Abstract
This study aimed to compare head impact exposures between practices and games in football players ages 9 to 14, who account for approximately 70% of all football players in the US. Over a period of two seasons, 136 players were enrolled from three youth programs and 49,847 head impacts were recorded from 345 practices and 137 games. During the study, individual players sustained a median of 211 impacts per season, with a maximum of 1226 impacts. Players sustained 50th (95th) percentile peak linear acceleration of 18.3 (46.9) g, peak rotational acceleration of 1305.4 (3316.6) rads−2, and HITsp of 13.7 (24.3), respectively. Overall, players with a higher frequency of head impacts at practices recorded a higher frequency of head impacts at games (p < 0.001, r2 = 0.52) and players who sustained a greater average magnitude of head impacts during practice also recorded a greater average magnitude of head impacts during games (p < 0.001). The youth football head impact data quantified in this study provides valuable insight into the player exposure profile, which should serve as a key baseline in efforts to reduce injury.
Keywords: linear acceleration, rotational acceleration, HIT system, impacts per practice, impacts per game
INTRODUCTION
Sports-related brain injuries, especially mild traumatic brain injury (mTBI), have garnered public attention and led to questions on how to make sports safer for the athletes.1–6 Bryan et al. estimates an annual occurrence of 1.1 to 1.9 million sports- and recreation-related concussions in children under the age of 18 in the US.7 While concussions are defined as a transient disruption of brain function due to a direct or indirect biomechanical force to the brain, studies suggest subconcussive head impacts may lead to pathophysiological changes in brain function without the manifestation of concussion symptoms.8 Therefore, documenting exposure (magnitude, frequency, and location) of subconcussive head impacts remains an important challenge.
Injury statistics from the Consumer Product Safety Commission reported football (touch and tackle) to have the highest number of head injuries due to helmet to helmet collisions, and collision with a goal post, with some of these injuries being fatal.9 Initial studies quantifying the frequency and severity of head impacts in football have focused primarily on high school and collegiate players.10–14 However, there has been a recent increase in studies investigating head impact exposure in football players under the age of 14, who account for over 70% of the 5 million athletes participating in organized football each year.15–18 Daniel et al. reported an increase in magnitude and frequency of impacts as youth players progressed to higher age and weight groups.15 Their findings were consistent with other studies on age groups 7–8, 9–13, 14–18 and 18–22.19–23 While the relationship between an increase in the frequency of high magnitude impacts with age has previously been established, it is pertinent to understand the trends at the youth level, to gauge the cumulative effect of the head impacts that the players sustain throughout their career.
Recent studies have compared head impact exposure of practice and game sessions,13,21,22 citing specific drills as having the highest rate of high magnitude impacts during practice.24,25 Wong et al. also studied exposure in practices and games for individual players in the youth population, but the study was limited by a small sample size and the binary switch based impact sensor (Shockbox Impact Alert Sensor, Impakt Protective Inc., Canada) utilized in the study excluded all head impacts below 30 g,18 which would eliminate over 50% of the impacts reported by previous studies.12–15,21,26–29 Currently with no rigorous tool to diagnose, treat and prevent concussions in football, reducing head impact exposure is potentially an effective approach for reducing the risk of brain injury in this population.30–33
In addition to limiting contact during practice and changing practice structure, the relationship between head impact exposure at practices, and games for individual players at the youth level is also important but remains unknown. Analyzing the correlation between practices and games for individual players can provide more specifics on play technique and behavior, which may help identify specific players who could be at a higher risk for injury. Moreover, identifying player exposure profile could then allow coaches to implement strategies to reduce head impacts, ultimately mitigating the risk of injury. Therefore, this study aimed to investigate if individual players who sustain higher frequency of impacts per practice also sustain higher frequency of impacts per game and if individual players who receive greater magnitude impacts during practice also receive greater magnitude impacts during games.
METHODS
After IRB approval, 74 players (mean 10.9 + 1.2 years) were recruited from three youth programs (A, B and C) in 2015 and 96 players (mean 11.8 + 1.3 years) were recruited from the same youth programs in 2016. Informed assents were obtained from players, and informed consents were obtained from their parents. Thirty-four players contributed to both years of the study. Players from program A (n = 59) participated in an unaffiliated league, players from program B (n = 51) participated in the American Youth Football (AYF) league and players from program C (n = 26) participated in the Pop-Warner league. Data collection was conducted throughout two seasons (2015 and 2016) during practices (n = 345) and games (n = 137).
Players wore either Riddell Revolution or Speed football helmets that were instrumented with the Head Impact Telemetry (HIT) System (Simbex, Lebanon, NH) that is part of the [Riddell] Sideline Response System (SRS) (Riddell, Elyria, OH). The HIT System measures linear acceleration of the center of gravity (CG) of the head, estimates rotational acceleration at the CG, and impact location on the helmet.11,29,34–36 The HIT system includes a sideline receiver unit, laptop with radio receiver and sensor unit for each helmet. The sensor unit is comprised of an array of non-orthogonal single-axis accelerometers, and when a single accelerometer exceeds 9.6 g during an impact, the impact is recorded over a 40-millisecond duration, including 8-milliseconds of pre-trigger data. The HIT system has been validated and the errors associated with the system have been reported extensively.15,37–39
A session was defined as either a practice or a game. Practices were defined as sessions with a potential of contact to the head in which players wore helmets and pads. This definition included practices with helmet only and/or helmet and shoulder pads only sessions, which accounted for less than 0.8% of all practice impacts. Games included both competitions and scrimmages. Participation in a session was defined as a player receiving at least one impact for a given practice or game session.11
The biomechanical data consisted of head-impact events that exceeded a peak resultant linear acceleration of 10 g. In this study, as in our previous studies, the peak resultant linear acceleration threshold of 10 g was implemented to eliminate head accelerations from non-injurious acceleration events (e.g. running, jumping, etc.). 11,40 Video footage was collected at all sessions and researchers verified impacts above 60 g through video identification to avoid overestimation of the frequency of these higher magnitude impacts. Events recorded outside of an organized team sessions (game, practice, or scrimmage) and during water breaks were removed before analysis. Other recorded events that do not represent typical rigid body head acceleration patterns, such as those from a helmet being kicked or thrown, were also excluded from the dataset.35
Five measures of head impact frequency were analyzed for each player: number of practice impacts, the total number of head impacts a player sustained during all practices; number of game impacts, the total number of head impacts a player sustained during all games; impacts per season, the total number of head impacts for a player during all team sessions in a single season; impacts per practice, the average number of head impacts a player sustained during practices; and impacts per game, the average number of head impacts a player sustained during games.10 For all exposure measures, each impact was analyzed individually but the cumulative number of impacts, for players that participated in both years of the study, was averaged to report impacts per season. Each individual player’s distribution of peak linear acceleration (g), peak rotational acceleration (rad s−2), and peak HITsp were quantified by the 50th and 95th percentile value for each session type. HITsp is a non-dimensional measure of head impact severity.41 It is measured by transforming the computed head impact measures into a single latent variable using Principal Component Analysis and applying a weighting factor based on impact location.41
Data was analyzed using Matlab (Mathworks,Natick,MA), and exported to SigmaPlot (Systat Software, Chicago, IL) and GraphPad (GraphPad Software, San Diego, CA) for statistical analysis. Measures of impact frequency and magnitude were expressed as median values and [25% - 75%] inter-quartile range, as the study measures were not normally distributed, according to the Shapiro-Wilk Normality test. Correlations in head impact exposure measures between practices and games were assessed using linear regression analysis and outliers were not removed. Wilcoxon signed rank tests were performed to analyze differences in acceleration values between practices and games. Differences in impacts per season across programs were examined using a Kruskal-Wallis one-way ANOVA on ranks.
RESULTS
A total of 49,847 head impacts were recorded over the two seasons within 482 sessions (345 practices and 137 games). Players participated in a median of 19.0 [15.0–23.3] practices per season and 9.0 [7.0–10.0] games per season.
The median total number of head impacts per season received by an individual player was 211.0 [122.3–371.5] with a maximum of 1225.5 impacts. The median total number of impacts sustained per season during practices was 132.0 [69.5–235.5], with a maximum of 660.0 impacts. The median total number of impacts sustained per season during games was 71.3 [36.0–139.0], with a maximum of 581.5 impacts. For individual sessions, the median number of impacts received by a player was 7.2 [4.6–10.5] per practice and 7.9 [4.6–15.4] per game.
The number of head impacts per practice had a significant positive correlation (p < 0.001, r2 = 0.52) with the number of head impacts per game for individual players (Figure 1). All three programs had a significant (p = 0.003, r2 = 0.63(A), 0.38(B), 0.31(C)) relationship between impacts per practice and impacts per game across individual players (Figure 2) even though the total number of impacts varied significantly (p < 0.0001) among the different programs (Figure 3).
Figure 1.
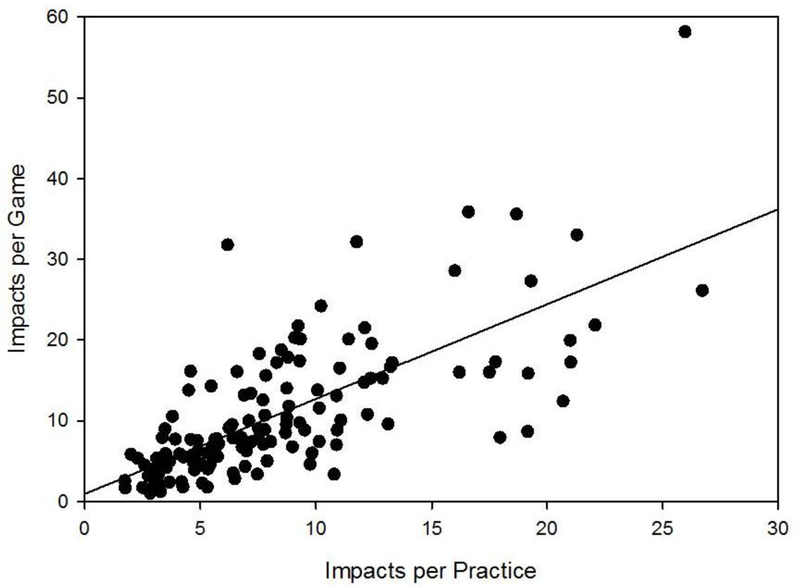
Impacts per game correlated linearly (r2 = 0.52, p < 0.001) with impacts per practice for individual players. Each data point represents an individual player.
Figure 2.
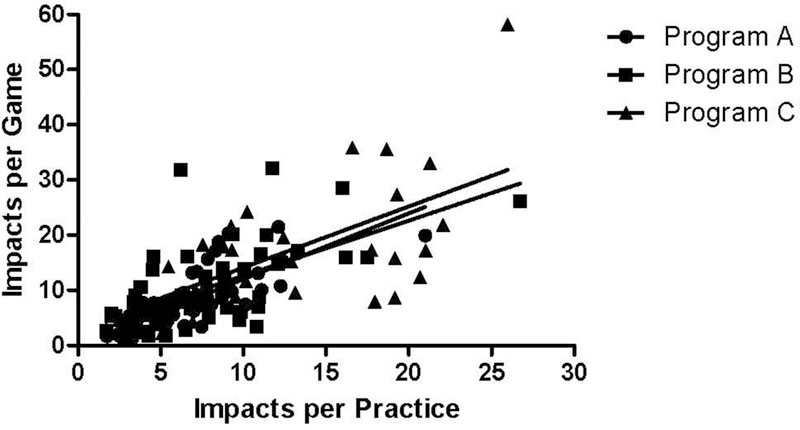
Correlation between impact frequency per practice and per game for individual players did not differ significantly by program.
Figure 3.
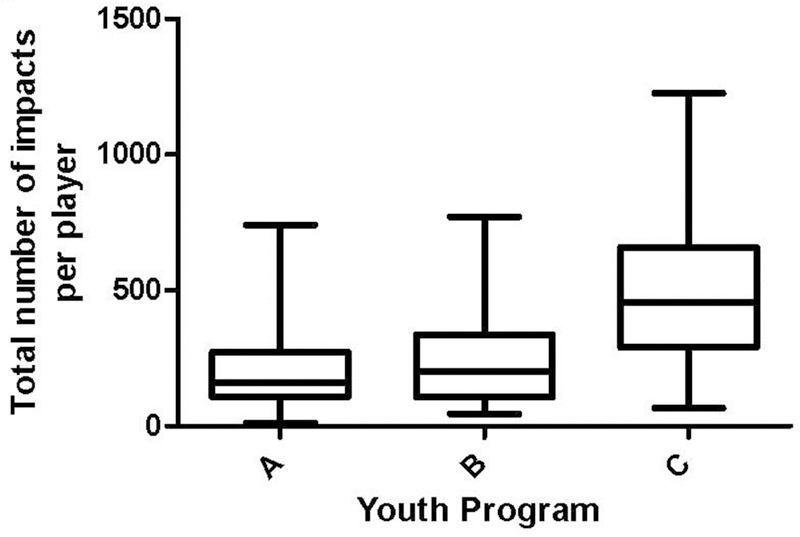
Distribution of total number of impacts per player per season differed substantially among the three youth programs.
Study-wide, 10.0% of head impacts (n = 4959.0) were greater than 40 g, 2.8% of impacts (n = 1397.0) were greater than 60 g, and 0.8% of impacts (n = 414.0) were greater than 80 g. By location, 51.6% of head impacts were to the front of the helmet, 20.1% were to the back of the helmet, 18.6% were to the side of the helmet and 9.7% were to the top of the helmet. The exposure data for right and left head impact locations did not differ significantly (p = 0.346), so they were combined and reported as head impacts to the side.
Although the median difference was minimal (0.20 g), players experienced significantly lower median linear acceleration during practices than games (p = 0.039, Table 1). Players also experienced impacts with significantly lower estimated median rotational acceleration and 95th percentile peak HITsp during practices than games (p = 0.023, p = 0.036 and median difference = 47 rad s−2, 0.7). There were no significant differences between practices and games for 95th percentile peak linear acceleration (p = 0.833), 95th percentile peak rotational acceleration (p = 0.109), or 50th percentile peak HITsp (p = 0.133) (Table 1). There was, however, a significant positive correlation (p < 0.001) within the study population between practices and games for the 50th and 95th linear acceleration, rotational acceleration and HITsp (Figure 4 & Table 1). Correlations between impacts per season and the 95th percentile peak linear acceleration, rotational acceleration and HITsp were not as strong (r2 = 0.07, 0.04 and 0.09 respectively) as the correlations for the 50th and 95th linear acceleration, rotational acceleration and HITsp.
Table 1:
Linear regression analysis for games vs practice and study wide 50th and 95th percentile peak linear acceleration, peak rotational acceleration and peak HITsp for the season, practices and games.
| Season | Practice | Game |
Slope of best fit |
p-value | r2 | ||
|---|---|---|---|---|---|---|---|
| 50th % | Linear Acc (g) | 18.3[17.1–19.3] | 18.2[16.6–19.4] | 18.4[16.8–19.8] | 0.54 ± 0.09 | p < 0.001 | 0.21 |
| Rotational Acc (rad.s−2) | 1305.4[1188.2–1397.4] | 1290.0[1151.0–1404.0] | 1337.0[1217.0–1441.0] | 0.79 ± 0.07 | p < 0.001 | 0.46 | |
| HITsp | 13.7[13.2–14.2] | 13.6[13.0–14.2] | 13.9[13.1–14.5] | 0.83 ± 0.08 | p < 0.001 | 0.42 | |
| 95th % | Linear Acc (g) | 46.9[40.5–52.5] | 47.0[38.8–52.9] | 46.5[40.8–54.1] | 0.46 ± 0.06 | p < 0.001 | 0.28 |
| Rotational Acc (rad.s−2) | 3316.6[2852.3–3664.9] | 3187.0[2772.0–3658.0] | 3278.0[2844.0–3920.0] | 0.49 ± 0.09 | p < 0.001 | 0.18 | |
| HITsp | 24.3[22.0–27.3] | 24.1[21.4–27.2] | 24.9[21.4–28.2] | 0.60± 0.07 | p < 0.001 | 0.34 |
Note. Results expressed as mean + SD. Results expressed as Median [25th-75th] percentile
Symbolizes significance difference between accelerations at practice and games
Figure 4.
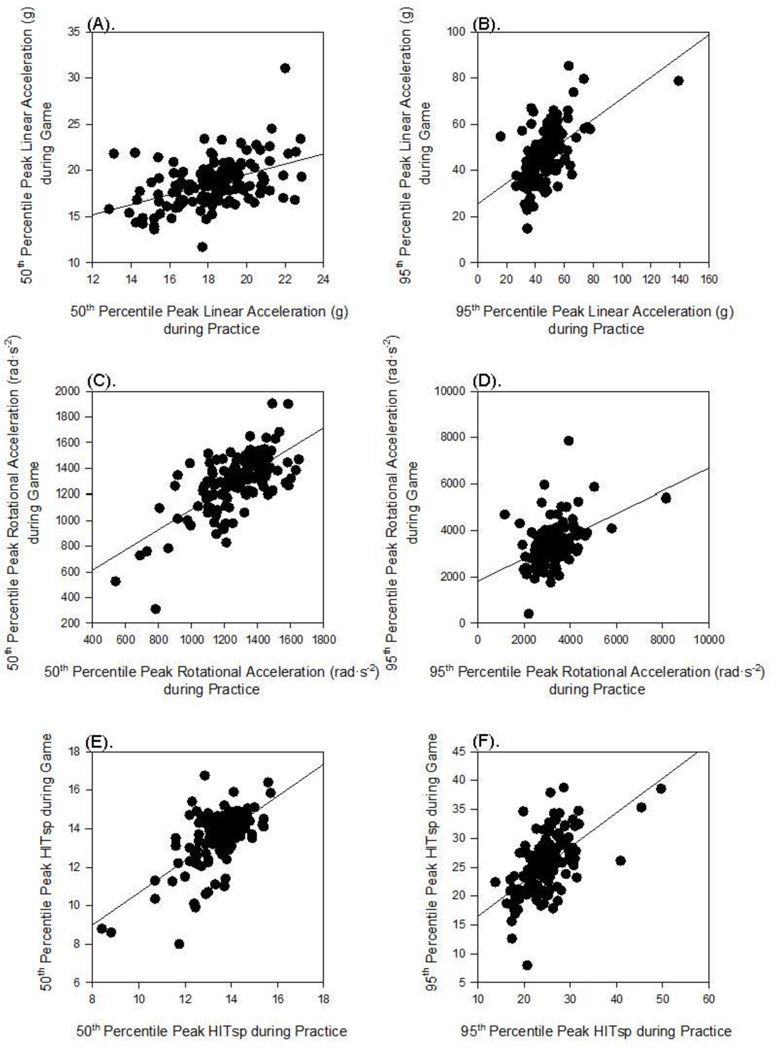
Positive significant correlation was found between head impacts during practice and games for median peak linear acceleration (g) (A), 95th percentile peak linear acceleration (g) (B), median peak rotational acceleration (rad s−2) (C), 95th percentile peak rotational acceleration (rad s−2) (D), median peak HITsp and (E), 95th percentile peak HITsp (F).
DISCUSSION
The purpose of this study was to quantify head impact exposure in youth football players ages 9–14 and analyze the relationships between impact frequency and magnitude per individual player by session type. From two years of data, we found that a higher number of impacts per practice correlated with a higher number of impacts per game for individual players. Additionally, greater magnitude impacts during practices were also correlated with greater magnitude impacts during games for individual players. There was, however, no correlation between head impact frequencies and head impact magnitudes. Collectively, these findings indicate that there is a correlation in head impact exposure between practices and games, but that players who experience the largest magnitude head impacts do not necessarily receive the most frequent head impacts.
Overall, the median number of head impacts recorded per player was 7.2 per practice and 7.9 per game. These values are within the range of values reported by Cobb et al. (9.7 per practice, 11.3 per game), Young et al. (9.0 per practice, 11.0 per game), Munce et al. (9.0 per practice, 12.0 per game) and Daniel et al. (6.7 per practice, 5.8 per game) at the youth level.15,16,19,20 Our results were also consistent with studies that reported an increase in head impact exposure with age and level of play (youth to high school, high school to college).15,23,42 The frequency of impacts by session for players in this youth study was less than the range of impacts reported in previous studies for high school (5.3–9.4 impacts per practice and 13.0–15.5 impacts per game) and collegiate players (6.3–13.2 impacts per practice and 14.3–24.2 impacts per game).10,14,21,22,28,43 Cobb et al., postulated that this increase in impact frequency from youth to high school and high school to collegiate level was due to an increase in size, strength, and speed of the players.17 It is also interesting to note that even though the total number of head impacts significantly differed across the three observed youth programs (Figure 3), the positive correlation of impact frequency between practices and games remained across the three youth programs (Figure 2).
In considering impact magnitudes, the median linear acceleration for practices (18.2 g) and games (18.4 g) measured in this study were similar to those reported by Cobb et al. (18.0 g in practices, 19.0 g in games), Young et al. (17.0 g in practices, 17.0 g in games) and Munce et al. (19.9 g in practices, 20.9 g in games) at the youth level.16,19,20 While the median linear and rotational acceleration values of the current study (18.3 g, 1305.4 rads−2) were in approximately the same range as that of the high school population (20.5–27.1 g, 942.0–1468.6 rads−2) and the collegiate population (20.5–32.0 g, 981.0–1400.0 rads−2), the 95th percentile magnitude values (46.7 g, 3316.6 rads−2) of this study were lower when compared to their high school and collegiate counterparts (53.7–62.7 g, ~4378 rads−2).11–13,21,22,26,44,45 This indicates that the youth players in this study population are sustaining lower high magnitude impacts. Other researchers have hypothesized that youth players may be at a greater risk of injury compared with high school and collegiate players because they possess lower body mass and neck strength.46–49 However, our study protocol did not control for factors such as player mass, neck strength, and preparedness. It is also important to appreciate that wearable sensors, such as the HIT system used in this study, measure resultant head accelerations and not the impact force.
While evaluating the correlation of the frequency and magnitude variables between practice and game for individual players provided a unique opportunity to identify player profile, the study also has several limitations. A player was designated as participating in a session only if the player received at least one head impact above 10 g. This definition is enabled using exposure sensors such as the HIT system, which allows us to specifically study head impact exposure instead of the often-used metric of athletic exposure (AE).50 Our previous studies have shown that AE can be a very poor measure of head injury risk. It was shown that players with the same risk of head injury as defined by AE (e.g. 50) had dramatically different numbers of head impact that varied from approximately 200 to 1400. Impacts lower than 60 g did not go through the same validation process because of the challenges involved in identifying impacts (e.g. low resolution, occluded views, etc.).51 Additionally, impacts above 60 g are more readily verified, whereas lower magnitude impacts are difficult to locate on video and far greater in frequency. Players with elevated head impact exposure were included in the analysis, as they may offer better insight into players associated with high magnitude and/or frequency impacts. A more detailed behavioral analysis of these players may be warranted, as they may benefit from interventions in attempts to reduce head impacts. While player position has demonstrated to be a strong factor in head impact exposures with high school and collegiate population,10–14,22,50 it was not used as a factor to analyze impact exposure in this study because assigning a specific position to each youth player was challenging; majority of youth players in these programs participated in offense, defense, and special teams, including various positions within each unit.
Previous studies have attributed differences in head impact exposure among teams and programs to variations in style of play,52,53 practice drill implementation,24 coaching style,54 tackling style,55–57 difference in the number of players per team, or difference in league rules.16 The study analysis presented herein did not control for these factors. However, the fact that the correlation in head impact exposures between practices and games persisted despite the variations in these factors suggest that a player’s specific behavior may play a large role in their exposures. In that case, coaches being provided with resources to monitor head impact, and implement strategies to reduce head impact33,58 may be an efficient way of limiting impact exposure.
In conclusion, findings of this study suggest the frequency and magnitude of impacts that players sustain during practice have a positive association with impacts they sustain during games. Players who experience elevated magnitude and/or frequency of head impacts in practices also experience elevated magnitude and/or high frequency of head impacts in games. Ultimately, these findings, along with more data collection and analysis at the youth level, may give researchers an insight into players with tendencies for elevated head impact exposure. Understanding these associations should help in reducing the risk of brain injury in youth football.
Acknowledgement
Research reported in this publication was supported by the National Institutes of Health under the Award Number NIH R01NS094410. HIT System technology was developed in part under NIH R44HD40743 and research and development support from Riddell, Inc. (Elyria, OH). We appreciate and acknowledge the researchers and institutions from which the data were collected and would also like to thank Bethany Wilcox and Arlene Garcia from Brown University.
Disclosure of Funding: Research reported in this publication was supported by the National Institutes of Health under the Award Number NIH R01NS094410. HIT System technology was developed in part under NIH R44HD40743 and research and development support from Riddell, Inc. (Elyria, OH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: Joseph J. Crisco, Richard M. Greenwald, Jonathan G. Beckwith and Simbex have a financial interest in the instruments (HIT System, Sideline Response System, Riddell, Inc.) that were used to collect the biomechanical data reported in this study.
References
- 1.Gerberding JL. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Cent Dis Control Prev. September 2003. [Google Scholar]
- 2.Thunnan DJM, Branche CM, Sniezek JEM. The Epidemiology of Sports-Related Traumatic Brain Injuries in the United States: Recent Developments. J Head Trauma Rehabil. 1998;13(2):1–8. [DOI] [PubMed] [Google Scholar]
- 3.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. [DOI] [PubMed] [Google Scholar]
- 4.Powell JW, Barber-Foss KD. Injury Patterns in Selected High School Sports: A Review of the 1995–1997 Seasons. J Athl Train. 1999;34(3):277–284. [PMC free article] [PubMed] [Google Scholar]
- 5.Collins MW, Lovell MR, Mckeag DB. Current issues in managing sports-related concussion. JAMA. 1999;282(24):2283–2285. [DOI] [PubMed] [Google Scholar]
- 6.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. [DOI] [PubMed] [Google Scholar]
- 7.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F, Collaborative on behalf of the SSCR. Sports- and Recreation-Related Concussions in US Youth. Pediatrics. 2016;138(1):e20154635. [DOI] [PubMed] [Google Scholar]
- 8.Broglio SP, Eckner JT, Paulson HL, Kutcher JS. Cognitive Decline and Aging: The role of Concussive and Subconcussive Impacts. Exerc Sport Sci Rev. 2012;40(3):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brien C, Rutherford G, Marcy N. Injury Statistic - Hazard Screening Report. July 2004. [Google Scholar]
- 10.Crisco JJ, Fiore R, Beckwith JG, et al. Frequency and location of head impact exposures in individual collegiate football players. J Athl Train. 2010;45(6):549–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crisco JJ, Wilcox BJ, Beckwith JG, et al. Head impact exposure in collegiate football players. J Biomech. 2011;44(15):2673–2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Broglio SP, Sosnoff JJ, Shin S, He X, Alcaraz C, Zimmerman J. Head Impacts During High School Football: A Biomechanical Assessment. J Athl Train. 2009;44(4):342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mihalik JP, Bell DR, Marshall SW, Guskiewicz KM. Measurement of head impacts in collegiate football players: An investigation of positional and event-type differences. Neurosurgery. 2007;61(6):1229–1235. [DOI] [PubMed] [Google Scholar]
- 14.Schnebel B, Gwin JT, Anderson S, Gatlin R. In Vivo Study of Head Impacts in Football: A Comparison of National Collegiate Athletic Association Division I versus High School Impacts. Neurosurgery. 2007;60(3):490–496. [DOI] [PubMed] [Google Scholar]
- 15.Daniel RW, Rowson S, Duma SM. Head impact exposure in youth football. Ann Biomed Eng. 2012;40(4):976–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cobb BR, Urban JE, Davenport EM, et al. Head Impact Exposure in Youth Football: Elementary School Ages 9–12 Years and the Effect of Practice Structure. Ann Biomed Eng. July 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cobb BR, Rowson S, Duma SM. Age-related differences in head impact exposure of 9–13 year old football players. BiomedSci Instrum. 2014;50:285–290. [PubMed] [Google Scholar]
- 18.Wong RH, Wong AK, Bailes JE. Frequency, magnitude, and distribution of head impacts in Pop Warner football: the cumulative burden. Clin Neurol Neurosurg. 2014;118:1–4. [DOI] [PubMed] [Google Scholar]
- 19.Young TJ, Daniel RW, Rowson S, Duma SM. Head impact exposure in youth football: elementary school ages 7–8 years and the effect of returning players. Clin J Sport Med Off J Can Acad Sport Med. 2014;24(5):416–421. [DOI] [PubMed] [Google Scholar]
- 20.Munce TA, Dorman JC, Thompson PA, Valentine VD, Bergeron MF. Head Impact Exposure and Neurologic Function of Youth Football Players. Med Sci Sports Exerc. November 2014. [DOI] [PubMed] [Google Scholar]
- 21.Urban JE, Davenport EM, Golman AJ, et al. Head Impact Exposure in Youth Football: High School Ages 14 to 18 Years and Cumulative Impact Analysis. Ann Biomed Eng. July 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds BB, Patrie J, Henry EJ, et al. Comparative Analysis of Head Impact in Contact and Collision Sports. J Neurotrauma. 2017;34(1):38–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelley ME, Urban JE, Miller LE, et al. Head Impact Exposure in Youth Football: Comparing Age- and Weight-Based Levels of Play. J Neurotrauma. April 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campolettano ET, Rowson S, Duma SM. Drill-specific head impact exposure in youth football practice. J Neurosurg Pediatr. 2016;18(5):536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelley ME, Kane JM, Espeland MA, et al. Head impact exposure measured in a single youth football team during practice drills. J Neurosurg Pediatr. 2017;20(5):489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brolinson PG, Manoogian S, McNeely D, Goforth M, Greenwald R, Duma S. Analysis of linear head accelerations from collegiate football impacts. Curr Sports Med Rep. 2006;5(1):23–28. [DOI] [PubMed] [Google Scholar]
- 27.Naunheim RS, Standeven J, Richter C, Lewis LM. Comparison of impact data in hockey, football, and soccer. J Trauma Inj Infect Crit Care. 2000;48:1–4. [DOI] [PubMed] [Google Scholar]
- 28.Duma SM, Manoogian SJ, Bussone WR, et al. Analysis of real-time head accelerations in collegiate football players. Clin J Sport Med Off J Can Acad Sport Med. 2005;15(1):3–8. [DOI] [PubMed] [Google Scholar]
- 29.Crisco JJ, Wilcox BJ, Machan JT, et al. Magnitude of head impact exposures in individual collegiate football players. J Appl Biomech. 2012;28(2):174–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crisco JJ, Greenwald RM. Let’s get the head further out of the game: a proposal for reducing brain injuries in helmeted contact sports. Curr Sports Med Rep. 2011;10(1):7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Broglio SP, Martini D, Kasper L, Eckner JT, Kutcher JS. Estimation of head impact exposure in high school football: Implications for regulating contact practices. Am J Sports Med. 2013;41(12):2877–2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of Concussion During Practice and Games in Youth, High School, and Collegiate American Football Players. JAMA Pediatr. 2015;169(7):659–665. [DOI] [PubMed] [Google Scholar]
- 33.Cantu R, Nowinski C. Sports Legacy Institute “Hit Count” White Paper. February 2012. [Google Scholar]
- 34.Beckwith JG, Chu JJ, Greenwald RM. Validation of a noninvasive system for measuring head acceleration for use during boxing competition. J Appl Biomech. 2007;23(3):238–244. [DOI] [PubMed] [Google Scholar]
- 35.Crisco JJ, Chu JJ, Greenwald RM. An algorithm for estimating acceleration magnitude and impact location using multiple nonorthogonal single-axis accelerometers. J Biomech Eng. 2004;126(6):849–854. [DOI] [PubMed] [Google Scholar]
- 36.Manoogian S, McNeely D, Duma S, Brolinson G, Greenwald R. Head acceleration is less than 10 percent of helmet acceleration in football impacts. BiomedSci Instrum. 2006;42:383–388. [PubMed] [Google Scholar]
- 37.Rowson S, Duma SM, Beckwith JG, et al. Rotational head kinematics in football impacts: an injury risk function for concussion. Ann Biomed Eng. 2012;40(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rowson S, Beckwith JG, Chu JJ, Leonard DS, Greenwald RM, Duma SM. A six degree of freedom head acceleration measurement device for use in football. J Appl Biomech. 2011;27(1):8–14. [DOI] [PubMed] [Google Scholar]
- 39.Beckwith JG, Greenwald RM, Chu JJ. Measuring head kinematics in football: correlation between the head impact telemetry system and Hybrid III headform. Ann Biomed Eng. 2012;40(1):237–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ng TP, Bussone WR, Duma SM. The effect of gender and body size on linear accelerations of the head observed during daily activities. Biomed Sci Instrum. 2006;42:25–30. [PubMed] [Google Scholar]
- 41.Greenwald RM, Gwin JT, Chu JJ, Crisco JJ. Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery. 2008;62(4):789–798; discussion 798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fitness C on SMA. Tackling in Youth Football. Pediatrics. 2015;136(5):e1419–e1430. [DOI] [PubMed] [Google Scholar]
- 43.Talavage TM, Nauman EA, Breedlove EL, et al. Functionally-Detected Cognitive Impairment in High School Football Players without Clinically-Diagnosed Concussion. J Neurotrauma. 2014;31(4):327–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eckner JT, Sabin M, Kutcher JS, Broglio SP. No Evidence for a Cumulative Impact Effect on Concussion Injury Threshold. J Neurotrauma. 2011;28(10):2079–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breedlove EL, Robinson M, Talavage TM, et al. Biomechanical correlates of symptomatic and asymptomatic neurophysiological impairment in high school football. J Biomech. 2012;45(7):1265–1272. [DOI] [PubMed] [Google Scholar]
- 46.Viano DC, Casson IR, Pellman EJ. Concussion in professional football: biomechanics of the struck player--part 14. Neurosurgery. 2007;61:313–27; discussion 327–8. [DOI] [PubMed] [Google Scholar]
- 47.Collins CL, Fletcher EN, Fields SK, et al. Neck Strength: A Protective Factor Reducing Risk for Concussion in High School Sports. J Prim Prev. 2014;35(5):309–319. [DOI] [PubMed] [Google Scholar]
- 48.Gutierrez GM, Conte C, Lightbourne K. The relationship between impact force, neck strength, and neurocognitive performance in soccer heading in adolescent females. Pediatr Exerc Sci. 2014;26(1):33–40. [DOI] [PubMed] [Google Scholar]
- 49.Eckner JT, Oh YK, Joshi MS, Richardson JK, Ashton-Miller JA. Effect of Neck Muscle Strength and Anticipatory Cervical Muscle Activation on the Kinematic Response of the Head to Impulsive Loads. Am J Sports Med. 2014;42(3):566–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dick R, Lincoln AE, Agel J, Carter EA, Marshall SW, Hinton RY. Descriptive epidemiology of collegiate women’s lacrosse injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):262–269. [PMC free article] [PubMed] [Google Scholar]
- 51.Meeuwisse WH, Love EJ. Development, implementation, and validation of the Canadian Intercollegiate Sport Injury Registry. Clin J Sport Med Off J Can Acad Sport Med. 1998;8(3):164–177. [DOI] [PubMed] [Google Scholar]
- 52.Kucera KL, Yau RK, Register-Mihalik J, et al. Traumatic Brain and Spinal Cord Fatalities Among High School and College Football Players - United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2017;65(52):1465–1469. [DOI] [PubMed] [Google Scholar]
- 53.Kerr ZY, Yeargin SW, Valovich McLeod TC, Mensch J, Hayden R, Dompier TP. Comprehensive Coach Education Reduces Head Impact Exposure in American Youth Football. Orthop J Sports Med. 2015;3(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kerr ZY, Kroshus E, Lee JGL, Yeargin SW, Dompier TP. Coaches’ Implementation of the USA Football “Heads Up Football” Educational Program. Health Promot Pract. March 2017:1–10. [DOI] [PubMed] [Google Scholar]
- 55.Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35(8):1295–1303. [DOI] [PubMed] [Google Scholar]
- 56.Badgeley MA, McIlvain NM, Yard EE, Fields SK, Comstock RD. Epidemiology of 10,000 high school football injuries: patterns of injury by position played. J Phys Act Health. 2013;10(2):160–169. [DOI] [PubMed] [Google Scholar]
- 57.Kontos AP, Elbin RJ, Fazio-Sumrock VC, et al. Incidence of Sports-Related Concussion among Youth Football Players Aged 8–12 Years. J Pediatr. 2013;163(3):717–720. [DOI] [PubMed] [Google Scholar]
- 58.Greenwald RM, Chu JJ, Beckwith JG, Crisco JJ. A proposed method to reduce underreporting of brain injury in sports. Clin J Sport Med Off J Can Acad Sport Med. 2012;22(2):83–85. [DOI] [PubMed] [Google Scholar]


