Abstract
Tobacco smoking with a water pipe or hookah is increasing globally. There are millions of water pipe tobacco smokers worldwide, and in the United States, water pipe use is more common among youth and young adults than among adults. The spread of water pipe tobacco smoking has been abetted by the marketing of flavored tobacco, a social media environment that promotes water pipe smoking, and misperceptions about the addictive potential and potential adverse health effects of this form of tobacco use. There is growing evidence that water pipe tobacco smoking affects heart rate, blood pressure regulation, baroreflex sensitivity, tissue oxygenation, and vascular function over the short term. Long-term water pipe use is associated with increased risk of coronary artery disease. Several harmful or potentially harmful substances present in cigarette smoke are also present in water pipe smoke, often at levels exceeding those found in cigarette smoke. Water pipe tobacco smokers have a higher risk of initiation of cigarette smoking than never smokers. Future studies that focus on the long-term adverse health effects of intermittent water pipe tobacco use are critical to strengthen the evidence base and to inform the regulation of water pipe products and use. The objectives of this statement are to describe the design and operation of water pipes and their use patterns, to identify harmful and potentially harmful constituents in water pipe smoke, to document the cardiovascular risks of water pipe use, to review current approaches to water pipe smoking cessation, and to offer guidance to healthcare providers for the identification and treatment of individuals who smoke tobacco using water pipes.
Keywords: AHA Scientific Statements, cardiovascular disease, epidemiology, nicotine, particulate matter, smoking water pipes, tobacco, volatile organic compounds
Recent estimates suggest that between 0.85 and 1.1 billion people use tobacco products world-wide.1 These products include cigarettes, cigars, cigarillos, pipes, water pipes, and smokeless tobacco. The global use of electronic cigarettes (e-cigarettes) remains unknown, but among the tobacco products queried, manufactured cigarettes are favored by most smokers (82%). The use of tobacco is particularly high in middle-income countries such as China, India, and Russia. Nearly 300 million individuals in China and 275 million in India use tobacco products daily.1 In countries such as Russia and the Ukraine, 50% to 60% of adult men use some form of tobacco.1 The use of tobacco products is also high in high-income countries such as the United States and the United Kingdom. Although there have been significant declines in the rate of tobacco product use in some countries, an increase in population has led the number of cigarette smokers worldwide to grow from 721 million in 1980 to 967 million in 2012.2 Tobacco, therefore, is likely to remain a major global public health threat for the foreseeable future.
Tobacco use remains a leading cause of disease and premature death. The World Health Organization estimates that tobacco accounts for 9% of deaths world-wide3 and that globally nearly 6 million people die of tobacco-related causes every year.4 To date, nearly 100 million deaths are attributable to tobacco use, and if current use patterns persist, tobacco use could kill >1 billion people in this century.4 Extensive literature documents the adverse health effects of tobacco use, and although cigarette smoking increases the risk of many chronic illnesses, cardiovascular disease (CVD; inclusive of stroke) remains a leading cause of death in smokers.5 In the United States, as many as 30% of the all coronary heart disease deaths each year are related to cigarette smoking,6 and smoking doubles the risk of premature cardiovascular mortality.7
As a result of the recognition of the high impact of tobacco use on cardiovascular health, tobacco control efforts are underway worldwide. In the United States, the American Heart Association (AHA) supports the implementation of proven population-based tobacco control interventions, including antitobacco mass media campaigns and comprehensive smoke-free laws at the state and local levels. Proven tobacco prevention and control measures, including comprehensive clean indoor air laws, increases in tobacco product prices, restriction of tobacco sales to those ≥21 years of age, and US Food and Drug Administration regulation of tobacco products, are critical population-based strategies endorsed by the AHA.8 The AHA identifies never having tried smoking and never having smoked or having quit >12 months as 1 of the 7 components of ideal cardiovascular health in Lifés Simple 7, selected on the basis of their contributions to incident CVD.9
Although the AHA has published policy statements on smokeless tobacco10 and e-cigarettes,11 to date, no AHA scientific statement has addressed the cardiovascular impact of water pipe tobacco smoking. Hence, the objectives of this statement are to describe the design and operation of water pipes and the patterns of use by adults and youths, to identify different harmful or potentially harmful constituents (HPHCs) of water pipe smoke, and to review potential cardiovascular effects of water pipe use. The statement also offers a broad range of proven strategies to reduce and prevent water pipe tobacco use and associated adverse cardiovascular effects, discusses knowledge gaps that still need to be addressed, and provides concrete guidance to health-care providers for the identification and treatment of patients who smoke water pipes.
DESIGN AND OPERATION
Water pipe that is used to smoke tobacco is known by many different terms, including hookah, narghile, argileh, shisha, and goza. This review uses the term water pipe to universally denote this product class. Over the years, the water pipe has had a variety of configurations, but as used today, it consists of a head or bowl (where tobacco is placed), a body, a water base, and a hose that ends with a mouthpiece (Figure 1). Burning charcoal briquettes/pieces are placed on top of the tobacco-filled bowl, which is usually made of clay, marble, or glass. The charcoal pieces are often separated from the tobacco by a perforated aluminum foil to allow the heated air to pass through the tobacco, and the holes in the bottom of the head allow the smoke to pass down through the stem, which can be of varying sizes and lengths. The down stem is immersed in water to allow smoke to bubble through, which cools and humidifies the smoke. Sometimes, mint leaves, fruits, or crushed ice are added to the water. Smoke emerging from the water passes through a hose, usually made of leather, vinyl, or plastic, which allows the smoke to be drawn by the user. Some water pipes have rigid mouth-piece reeds, whereas others may have multiple hose ports for simultaneous use by several smokers. The end of the hose is usually capped by a metal, wooden, or plastic mouth tip that can be covered by a disposable mouthpiece (to allow multiple users and repeated use of the same water pipe hose).
Figure 1. A typical water pipe and its main components.
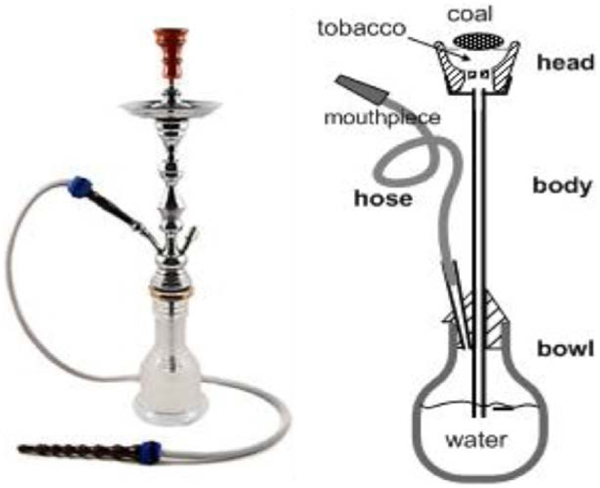
Adapted from Maziak et al.12 Copyright © 2015, The Authors. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC-BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.
Both the water pipe design and use patterns can affect smoke constituents and flavor. During a smoking session, the charcoal briquettes are adjusted and replenished to maintain the desired taste, smoke concentration, and smoke volume. Either natural or quick-lighting charcoals, which are combusted, are used to heat the tobacco. Although not systematically studied, the extent of nicotine generated from tobacco is likely affected by the heating temperature, tobacco mixture used (including flavors, humectants, and additives), puffing topography, water pipe size, and amount of water in the water pipe bowl.13,14 Water pipe tobacco is usually a combination of dried fruit, tobacco, and humectants. Data from many countries show that maassel is the currently preferred form of tobacco for water pipe smokers, especially among youth and young adults.12,15–18 Maassel (Arabic for honeyed) is a sweetened and flavored tobacco mixture. Before the introduction of maassel, most water pipe smokers globally used some form of raw tobacco that was crushed, mixed with water, squeezed, and molded before use.12 Unlike the smooth aromatic smoke produced from maassel, this method usually produces a strong, harsh smoke.12 In the United States, nearly 90% of youth use flavored tobacco when smoking a water pipe.16,19
Water pipes and their components (eg, charcoal, devices, and tobacco) and accessories can be purchased from dedicated supply shops and increasingly from internet vendors.19 Some vendors claim that the harmful effects of water pipe smoking are reduced by using accessories such as electronic heaters, mouthpiece Alters, water additives, and mesh fittings to create smaller bubbles. However, the veracity of these claims remains uncertain. Conventional water pipes are different from the electronic devices known as e-hookahs, e-shisha, or hookah pens, which are electronic nicotine delivery systems that involve heating of a liquid (often containing nicotine) that can be flavored to mimic the taste of flavored water pipe tobacco. These electronic devices do not involve the use of water pipe tobacco products/mixtures or charcoal combustion, 2 main features of conventional water pipes.
Water pipe tobacco is sold in a wide variety of flavors, including apple, banana, berry, cherry, chocolate, coconut, coffee, cola, grape, kiwi, lemon, licorice, mango, mint, orange, peach, pineapple, rose, strawberry, tutti fruity, vanilla, and watermelon.20 The names given to water pipe tobacco leverage the positive association that people have with fruit, desserts, soft drinks, and candy. Flavored products are sold in colorful packaging that usually does not carry health warnings and are targeted to younger consumers.21,22 The sweetened aroma of water pipe tobacco is not as harsh as cigarette smoke, and water pipe tobacco is associated with less throat and upper respiratory tract irritation, thereby masking the harshness of the tobacco smoke and making it easier to start and continue smoking.16,23
EPIDEMIOLOGY
Patterns of Water Pipe Smoking Among Youth
Prevalence of Use
The worldwide use of water pipes is extensive. In the 2016 NYTS (National Youth Tobacco Survey), a US nationally representative school-based study, 4.8% (95% CI, 4.1–5.7%) of high school students (n=700 000) reported smoking tobacco using a water pipe over the prior 30 days, with similar rates among male (4.5%) and female (5.1%) students.24 In the 2016 MTF survey (Monitoring the Future), 13.0% of 12th graders reported water pipe tobacco use in the past year, with boys (15%) more likely to report water pipe use than girls (11%).25 In wave 1 (2013–2014) data from the PATH study (Population Assessment of Tobacco and Health) of >13 000 youths 12 to 17 years of age,26 7.5% (95% CI, 6.8–8.2) reported ever water pipe use, and 1.7% reported smoking water pipe tobacco in the prior 30 days. Ever use and past-30-day use were higher among 15- to 17-year-olds (13.0% and 2.9%, respectively) than 12- to 14-year-olds (2.0% and 0.5%, respectively). Ever water pipe use was higher among bisexual (19.3%) and gay/lesbian (17.7%) 14- to 17-year-olds than those identified as heterosexual (10.4%). Ever water pipe use was comparable between male (7.1%) and female (7.8%) participants but increased with each year of age.26
Trends in Use
The NYTS found a nonlinear increase in past-30-day (current) water pipe tobacco use among high school students (4.1% to 4.8%) between 2011 and 201624; past-30-day use among high school students increased between 2011 and 2014; and use peaked at 9.4% in 2014 before declining to 4.8% in 2016. The MTF study found a steady increase in annual water pipe use among 12th graders from 2010 (17.1%) to 2014 (22.9%), followed by a decrease in 2015 (19.8%) and 2016 (13.0%).25 Reasons for this decline remain unclear.
International Use
The spread of water pipe use among younger populations is global. Data from the Global Youth Tobacco Survey, which included 13- to 15-year-olds in 7 Middle Eastern countries, showed that the rates of water pipe smoking ranged from 9% to 15%, which were higher than cigarette smoking rates in almost all countries studied.27 Studies from some countries now show that water pipe tobacco smoking is eclipsing cigarette smoking. For example, a study of students in the United Kingdom during 2011 to 2012 found that current water pipe use was more than twice as common as cigarette smoking (7.6% versus 3.4%).28
Characteristics of Water Pipe Smoking Among Youth
Flavored Use
Data from the 2014 NYTS revealed that 63.8% of high school students who reported water pipe use within the prior 30 days smoked flavored tobacco. Data from wave 1 of the PATH study showed that among youth 12 to 17 years of age, 89% of those who had ever used water pipe reported that their first use involved a flavored product.29
Frequency of Use
Most youth use water pipes intermittently. Data from PATH wave 1 revealed that <1% (0.1%) of youth 12 to years of age use water pipe daily.26
Polytobacco Use
The PATH wave 1 data showed that 43% of youth who used tobacco in the past 30 days used >1 tobacco product. Of the 116 different product combinations, the combination of e-cigarettes and water pipe was the third most common one reported (5% of past-30-day tobacco users). An additional 4% of past-30-day tobacco users reported smoking cigarettes and water pipe, and 3% used cigarettes, e-cigarettes, and water pipes.26 Longitudinal studies in the Middle East found that the risk of initiation of cigarette smoking was higher among water pipe smokers than among never smokers (adjusted hazard ratio, 1.67 [95% CI, 1.46–1.92]) and that the risk increased with the frequency of water pipe smoking.30
Reasons for and Perceptions About Water Pipe Smoking Among Youth
Reasons for Use
Youths cite several reasons for water pipe use: entertainment, relaxation, boredom, curiosity, and somatic experiences, including the pleasant taste and smell, as well as tactile and visual elements, specifically the voluminous smoke.15 Culture is often cited as a reason for use among those from the Middle East, although for many years, use was largely confined to older men. However, use became more prominent among young people in the 1990s with the introduction and mass marketing of flavored water pipe tobacco.31 Youth indicate that water pipe smoking allows them to meet others with a shared cultural background.32 Data from wave 1 of PATH found that 12- to 17-year-olds reported using water pipes use for several reasons, including the following: ˝I like socializing while using them˝ (80%); ˝comes in flavors I like˝ (79%); ˝less harmful to me than cigarettes˝ (61%); ˝affordability˝ (44%); and ˝people who are important to me use them˝ (36%).29
Perceptions About Use
Water pipe use among youth is influenced by perceptions of its addictiveness and harm. Many youth believe that the chance of becoming addicted to water pipe is low, perhaps because of their intermittent use patterns.29 The youth also perceive a lower risk of health harms associated with water pipe smoking compared with cigarette smoking. For example, youth water pipe users and nonusers often believe that it is safer than smoking cigarettes because they think that the water ˝filters out toxins.˝33,34 The wide variety of flavors of water pipe tobacco and the cooling features of the water produce a mild smoke, which may lead to misperceptions of safety.16 Youth also cite the absence of health warnings and media campaigns describing harms as a reason that they perceive water pipes to be a safer tobacco product.16
Interest in Water Pipe Smoking
The increasing interest in water pipe smoking is evident from the volume of related online searches. Between January 2004 and December 2013, water pipe online shopping searches increased by 291%, with hookah being the most common water pipe search term (190 000 average weekly searches), followed by shisha (127 000 searches). Other relevant searches include Starbuzz, which is a common brand of water pipe tobacco and accessories. Comparing the relative search volume in 2013 for water pipe across the United States, United Kingdom, Australia, and Canada shows that the online interest in water pipe was highest in the United States (100% relative search volume, December 2013), followed by the United Kingdom (48.2% mean weekly relative search volume for 2013), Canada (42.6%), and Australia (27.2%).35
Growth in water pipe establishments or lounges as key places for smoking continues, with many locations in areas of high population density or near colleges and universities. In 2011, there were an estimated 725 US-based water pipe establishments with at least 1 location in 43 states and the District of Columbia.34 By 2015, 1690 US water pipe establishments were reported, primarily in large metropolitan areas (ie, Los Angeles, New York, Chicago, Atlanta, and Miami). Most of these establishments were within 3 to 9 miles of college or university campuses with a student population of ≥20 000.36 These establishments or lounges could also influence youth interest in and use of these products. Nearly 30% of high school students in San Diego learned about water pipe smoking by seeing a water pipe lounge, and current water pipe users were more likely to know of a water pipe lounge in their community.37 Furthermore, lounges have reinforced pro-water pipe messages in advertisements and on social networking sites.38
Influence of Social Media
Pro–water pipe messages on social media, which are widespread and unregulated, are likely to add to the proliferation of water pipe use. A study of the profiles of 307 Facebook users, recruited from among students at 2 US universities, found that 27.8% of participants had ever smoked water pipe and 5.3% of the profiles contained water pipe references.36 Water pipe users reported smoking tobacco (78%), hash (12%), or both tobacco and marijuana/hash (10%) in their apparatus. There were no significant differences in water pipe use based on age, sex, or race.39 Nearly a quarter of the pro-water pipe tweets on Twitter are commercial promotions of water pipe at bars, clubs, events, and other venues, encouraging the social aspects of water pipe that appeal to young people.40 In 2014, >12 000 water pipe–related tweets were sent daily, mostly from Twitter users with high influence and many who are pro water pipe. Eighty-seven percent of these tweets normalized water pipe or promoted its use, whereas 7% were against water pipe or discouraged its use.41 Positive tweets from individuals tend to emphasize the enjoyable experience of water pipe smoking, and tweets from business entities often highlight the potential to have a positive water pipe smoking experience.42
A vast majority of the water pipe pins on Pinterest are image-based40 and more often portray water pipe smoking in a more positive than negative light, which tends to trigger more repins, likes, and higher levels of engagement.43 On YouTube, water pipe–related videos are more likely than cigarette-related videos to portray tobacco use positively, to describe smoking water pipe tricks, and to provide practical information on how to smoke water pipe. Some videos frame water pipe preparation as an art form or hobby, requiring patience and experience to cultivate and perfect.44
Enticement to engage in water pipe use by water pipe establishments has been depicted on photo-based and microblog websites. For example, a recent study of water pipe promotion and use on Instagram found cross-promotion of water pipe and alcohol use by water pipe establishments, suggesting that these venues regularly depict and promote polysubstance use.45 On Tumblr, the most prominent features portrayed by those who post include references to or images of water pipes, sexuality, socializing, alcohol, water pipe smoke, and tricks performed with the water pipe smoke.46
Patterns of Water Pipe Smoking Among Adults
Prevalence of Use
Water pipe use varies across population subgroups. During 2013 to 2014, the proportion of US adults (age >18 years) who reported using a water pipe in the NATS (National Adult Tobacco Survey) everyday, some days, or rarely was 4.3%, which translates to ≈10 million adults.47 The proportion who reported at least some frequency of water pipe use varied with sociodemographic groups, most notably with age. Prevalence was highest among those 18 to 24 years of age (13.6%) compared with those 25 to 44 (9.0%), 45 to 64 (4.7%), or ≥65 (1.5%) years of age. Young adults, 18 to 24 years of age, accounted for 55.8% of water pipe smokers nationwide.47
Trends in Use
Although water pipe use has generally increased over time, this pattern has varied with age. In the United States, data on trends in adult water pipe tobacco use are limited given that questions about these products were first added to national surveys beginning in 2009 to 2010 and that different definitions, methods, and samples were used in different populations over time. Findings from the NATS indicate that past-30-day (current) water pipe use among US adults has generally increased from 1.5% during 2009 to 2010 to 3.2% in 2013 to 2014.47,48 This increase was driven largely by young adults, with prevalence among those 18 to 24 years of age increasing from 7.8% in 2009 to 2010 to 15.8% in 2013 to 2014.47,48
International Use
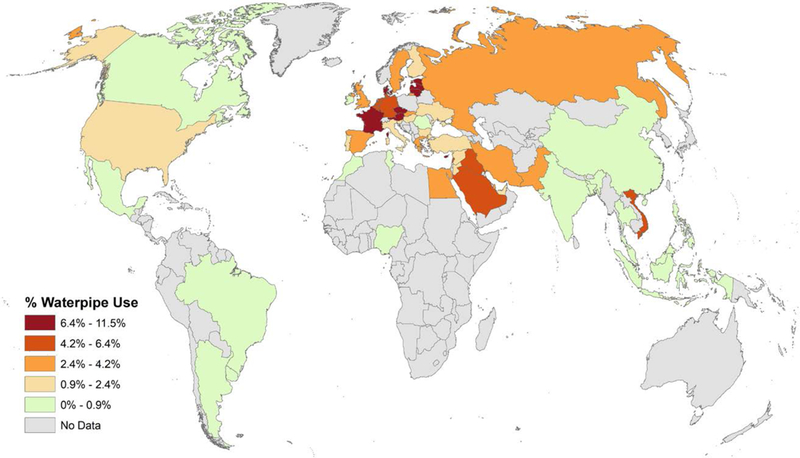
Outside the United States, data on prevalence and trends of water pipe use indicate markedly increasing interest in these products, including among adults. The worldwide prevalence of hookah use12,49–53 is shown in Figure 2. The rates of current use, however, are generally lower among adults compared with young people.12 Moreover, use varies considerably across countries and regions.12,54 Among individuals ≥15 years of age from 44 countries who participated in the Global Adult Tobacco Survey or the Special Eurobarometer 385 during 2008 to 2012, there was virtually no water pipe smoking in assessed countries from the Americas, Southeast Asia, and Africa.54 Within the Eastern Mediterranean region, prevalence of current water pipe use was 3.3% in Egypt.54 In the Western Pacific region, prevalence ranged from virtually no use in China, the Philippines, and Malaysia to 6.4% in Vietnam.54 Some of the countries with the highest prevalence of adult water pipe smoking are located in Europe; current use was highest in Denmark (8.4%), Cyprus (8.5%), Lithuania (9.0%), and Latvia (11.5%).54 Across many countries and regions, current use of water pipes is generally higher / among men than among women.54
Figure 2. Global prevalence of adult water pipe smoking.
Characteristics of Water Pipe Smoking Among Adults
Flavored Use
Flavored tobacco is commonly used by water pipe smokers. During 2013 to 2014, an estimated 82.3% of US adults assessed via the NATS who used water pipe in the prior 30 days reported using a flavored product.55 Among users, the most prevalent flavor used was fruit (74.0%), followed by menthol/mint (18.9%), candy/chocolate/other sweet (17.4%), clove/spice/herb (4.3%), alcohol (3.2%), and other (3.0%).55 Among those who used water pipe in the past 30 days, flavored use was similar among men (81.3%) and women (83.6%) and generally decreased with age. Among 18- to 24-year-olds who used a water pipe in the past 30 days, flavored product use was 85.9% compared with 66.8% among 45- to 64-year-olds.55 Flavored use did not vary by race/ethnicity.55 Flavored use ranged from 81.1% among those with annual household income of >$100 000 to 85.4% among those with annual household income of <$20 000.55 Among past-30- day users, the prevalence of flavored use ranged from 75.2% among those with a bachelor’s degree or higher to 83.9% among those with less than a high school diploma.55 Flavored use was 89.6% among lesbian, gay, or bisexual adults compared with 81.2% among heterosexual adults.55 By US region, flavored use was 77.7% in the West, 82.1% in the South, 86.1% in the Midwest, and 86.3% in the Northeast.55 During 2013 to 2014, the prevalence of flavored water pipe use was 83.8% among current cigarette smokers, 82.2% among recent former cigarette smokers, 81.2% among long-term former cigarette smokers, and 81.4% among never cigarette smokers.55
Frequency of Use
Many water pipe users also partake of other tobacco products. During 2013 to 2014, the proportion of US adults assessed via the NATS who reported using a water pipe every day or some days was 0.6% (1.4 million adults); with the inclusion of adults who reported that they rarely use a water pipe, the proportion increased to 4.3% (10.0 million adults).47 Among adults who smoked during the prior 30 days, the use of flavored water pipe was more common among some-days users (91.7%) compared with rare users (80.8%).55
Polytobacco Use
Among US adults who reported using tobacco during 2013 to 2014 assessed via the PATH survey, 62.2% used 1, 22.5% used 2, and 15.3% used ≥3 types of tobacco products.26 Among the 331 reported combinations of polytobacco use among US adult tobacco users, the combination of cigarettes and e-cigarettes was the most common (23%), followed by the use of cigarettes and water pipes (6%).26 In addition, 3% of US adult tobacco users reported current cigarette, e-cigarette, and water pipe use; 2% reported current e-cigarette and water pipe use; 2% reported current cigarillo and water pipe use; and 1% reported traditional cigar and water pipe use.26 Current water pipe tobacco smoking is associated with increased risk of cigarette smoking among young adults; among those who had never smoked cigarettes, those who smoked water pipe at least rarely were 2.3 times more likely to begin cigarette smoking compared with those who were not current water pipe smokers.56
Reasons for and Perceptions About Water Pipe Smoking Among Adults
Reasons for Use
Multiple reasons have been cited for water pipe tobacco smoking, including social and cultural acceptability. More specifically, some adult water pipe smokers, particularly those from the Middle East or of Middle Eastern descent, report that water pipe use is rooted in their cultural traditions and occurs during family and other social gatherings.57 Additional factors influencing water pipe use include ease of access through family, friends, and storefronts such as cafés and bars.57 In addition, promotion of water pipes through traditional advertising, the internet, and social networks is a driver for water pipe initiation and use, particularly among younger adults.57 Finally, some studies suggest that smoking water pipe may have self-perceived positive psychological effects on users, including improved concentration and self-efficiency, as well as reductions in stress, anger, and depression,57 perhaps in part as a result of nicotine exposure, which can increase attention and scores in vigilance tasks.58
Perceptions About Use
The use of water pipes among adults may be influenced by misperceptions about its addictiveness and health risks, particularly among younger adults.57 For example, some users perceive that the probability of addiction is low if the product is used occasionally, and most users believe that they can easily quit water pipe smoking.57 There is evidence, however, that adolescent water pipe users begin exhibiting signs of dependence relatively quickly (<1 year after their first use) and when smoking only occasionally (7.5 water pipes per month or 6 d/mo, on average).59 The initiation and use of water pipes might also be influenced by perceptions of the risk of smoking water pipes compared with cigarettes.For example, 1 study found that the majority of water pipe users (58.3%) perceived water pipe smoking to be less harmful than cigarette smoking, with more frequent users being more likely to have this perception.60 This perception could be based on the belief that these products contain less nicotine and harmful chemicals than cigarettes because the smoke passes through water.57 Other studies, however, indicate that some users consider the risk of smoking water pipe to be equal to or more than that of smoking cigarettes57 and that individuals who receive educational information about the harms of water pipe smoking report greater perceived risk about the use of these products.61
WATER PIPE SMOKE CONSTITUENTS
The range of HPHCs found in water pipe tobacco smoke is similar to that of the chemicals found in the smoke of combustible cigarettes.53 There are, however, important differences. The HPHC profiles of water pipes differ from those of cigarettes because of the use of charcoal to heat the tobacco, the temperature at which the tobacco is heated or burned, and the volume of delivered smoke.53 Moreover, the patterns of water pipe use and cigarette smoking differ, resulting in differing exposures. In water pipes, tobacco is heated to ≈450°C with typical quick-lighting charcoal, which is lower than the temperature in cigarettes (≈900°C).13 Thus, the temperature attained in water pipes is usually below that required for pyrolysis or outright combustion. Nevertheless, under standard smoking machine protocols based on Middle Eastern smoking patterns (which may be different from those in the United States),13 a single water pipe smoking session generates on average 70 times higher levels of tar, 2.5 times greater levels of phenanthrene, and 11-fold higher levels of carbon monoxide (CO) than cigarettes. Even when normalized per 1 mg of nicotine in the tobacco, the CO yield is ≈3-fold higher from water pipe than from a standard cigarette.14 It is likely, however, that the true level of HPHC exposure differs from the levels generated by smoking machines because of differences in use patterns.
Water pipe smoking is a social activity, and typical users are likely to be exposed to secondhand smoke from the product itself (ie, sidestream smoke), as well as secondhand smoke exhaled by users (ie, mainstream smoke). The complex patterns of exposure during typical water pipe smoking sessions remain unclear, but biomarker-based estimates provide a reasonable assessment of HPHC exposure in water pipe users. The main HPHCs of cardiovascular concern in water pipe users include nicotine, particulate matter (PM), CO, volatile organic chemicals, polycyclic aromatic hydrocarbons (PAHs), acrolein, heavy metals, and arsenic. The comparative levels of different HPHCs in water pipe emissions versus combustible cigarettes13,62,63 are shown in Figure 3.
Figure 3. Approximate abundance of harmful or potentially harmful substances in water pipe tobacco smoke relative to standard cigarette smoke.
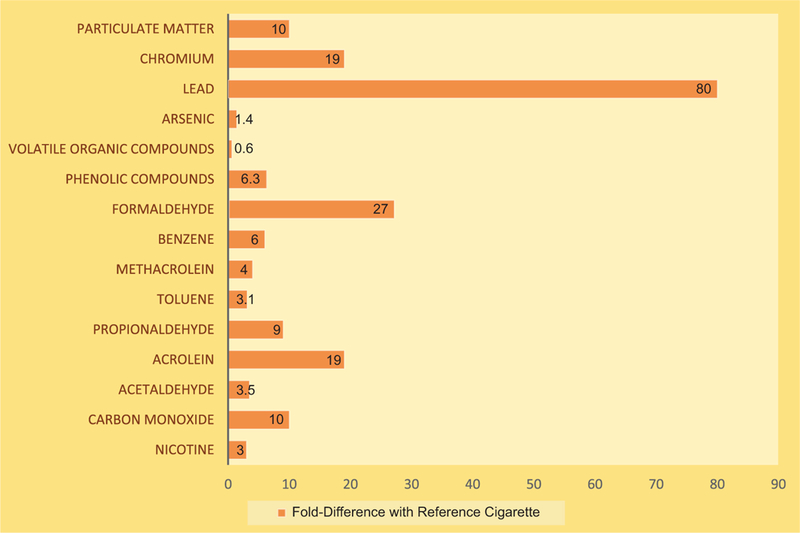
Data are presented as fold difference between a typical session of water pipe use and a single cigarette.13,62,63
Nicotine
Like cigarette smoke, water pipe smoke is high in nicotine. A meta-analysis of water pipe users from 4 countries indicates that, on average, daily use of water pipe tobacco produced a 24-hour urinary cotinine level of 0.783 mg/mL, which is equivalent to smoking 10 cigarettes per day. Even a single session of water pipe use over a 4-day period delivered the nicotine equivalent of smoking 2 cigarettes over a 1-day period.64 During a typical isolated water pipe use session in a clinical research unit, water pipe tobacco smokers had a systemic dose of 2.5 mg of nicotine, which is equivalent to the dose of smoking 2 to 3 cigarettes.65 In a naturalistic study of water pipe tobacco smokers in water pipe bars or lounges, a 73-fold increase in urine nicotine concentration was reported in water pipe smokers after a single typical session.57 The average plasma nicotine concentration over the first 24 hours after smoking a full bowl of water pipe tobacco was equivalent to that after smoking 2 to 3 cigarettes.66
Particulate Matter
Water pipe tobacco smoking generates high levels of PM. The size of the particles generated in mainstream smoke ranges from 0.01 to 0.2 μm, with a median diameter of 0.04 to 0.05 μm,62,67 although the particle size can be as large as 0.15 μm.68 In comparison, cigarette smoke generates particles between 0.15 and 0.5 μm, with a median particle size of 0.1 pm.62,67 The breathing volume of water pipe smoke (1 L in this study) was found to contain a greater number of particles (70×109) than 1 breath (45 mL) of a cigarette (9.2×109 particles).62 Given that a typical 1-hour session of water pipe consists of «100 puffs compared with ≈11 puffs of a cigarette, a single session of water pipe use is likely to lead to at least a 10-fold greater exposure to tobacco PM. Even after 5 minutes, the number of particles drawn from a water pipe is twice that generated by a cigarette in a smoking machine.67
Carbon Monoxide
Water pipes are also a significant source of CO exposure. In standardized smoking machine protocols, a single water pipe tobacco use session generates 35 times more CO than a cigarette.67 In addition, side-stream emission of CO during a single session is estimated to be equivalent to the amount of CO emitted by 10 cigarette smokers in the same space.67 Most of the CO emitted by water pipes seems to be from charcoal because replacing charcoal with an electric heater decreases CO emissions by 90%.69 Exposure estimates from water pipe users show that a single 30- to 90-minute water pipe smoking session exposes smokers to high levels of CO with exhaled levels between 12 and 60 ppm.65,70–72 The levels of CO in water pipe bar patrons (mean, 30.8 ppm) were much higher than in patrons of traditional bars where cigarette smoking was permitted (mean, 8.9 ppm).71 The exhaled CO of water pipe smokers after 1 session (43 ppm) was found to be greater than the amount reported for 1-pack-per-day cigarette smokers (17 ppm).72 In a laboratory study, CO increased by 24 ppm after 45 minutes of water pipe smoking and 3 ppm after smoking a single cigarette (a nearly 8-fold greater abundance in water pipe than cigarette smoke).70 Relative to a single cigarette, a single session of water pipe use is associated with 3-times-greater blood carboxyhemoglobin levels, even when peak plasma nicotine levels are comparable.70 The mean levels of CO (mean, 6.7 ppm) and PM <2.5 μm (PM2.5; mean, 264 μg/m3) in water pipe establishments were higher than the levels of CO (0.4 ppm) and PM2.5 (215 μg/m3) in a casino where smoking was permitted.73 Exposure to high levels of CO in water pipe smoke could lead to acute poisoning,74 which includes side effects such as syncope, headache, nausea, or seizure. These symptoms usually appear when the carboxyhemoglobin levels equal or exceed 17%.75 Several cases of CO poisoning related to water pipe smoking in young, otherwise healthy adults have been reported in the literature.75–78
Volatile Organic Compounds
The mainstream tobacco smoke of water pipes contains many of the same volatile organic chemicals present in cigarette smoke that have been associated with adverse cardiovascular effects. These include acrolein, benzene, phenols, and propioaldehyde.72–75 Compared with 1 reference 1R4F cigarette smoke session, a single water pipe tobacco smoke session (generated with a standardized smoking machine protocol) produced 27-fold greater levels of formaldehyde, 4-fold greater acetaldehyde, 19-fold greater acrolein, 9-fold greater propional-dehyde, and 4-fold greater methacrolein levels.79 Water pipe mainstream tobacco smoke also contains 6-fold higher benzene (micrograms per session) than cigarette smoke (micrograms per cigarette).63 The levels of carbonyls in water pipe emissions could be decreased by increasing the amount of humectants in the unburned tobacco, which lowers the temperature in the water pipe head.80 Estimates of exposure to typical users, assessed by measuring the urinary volatile organic chemical metabolites, suggest that water pipe smokers are exposed to much higher levels of benzene than cigarette smokers.81 In a short-term exposure study, the urinary levels of the acrolein metabolite 3-hydroxypropyl mercapturic acid increased 1.4 times after water pipe smoking.82 Similarly, urinary levels of S-phenylmercapturic acid, a metabolite of benzene, were increased 4.2 times after water pipe social events,83 suggesting that water pipe smoking may be a significant source of both benzene and acrolein exposure.
Polycyclic Aromatic Hydrocarbons
A range of PAHs has been identified in water pipe mainstream tobacco smoke under standardized machine smoking protocols.14,67,84 The profile of PAH emissions by water pipes differs from that of cigarettes. Although the concentration of PAH per 1 mL smoke is lower than in cigarettes, a typical water pipe smoking session, because of its length, delivers 20 times the total PAH yields and 50 times the heavy (4- to 5-ring) PAHs. The levels of some PAHs in water pipe emissions may be 2 to 3 orders of magnitude higher than in cigarette emissions. Overall, a typical water pipe smoking session can potentially result in PAH exposure equivalent to 50 cigarettes, in part because of the significantly larger amount of smoke volume generated during 1 water pipe session.84 As with CO, most (50%85 or 75%–92%69) PAHs emitted in mainstream (exhaled from the user) and sidestream (emitted from the burning tobacco) water pipe smoke may be derived from charcoal rather than tobacco and therefore not affected by the presence of nicotine.86 Estimates of exposure to PAHs by measuring urinary metabolites indicate that water pipe users take in more of the higher-molecular-weight PAHs such as phenanthrene. In comparison, the intake of low-molecular-weight PAHs, naphthalene and fluorine is higher during cigarette smoking.81
Heavy Metals and Arsenic
Multiple heavy metals (Be, Ni, Co, Cr, and Pb) have been detected in water pipe tobacco smoke.13 As13 and Zn68 have also been detected in some samples of water pipe smoke. Although the concentrations of As, Be, and Ni are similar or lower in water pipe condensates, the concentrations of Co, Cr, and Pb are higher than in commercial cigarettes. The source of the metals is not clear but may derive from a combination of emissions from tobacco and charcoal. Different types of raw synthetic and natural charcoals contain heavy metals such as Zn, Fe, Cd, Vd, Al, Pb, Cr, Mn, and Co, which are at concentrations similar to or higher than the concentration in cigarette smoke.87
CARDIOVASCULAR EFFECTS OF WATER PIPE SMOKING
Because both mainstream and sidestream water pipe tobacco smoke contains constituents similar to those generated by cigarettes, the use of water pipes could similarly lead to short-term cardiovascular changes in addition to long-term cardiovascular effects. These short-and long-term effects could increase CVD risk and precipitate cardiovascular events. Although the cardiovascular health effects and the underlying mechanisms by which water pipe tobacco smoking increases CVD risk have not been studied to the same extent as those of cigarettes, there are likely similar. Overlapping mechanisms underlying the effects of both tobacco products include sympathetic activation, vascular dysfunction, systemic inflammation and oxidative stress, insulin resistance, enhanced coagulation and thrombosis, and lipid peroxidation (Figure 4). Additional constituents specific to water pipe tobacco smoking that are emitted from the burning charcoal, such as the high levels of CO and benzene, must be considered when data are extrapolated from cigarette smoking.
Figure 4. Potential constituents of water pipe tobacco smoke and their associated cardiovascular effects.
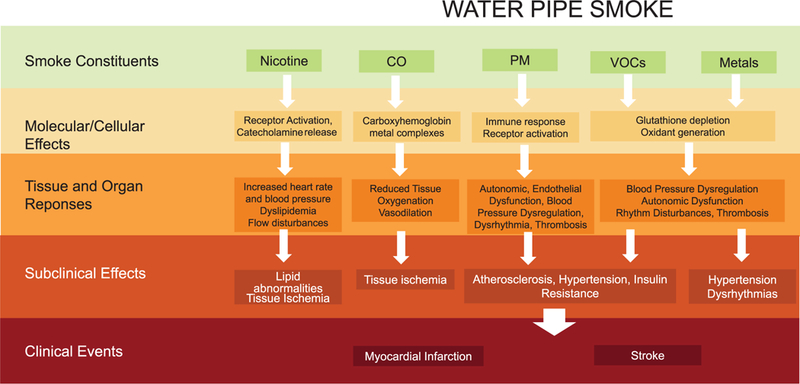
CO indicates carbon monoxide; PM, particulate matter; and VOC, volatile organic chemical
Cardiovascular Effects of Short-Term Water Pipe Smoking
As with cigarette smoking, water pipe tobacco smoking leads to an immediate and transient increase in heart rate and systolic blood pressure. The extent of these changes varies across studies because of the difference in exposure conditions, participant demographics, and use patterns. In general, in young, healthy individuals, smoking tobacco via a water pipe for 15 to 30 minutes increases heart rate by 6 to 13 beats per minute, systolic blood pressure by 3 to 16 mm Hg,88–91 and diastolic blood pressure by 2 to 14 mm Hg.88,89,91 These changes are accompanied by a decrease in heart rate variability91–93 and a modest increase in coronary blood flow.93 Water pipe tobacco smoking increases myocardial oxygen demand similar to the effects of cigarette smoking.93 Overall, the short-term cardiovascular effects are consistent with the sympathomimetic effects of nicotine, which are mediated by β-adrenergic activation. Indeed, in a double-blind placebo-controlled study, no changes in heart rate were observed when a flavor-matched, tobacco-free preparation was smoked.94 Like-wise, the decrease in heart rate variability with water pipe smoking was prevented by β-adrenergic blockade.93 Therefore, the short-term hemodynamic effects of water pipe tobacco smoking may be attributed to nicotine-induced β-adrenergic stimulation.
In addition to changes in cardiac function and blood flow, water pipe tobacco smoking has been found to affect vascular function in some,95,96 but not all studies.97 Measurements of vascular function with plethysmography found that water pipe smoking for 30 minutes immediately increases vascular resistance and decreases forearm blood flow, venous outflow, and venous capacitance.96 Both central and peripheral components are affected immediately after smoking.95 These effects are similar to those associated with cigarette smoking and have been related to attenuated endothelium-dependent vasodilation and hyperactive neurohormonal response to nicotine exposure or potentially other oxidants in water pipe smoke, increasing oxidative stress.96 Indeed, although water pipe tobacco smoking immediately increases the plasma concentration of 8-epi-prostaglandin F2α (a biomarker for oxidative injury),98 it decreases proinflammatory cytokines, including interleukin-4, interleukin-5, interleukin-17, and γ-interferon.97
The short-term hemodynamic effects of water pipe tobacco smoking may also be related to changes in exercise capacity. The vascular responses to water pipe smoking are exacerbated among individuals with lower levels of physical activity or physical fitness.96 In a pilot study of healthy participants, water pipe tobacco smoking was associated with an impairment of lung function and exercise capacity. During exercise, after water pipe tobacco smoking, a decrease in oxygen pulse (from 10.89 to 9.97 mL oxygen per beat) was found, which was also associated with an increase in the heart rate–oxygen consumption relationship.90 These changes may be related to the increase in blood CO levels, which may, in turn, result in a decrease in the oxygen-carrying capacity of the blood.90
Cardiovascular Effects of Long-Term Water Pipe Smoking
Several studies have reported an association of long-term water pipe use with increased CVD risk, severity, and mortality.92–94 Most such studies are from the Middle East and Southeast Asia, where water pipe use is most prevalent. However, the applicability of these findings to other geographic areas where population demographics and use patterns differ is uncertain. Moreover, most of these studies have a small sample size, incomplete exposure assessment, and a lack of clinical verification of events. Nevertheless, taken together, these data provide an overall indication of a potential for cardiovascular effects from long-term water pipe smoking.
In a small cohort of participants with established CVD (documented by coronary angiography), water pipe smoking has been associated with higher blood pressure and heart rate. Elevated blood pressure was more pronounced with dual use (cigarette and water pipe), although exclusive water pipe use was associated with higher blood pressure than nonsmoking.99 In a population-based study from Syria, daily water pipe smokers compared with never smokers were found on average to be 2.26 kg/m2 (95% CI, 0.79–3.72; ≈12 lb) heavier, even after adjustment for cigarette smoking, number of chronic diseases, age, sex, income, and marital status. They also had nearly 3-fold higher odds of being obese (odds ratio [OR], 2.87).100 In a study from the Punjab province of Pakistan, long-term water pipe use was associated with hypertension (OR, 1.95), hyperlipidemia (OR, 1.63), hyperglycemia (OR, 1.82), and abdominal obesity (OR, 1.93) but not with circulating levels of high-density lipoprotein.101 Age-adjusted prevalence of metabolic syndrome (identified in accordance with the International Diabetes Federation definition) was higher among current water pipe smokers than nonsmokers.101 Taken together, these findings suggest that the cardiovascular risk profile associated with long-term water pipe use is similar, but not identical, to that of cigarette smoking.
A direct comparison of vascular function in cigarette and water pipe tobacco smokers shows that long-term water pipe users have more severe decrements in endothelium-dependent, flow-mediated dilation than cigarette smokers. This difference may be related to the extent of exposure.102 Most water pipe users in the study smoked 3 to 5 sessions per day, whereas most cigarette smokers smoked 10 to 20 cigarettes per day. Because differences in the frequency of use between both products could result in higher exposure to HPHCs and nicotine in water pipe smokers, it seems likely that more severe depression of vascular function in water pipe smokers may be related to a higher level of exposure, particularly because there was an inverse correlation between flow-mediated dilation and smoking duration.102 Although the mechanisms by which long-term water pipe smoking leads to endothelial dysfunction remain to be determined, it is speculated that these may be the result of an underlying chronic inflammatory state. Indeed, there is a dose-dependent relationship between plasma fibrinogen levels and cigarette and water pipe smoking. In otherwise healthy men 20 to 75 years of age, the plasma levels of fibrinogen were elevated markedly in long-term water pipe users (especially those who smoked for >10 years) compared with nonsmokers,103 indicating again that CVD risk burden associated with water pipe smoking may be higher than that associated with cigarette smoking.
There are only limited data to assess the impact of water pipe use directly on the severity of CVD and associated mortality rates. Nevertheless, lifetime exposures exceeding 40 water pipe-years (2 water pipes per day for a total of 20 years or 1 water pipe for 40 years) are associated with a 3-fold increase in the odds of angio-graphically diagnosed coronary artery stenosis.104 Coronary disease, estimated as the mean Duke Jeopardy Score, was much higher in water pipe smokers than in cigarette smokers or nonsmokers.99 Even those who smoked both cigarettes and water pipe had a lower score than smokers of water pipe exclusively, suggesting that water pipe users have a higher burden of atherosclerotic disease resulting from greater use, greater exposure, or greater toxicity of water pipe smoke than cigarette smoke. As with cigarette smokers, water pipe smokers have a higher propensity for ST-segment-elevation myocardial infarction than nonsmokers, who tend to have non-ST-segment-elevation myocardial infarction acute coronary syndromes.105 Moreover, water pipe smokers have poorer in-hospital outcomes with higher mortality, more frequent myocardial ischemia, and higher recurrent myocardial infarction rates compared with cigarette smokers. In a prospective population-based study from Iran, heavy water pipe use was associated with a greater prevalence of heart disease, even when accounting for medication use and cigarette smoking.106 Fewer studies have evaluated the association between water pipe smoking and all-cause and cardiovascular mortality. In 1 study from Bangladesh, water pipe smoking was associated with higher odds of ischemic heart disease.107 In another study, there was no association between stroke deaths and water pipe smoking.108 No studies have assessed the relationship between water pipe and stroke risk, although, on the basis of the content of the smoke, the risk is anticipated to be at least similar to that of cigarette smoking. Additional work is warranted to assess the CVD risk burden associated with water pipe smoking and the risk of all-cause and cardiovascular mortality in those who smoke water pipes long term.
EFFECTS OF SECONDHAND EXPOSURE TO WATER PIPE TOBACCO SMOKE
As has been found with those exposed to cigarette smoking, individuals exposed to secondhand water pipe tobacco smoke and residual matter from water pipe use (ie, third-hand smoke) are at risk for negative health outcomes.6,109 Numerous studies have examined the environmental and health effects of secondhand exposure to water pipe tobacco smoke in various geographic regions, including the United States, Canada, the United Kingdom, Russia, India, and the eastern Mediterranean region.110–115 In terms of environmental air quality indicators, a primary outcome typically assessed is the level of PM2.5,116 a known cardiovascular risk agent.117 Although outdoor PM2.5 (originating primarily from fossil fuel combustion) is not directly comparable to PM generated from water pipes or other tobacco products, PM concentrations are commonly used to index the presence of secondhand smoke more generally.118
Significantly elevated PM25 levels have been detected in water pipe cafés/bars or places with high water pipe smoke density (349 μg/m3).110,112,114,119,120 Although PM levels associated with water pipe smoke vary with the number of individuals smoking, building size/dimensions, and ventilation characteristics, PM2.5 concentrations of 287,121 400,122 1420,119 and 1 180123 μg/m3 have been reported at different locations. In each study, the levels of PM2.5 in the bars were higher than in the ambient air outside the bar, but the levels of PM2.5 were higher in locations near the water pipe bars, suggesting that PM2.5 from water pipe bars could elevate PM2.5 levels in the vicinity of these establishments.121 The PM25 concentrations reported in many of these studies have been cited to exceed the air quality guides set by the Environmental Protection Agency (annual mean, 12 μg/m3; 24-hour average, 35 μg/m3). Nevertheless, the composition of the tobacco smoke and therefore its health effects are likely to be quite different from typical ambient air pollution from fossil fuel combustion, making it difficult to assess the health impact of water pipe emissions relative to ambient pollution.
In addition to PM, secondhand water pipe smoke contains other potentially hazardous constituents such as CO, nicotine, tobacco-specific nitrosamines, and PAHs. Significantly higher levels of ambient CO were observed inside water pipe bars/restaurants (7.3±2.4 mg/m3) in London, United Kingdom, relative to levels measured outside these venues (0.9±0.7 μg/m3).121 Results from a study of the home environments of daily water pipe smokers indicated significantly higher levels of air-based nicotine and surface-based nicotine compared with nonsmoking homes. In addition, urinary levels of nicotine metabolites (cotinine), tobacco-specific carcinogenic nitrosamine [nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol], and acrolein (3-hydroxypropyl mercapturic acid), a respiratory and cardiovascular toxicant, were significantly higher among children living in daily water pipe smoking homes, reflecting secondhand smoke exposure.124 There are few reports of direct health effects associated with secondhand water pipe smoke exposure. Two studies performed in Lebanon indicated that occupational or home-based exposure is associated with negative respiratory symptoms (eg, wheezing, chronic cough).125,126 Taken together, this body of work suggests that secondhand water pipe smoke may expose individuals, particularly children and those who work in the water pipe hospitability industry, to several types of water pipe-associated toxic exposures and potential health risks. Although there are no specific data detailing the relationship between secondhand water pipe smoke and chronic disease progression or mortality, similarities to evidence for secondhand cigarette smoke exposure suggest a similar risk profile.118,127
CESSATION OF WATER PIPE TOBACCO SMOKING
Approximately one-quarter to one-half of water pipe tobacco smokers in the United States and Middle East want to quit, including youth and young adults.32 Across several populations, 25% to 75% of those who want to quit make a quit attempt each year.128–132 Individuals interested in quitting are more likely than those not interested in quitting to believe that water pipe smoking damages health,32,133,134 are less nicotine dependent,130,133,135 are more likely to have received physician advice to quit,136 and have family or friends who disapprove its use.130,133,136 In a study from Syria, most water pipe tobacco smokers who sought cessation treatment smoked at least 6 times per week, had smoked for several years, and made at least 1 previous unsuccessful quit attempt.137 The development of cessation interventions for water pipe tobacco use, both behavioral and pharmacological, is in its infancy. An expert consensus panel evaluated a wide range of behavior change techniques deemed to be relevant for supporting water pipe smokers to quit.138 The panel achieved moderate to strong agreement on 3 broad categories: preparation and planning to quit (eg, assessing readiness to quit and previous quit attempts and facilitating identification of barriers to cessation and problem solving), increasing awareness of harms of water pipe smoking and advantages of quitting (eg, providing information on the consequences of smoking and cessation, assessing the pros and cons of quitting and not quitting), and relapse prevention and sustaining ex-smoker identity (eg, assessing and providing information on withdrawal symptoms and facilitating relapse prevention).
Systematic reviews of the impact of cessation interventions for water pipe smokers identified 5 randomized or cluster-randomized controlled studies that tested behavioral or pharmacological approaches.139,140 All 5 studies showed unclear or high risk of bias on key indicators such as blinding and selective outcome reporting. Two studies showed significantly higher quit rates in the intervention group. In Pakistan, Dogar and colleagues141 conducted a secondary analysis of a large cluster-randomized cessation trial that enrolled 1955 patients from 33 health centers who had suspected pulmonary tuberculosis and smoked water pipe or cigarettes. Health centers were randomized to provide 1 of 3 treatments: behavioral support (2 brief consultations that included preparing for the quit day, encouraging viewing oneself as a nonsmoker, and reviewing progress, consistent with recommendations by O’Neill et al138), behavioral support plus 7 weeks of treatment with buproprion, and usual care. Among the 215 water pipe–only smokers, 6-month quit rates were higher among those who received behavioral support compared with those who received usual care (45.7% versus 20.3%, respectively; adjusted relative risk, 2.5 [95% CI, 1.3–4.8]) and among those who received behavioral support plus buproprion compared with those who received usual care (50.0% versus 20.3%, respectively; adjusted relative risk, 2.2 [95% CI, 1.3–3.7]). A community-based cluster trial conducted in Egypt randomized villages to receive a behavioral intervention consisting of several community health promotion activities (eg, school prevention efforts, antismoking education in mosques and churches, peer educators) or no intervention.142 Men in intervention villages who were current water pipe smokers at baseline were more likely to no longer smoke at 12 months after treatment than men in control villages (relative risk, 3.3 [95% CI, 1.4–8.9]; calculated by Jawad et al139).
Three other small randomized trials found positive but nonsignificant effects of behavioral interventions, including a single-session educational intervention delivered as a PowerPoint presentation to US college students,61 a multisession school-based intervention in Lebanon and Qatar,143 and a multicomponent, physician-delivered, one-on-one behavioral intervention among Syrian adults.137 Another small trial of 109 US water pipe café customers who were randomized to a brief, single session of health risk information and personalized feedback about expired CO levels versus an assessment-only control found that ≈45% of subjects in both conditions reported no water pipe use at 3 months after treatment.144
Most evaluations of water pipe cessation to date are pilot studies, usually with only small sample sizes, short follow-up periods, no biochemical verification of abstinence status, and nonrandomized designs.139 From these studies it appears that certain behavioral strategies that have proved effective for cigarette cessation may be useful when adapted for water pipe cessation. These techniques include educating the smoker about the health consequences of water pipe use, increasing motivation to quit by reviewing the pros and cons of smoking and quitting, setting and preparing for the quit day, and providing coping assistance to prevent relapse. Data from controlled trials are not yet available to determine the efficacy of pharmacological interventions, but a double-blind randomized controlled trial is underway to test the efficacy of varenicline for water pipe cessation.145
OVERALL SUMMARY
The data reviewed here support several conclusions:
Water pipe tobacco smoking is prevalent worldwide, especially among youth and young adults. Most users in Western countries smoke water pipe intermittently. Many water pipe users concurrently use other forms of tobacco products.
The spread of water pipe tobacco smoking is promoted by several factors, including sweetened and flavored water pipe tobacco, social media that promotes this method of tobacco use, and misperceptions about its addictive potential and adverse health effects.
A majority of users believe that water pipe tobacco smoking is less harmful than cigarette smoking, that the probability of addiction is low, and that quitting water pipe tobacco smoking is not difficult.
The risk of initiation of cigarette smoking may be higher among water pipe smokers than among never smokers.
The level of nicotine to which water pipe tobacco smokers are exposed has been demonstrated to be physiologically active in the short term94 and can produce dependence with repeated exposure.146
While direct comparisons have some limitations, compared with smoking a single cigarette, a single session of water pipe smoking typically results in greater exposure to CO. The CO levels to which water pipe users are exposed can produce toxicity with short-term exposure at high levels and interfere with exercise capacity.
The smoking behavior associated with water pipe tobacco smoking—sessions lasting ≥30 minutes and involving the inhalation of many liters of smoke—can result in water pipe smokers inhaling substantial quantities of toxicants during each use episode.147,148 Water pipe smoke contains high levels of PM, which contains smaller particles at higher concentrations than cigarettes. Comparing a single cigarette with a single water pipe session shows that water pipe use exposes smokers to significantly higher levels of heavier and more toxic PAHs than cigarette smoking, as well as cardiorespiratory toxicants such as volatile organic compounds and heavy metals such as cadmium and lead that can injure the blood vessels and the brain.
Although evidence for water pipe–attributable disease is not as robust as the evidence for cigarette smoking, a growing number of studies suggest that water pipe tobacco smoking is a risk factor for pulmonary disease and CVD.
KNOWLEDGE GAPS
There are many knowledge gaps on the subject of water pipe tobacco smoking that provide opportunities for more rigorous studies evaluating the link between this form of tobacco smoking and a variety of disease outcomes, including CVD and stroke. Conducting such studies is challenging because the regions where frequent and long-term water pipe tobacco smoking is most prevalent often lack the resources required for large-scale epidemiological studies. In addition, the frequency of dual use of waterpipe and cigarettes can make identifying the specific effects of water pipe tobacco smoking more difficult. Additional work is needed to test and develop empirically supported, water pipe–specific cessation interventions. It would also be beneficial to test both behavioral and pharmacological methods to promote cessation in adequately powered randomized controlled trials using standardized outcome criteria, including adequate follow-up durations, biochemical verification of abstinence, intention-to-treat analysis to maintain prognostic balance when loss to follow-up occurs, and blinded follow-up assessment.132
Opportunities also exist to address knowledge gaps in communication of the health effects of water pipe tobacco smoking, cultural influences that may promote and sustain use across certain population groups, and the development of policies that can decrease the likelihood of water pipe–induced dependence, disease, disability, and death among youth worldwide. Currently, there is a persistent misperception among water pipe users that this method of tobacco use is harmless. In contrast, many youths are aware of the risks associated with cigarette smoking and avoid that method of tobacco use because of those risks.
Further research is needed to determine how best to communicate to youth that the same toxicants that are present in cigarette smoke are present in water pipe smoke and that any individual who avoids cigarette smoking to avoid inhaling lethal chemicals should avoid water pipe tobacco smoking for the same reason. This effort may require a transdisciplinary approach in which health communication scientists work with other investigators who are familiar with water pipe smoke toxicant content, user toxicant exposure, and disease risk to craft messages that are accurate and meaningful to the target audience. The information for such messaging is available now to inform public health policy, planning, and practice.
There are also important knowledge gaps in policies that might be most effective in curtailing the worldwide spread of water pipe tobacco smoking. For example, although considerable effort has been spent in developing and evaluating effective policies on cigarette taxation, labeling, advertisement, availability, and other factors, little policy-related research has addressed water pipe tobacco smoking. Many of the same policy interventions are likely to be relevant to water pipe smoking and could be readily adapted to address this form of tobacco use, although additional innovation may be warranted. For example, because water pipe tobacco smoking often occurs in dedicated commercial venues where the water pipe tobacco is handled by staff rather than by user (ie, water pipe bars), these venues could be taxed (in addition to the tobacco itself). Health warning labeling could be extended to these venues (eg, required graphic health warning signage in each venue) and, in addition to tobacco packaging, to the water pipe itself. However, identification of the characteristics and evaluation of the effectiveness of such strategies require empirical study.
SUGGESTIONS FOR CLINICAL PRACTICE
To identify and treat water pipe tobacco smokers in clinical settings, healthcare providers are encouraged to do the following:
Ask users about water pipe use and frequency explicitly, using a variety of terms if necessary, as well as use of other tobacco products, as part of routine clinical examinations.
Advise users to quit water pipe and other tobacco product use.
Assist water pipe smokers to quit by providing cessation counseling, including setting a quit date and providing social support and coping assistance.
Refer water pipe smokers to credible sources for information on potential addictiveness and health consequences of water pipe use, including this statement.
Acknowledgments
This statement was approved by the American Heart Association Science Advisory and Coordinating Committee on November 1, 2018, and the American Heart Association Executive Committee on November 27, 2018. A copy of the document is available at https://professional.heart.org/statements by using either “Search for Guidelines & Statements” or the “Browse by Topic” area. To purchase additional reprints, call 843–216-2533 or e-mail kelle.ramsay@wolterskluwer.com.
The American Heart Association requests that this document be cited as follows:
Bhatnagar A, Maziak W, Eissenberg T, Ward KD, Thurston G, King BA, Sutfin EL, Cobb CO, Griffiths M, Goldstein LB, Rezk-Hanna M; on behalf of the American Heart Association Behavioral Change for Improving Health Factors Committee of the Council on Lifestyle and Cardiometabolic Health and Council on Epidemiology and Prevention; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Stroke Council. Water pipe (hookah) smoking and cardiovascular disease risk: a scientific statement from the American Heart Association. Circulation. 2019;139:e917-e936. doi: 10.1161/CIR.0000000000000671.
The expert peer review of AHA-commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit https://professional.heart.org/statements. Select the “Guidelines & Statements” drop-down menu, then click “Publication Development.”
Permissions: Multiple copies, modification, alteration, enhancement, and/ or distribution of this document are not permitted without the express permission of the American Heart Association. Instructions for obtaining permission are located at https://www.heart.org/permissions. A link to the “Copyright Permissions Request Form” appears in the second paragraph (https://www.heart.org/en/about-us/statements-and-policies/copyright-request-form).
Disclosures
Writing Group Disclosures
| Writing Group Member |
Employment | Research Grant | Other Research Support |
Speakers’
Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Aruni Bhatnagar | University of Louisville | NIH/FDA (PI)† | None | None | None | None | None | NIH/FDA (salary[principalinvestigator])† |
| Caroline O. Cobb | Virginia Commonwealth University | None | None | None | None | None | None | None |
| Thomas Eissenberg | Virginia Commonwealth University | NIH (PI and coinvestigator on various grants)† | None | None | None | None | None | None |
| Larry B. Goldstein | University of Kentucky | None | None | None | None | None | None | None |
| Merlyn Griffiths | University of North Carolina–Greensboro | NIH (grant $420 830 project)† | None | None | None | None | None | None |
| Brian A. King | Centers for Disease Control and Prevention, Office on Smoking and Health | None | None | None | None | None | None | None |
| Wasim Maziak | Florida International University | None | None | None | None | None | None | None |
| Mary Rezk-Hanna | UCLA School of Nursing | None | None | None | None | None | None | None |
| Erin L. Sutfin | Wake Forest School of Medicine Social Sciences and Health Policy Medical Center | NIH (PI and coinvestigator on several NIH-funded grants)† | None | None | None | None | None | None |
| George Thurston | New York University School of Medicine | None | None | None | None | None | None | None |
| Kenneth D. Ward | University of Memphis School of Public Health | None | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if
the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or
the person owns 5% or more of the voting stock or share of the entity or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Significant.
Reviewer Disclosures
| Reviewer | Employment | Research Grant | Other Research Support |
Speakers’
Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Neal L. Benowitz | University of California, San Francisco | NIH†; Flight Attendant Medical Research Institute†; California Tobacco Related Disease Research Program† | None | None | None | None | Pfizer* | None |
| Debabrata Mukherjee | Texas Tech University | None | None | None | None | None | None | None |
| Mariann R. Piano | Vanderbilt University | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if
the person receives $10,000 or more during any 12-month period, or 5% or more of the person’s gross income; or
the person owns 5% or more of the voting stock or share of the entity, or owns $10,000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
Significant.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
REFERENCES
- 1.Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, Bhala N, Peto R, Zatonski W, Hsia J, Morton J, Palipudi KM, Asma S; GATS Collaborative Group. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380:668–679. doi: 10.1016/S0140-6736(12)61085-X [DOI] [PubMed] [Google Scholar]
- 2.Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, Wollum A, Sanman E, Wulf S, Lopez AD, Murray CJ, Gakidou E. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. 2014;311:183–192. doi: 10.1001/jama.2013.284692 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks: Cancer. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 4.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2011: Warning About the Dangers of Tobacco. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 5.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–852. doi: 10.1016/S0140-6736(03)14338-3 [DOI] [PubMed] [Google Scholar]
- 6.Surgeon General. The health consequences of smoking-50 years of progress: a report of the surgeon general, 2014. US Department of Health and Human Services; https://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html. Accessed April 10, 2018. [Google Scholar]
- 7.Mons U, Müezzinler A, Gellert C, Schöttker B, Abnet CC, Bobak M, de Groot L, Freedman ND, Jansen E, Kee F, Kromhout D, Kuulasmaa K, Laatikainen T, O’Doherty MG, Bueno-de-Mesquita B, Orfanos P, Peters A, van der Schouw YT, Wilsgaard T, Wolk A, Trichopoulou A, Boffetta P, Brenner H; CHANCES Consortium. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: metaanalysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ. 2015;350:h1551. doi: 10.1136/bmj.h1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Labarthe DR, Goldstein LB, Antman EM, Arnett DK, Fonarow GC, Alberts MJ, Hayman LL, Khera A, Sallis JF, Daniels SR, Sacco RL, Li S, Ku L, Lantz PM, Robinson JG, Creager MA, Van Horn L, Kris-Etherton P, Bhatnagar A, Whitsel LP; on behalf of the American Heart Association Advocacy Coordinating Committee, Council on Hypertension, Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Quality of Care and Outcomes Research, Council on Cardiovascular Surgery and Anesthesia, Council on Functional Genomics and Translational Biology, and Council on Epidemiology and Prevention. Evidence-based policy making: assessment of the American Heart Association’s strategic policy portfolio: a policy statement from the American Heart Association. Circulation. 2016;133:e615–e653. doi: 10.1161/CIR.0000000000000410 [DOI] [PubMed] [Google Scholar]
- 9.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2018 update: a report from the American Heart Association [published correction appears in Circulation. 2018;137:e493]. Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 10.Piano MR, Benowitz NL, Fitzgerald GA, Corbridge S, Heath J, Hahn E, Pechacek TF, Howard G; on behalf of the American Heart Association Council on Cardiovascular Nursing. Impact of smokeless tobacco products on cardiovascular disease: implications for policy, prevention, and treatment: a policy statement from the American Heart Association. Circulation. 2010;122:1520–1544. doi: 10.1161/CIR.0b013e3181f432c3 [DOI] [PubMed] [Google Scholar]
- 11.Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, Robertson RM, McAuley T, Goff D, Benowitz N; on behalf of the American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130:1418–1436. doi: 10.1161/CIR.0000000000000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shihadeh A Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003;41:143–152. [DOI] [PubMed] [Google Scholar]
- 14.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar,” and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43:655–661. doi: 10.1016/j.fct.2004.12.013 [DOI] [PubMed] [Google Scholar]
- 15.Akl EA, Ward KD, Bteddini D, Khaliel R, Alexander AC, Lotfi T, Alaouie H, Afifi RA. The allure of the waterpipe: a narrative review of factors affecting the epidemic rise in waterpipe smoking among young persons globally. Tob Control. 2015;24(suppl 1):i13–i21. doi: 10.1136/tobaccocontrol-2014-051906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutfin EL, Song EY, Reboussin BA, Wolfson M. What are young adults smoking in their hookahs? A latent class analysis of substances smoked. AddictBehav. 2014;39:1191–1196. doi: 10.1016/j.addbeh.2014.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambrose BK, Day HR, Rostron B, Conway KP, Borek N, Hyland A, Villanti AC. Flavored tobacco product use among US youth aged 12–17 years, 2013–2014. JAMA. 2015;314:1871–1873. doi: 10.1001/jama.2015.13802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rastam S, Ward KD, Eissenberg T, Maziak W. Estimating the beginning of the waterpipe epidemic in Syria. BMC Public Health. 2004;4:32. doi: 10.1186/1471-2458-4-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salloum RG, Asfar T, Maziak W. Toward a regulatory framework for the waterpipe. Am J Public Health. 2016;106:1773–1777. doi: 10.2105/AJPH.2016.303322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Lung Association. An Emerging Deadly Trend: Waterpipe Tobacco Use; PDF-222 KB. Washington, DC: American Lung Association; 2007. [Google Scholar]
- 21.Jawad M, Nakkash RT, Hawkins B, Akl EA. Waterpipe industry products and marketing strategies: analysis of an industry trade exhibition. Tob Control. 2015;24:e275–e279. doi: 10.1136/tobaccocontrol-2015-052254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakkash R, Khalil J. Health warning labelling practices on narghile (shisha, hookah) waterpipe tobacco products and related accessories. Tob Control. 2010;19:235–239. doi: 10.1136/tc.2009.031773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bird Y, May J, Nwankwo C, Mahmood R, Moraros J. Prevalence and characteristics of flavoured tobacco use among students in grades 10 through 12: a national cross-sectional study in Canada, 2012–2013. Tob Induc Dis. 2017;15:20. doi: 10.1186/s12971-017-0124-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jamal A, Gentzke A, Hu SS, Cullen KA, Apelberg BJ, Homa DM, King BA. Tobacco use among middle and high school students-United States, 201 1–2016. MMWR Morb Mortal Wkly Rep. 2017;66:597–603. doi: 10.15585/mmwr.mm6623a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech R. Monitoring the Future: National Survey Results on Drug Use, 1975–2015, Volume II, College Students and Adults Ages 19–55. Bethesda, MD: National Institute of Drug Abuse; 2016. http://www.monitoringthefuture.org/pubs/monographs/mtf-vol2_2016.pdf. Accessed March 10, 2018. [Google Scholar]
- 26.Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, Green VR, Kaufman AR, Bansal¬Travers M, Travers MJ, Kwan J, Tworek C, Cheng YC, Yang L, Pharris-Ciurej N, van Bemmel DM, Backinger CL, Compton WM, Hyland AJ. Tobacco- product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376:342–353. doi: 10.1056/NEJMsa1607538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Mulla Moh’d A, Abdou Helmy S, Al-Lawati J, Al Nasser S, Ali Abdel Rahman S, Almutawa A, Abi Saab B, Al-Bedah AM, Al-Rabeah AM, Ali Bahaj A, El-Awa F, Warren CW, Jones NR, Asma S. Prevalence of tobacco use among students aged 13–15 years in Health Ministers’ Council/ Gulf Cooperation Council Member States, 2001–2004. J Sch Health. 2008;78:337–343. doi: 10.1111/j.1746-1561.2008.00311.x [DOI] [PubMed] [Google Scholar]
- 28.Jawad M, Wilson A, Lee JT, Jawad S, Hamilton FL, Millett C. Prevalence and predictors of water pipe and cigarette smoking among secondary school students in London. Nicotine Tob Res. 2013;15:2069–2075. doi: 10.1093/ntr/ntt103 [DOI] [PubMed] [Google Scholar]
- 29.Villanti AC, Johnson AL, Ambrose BK, Cummings KM, Stanton CA, Rose SW, Feirman SP, Tworek C, Glasser AM, Pearson JL, Cohn AM, Conway KP, Niaura RS, Bansal-Travers M, Hyland A. Flavored tobacco product use in youth and adults: findings from the first wave of the PATH study (2013–2014). Am J Prev Med. 2017;53:139–151. doi: 10.1016/j.amepre.2017.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaber R, Madhivanan P, Veledar E, Khader Y, Mzayek F, Maziak W. Water- pipe: a gateway to cigarette smoking initiation among adolescents in Ir- bid, Jordan: a longitudinal study. Int J Tuberc Lung Dis. 2015;19:481–487. doi: 10.5588/ijtld.14.0869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tob Control. 2004;13:327–333. doi: 10.1136/tc.2004.008169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akl EA, Jawad M, Lam WY, Co CN, Obeid R, Irani J. Motives, beliefs and attitudes towards waterpipe tobacco smoking: a systematic review. Harm Reduct J. 2013;10:12. doi: 10.1186/1477-7517-10-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cornacchione J, Wagoner KG, Wiseman KD, Kelley D, Noar SM, Smith MH, Sutfin EL. Adolescent and young adult perceptions of hookah and little cigars/cigarillos: implications for risk messages. J Health Commun. 2016;21:818–825. doi: 10.1080/10810730.2016.1177141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Griffiths MA, Harmon TR, Gilly MC. Hubble bubble trouble: the need for education about and regulation of hookah smoking. J Public Policy Mar¬keting. 2011;30:119–132. [Google Scholar]
- 35.Salloum RG, Osman A, Maziak W, Thrasher JF. How popular is waterpipe tobacco smoking? Findings from internet search queries. Tob Control. 2015;24:509–513. doi: 10.1136/tobaccocontrol-2014-051675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kates FR, Salloum RG, Thrasher JF, Islam F, Fleischer NL, Maziak W. Geographic proximity of waterpipe smoking establishments to colleges in the U.S. Am J Prev Med. 2016;50:e9–e14. doi: 10.1016/j.amepre.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith JR, Novotny TE, Edland SD, Hofstetter CR, Lindsay SP, Al-Delaimy WK. Determinants of hookah use among high school students. Nicotine Tob Res. 2011;13:565–572. doi: 10.1093/ntr/ntr041 [DOI] [PubMed] [Google Scholar]
- 38.Morris DS, Fiala SC, Pawlak R. Opportunities for policy interventions to reduce youth hookah smoking in the United States. Prev Chronic Dis. 2012;9:E165. doi: 10.5888/pcd9.120082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brockman LN, Pumper MA, Christakis DA, Moreno MA. Hookah’s new popularity among US college students: a pilot study of the characteristics of hookah smokers and their Facebook displays. BMJ Open. 2012;2:e001709. doi: 10.1136/bmjopen-2012-001709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Braun RE, Glassman T, Wohlwend J, Whewell A, Reindl DM. Hookah use among college students from a Midwest university. J Community Health. 2012;37:294–298. doi: 10.1007/s10900-011-9444-9 [DOI] [PubMed] [Google Scholar]
- 41.Krauss MJ, Sowles SJ, Moreno M, Zewdie K, Grucza RA, Bierut LJ, Cavazos-Rehg PA. Hookah-related Twitter chatter: a content analysis. Prev Chronic Dis. 2015;12:E121. doi: 10.5888/pcd12.150140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grant A, O’Mahoney H. Portrayal of waterpipe (shisha, hookah, nar-gile) smoking on Twitter: a qualitative exploration. Public Health. 2016;140:128–135. doi: 10.1016/j.puhe.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 43.Guidry J, Jin Y, Haddad L, Zhang Y, Smith J. How health risks are pinpointed (or not) on social media: the portrayal of waterpipe smoking on Pinterest. Health Commun. 2016;31:659–667. doi: 10.1080/10410236.2014.987468 [DOI] [PubMed] [Google Scholar]
- 44.Carroll MV, Shensa A, Primack BA. A comparison of cigarette- and hookah-related videos on YouTube. Tob Control. 2013;22:319–323. doi: 10.1136/tobaccocontrol-2011-050253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allem JP, Chu KH, Cruz TB, Unger JB. Waterpipe promotion and use on Instagram: #hookah. Nicotine Tob Res. 2017;19:1248–1252. doi: 10.1093/ntr/ntw329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Primack BA, Carroll MV, Shensa A, Davis W, Levine MD. Sex differences in hookah-related images posted on Tumblr: a content analysis. J Health Commun. 2016;21:366–375. doi: 10.1080/10810730.2015.1095814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hu SS, Neff L, Agaku IT, Cox S, Day HR, Holder-Hayes E, King BA. Tobacco product use among adults-United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65:685–691. doi: 10.15585/mmwr.mm6527a1 [DOI] [PubMed] [Google Scholar]
- 48.King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102:e93–e100. doi: 10.2105/AJPH.2012.301002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abudayyeh HS, Glasser AM, Johnson AL, Cohn AM, Wagener TL, Mays D, Villanti AC. Social and substance use correlates of adult hookah use, 2016. AddictBehav. 2018;79:39–44. doi: 10.1016/j.addbeh.2017.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abdullah P, Costanian C, Khanlou N, Tamim H. Prevalence and characteristics of water-pipe smoking in Canada: results from the Canadian Tobacco Use Monitoring Survey. Public Health. 2017;148:102–108. doi: 10.1016/j.puhe.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 51.Nemati S, Rafei A, Freedman ND, Fotouhi A, Asgary F, Zendehdel K. Cigarette and water-pipe use in Iran: geographical distribution and time trends among the adult population; a pooled analysis of national STEPS surveys, 2006–2009. Arch Iran Med. 2017;20:295–301. doi: 0172005/AIM.007 [PubMed] [Google Scholar]
- 52.Al-Hemiery N, Dabbagh R, Hashim MT, Al-Hasnawi S, Abutiheen A, Abdulghani EA, Al-Diwan JK, Kak N, Al Mossawi H, Maxwell JC, Brecht ML, Antonini V, Hasson A, Rawson RA. Self-reported substance use in Iraq: findings from the Iraqi National Household Survey of Alcohol and Drug Use, 2014. Addiction. 2017;112:1470–1479. doi: 10.1111/add.13800 [DOI] [PubMed] [Google Scholar]
- 53.Khattab A, Javaid A, Iraqi G, Alzaabi A, Ben Kheder A, Koniski ML, Shahrour N, Taright S, Idrees M, Polatli M, Rashid N, El Hasnaoui A; BREATHE Study Group. Smoking habits in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106(suppl 2):S16–S24. doi: 10.1016/S0954-6111(12)70011-2 [DOI] [PubMed] [Google Scholar]
- 54.Agaku IT, Filippidis FT, Vardavas CI, Odukoya OO, Awopegba AJ, Ayo-Yusuf OA, Connolly GN. Poly-tobacco use among adults in 44 countries during 2008–2012: evidence for an integrative and comprehensive approach in tobacco control. Drug Alcohol Depend. 2014;139:60–70. doi: 10.1016/j.drugalcdep.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 55.Bonhomme MG, Holder-Hayes E, Ambrose BK, Tworek C, Feirman SP, King BA, Apelberg BJ. Flavoured non-cigarette tobacco product use among US adults: 2013–2014. Tob Control. 2016;25:ii4–ii13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salloum RG, Haider MR, Barnett TE, Guo Y, Getz KR, Thrasher JF, Maziak W. Peer reviewed: waterpipe tobacco smoking and susceptibility to cigarette smoking among young adults in the United States, 2012–2013. Prev Chronic Dis. 2016;13:E24. doi: 10.5888/pcd13.150505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Momenabadi V, Hossein Kaveh M, Hashemi SY, Borhaninejad VR. Factors affecting hookah smoking trend in the society: a review article. Addict Health. 2016;8:123–135. [PMC free article] [PubMed] [Google Scholar]
- 58.Trimmel M, Wittberger S. Effects of transdermally administered nicotine on aspects of attention, task load, and mood in women and men. Pharmacol Biochem Behav. 2004;78:639–645. doi: 10.1016/j.pbb.2004.04.030 [DOI] [PubMed] [Google Scholar]
- 59.Bahelah R, DiFranza JR, Fouad FM, Ward KD, Eissenberg T, Maziak W. Early symptoms of nicotine dependence among adolescent waterpipe smokers. Tob Control. 2016;25:e127–e134. doi: 10.1136/tobaccocontrol-2015-052809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: predictors and characteristics among current hookah users. Tob Induc Dis. 2009;5:16. doi: 10.1186/1617-9625-5-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lipkus IM, Eissenberg T, Schwartz-Bloom RD, Prokhorov AV, Levy J. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine Tob Res. 2011;13:599–610. doi: 10.1093/ntr/ntr049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Monn Ch, Kindler P, Meile A, Brändli O. Ultrafine particle emissions from waterpipes. Tob Control. 2007;16:390–393. doi: 10.1136/tc.2007.021097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schubert J, Müller FD, Schmidt R, Luch A, Schulz TG. Waterpipe smoke: source of toxic and carcinogenic VOCs, phenols and heavy metals? Arch Toxicol. 2015;89:2129–2139. doi: 10.1007/s00204-014-1372-x [DOI] [PubMed] [Google Scholar]
- 64.Neergaard J, Singh J P Job, Montgomery S. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine Tob Res. 2007;9:987–994. doi: 10.1080/14622200701591591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jacob P 3rd, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Nicotine, carbon monoxide, and carcinogen exposure after a single use of a water pipe. Cancer Epidemiol Biomarkers Prev. 2011;20:2345–2353. doi: 10.1158/1055-9965.EPI-11-0545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.St Helen G, Benowitz NL, Dains KM, Havel C, Peng M, Jacob P 3rd. Nicotine and carcinogen exposure after water pipe smoking in hookah bars. Cancer Epidemiol Biomarkers Prev. 2014;23:1055–1066. doi: 10.1158/1055-9965.EPI-13-0939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Daher N, Saleh R, Jaroudi E, Sheheitli H, Badr T, Sepetdjian E, Al Rashidi M, Saliba N, Shihadeh A. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ (1994). 2010;44:8–14. doi: 10.1016/j.atmosenv.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Apsley A, Galea KS, Sánchez-Jiménez A, Semple S, Wareing H, van Tongeren M, Galea K. Assessment of polycyclic aromatic hydrocarbons, carbon monoxide, nicotine, metal contents and particle size distribution of mainstream shisha smoke. J Environ Health Res. 2011;11:93–103. [Google Scholar]
- 69.Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol. 2008;46:2991–2995. doi: 10.1016/j.fct.2008.05.031 [DOI] [PubMed] [Google Scholar]
- 70.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37:518–523. doi: 10.1016/j.amepre.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barnett TE, Curbow BA, Soule EK Jr, Tomar SL, Thombs DL. Carbon monoxide levels among patrons of hookah cafes. Am J Prev Med. 2011;40:324–328. doi: 10.1016/j.amepre.2010.11.004 [DOI] [PubMed] [Google Scholar]
- 72.El-Nachef WN, Hammond SK. Exhaled carbon monoxide with waterpipe use in US students. JAMA. 2008;299:36–38. doi: 10.1001/jama.2007.6 [DOI] [PubMed] [Google Scholar]
- 73.Hammal F, Chappell A, Wild TC, Kindzierski W, Shihadeh A, Vanderhoek A, Huynh CK, Plateel G, Finegan BA. “Herbal” but potentially hazardous: an analysis of the constituents and smoke emissions of tobacco-free wa- terpipe products and the air quality in the cafés where they are served. Tob Control. 2015;24:290–297. doi: 10.1136/tobaccocontrol-2013-051169 [DOI] [PubMed] [Google Scholar]
- 74.Eichhorn L, Michaelis D, Kemmerer M, Jüttner B, Tetzlaff K. Carbon monoxide poisoning from waterpipe smoking: a retrospective cohort study. Clin Toxicol(Phila). 2018;56:264–272. doi: 10.1080/15563650.2017.1375115 [DOI] [PubMed] [Google Scholar]
- 75.von Rappard J, Schönenberger M, Bärlocher L. Carbon monoxide poisoning following use of a water pipe/hookah. Dtsch Arztebl Int. 2014;111:674–679. doi: 10.3238/arztebl.2014.0674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Türkmen S, Eryigit U, Sahin A, Yeniocak S, Turedi S. Carbon monoxide poisoning associated with water pipe smoking. Clin Toxicol (Phila). 2011;49:697–698. doi: 10.3109/15563650.2011.598160 [DOI] [PubMed] [Google Scholar]
- 77.Ashurst JV, Urquhart M, Cook MD. Carbon monoxide poisoning secondary to hookah smoking. J Am Osteopath Assoc. 2012;112:686–688. [PubMed] [Google Scholar]
- 78.Retzky SS. Carbon monoxide poisoning from hookah smoking: an emerging public health problem. J Med Toxicol. 2017;13:193–194. doi: 10.1007/s13181-017-0617-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem Toxicol. 2008;46:3546–3549. doi: 10.1016/j.fct.2008.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schubert J, Heinke V, Bewersdorff J, Luch A, Schulz TG. Waterpipe smoking: the role of humectants in the release of toxic carbonyls. Arch Toxicol. 2012;86:1309–1316. doi: 10.1007/s00204-012-0884-5 [DOI] [PubMed] [Google Scholar]
- 81.Jacob P 3rd, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Comparison of nicotine and carcinogen exposure with water pipe and cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2013;22:765–772. doi: 10.1158/1055-9965.EPI-12-1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kassem NOF, Kassem NO, Liles S, Zarth AT, Jackson SR, Daffa RM, Chatfield DA, Carmella SG, Hecht SS, Hovell MF. Acrolein exposure in hookah smokers and non-smokers exposed to hookah tobacco secondhand smoke: implications for regulating hookah tobacco products. Nicotine Tob Res. 2018;20:492–501. doi: 10.1093/ntr/ntx133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kassem NO, Kassem NO, Jackson SR, Liles S, Daffa RM, Zarth AT, Younis MA, Carmella SG, Hofstetter CR, Chatfield DA, Matt GE, Hecht SS, Hovell MF. Benzene uptake in hookah smokers and non-smokers attending hookah social events: regulatory implications. Cancer Epidemiol Biomarkers Prev. 2014;23:2793–2809. doi: 10.1158/1055-9965.EPI-14-0576 [DOI] [PubMed] [Google Scholar]
- 84.Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food Chem Toxicol. 2008;46:1582–1590. doi: 10.1016/j.fct.2007.12.028 [DOI] [PubMed] [Google Scholar]
- 85.Sepetdjian E, Saliba N, Shihadeh A. Carcinogenic PAH in waterpipe charcoal products. Food Chem Toxicol. 2010;48:3242–3245. doi: 10.1016/j.fct.2010.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shihadeh A, Salman R, Jaroudi E, Saliba N, Sepetdjian E, Blank MD, Cobb CO, Eissenberg T. Does switching to a tobacco-free waterpipe product reduce toxicant intake? A crossover study comparing CO, NO, PAH, volatile aldehydes, “tar” and nicotine yields. Food Chem Toxicol. 2012;50:1494–1498. doi: 10.1016/j.fct.2012.02.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Elsayed Y, Dalibalta S, Abu-Farha N. Chemical analysis and potential health risks of hookah charcoal. Sci Total Environ. 2016;569–570:262–268. doi: 10.1016/j.scitotenv.2016.06.108 [DOI] [PubMed] [Google Scholar]
- 88.Azar RR, Frangieh AH, Mroue J, Bassila L, Kasty M, Hage G, Kadri Z. Acute effects of waterpipe smoking on blood pressure and heart rate: a real-life trial. Inhal Toxicol. 2016;28:339–342. doi: 10.3109/08958378.2016.1171934 [DOI] [PubMed] [Google Scholar]
- 89.Shaikh RB, Vijayaraghavan N, Sulaiman AS, Kazi S, Shafi MS. The acute effects of waterpipe smoking on the cardiovascular and respiratory systems. J Prev Med Hyg. 2008;49:101–107. [PubMed] [Google Scholar]
- 90.Hawari FI, Obeidat NA, Ayub H, Ghonimat I, Eissenberg T, Dawahrah S, Beano H. The acute effects of waterpipe smoking on lung function and exercise capacity in a pilot study of healthy participants. Inhal Toxicol. 2013;25:492–97. doi: 10.3109/08958378.2013.806613 [DOI] [PubMed] [Google Scholar]
- 91.Al-Kubati M, Al-Kubati AS, al’Absi M, Fiser B. The short-term effect of water-pipe smoking on the baroreflex control of heart rate in normotensives. Auton Neurosci. 2006; 126–127:146–149. doi: 10.1016/j.autneu.2006.03.007 [DOI] [PubMed] [Google Scholar]
- 92.Cobb CO, Sahmarani K, Eissenberg T, Shihadeh A. Acute toxicant expo¬sure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a “healthy” tobacco-free alternative. ToxicolLett. 2012;215:70–75. doi: 10.1016/j.toxlet.2012.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nelson MD, Rezk-Hanna M, Rader F, Mason OR, Tang X, Shidban S, Rosenberry R, Benowitz NL, Tashkin DP, Elashoff RM, Lindner JR, Victor RG. Acute effect of hookah smoking on the human coronary microcirculation. Am J Cardiol. 2016; 117:1747–1754. doi: 10.1016/j.amjcard.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Blank MD, Cobb CO, Kilgalen B, Austin J, Weaver MF, Shihadeh A, Eissenberg T. Acute effects of waterpipe tobacco smoking: a double-blind, placebo-control study. Drug Alcohol Depend. 2011;116:102–109. doi: 10.1016/j.drugalcdep.2010.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Alomari MA, Khabour OF, Alzoubi KH, Shqair DM, Eissenberg T. Central and peripheral cardiovascular changes immediately after waterpipe smoking. Inhal Toxicol. 2014;26:579–587. doi: 10.3109/08958378.2014.936572 [DOI] [PubMed] [Google Scholar]
- 96.Alomari MA, Khabour OF, Alzoubi KH, Shqair DM, Stoner L. Acute vascular effects of waterpipe smoking: importance of physical activity and fitness status. Atherosclerosis. 2015;240:472–476. doi: 10.1016/j.atherosclerosis.2015.02.047 [DOI] [PubMed] [Google Scholar]
- 97.Bentur L, Hellou E, Goldbart A, Pillar G, Monovich E, Salameh M, Scherb I, Bentur Y. Laboratory and clinical acute effects of active and passive indoor group water-pipe (narghile) smoking. Chest. 2014;145:803–809. doi: 10.1378/chest.13-0960 [DOI] [PubMed] [Google Scholar]
- 98.Wolfram RM, Chehne F, Oguogho A, Sinzinger H. Narghile (water pipe) smoking influences platelet function and (iso-)eicosanoids. Life Sci. 2003;74:47–53. [DOI] [PubMed] [Google Scholar]
- 99.Selim GM, Fouad H, Ezzat S. Impact of shisha smoking on the extent of coronary artery disease in patients referred for coronary angiography. Anadolu Kardiyol Derg. 2013;13:647–654. doi: 10.5152/akd.2013.191 [DOI] [PubMed] [Google Scholar]
- 100.Ward KD, Ahn S, Mzayek F, Al Ali R, Rastam S, Asfar T, Fouad F, Maziak W. The relationship between waterpipe smoking and body weight: population-based findings from Syria. Nicotine Tob Res. 2015;17:34–40. doi: 10.1093/ntr/ntu121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shafique K, Mirza SS, Mughal MK, Arain ZI, Khan NA, Tareen MF, Ahmad I. Water-pipe smoking and metabolic syndrome: a population-based study. PLoS One. 2012;7:e39734. doi: 10.1371/journal.pone.0039734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Selim GM, Elia RZ, El Bohey AS, El Meniawy KA. Effect of shisha vs. cigarette smoking on endothelial function by brachial artery duplex ultrasonography: an observational study. Anadolu Kardiyol Derg. 2013;13:759–765. doi: 10.5152/akd.2013.4499 [DOI] [PubMed] [Google Scholar]
- 103.Sezavar SH, Abedi A, Sadeghi BH. A comparative study of plasma fibrinogen among hookah smokers, cigarette smokers and non-smokers. Iranian Heart J. 2004;5:48–54. [Google Scholar]
- 104.Sibai AM, Tohme RA, Almedawar MM, Itani T, Yassine SI, Nohra EA, Isma’eel HA. Lifetime cumulative exposure to waterpipe smoking is associated with coronary artery disease. Atherosclerosis. 2014;234:454–460. doi: 10.1016/j.atherosclerosis.2014.03.036 [DOI] [PubMed] [Google Scholar]
- 105.Al Suwaidi J, Zubaid M, El-Menyar AA, Singh R, Asaad N, Sulaiman K, Al Mahmeed W, Al-Shereiqi S, Akbar M, Al Binali HA. Prevalence and outcome of cigarette and waterpipe smoking among patients with acute coronary syndrome in six Middle-Eastern countries. Eur J Prev Cardiol. 2012;19:118–125. doi: 10.1177/1741826710393992 [DOI] [PubMed] [Google Scholar]
- 106.Islami F, Pourshams A, Vedanthan R, Poustchi H, Kamangar F, Golozar A, Etemadi A, Khademi H, Freedman ND, Merat S, Garg V, Fuster V, Wakefield J, Dawsey SM, Pharoah P, Brennan P, Abnet CC, Malekzadeh R, Boffetta P. Smoking water-pipe, chewing nass and prevalence of heart disease: a cross-sectional analysis of baseline data from the Golestan Cohort Study, Iran. Heart. 2013;99:272–278. doi: 10.1136/heartjnl-2012-302861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wu F, Chen Y, Parvez F, Segers S, Argos M, Islam T, Ahmed A, Rakibuz-Zaman M, Hasan R, Sarwar G, Ahsan H. A prospective study of tobacco smoking and mortality in Bangladesh. PLoS One. 2013;8:e58516. doi: 10.1371/journal.pone.0058516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mateen FJ, Carone M, Alam N, Streatfield PK, Black RE. A population-based case-control study of 1250 stroke deaths in rural Bangladesh. Eur J Neurol. 2012;19:999–1006. doi: 10.1111/j.1468-1331.2012.03666.x [DOI] [PubMed] [Google Scholar]
- 109.Northrup TF, Jacob P 3rd, Benowitz NL, Hoh E, Quintana PJ, Hovell MF, Matt GE, Stotts AL. Thirdhand smoke: state of the science and a call for policy expansion. Public Health Rep. 2016;131:233–238. doi: 10.1177/003335491613100206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cobb CO, Vansickel AR, Blank MD, Jentink K, Travers MJ, Eissenberg T. Indoor air quality in Virginia waterpipe cafes. Tob Control. 2013;22:338–343. doi: 10.1136/tobaccocontrol-2011-050350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Moon KA, Rule AM, Magid HS, Ferguson JM, Susan J, Sun Z, Torrey C, Abubaker S, Levshin V, Carkoglu A, Radwan GN, El-Rabbat M, Cohen JE, Strickland P, Breysse PN, Navas-Acien A. Biomarkers of secondhand smoke exposure in waterpipe tobacco venue employees in Istanbul, Moscow, and Cairo. Nicotine Tob Res. 2018;20:482–491. doi: 10.1093/ntr/ntx125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Raute LJ, Gupta PC, Pednekar MS. Smoking ban and indoor air quality in restaurants in Mumbai, India. Indian J Occup Environ Med. 2011;15:68–72doi: 10.4103/0019-5278.90377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Al-Bakri A, Jawad M, Salameh P, al’Absi M, Kassim S. Opportunistic insights into occupational health hazards associated with waterpipe tobacco smoking premises in the United Kingdom. Asian Pac J Cancer Prev. 2015;16:621–626. [DOI] [PubMed] [Google Scholar]
- 114.Saade G, Seidenberg AB, Rees VW, Otrock Z, Connolly GN. Indoor secondhand tobacco smoke emission levels in six Lebanese cities. Tob Control. 2010;19:138–142. doi: 10.1136/tc.2009.030460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Beachey EH. Protective immunity evoked by synthetic peptides of streptococcal M proteins. Adv Exp Med Biol. 1985;185:193–200. [DOI] [PubMed] [Google Scholar]
- 116.Maziak W, Rastam S, Ibrahim I, Ward KD, Eissenberg T. Waterpipe- associated particulate matter emissions. Nicotine Tob Res. 2008;10:519–523. doi: 10.1080/14622200801901989 [DOI] [PubMed] [Google Scholar]
- 117.Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD; on behalf of the American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 118.Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006:709. [PubMed] [Google Scholar]
- 119.Zhang B, Haji F, Kaufman P, Muir S, Ferrence R. “Enter at your own risk”: a multimethod study of air quality and biological measures in Canadian waterpipe cafes. Tob Control. 2015;24:175–181. doi: 10.1136/tobaccocontrol-2013-051180 [DOI] [PubMed] [Google Scholar]
- 120.Al Mulla A, Fanous N, Seidenberg AB, Rees VW. Secondhand smoke emission levels in waterpipe cafes in Doha, Qatar. Tob Control. 2015;24:e227–e231. doi: 10.1136/tobaccocontrol-2014-051717 [DOI] [PubMed] [Google Scholar]
- 121.Gurung G, Bradley J, Delgado-Saborit JM. Effects of shisha smoking on carbon monoxide and PM2.5 concentrations in the indoor and outdoor microenvironment of shisha premises. Sci Total Environ. 2016; 548–549:340–346. doi: 10.1016/j.scitotenv.2015.12.093 [DOI] [PubMed] [Google Scholar]
- 122.Fromme H, Schober W. Waterpipes and e-cigarettes: impact of alternative smoking techniques on indoor air quality and health. Atmos Environ. 2015;106:429–441. [Google Scholar]
- 123.Zhou S, Weitzman M, Vilcassim R, Wilson J, Legrand N, Saunders D, Travers M, Chen LC, Peltier R, Gordon T. Air quality in New York City hookah bars. Tob Control. 2015;24:e193–e198. doi: 10.1136/tobaccocontrol-2014-051763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kassem NO, Daffa RM, Liles S, Jackson SR, Kassem NO, Younis MA, Mehta S, Chen M, Jacob P 3rd, Carmella SG, Chatfield DA, Benowitz NL, Matt GE, Hecht SS, Hovell MF Children’s exposure to secondhand and thirdhand smoke carcinogens and toxicants in homes of hookah smok¬ers. Nicotine Tob Res. 2014;16:961–975. doi: 10.1093/ntr/ntu016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tamim H, Musharrafieh U, El Roueiheb Z, Yunis K, Almawi WY . Exposure of children to environmental tobacco smoke (ETS) and its association with respiratory ailments. J Asthma. 2003;40:571–576. [DOI] [PubMed] [Google Scholar]
- 126.Zeidan RK, Rachidi S, Awada S, El Hajje A, El Bawab W, Salame J, Bejjany R, Salameh P. Carbon monoxide and respiratory symptoms in young adult passive smokers: a pilot study comparing waterpipe to cigarette. Int J Occup Med Environ Health. 2014;27:571–582. doi: 10.2478/s13382-014-0246-z [DOI] [PubMed] [Google Scholar]
- 127.Kumar SR, Davies S, Weitzman M, Sherman S. A review of air quality, biological indicators and health effects of second-hand water-pipe smoke exposure. Tob Control. 2015;24(suppl 1):i54–i59. doi: 10.1136/tobaccocontrol-2014-052038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Anjum Q, Ahmed F, Ashfaq T. Knowledge, attitude and perception of water pipe smoking (shisha) among adolescents aged 14–19 years. J Pak Med Assoc. 2008;58:312–317. [PubMed] [Google Scholar]
- 129.Jaber R, Taleb ZB, Bahelah R, Madhivanan P, Maziak W. Perception, intention and attempts to quit smoking among Jordanian adolescents from the Irbid Longitudinal Study. Int J Tuberc Lung Dis. 2016;20:1689–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ward KD, Hammal F, VanderWeg MW, Eissenberg T, Asfar T, Rastam S, Maziak W. Are waterpipe users interested in quitting? Nicotine Tob Res. 2005;7:149–156. doi: 10.1080/14622200412331328402 [DOI] [PubMed] [Google Scholar]
- 131.Ward KD, Eissenberg T, Rastam S, Asfar T, Mzayek F, Fouad MF, Hammal E, Mock J, Maziak W. The tobacco epidemic in Syria. Tob Control. 2006;15(suppl 1):i24–i29. doi: 10.1136/tc.2005.014860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ward KD, Siddiqi K, Ahluwalia JS, Alexander AC, Asfar T. Waterpipe tobacco smoking: the critical need for cessation treatment. Drug Alcohol Depend. 2015;153:14–21. doi: 10.1016/j.drugalcdep.2015.05.029 [DOI] [PubMed] [Google Scholar]
- 133.Athamneh L, Sansgiry SS, Essien EJ, Abughosh S. Predictors of intention to quit waterpipe smoking: a survey of Arab Americans in Houston, Texas. J Addict. 2015;2015:575479. doi: 10.1155/2015/575479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Athamneh L, Essien EJ, Sansgiry SS, Abughosh S. Intention to quit water pipe smoking among Arab Americans: application of the theory of planned behavior. J Ethn Subst Abuse. 2017;16:80–90. doi: 10.1080/15332640.2015.1088423 [DOI] [PubMed] [Google Scholar]
- 135.Asfar T, Ward KD, Eissenberg T, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5:19. doi: 10.1186/1471-2458-5-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Borgan SM, Marhoon ZA, Whitford DL. Beliefs and perceptions toward quitting waterpipe smoking among cafe waterpipe tobacco smokers in Bahrain. Nicotine Tob Res. 2013;15:1816–1821. doi: 10.1093/ntr/ntt064 [DOI] [PubMed] [Google Scholar]
- 137.Asfar T, Al Ali R, Rastam S, Maziak W, Ward KD. Behavioral cessation treatment of waterpipe smoking: the first pilot randomized controlled trial. AddictBehav. 2014;39:1066–1074. doi: 10.1016/j.addbeh.2014.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.O’Neill N, Dogar O, Jawad M, Kellar I, Kanaan M, Siddiqi K. Which behavior change techniques may help waterpipe smokers to quit? An expert consensus using a modified Delphi technique. Nicotine Tob Res. 2018;20:154–160. doi: 10.1093/ntr/ntw297 [DOI] [PubMed] [Google Scholar]
- 139.Jawad M, Jawad S, Waziry RK, Ballout RA, Akl EA. Interventions for waterpipe tobacco smoking prevention and cessation: a systematic review. Sci Rep. 2016;6:25872. doi: 10.1038/srep25872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Maziak W, Jawad M, Jawad S, Ward KD, Eissenberg T, Asfar T . Interventions for waterpipe smoking cessation. Cochrane Database Syst Rev. 2015:CD005549. doi: 10.1002/14651858.CD005549.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Dogar O, Jawad M, Shah SK, Newell JN, Kanaan M, Khan MA, Siddiqi K. Effect of cessation interventions on hookah smoking: post-hoc analysis of a cluster-randomized controlled trial. Nicotine Tob Res. 2014;16:682–688. doi: 10.1093/ntr/ntt211 [DOI] [PubMed] [Google Scholar]
- 142.Mohlman MK, Boulos DN, El Setouhy M, Radwan G, Makambi K, Jillson I, Loffredo CA. A randomized, controlled community-wide intervention to reduce environmental tobacco smoke exposure. Nicotine Tob Res. 2013;15:1372–1381. doi: 10.1093/ntr/nts333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nakkash RT, Al Mulla A, Torossian L, Karhily R, Shuayb L, Mahfoud ZR, Janahi I, Al Ansari AA, Afifi RA. Challenges to obtaining parental permission for child participation in a school-based waterpipe tobacco smok¬ing prevention intervention in Qatar. BMC Med Ethics. 2014;15:70. doi: 10.1186/1472-6939-15-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Leavens ELS, Meier E, Tackett AP, Miller MB, Tahirkheli NN, Brett EI, Carroll DM, Driskill LM, Anderson MP, Wagener TL. The impact of a brief cessation induction intervention for waterpipe tobacco smoking: a pilot randomized clinical trial. Addict Behav. 2018;78:94–100. doi: 10.1016/j.addbeh.2017.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zahid R, Dogar O, Mansoor S, Khan A, Kanaan M, Jawad M, Ahluwalia JS, Siddiqi K. The efficacy of varenicline in achieving abstinence among waterpipe tobacco smokers: study protocol for a randomized controlled trial. Trials. 2017;18:14. doi: 10.1186/s13063-016-1761-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Aboaziza E, Eissenberg T. Waterpipe tobacco smoking: what is the evidence that it supports nicotine/tobacco dependence? Tob Control. 2015;24(suppl 1):i44–i53. doi: 10.1136/tobaccocontrol-2014-051910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Shihadeh AL, Eissenberg TE. Significance of smoking machine toxicant yields to blood-level exposure in water pipe tobacco smokers. Cancer Epidemiol BiomarkersPrev. 2011;20:2457–2460. doi: 10.1158/1055-9965.EPI-11-0586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2011;13:78–87. doi: 10.1093/ntr/ntq212 [DOI] [PMC free article] [PubMed] [Google Scholar]


