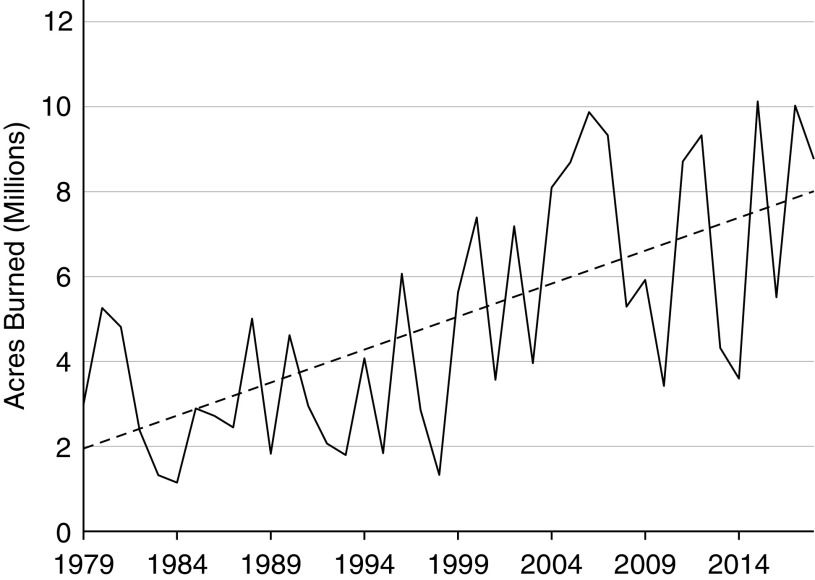
Wildfires are a growing threat to public health in the United States and around the world, as evidenced by the recent catastrophic fires in California, the Pacific Northwest, and Greece. Due to climate change, hotter and drier weather in the western United States and other areas of the globe is likely to accelerate this trend (1). Greater frequency, intensity, and duration of wildland fires have combined with an expanding wildland–urban interface to cause widespread impacts on air quality and public health, as well as devastating local losses of life, health, and property (2) (Figure 1). Rapidly increasing and shifting concentrations of wildfire smoke causing unhealthy levels of air pollution downwind of wildfires demand effective responses at the individual, family, community, and population levels (3).
Figure 1.
Total acres burned in wildfires in the United States, 1979 through 2018, with linear regression trend line (dashed). Source: National Interagency Fire Center. (https://www.nifc.gov/fireInfo/fireInfo_stats_totalFires.html).
Smoke from large fires can spread over thousands of square kilometers, potentially affecting the air breathed by millions of people. Annual global mortality from wildfire smoke has been estimated to be over 300,000 persons (4). With increasing frequency of wildfires has come increasing awareness of adverse health effects of wildfire smoke. What are effective actions that individuals, especially those at higher risk, can take to reduce personal exposure to ambient air pollution, including wildfire smoke? What is the balance of potential benefits and harms that may result from individual actions to reduce exposure? A May 2018 American Thoracic Society workshop, “Personal Interventions for Reducing Exposure and Risk from Air Pollution,” sought to begin to answer these questions, with a report anticipated in 2019.
Wildfire smoke is a complex mixture of fine and course particulate matter (PM) and gases, including carbon monoxide, nitrogen oxides, volatile organic compounds, and air toxics. The chemical composition of wildfire smoke particles and gases varies with the types of fuel, moisture, intensity of the fire, and other factors. Systematic reviews have found strong evidence of associations between wildfire smoke and all-cause mortality and exacerbation of asthma, chronic obstructive pulmonary disease, and respiratory infection (5, 6). Individual components of wildfire smoke (e.g., PM, carbon monoxide, and nitrogen oxides) have established links to cardiovascular and respiratory mortality and morbidity, and more recent evidence suggests associations with adverse reproductive, developmental, and neurodegenerative diseases (7). Groups that are considered more susceptible to smoke and other air pollutants include those with pre-existing respiratory and cardiovascular disease, pregnant women and their fetuses, young children, and older adults (8).
Personal Interventions
Options for personal action to reduce exposure to wildfire smoke include evacuation, staying indoors, limiting physical activity, air filtration, and wearing respiratory protective devices (respirators, a.k.a. “masks”; Table 1). Each of these interventions has important limitations, and may have unintended adverse effects. No large-scale observational studies or clinical trials have tested the efficacy, effectiveness, or potential harms of these interventions when recommended by public health officials or health care providers for wildfire smoke exposure. Evidence is largely limited to small-scale studies of efficacy and/or effectiveness of air filtration or use of respirators for reducing exposure to ambient air pollution in experimental settings.
Table 1.
Summary of personal actions for reducing exposure to particulate matter from wildfire smoke, in order of priority according to the hierarchy of controls
| Tier in Hierarchy of Controls | Exposure Control Action | Estimated Exposure Reduction | Considerations |
|---|---|---|---|
| 1. Elimination | Relocation | 100% |
|
| 2. Engineering |
|
20–80% |
|
| 3. Administrative | Stay indoors | ∼50% on average, but varies widely | Without added filtration, the building envelope limits infiltration to a widely variable extent depending on tightness |
| Avoid heavy or prolonged physical activity | Lowers inhaled dose of pollutants |
|
|
| 4. Personal protective equipment | Wear a NIOSH-approved N95 or P100 filtering facepiece respirator | 90% or greater, depending on quality of fit. Near 0% if poorly fitted |
|
Definition of abbreviations: HEPA = high-efficiency particulate air; NIOSH = National Institute for Occupational Safety and Health; PM = particulate matter.
Avoiding wildfire smoke by evacuating may be the most prudent action, depending on the severity of the conditions, balanced against the stress of evacuation, which has been associated with increased mortality in vulnerable people (9). Staying indoors, where levels of outdoor pollutants are typically lower if windows and doors are closed, and limiting physical activity, which decreases inhaled doses of pollutants (10), have been the mainstays of advice from the U.S. Environmental Protection Agency and others for “bad air” days. Applied over relatively short durations and in the absence of indoor air pollutant sources, these recommendations are unlikely to cause unintended adverse effects on health and well-being. Indoor air filtration with properly sized, high-efficiency particulate air filters can further reduce indoor concentrations of PM by up to about 80% (11). The effectiveness of portable filters for reducing indoor concentrations of wildfire smoke PM depends on the clean air delivery rate and rate at which smoke PM infiltrates the indoor space. Air filtration in a designated “clean room” with the fewest doors and windows can further ensure exposure reduction (12). Air-purifying respirators certified by the National Institute for Occupational Safety and Health (NIOSH) can reduce inhalation exposure, but respirators have significant limitations and may present additional health risks, especially with prolonged use.
Prioritizing Personal Interventions
How can one prioritize interventions to maximize potential benefits and minimize potential risks of personal actions in complex and changing wildfire circumstances? Making decisions about how to control personal exposure to air contaminants has a long history in occupational/industrial settings. In particular, the traditional “hierarchy of controls” for workplace hazards, dating back at least to the mid-20th century, provides a useful framework for controlling individual exposure to wildfire smoke (13). The underlying principle is to control the hazard as close to the source as possible. Controls are prioritized in descending order of: 1) elimination of the hazard at the source (fire prevention, fire suppression, relocation); 2) engineering controls (filtration by the building “envelope” and added mechanical air filtration); 3) administrative controls (staying indoors, reducing physical activity): and, finally, 4) personal protective equipment (respirators). According to established principles and practices of workplace health and safety, respirators are only to be used when higher-level controls are not feasible or are not yet implemented, or in emergencies (13).
The rationale for using respirators temporarily and as a last resort in occupational settings among workers also applies to the use of respirators for air pollution among members of the general public. Respirators place significant burdens for control of exposure on the individual, and they have important limitations. Filtering-facepiece respirators (N95 or P100) that have been tested and approved by NIOSH can be effective against PM, the component of wildfire smoke most clearly related to adverse health effects, but they do not provide protection against gasses. The protection afforded by these respirators depends on a tight seal between the respirator and the face. During inhalation, the wearer generates a negative pressure inside the respirator facepiece to drive air through the filter material. If there are any breaks in the face seal, contaminated air will tend to pass through these openings, bypassing the filter material. Facial hair, large scars, and other facial irregularities may prevent a tight seal, and no respirators are approved for use by children. Fit testing is generally not available for members of the general public. A poorly fitted respirator may provide little more than a false sense of protection.
Respirators place additional burdens on the wearer. They increase the work of breathing and create a dead space under the facepiece, contributing to discomfort and potentially to heat stress (14). Although a few studies have indicated that respirators may prevent increased blood pressure associated with short-term exposure to urban PM (15), other studies have suggested that respirator use itself may cause acute increases in blood pressure (16). Due to the potential adverse respiratory and cardiovascular effects of respirator use, the Occupational Safety and Health Administration requires medical clearance for occupational respirator use. The evidence basis for medical clearance for use of respirators among workers is limited (17), and there are no guidelines for clearing members of the general public. Moreover, individuals with respiratory and cardiovascular disease who may benefit most from reductions in exposure to wildfire PM are also likely to be those most at risk of adverse health effects from wearing respirators. For these reasons, respirators for control of exposure to wildfire PM are generally recommended only for short periods of unavoidable outdoor activity. Caution in the use of respirators is especially advised for individuals who may be vulnerable to the increases in cardiovascular and respiratory stress involved in use of tight-fitting, air-purifying, negative-pressure respirators.
Information Needs
Effective personal action to reduce risk from wildfire smoke requires knowledge of current or future anticipated levels of personal exposure in different microenvironments (outdoors, indoors, transportation, etc.). Sensory cues, such as visible haze, odor, and irritation, are not calibrated to provide sensitive, quantitative assessments of pollutant concentrations or attendant risk. Individuals can follow the Environmental Protection Agency’s AirNow website and Air Quality Index (18), or similar indices in other countries, for current and predicted ambient air quality effects of wildfires. Limitations of available air quality data for guiding personal actions to reduce exposure include error in estimating personal exposure from central site and satellite data combined with modeling. Rapid changes and fewer air monitors in nonurban areas increase this error in locations where fires are more prevalent. To address these challenges, low-cost sensors that can be widely deployed for assessing personal or community-level air pollution levels are in development (19). Low-cost, commercial air sensors that purport to measure PM with a diameter of less than 2.5 μm (PM2.5) are widely available, but their accuracy and reliability varies widely (20).
In wildfire-prone areas, individuals may benefit from increased awareness and proactive preparation, including plans to control exposure to wildfire smoke air pollution. Having portable or central air filtration and respirators on hand can ensure availability and ready access to these control measures when needed. Improvements in indoor air quality from increased filtration of indoor air may have year-round benefits, depending on local air quality, other conditions in the home, and susceptibility of the occupants to PM-related health effects.
One thing is clear: more research is needed to understand the effectiveness of personal interventions to reduce exposure to air pollution and improve health outcomes related to episodic wildfire events, as well as longer-term poor air quality. Interventions, such as air filtration and respiratory protection, can be studied with controlled trials to evaluate both short-term and long-term health outcomes. Innovations in building science and respirators may improve these controls. In the meantime, cautious application of a hierarchical approach to exposure reduction should guide advice to patients and the general public regarding personal actions to reduce exposure to wildfire smoke and other episodic ambient air pollution events.
Supplementary Material
Footnotes
Supported by National Institute of Environmental Health Sciences (NIEHS) P30 grant ES005022.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.et al. USGCRP. Impacts, risks, and adaptation in the United States. In: Reidmiller DR, Avery CW, Easterling DR, Kunkel KE, Lewis KLM, Maycock TK, editors; Fourth National Climate Assessment, Vol. 2. Washington, DC: U.S. Global Change Research Program; 2018. [Google Scholar]
- 2.Cascio W. Wildland fire smoke and human health. Sci Total Environ. 2018;624:586–595. doi: 10.1016/j.scitotenv.2017.12.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balmes JR. Where there’s wildfire, there’s smoke. N Engl J Med. 2018;378:881–883. doi: 10.1056/NEJMp1716846. [DOI] [PubMed] [Google Scholar]
- 4.Johnston FH, Henderson SB, Chen Y, Randerson JT, Marlier M, Defries RS, et al. Estimated global mortality attributable to smoke from landscape fires. Environ Health Perspect. 2012;120:695–701. doi: 10.1289/ehp.1104422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–1343. doi: 10.1289/ehp.1409277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu JC, Pereira G, Uhl SA, Bravo MA, Bell ML. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ Res. 2015;136:120–132. doi: 10.1016/j.envres.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thurston GD, Kipen H, Annesi-Maesano I, Balmes J, Brook RD, Cromar K, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J. 2017;49:1600419. doi: 10.1183/13993003.00419-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hooper LG, Kaufman JD. Ambient air pollution and clinical implications for susceptible populations. Ann Am Thorac Soc. 2018;15(suppl 2):S64–S68. doi: 10.1513/AnnalsATS.201707-574MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Willoughby M, Kipsaina C, Ferrah N, Blau S, Bugeja L, Ranson D, et al. Mortality in nursing homes following emergency evacuation: a systematic review. J Am Med Dir Assoc. 2017;18:664–670. doi: 10.1016/j.jamda.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 10.Giorgini P, Rubenfire M, Bard RL, Jackson EA, Ferri C, Brook RD. Air pollution and exercise: a review of the cardiovascular implications for health care professionals. J Cardiopulm Rehabil Prev. 2016;36:84–95. doi: 10.1097/HCR.0000000000000139. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Environmental Protection Agency. Residential air cleaners: a technical summary. EPA Indoor Environments Division. EPA 402-F-09-002. 2018 Jul [accessed 2018 Dec 16]. Available from: https://www.epa.gov/sites/production/files/2018-07/documents/residential_air_cleaners_-_a_technical_summary_3rd_edition.pdf.
- 12.US Environmental Protection Agency, US Forest Service, US Centers for Disease Control and Prevention, California Air Resources Board. Wildfire smoke: a guide for public health professionals. 2016 May [accessed 2018 Dec 16]. Available from: https://www3.epa.gov/airnow/wildfire_may2016.pdf.
- 13.Preventing Illness and Injury in the Workplace. Washington, DC: U.S. Congress, Office of Technology Assessment, OTA-H-256. 1985 Apr [accessed 2018 Dec 16]. Available from: http://govinfo.library.unt.edu/ota/ota_4/data/1985/8519.pdf.
- 14.Johnson AT. Respirator masks protect health but impact performance: a review. J Biol Eng. 2016;10:4. doi: 10.1186/s13036-016-0025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langrish JP, Mills NL, Chan JK, Leseman DL, Aitken RJ, Fokkens PH, et al. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009;6:8. doi: 10.1186/1743-8977-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones JG. The physiological cost of wearing a disposable respirator. Am Ind Hyg Assoc J. 1991;52:219–225. doi: 10.1080/15298669191364631. [DOI] [PubMed] [Google Scholar]
- 17.Belafsky S, Vlach J, McCurdy SA. Cardiopulmonary fitness and respirator clearance: an update. J Occup Environ Hyg. 2013;10:277–285. doi: 10.1080/15459624.2013.774631. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Environmental Protection Agency. AirNow. [Updated 2019 May 17; accessed 2018 Dec 16]. Available from: https://airnow.gov/ [PubMed]
- 19.US Environmental Protection Agency. Evaluating low-cost air sensors performance near wildfires. 2018 Nov 1 [accessed 2019 Jan 19]. Available from: https://www.epa.gov/sciencematters/evaluating-low-cost-air-sensor-performance-near-wildfires.
- 20.Castell N, Dauge FR, Schneider P, Vogt M, Lerner U, Fishbain B, et al. Can commercial low-cost sensor platforms contribute to air quality monitoring and exposure estimates? Environ Int. 2017;99:293–302. doi: 10.1016/j.envint.2016.12.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.