Abstract
Background
Acupuncture has been using as an alternative non-pharmacological therapy in the management of post stroke depression and cognitive impairment but its effectiveness and safety remain controversial. We conducted an overview of systematic reviews with meta-analyses to evaluate the evidence on the effect of acupuncture in the treatment of stroke with conventional medicine intervention.
Methods
Systematic reviews summarized the treatment effects of acupuncture for post stroke cognitive impairment and post stroke depression were considered eligible. Methodological quality of included systematic reviews was assessed using A MeaSurement Tool to Assess systematic Reviews 2 (AMSTAR 2).
Results
Four systematic reviews on post stroke cognitive impairment and ten systematic reviews on post stroke depression with good methodological quality were included. Meta-analyses revealed that acupuncture plus cognitive rehabilitation; and acupuncture or moxibustion plus cognitive rehabilitation, versus cognitive rehabilitation demonstrated statistically significant increase in Mini-Mental State Examination scores in compared to cognitive rehabilitation after 4 weeks treatment [Pooled weighted mean difference (WMD) = 3.14, 95% confidence interval (CI) = 2.06 to 4.21, I2 = 36%]; and (Pooled WMD = 3.22, 95% CI = 2.09 to 4.34, I2 = 0%). Furthermore, acupuncture versus antidepressant demonstrated statistically significant improve depression measured by increasing in 17-item Hamilton Depression Rating Scale in comparing to cognitive rehabilitation after 2 weeks treatment (Pooled WMD= -2.34, 95% CI= -3.46 to -1.22, I2 = 5%). Acupuncture usage was not associated with increased risk of adverse events.
Conclusions
Acupuncture is safe and improves cognitive function and depressive disorder without obvious serious adverse events for post stroke patients.
Keywords: Systematic review, acupuncture, cognitive impairment, depression, stroke, Child
1. Introduction
Incident stroke could lead to emotional changes and an acute decline in cognitive function.1, 2 The emotional changes after stroke are thought to result from disruption of prefrontal system and lesions damaging the striato-pallido-thalamo-cortical pathways3, 4, 5 while the decline in cognitive function after stroke is due to the reduction of regional blood flow blocked by recurrent and multiple infarctions.6 Post stroke depression (PSD) is associated with poor functional outcomes, and consistently high mortality rates7, 8 and post-stroke cognitive impairment is associated with increase mortality,9 hospitalization,10 disability,11 and poorer quality of life.12 It has been found that cognitive performance was associated with symptoms of depression and with self-reported cognitive function on patient after stroke.13
In the management of post stroke depression, it has been suggested that Selective Serotonin Reuptake Inhibitors (SSRIs) is the first line treatment.8 It has been proven that SSRI (Fluoxetine) had lower rates of depression and better motor function as compared to the placebo group at 3 months.14 Whereas, drug therapy of post-stroke cognitive impairment remains unclear.6 Currently, there are no evidence-based interventions that can successfully treat post-stroke cognitive decline. Alternatives therapy such as cognitive rehabilitation may be beneficial for enhancing their attention deficits and activities of daily living (ADL) immediately following less than 3 months and 6 months of treatment respectively.15 However, there is still insufficient evidence and unclear effectiveness of cognitive rehabilitation for improving individuals cognitive function.16, 17
Acupuncture has been using as an alternative non-pharmacological therapy that involves the insertion of needles into acupuncture points in the skin as to correct imbalances of the flow of Qi through meridians.18 Preclinical evidence demonstrated that acupuncture associates with the potential of DNA methylation and histone modifications of brain-derived neurotropic factor in epigenetic mechanism that may produce antidepressant effect in animal study.19, 20 Acupuncture incorporation with electrotherapy also improves cognitive function and synaptic plasticity21 by attenuating left cortex, hippocampus, corpus striatum, and thalamus lesions and increasing the density of dendritic spines and number of CA1 synapse in the hippocampus of middle cerebral artery occlusion induced cognitive deficit rats.22, 23 Many clinical studies have suggested the use of acupuncture in the management of post stroke depression24, 25, 26, 27, 28, 29, 30, 31, 32 and cognitive impairment.33, 34, 35, 36, 37, 38 These trials were implemented with different methodologies and outcome measures. The treatment effects of acupuncture on post-stroke cognitive impairment and depression were inconclusive from systematic reviews.39, 40, 41, 42 Systematic reviews have been conducted to examine the potential relative benefits or harms of acupuncture in the treatment of post-stroke cognitive impairment and depression. However, the treatment benefits of acupuncture on post-stroke cognitive impairment and depression are still unclear due to the differences of methods, and quality of systematic reviews. We conduct an overview of systematic reviews to overcome the gaps by composing, appraising, and summarizing all relevant systematic reviews into a single document, which has potential usefulness for therapeutic and policy decision-making. Furthermore, there has been no overview of systematic reviews to analyze the effectiveness and safety of acupuncture for improving cognitive function and depression in post-stroke patient. In this overview of systematic reviews, we aim to summarize the best available clinical evidence on the effectiveness and safety of acupuncture on post-stroke cognitive impairment and depression management. This study will provide a comprehensive synthesis of clinical evidence on acupuncture on post-stroke cognitive impairment and depression receiving routine stroke care, which may help in identifying treatment alternatives with acupuncture on post-stroke cognitive impairment and depression management so as to provide a basis to develop an integrative medicine model for post-stroke cognitive impairment and depression.
2. Methods
2.1. Search strategy
A literature search of online databases MEDLINE, Excerpta Medica dataBASE (EMBASE), Cochrane Database of Systematic Reviews (CDSR) and Database of abstracts of reviews of effects (DARE) and Chinese databases [Chinese Biomedical Database (CBM), Wan Fang Digital journals and Taiwan Periodical Literature Databases] from inception to August 2017 was performed. Specialized search filter for reviews was used for MEDLINE and EMBASE.43, 44 Detailed searching strategies were reported in Supplment 1.
2.2. Eligibility criteria
2.2.1. Types of studies
We included systematic reviews (SRs) with meta-analysis of randomized controlled trials (RCTs) in this overview. RCTs are trials that group patients by simple random methods. We excluded SRs with meta-analysis of observational studies, which included case-control studies, cross-sectional studies, longitudinal studies, and cohort studies. We used the Cochrane Collaboration definition for systematic review, that is a form of publication that searches, identifies, appraises, and collates all empirical evidence according to the pre-specified eligibility criteria to answer the objectives or specific research questions, using systematic methods to minimize risk of bias.45 We only included the SRs that used validated method to measure the outcome. We evaluated all possible clinical evidence in the use of acupuncture versus conventional intervention for post-stroke cognitive impairment management and the use of acupuncture versus anti-depressant for post stroke depression treatment.
2.2.2. Subjects
We included patients diagnosed with any type of stroke by World Health Organization stroke criteria46 (ischemic stroke, acute ischemic stroke, intracerebral haemorrhage, subarachnoid haemorrhage, acute stroke, progressive cerebral infarction, acute cerebral infarction, cerebral haemorrhage, and cerebral ischemic stroke) or America stroke association criteria47 (ischemic, haemorrhagic, transient ischemic) and received acupuncture along with conventional intervention (cognitive rehabilitation and conventional therapy) in post-stroke management. The participants in the included reviews were not limited by gender, age, course of the disease, and treatment duration.
2.2.3. Intervention and control
We included peer-reviewed full articles published in English and Chinese language. Subjects were defined by a diagnosis of stroke46, 47 and were using acupuncture and conventional intervention. Acupuncture included (needle) acupuncture, electro-acupuncture, and moxibustion therapy. The specific types of (needle) acupuncture and moxibustion referred to ‘Acupuncture and moxibustion law, 7th edition’ as the selection criteria.48 We included acupuncture interventions regardless of needle material, treatment points (e.g., single head acupuncture treatment or scalp), the implementation of techniques, selected points to implement the hands of time, leaving the needle time and treatment is not limited. Cognitive rehabilitation, which included physiotherapy, occupational therapy, speech therapy, and nursing care, was used in the management of post-stroke cognitive impairment. Conventional therapy included use of drugs, such as antiplatelet agents, anticoagulants, fibrinogen-depleting agents, and volume expansion and vasodilators, and neuroprotective agents; but not including thrombolytic agents. Conventional care also included treatment for stroke related complications, such as brain edema, seizures, dysphagia, pneumonia, voiding dysfunction and urinary tract infections, and deep vein thrombosis. Anti-depressants were included monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants (TCAs), tetracyclic antidepressants (TeCAs) and SSRIs for the treatment of post stroke depression. In the management of post-stroke cognitive impairment, two types of comparisons were considered to be included in this overview of SRs: (1) acupuncture plus cognitive intervention versus cognitive intervention only; and (2) acupuncture plus cognitive intervention versus placebo of acupuncture plus cognitive intervention.
For the treatment of post stroke depression, two types of comparisons were considered to be included in this overview of SRs: (1) acupuncture versus anti-depressant only; and (2) acupuncture versus placebo of acupuncture plus anti-depressant.
2.3. Selection of systematic reviews
2.3.1. Data extraction
We extracted the following data from full-text articles: (i) basic characteristics of the SRs, searching date of the study, number of included studies, total number of patients and bibliographic information; (ii) detail information on study design and patient, intervention, control and outcomes; (iii) meta-analysis results of the including pooled effects of each comparison for each outcome; and (iv) results of methodological quality assessment.
2.4. Quality assessment of systematic reviews
Methodological quality of all included SRs was assessed using Assessing the Methodological Quality of Systematic Reviews (AMSTAR 2).49 The judgments were given in 11 items as ‘yes’, “no”, “cannot answer” or “not applicable” based on the information provided. The detail description of AMSTAR 2 is provided in Table 2. Two researchers conducted literature selection, data extraction and methodological quality assessment independently. Any disagreement was discussed with consensus. A third reviewer assessed unresolved discrepancy when necessary.
Table 2.
Methodological Quality of Included Meta-analyses on Acupuncture in the Treatment of Cognitive Impairment and Post Stroke Depression Management
| First author and year of publication | AMSTAR 2 item |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| Treatment of cognitive impairment | ||||||||||||||||
| Liu, 201442 | Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Partial Yes | Partial Yes | Yes | Yes | Yes | No | Yes | No | Yes |
| Liu, 201562 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | No | Yes | Yes | Yes | No | No | No | No |
| Xiong, 201664 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Yes | Partial Yes | Yes | Yes | Yes | No | Yes | No | No |
| Zhang, 201563 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| # of Yes | 4 | 0 | 4 | 1 | 4 | 4 | 0 | 2 | 1 | 4 | 4 | 4 | 1 | 3 | 0 | 1 |
| Treatment of depression | ||||||||||||||||
| Li, 201271 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Li, 201874 | Yes | Yes | Yes | Partial Yes | Yes | Yes | No | Yes | Yes | No | Yes | No | No | Yes | No | No |
| Niu, 201469 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No | No | No | No |
| Que, 201870 | Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | No | No |
| Wu, 201573 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | No | No | Yes | No | No | Yes | No | No |
| Xiong, 201067 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Xu, 201468 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | No | No | Yes | No | No | Yes | No | No |
| Zhang, 201465 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | No | No | Yes | No | Yes | Yes | Yes | No |
| Zhang, 201466 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Zhan, 201672 | Yes | Partial Yes | Yes | Partial Yes | Yes | Yes | No | Partial Yes | No | No | Yes | No | No | Yes | Yes | Yes |
| # of Yes | 10 | 1 | 10 | 1 | 10 | 10 | 0 | 3 | 5 | 3 | 10 | 5 | 5 | 8 | 3 | 2 |
| (%) in total | 100 | 7 | 100 | 14 | 100 | 100 | 0 | 36 | 43 | 50 | 100 | 64 | 43 | 79 | 21 | 21 |
AMSTAR 2 check list:
1. Did the research questions and inclusion criteria for the review include the components of PICO?
2. Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol?
3. Did the review authors explain their selection of the study designs for inclusion in the review?
4. Did the review authors use a comprehensive literature search strategy?
5. Did the review authors perform study selection in duplicate?
6. Did the review authors perform data extraction in duplicate?
7. Did the review authors provide a list of excluded studies and justify the exclusions?
8. Did the review authors describe the included studies in adequate detail?
9. Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review?
10. Did the review authors report on the sources of funding for the studies included in the review?
11. If meta-analysis was performed did the review authors use appropriate methods for statistical combination of results?
12. If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis?
13. Did the review authors account for RoB in individual studies when interpreting/discussing the results of the review?
14. Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review?
15. If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review?
16. Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review?
2.5. Data analyses
The acupuncture treatments were assessed at SRs level. The pool effect estimates were extracted from each meta-analyses. We extracted pooled relative risk (RR) or pooled odds ratio (OR) for dichotomous outcomes, and pooled weighted mean difference (WMD) for continuous outcomes with 95% confidence interval (CI). For publication bias, funnel plot results would be reported if it was being mentioned in the included SRs. Heterogeneity across RCTs was reported by describing I2 values reported in included meta-analysis; I2 values of 0–25%, 26–50%, and above 50% represented low, medium and high heterogeneity, respectively.50
2.6. Outcome
We evaluated all possible clinical evidence in the use of acupuncture along with conventional medicine intervention for post-stroke cognitive impairment and depression. Cognitive function and depressive disorder were the two major outcomes for evaluating the effectiveness of acupuncture. The primary clinical outcomes were cognitive function improvement and depression symptoms improvement. Cognitive function was assessed at the end of treatment course by Mini-Mental State Exam (MMSE).51 Depression were assessed at the end of treatment course by Hamilton Rating Scale for Depression (HAMD).52 We also reported on other outcomes, including ADL,53 change of P300 amplitude,54 change of P300 latency,54 and change of neurobehavioral cognitive status examination55 total scores, change of BI,56 Mangled Extremity Severity Score (MESS)57 reduction rate, change of Fugl–Meyer scales,58 change of Sandoz clinical assessment geriatric scale,59 change of functional independence measure,60 and change of the antidepressant side-effect checklist.61
3. Results
3.1. Study characteristics
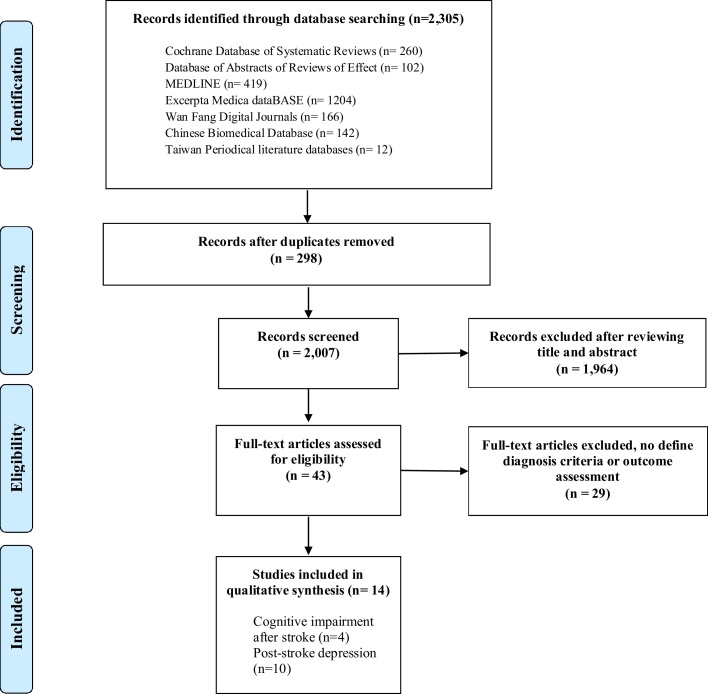
A total of 2305 citations were retrieved from the electronic databases, among which 14 SRs42, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74 fulfilled the inclusion criteria (Fig. 1). These eligible SRs were published between 2010 and 2018. The characteristics of included SRs have been summarized in Table 1. All SRs42, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74 that provided a cutoff date on literature search, 13 of SRs42, 62, 63, 64, 65, 66, 68, 69, 70, 71, 72, 73, 74 (92.9%) conducted literature search after 2010 with the most recent search conducted in 2016.
Fig. 1.
Flowchart of literature selection on meta-analyses of acupuncture in post-stroke cognitive impairment and depression management.
Table 1.
Characteristics of Included Meta-analyses on Acupuncture in the Treatment of Cognitive Impairment and Post-Stroke Management
| First author and year of publication | Search until (year) | Age (year-old) | Treatment duration | No. of studies (no. of patients) | Nature of acupuncture | Nature of control interventions | Outcomes reported |
|---|---|---|---|---|---|---|---|
| Treatment of cognitive impairment | |||||||
| Liu, 201442 | 2012 | 18–80 | 2–24 weeks | 21 (1421) | Acupuncture | Cognitive rehabilitation (physiotherapy, occupational therapy, speech therapy) | Cognitive function* |
| Liu, 201562 | 2013 | NA | 4–8 weeks | 9 (325) | Electro-acupuncture | Cognitive rehabilitation/conventional intervention (Nimodipin) | Cognitive function† |
| Xiong, 201664 | 2014 | 53–78 | 4 weeks–1 year | 13 (1113) | Scalp acupuncture | Cognitive rehabilitation/conventional intervention | Cognitive function‡ |
| Zhang, 201563 | 2015 | 30–79 | 4 weeks–3 months | 11 (395) | Acupuncture/moxibustion (Acupuncture, scalp acupuncture, electro-acupuncture) | Cognitive rehabilitation/conventional intervention (Nimodipin) | Cognitive function,§ activities of daily living (ADL) |
| Treatment of depression | |||||||
| Li, 201271 | 2011 | NA | 4–8 weeks | 13 (1062) | Electro-acupuncture | Antidepressants (tricyclic antidepressants, primary serotonin reuptake inhibitors) | Level of depression||,¶, ADL** |
| Li, 201874 | 2016 | NA | 4–12 weeks | 18 (1536) | Electro-acupuncture | Antidepressants (selective 5-HT reuptake inhibitors) | Level of depression,|| adverse events |
| Niu, 201469 | 2014 | NA | 4–8 weeks | 20 (1372) | Electro-acupuncture | Antidepressants (selective 5-HT reuptake inhibitors, monoamine oxidase inhibitors) | Level of depression,¶ cognitive function,† sensorimotor function,†† ADL** |
| Que, 201870 | 2014 | NA | 4–8 weeks | 18 (1813) | Acupuncture/Electro-acupuncture | Fluoxetine hydrochloride (formulation, route of administration, and dose were not limited) | Level of depression||,¶,‡‡ cognitive function,† ADL,** function independent measure,§§ adverse events |
| Wu, 201573 | 2011 | NA | 2–6 weeks | 5 (728) | Acupuncture | Fluoxetine hydrochloride | Level of depression||,¶ |
| Xiong, 201067 | 2009 | NA | 1–8 weeks | 20 (2031) | Acupuncture/moxibustion | Antidepressants (type were not limited) | Level of depression||,¶,‡‡, adverse events |
| Xu, 201468 | 2013 | NA | 2–8 weeks | 20 (2083) | Acupuncture/moxibustion | Antidepressant (type were not limited) | Level of depression||,¶ |
| Zhang, 201465 | 2013 | NA | 4–8 weeks | 13 (845) | Acupuncture | Antidepressants (type were not limited) | Level of depression,¶ adverse events |
| Zhang, 201466 | 2012 | NA | 2–8 weeks | 17 (1132) | Acupuncture (Filiform needle) | Antidepressants (type were not limited) | Level of depression,||,¶ adverse events |
| Zhan, 201672 | 2015 | NA | 4–8 weeks | 14 (1180) | Electro-acupuncture | Antidepressants (type, dosage form, and dose were not limited) | Level of depression||,¶,‡‡ |
*Change of Mini-mental state examination (MMSE) scores; Change of P300 amplitude; Change of P300 latency, Change of Neurobehavioral cognitive state examination total score.† Change of MMSE.
‡ Change of MMSE, Change P300 latency.
§ Change of MMSE scores, Change of P300 amplitude, Change of P300 latency.
|| Change of Hamilton Depression Rating Scale (HAMD).
¶ The reduction score rate of HAMD = [(total score pretreatment - total score post-treatment)/total score pretreatment] × 100%.
** Change of Barthel index (BI).
†† Change of Fugl-Meyer scales (FMS).
‡‡ Change of Self-rating depression scale (SDS).
§§ Change of Sandoz clinical assessment geriatric scale (SCAG).
The percentage of male participants was ranged from 53.5% to 61.4% (from three SRs64, 65, 73). The reported age of participants was ranged from 30 to 79 years (from two SRs63, 64). The range of duration of disease since onset was ranged from 12 days to 1 year from one SR.64 The treatment during of disease since onset was ranged from 2 to 24 weeks from thirteen SRs.42, 62, 63, 64, 65, 66, 67, 69, 70, 71, 72, 73, 74
Four SRs42, 62, 63, 64 focused on post-stroke cognitive impairment and ten SRs65, 66, 67, 68, 69, 70, 71, 72, 73, 74 summarized the evidence on post stroke depression.
3.2. Methodological quality of included SRs
All SRs42, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74 performed comprehensive literatures search and evaluated the scientific quality of the included studies (Table 2). All SRs42, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74 included the components of Population, Intervention, Comparator group, and Outcome (PICO) and timeframe for follow-up in the research questions and inclusion criteria, explained their selection of RCTs for inclusion in the review, involved at least two reviewers independently agreed on selection of eligible studies and achieved consensus on which studies to include and also which data to extract from included studies, and used appropriate methods for statistical combination of results. Eleven SRs42, 63, 64, 65, 67, 68, 70, 71, 72, 73, 74 provided a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of review. Nine SRs42, 62, 63, 64, 66, 67, 69, 70, 71 only included low risk of bias RCTs in individual studies on the results of the meta-analysis. Seven SRs42, 62, 63, 64, 66, 67, 71 reported on the sources of funding for the studies included in the review. Six SRs63, 67, 69, 70, 71, 74 assessed risk of bias in individual studies that were included in the review. Six SRs63, 65, 66, 67, 70, 71 included only low risk of bias RCTs when interpreting or discussing the results of the review. Five SRs63, 64, 69, 70, 74 described the details of populations, interventions, comparators, outcomes, and research design. Three SRs65, 66, 72 performed graphical tests for publication bias and discussed the likelihood and magnitude of impact of publication bias. Three SRs42, 66, 72 reported their funding sources and any potential sources of conflict of interest. Two SRs,42, 70 used a comprehensive literature search strategy. None of SR provided a list of excluded studies and justify the exclusions.
3.3. Outcome measures
The types of outcomes measures used across the SRs were summarized in Table 3. Other reported outcomes were listed in Appendix II. Four (28.6%) SRs42, 62, 63, 64 provided meta-analytic results on cognitive function. Ten (71.4%) SRs65, 66, 67, 68, 69, 70, 71, 72, 73, 74 reported meta-analytic results on depression.
Table 3.
Acupuncture in the Treatment of Cognitive Impairment and Depression After Stroke: Overview of Meta-Analyses Results
| First author and year of publication | Comparison | Time of assessment | No. of studies (no. of patients) | Pooled results (95%CI) | Heterogeneity I2 (%) |
|---|---|---|---|---|---|
| The overview of meta-analysis result of acupuncture in the treatment of cognitive impairment after stroke | |||||
| Change of Mini-mental state examination (MMSE) total scores | |||||
| Liu, 201442 | Acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional intervention | After 4 weeks treatment | 4 (232) | Pooled WMD: 3.14 (2.06, 4.21) | 36 |
| Liu, 201442 | Acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional | After 8 weeks treatment | 3 (128) | Pooled WMD: 2.03 (0.26, 3.80) | 72 |
| Liu, 201562 | Electro-acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional | After 4–8 weeks treatment | 8 (NA) | Pooled WMD: 2.12 (0.16, 4.08) | 95 |
| Xiong, 201664 | Scalp acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional | After 8–12 weeks treatment | 10 (732) | Pooled WMD: 2.22 (1.38, 3.07) | 76 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation | After 4 weeks treatment | 3 (208) | Pooled WMD: 3.22 (2.09, 4.34) | 0 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. Nimodipin | After 4–8 weeks treatment | 2 (175) | Pooled WMD: 1.84 (0.51, 3.16) | 0 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation/Nimodipin | After 4–8 weeks treatment | 5 (383) | Pooled WMD: 2.64 (1.78, 3.50) | 0 |
| Change of Activities of Daily Living (ADL) scales | |||||
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation | After 4 weeks to 3 months treatment | 4 (249) | Pooled WMD: 0.62 (0.36, 0.88) |
46 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation/conventional intervention | After 4 weeks to 3 months treatment | 6 (364) | Pooled WMD: 0.52 (0.31, 0.73) | 46 |
| The overview of meta-analysis result of acupuncture in the treatment of post stroke depression | |||||
| Change of Hamilton Rating Scale for Depression (HAMD) (17 items) | |||||
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 4 (270) | Pooled WMD: −3.29 (−6.87, 0.29) | 95 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4–6 weeks treatment | 5 (313) | Pooled WMD: −2.84 (−6.04, 0.36) | 93 |
| Zhang, 201466 | Acupuncture vs. antidepressants (Fluoxetine) | After 2 weeks treatment | 4 (192) | Pooled WMD: −2.34 (−3.46, −1.22) | 5 |
| Change of HAMD (24 items) | |||||
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 8 weeks treatment | 2 (531) | Pooled WMD: −3.17 (−6.16, −0.18) | 96 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 4 (268) | Pooled WMD: −1.42 (−3.45, 0.61) | 79 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4–8 weeks treatment | 7 (919) | Pooled WMD: −2.58 (−4.06, −1.09) | 90 |
| Xiong, 201067 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 7 (458) | Pooled WMD: −1.34 (−2.67, −0.02) | 69 |
| Zhang, 201466 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 7 (382) | Pooled WMD: −0.49 (−1.72, 0.74) | 52 |
| HAMD (24 items) reduction rate | |||||
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 6 (358) | Pooled OR: 1.57 (0.78, 3.16) | 0 |
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 8 weeks treatment | 5 (527) | Pooled OR: 1.72 (1.05, 2.28) | 0 |
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4–8 weeks treatment | 12 (946) | Pooled OR: 1.61 (1.09, 2.38) | 0 |
| Xiong, 201067 | Acupuncture vs. antidepressants | After 1–8 weeks treatment | 5 (595) | Pooled RR: 1.15 (1.07, 1.24) | 24 |
| Zhang, 201466 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 8 (422) | Pooled RR: 1.11 (1.03, 1.21) | 0 |
| Zhang, 201466 | Acupuncture vs. antidepressants | After 6 weeks treatment | 3 (183) | Pooled RR: 1.10 (0.94, 1.28) | 40 |
| Incidence of adverse event | |||||
| Li, 201874 | Electro-acupuncture vs. antidepressants | After 4–8 weeks treatment | 8 (798) | Pooled RR: 0.21 (0.14,0.33) | 0 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4–8 weeks treatment | 9 (628) | Pooled OR: 0.10 (0.05,0.19) | 42 |
| Zhang, 201465 | Acupuncture vs. antidepressants | After 4 weeks treatment | 8 (502) | Pooled RR: 0.32 (0.19, 0.53) | 0 |
3.4. Outcomes
3.4.1. Post-stroke cognitive impairment
Four SRs42, 62, 63, 64 evaluated the evidence of acupuncture for improving cognitive function in post-stroke patient versus cognitive rehabilitation. Two SRs42, 63 showed significant clinical benefit in cognitive impairment improvement after acupuncture treatment when compared to cognitive rehabilitation. Acupuncture plus cognitive rehabilitation versus cognitive rehabilitation demonstrated statistically significant increase in MMSE scores in compared to cognitive rehabilitation after 4 weeks treatment with medium heterogeneity (Pooled WMD = 3.14, 95% CI = 2.06 to 4.21, 4 RCTs, I2 = 36%).42 Acupuncture or moxibustion plus cognitive rehabilitation versus cognitive rehabilitation demonstrated statistically significant improvement in MMSE scores in compared to conventional stroke after 4 weeks treatment with low heterogeneity (Pooled WMD = 3.22, 95% CI = 2.09 to 4.34, 3 RCTs, I2 = 0%).63 Acupuncture or moxibustion plus cognitive rehabilitation versus cognitive rehabilitation or Nimodipin showed clinical benefit in MMSE scores improvement after 4–8 weeks treatment with low heterogeneity (Pooled WMD = 2.64, 95% CI = 1.78 to 3.50, 5 RCTs, I2 = 0%).63 Three SRs42, 62, 64 studied the clinical effect of acupuncture, electro-acupuncture, or scalp acupuncture plus cognitive rehabilitation on post-stroke cognitive impairment. The clinical benefit of cognitive function improvement was inconclusive due to heterogeneity across the underlying studies. None of the four SRs42, 62, 63, 64 reported adverse events (AE) of acupuncture or moxibustion plus cognitive rehabilitation versus cognitive rehabilitation.
3.4.2. Post stroke depression
Ten SRs65, 66, 67, 68, 69, 70, 71, 72, 73, 74 evaluated the evidence of acupuncture for improvement of depression in post-stroke patient versus antidepressants. One SR66 showed acupuncture versus antidepressants demonstrated statistically significant improve depression measured by increase in HAMD 17 items in compared to cognitive rehabilitation after 2 weeks treatment with low heterogeneity (Pooled WMD = −2.34, 95% CI = −3.46 to −1.22, 4 RCTs, I2 = 5%). The clinical benefit of depression improvement from two SRs67, 70 was inconclusive due to heterogeneity across the underlying studies and inclusion a single study result. Three SRs66, 67, 69 measured HAMD 24 items reduction rate of acupuncture versus antidepressants in post-stroke patient. One SR69 reported electro-acupuncture versus antidepressants demonstrated statistically significant improvement in HAMD 24 items reduction rate after 8 weeks or 4 to 8 weeks of treatment with low heterogeneity (Pooled OR = 1.72, 95% CI = 1.05 to 2.28, 5 RCTs, I2 = 0%) (Pooled OR = 1.61, 95% CI = 1.09 to 2.38, 12 RCTs, I2 = 0%).
Eight SRs65, 66, 67, 69, 70, 71, 72, 74 reported AE of acupuncture versus antidepressants. One SR74 reported electro-acupuncture treatment was associated with fewer AEs in comparing to antidepressants (Pooled RR = 0.21, 95% CI = 0.14 to 0.33, 8 RCTs, I2 = 0%). Two SRs65, 70 showed acupuncture versus antidepressants demonstrated statistically significant reduction in the incidence of AE (Pooled RR = 0.32, 95% CI = 0.19 to 0.53, 8 RCTs, I2 = 0%) (Pooled OR = 0.10, 95% CI = 0.05 to 0.19, 9 RCTs, I2 = 42%) respectively. Five SRs66, 67, 69, 71, 72 reported AE were described generally in SRs level. Most AE were reported in patients who received antidepressants which included dizziness, drowsiness, nausea, abnormal electrocardiogram, sweating, constipation, nausea, loss of appetite, abdominal pain, insomnia, elevated alanine aminotransferase, urinary retention, dry mouth, constipation, rash, and headache. The main AE from acupuncture group were soreness at the needle site, dizziness, sweating, gastrointestinal discomfort, skin allergy, and fatigue. None of these eight SRs65, 66, 67, 69, 70, 71, 72, 74 showed that acupuncture usage would increase the risk of AE. No life-threatening adverse effects were noted in all these SRs.
3.5. Other outcomes
3.5.1. Post-stroke cognitive impairment
One SR42 reviewed acupuncture plus cognitive rehabilitation demonstrated significant benefit in improving cognitive functions measured by increase Neurobehavior Cognitive State Examination Total Score after 3–4 weeks of treatment with low heterogeneity (Pooled OR = 5.63, 95% CI = 3.95 to 7.31, 2 RCTs, I2 = 0%). One SR63 showed that acupuncture or moxibustion plus cognitive rehabilitation versus cognitive rehabilitation has significant benefit in improving functional disability measured by ADL after 4 weeks to 3 months treatment with medium heterogeneity (Pooled WMD = 0.52, 95% CI = 0.31 to 0.73, 6 RCTs, I2 = 46%).
3.5.2. Post stroke depression
Three SRs66, 67, 69 reviewed acupuncture or Electro-acupuncture versus antidepressants for improvement of depression measure by HAMD (24 items) reduction rate. Acupuncture versus antidepressants demonstrated statistically significant improvement in HAMD reduction rate after 1–8 weeks treatment with low heterogeneity (Pooled OR = 1.15, 95% CI = 1.07 to 1.24, 5 RCTs, I2 = 24%).67 This result was consistence another SR66 which acupuncture versus Fluoxetine showed statistically significant improvement in HAMD reduction rate after 4 weeks treatment with low heterogeneity (Pooled OR = 1.11, 95% CI = 1.03 to 1.21, 8 RCTs, I2 = 0%). Electro-acupuncture versus Fluoxetine demonstrated statistically significant improvement in HAMD reduction rate after 4–8 weeks treatment with low heterogeneity (Pooled OR = 1.61, 95% CI = 1.09 to 2.38, 12 RCTs, I2 = 0%).69
4. Discussion
To the best of our knowledge, this review is the first overview of systematic reviews to explore the efficacy and safety of acupuncture for the management of cognitive impairment and depression after stroke. The evidence compiled by this overview indicated that acupuncture in addition to conventional intervention could improve cognitive function. Furthermore, acupuncture can be more effective and safe than antidepressants in the treatment of post stroke depression.
4.1. Implication of practice
Our main aim in this study was to address the research evidence on acupuncture in post-stroke cognitive impairment and depression. We have conducted comprehensive searches of published reviews and electronic databases from both Chinese and English languages to minimize the potential publication bias and executed rigorous procedures for study selection, quality assessment and data extraction. The major practical contribution of our research is that it provides evidence for clinicians and policy makers to identify treatment alternatives with acupuncture in managing post-stroke cognitive impairment and depression. In the management of post-stroke cognitive impairment, it is been suggested that cognitive rehabilitation could be a treatment of choice. However, Cochrane Systematic Reviews have showed that cognitive rehabilitation can only demonstrate the treatment benefits in independent living,75 and improving memory deficits.76 Thus, acupuncture is demonstrated as a potential alternative intervention for treating post-stroke patient with cognitive impairment.
A second important implication of our study derives from our finding on the depression management by acupuncture. Antidepressants have been used for treating post stroke depression more than 30 years. Nortriptyline was the first antidepressants studied in patients with post stroke depression and showed significant clinical benefit in comparing to placebo for reducing HAMD scores over 6 weeks in 1984.77 Ten years later, Citalopram, the first SSRI, was also demonstrated the clinical benefit of reducing HAMD scores over 6 weeks in patients with post stroke depression.78 Have not said that, treatment with antidepressants is not without risk. Side effects associated with antidepressants can leads to premature drug discontinuation. For example, patients who take TCA could experience peripheral anticholinergic side effects, which are dry month, constipation, and urinary hesitancy.79 Furthermore, SSRI use is associated with increased risk of hemorrhagic complications in elderly,80, 81 and stroke, myocardial infarction, and all-cause mortality in postmenopausal women.82 The potential common adverse events associated with acupuncture is transient which included fainting during treatment, nausea and vomiting, increased pain, diarrhea, local skin irritation, headaches, sweating, and dizziness. Using unused sterile needle could further prevent the transmission of infectious diseases. Acupuncture is potentially effective and safe monotherapy for post stroke depression.
4.2. Implication of research
4.2.1. Study design
It has been found that cognitive performance was associated with symptoms of depression and with self-reported cognitive function on patient after stroke83 and there is strong association exiting between depression and the presence of cognitive deficits.84 However, none of the included SRs studied the treatment benefits of acupuncture in post-stroke patients with both cognitive impairment and depression. Researcher should explore the potential treatment benefits in acupuncture for post-stroke patients with both cognitive impairment and depression. Furthermore, the treatment duration of all included SRs were below 24 weeks. The treatment benefits of acupuncture in post-stroke cognitive impairment and depression cannot be concluded in long-term treatment. In the future research, a consensus on study design and relevant outcome measures in conducting appropriate RCTs should be establishing in post-stroke cognitive impairment and depression management trials.
4.2.2. Study methodology
We did not cover Korean and Japanese database in our study. We are limited by our own language skills or ability to cover multi-countries’ database and to access potentially relevant studies in other language. It is advisable to form an international review teams to enhance the diversity of language resources and publication channels than a local teamwork.
There is room for improvement in methodological quality of the SRs. None of SR provided the protocol and list out all excluded and included studies. The included systematic reviews were not reported optimally. The outcome measures were generally poorly elaborated. Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) statement was not fully executed in the SRs; for instance, study characteristics, reporting risk of bias of individual studies and how it could affect publication and selection bias, and funding sources should be reported. Researchers should implement the reporting of RCTs following to the Consolidated Standards of Reporting Trials (CONSORT) statement to facilitate reliable, transparent and complete reporting of trials.
From the available evidence, acupuncture may be beneficial for improving cognitive function and depressive disorder without obvious serious adverse events for post-stroke patients in the convalescent stage. However, various limitations of the origanal studies, lack of methodological details, and insufficient reporting of trials hinder the strength of this recommendation and argue for further research to support this claim and implement changes to clinical practice.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
No ethical approval was required for this manuscript as this study did not involve human subjects or laboratory animals.
Data availability
All data related to this study are within this article (Refer to Appendix).
Contributor Information
Caroline Yik-fong Hung, Email: carolinehyf@gmail.com.
Xin-yin Wu, Email: xinyin.wu@csu.edu.cn.
Vincent Chi-ho Chung, Email: vchung@cuhk.edu.hk.
Endy Chun-hung Tang, Email: endytang@gmail.com.
Justin Che-yuen Wu, Email: justinwu@cuhk.edu.hk.
Alexander Yuk-lun Lau, Email: alexlau@cuhk.edu.hk.
Appendix I, II. Search strategies and results for overview review on systematic review with meta-analysis on acupuncture in the treatment of cognitive impairment and post stroke depression management all appendix.
1. Cochrane database of systematic reviews (CDSR) from inception to 5 April 2019
| No. | Searches | Results |
|---|---|---|
| 1 | (cerebrovascular disorders) | 565 |
| 2 | (basal ganglia cerebrovascular disease) | 119 |
| 3 | (brain ischemia) | 352 |
| 4 | (carotid artery disease) | 217 |
| 5 | (intracranial arterial diseases) | 214 |
| 6 | (intracranial arteriovenous malformations) | 43 |
| 7 | (intracranial embolism and thrombosis) | 163 |
| 8 | (intracranial haemorrhages) | 244 |
| 9 | (brain infarction) | 388 |
| 10 | (vasospasm, intracranial) | 81 |
| 11 | (vertebral artery dissection) | 77 |
| 12 | (stroke, lacunar) | 73 |
| 13 | (cerebrovascular trauma) | 186 |
| 14 | (hypoxia-ischemia, brain) | 44 |
| 15 | (stroke) | 1261 |
| 16 | (poststroke) | 138 |
| 17 | (post-stroke) | 133 |
| 18 | (cerebrovasc$) | 139 |
| 19 | (brain vascu$) | 1 |
| 20 | (cerebral vasc$) | 110 |
| 21 | (cva$) | 165 |
| 22 | (apoplex$) | 105 |
| 23 | (SAH) | 97 |
| 24 | (brain$) | 1870 |
| 25 | (cerebr$) | 654 |
| 26 | (intracran$) | 135 |
| 27 | (intracerebral) | 228 |
| 28 | (isch$emi$) | 144 |
| 29 | (infarct$) | 293 |
| 30 | (thrombo$) | 247 |
| 31 | (emboli$) | 340 |
| 32 | (occlus$) | 164 |
| 33 | (intracranial) | 554 |
| 34 | (subarachnoid) | 205 |
| 35 | (haemorrhage$) | 1480 |
| 36 | (hemorrhage$) | 1481 |
| 37 | (haematoma$) | 518 |
| 38 | (hematoma$) | 531 |
| 39 | (bleed$) | 365 |
| 40 | (hemiplegia) | 95 |
| 41 | (paresis) | 122 |
| 42 | (hemipleg$) | 65 |
| 43 | (hemipar$) | 62 |
| 44 | (paretic) | 58 |
| 45 | (cerebrovascular accident) | 689 |
| 46 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 | 3788 |
| 47 | (acupuncture*) | 384 |
| 48 | (electroacupunctur*) | 86 |
| 49 | (electro-acupunctur*) | 86 |
| 50 | (acupoint*) | 66 |
| 51 | (Transcutaneous Electric Nerve Stimulat*) | 87 |
| 52 | (percutaneous electrical nerve stimulat*) | 30 |
| 53 | (TENS) | 176 |
| 54 | #47 or #48 or #49 or #50 or #51 or #52 or #53 | 494 |
| 55 | #46 and #54 | 260 |
2. Database of abstracts of reviews of effects (DARE) from inception to 5 April 2019
| No. | Searches | Results |
|---|---|---|
| 1 | cerebrovascular disorders | 94 |
| 2 | brain ischemia | 123 |
| 3 | carotid artery disease | 12 |
| 4 | intracranial arteriovenous malformations | 7 |
| 5 | intracranial embolism and thrombosis | 1 |
| 6 | intracranial haemorrhages | 8 |
| 7 | brain infarction | 7 |
| 8 | vasospasm | 37 |
| 9 | vertebral artery dissection | 5 |
| 10 | cerebrovascular trauma | 1 |
| 11 | hypoxia-ischemia | 19 |
| 12 | stroke | 1968 |
| 13 | poststroke | 22 |
| 14 | post-stroke | 116 |
| 15 | cerebrovasc* | 348 |
| 16 | cerebral vasc* | 8 |
| 17 | cva* | 14 |
| 18 | apoplex* | 2 |
| 19 | SAH | 19 |
| 20 | brain* | 1018 |
| 21 | cerebr* | 1012 |
| 22 | intracran* | 338 |
| 23 | intracerebral* | 87 |
| 24 | isch*emi* | 1103 |
| 25 | infarct* | 1613 |
| 26 | thrombo* | 1645 |
| 27 | emboli* | 574 |
| 28 | occlus* | 454 |
| 29 | intracranial | 338 |
| 30 | subarachnoid | 110 |
| 31 | haemorrhage* | 581 |
| 32 | hemorrhage* | 878 |
| 33 | haematoma* | 154 |
| 34 | hematoma* | 48 |
| 35 | bleed* | 1289 |
| 36 | hemiplegia | 40 |
| 37 | paresis | 37 |
| 38 | hemipleg* | 53 |
| 39 | hemipar* | 22 |
| 40 | paretic | 16 |
| 41 | cerebrovascular accident | 45 |
| 42 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 | 7025 |
| 43 | acupuncture* | 605 |
| 44 | electroacupunctur* | 67 |
| 45 | electro-acupunctur* | 33 |
| 46 | acupoint* | 54 |
| 47 | Transcutaneous Electric Nerve Stimulat* | 55 |
| 48 | percutaneous electrical nerve stimulat* | 1 |
| 49 | TENS | 85 |
| 50 | #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 | 689 |
| 51 | #42 AND #50 | 102 |
3. MEDLINE from inception to 5 April 2019
| No. | Searches | Results |
|---|---|---|
| 1 | exp brain disease/or exp cerebrovascular disorders/or exp carotid artery diseases/or exp cerebrovascular trauma/or exp intracranial arterial diseases/or exp intracranial arteriovenous malformations/or exp *intracranial embolism and thrombosis*/or exp intracranial haemorrhages/or exp stroke/or exp vasospasm, intracranial/or exp vertebral artery dissection/ | 124,290 |
| 2 | (stroke or poststroke or post-stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cerebral vasc$ or cva$ or apoplex$ or SAH).tw. | 238,828 |
| 3 | ((brain$ or cerebr$ or cerebrell$ or intracerebral) adj5 (inch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. | 49,851 |
| 4 | ((brain$ or cerebr$ or cerebrell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. | 53,880 |
| 5 | hemiplegia/or exp paresis/ | 18,761 |
| 6 | (hemipleg$ or hemipar$ or paresis or paretic).tw. | 29,846 |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 | 347,012 |
| 8 | Search:.tw. | 334,997 |
| 9 | meta analysis.mp,pt. | 134,794 |
| 10 | review.pt. | 2,334,147 |
| 11 | di.xs. | 3,343,294 |
| 12 | associated.tw. | 2,927,523 |
| 13 | 8 or 9 or 10 or 11 or 12 | 7,576,754 |
| 14 | exp acupuncture/ | 1596 |
| 15 | acupuncture*.mp. | 23,544 |
| 16 | exp acupuncture points/ | 6044 |
| 17 | exp acupuncture therapy/ | 22,520 |
| 18 | exp acupuncture analgesia/ | 1181 |
| 19 | exp electroacupuncture/ | 3565 |
| 20 | electroacupunctur*.mp. | 4285 |
| 21 | electro-acupunctur*.mp. | 706 |
| 22 | acupoint*.mp. | 3963 |
| 23 | exp Transcutaneous Electric Nerve Stimulation/ | 7857 |
| 24 | Transcutaneous Electric Nerve Stimulat*.mp. | 4424 |
| 25 | percutaneous electrical nerve stimulat*.mp. | 43 |
| 26 | TENS.mp. | 9583 |
| 27 | 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 | 37,765 |
| 28 | 7 and 13 and 27 | 419 |
4. Excerpta Medica dataBASE (EMABSE) from inception to 5 April 2019
| No. | Searches | Results |
|---|---|---|
| 1 | exp cerebrovascular accident/or exp cerebrovascular disease/or exp brain disease/or exp brain disease/or exp basal ganglion haemorrhage/or exp brain hemangioma/or exp brain hepatoma/or exp brain haemorrhage/or exp brain infarction/or exp brain schema/or exp carotid artery disease/or exp cerebral artery disease/or exp cerebrovascular malformation/or exp hypophysis apoplexy/or exp intracranial aneurysm/ | 1,849,939 |
| 2 | exp basal ganglion hemorrhage/ | 683 |
| 3 | exp brain arteriovenous malformation/or exp brain malformation/ | 72,315 |
| 4 | (intracranial embolism and thrombosis).mp. | 55 |
| 5 | exp brain hematoma/or exp brain hemorrhage/ | 140,960 |
| 6 | exp cerebrovascular accident/or exp lacunar stroke/ | 183,717 |
| 7 | exp brain vasospasm/ | 7546 |
| 8 | exp artery dissection/ | 8688 |
| 9 | (stroke or poststroke or post-stroke or cerebrovasc$ or brain vasc$ or cerebral vasc$ or cerebral vasc$ or cva or apoplex$ or SAH).tw. | 419,240 |
| 10 | ((brain$ or cerebr$ or cerebrell$ or intracran$ or intracerebral) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$)).tw. | 137,390 |
| 11 | ((brain$ or cerebr$ or cerebrell$ or intracerebral or intracranial or subarachnoid) adj5 (haemorrhage$ or hemorrhage$ or haematoma$ or hematoma$ or bleed$)).tw. | 86,174 |
| 12 | hemiparesis/or hemiplegia/or paresis/ | 43,704 |
| 13 | (hemipeg$ or hemipar$ or paresis or paretic).tw. | 33,205 |
| 14 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 | 2,027,351 |
| 15 | meta-analys:.mp. | 253,701 |
| 16 | search:.tw. | 508,699 |
| 17 | review.pt. | 2,420,973 |
| 18 | 15 or 16 or 17 | 2,896,149 |
| 19 | exp acupuncture/ | 43,178 |
| 20 | acupuncture*.mp. | 42,646 |
| 21 | exp acupuncture analgesia/ | 1568 |
| 22 | exp acupuncture needle/ | 997 |
| 23 | exp electroacupuncture/ | 6009 |
| 24 | electroacupunctur*.mp. | 6838 |
| 25 | electro-acupunctur*.mp. | 1175 |
| 26 | acupoint*.mp. | 5806 |
| 27 | exp transcutaneous nerve stimulation/ | 1278 |
| 28 | Transcutaneous Electric Nerve Stimulat*.mp. | 369 |
| 29 | percutaneous electrical nerve stimulat*.mp. | 82 |
| 30 | TENS.mp. | 14,500 |
| 31 | 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 | 60,647 |
| 32 | 14 and 18 and 31 | 1204 |
5. Wan Fang from inception to 5 April 2019
cql://(“META”) AND (“acupuncture” OR “electroacupuncture” OR “Auricular acupuncture” OR “scalp acupuncture” OR “aqua acupuncture”) AND (“Stroke” OR “Cerebral infarction” OR “Cerebral hemorrhage” OR “Cerebral embolism” OR “Cerebrovascular disease” OR “Cerebrovascular disease” OR “Cerebrovascular accident” OR “Acute” OR “Integrated stroke unit” OR “Stroke unit”)
Search result = 166
6. Chinese Biomedical Database (CBM) from inception to 5 April 2019
(“System Review” [full field] OR “meta-analysis” [full field] OR “META” [full field]) AND (“Acupuncture” [full field] OR “Acupuncture” [full field] OR “Electroacupuncture” [full field] OR “Auricular acupuncture” [full field] OR “scalp acupuncture” [full field] OR “aqua acupuncture” [full field]) AND (“stroke” [full field] OR “stroke” [full field] OR “cerebral infarction” [full field] OR “brain hemorrhage” [full field] OR “brain embolism” [full field] OR “cerebrovascular disease” [full field] OR “cerebrovascular accident” [full field] OR “acute phase” “[full field] OR” Chinese and Western medicine combined stroke unit “[full field] OR” Chinese medicine stroke unit “[full field]”
Search result = 142
7. Taiwan Periodical literature databases from inception to 5 April 2019
(TX = System Review OR Meta-analysis OR META) [AND] (TX = Acupuncture OR Acupuncture OR Electroacupuncture OR Auricular acupuncture OR scalp acupuncture OR aqua acupuncture) [AND] (TX = Stroke OR Stroke OR Cerebral Infarction OR Cerebral Hemorrhage OR Cerebral embolism OR cerebrovascular disease OR cerebrovascular accident OR acute phase OR TCM combined stroke unit OR TCM stroke unit)
Search result = 12
Appendix II. Acupuncture in the treatment of cognitive impairment and depression after stroke: Overview of Meta-Analyses Results (Other reported outcomes)
| First author and year of publication | Comparison | Time of assessment | No. of studies (no. of patients) | Pooled results (95%CI) | Heterogeneity I2 (%) |
|---|---|---|---|---|---|
| The overview of meta-analysis result of acupuncture in the treatment of cognitive impairment after stroke | |||||
| Change of P300 amplitude | |||||
| Liu, 201442 | Acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional intervention | After 8 weeks to 3 months treatment | 4 (194) | Pooled WMD: 1.38 (0.93, 1.82) | 0 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation/conventional intervention | After 4 weeks to 3 months treatment | 4 (243) | Pooled WMD: 1.23 (0.82, 1.63) | 17 |
| Change of P300 latency | |||||
| Liu, 201442 | Acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional intervention | After 8 weeks to 3 months treatment | 4 (194) | Pooled WMD: −12.80 (−21.08, −4.51) | 93 |
| Xiong, 201664 | Scalp acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional intervention | After 8 weeks to 3 months treatment | 3 (180) | Pooled WMD: −1.85 (−3.04, −0.66) |
91 |
| Zhang, 201563 | Acupuncture/moxibustion + cognitive rehabilitation vs. cognitive rehabilitation | After 4 weeks to 3 months treatment | 4 (243) | Pooled WMD: −18.46 (−30.51, −6.41) | 91 |
| Change of Neurobehavioral cognitive state examination total score | |||||
| Liu, 201442 | Acupuncture + cognitive rehabilitation/conventional intervention vs. cognitive rehabilitation/conventional intervention | After 3–4 weeks treatment | 2 (121) | Pooled OR: 5.63 (3.95, 7.31) | 0 |
| Li, 201874 | Electro-acupuncture vs. antidepressants | After 4 weeks treatment | 7 (503) | Pooled WMD: −0.04 (−0.18, 0.10) | 23 |
| Li, 201874 | Electro-acupuncture vs. antidepressants | After 6 weeks treatment | 3 (186) | Pooled WMD: 0.04 (−0.43, 0.51) | 62 |
| Li, 201874 | Electro-acupuncture vs. antidepressants | After 8 weeks treatment | 5 (542) | Pooled WMD: −0.01 (−0.23, 0.22) | 28 |
| Wu, 201573 | Xingnao KaiQiao acupuncture vs. antidepressants (Fluoxetine) | Not reported | 5 (728) | Pooled WMD: −3.07 (−6.10, −0.05) | 98 |
| Xu, 201468 | Acupuncture vs. antidepressants | Not reported | 18 (NR) | Pooled WMD: −0.42 (−0.52, −0.32) | 90 |
| Zhang, 201465 | Acupuncture vs. antidepressants | Not reported | 12 (731) | Pooled WMD: 0.26 (0.11, 0.40) | 29 |
| Zhan, 201672 | Electro-acupuncture vs antidepressants | Not reported | 12 (1040) | Pooled WMD: −0.77 (−1.47, −0.07) | 85 |
| Zhang, 201466 | Acupuncture vs. antidepressants | (Exclude physiotherapy evidence database scale score < 6) Not reported | 3 (163) | Pooled WMD: −0.06 (−0.37, 0.25) | 8 |
| The overview of meta-analysis result of acupuncture in the treatment of post stroke depression | |||||
| HAMD (17 or 24 items) reduction rate | |||||
| Wu, 201573 | Xingnao KaiQiao acupuncture vs. antidepressants | Not reported | 5 (728) | Pooled RR: 1.06 (0.93, 1.22) | 72 |
| Change of Self-rating Depression Scale | |||||
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | Not reported | 3 (247) | Pooled WMD: −1.40 (−3.10, 0.30) | 77 |
| Xiong, 201067 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 3 (194) | Pooled WMD: −6.02 (−8.73, −3.30) | 90 |
| Change of Barthel index | |||||
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 4 (242) | Pooled WMD: −0.07 (−2.78, 2.64) | 57 |
| Niu, 201469 | Electro-acupuncture vs. antidepressants | After 8 weeks treatment | 2 (100) | Pooled WMD: 6.67 (−8.01, 21.35) | 91 |
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4–8 weeks treatment | 6 (342) | Pooled WMD: 1.38 (−1.88, 4.65) | 75 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | Not reported | 3 (180) | Pooled WMD: 16.32 (13.92, 18.71) | 16 |
| Change of Modified Edinburgh-Scandinavian Stroke Scale (MESSS) reduction scores | |||||
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 2 (130) | Pooled WMD: −1.89 (−4.77, −0.99) | 70 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4–8 weeks treatment | 3 (351) | Pooled WMD: −5.23 (−10.57, 0.11) | 92 |
| Que, 201870 | Acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 2 (120) | Pooled WMD: −7.46 (−12.2, −2.72) | 71 |
| Modified Edinburgh-Scandinavian Stroke Scale (MESSS) reduction rate | |||||
| Niu, 201469 | Electro-acupuncture vs. antidepressants (Fluoxetine) | After 4 weeks treatment | 2 (130) | Pooled OR: 1.80 (0.61, 5.31) | 0 |
| Change of Fugl–Meyer scales (FMS) | |||||
| Niu, 201469 | Electro-acupuncture vs. antidepressants | After 4 weeks treatment | 2 (152) | Pooled WMD: 3.50 (0.14, 6.86) | 86 |
Appendix III. Study protocol
Protocol Title: Overview of systematic reviews with meta-analyses on acupuncture in post-stroke cognitive impairment and depression management
Protocol Version: 1
Protocol Date: 5 August 2016
Principal Investigator: Caroline, yik-fong, Hung
Research Team: Xin-yin Wu, Vincent Chi-ho Chung, Endy Chun-hung Tang, Justin Che-yuen Wu, Alexander Yuk-lun Lau
I Abstract
Incident stroke could lead to emotional changes and an acute decline in cognitive function [1,2]. The emotional changes after stroke is thought to result from disruption of prefrontal system and lesions damaging the striato-pallido-thalamo-cortical pathways [3–5] while the decline in cognitive function after stroke is due to the reduction of regional blood flow blocked by recurrent and multiple infarctions [6]. It has been found that cognitive performance was associated with symptoms of depression and with self-reported cognitive function on patient after stroke [7]. Although it has been suggested that Selective Serotonin Reuptake Inhibitors (SSRIs) is the first line treatment for post stroke depression [8], there is still insufficient evidence and unclear effectiveness of cognitive rehabilitation for improving individuals cognitive function [9,10].
II Background and significance/preliminary studies
Systematic reviews (SRs) with meta-analysis have also been conducted to examine the relative benefits or harms of acupuncture together with conventional medicine intervention in the treatment of cognitive impairment and depression. An overview of SRs with meta-analyses on acutpuncuture in post-stroke cognitive impairment and depression management can provide a concise summary of results from SRs, and is essential for overcoming the knowledge gaps by composing, appraising, and summarizing all critical information from individual SRs.
III Study aim
This study aims to provide an overview of the effectiveness and safety of different CHM for post-stroke management. With a comprehensive synthesis of clinical evidence on the add-on effect of CHM in routine stroke care, this study will provide support to evaluate the effectiveness of CHM in combination with conventional medicine intervention in stroke management.
IV Administrative organization
-
a.
Department of Medicine and Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong; 9/F, Lui Che Woo Clinical Sciences Building, Prince of Wales Hospital, Shatin, N.T., Hong Kong
-
b.
Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong; 4/F, School of Public Health, Prince of Wales Hospital, Shatin, N.T., Hong Kong
-
c.
The Hong Kong Institute of Integrative Medicine, The Chinese University of Hong Kong, Hong Kong; 4L, 4/F, Day Treatment Block, Prince of Wales Hospital, 30-32 Ngan Shing Street, Shatin, New Territories, Hong Kong
V Study design
This is an overview of the effectiveness and safety of acupuncture for post-stroke cognitive impairment and post stroke depression.
VI Study procedures
-
a.Eligibility criteria
-
1.Types of studies
-
•We include SRs with meta-analysis of randomized controlled trials (RCTs) and quasi-randomized controlled trials in this overview.
-
•We exclude SRs with meta-analysis of observational studies, which include case-control studies, cross-sectional studies, longitudinal studies, and cohort studies.
-
•We use the Cochrane Collaboration definition for systematic review.
-
•
-
2.Subjects
-
•We include patients diagnosed with any type of stroke by World Health Organization stroke criteria [11] (ischemic stroke, acute ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, acute stroke, progressive cerebral infarction, acute cerebral infarction, cerebral hemorrhage, and cerebral ischemic stroke), or American Stroke Association criteria [12] (ischemic, hemorrhagic, transient ischemic) and received acupuncture along with conventional intervention (cognitive rehabilitation and conventional therapy) in post-stroke management.
-
•The subjects in the included reviews are not limited by gender, age, course of the disease, and treatment duration.
-
•
-
3.Intervention and control
-
•We include peer-reviewed full articles published in English and Chinese language.
-
•Subjects are using were using acupuncture and conventional intervention.
-
•Acupuncture included (needle) acupuncture, electro-acupuncture, and moxibustion therapy. The specific types of (needle) acupuncture and moxibustion referred to ‘Acupuncture and moxibustion law, 7th edition’ as the selection criteria [13].
-
•We include acupuncture interventions regardless of needle material, treatment points (e.g., single head acupuncture treatment or scalp), the implementation of techniques, selected points to implement the hands of time, leaving the needle time and treatment is not limited.
-
•Conventional medicine intervention is defined by American Stroke Association and European Stroke Organization [14,15].
-
•Conventional therapy include the use of drugs, such as antiplatelet agents, anticoagulants, fibrinogen-depleting agents, and volume expansion and vasodilators, and neuroprotective agents; but not including thrombolytic agents.
-
•
-
1.
-
b.Information sources
-
1.We perform a literature search of online databases [MEDLINE, EMBASE, Cochrane Database of Systematic Reviews (CDSR) and Database of Abstracts of Reviews of Effect (DARE)] and Chinese databases [Chinese Biomedical Databases (CBM), Wan Fang Digital journals and Taiwan Periodical Literature Databases] from inception to August 2017.
-
1.
-
c.Data management
-
1.We extract the following data from full-text articles: (i) basic characteristics of the SRs, searching date of the study, number of included studies, total number of patients and bibliographic information; (ii) detail information on study design and patient, intervention, control and outcomes; (iii) meta-analysis results of the including pooled effects of each comparison for each outcome; and (iv) results of methodological quality assessment.
-
1.
-
d.Selection process
-
1.Methodological quality of SRs is assessed using Assessing the Methodological Quality of Systematic Review (AMSTAR). The judgments are given in 11 items as “yes”, “no”, “cannot answer” or “not applicable” based on the information provided.
-
1.
-
e.Data collection process
-
1.Two researchers (CYFH and XYW) conduct literature selection, data extraction and methodological quality assessment independently. Any disagreement will be discussed with consensus. A third reviewer (VCHC) will assess unresolved discrepancy when necessary.
-
1.
-
f.Data items and synthesis
-
1.The acupuncture treatments are assessed at SRs level.
-
2.The pool effect estimates are extracted from each meta-analyses.
-
3.We extract pooled relative risk (RR) or pooled odds ratio (OR) for dichotomous outcomes, and pooled weighted mean difference (WMD) for continuous outcomes with 95% confidence interval (CI). Heterogeneity across RCTs is reported by describing I2 values reported in included meta-analysis; I2 values of 0–25%, 26–50%, and above 50% represented low, medium and high heterogeneity, respectively [16].
-
1.
4.3. Outcomes and prioritization
-
•
The primary clinical outcomes are cognitive function improvement and depression symptoms improvement.
-
•
Cognitive function is assessed at the end of treatment course by MMSE [17]. Depression were assessed at the end of treatment course by Hamilton Rating Scale for Depression (HAMD) [18].
-
•
All adverse events will be reported.
-
•
We also report on other outcomes, including activity of daily living, change of Barthel index, Change of Mini-mental state examination, change of Fugl-Meyer scales in this paper.
VII Literature cited
-
1.
D.A. Levine, A.T. Galecki, K.M. Langa, F.W. Unverzagt, M.U. Kabeto, B. Giordani, V.G. Wadley: Trajectory of cognitive decline after incident stroke. JAMA Jul 2015, 314:41–51.
-
2.
Y. Shi, D.D. Yang, Y.Y. Zeng, W. Wu: Risk factors for post-stroke depression: a meta-analysis. Front Aging Neurosci 2017, 9.
-
3.
G.S. Alexopoulos, B.S. Meyers, R.C. Young, S. Campbell, D. Silbersweig, M. Charlson: ‘Vascular depression’ hypothesis. Archives of General Psychiatry 1997, 54:915–922.
-
4.
M. Kimura, K. Shimoda, S. Mizumura, A. Tateno, T. Fujito, T. Mori, S. Endo: Regional cerebral blood flow in vascular depression assessed by 123I-IMP SPECT. Journal of Nippon Medical School 2003, 70:321–326.
-
5.
K.R. Krishnan, J.C. Hays, D.G. Blazer: MRI-defined vascular depression. The American Journal of Psychiatry 1997, 154:497–501.
-
6.
M. Danovska, B. Stamenov, M. Alexandrova, D. Peychinska: Post-stroke cognitive impairment- phenomenology and prognostic factors Journal of IMAB 2012, 18.
-
7.
A.E. Nakling, D. Aarsland, H. Næss, D. Wollschlaeger, T. Fladby, H. Hofstad, E. Wehling: Cognitive deficits in chronic stroke patients: neuropsychological assessment, depression, and self-reports. Dement Geriatr Cogn Dis Extra 2017, 7:283–296.
-
8.
G. Esparrago Llorcaa, L. Castilla-Guerrab, M.C. Fernández Morenoc, S. Ruiz Dobladoa, Hernándezd MDJn: Post-stroke depression: an update Neurologia 2015, 30:23–31.
-
9.
T. Loetscher, N.B. Lincoln: Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst Rev 2013, 31.
-
10.
C.S. Chung, A. Pollock, T. Campbell, B.R. Durward, S. Hagen: Cognitive rehabilitation for executive dysfunction in adults with stroke or other adult non-progressive acquired brain damage. Cochrane Database Syst Rev 2013, 30.
-
11.
World Health Organization: WHO Monica Project: MONICA manual. Part IV: Event Registration. http://www.ktl.fi/publications/monica/manual/part4/iv-2.htm – s1-1 (accessed 21.08.2018).
-
12.
America stroke association criteria. http://www.strokeassociation.org/STROKEORG/AboutStroke/TypesofStroke/Types-of-Stroke_UCM_308531_SubHomePage.jsp (accessed 21.08.2018).
-
13.
S.K. Lu: Acupuncture and moxibustion law, 7th edition. 2002.
-
14.
European Stroke Organisation Executive, ESO Writing Committee: Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovascular Diseases 2008, 25:457–507.
-
15.
Jauch EC, J.L. Saver, H.P.J. Adams, A. Bruno, J.J. Connors, B.M. Demaerschalk, P. Khatri, P.W.J. McMullan, A.I. Qureshi, K. Rosenfield, et al.: Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke; a Journal of Cerebral Circulation 2013, 44:870–947.
-
16.
Higgins JPT, S.G. Thompson, J.J. Deeks, et al.: Measuring inconsistency in meta-analyses. British Medical Journal 2003, 327:557–560.
-
17.
M.F. Folstein, S.E. Folstein, P.R. McHugh: “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975, 12:189–198.
-
18.
K.A. Kobak: Hamilton Depression Rating Scale. 2010.
Appendix IV. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist
| Treatment of post-stroke cognitive impairment |
Treatment of post stroke depression |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu, 201442 | Liu, 201562 | Xiong, 201664 | Zhang, 201563 | Li, 201271 | Li, 201874 | Niu, 201469 | Que, 201870 | Wu, 201573 | Xiong, 201067 | Xu, 201468 | Zhang, 201465 | Zhang, 201466 | Zhan, 201672 | |||
| 1 | Title | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2 | Abstract | Structured summary | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3 | Introduction | Rationale | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4 | Objectives | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 5 | Methods | Protocol and registration | No | No | No | No | No | Yes | No | No | No | No | No | No | No | No |
| 6 | Eligibility criteria | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 7 | Information sources | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 8 | Search | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 9 | Study selection | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 10 | Data collection process | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 11 | Data items | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 12 | Risk of bias in individual studies | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | |
| 13 | Summary measures | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 14 | Synthesis of results | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 15 | Risk of bias across studies | No | No | No | Yes | No | Yes | No | No | Yes | Yes | No | Yes | No | Yes | |
| 16 | Additional analyses | Yes | No | No | No | No | Yes | No | No | No | No | No | Yes | No | No | |
| 17 | Results | Study selection | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 18 | Study characteristics | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 19 | Risk of bias within studies | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | No | |
| 20 | Results of individual studies | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 21 | Synthesis of results | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 22 | Risk of bias across studies | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | No | |
| 23 | Additional analysis | Yes | No | No | Yes | No | Yes | No | No | No | No | No | Yes | No | No | |
| 24 | Discussion | Summary of evidence | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 25 | Limitations | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 26 | Conclusions | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 27 | Funding | Funding | Yes | Yes | No | Yes | No | No | No | No | No | Yes | No | Yes | Yes | No |
References
- 1.Levine D.A., Galecki A.T., Langa K.M., Unverzagt F.W., Kabeto M.U., Giordani B. Trajectory of cognitive decline after incident stroke. JAMA. 2015;314:41–51. doi: 10.1001/jama.2015.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi Y., Yang D.D., Zeng Y.Y., Wu W. Risk factors for post-stroke depression: a meta-analysis. Front Aging Neurosci. 2017;9 doi: 10.3389/fnagi.2017.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexopoulos G.S., Meyers B.S., Young R.C., Campbell S., Silbersweig D., Charlson M. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry. 1997;54:915–922. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- 4.Kimura M. Regional cerebral blood flow in vascular depression assessed by 123I-IMP SPECT. J Nippon Med School. 2003;70:321–326. doi: 10.1272/jnms.70.321. [DOI] [PubMed] [Google Scholar]
- 5.Krishnan K.R., Hays J.C., Blazer D.G. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- 6.Danovska M., Stamenov B., Alexandrova M., Peychinska D. Post-stroke cognitive impairment – phenomenology and prognostic factors. J IMAB. 2012;18 [Google Scholar]
- 7.Robinson R.G., Spalletta G. Poststroke depression: a review. Can J Psychiatry. 2013;55:341–349. doi: 10.1177/070674371005500602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Espárrago Llorcaa G., Castilla-Guerrab L., Fernández Morenoc M.C., Ruiz Dobladoa S., Hernándezd M.D.J. Post-stroke depression: an update. Neurologia. 2015;30:23–31. doi: 10.1016/j.nrl.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Rajan K.B., Aggarwal N.T., Wilson R.S., Everson-Rose S.A., Evans D.A. Association of cognitive functioning. Incident stroke, and mortality in older adults. Stroke J Cereb Circ. 2014;45:2563–2567. doi: 10.1161/STROKEAHA.114.005143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel M., Coshall C., Rudd A.G., Wolfe C.D. Natural history of cognitive impairment after stroke and factors associated with its recovery. Clin Rehabil. 2003;17:158–166. doi: 10.1191/0269215503cr596oa. [DOI] [PubMed] [Google Scholar]
- 11.Patel M.D., Coshall C., Rudd A.G., Wolfe C.D. Cognitive impairment after stroke: clinical determinants and its associations with long-term stroke outcomes. J Am Geriatr Soc. 2002;50:700–706. doi: 10.1046/j.1532-5415.2002.50165.x. [DOI] [PubMed] [Google Scholar]
- 12.Park J.H., Kim B.J., Bae H.J., Lee J., Lee J.Y., Han M.K. Impact of post-stroke cognitive impairment with no dementia on health-related quality of life. J Stroke. 2013;15:49–56. doi: 10.5853/jos.2013.15.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakling A.E., Aarsland D., Næss H., Wollschlaeger D., Fladby T., Hofstad H. Cognitive deficits in chronic stroke patients: neuropsychological assessment. Depression, and self-reports. Dement Geriatr Cogn Dis Extra. 2017;7:283–296. doi: 10.1159/000478851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chollet F., Tardy J., Albucher J.F., Thalamas C., Berard E., Lamy C. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): a randomised placebo-controlled trial. Lancet Neurol. 2011;10:123–130. doi: 10.1016/S1474-4422(10)70314-8. [DOI] [PubMed] [Google Scholar]
- 15.Gillespie D.C., Bowen A., Chung C.S., Cockburn J., Knapp P., Pollock A. Rehabilitation for post-stroke cognitive impairment: an overview of recommendations arising from systematic reviews of current evidence. Clin Rehabil. 2014;29:120–128. doi: 10.1177/0269215514538982. [DOI] [PubMed] [Google Scholar]
- 16.Loetscher T., Lincoln N.B. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst Rev. 2013;31 doi: 10.1002/14651858.CD002842.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung C.S., Pollock A., Campbell T., Durward B.R., Hagen S. Cognitive rehabilitation for executive dysfunction in adults with stroke or other adult non-progressive acquired brain damage. Cochrane Database Syst Rev. 2013;30 doi: 10.1002/14651858.CD008391.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maciocia G. 2015. The foundations of Chinese medicine. [Google Scholar]
- 19.Jiang H., Zhang X.H., Lu J., Meng H., Sun Y., Yang X.J. Antidepressant-like effects of acupuncture-insights from DNA methylation and histone modifications of brain-derived neurotrophic factor. Front Psychiatry. 2018;9:102. doi: 10.3389/fpsyt.2018.00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang J., Lu J., Cui S.F., Wang J.R., Tu Y. Effect of acupuncture on expression of brain-derived neurotrophic factor gene and protein in frontal cortex and hippocampus of depress rats. Zhen Ci Yan Jiu. 2012;37:20–24. [PubMed] [Google Scholar]
- 21.Lin R.H., Wu Y.N., Tao J., Chen B., Chen J.X., Zhao C.K. Electroacupuncture improves cognitive function through Rho GTPases and enhances dendritic spine plasticity in rats with cerebral ischemia-reperfusion. Mol Med Rep. 2016;13:2655–2660. doi: 10.3892/mmr.2016.4870. [DOI] [PubMed] [Google Scholar]
- 22.Liu W., Wu J., Huang J., Zhuo P., Lin Y.J., Wang L.L. Electroacupuncture regulates hippocampal synapitc plasticity via miR-134-mediated LIMK1 function in rats with ischemic stroke. Neural Plast. 2017;2017 doi: 10.1155/2017/9545646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wen T., Zhang X., Liang S., Li Z., Xing X., Liu W. Electroacupuncture ameliorates cognitive impairment and spontaneous low-frequency brain activity in rats with ischemic stroke. J Stroke Cerebrovasc Dis. 2018;27:2596–2605. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 24.Tseng S.P., Hsu Y.C., Chiu C.J., Wu S.T. A population-based cohort study on the ability of acupuncture to reduce post-stroke depression. Medicines (Basel) 2017;4 doi: 10.3390/medicines4010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Y., Bao Y., Wang S., Chu J., Li L. Efficacy on post-stroke depression treated with acupuncture at the acupoints based on ziwuliuzhu and prozac. Zhongguo Zhen Jiu. 2015;35:119–122. [PubMed] [Google Scholar]
- 26.Man S.C., Hung B.H., Ng R.M., Yu X.C., Cheung H., Fung M.P. A pilot controlled trial of a combination of dense cranial electroacupuncture stimulation and body acupuncture for post-stroke depression. BMC Complement Altern Med. 2014;14 doi: 10.1186/1472-6882-14-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Youn J.I., Sung K.K., Song B.K., Kim M., Lee S. Effects of electro-acupuncture therapy on post-stroke depressionin patients with different degrees of motor function impairments: a pilot study. J Phys Ther Sci. 2013;25:725–728. doi: 10.1589/jpts.25.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nie R.R., Huang C.H. Post-stroke depression treated with acupuncture and moxibustion: an evaluation of therapeutic effect and safety. Zhongguo Zhen Jiu. 2013;33:490–494. [PubMed] [Google Scholar]
- 29.Zhang G.C., Fu W.B., Xu N.G., Liu J.H., Zhu X.P., Liang Z.H. Meta analysis of the curative effect of acupuncture on post-strokedepression. J Tradit Chin Med. 2012;32:6–11. doi: 10.1016/s0254-6272(12)60024-7. [DOI] [PubMed] [Google Scholar]
- 30.Wu J.P. [Clinical observation on acupuncture treatment of 150 cases of post-stroke depression according to syndrome differentiation] Zhen Ci Yan Jiu. 2010;35:303–306. [PubMed] [Google Scholar]
- 31.He J., Shen P.F. Clinical study on the therapeutic effect of acupuncture in the treatment of post-stroke depression. Zhen Ci Yan Jiu. 2007;32:58–61. [PubMed] [Google Scholar]
- 32.Zhang L., Zhong Y., Quan S.L., Liu Y.H., Shi X.H., Li Z.G. Acupuncture combined with auricular point sticking therapy for post stroke depression: a randomized controlled trial. Chin Acupunct Moxibust. 2017;37:581–585. doi: 10.13703/j.0255-2930.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 33.Yang S., Ye H., Huang J., Tao J., Jiang C., Lin Z. The synergistic effect of acupuncture and computer-based cognitive training on post-stroke cognitive dysfunction: a study protocol for a randomized controlled trial of 2 × 2 factorial design. BMC Complement Altern Med. 2014;7:290. doi: 10.1186/1472-6882-14-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang J.J. Fujian University of Traditional Chinese Medicine; Fujian, China: 2011. Clinical study of effect of electroacupuncture on GV20 and EX-HN1 on stroke patients with cognitive impairment. [Thesis] [Google Scholar]
- 35.Jiang Y.J. Fujian University of Traditional Chinese Medicine; 2011. Electroacupuncture DU20 and DU24 treatment on cognitive impairment after stroke. [Thesis] [Google Scholar]
- 36.Yang J. Fujian University of Traditional Chinese Medicine; Fujian, China: 2011. The clinical study on cognitive impairment after stroke by using the treatment of electroacupuncture given at DU20 and GB20. [Thesis] [Google Scholar]
- 37.Liu H., Wang Y., Ren H. An effect of acupuncture on ADL and cognitive function in patients with ischemic stroke. Chin J Rehab Med. 2006:444–448. [Google Scholar]
- 38.Xie D.L., Zhu L.F., Liu H.Y. Application of P300 in scalp acupuncture for cognitive disorder due to cerebral infarction. J Acupunct Tuina Sci. 2012:26–28. [Google Scholar]
- 39.Leo R.J., Ligot J.S. A systematic review of randomized controlled trials of acupuncture in the treatment of depression. J Affect Disord. 2007:13–22. doi: 10.1016/j.jad.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 40.Smith C.A., Hay P.P., Macpherson H. Acupuncture for depression. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD004046.pub3. [DOI] [PubMed] [Google Scholar]
- 41.Deng M., Wang X.F. Acupuncture for amnestic mild cognitive impairment: a meta-analysis of randomised controlled trials. Acupunct Med. 2016:1–7. doi: 10.1136/acupmed-2015-010989. [DOI] [PubMed] [Google Scholar]
- 42.Liu F., Li Z.M., Jiang Y.J., Chen L.D. A meta-analysis of acupuncture use in the treatment of cognitive impairment after stroke. J Altern Complement Med. 2014;20:535–544. doi: 10.1089/acm.2013.0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Montori V.M., Wilczynski N.L., Morgan D., Haynes R.B., Hedges Team Optimal search strategies for retrieving systematic reviews from Medline: analytical survey. BMJ. 2005;330:68. doi: 10.1136/bmj.38336.804167.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilcynski N.L., Haynes R.B., Hedges Team. EMBASE search strategies achieved high sensitivity and specificity for retrieving methodologically sound systematic reviews. J Clin Epidemiol. 2007;60:29–33. doi: 10.1016/j.jclinepi.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 45.Higgins J.P.T., Green S. The Cochrane Collaboration; 2011. Cochrane handbook for systematic reviews of interventions. [Google Scholar]
- 46.World Health Organization: WHO Monica Project: MONICA manual. Part IV: Event Registration. http://www.ktl.fi/publications/monica/manual/part4/iv-2.htm-s1-1 (accessed 01.04.19).
- 47.America Stroke Association criteria. http://www.strokeassociation.org/STROKEORG/AboutStroke/TypesofStroke/Types-of-Stroke_UCM_308531_SubHomePage.jsp (accessed 01.04.19).
- 48.Lu S.K. 7th ed. 2002. Acupuncture and moxibustion law. [Google Scholar]
- 49.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;21:358. doi: 10.1136/bmj.j4008. j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Higgins J.P.T., Thompson S.G., Deeks J.J. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Folstein M.F., Folstein S.E., McHugh P.R. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 52.Kobak K.A. 2010. Hamilton Depression Rating Scale. [Google Scholar]
- 53.Katz S., Apkom C.A. Studies of illness of the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 54.Hansenne M., Pitchot W., Gonzalez Moreno A., Zaldua I.U., Ansseau M. Suicidal behavior in depressive disorder: an event-related potential study. Biol Psychiatry. 1996;40:116–122. doi: 10.1016/0006-3223(95)00372-x. [DOI] [PubMed] [Google Scholar]
- 55.Oehlert M.E. Accuracy of the Neurobehavioral Cognitive Status Examination's screen-metric approach. Rehabil Psychol. 1996;162 doi: 10.1002/(sici)1097-4679(199711)53:7<733::aid-jclp11>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 56.Collin C., Wade D.T., Davies S., Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10:61–63. doi: 10.3109/09638288809164103. [DOI] [PubMed] [Google Scholar]
- 57.Shen Z.H., Ke J., Zhi Z. Diagnostic criteria and disability scale for cerebrovascular diseases. Chin Soc Neurol. 1996:379–380. [Google Scholar]
- 58.Fugl-Meyer A.R., Jaasko L., Leyman I., Olsson S., Steglind S. The post- stroke hemiplegic patient – a method for evaluation of physical performance. ScandJ Rehabil Med. 1975:13–31. [PubMed] [Google Scholar]
- 59.Venn R.D. The Sandoz Clinical Assessment-Geriatric (SCAG) Scale. A general-purpose psychogeriatric rating scale. Gerontology. 1983:185–198. doi: 10.1159/000213113. [DOI] [PubMed] [Google Scholar]
- 60.Keith R.A., Granger C.V., Hamilton B.B., Sherwin F.S. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987:6–18. [PubMed] [Google Scholar]
- 61.Uher R. Adverse reactions to antidepressants. Br J Psychiatry. 2009:202–210. doi: 10.1192/bjp.bp.108.061960. [DOI] [PubMed] [Google Scholar]
- 62.Liu W.L., Wong J., Tao J. A systematic review of the effect of electroacupuncture on cognitive dysfunction after ischemic stroke. Med Inform. 2015;28:64. [Google Scholar]
- 63.Zhang Y., Tang W., Song X., Wu S., Zhang G.Y., Xu H. Systematic evaluation and meta-analysis of the effect of acupuncture and moxibustion combined with cognitive rehabilitation training on cognitive impairment after stroke. Shanghai J Acupunct Moxibust. 2015;34:1013. [Google Scholar]
- 64.Xiong J., Liao W.J., Liu Q., Zhang Z., Guo Y., Xue L. A systematic review of stylus after treatment of cognitive dysfunction after stroke. Chin J Rehabil Med. 2016;31:333–339. [Google Scholar]
- 65.Zhang W., Sun J.H., Gao Y., Pei L.X., Wu X.L., Chen L. System review on treating post-stroke depression with acupuncture. World J Acupunct-Moxibust. 2014;24:52–59. [Google Scholar]
- 66.Zhang J.P., Chen J., Chen J.Q., Li X.H., Lai X.Y., Zhang S.Q. Early filiform needle acupuncture for poststroke depression: a meta-analysis of 17 randomized controlled clinical trials. Neural Regener Res. 2014;9:773–784. doi: 10.4103/1673-5374.131590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xiong J., Du Y.H., Liu J.L., Lin X.M., Sun P., Xiao L. Acupuncture versus western medicine for post stroke depression: a systematic review. J Evid-Based Med. 2010;10:179–192. [Google Scholar]
- 68.Xu Y. Guangzhou University of Chinese; 2014. Acumulative meta-analysis study of comparing the efficacy of the treatment of post stroke depression by acupuncture and western medicine. [Google Scholar]
- 69.Niu L. Chengdu University of Traditional Chinese Medicine (Acupuncture and Massage College); 2014. Systematic review of electro-acupuncture treatment for post-stroke depression. [Google Scholar]
- 70.Que F.X. Acupuncture compares with Prozac for Post stroke depression: Systematic review and meta-analysis. Acupuncture and Massage College (2014)./F.X. Que, Y.Z. Wen & W.C. Wang. A systematic review of the efficacy of acupuncture versus prozac in the treatment of post-stroke depression. Hunan J Trad Chin Med. 2018;34:141–145. [Google Scholar]
- 71.Li X.H., Chen J.Q., Wang H.T., Chen Q.Y., Wang S.X. Comparison between effects of electroacupuncture and antidepressants for post stroke depression: a systematic review. Chin Gen Pract. 2012;15:802–806. [Google Scholar]
- 72.Zhan J., Tan F., Cheng N.F., Tan J.Q. Efficacy of electroacupuncture and antidepressants for post-stroke depression: a systematic review of randomized controlled trials. Chin Arch Trad Chinese Med. 2016;34:2379–2383. [Google Scholar]
- 73.Wu Y.Q., Yang N.Z. Therapeutic effect of Xingnaoqiaoqiao acupuncture on post-stroke depression. J Qiqihar UnivMed. 2015;36:1017–1019. [Google Scholar]
- 74.Li X.B., Wang J., Xu A.D., Huang J.M., Meng L.Q., Huang R.Y. Clinical effects and safety of electroacupuncture for the treatment of post-stroke depression: a systematic review and meta-analysis of randomised controlled trials. Acupunct Med: J Br Med Acupunct Soc. 2018;36:284–293. doi: 10.1136/acupmed-2016-011300. [DOI] [PubMed] [Google Scholar]
- 75.Hoffmann T., Bennett S., Koh C.L., McKenna K.T. Occupational therapy for cognitive impairment in stroke patients. Cochrane Database Syst Rev. 2010;9 doi: 10.1002/14651858.CD006430.pub2. CD006430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.das Nair R., Cogger H., Worthington E., Lincoln N.B. Cognitive rehabilitation for memory deficits after stroke. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD002293.pub3. CD002293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lipsey J.R., Pearlson G.D., Robinson R.G., Rao K., Price T.R. Nortriptyline treatment of post-stroke depression: a double-blind study. Lancet. 1984;323:297–300. doi: 10.1016/s0140-6736(84)90356-8. [DOI] [PubMed] [Google Scholar]
- 78.Andersen G., Vestergaard K., Lauritzen L. Effective treatment of poststroke depression with the selective serotonin reuptake inhibitor citalopram. Stroke J Cereb Circ. 1994;25:1099–1104. doi: 10.1161/01.str.25.6.1099. [DOI] [PubMed] [Google Scholar]
- 79.Remick R.A. Anticholinergic side effects of tricyclic antidepressants and their management. Prog Neuropsychopharmacol Biol Psychiatry. 1988;12:225–231. doi: 10.1016/0278-5846(88)90039-5. [DOI] [PubMed] [Google Scholar]
- 80.Coupland C., Dhiman P., Morriss R., Arthur A., Barton G., Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ. 2011;343 doi: 10.1136/bmj.d4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bowen A., Knapp P., Gillespie D., Nicolson D.N., Vail A. Non-pharmacological interventions for perceptual disorders following stroke and other adult, acquired, nonprogressive brain injury. Cochrane Database Syst Rev. 2011;4 doi: 10.1002/14651858.CD007039.pub2. CD007039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Smoller J.W., Allison M., Cochrane B.B., Curb J.D., Perlis R.H., Robinson J.G. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women's Health Initiative Study. Arch Intern Med. 2009;169:2128–2139. doi: 10.1001/archinternmed.2009.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Robinson R.G. vol. 2. Cambridge University Press; New York: 2006. p. 470. (The clinical neuropsychiatry of stroke). [Google Scholar]
- 84.Bolla-Wilson K., Robinson R.G., Starkstein S.E., Boston J., Price T.R. Lateralization of dementia of depression in stroke patients. Am J Psychiatry. 1989;146:627–634. doi: 10.1176/ajp.146.5.627. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data related to this study are within this article (Refer to Appendix).