PA related to odds of high nausea. Total time spent at work, time spent standing, physician-instructed bed rest, and use of antinausea medication were all entered as covariates within the LTPA/nausea analyses, whereas total time spent at work, having met the LTPA guideline, physician-instructed bed rest, and use of antinausea medication were adjusted for in determining the relationship between work PA and nausea. All statistical analyses were performed using SPSS version 20.0 software (SPSS Inc, Chicago, IL).
Results
The analytic sample was predominantly white (87%), with approximately 93% having received at least a high school education and about half being nulliparous (54%; Table 1). A total of 42 women (60%) were categorized as having high nausea (≥2 h/d of nausea/vomiting). High-nausea women were less likely to report smoking prepregnancy or in the first trimester, and were also less likely to report drinking alcohol in the first trimester (P < .05); otherwise participant characteristics did not differ by nausea status. High-nausea women were more likely to take medication (P < .001) and use nondrug treatments (P = .002) compared with low-nausea women to combat their nausea (Table 2). Additionally, high-nausea women were more likely to experience nausea after the first trimester (P < .001).
Table 1.
Demographic Characteristics Among High- and Low-Nausea Pregnant Women.a
| Total (n = 70) | High Nauseab (n = 42) | Low Nausea (n = 28) | χ2 P Value | |
|---|---|---|---|---|
| Education | ||||
| ≤High school | 5 (7.1) | 3 (7.1) | 2 (7.1) | 1.000 |
| >High school | 65 (92.9) | 39 (92.9) | 26 (92.9) | |
| Income | ||||
| <$50 000 | 23 (32.9) | 13 (31.0) | 10 (35.7) | .678 |
| ≥$50 000 | 47 (67.1) | 29 (69.1) | 18 (64.3) | |
| Race | ||||
| White | 61 (87.1) | 36 (85.7) | 25 (89.3) | .732 |
| Nonwhite | 9 (12.9) | 6 (14.3) | 3 (10.7) | |
| Relationship status | ||||
| Married/Cohabitating | 61 (87.1) | 39 (92.9) | 22 (78.6) | .247 |
| Single | 9 (12.9) | 4 (9.5) | 5 (17.9) | |
| Primary job | ||||
| Specified occupation | 48 (68.6) | 29 (69.0) | 19 (67.9) | .916 |
| Homemaker | 22 (31.4) | 13 (31.0) | 9 (32.1) | |
| Parity | ||||
| Nulliparous | 38 (54.3) | 25 (59.5) | 13 (46.4) | .281 |
| Parous | 32 (45.7) | 17 (40.5) | 15 (53.6) | |
| Baby’s gender | ||||
| Male | 36 (51.4) | 20 (47.6) | 16 (57.1) | .345 |
| Female | 34 (48.6) | 22 (52.4) | 12 (42.9) | |
| Smoking | ||||
| Any prepregnancy | 15 (21.4) | 5 (11.9) | 10 (35.7) | .017c |
| Any first trimester | 8 (11.4) | 1 (2.4) | 7 (25.0) | .006c |
| Alcohol | ||||
| Any prepregnancy | 45 (64.3) | 27 (64.3) | 18 (64.3) | 1.000 |
| Any first trimester | 9 (12.9) | 2 (4.7) | 7 (25.0) | .025c |
| Prepregnancy body mass index | ||||
| <25 kg/m2 | 56 (80.0) | 33 (78.6) | 23 (82.1) | .678 |
| ≥25 kg/m2 | 14 (20.0) | 9 (21.4) | 5 (17.9) | |
| Met pregnancy weight gain recommendations | ||||
| Yes | 28 (40.0) | 17 (40.5) | 11 (39.3) | .921 |
| No | 42 (60.0) | 25 (59.5) | 17 (60.7) | |
Frequency (%).
High nausea defined as ≥2 h/d of feeling nauseous or vomiting.
Significant difference comparing high-nausea and low-nausea women (P value <.05).
Table 2.
Nausea-Related Characteristics of High and Low-Nausea Pregnant Women.a
| Total (n = 70) | High Nauseab (n = 42) | Low Nausea (n = 28) | P Value | |
|---|---|---|---|---|
| Reported no medication use | 52 (74.3) | 25 (59.5) | 27 (96.4) | .001c |
| Reported over-counter medication use | 16 (22.9) | 15 (35.7) | 1 (3.6) | .001c |
| Reported prescribed medication use | 6 (8.6) | 6 (14.3) | 0 (0) | .074 |
| Reported using nondrug treatments | 11 (15.7) | 11 (26.2) | 0 (0) | .002c |
| Nausea-related hospitalization | 3 (4.3) | 3 (7.1) | 0 (0) | .270 |
| Experienced nausea after first trimester | 18 (25.7) | 17 (40.5) | 1 (3.6) | .001c |
Frequency (%).
High nausea defined as ≥2 h/d of feeling nauseous or vomiting.
Significant difference comparing high- and low-nausea women (P value <.05).
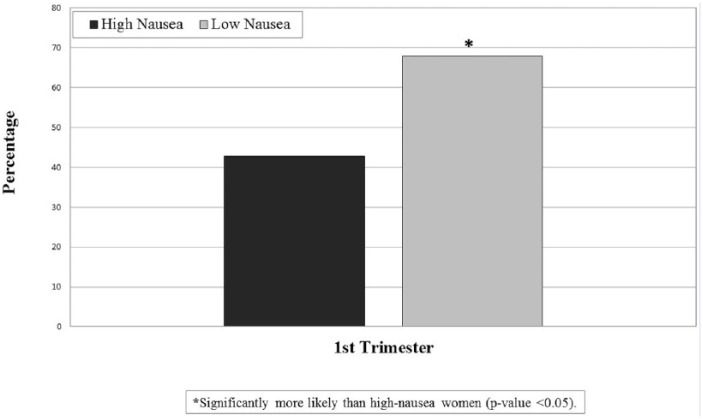
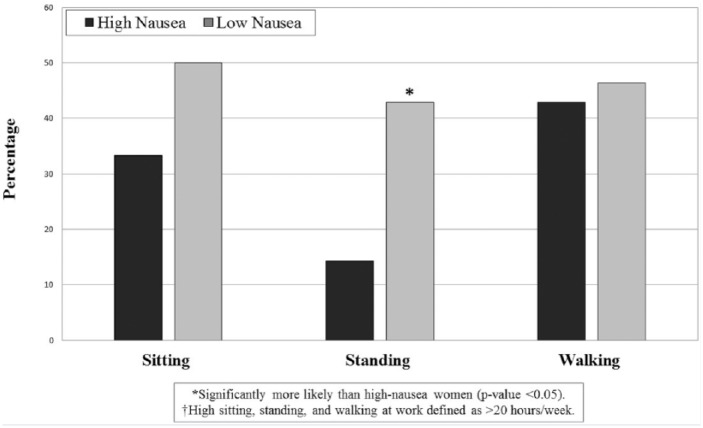
Mann-Whitney U tests showed that low-nausea women had significantly higher levels of LTPA (P = .05) compared with high-nausea women (median = 764.0 vs 385.5 MET minutes per week; Table 3). Low-nausea women also reported significantly more time spent standing at work (P = .03) compared with high-nausea women (median = 14 vs 6.3 h/wk). Also, 28.6% of women (n = 20) reported their primary occupation during their first trimester of pregnancy as a homemaker, whereas 71.4% (n = 50) reported their occupation being some position outside of the home. Occupation type was not related to level of nausea, LTPA, or work PA. Nearly 53% of the analytic sample reported meeting the current PA guidelines of at least 150 min/wk during the first trimester. χ2 Results indicated that first-trimester low-nausea women were significantly more likely to meet these guidelines than high-nausea women (68% vs 43%, P = .04; Figure 1). Furthermore, low-nausea participants were more likely to have spent more time standing at work (43% vs 14%, P = .03; Figure 2).
Table 3.
Characteristics of First-Trimester LTPA and Work PA Among High and Low-Nausea Pregnant Women.a
| Total (n = 70) | High Nauseab (n = 42) | Low Nausea (n = 28) | P Value | |
|---|---|---|---|---|
| LTPA MET minutes per week | ||||
| First trimester | 516.5 (0, 2985) | 385.5 (0, 2985) | 764 (0, 2820) | .050c |
| Work PA (h/wk) | ||||
| First trimester sitting | 9.9 (0, 94.5) | 7.4 (0, 94.5) | 13.8 (1.5, 48) | .058 |
| First trimester standing | 8.3 (0, 63.7) | 6.3 (0, 32.4) | 14 (0, 63.7) | .033c |
| First trimester walking | 13.1 (0, 73.5) | 12.3 (0, 73.5) | 13.8 (0, 63) | .783 |
Abbreviations: PA, physical activity; LTPA, leisure-time PA; MET, metabolic equivalent.
Median (range).
High nausea defined as ≥2 h/d of feeling nauseous or vomiting.
Significant difference comparing high- and low-nausea women (P value <.05).
Figure 1.
Relative frequency of meeting the current leisure-time physical activity guidelines during the first trimester among high- and low-nausea pregnant women.
Figure 2.
Relative frequency of “high” sitting, standing, and walking at work during the first trimester among high- and low-nausea pregnant women.
In examining these relationships further, logistic regression results (Table 4) revealed meeting the current LTPA guidelines and high standing at work in the first trimester were related to reduced odds of high nausea (odds ratio [OR] = 0.22, 95% CI = 0.06-0.74; OR = 0.43, 95% CI = 0.13-0.97). High standing at work remained significantly related to reduced high nausea, even after adjusting for meeting the LTPA guidelines, total time at work, physician-instructed bed rest, and antinausea medication use (adjusted OR [aOR] = 0.23, 95% CI = 0.06-0.96). However, meeting LTPA guidelines was no longer statistically significant (aOR = 0.45; 95% CI = 0.16-1.30) after adjusting for potential covariates.
Table 4.
Odds of High Nausea With Meeting LTPA Guidelines and Standing at Work During the First Trimester.a
| Unadjusted Model | Adjusted Model | |||
|---|---|---|---|---|
| OR [95% CI] | P Value | OR [95% CI] | P Value | |
| Met LTPA guidelinesb | ||||
| No | — | — | — | — |
| Yes | 0.43 [0.13-0.97] | .04c | 0.45 [0.16-1.3] | .14 |
| Standing at work | ||||
| <10 h/wk | — | — | — | — |
| 10-20 h/wk | 0.94 [0.28-3.19] | .92 | 0.99 [0.23-3.49] | .98 |
| >20 h/wk | 0.22 [0.06-0.74] | .02c | 0.23 [0.06-0.96] | .04c |
Abbreviations: LTPA, leisure-time physical activity; OR, odds ratio.
Met LTPA guidelines adjusted for total time spent at work, standing at work, bed rest, and use of antinausea medication; standing at work adjusted for total time spent at work, bed rest, use of antinausea medication, and met LTPA guidelines).
Meeting current LTPA guidelines defined as participating in ≥150 min/wk.
Significant difference comparing high- and low-nausea women (P value <.05).
Discussion
This investigation represents the first to examine how the amount and intensity of LTPA is related to the level of pregnancy-induced nausea. As we hypothesized, women categorized as low-nausea (≤1 h/wk) participated in higher levels of LTPA and were more likely to meet the current LTPA recommendations compared with high-nausea women (≥2 h/wk). Our results for first-trimester women are in line with the population-based findings of Owe et al15—namely, that second-trimester pregnant women (n = 34 508) who did not experience nausea were more likely to exercise regularly. However, Owe et al15 only considered frequency, but not the intensity or total amount of LTPA. Our findings also are congruent with results of qualitative investigations, which have sought a deeper understanding of the barriers to pregnancy LTPA. As a part of these investigations, first-trimester pregnant women have reported that higher levels of nausea and vomiting meaningfully impede their LTPA participation. Thus, our findings add to the small body of evidence that pregnancy LTPA and pregnancy-induced nausea are inversely related.
To our knowledge, this investigation is the first to consider the relationship between work PA and nausea and vomiting during pregnancy. Similar to LTPA, we found that low-nausea pregnant women participated in more work PA and standing at work than did high-nausea pregnant women. One might speculate that pregnant women replace work standing time with something less strenuous (eg, sitting) to reduce feelings of nausea. However, low-nausea women also participated in more sitting at work compared with high-nausea women (P = .058). This finding suggests that high-nausea women did not remedy their feelings of nausea by sitting instead of standing at work, but rather by working less. It is possible that pregnant women with high levels of nausea feel more compelled to take time off from work than do low-nausea pregnant women, which is in line with previous findings.5 In our investigation, when total work time was controlled for, women standing >20 h/wk at work had a 77% reduced odds of high nausea compared with women standing <10 h/wk. Curiously, nausea level was not related to time spent walking at work; this is in contrast to our original hypothesis. It is possible that work tasks involving walking are more important to complete than those requiring standing and, therefore, cannot be sacrificed when pregnancy nausea and vomiting are experienced. Kallen et al23 showed that first- and second-trimester pregnant women (n = 3675) working outside the home had lower levels of pregnancy-induced nausea than did pregnant women whose primary occupation was homemaking. Our findings did not support this, possibly as a result of our comparatively small sample size or our focus on only the first trimester.
Strengths and Limitations
Although our results provide valuable insight into the relationship between PA behavior and first-trimester nausea, this investigation is limited by a few factors. Data with respect to LTPA, work-related PA, and nausea/vomiting during pregnancy were recalled by women approximately 15 months postpartum. In general, investigative efforts that involve recalling PA levels may be susceptible to recall bias; however, the instrument used in this investigation has shown acceptable accuracy for recalling PA up to 5 years postpartum.21 Additionally, data for this investigation were not collected prospectively throughout the first trimester. We did not investigate some factors that may influence early-pregnancy PA and nausea levels, such as fatigue and direct side effects of antinausea medication use. Our findings are partially limited by our inability to statistically control for these variables and other potential barriers to PA.
Despite the aforementioned limitations, this investigation provides critical information with respect to a common first-trimester condition (and barrier to PA) that has received limited attention in the scientific literature. Our findings are novel given the lack of available information on how the intensity and amount of LTPA relates to first-trimester nausea. Furthermore, our findings provide novel information with respect to the potential influence of first-trimester nausea and vomiting on work PA or vice versa. This specific relationship has not been assessed previously, and our findings provide insight into specific and common modalities of activity (walking, standing, and sitting) that are required for various occupations.
Conclusions
In summary, we present preliminary evidence that level of nausea is inversely related to LTPA and work PA in the first trimester of pregnancy. Given the nature of our cross-sectional data, we were not able to establish time order in examining these relationships. Therefore, it cannot be determined from our findings whether PA during pregnancy reduces the effects of nausea and vomiting or, rather, whether lower levels of nausea and vomiting allow pregnant women to be more physically active. Future investigations should seek to assess this relationship through longitudinal methods, specifically beginning data collection before pregnancy-induced nausea begins and following throughout the first trimester. Future investigative efforts should also seek to utilize objective measures of PA behavior in leisure time and at work.
Acknowledgments
This work was supported by funding from the Centers for Disease Control and Prevention (Grant R36 DP001322-01) and the Blue Cross Blue Shields of Michigan Foundation (Grant 1416SAP).
Footnotes
Authors’ Note: Data from this project were presented at the American College of Sports Medicine Annual Meeting (2013) in Indianapolis, Indiana. This article was prepared while Dr Mudd was employed at Michigan State University. The opinions expressed in this article are the author’s own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Gadsby R, Barnie-Adshead AM, Jagger C. A prospective study of nausea and vomiting during pregnancy. Br J Gen Pract. 1993;43:245-248. [PMC free article] [PubMed] [Google Scholar]
- 2. Lacroix R, Eason E, Melzack R. Nausea and vomiting during pregnancy: a prospective study of its frequency, intensity, and patterns of change. Am J Obstet Gynecol. 2000;182:931-937. [DOI] [PubMed] [Google Scholar]
- 3. Lacasse A, Rey E, Ferreira E, et al. Epidemiology of nausea and vomiting of pregnancy: prevalence, severity, determinants, and the importance of race/ethnicity. BMC Pregnancy Childbirth. 2009;9:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lacasse A, Rey E, Ferreira E, et al. Nausea and vomiting of pregnancy: what about quality of life? BJOG. 2008;115:1484-1493. [DOI] [PubMed] [Google Scholar]
- 5. Attard CL, Kohli MA, Coleman S, et al. The burden of illness of severe nausea and vomiting of pregnancy in the United States. Am J Obstet Gynecol. 2002;186:S220-S227. [DOI] [PubMed] [Google Scholar]
- 6. Mazzotta P, Stewart D, Atanackovic G, et al. Psychosocial morbidity among women with nausea and vomiting of pregnancy: prevalence and association with anti-emetic therapy. J Psychosom Obstet Gynecol. 2000;21:129-136. [DOI] [PubMed] [Google Scholar]
- 7. Bailit JL. Hyperemesis gravidarium: epidemiologic findings from a large cohort. Am J Obstet Gynecol. 2005;193:811-814. [DOI] [PubMed] [Google Scholar]
- 8. Eliakim R, Abulafia O, Sherer DM. Hyperemesis gravidarum: a current review. Am J Perinatol. 2000;17:207-218. [DOI] [PubMed] [Google Scholar]
- 9. Dodds L, Fell DB, Joseph KS, et al. Outcomes of pregnancies complicated by hyperemesis gravidarum. Obstet Gynecol. 2006;107:285-292. [DOI] [PubMed] [Google Scholar]
- 10. Tsang IS, Katz VL, Wells SD. Maternal and fetal outcomes in hyperemesis gravidarum. Int J Gynecol Obstet. 1996;55:231-235. [DOI] [PubMed] [Google Scholar]
- 11. Buckwalter JG, Simpson SW. Psychological factors in the etiology and treatment of severe nausea and vomiting in pregnancy. Am J Obstet Gynecol. 2002;186:S210-S214. [DOI] [PubMed] [Google Scholar]
- 12. Beilock SL, Feltz DL, Pivarnik JM. Training patterns of athletes during pregnancy and postpartum. Res Q Exerc Sport. 2001;72:39-46. [DOI] [PubMed] [Google Scholar]
- 13. Bennett EV, McEwen CE, Clarke LH. It’s all about modifying your expectations: women’s experiences with physical activity during pregnancy. Qual Res Sport Exerc Health. 2013;5:267-286. [Google Scholar]
- 14. Symons Downs D, Hausenblas HA. Women’s exercise beliefs and behaviors during their pregnancy and postpartum. J Midwifery Womens Health. 2004;49:138-144. [DOI] [PubMed] [Google Scholar]
- 15. Owe KM, Nystad W, Bo K. Correlates of regular exercise during pregnancy: the Norwegian Mother and Child Cohort Study. Scand J Med Sci Sports. 2009;19:637-645. [DOI] [PubMed] [Google Scholar]
- 16. Hegaard HK, Kjaergaard H, Damm PP, et al. Experiences of physical activity during pregnancy in Danish nulliparous women with a physically active life before pregnancy: a qualitative study. BMC Pregnancy Childbirth. 2010;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mudd LM, Nechuta S, Pivarnik JM, et al. Factors associated with women’s perceptions of physical activity safety during pregnancy. Prev Med. 2009;49:194-199. [DOI] [PubMed] [Google Scholar]
- 18. Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. https://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines/Report%20Brief%20-%20Weight%20Gain%20During%20Pregnancy.pdf. Accessed January 23, 2016.
- 19. Koren G, Boskovic R, Hard M, et al. Motherisk-PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. Am J Obstet Gynecol. 2002;186:S228-S231. [DOI] [PubMed] [Google Scholar]
- 20. Koren G, Piwko C, Ahn E, et al. Validation studies of the Pregnancy Unique-Quantification of Emesis (PUQE) scores. J Obstet Gynecol. 2005;25:241-244. [DOI] [PubMed] [Google Scholar]
- 21. Bauer PW, Pivarnik JM, Feltz DL, et al. Validation of an historical physical activity recall tool in postpartum women. J Phys Act Health. 2010;7:658-661. [DOI] [PubMed] [Google Scholar]
- 22.United States Department of Health and Human Services. Physical activity guidelines for Americans. http://www.health.gov/paguidelines/guidelines/default.aspx. Accessed January 23, 2016.
- 23. Kallen B, Lundberg G, Aberg A. Relationship between vitamin use, smoking, and nausea and vomiting of pregnancy. Acta Obstet Gynecol Scand. 2003;82:916-920. [PubMed] [Google Scholar]