Abstract
Rhythmic oscillatory patterns sustain cellular dynamics, driving the concerted action of regulatory molecules, microtubules, and molecular motors. We describe cellular microtubules as oscillators capable of synchronization and swarming, generating mechanical and electric patterns that impact biomolecular recognition. We consider the biological relevance of seeing the inside of cells populated by a network of molecules that behave as bioelectronic circuits and chromophores. We discuss the novel perspectives disclosed by mechanobiology, bioelectromagnetism, and photobiomodulation, both in term of fundamental basic science and in light of the biomedical implication of using physical energies to govern (stem) cell fate. We focus on the feasibility of exploiting atomic force microscopy and hyperspectral imaging to detect signatures of nanomotions and electromagnetic radiation (light), respectively, generated by the stem cells across the specification of their multilineage repertoire. The chance is reported of using these signatures and the diffusive features of physical waves to direct specifically the differentiation program of stem cells in situ, where they already are resident in all the tissues of the human body. We discuss how this strategy may pave the way to a regenerative and precision medicine without the needs for (stem) cell or tissue transplantation. We describe a novel paradigm based upon boosting our inherent ability for self-healing.
Keywords: Stem cells, Physical energies, Mechanical forces, Electric fields, Electromagnetic fields, Electromagnetic radiation, Photobiomodulation, Damaged tissues
Core tip: Rhythmic oscillatory patterns permeate the entire universe and sustain cellular dynamics. Our cells encompass a seemingly infinity of rhythms, unfolding at the nanomechanical and electric level in the microtubular network. Essential signaling molecules are shown to behave as chromophores, supporting the absorbance and emission of light. Photobiomodulation is a rapidly growing area of inquiry for both deciphering novel signaling mechanisms and affording unprecedented clinical applications. The deployment of the diffusive features of physical energies is leading to a regenerative/precision medicine, based upon the reprogramming in situ of tissue-resident stem cells, without the needs for cell or tissue transplantation.
INTRODUCTION
We are immersed in and we are a part of the oscillatory nature of the universe. In today’s physical age, on the threshold of the 4th Industrial revolution, most basic issues will be about electronics, machines, and the future of what we call artificial intelligence (AI). Science is increasingly looking at cell biology with the eyes of physics and electronics, providing compelling evidence that life is embedded within oscillatory patterns that create coherent rhythms, now recordable at cellular, subcellular, and even molecular levels. In addition to expressing rhythmically their molecular dynamics, cells are able to organize their decisions and fate by detecting and deploying the physical energies that permeate nature, including extremely weak mechanical vibrations (nanomotions), magnetic fields, and electromagnetic radiations (light).
As in the universe, in biological organisms, rhythmic oscillations and syn-chronization of oscillatory patterns are an essential requisite for recognition and connectedness. Sophisticated approaches, including atomic force microscopy (AFM)[1-4], scanning tunneling microscopy (STM)[5,6], terahertz field microscopy (TFM)[7], and hyperspectral imaging (HSI)[8-10] are now providing a dynamic picture of the cellular environment at a nanoscale level, showing that mobile elements of the cyto- and nucleo-skeleton are dancing with patterns that display features of coherence, short- and long-range signal propagation, networking, and memory. Tubulin dimers, and microtubules are now emerging as the constituents of a highly dynamic web, acting both as a source for the generation and the context for the interplay of physical energies[5,6]. These energies include mechanical forces[11-13] as well as the production of electric and very likely electromagnetic fields, with radiation characteristics[5,6,14], and even the occurrence of electromagnetic radiation (light), as a result of biophysical dynamics of a number of molecules increasingly regarded as chromophores[15-17]. To this end, the list of intracellular chromophores is now progressively increasing, including flavins, flavoproteins, and cytochromes[18-22], which are thought to be involved in the generation of reactive oxygen species (ROS) and nitric oxide[19,23-25], behaving as major pleiotropic conductors in cell biology.
Although it is not clear to what extent chromophores are expressed in mammalian cells compared to insects, there is now evidence for the presence of different members of the opsin (a group of cis-retinal dependent G-protein coupled receptors) family in mammalian cells, controlling crucial downstream signaling pathways involving members of the family of transient receptor potential cation channels (TRPs)[26-28]. TRPs are a superfamily of multiple members, which have been shown to be selectively activated by defined wavelengths of light, playing a major role in cellular dy-namics[29-33], as photoentrainment and modulation of cellular circadian rhythms[34].
These new achievements in science pose the more general issue of how and to what extent signaling molecules may be viewed as both generators and sensors of physical energies. They also highlight the particular relevance of the identification of frequency region selectivities for inducing defined morphological and functional paths, by precisely tuning the delivery at the cellular or tissue level of specific patterns/ signatures of frequencies, wave forms, and pause intervals for each energy alone (mechanical, electric-electromagnetic or light) or in combinatorial modes.
Within such a dynamic landscape, signaling molecules, like small peptides, based upon their intrinsic helix-turn-helix repeated modules, may be viewed as oscillatory entities[7], walking onto microtubular and microfilament routes in close association with molecular motors[35]. The cellular environment acquires notation of an intracellular niche whose characteristics are forcing Scientists to revisit their knowledge and interpretation of crucial issues that include the biomolecular recognition patterning, the inherent meaning and implication of cell polarity, the modalities through which cellular information is built and unfolded, and the determination of complex cellular decisions and fates. Accordingly, the use of innovative approaches, such as the Resonant Recognition Model (RRM), has led to the conclusion that DNA can also be viewed as an oscillatory entity resonating with electromagnetic frequencies spanning from THz to KHz[36]. RRM relies upon the finding that the function of proteins may be controlled by periodic distribution in the energy of their delocalized electrons, affecting protein dynamics, or protein-DNA interplay, a fundamental step in DNA remodeling and epigenetic control operated by a wide variety of transcription factors[37]. To this end, RRM also postulated that protein conductivity could be associated with defined spectral signatures, resulting from electromagnetic radiation/absorption patterns generated by the flow of electric charges through the protein backbone[37,38]. Interestingly, spectral signatures postulated on the basis of RRM have been verified and supported by experimental evidence[5,39]. Another advantage in the use of RRM is the chance of excogitating novel peptides with unprecedented spectral features and bioactivities[40].
The overall scenario is emerging of an intracellular environment where complex nanoarchitectonics are fashioned within a dynamic assembly of microtubules and microfilaments. These elements can now be regarded as a bioelectronic circuit embedding a multitude of signaling molecules that, besides interacting only with lock-and-key modalities, may also behave as actuators capable of generating phase coherent oscillatory patterns where the building blocks of information arise from the facilitation or dumping of the transfer of physical forces.
Here, we will discuss these issues with particular regard to stem cell biology and the use of physical energies to control stem cell decisions and afford somatic cell reprogramming. We will highlight the relevance of mechanobiology, and the possibility to use mechanical waves to elicit self-repairing mechanisms and tissue rescue in a number of pathological conditions. We will describe the effectiveness of radioelectric fields in enhancing the differentiating potential of stem cells, even reversing their senescence patterning. We will address the various facets of using electromagnetic radiation (light) of defined wavelengths to orchestrate selectively stem cell commitment and tissue repair. We will describe the innovative use of AFM and HSI to decipher the cellular emission of vibrational patterns, in terms of mechanical vibration (AFM) or electromagnetic radiation (HSI), corresponding to specific signatures of growth regulatory and differentiation processes. We will highlight the potential for exploiting the diffusive features of these energies and convey vibrational signatures in the form of nanomechanical motions and/or light patterns to the stem cells in situ to afford their reprogramming where they already are, resident in all tissues of the human body. We will finally discuss how this strategy will involve the development of novel interfaces between the human body and machines, as well as AI, paving the way to a precision regenerative medicine without the needs for (stem) cell or tissue transplantation, a novel paradigm based upon boosting our inherent ability for self-healing.
CELLULAR MICROTUBULES: A NETWORK OF OSCILLATORS THAT SYNC AND SWARM
There is increasing evidence that cells and subcellular domains are mechanosensitive. Mechanobiology is a growing area of interest that deals with the mechanical processes in biological systems. It ranges from cellular mechanics to molecular motors and single molecule binding forces. In addition to tuning the stiffness and shape of cell scaffolding and substrates, mechanical cues and mechanosensitivity are attracting much attention as they represent the context for sensing a wide variety of different stimuli, including osmotic changes, gravity, electromagnetic fields, (nano) motions falling both in an audible range (sound), or even fashioned at subsonic or ultrasonic levels.
The frequency-dependent transport of mechanical stimuli by single microtubules and small networks has been recently studied in a bottom-up approach, using optically trapped beads as anchor points[41]. When microtubules were interconnected to linear and triangular geometries to perform microrheology by defined oscillations of the beads relative to each other, a substantial stiffening of single filaments was detected above a characteristic transition frequency of 1-30 Hz, depending upon the molecular composition of the filament itself[41]. Below such frequency range, filament elasticity was only controlled by its contour and length persistence. This elastic pattern showed networking features, with the longitudinal momentum being facilitated through linear microtubular constructs in vitro, while the lateral mo-mentum was dumped so that the linear construct behaved as a transistor-like, angle dependent momentum filter[41]. These in vitro experiments also showed that the overall geometry of the microtubular network was a remarkable cue, since closing the construct circuitry by imposing a triangular shape resulted in stabilization of the microtubular elements in term of the overall molecular architecture and direction of oscillation. These findings suggest that within intact cells microtubular dynamics may afford generation and fine tuning of mechanical signals with a stronger degree of force generation and/or filtering and more flexibly than expected[41]. The complexity in the deformation pattern of microtubules is now prompting further studies to unravel their mechanics through sophisticated atomistic approaches[42].
A major feature of microtubular networks is their ability to exhibit synchronization patterns and even manifest a collective behavior. Synchronization may be viewed as a form of self-organization that occurs in multiple natural and technological systems, from spontaneously excitable cells, like pacemaker cells and neural cells, to coupled lasers, metallic rods, or even robots. On a molecular scale, the observation that simple mixtures of microtubules, kinesin clusters, and a bundling agent assemble into structures that produce spontaneous oscillations, suggests that self-organized beating may be a generic feature of internally driven bundles[43]. These synthetic cilia-like structures exhibit self-assembling at high density, leading to synchronization and metachronal traveling waves, reminiscent of the waves seen in biological ciliary fields[43]. From governing motility in simple protists to establishing the handedness of complex vertebrates, highly conserved eukaryotic cilia and flagella are essential for the reproduction and survival of many biological organisms. Likewise, the emergence of synchronization patterns in eukaryotic microtubules may be essential in the generation and spreading of nanomechanical and electric signaling orchestrated by these nanowires. Despite the fact that synchronization of oscillatory patterns appears to result from intrinsic properties of microtubules under critical, timely/spatial bundling conditions, the intimate mechanism by which individual components coordinate their activity to produce synchronized oscillatory patterns remains unknown.
Another form of self-organization is swarming insects, flocking birds, or schooling fish, where individuals also move through space exhibiting a collective behavior without remarkably changing their internal state(s)[44]. In their pioneer work, Sumino et al[45] have shown that an artificial system of microtubules propelled by dynein motor proteins self-organizes into a pattern of whirling rings. They found that colliding microtubules align with each other with high probability. As a function of increasing microtubular density, the alignment ensued in self-organization of microtubules into vortices of defined diameters, inside which microtubules were observed to move in both clockwise and anticlockwise fashion[45]. Besides exhibiting these spatial traits, the phenomenon also evolved on timely bases, since over time the vortices coalesced into a lattice structure. The emergence of these structures appeared to be the result of smooth, reptation-like motion of single microtubules in combination with local interactions (collision dependent nematic alignment)[45]. These discoveries have put forward the issue of previously unsuspected universality classes of collective motion phenomena that are mirrored even at the subcellular level, where microtubules have shown the capability, at least in vitro, to behave as swarming oscillatory elements, whose phase dynamics and spatial/temporal dynamics are coupled.
The possibility that microtubules may not only generate and propagate mechanical signals but that they may also be implicated in electric signaling acting as biological nanowires is suggested by the fact that tubulin has a large dipole moment. As a result, microtubules will exhibit a large cumulative dipole moment, imparting features of electrostatic polarity and functional directionality[46]. Within the microtubules, tubulin dimers have highly electronegative C-termini, attracting electrically positive counterions, a mechanism that may account for the observed amplification of ionic signaling[47-49]. These hypotheses have received significant support from the observation that microtubules were able to modify remarkably the electric conductance in solutions with varying concentrations of microtubules made by different concentrations of tubulin and tubulin dimers at a frequency range of alternating electric fields between 1 kHz and 10 MHz[46]. A consistent increase in solution conductance was observed at an alternating current frequency of 100 kHz, this effect being directly proportional to the concentration of microtubules in solution. Like mechano-transduction, the alternating current frequency dependent response of microtubules-containing electrolytes was also finely regulated, exhibiting a concentration independent peak in the conductance spectrum at 111 kHz, an observation that suggests the presence of intrinsic electric signaling properties of microtubules in aqueous environments[46]. Intriguingly, these properties did not result from conductance patterns elicited by their building blocks, since tubulin dimers exhibited a completely different behavior by decreasing solution conductance at 100 kHz under similar conditions[46].
The microtubular wall is interspersed by nanopores formed by the lateral arrangement of tubulin dimers. The application of patch clamp technique to in vitro generated two-dimensional microtubular sheets revealed that voltage-clamped sheets generated cation-selective oscillatory electrical currents whose magnitude depended on the holding potential, ionic strength, and composition[50]. The oscillations progressed through various modes including single and double periodic regimes and more complex behaviors with prominent fundamental frequencies. In physiological potassium concentrations, oscillations represented remarkable changes in conductance that were also affected by the prevalent anion[50]. Current injection elicited voltage oscillations, showing excitability similar to action potentials[50], suggesting a functional role of wall nanopores in the handling of the electrodynamic capabilities of microtubules.
Microtubules have also been shown to form bundles, particularly in neurons. Intriguingly, bundles of brain microtubules have been recently reported to behave as bio-electrochemical transistors that form nonlinear electrical transmission lines[51]. These bundles were shown to generate electrical oscillations and bursts of electrical activity similar to action potentials[51], indicating that electrical oscillatory patterns represent an inherent microtubular feature. These findings may have remarkable biomedical implications in the unfolding of both neuronal and non-neuronal functions. These may include the fine tuning of cytoskeleton-regulated ion channels and may even play a role in higher brain functions, including memory and cons-ciousness.
The biomedical implications of considering the microtubular network as a bioelectronic circuit are further inferred by other observations showing that exposure to alternating electric fields between 100–300 kHz of strength approximately 1.0–2.5 V/cm is able to arrest cell mitosis[52]. This finding has led to a Food and Drug Administration approved treatment for glioblastoma multiforme[53], with the electric field effects on microtubules being considered as the main underlying mechanism of action[52,54,55]. This clinical outcome prompts strong motivation to pursue additional studies aimed at further elucidating the electric signaling features of mammalian microtubules. For this purpose, contributions due to the dipole moments, charges, van der Waals, and solvation energy have been taken into account to dissect and explain microtubular energy balance[56], and optomechanical approaches have been proposed for monitoring microtubule vibration patterns[57]. Moreover, alterations of collective terahertz oscillations have been found to be induced in tubulin by anesthetics, correlating with their clinical potency[58]. This observation may have implications for anesthetic action and post-operative cognitive dysfunction.
There is now evidence that resonance modes not only occur in microtubules at the (nano) mechanical level but can even be detected at the level of their electric conductivity. Even more intriguingly, mechanical and electromagnetic resonance modes can coexist and affect each other within the microtubular network. STM, coupled with an ad-hoc designed cell replica developed to deliver electromagnetic fields of defined frequencies to microtubules growing on platinum nanoelectrodes, has shown that tubulins, tubulin dimers, and microtubules exhibited electric conductivity profiles resonating only with specific electromagnetic frequencies applied to the in vitro system[5]. STM analysis also provided evidence that the resonant tunneling currents elicited by microtubules occurred in response to electromagnetic fields applied within a MHz range[5].
These findings indicate that microtubules can generate specific electromechanical oscillations as a consequence of a resonant response to defined electromagnetic frequencies produced or delivered within their environment[5]. These observations further support the idea that microtubules may act as an intracellular bioelectronic circuit. Consonant with such perspective are (A) theoretical calculations considering the microtubules as elements generating electric fields of high frequency and radiation features[14]; and (B) experimental assays demonstrating that even a single brain microtubule behaves as a nanowire harboring “memory states” depending on its protein arrangement symmetry, coupled with conductivity state embedded in the microtubule itself, equitable to a memory switch device with a near-to-zero hysteresis loss[59] (Figure 1).
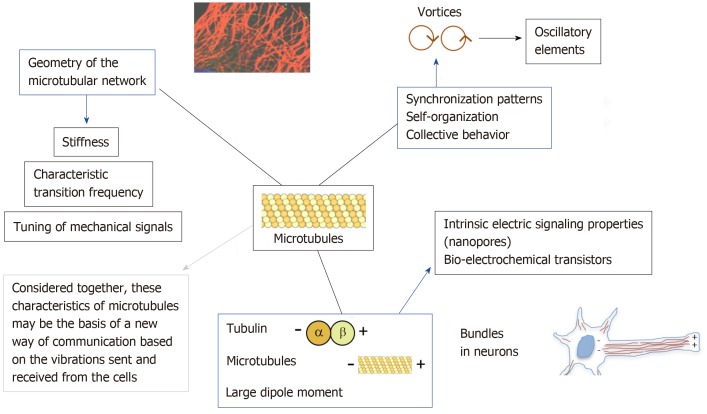
Figure 1.
Cellular microtubules: A network of oscillators that sync and swarm. Microtubules are emerging as major players in crucial cellular activities, on the basis of a number of interrelated characteristics. These include: (A) The transfer of mechanical waves, changing their stiffness, and the transmission of longitudinal and lateral momentum on the basis of the frequency of their oscillation and the geometry afforded by their timely 3D assembly and disassembly within the cells; (B) The onset and propagation of electric fields and signaling, depending upon the large dipole moment of tubulin, developing both electrostatic polarity and functional directionality, and upon the lateral arrangement of tubulin dimers to create nanopores, interspersing the microtubular wall, and generating cation-selective oscillatory electrical currents; (C) The generation of bundles, as shown in brain microtubules, behaving as bio-electrochemical transistors forming nonlinear electrical transmission lines; (D) The ability to resonate mechanically in the presence of electromagnetic fields of defined frequencies, retaining memory states coupled with conductivity states, like a memory switch device; and (E) The property of synchronizing their oscillatory pattern and swarming into vortices, affecting the vibrational features of signaling peptides moving across the microtubular network by the aid of molecular motor machines, thus modulating biomolecular recognition patterning.
BIOMOLECULAR RECOGNITION PATTERNING
The microtubular network and its sync and swarming behavior may help develop a novel hypothesis on biomolecular recognition within the intracellular environment. The “key-and-lock” dynamics, while fitting the description for the interaction of few molecules in aqueous solutions, fails to adequately describe and predict the collective behavior of a high number of different signaling players that cohabit the intracellular environment and share overlaying space and time domains of interaction to afford integrated cellular decisions. In addition, the time needed for cellular proteins to create productive interaction through intracellular diffusion mechanisms would be highly unpredictable on large-scale colliding bases. The high speed and fine coordination of molecular interplay within complex cellular decisions, including stem cell differentiation, cannot be solely explained on the basis of molecular diffusion and collision within the intracellular environment. At this level, a diffusive mechanism would become hampered and highly unpredictable, due to the synthesis and accumulation of a wide variety of glycosaminoglycans, such as hyaluronan, imparting the features of an aqueous gel dynamically modifying its composition and diffusive properties in response to cell metabolism.
The growing discernment of a microtubular role in tuning intracellular and intercellular communication may offer a clue to formulate novel hypotheses on the mechanisms underlying the astounding speed at which cellular fate is devised. The vast majority of signaling proteins exhibit helix-turn-helix modules, where the helices can be reckoned as oscillating springs, and the turns can be viewed as inter-oscillator linkers. A single peptide becomes a vibrational element capable of phase-resonant oscillatory patterns[7]. TFM has been exploited to detect protein vibrations, midget motions essential for Life[7]. These observations suggest that, like violin strings or pipes of an organ, proteins can vibrate in different patterns within our cells[7]. Cell proteins not only diffuse through water, but they can “walk” onto microtubular tracks availing of kinesins and dyneins motors as their molecular machines[35]. Signaling peptides can be therefore regarded as a multitude of oscillatory devices using molecular machines to move along the microtubular net, with the microtubules acting themselves as multi-level connections affording efficient phase synchronization between multiple oscillators.
The resonant behavior described in microtubules[5] holds promise for remarkable impact in further elucidation of biomolecular recognition patterning. The chance of using a selective frequency region to induce defined morphological patterns in microtubules has shown that mechanical patterns can be precisely orchestrated through the remote application of electromagnetic fields[5]. Therefore, the finding that local density states in tubulin dimers, microtubules, and possibly other proteins can be modified by changing the frequency of their electromagnetic exposure entails that unfurling of protein structure into rhythmic resonance patterns may result as a relevant inherent mechanism sustaining both intracellular, and intercellular communication. Dissecting the resonance patterns intervening within clusters of signaling molecules, and between such molecules and the microtubular networks, and providing suitable methods to investigate the establishment of collective behavior among oscillators that undergo both sync and swarming will likely represent a novel paradigm for investigating the onset and spread of informational processes in biological systems.
Despite continuous progress in investigating this complex matter, the intimate origin of the observed resonant behavior remains largely elusive, particularly if the correspondence between electromagnetic and mechanical oscillation assessed in vitro is translated into an in vivo setting.
During electromagnetic exposure of protein and protein complexes, in case of electromagnetic resonance, photons would be expected to find domains in the protein structure amenable for both electric and magnetic absorption. Protein cavities would appear as domains arranged for the interaction of the electric and magnetic components of an incoming electromagnetic field. Although nanotopography within these cavities may be suitable for electric resonance, the issue as to whether these cavities may act as sensors generating resonances in the presence of an electro-magnetic field remains an open and difficult to answer question.
A remarkable challenge is represented by the fact that, different from simplified in vitro systems, the intact cellular level electromagnetic and nanomechanical oscillations are supposed to be highly interconnected with none of their resonance-elicited responses separately emerging as electrical, magnetic, or mechanical. Within this context, a significant step forward may be provided by the recent invention of an atomic resolution scanning dielectric microscopy capable of seeing a single protein complex operating live at resonance in a single neuron without touching or adu-lterating the cell[6].
Overall, while our view of intracellular and intercellular connectedness is dra-matically evolving over time, a novel paradigm is emerging, which considers the cellular and subcellular structures as senders and receivers of electromagnetic and nanomechanical fields. Unfolding this new paradigm may lead to the use of physical energies to orchestrate complex cellular decisions. Translating this perspective at the level of stem cells would result in unprecedented implication in precision rege-nerative medicine, as discussed below.
PHYSICAL ENERGIES TO THE RESCUE OF DAMAGED TISSUES: CAN TISSUE RESIDENT STEM CELLS BE A TARGET?
Targeting stem cells with mechanical vibrations
Mechanical signals minutely travel inside and across our cells, with our molecular players and the cyto-nucleo-skeleton behaving as sender and receiver of patterns manifesting with different frequencies, wave form and intensity, as well as pause intervals that are also essential in shaping the ensuing cellular responses. Complexity of biological systems is now emerging through a new landscape made of symmetry breaking, switching among various oscillatory patterns, synchronization of oscillators into clusters, and the swarming of oscillatory clusters that exhibit a collective behavior without necessarily altering their internal states. These dynamics are deeply inbred in a wide variety of cellular nanomotions, including those in the mitotic spindle, the bidirectional organelle transport, and the trafficking of molecular motors and signaling molecules. Within this environment, shaping of mechanical signaling has the advantage of bridging nanomotions with the generation and transfer of information processes across long distances in short time frameworks.
Can this growing body of knowledge be translated into a biomedical application? A positive answer came from the pioneer studies of Rubin et al[60], showing that low-level mechanical stimuli could be delivered to afford strengthening and normalization of anabolic activity in long bones[60-62]. These authors showed that brief daily treatments with mechanical vibrations of high-frequency and very low magnitude could inhibit adipogenesis, while promoting osteogenesis in vivo[63] as well as in isolated human stem cells in vitro[64,65], up to the point of maintaining the osteogenic potential in bone marrow stem cells, and advancing trabecular bone formation during reambulation[66]. Mechanical vibrations can also be deployed to modulate nuclear signaling and afford significant transcriptional responses. In this regard, an important role is played by the so-called “Linker between Nucleoskeleton and Cytoskeleton”, a mechanosensitive network of molecules implicated in chromatin remodeling and epigenetic modification upon nuclear transfer of extremely low-magnitude me-chanical signals[67-69]. Based upon consideration that an electromagnetic field may originate from the electrical polarity of microtubules that form the mitotic spindle, a model enabling calculation of such electromagnetic field coupled to acoustic vibrations of the mitotic spindle has been recently developed to describe mitotic spindle kinetics[70], still a poorly understood phenomenon of critical relevance in both physiological and pathological (i.e., cancer) states.
These findings clearly indicate that modulation of cell mechanosensitivity has relevant biomedical implication and may pave the route for developing novel approaches to stem cell biology and regenerative medicine.
Shock waves
Shock waves are mechanical pressure waves with defined wave profile used in clinical practice since more than 30 years[71]. Low-energy shock wave therapy (SWT) has been successfully used in vivo to treat problematic wound-healing distur-bances[72-74], tendinopathies, and non-healing bone fractures[75-77]. The ability of SWT to promote tissue regeneration has been initially ascribed to the activation of angiogenic pathways sustained in a paracrine fashion by local release of trophic mediators[78-81]. These findings have fostered extensive investigations to extend further the potential clinical contexts susceptible for SWT application and to elucidate the underlying mechanistic bases. The application of extracorporeal or epicardial shock waves to a porcine model of myocardial infarction has led to a significant improvement of vascularization with increased number of capillaries and arterioles at the infarct border zone, ameliorating ischemia-induced dysfunction and left ventricular function[82,83]. Subsequent studies in infarcted mice indicated that the ability of SWT to prevent left ventricular remodeling and failure through the induction of angiogenesis involved a complex circuitry, encompassing the mechanical stress-induced release of the antimicrobial peptide LL37, its ability to form complexes with nucleic acids, and the release of RNA/protein complexes converging to the activation of Toll-like 3 receptors[84].
The possibility that the angiogenic action of SWT may occur through stem mobilization from the bone marrow has been suggested in studies providing evidence that the beneficial effect of SWT in a hindlimb ischemia model was associated with the mobilization of endogenous endothelial progenitor cells into the systemic cir-culation[85,86]. Recent studies in an animal model of chronic myocardial ischemia, using wild-type mice receiving bone marrow transplantation from green fluorescent protein donor mice, demonstrated that besides local angiogenesis, cardiac SWT was also inducing the recruitment of bone marrow resident endothelial cells to the damaged myocardium[87]. This response was associated with enhanced expression of the chemoattractant stromal cell-derived factor 1 in the ischemic myocardium and serum. In vitro analyses revealed that the ability of SWT to induce endothelial cell proliferation, their enhanced survival, and capillary sprouting was dependent on both vascular endothelial growth factor (VEGF) 2 and heparan sulfate proteoglycan[87]. Besides affecting the release of stored VEGF reservoir bound to heparan sulfate proteoglycan, facilitating VEGF binding to its receptors, SWT has been shown to induce angiogenesis by acting at the transcriptional level, triggering the gene and protein expression of VEGF and endothelial nitric oxide synthase[88]. The tight dependence of these responses upon a mechano-sensing/transduction mechanism could be inferred by the finding that (A) SWT enhanced the phosphorylation of caveolin-1; (B) it increased the expression of HUTS-4, which represents β-1 integrin activity; and (C) knockdown of either caveolin-1 and β-1 integrin suppressed SWT induced enhancement of human umbilical vein endothelial cell migration in vitro[88].
These molecular findings can also be viewed as a reverse story - from the bed to the bench side - as they provide a mechanistic underpinning on a number of studies that were earlier conducted in patients with severe coronary artery disease, showing that SWT was able to ameliorate myocardial ischemia in patients with severe coronary artery disease[89]. Accordingly, a double-blind and placebo-controlled study demonstrated that SWT improved chest pain and myocardial function without any complication or side effects in patients with severe angina, leading to the conclusion that SWT was an effective, safe, and non-invasive option for these patients[90]. Following these initial clinical studies, the molecular dissection of mechano-transduction and signaling patterning primed by SWT served as a driving force for further expanding the clinical application of SWT. In a human study, low-energy cardiac SWT was found to suppress left ventricular remodeling and enhance myocardial function in patients with acute myocardial infarction, suggesting that extracorporeal SWT may represent a safe, effective adjunctive therapy to primary percutaneous coronary intervention[91].
A remarkable perspective for using SWT in regenerative medicine approaches is now emerging from an increasing variety of studies conducted in vitro in isolated stem cells as well as in animal models of tissue damage. Evidence includes the ability of SWT to promote the osteogenic differentiation in adipose- and bone marrow-derived mesenchymal stem cells[92-94] and the proliferation and migration of rat adipose derived stem cells[95]. Shock wave treatment induced ATP release, increased Erk1/2 and p38 MAPK activation, and enhanced proliferation in vitro in different stem cell types, including C3H10T1/2 murine mesenchymal progenitor cells and primary human adipose tissue-derived stem cells (hADSCs)[81]. Purinergic signaling-induced Erk1/2 activation was found to be essential for the proliferative effect of shock waves, which was further confirmed by in vivo studies in a rat wound healing model, where shock wave treatment induced proliferation and increased wound healing in an Erk1/2-dependent fashion[81]. Interestingly, converging genetic and molecular evidence has been provided that the miR-138-FAK-ERK1/2-RUNX2 machinery can be generally activated by extracorporeal SWT in tendon-derived and adipose derived stem cells, promoting efficient osteogenic differentiation irrespective of the stem cell origin[93]. In vivo, SWT promoted the induction of endogenous neural stem cells and functional improvement after spinal cord injury in rats[96]. Recruitment and induction of endogenous stem cells were also at the basis of the capability of SWT to ameliorate voiding function and improve the innervation and vascularization in a rat model of diabetic bladder dysfunction[97] (Table 1).
Table 1.
Low-energy shock wave therapy studies
| Low-energy shock wave therapy | Conditions | Biological effects | References number |
| In vivo studies | Wound-healing disturbances, tendinopathies, and non-healing bone fractures | Activation of angiogenic pathways with local release of trophic mediators | [72-77] |
| Myocardial infarction in animal models | Improvement of vascularization at the infarction border zone; Mobilization of endogenous progenitor cells from bone marrow into the systemic circulation and to the damaged myocardium; Increase in VEGF gene and protein expression with endothelial cell proliferation | [82-88] | |
| Human severe coronary artery disease or severe angina | Improvement of myocardial ischemia and chest pain | [89-90] | |
| Human acute myocardial infarction | Suppression of left ventricular remodeling and enhancement of myocardial function | [91] | |
| Spinal cord injury in rats | Induction of endogenous neural stem cells and functional improvement | [96] | |
| Diabetic bladder dysfunction in rat model | Improvement of voiding function; Enhancement of innervation and vascularization | [97] | |
| In vitro studies | Adipose- and bone marrow-derived mesenchymal stem cells | Induction of osteogenic differentiation | [92-94] |
| Murine adipose derived stem cells | Stem cell proliferation and migration in an Erk1/2-dependent fashion | [81,95] |
Exogenous stem cell transplantation is often hampered by the invasiveness of delivery in certain districts, such as the central or peripheral nervous system, and by other limitations that need to be addressed, including the ideal stem cell source, the timing and modality of delivery, and uncertain fate, especially after transplantation in complex tissues.
In this regard, SWT is emerging as a feasible, efficacious, non-invasive, safe, and cost-effective tool to elicit mechanical signaling and multiple interconnected downstream patterning that converge in optimization of the intrinsic potential of tissue rescue, through the activation of rapid release of trophic mediators, as well as the recruitment and induction of endogenous tissue resident and/or mobilized stem cells.
Cellular nanomotions: Vibrational signatures to direct stem cell fate
It is now clear that cytoskeletal and organelle biology is tightly coupled and that complex connections are dynamically featured at the level of cellular membranes, from the endoplasmic reticulum and the Golgi up to the plasma membranes. The rhythmic patterning and the unfolding of synchronization and swarming modes within the microtubular network are fast remodeling dynamics of the intracellular environment and behave as a vibrational system capable of force generation leading to rhythmic membrane movement.
The nanomechanical oscillatory features of subcellular structures, including the cellular membranes, govern essential biological processes in living cells, including, for example, organelle translocation, nanovescicular assembly and motion, as well as the trafficking and release/cellular exchange of signaling molecules[98]. AFM is based upon the use of a scanning probe that detects local mechanical features, nano-architectonics, and even thermal or electrical characteristics with a particular probe (tip) positioned very close to a target. The extremely close vicinity between the tip and the target sample allows conducting fine analyses even within a nanoscopic environment. The possibility to use AFM in an aqueous milieu makes this system suitable for characterizing living cells, or their subcellular components, with subnanometer resolution grades. These features have made possible to apply AFM to the analysis of cellular/subcellular nanomotions under physiologic conditions, sensing or conveying weak forces with extreme sensitivity[99].
In yeasts or bacteria, cell growth, morphogenesis, and metabolic activity are coupled with characteristic nanomotions that coalesce at the cell surface with defined vibrational blueprint[99]. To this end, a novel area of inquiry has been developed and referred to as “sonocytology”, which is based upon the initial observation that nanomechanical motions detected from these small cells could be transformed into audible sounds, following accurate amplification of AFM cantilever vibration, providing a thorough mechanistic analysis of cellular activity[99]. This approach can also be extended to the analysis of complex adaptive behavior in eukaryotic cells. For instance, in vitro cardiogenesis, the process of differentiation of stem cells into spontaneously beating cardiomyocytes, entails a major remodeling of the microtubular network, and overall of the cyto- nucleo-skeleton, which will be reflected in remarkable changes in nanomechanical patterning recordable at the level of cellular plasma membrane. In this regard, we have shown and patented for the first time the possibility of using atomic force microscopy (AFM) to afford a nano-mechanical characterization of cellular activity, detecting defined signatures corresponding to the cellular healthy or non-healthy status or to specific dif-ferentiating pathways[100]. In particular, we found that stem cells express nanomechanical patterns that can be harvested by AFM and processed into vibrational signatures of their commitment along defined lineages[100]. Our ongoing work is based upon the development of high-fidelity multifrequency mechanical transducers capable of conveying back such signatures to undifferentiated stem cells to direct their commitment towards specific fates. Differently from SWT, this strategy would allow orchestration of the differentiating potential of stem cells on the basis of specific nanomechanical codes, instead of relying upon non-specific, empirically designed, and high-intensity mechanical waveforms.
Electromagnetic fields
A significant biomedical deployment of the “nanoworld” described above is the chance of using physical energies to modulate cellular dynamics and fate. In this regard, we first provided evidence that extremely low-frequency pulsed magnetic fields acted on adult ventricular cardiomyocytes to induce the expression of endorphin genes and peptides[101], playing a major role in intracellular calcium[102] and pH[103] handling, in the regulation of myocardial growth[104-106] and the orchestration of stem cell cardiogenesis[107-109]. In mouse embryonic stem (ES) cells, extremely low-frequency pulsed magnetic fields induced the transcription of cardiogenic and cardiac specific genes and proteins, ensuing into a high-throughput of spontaneously beating cardiomyocytes[110].
We found that a radioelectric field of 2.4 GHz, the same frequency used in wireless fidelity technologies, can be conveyed in vitro to stem and somatic cells via an ad hoc designed radio electric asymmetric conveyer (REAC)[111]. Thanks to its probe, tissue or cell exposure to REAC induce local microcurrents that are attracted and conveyed back to the treated targets without depth limit[111]. The sum of these microcurrents elicited in the patient’s tissue target in vivo, or in isolated cells in vitro, are concentrated by the asymmetric conveyer-probe of the device, optimizing tissue or cellular bioelectrical activity[111]. This innovative approach proved effective in the modulation of stem cell biology at multiple intertwined layers, including the transcription of stemness genes, the expression of tissue-restricted genes and proteins, and the commitment or terminal differentiation along different lineages. In mouse ES cells[111], as well as hADSCs, REAC exposure optimized the expression of pluripotency and multipotency, respectively, and primed a consistent increase in the yield of stem cells committed along myocardial, skeletal muscle, and neuronal fates[111,112]. Interestingly, following REAC exposure, even human skin fibroblasts could be committed to the same lineages[113]. This observation shows the feasibility of directing human somatic cells to fates in which these cells would never spontaneously appear. This approach did not require methods that so far cannot be easily translated into a clinical practice, such as the use of lentiviral vectors for target gene delivery or the somatic cell reprogramming by cumbersome non-integrating technologies. In addition, REAC-mediated reprogramming of somatic cells involved a biphasic effect on the transcription of stemness genes - a rapid overexpression followed by a down regulation[113] - mimicking the embryogenetic patterning, where the onset of multi-lineage commitment follows, and requires, the transcriptional shutdown of these genes[114-117]. This observation not only may account for the relatively high yield of commitment observed in each lineage (about 10%-15% of the REAC exposed cell population was oriented towards cardiogenesis, skeletal myogenesis, or neu-rogenesis)[113], but it implies that the transcriptional inhibition of the stemness genes would avoid freezing of the REAC treated cells into an embryonic-like state, which may potentially evolve into malignant cells.
Another breakthrough coming from analysis of biological effects produced by REAC conveyed radioelectric fields was the observation that this treatment proved effective in reversing human stem cell senescence[118]. In fact, a significant decrease in the number of hADSCs expressing senescence-associated β-galactosidase, a marker of cellular senescence, could be observed following REAC exposure throughout long-term cell culture, extended up to the 30th passage[118]. At the 30th passage in culture, REAC-treated hADSCs showed a remarkable overexpression of the TERT gene, encoding the catalytic core of telomerase. This effect was paralleled by an increase in telomere length and telomerase activity, with complete restoration of the ability to differentiate along multiple lineages[118]. The antisenescence effect of REAC also involved the activation of a telomerase-independent route, as shown by the increase in the transcription of Bmi-1, a pleiotropic inducer of stemness genes and proteins, which, accordingly, were found to be upregulated even at the latest 30th passage in the exposed cells[118].
These observations may also be relevant at the biomedical level. It is now generally accepted that the progressive senescence of tissue resident stem cells across our life span may be responsible for the impairment in tissue self-healing potential. Moreover, from a cell therapy perspective, the strategy of prolonging stem cell culture to yield a high number of transplantable elements, involves the paradox of promoting cellular senescence, thus mocking the initial aim of the cellular expansion of increasing the change of post-transplant tissue recovery.
The “time machine” effect elicited by an electromagnetic energy on stem cell chronobiology may not only prompt innovative approaches for tissue rejuvenation, but it may provide the opportunity of affording (stem) cell expansion procedures without undesired senescence of the cultured cells.
In separate studies, we found that the antisenescence action of REAC was counteracted by 4-methylumbelliferone, a powerful inhibitor of type-2 hyaluronan synthase (HAS2)[119]. The main implication of this finding lies on the fundamental role of HA in maintaining cell polarity and on the possibility of using electromagnetic energy as a tool to optimize cell polarity at the stem cell level. The intracellular role of HA is highlighted by many interrelated observations: (A) The cardiovascular differentiation of ES cells is abrogated by suppression of HAS2[120]; (B) Embryogenesis itself is suppressed by HAS2 knockout due to lethal cardiovascular abnormalities[121]; (C) Intracellular HA acts as docking anchor for hyaluronan binding proteins (hyaladherins), mainly including protein kinases and tissue-restricted transcription factors, favoring targeted phosphorylation steps that are essential for transcriptional efficiency[121-123]; (D) Most of HA mediated interactions encompass molecular motors and are executed at the level of microtubules, providing a dynamic environment that sustains and directs cell polarity[124]; (E) Akin to its pleiotropic functions, HA has been used in the form of mixed ester of butyric and retinoic acids to induce a cardiogenic program of differentiation in mouse ES cells[125]; and (F) In human mesenchymal stem cells, in vitro, as well as in vivo models of myocardial infarction[126-128], even affording efficient myocardial repair in vivo without stem cell transplantation in infarcted rat hearts[129].
Compelling evidence relates impairment in cellular polarity to stem cell senescence, or the development of an oncogenic risk[124]. Senescent stem cells in Drosophila exhibited reduced self-renewal capability as a consequence of centrosome miso-rientation and altered cell polarity within their stem cell niche[124,130]. The relevance of preserving cell polarity in biological systems is further highlighted by the results of targeted mutation of tumor suppressor p53 in mammary stem cells, where symmetric division and oncogenesis develop in tight association with cell polarity loss[131].
Collectively, these observations point at maintenance of cell polarity as to an underlying attribute for an optimal health. The fact that the antisenescence effect of REAC treatment depended upon intracellular HA availability indicates that proper delivery of electromagnetic fields may represent a tool for optimizing cell polarity in cells and tissue. Such a possibility entails the perspective of conveying radioelectric fields to afford a “one component (cell polarity) - multiple target (stem cell pluripotency, reprogramming, and rejuvenation)” strategy of boosting our self-healing potential.
Deepening the interest for the use of electromagnetic energy in cell biology, the REAC approach also proved effective in inducing the neurological and mor-phofunctional differentiation of PC12 cells, a rat cell line of pheochromocytoma, retaining metabolic characteristics of Parkinson’s disease[132]. The REAC effect included the transcriptional up-regulation of neurogenin-1, β3-tubulin, and nerve growth factor, a set of neurogenic genes, and increased the number of both β3-tubulin and tyrosine hydroxylase expressing cells. The induction of a neurogenic phenotype was associated with the appearance of neuron-like cells[132]. Worthy to note, the differentiating effect of REAC was paralleled by a decrease in the number of PC12 tumor cells, while our previous studies showed no decrease in viability of normal human skin fibroblasts and hADSCs. On the whole, these observations suggest that the REAC treatment may be beneficial in the handling of Parkinson’s disease, and further studies are currently ongoing by our Group on this direction (Table 2).
Table 2.
Electromagnetic field studies
| Electromagnetic fields | Conditions | Biological effects | References number |
| Extremely low-frequency pulsed magnetic fields | Adult ventricular cardiomyocytes | Induction of the expression of endorphin genes and peptides; Control of intracellular calcium and pH homeostasis; Regulation of myocardial growth; Orchestration of stem cell cardiogenesis | [101-109] |
| Mouse embryonic stem (ES) cells | Induction of cardiogenesis, cardiac gene and protein expression, ensuing into a high-throughput of spontaneously beating cardiomyocytes | [110] | |
| Radioelectric field of 2.4 GHz (REAC) | Mouse ES cells, hADSCs and human skin fibroblasts | Optimization in the expression of pluripotency/multipotency; Increase in commitment along myocardial, skeletal muscle, and neuronal fates, with a biphasic effect on the transcription of stemness genes | [111-117] |
| hADSCs | Reduction of senescence-associated β-galactosidase expression; Overexpression of the TERT gene associated with an increase in telomerase activity; Overexpression of the BMI1 gene; REAC effects counteracted by chemical inhibition of type-2 hyaluronan synthase | [118-120] | |
| PC12 cells, a rat cell line of pheochromocytoma | Induction of the neurological and morphofunctional differentiation; Up-regulation of neurogenic genes; Decrease in PC12 cells | [132] |
ES cells: Embryonic stem cells; hADSCs: Human adipose tissue-derived stem cells; REAC: Radio electric asymmetric conveyer.
Photobiomodulation
The origin of the term Photobiomodulation (PBM), considered as the possibility of using light to afford modulation of biological processes and tissue healing in various pathological conditions, probably dates back to 1967, when the Hungarian scientist Endre Mester tried to replicate an experiment performed at that time by McGuff in Boston[133,134]. The latter had been using a beam from ruby laser to eliminate a tumor previously implanted in a rat. Mester was not aware that the system built for him was delivering a ruby laser of only a minimal fraction of power of the laser used by McGuff. As a result, Mester failed to affect the implanted tumor but, he came up with hair regrowth and wound healing at the site of the tumor implantation[135-138]. Initially referred to as “low level laser therapy (LLLT)”, this kind of approach was successfully applied over time to afford wound healing and counteract inflammation and pain in orthopedic diseases. Following the recent consensus that light-emitting diodes could successfully replace the use of coherent lasers, the term LLLT has been employed to identify generally a “low level light therapy”. Since 2015, the acronym LLLT has been replaced by the term PBM, based upon the difficulty of expressing “low level” as a defined quantity range.
The biological responses elicited by PBM raise the major question as to whether our cells may also use and process electromagnetic signals by themselves, instead of only sensing an exogenously applied electromagnetic radiation (light). A positive answer to this question came from the seminal discovery of Guenter Albrecht-Buehler in 1992, when he analyzed the cellular behavior of Baby hamster kidney cells inoculated sparsely on one face (s-face) and grown as a confluent layer on the opposite face (c-face) of the same thin glass film, using specially prepared substrates to make the confluent cells preferentially oriented and lined up along parallel stripes[139]. Albrecht-Buehler found that after 7 h and in the absence of visible light most of the cells on the s-face traversed with their long axes and with defined angles the direction of the whorls of the confluent cells on the opposed c-face[139]. This cell behavior was abolished by a thin metal coating, absorbing visible and infrared light across the range of wavelengths. On the contrary, the orienting pattern was maintained after coating of the s-face by a thin silicone coating of the glass, which strongly absorbed in the blue end of the visible spectrum but was transparent for red and infrared light[139]. These findings indicated that cells are capable of detecting the orientation of each other by the generation and processing of signals carried by electromagnetic radiation penetrating a thin glass but not a thin metallic film. Moreover, the results from these studies provided evidence that the wavelength of such radiation was likely in the red to infrared range. The author concluded that “the ability of cells to detect the direction of others by electromagnetic signals points to a rudimentary form of cellular “vision”[139]. Subsequent studies performed by Albrecht-Buehler were published in 2005, showing that near infrared light scattering in dynamic cells was exploited to afford long-range attraction in culture, even when cells were initially seeded in single non-aggregated elements and located randomly onto the tissue culture dish[140]. Nevertheless, cells were able to detect each other within a certain range and move together to form aggregates. In this study the author described a valid assay to calculate the value of range, which resulted to be much larger than one cell diameter and remarkably dependent upon the measured intensity of near-infrared light scattering produced by the cultured cells[140]. For the first time, this milestone study showed that “near-infrared light scattering by the cells mediate a long-range attraction between them, which does not require physical contact and enables them to detect each other’s presence”.
More than 20 years later, light has been conveyed in the form of PBM to afford wavelength-dependent selective regulation of differentiation and proliferation in hADSCs. In these stem cells, PBM with blue (420 nm) or green (540 nm) light was found to promote osteoblastic differentiation[141]. The effect was mediated at the transcriptional level, recruiting a gene program of osteogenesis, including RUNX2, osterix, and the osteoblast protein, osteocalcin. The 420 nm and 540 nm wavelengths were more effective in stimulating osteoblast differentiation compared to red or near infrared PBM[141]. Intracellular calcium was higher after exposure to light of 420 nm and 540 nm, an effect that could be inhibited by capsazepine (CPZ) and SKF96365 (SKF), which also inhibited osteogenic differentiation[141]. These effects were likely mediated by the activation of light-gated calcium ion channels, as it was inferred by the ability of both CPZ and SKF to suppress the hADSC response to blue or green light[141]. Members of the superfamily of TRPs channels appear to be the class of light-gated ion channels responsible for the differentiating action of blue and green PBM. Consistent with this view, TRPs are present in almost all known living forms[142]. In particular, the vanilloid TRP sub-class (TRPV) was identified as including the receptor TRPV1, specific for capsaicin[143]. TRPV1, exogenously expressed in Xenopus, has been shown to be activated by red and even to a greater extent by green light[144]. It is now evident that multiple TRPVs play a relevant role in many biological responses, including pain, inflammation, and regulation of pressure and heat[145]. Opsins are currently believed to represent the major group of intracellular light-sensitive proteins (chromophores) involved in selective photon absorption (especially blue and green photons) and subsequent activation of TRPs[146,147]. In particular, melanopsin, which relies upon 11-cis retinal isomerization (peaking at 479 nm), is potentially expressed in hADSCs and has been shown to form a pigment maximally sensitive to blue light (with a peak at 479 nm), supporting activation of G(q/11) and G(i/o) signaling cascades, ultimately promoting TRPs-mediate raise in intracellular calcium[22]. Melanopsin has also been targeted by therapeutic devices utilizing blue light to treat jet-lag, affective disorders, depression, and insomnia[148-150]. The fact that SKF, a non-selective TRP inhibitor, was more effective than the selective TRPV1 inhibitor CPZ in abrogating the effects of green and blue light on hADSC osteogenesis[141] suggests that TRPV1 may not be the only light-gated ion channel involved in the osteogenic patterning triggered by blue or green PBM in hADSCs.
Further compounding the complexity and selectivity of PBM in stem cell biology is the finding that red (660 nm) or near-infrared (810 nm) light was able to stimulate, while PBM with blue (415 nm) or green (540 nm) light was found to inhibit the proliferation of hADSCs[151]. In these experiments, PBM with blue/green light produced a CPZ-inhibitable increase in intracellular calcium, and in the amount of ROS, while red/near-infrared light produced a comparable lower increase in intracellular calcium and ROS levels[151]. Moreover, the slight raise in intracellular calcium elicited by red/near-infrared PBM could not be blocked by CPZ. At the same dose of irradiation (3 J/cm2), blue/green light decreased cellular ATP, lowering both mitochondrial membrane potential and intracellular pH, which may account for a significant increase in ROS, while red/near-infrared PBM had the opposite effect[151]. In the same study, the possibility that the blue/green light may have decreased hADSC proliferation by activating TRPV1 ion channel and increasing calcium and ROS was inferred by the observation that TRPV1 was expressed in hADSCs, and CPZ itself, as well as the antioxidant N-acetylcysteine, abolished the inhibition of proliferation induced by blue/green PBM. These findings also highlighted the subtle differences between the effects produced by blue and green PBM, being their action superimposable in reducing hADSC proliferation and intracellular ATP, while the blue light triggered a more pronounced increase in ROS and drop in mitochondrial membrane potential, as compared with green PBM[151]. It was hypothesized that different sensitivities of mitochondrial chromophores may at least account for these differential responses, with red/near-infrared light conversely increasing intracellular ATP and only inducing low levels of ROS.
Taken together, these findings point at the possibility of deploying the diffusive features of PBM to afford a fine tuning of stem cell dynamics and suggest that the ability of PBM to promote tissue repair previously observed in vivo may have involved in situ reprogramming of tissue-resident stem cells.
Various forms of PBM have been proved effective in ameliorating the outcome of acute stroke in both animal models[152-157] and humans. In a number of, although not all, controlled clinical trials enrolling patients with ischemic stroke associated with measurable neurological defects, 810 nm laser light conveyed to shaved head induced a significant and long-lasting neurological improvement, especially for patients with moderate and moderate-to-severe stroke[158-160].
Application of near-infrared light in animal models of traumatic brain injury (TBI) has been consistently shown to rescue neurological performance and reduce the size of brain lesions in different research laboratories[161,162]. In some studies, the favorable effect of PBM was selectively induced at defined wavelengths, with 665 nm and 810 nm proving the most effective, and with lack of improvement at 730 nm and 980 nm[162]. Based upon this window of selectivity, the chromophore cytochrome c oxidase has been proposed as the putative target responsible for the observed tissue repair[163]. These results were further confirmed in TBI animal models subjected to PBM with either pulsed or continuous wave lasers, with the group treated with 10 Hz pulsed waves exhibiting the most pronounced improvement[164]. The link between these findings and the observed in vitro action of PBM on stem cell dynamics is supported by the finding that PBM was found to increase neuroprogenitor cells in mouse dentate gyrus and subventricular zone[165], along with an increase in brain derived neu-rotrophic factor after 7 d of treatment, followed by a later increase in synapsin-1, underlying a significant enhancement in synaptogenesis and neuroplasticity[166]. Also, learning memory was increased in both mouse and rat models of TBI[167]. These beneficial outcomes were further improved by the combinatorial delivery of PBM and metabolic substrates, including pyruvate and lactate, which were supposed to ameliorate the mitochondrial function[168]. Clinical trials, although still performed in a limited number of patients with TBI, appear to confirm in human subjects the results initially yielded in experimental animal models, as it has been indicated by post-treatment improvement of both language[169] and cognitive performance[170] as well as brain tissue recovery, as assessed by anatomical magnetic resonance imaging and perfusion single-photon emission computed chromatography[171].
Another major field of potential clinical application of PBM deals with the treatment of neurodegenerative diseases. In animal model of Alzheimer’s disease (AD), established through the generation of amyloid beta precursor protein transgenic mice, the number of amyloid beta plaques was remarkably diminished by the application of 810 nm PBM[172]. The behavioral pattern of affected mice was also improved, together with a consistent decrease in the expression of pro-inflammatory cytokines[172]. The rescuing effect of PBM was associated with an increase in mitochondrial function and ATP levels[172]. Despite these encouraging results in experimental animal models, surprisingly no major clinical trials have been conducted using PBM in AD patients. In a small-sample, preliminary (so far only appeared in abstract form) but randomized controlled trial, in patients with moderate-to-severe AD (Mini-Mental State Examination scores ranging 5-24), the combinatorial delivery of PBM through the trans-cranial and intranasal routes afforded a significant improvement (5-point Mini-Mental State Examination score) after 12 wk, with a concomitant improvement in Alzheimer's Disease Assessment Scale - Cognitive assessment[173]. In a recently published study, where patients with AD were subjected to intravascular PBM (final positioning of the optic fiber emitter lined up to the distal site of anterior and middle cerebral arteries), authors reported a significant, long-lasting (up to 7 years) enhancement of cerebral microcirculation and cognitive improvement[174].
Another set of studies performed in both acute and chronic mouse models of pharmacologically-induced Parkinson’s disease revealed a remarkable increase in the number of dopaminergic neurons[175]. These studies were confirmed in a tau transgenic mouse model of Parkinson’s disease[176]. The only available clinical trial presented so far in the abstract form, enrolling subjects whose age ranged between 18 and 80 years, reported a significant improvement of the investigated indicators of balance, including gait, cognitive function, and speech[177].
Remarkably, LLLT (808 nm) has been recently applied in vivo to the tibia and iliac bones of pigs subjected to experimental acute myocardial infarction, leading to a significant reduction in cardiac scarring, with increased density of small blood vessels in the infarcted area, and consistent improvement of heart function[178]. The LLLT action was mediated by an increase in the number of circulating c-kit+ stem cells during the first 48 h post-infarction[178]. These beneficial effects resulted to be a long-lasting outcome of the laser treatment, since they were documented 90 d after the infarct induction[178]. These findings provided the first evidence on the use of light radiation to afford a non-invasive cardioprotection of the heart in the acute phase post myocardial infarction, mediated by endogenous stem cell proliferation and recruitment to the ischemic heart, without resorting to stem cell transplantation strategies (Table 3).
Table 3.
Photobiomodulation studies
| Photobiomodulation | Conditions | Biological effects | References number |
| LLLT | Tumor transplantation in rats | Failure to affect the implanted tumor; Stimulation of hair regrowth and wound healing | [135-138] |
| Cell-generated electromagnetic (light) signals | Baby hamster kidney cells on thin glass film | Cell migration and orientation afforded by endogenous generation and processing of signals carried out by electromagnetic radiation (light) | [139] |
| Near-infrared light scattering | Cell culture | Near-infrared light scattering by cells mediates long-range attraction between them and aggregation within the culture system | [140] |
| PBM with blue (420 nm) or green (540 nm) light | hADSCs | Promotion of osteoblastic differentiation; Overexpression of a gene program of osteogenesis; Increase of intracellular calcium mediated by the activation of light-gated calcium ion channels | [141, 142] |
| PBM with red (660 nm) or near-infrared (810 nm) light | hADSCs | Induction of cell proliferation; Maintenance of low ROS level | [151] |
| PBM with blue (415 nm) or green (540 nm) light | hADSCs | Inhibition of cell proliferation; Increase of low ROS level; Lowering of mitochondrial membrane potential and intracellular pH | [151] |
| Various forms of PBM | Acute stroke in animal models | Improvement of the outcome of acute stroke | [152-157] |
| PBM with 810 nm laser light | Human moderate-to-severe stroke associated with neurological defects | Long-lasting neurological improvement | [158-160] |
| Near-infrared light scattering (665 nm and 810 nm) | Traumatic brain injury in animal models | Rescue of neurological performance and reduction of the size of brain lesions; Increase of neuroprogenitor cells in mouse dentate gyrus and subventricular zone; Increase of learning memory; Improvement of mitochondrial function | [161-168] |
| Near-infrared light scattering (665 nm and 810 nm) | Human traumatic brain injury | Improvement of both language and cognitive performance, as well as brain tissue recovery | [169-171] |
| PBM with near-infrared (810 nm) light | Alzheimer’s disease in animal models | Reduction of amyloid beta plaques; Decrease in the expression of pro-inflammatory cytokines; Increase in mitochondrial function, and ATP levels | [172] |
| PBM with near-infrared (810 nm) light | Human Alzheimer’s disease | Improvement in Alzheimer's Disease Assessment Scale - Cognitive assessment; Enhancement of cerebral microcirculation | [173-174] |
| PBM with near-infrared (810 nm) light | Parkinson’s disease in animal models | Increase in the number of dopaminergic neurons | [175-176] |
| PBM with near-infrared (810 nm) light | Human Parkinson’s disease | Improvement of the investigated indicators of balance, including gait, cognitive function, and speech | [177] |
| LLLT | Acute Myocardial infarction in the pig | Reduction of scarring; Improvement of heart function; Stem cell mobilization and recruitment to the ischemic heart | [178] |
LLLT: Low level light therapy; hADSCs: Human adipose tissue-derived stem cells; PBM: Photobiomodulation.
On the whole, experimental and clinical evidence strongly support the feasibility and the remarkable degree of efficacy of PBM in a number of major pathological conditions that so far cannot be solved even by the most advanced pharmacological and/or surgical procedures.
CONCLUSION
Enhancing our self-healing potential
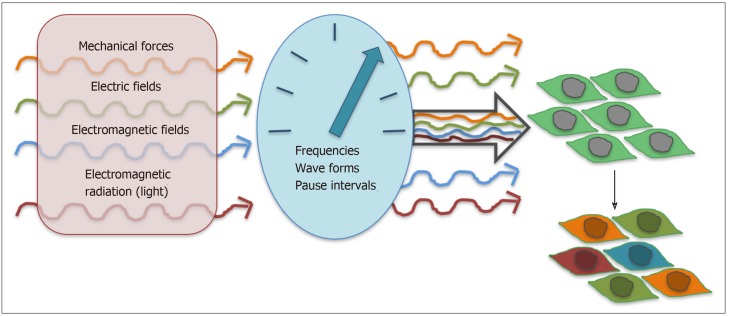
Cells are increasingly regarded as sensors and transducers of physical energies. Novel and probably unprecedented therapeutic strategies are emerging and will be further deployed in the near future, unfolding (stem) cell biology through the eyes of physics, electronics, and likely bioelectronics (Figure 2). Future approaches will increasingly aim at providing valuable, non-invasive, and cost-effective opportunities for boosting our inherent ability of self-healing. Owing to the diffusive features of mechanical, (electro)magnetic, and light waves, (stem) cell reprogramming may occur in place, without necessarily using transplantation (cells/tissue) procedures to rescue damaged tissues.
Figure 2.
(Stem) cells as sensors and transducers of physical energies. A growing number of signaling molecules inside and outside the cell has been shown to behave as mechanosensors/transducers and chromophores (see details in the text). These players modulate complex dynamics controlling multifaceted responses, including proliferation, migration, and differentiation.
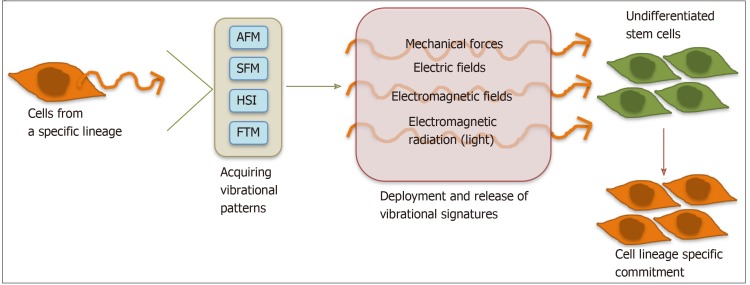
We envision the application of high-tech devices, including AFM, TFM, STM, and fast HSI cameras, to acquire specific signatures from mechanical and electromagnetic radiation (light) patterns of stem cells oriented towards defined fates (Figure 3). We also foresee the development of smart actuators, capable of delivering the acquired individual (i.e., mechanical, or electromagnetic) or combinatorial signatures to diseased tissues, selectively driving the fate and rescuing potential of resident stem cells, to afford a precision endogenous regenerative medicine (Figure 3).
Figure 3.
Harvesting and releasing vibrational signatures to afford commitment of undifferentiated stem cells towards targeted fates. Atomic force microscopy, terahertz field microscopy, scanning tunneling microscopy, and hyperspectral imaging can be used to harvest detailed oscillatory patterns, including mechanical, electric, and light waves. Computer analysis is then performed to acquire vibrational signatures from the investigated patterns. Ad hoc designed transducers are finally developed to provide high-fidelity and timely release of the acquired signatures onto undifferentiated (stem) cells to prime their lineage specific commitment. AFM: Atomic force microscopy; STM: Scanning tunneling microscopy; HIS: Hyperspectral imaging; TFM: Terahertz field microscopy.
Physical tissue stimulation and the merging of human body with machines. May future approaches change the way we are connected to ourselves?
In the next few years we will probably experience a fundamental transformation in the way we live, work, and relate to each-other. The so-called 4th Industrial revolution will trace the future of electronics, machines, and AI and may even change the way we are connected to and perceive ourselves. Future electronics will be focused more and more on health technologies and will be directed inwards, with respect to human beings, trying to promote self-healing mechanisms. Most of currently available technology has been pointing outwards, being focused of making available “something that accomplishes something”.
Emerging future technologies will promote novel interfaces of human beings with machines and AI. What if we may take signatures/codes of our (stem) cell ability to cope with a hostile environment (i.e., oxidative stress, hypoxia) or differentiate along the most complex fates, like the heart, the brain and so on? What if that piece of a stem cell code may be integrated with evolving forms of machines and AI to promote endogenous tissue regeneration? Within this futuristic scenario we may start exploring the synchronistic interchange of who we are and what we are able to become.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest.
Manuscript source: Invited manuscript
Peer-review started: February 13, 2019
First decision: April 12, 2019
Article in press: May 29, 2019
Specialty type: Cell and tissue engineering
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Atwood CS, Park JB S-Editor: Dou Y L-Editor: Filipodia E-Editor: Wu YXJ
Contributor Information
Federica Facchin, Department of Experimental, Diagnostic and Specialty Medicine (DIMES), School of Medicine, University of Bologna, Bologna 40100, Italy; National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Silvia Canaider, Department of Experimental, Diagnostic and Specialty Medicine (DIMES), School of Medicine, University of Bologna, Bologna 40100, Italy; National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Riccardo Tassinari, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Chiara Zannini, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Eva Bianconi, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Valentina Taglioli, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Elena Olivi, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Claudia Cavallini, National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy.
Marco Tausel, iB3 SA, Lugano 6900, Switzerland.
Carlo Ventura, Department of Experimental, Diagnostic and Specialty Medicine (DIMES), School of Medicine, University of Bologna, Bologna 40100, Italy; National Laboratory of Molecular Biology and Stem Cell Engineering, National Institute of Biostructures and Biosystems, CNR, Bologna 40100, Italy. carlo.ventura@unibo.it.
References
- 1.Segura-Valdez ML, Agredano-Moreno LT, Zamora-Cura AL, Lara-Martínez R, Jiménez-García LF. Visualization of internal in situ cell structure by atomic force microscopy. Histochem Cell Biol. 2018;150:521–527. doi: 10.1007/s00418-018-1721-6. [DOI] [PubMed] [Google Scholar]
- 2.Cosgrove DJ. Nanoscale structure, mechanics and growth of epidermal cell walls. Curr Opin Plant Biol. 2018;46:77–86. doi: 10.1016/j.pbi.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Amarouch MY, El Hilaly J, Mazouzi D. AFM and FluidFM Technologies: Recent Applications in Molecular and Cellular Biology. Scanning. 2018;2018:7801274. doi: 10.1155/2018/7801274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma S, LeClaire M, Gimzewski JK. Ascent of atomic force microscopy as a nanoanalytical tool for exosomes and other extracellular vesicles. Nanotechnology. 2018;29:132001. doi: 10.1088/1361-6528/aaab06. [DOI] [PubMed] [Google Scholar]
- 5.Sahu S, Ghosh S, Fujita D, Bandyopadhyay A. Live visualizations of single isolated tubulin protein self-assembly via tunneling current: effect of electromagnetic pumping during spontaneous growth of microtubule. Sci Rep. 2014;4:7303. doi: 10.1038/srep07303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agrawal L, Sahu S, Ghosh S, Shiga T, Fujita D, Bandyopadhyay A. Inventing atomic resolution scanning dielectric microscopy to see a single protein complex operation live at resonance in a neuron without touching or adulterating the cell. J Integr Neurosci. 2016;15:435–462. doi: 10.1142/S0219635216500333. [DOI] [PubMed] [Google Scholar]
- 7.Acbas G, Niessen KA, Snell EH, Markelz AG. Optical measurements of long-range protein vibrations. Nat Commun. 2014;5:3076. doi: 10.1038/ncomms4076. [DOI] [PubMed] [Google Scholar]
- 8.Cheng JX, Xie XS. Vibrational spectroscopic imaging of living systems: An emerging platform for biology and medicine. Science. 2015;350:aaa8870. doi: 10.1126/science.aaa8870. [DOI] [PubMed] [Google Scholar]
- 9.Browne AW, Arnesano C, Harutyunyan N, Khuu T, Martinez JC, Pollack HA, Koos DS, Lee TC, Fraser SE, Moats RA, Aparicio JG, Cobrinik D. Structural and Functional Characterization of Human Stem-Cell-Derived Retinal Organoids by Live Imaging. Invest Ophthalmol Vis Sci. 2017;58:3311–3318. doi: 10.1167/iovs.16-20796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heraud P, Cowan MF, Marzec KM, Møller BL, Blomstedt CK, Gleadow R. Label-free Raman hyperspectral imaging analysis localizes the cyanogenic glucoside dhurrin to the cytoplasm in sorghum cells. Sci Rep. 2018;8:2691. doi: 10.1038/s41598-018-20928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anlaş AA, Nelson CM. Tissue mechanics regulates form, function, and dysfunction. Curr Opin Cell Biol. 2018;54:98–105. doi: 10.1016/j.ceb.2018.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lele TP, Dickinson RB, Gundersen GG. Mechanical principles of nuclear shaping and positioning. J Cell Biol. 2018;217:3330–3342. doi: 10.1083/jcb.201804052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stein AA, Logvenkov SA, Volodyaev IV. Continuum modeling of mechano-dependent reactions in tissues composed of mechanically active cells. Biosystems. 2018;173:225–234. doi: 10.1016/j.biosystems.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Havelka D, Cifra M, Kučera O, Pokorný J, Vrba J. High-frequency electric field and radiation characteristics of cellular microtubule network. J Theor Biol. 2011;286:31–40. doi: 10.1016/j.jtbi.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Koka PS. Biomarker discovery and biotherapeutics applications of photosynthetic light-harvesting and bioluminescence light-emitting chromophore-protein complexes in stem cell biology and regenerative medicine. J Stem Cells. 2014;9:127–133. [PubMed] [Google Scholar]
- 16.Craddock TJ, Friesen D, Mane J, Hameroff S, Tuszynski JA. The feasibility of coherent energy transfer in microtubules. J R Soc Interface. 2014;11:20140677. doi: 10.1098/rsif.2014.0677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kianianmomeni A, Hallmann A. Transcriptional analysis of Volvox photoreceptors suggests the existence of different cell-type specific light-signaling pathways. Curr Genet. 2015;61:3–18. doi: 10.1007/s00294-014-0440-3. [DOI] [PubMed] [Google Scholar]
- 18.Blackshaw S, Snyder SH. Encephalopsin: a novel mammalian extraretinal opsin discretely localized in the brain. J Neurosci. 1999;19:3681–3690. doi: 10.1523/JNEUROSCI.19-10-03681.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoang N, Schleicher E, Kacprzak S, Bouly JP, Picot M, Wu W, Berndt A, Wolf E, Bittl R, Ahmad M. Human and Drosophila cryptochromes are light activated by flavin photoreduction in living cells. PLoS Biol. 2008;6:e160. doi: 10.1371/journal.pbio.0060160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parihar P, Singh R, Singh S, Tripathi DK, Chauhan DK, Singh VP, Prasad SM. Photoreceptors mapping from past history till date. J Photochem Photobiol B. 2016;162:223–231. doi: 10.1016/j.jphotobiol.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 21.Porter ML, Blasic JR, Bok MJ, Cameron EG, Pringle T, Cronin TW, Robinson PR. Shedding new light on opsin evolution. Proc Biol Sci. 2012;279:3–14. doi: 10.1098/rspb.2011.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bailes HJ, Lucas RJ. Human melanopsin forms a pigment maximally sensitive to blue light (λmax ≈ 479 nm) supporting activation of G(q/11) and G(i/o) signalling cascades. Proc Biol Sci. 2013;280:20122987. doi: 10.1098/rspb.2012.2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ankri R, Friedman H, Savion N, Kotev-Emeth S, Breitbart H, Lubart R. Visible light induces nitric oxide (NO) formation in sperm and endothelial cells. Lasers Surg Med. 2010;42:348–352. doi: 10.1002/lsm.20849. [DOI] [PubMed] [Google Scholar]
- 24.Garza ZCF, Born M, Hilbers PAJ, van Riel NAW, Liebmann J. Visible Blue Light Therapy: Molecular Mechanisms and Therapeutic Opportunities. Curr Med Chem. 2018;25:5564–5577. doi: 10.2174/0929867324666170727112206. [DOI] [PubMed] [Google Scholar]
- 25.Iyanagi T. Molecular mechanism of metabolic NAD(P)H-dependent electron-transfer systems: The role of redox cofactors. Biochim Biophys Acta Bioenerg. 2019;1860:233–258. doi: 10.1016/j.bbabio.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Terakita A, Nagata T. Functional properties of opsins and their contribution to light-sensing physiology. Zoolog Sci. 2014;31:653–659. doi: 10.2108/zs140094. [DOI] [PubMed] [Google Scholar]
- 27.Kojima D, Mori S, Torii M, Wada A, Morishita R, Fukada Y. UV-sensitive photoreceptor protein OPN5 in humans and mice. PLoS One. 2011;6:e26388. doi: 10.1371/journal.pone.0026388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koyanagi M, Terakita A. Diversity of animal opsin-based pigments and their optogenetic potential. Biochim Biophys Acta. 2014;1837:710–716. doi: 10.1016/j.bbabio.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Sakipov S, Sobolevsky AI, Kurnikova MG. Ion Permeation Mechanism in Epithelial Calcium Channel TRVP6. Sci Rep. 2018;8:5715. doi: 10.1038/s41598-018-23972-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu ZH, Zhou Y, Chen JY, Zhou LW. Mitochondrial signaling for histamine releases in laser-irradiated RBL-2H3 mast cells. Lasers Surg Med. 2010;42:503–509. doi: 10.1002/lsm.20924. [DOI] [PubMed] [Google Scholar]
- 31.Yang WZ, Chen JY, Yu JT, Zhou LW. Effects of low power laser irradiation on intracellular calcium and histamine release in RBL-2H3 mast cells. Photochem Photobiol. 2007;83:979–984. doi: 10.1111/j.1751-1097.2007.00116.x. [DOI] [PubMed] [Google Scholar]
- 32.Mure LS, Hatori M, Ruda K, Benegiamo G, Demas J, Panda S. Sustained Melanopsin Photoresponse Is Supported by Specific Roles of β-Arrestin 1 and 2 in Deactivation and Regeneration of Photopigment. Cell Rep. 2018;25:2497–2509.e4. doi: 10.1016/j.celrep.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagata T, Koyanagi M, Lucas R, Terakita A. An all-trans-retinal-binding opsin peropsin as a potential dark-active and light-inactivated G protein-coupled receptor. Sci Rep. 2018;8:3535. doi: 10.1038/s41598-018-21946-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bonmati-Carrion MA, Arguelles-Prieto R, Martinez-Madrid MJ, Reiter R, Hardeland R, Rol MA, Madrid JA. Protecting the melatonin rhythm through circadian healthy light exposure. Int J Mol Sci. 2014;15:23448–23500. doi: 10.3390/ijms151223448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schaap IA, Carrasco C, de Pablo PJ, Schmidt CF. Kinesin walks the line: single motors observed by atomic force microscopy. Biophys J. 2011;100:2450–2456. doi: 10.1016/j.bpj.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cosic I, Cosic D, Lazar K. Is it possible to predict electromagnetic resonances in proteins, DNA and RNA? EPJ Nonlinear Biomedical Physics. 2015;3:5. [Google Scholar]
- 37.Cosic I. Macromolecular bioactivity: is it resonant interaction between macromolecules?--Theory and applications. IEEE Trans Biomed Eng. 1994;41:1101–1114. doi: 10.1109/10.335859. [DOI] [PubMed] [Google Scholar]
- 38.Cosic I, Cosic D, Lazar K. Environmental Light and Its Relationship with Electromagnetic Resonances of Biomolecular Interactions, as Predicted by the Resonant Recognition Model. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13070647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cosic I, Lazar K, Cosic D. Prediction of Tubulin Resonant Frequencies Using the Resonant Recognition Model (RRM) IEEE Trans Nanobioscience. 2015;14:491–496. doi: 10.1109/TNB.2014.2365851. [DOI] [PubMed] [Google Scholar]
- 40.Cosic I, Pirogova E. Bioactive peptide design using the Resonant Recognition Model. Nonlinear Biomed Phys. 2007;1:7. doi: 10.1186/1753-4631-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koch MD, Schneider N, Nick P, Rohrbach A. Single microtubules and small networks become significantly stiffer on short time-scales upon mechanical stimulation. Sci Rep. 2017;7:4229. doi: 10.1038/s41598-017-04415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Havelka D, Deriu MA, Cifra M, Kučera O. Deformation pattern in vibrating microtubule: Structural mechanics study based on an atomistic approach. Sci Rep. 2017;7:4227. doi: 10.1038/s41598-017-04272-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sanchez T, Dogic Z. Engineering oscillating microtubule bundles. Methods Enzymol. 2013;524:205–224. doi: 10.1016/B978-0-12-397945-2.00012-3. [DOI] [PubMed] [Google Scholar]
- 44.O'Keeffe KP, Hong H, Strogatz SH. Oscillators that sync and swarm. Nat Commun. 2017;8:1504. doi: 10.1038/s41467-017-01190-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sumino Y, Nagai KH, Shitaka Y, Tanaka D, Yoshikawa K, Chaté H, Oiwa K. Large-scale vortex lattice emerging from collectively moving microtubules. Nature. 2012;483:448–452. doi: 10.1038/nature10874. [DOI] [PubMed] [Google Scholar]
- 46.Santelices IB, Friesen DE, Bell C, Hough CM, Xiao J, Kalra A, Kar P, Freedman H, Rezania V, Lewis JD, Shankar K, Tuszynski JA. Response to Alternating Electric Fields of Tubulin Dimers and Microtubule Ensembles in Electrolytic Solutions. Sci Rep. 2017;7:9594. doi: 10.1038/s41598-017-09323-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Priel A, Ramos AJ, Tuszynski JA, Cantiello HF. A biopolymer transistor: electrical amplification by microtubules. Biophys J. 2006;90:4639–4643. doi: 10.1529/biophysj.105.078915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sekulić DL, Satarić BM, Tuszynski JA, Satarić MV. Nonlinear ionic pulses along microtubules. Eur Phys J E Soft Matter. 2011;34:49. doi: 10.1140/epje/i2011-11049-0. [DOI] [PubMed] [Google Scholar]
- 49.Minoura I, Muto E. Dielectric measurement of individual microtubules using the electroorientation method. Biophys J. 2006;90:3739–3748. doi: 10.1529/biophysj.105.071324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cantero Mdel R, Perez PL, Smoler M, Villa Etchegoyen C, Cantiello HF. Electrical Oscillations in Two-Dimensional Microtubular Structures. Sci Rep. 2016;6:27143. doi: 10.1038/srep27143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cantero MDR, Villa Etchegoyen C, Perez PL, Scarinci N, Cantiello HF. Bundles of Brain Microtubules Generate Electrical Oscillations. Sci Rep. 2018;8:11899. doi: 10.1038/s41598-018-30453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kirson ED, Gurvich Z, Schneiderman R, Dekel E, Itzhaki A, Wasserman Y, Schatzberger R, Palti Y. Disruption of cancer cell replication by alternating electric fields. Cancer Res. 2004;64:3288–3295. doi: 10.1158/0008-5472.can-04-0083. [DOI] [PubMed] [Google Scholar]
- 53.Stupp R, Taillibert S, Kanner AA, Kesari S, Steinberg DM, Toms SA, Taylor LP, Lieberman F, Silvani A, Fink KL, Barnett GH, Zhu JJ, Henson JW, Engelhard HH, Chen TC, Tran DD, Sroubek J, Tran ND, Hottinger AF, Landolfi J, Desai R, Caroli M, Kew Y, Honnorat J, Idbaih A, Kirson ED, Weinberg U, Palti Y, Hegi ME, Ram Z. Maintenance Therapy With Tumor-Treating Fields Plus Temozolomide vs Temozolomide Alone for Glioblastoma: A Randomized Clinical Trial. JAMA. 2015;314:2535–2543. doi: 10.1001/jama.2015.16669. [DOI] [PubMed] [Google Scholar]
- 54.Kirson ED, Dbalý V, Tovarys F, Vymazal J, Soustiel JF, Itzhaki A, Mordechovich D, Steinberg-Shapira S, Gurvich Z, Schneiderman R, Wasserman Y, Salzberg M, Ryffel B, Goldsher D, Dekel E, Palti Y. Alternating electric fields arrest cell proliferation in animal tumor models and human brain tumors. Proc Natl Acad Sci U S A. 2007;104:10152–10157. doi: 10.1073/pnas.0702916104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tuszynski JA, Wenger C, Friesen DE, Preto J. An Overview of Sub-Cellular Mechanisms Involved in the Action of TTFields. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13111128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ayoub AT, Staelens M, Prunotto A, Deriu MA, Danani A, Klobukowski M, Tuszynski JA. Explaining the Microtubule Energy Balance: Contributions Due to Dipole Moments, Charges, van der Waals and Solvation Energy. Int J Mol Sci. 2017;18 doi: 10.3390/ijms18102042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barzanjeh S, Salari V, Tuszynski JA, Cifra M, Simon C. Optomechanical proposal for monitoring microtubule mechanical vibrations. Phys Rev E. 2017;96:012404. doi: 10.1103/PhysRevE.96.012404. [DOI] [PubMed] [Google Scholar]
- 58.Craddock TJA, Kurian P, Preto J, Sahu K, Hameroff SR, Klobukowski M, Tuszynski JA. Anesthetic Alterations of Collective Terahertz Oscillations in Tubulin Correlate with Clinical Potency: Implications for Anesthetic Action and Post-Operative Cognitive Dysfunction. Sci Rep. 2017;7:9877. doi: 10.1038/s41598-017-09992-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sahu S, Ghosh S, Hirata K, Fujita D, Bandyopadhyay A. Multi-level memory-switching properties of a single brain microtubule. Appl Phys Lett. 2013;102:123701. [Google Scholar]
- 60.Rubin C, Turner AS, Bain S, Mallinckrodt C, McLeod K. Anabolism. Low mechanical signals strengthen long bones. Nature. 2001;412:603–604. doi: 10.1038/35088122. [DOI] [PubMed] [Google Scholar]
- 61.Rubin C, Xu G, Judex S. The anabolic activity of bone tissue, suppressed by disuse, is normalized by brief exposure to extremely low-magnitude mechanical stimuli. FASEB J. 2001;15:2225–2229. doi: 10.1096/fj.01-0166com. [DOI] [PubMed] [Google Scholar]
- 62.Ozcivici E, Luu YK, Adler B, Qin YX, Rubin J, Judex S, Rubin CT. Mechanical signals as anabolic agents in bone. Nat Rev Rheumatol. 2010;6:50–59. doi: 10.1038/nrrheum.2009.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rubin CT, Capilla E, Luu YK, Busa B, Crawford H, Nolan DJ, Mittal V, Rosen CJ, Pessin JE, Judex S. Adipogenesis is inhibited by brief, daily exposure to high-frequency, extremely low-magnitude mechanical signals. Proc Natl Acad Sci U S A. 2007;104:17879–17884. doi: 10.1073/pnas.0708467104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Luu YK, Pessin JE, Judex S, Rubin J, Rubin CT. Mechanical Signals As a Non-Invasive Means to Influence Mesenchymal Stem Cell Fate, Promoting Bone and Suppressing the Fat Phenotype. Bonekey Osteovision. 2009;6:132–149. doi: 10.1138/20090371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chan ME, Adler BJ, Green DE, Rubin CT. Bone structure and B-cell populations, crippled by obesity, are partially rescued by brief daily exposure to low-magnitude mechanical signals. FASEB J. 2012;26:4855–4863. doi: 10.1096/fj.12-209841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ozcivici E, Luu YK, Rubin CT, Judex S. Low-level vibrations retain bone marrow's osteogenic potential and augment recovery of trabecular bone during reambulation. PLoS One. 2010;5:e11178. doi: 10.1371/journal.pone.0011178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sen B, Styner M, Xie Z, Case N, Rubin CT, Rubin J. Mechanical loading regulates NFATc1 and beta-catenin signaling through a GSK3beta control node. J Biol Chem. 2009;284:34607–34617. doi: 10.1074/jbc.M109.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Uzer G, Pongkitwitoon S, Ete Chan M, Judex S. Vibration induced osteogenic commitment of mesenchymal stem cells is enhanced by cytoskeletal remodeling but not fluid shear. J Biomech. 2013;46:2296–2302. doi: 10.1016/j.jbiomech.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Uzer G, Thompson WR, Sen B, Xie Z, Yen SS, Miller S, Bas G, Styner M, Rubin CT, Judex S, Burridge K, Rubin J. Cell Mechanosensitivity to Extremely Low-Magnitude Signals Is Enabled by a LINCed Nucleus. Stem Cells. 2015;33:2063–2076. doi: 10.1002/stem.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Havelka D, Kučera O, Deriu MA, Cifra M. Electro-acoustic behavior of the mitotic spindle: a semi-classical coarse-grained model. PLoS One. 2014;9:e86501. doi: 10.1371/journal.pone.0086501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet. 1980;2:1265–1268. doi: 10.1016/s0140-6736(80)92335-1. [DOI] [PubMed] [Google Scholar]
- 72.Ottomann C, Stojadinovic A, Lavin PT, Gannon FH, Heggeness MH, Thiele R, Schaden W, Hartmann B. Prospective randomized phase II Trial of accelerated reepithelialization of superficial second-degree burn wounds using extracorporeal shock wave therapy. Ann Surg. 2012;255:23–29. doi: 10.1097/SLA.0b013e318227b3c0. [DOI] [PubMed] [Google Scholar]
- 73.Schaden W, Thiele R, Kölpl C, Pusch M, Nissan A, Attinger CE, Maniscalco-Theberge ME, Peoples GE, Elster EA, Stojadinovic A. Shock wave therapy for acute and chronic soft tissue wounds: a feasibility study. J Surg Res. 2007;143:1–12. doi: 10.1016/j.jss.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 74.Ottomann C, Hartmann B, Tyler J, Maier H, Thiele R, Schaden W, Stojadinovic A. Prospective randomized trial of accelerated re-epithelization of skin graft donor sites using extracorporeal shock wave therapy. J Am Coll Surg. 2010;211:361–367. doi: 10.1016/j.jamcollsurg.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 75.Wang CJ, Yang KD, Ko JY, Huang CC, Huang HY, Wang FS. The effects of shockwave on bone healing and systemic concentrations of nitric oxide (NO), TGF-beta1, VEGF and BMP-2 in long bone non-unions. Nitric Oxide. 2009;20:298–303. doi: 10.1016/j.niox.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 76.Chen YJ, Kuo YR, Yang KD, Wang CJ, Sheen Chen SM, Huang HC, Yang YJ, Yi-Chih S, Wang FS. Activation of extracellular signal-regulated kinase (ERK) and p38 kinase in shock wave-promoted bone formation of segmental defect in rats. Bone. 2004;34:466–477. doi: 10.1016/j.bone.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 77.Wang CJ, Yang KD, Wang FS, Hsu CC, Chen HH. Shock wave treatment shows dose-dependent enhancement of bone mass and bone strength after fracture of the femur. Bone. 2004;34:225–230. doi: 10.1016/j.bone.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 78.Holfeld J, Tepeköylü C, Blunder S, Lobenwein D, Kirchmair E, Dietl M, Kozaryn R, Lener D, Theurl M, Paulus P, Kirchmair R, Grimm M. Low energy shock wave therapy induces angiogenesis in acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PLoS One. 2014;9:e103982. doi: 10.1371/journal.pone.0103982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen YJ, Wurtz T, Wang CJ, Kuo YR, Yang KD, Huang HC, Wang FS. Recruitment of mesenchymal stem cells and expression of TGF-beta 1 and VEGF in the early stage of shock wave-promoted bone regeneration of segmental defect in rats. J Orthop Res. 2004;22:526–534. doi: 10.1016/j.orthres.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 80.Tepeköylü C, Lobenwein D, Urbschat A, Graber M, Pechriggl EJ, Fritsch H, Paulus P, Grimm M, Holfeld J. Shock wave treatment after hindlimb ischaemia results in increased perfusion and M2 macrophage presence. J Tissue Eng Regen Med. 2018;12:e486–e494. doi: 10.1002/term.2317. [DOI] [PubMed] [Google Scholar]
- 81.Weihs AM, Fuchs C, Teuschl AH, Hartinger J, Slezak P, Mittermayr R, Redl H, Junger WG, Sitte HH, Rünzler D. Shock wave treatment enhances cell proliferation and improves wound healing by ATP release-coupled extracellular signal-regulated kinase (ERK) activation. J Biol Chem. 2014;289:27090–27104. doi: 10.1074/jbc.M114.580936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nishida T, Shimokawa H, Oi K, Tatewaki H, Uwatoku T, Abe K, Matsumoto Y, Kajihara N, Eto M, Matsuda T, Yasui H, Takeshita A, Sunagawa K. Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation. 2004;110:3055–3061. doi: 10.1161/01.CIR.0000148849.51177.97. [DOI] [PubMed] [Google Scholar]
- 83.Holfeld J, Zimpfer D, Albrecht-Schgoer K, Stojadinovic A, Paulus P, Dumfarth J, Thomas A, Lobenwein D, Tepeköylü C, Rosenhek R, Schaden W, Kirchmair R, Aharinejad S, Grimm M. Epicardial shock-wave therapy improves ventricular function in a porcine model of ischaemic heart disease. J Tissue Eng Regen Med. 2016;10:1057–1064. doi: 10.1002/term.1890. [DOI] [PubMed] [Google Scholar]
- 84.Tepeköylü C, Primessnig U, Pölzl L, Graber M, Lobenwein D, Nägele F, Kirchmair E, Pechriggl E, Grimm M, Holfeld J. Shockwaves prevent from heart failure after acute myocardial ischaemia via RNA/protein complexes. J Cell Mol Med. 2017;21:791–801. doi: 10.1111/jcmm.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tepeköylü C, Wang FS, Kozaryn R, Albrecht-Schgoer K, Theurl M, Schaden W, Ke HJ, Yang Y, Kirchmair R, Grimm M, Wang CJ, Holfeld J. Shock wave treatment induces angiogenesis and mobilizes endogenous CD31/CD34-positive endothelial cells in a hindlimb ischemia model: implications for angiogenesis and vasculogenesis. J Thorac Cardiovasc Surg. 2013;146:971–978. doi: 10.1016/j.jtcvs.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 86.Aicher A, Heeschen C, Sasaki K, Urbich C, Zeiher AM, Dimmeler S. Low-energy shock wave for enhancing recruitment of endothelial progenitor cells: a new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation. 2006;114:2823–2830. doi: 10.1161/CIRCULATIONAHA.106.628623. [DOI] [PubMed] [Google Scholar]
- 87.Gollmann-Tepeköylü C, Lobenwein D, Theurl M, Primessnig U, Lener D, Kirchmair E, Mathes W, Graber M, Pölzl L, An A, Koziel K, Pechriggl E, Voelkl J, Paulus P, Schaden W, Grimm M, Kirchmair R, Holfeld J. Shock Wave Therapy Improves Cardiac Function in a Model of Chronic Ischemic Heart Failure: Evidence for a Mechanism Involving VEGF Signaling and the Extracellular Matrix. J Am Heart Assoc. 2018;7:e010025. doi: 10.1161/JAHA.118.010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hatanaka K, Ito K, Shindo T, Kagaya Y, Ogata T, Eguchi K, Kurosawa R, Shimokawa H. Molecular mechanisms of the angiogenic effects of low-energy shock wave therapy: roles of mechanotransduction. Am J Physiol Cell Physiol. 2016;311:C378–C385. doi: 10.1152/ajpcell.00152.2016. [DOI] [PubMed] [Google Scholar]
- 89.Fukumoto Y, Ito A, Uwatoku T, Matoba T, Kishi T, Tanaka H, Takeshita A, Sunagawa K, Shimokawa H. Extracorporeal cardiac shock wave therapy ameliorates myocardial ischemia in patients with severe coronary artery disease. Coron Artery Dis. 2006;17:63–70. doi: 10.1097/00019501-200602000-00011. [DOI] [PubMed] [Google Scholar]
- 90.Kikuchi Y, Ito K, Ito Y, Shiroto T, Tsuburaya R, Aizawa K, Hao K, Fukumoto Y, Takahashi J, Takeda M, Nakayama M, Yasuda S, Kuriyama S, Tsuji I, Shimokawa H. Double-blind and placebo-controlled study of the effectiveness and safety of extracorporeal cardiac shock wave therapy for severe angina pectoris. Circ J. 2010;74:589–591. doi: 10.1253/circj.cj-09-1028. [DOI] [PubMed] [Google Scholar]
- 91.Kagaya Y, Ito K, Takahashi J, Matsumoto Y, Shiroto T, Tsuburaya R, Kikuchi Y, Hao K, Nishimiya K, Shindo T, Ogata T, Kurosawa R, Eguchi K, Monma Y, Ichijo S, Hatanaka K, Miyata S, Shimokawa H. Low-energy cardiac shockwave therapy to suppress left ventricular remodeling in patients with acute myocardial infarction: a first-in-human study. Coron Artery Dis. 2018;29:294–300. doi: 10.1097/MCA.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 92.Notarnicola A, Vicenti G, Maccagnano G, Silvestris F, Cafforio P, Moretti B. Extracorporeal shock waves induce osteogenic differentiation of human bone-marrow stromal cells. J Biol Regul Homeost Agents. 2016;30:139–144. [PubMed] [Google Scholar]
- 93.Hu J, Liao H, Ma Z, Chen H, Huang Z, Zhang Y, Yu M, Chen Y, Xu J. Focal Adhesion Kinase Signaling Mediated the Enhancement of Osteogenesis of Human Mesenchymal Stem Cells Induced by Extracorporeal Shockwave. Sci Rep. 2016;6:20875. doi: 10.1038/srep20875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schuh CM, Heher P, Weihs AM, Banerjee A, Fuchs C, Gabriel C, Wolbank S, Mittermayr R, Redl H, Rünzler D, Teuschl AH. In vitro extracorporeal shock wave treatment enhances stemness and preserves multipotency of rat and human adipose-derived stem cells. Cytotherapy. 2014;16:1666–1678. doi: 10.1016/j.jcyt.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 95.Xu L, Zhao Y, Wang M, Song W, Li B, Liu W, Jin X, Zhang H. Defocused low-energy shock wave activates adipose tissue-derived stem cells in vitro via multiple signaling pathways. Cytotherapy. 2016;18:1503–1514. doi: 10.1016/j.jcyt.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 96.Shin DC, Ha KY, Kim YH, Kim JW, Cho YK, Kim SI. Induction of Endogenous Neural Stem Cells By Extracorporeal Shock Waves After Spinal Cord Injury. Spine (Phila Pa 1976) 2018;43:E200–E207. doi: 10.1097/BRS.0000000000002302. [DOI] [PubMed] [Google Scholar]
- 97.Jin Y, Xu L, Zhao Y, Wang M, Jin X, Zhang H. Endogenous Stem Cells Were Recruited by Defocused Low-Energy Shock Wave in Treating Diabetic Bladder Dysfunction. Stem Cell Rev. 2017;13:287–298. doi: 10.1007/s12015-016-9705-1. [DOI] [PubMed] [Google Scholar]
- 98.Gurel PS, Hatch AL, Higgs HN. Connecting the cytoskeleton to the endoplasmic reticulum and Golgi. Curr Biol. 2014;24:R660–R672. doi: 10.1016/j.cub.2014.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pelling AE, Sehati S, Gralla EB, Valentine JS, Gimzewski JK. Local nanomechanical motion of the cell wall of Saccharomyces cerevisiae. Science. 2004;305:1147–1150. doi: 10.1126/science.1097640. [DOI] [PubMed] [Google Scholar]
- 100.Gimzewski JK, Pelling A, Ventura C, inventors Nanomechanical Characterization of Cellular Activity. International Patent WO 2008/105919 A2. 2008:Sep 4.
- 101.Ventura C, Maioli M, Pintus G, Gottardi G, Bersani F. Elf-pulsed magnetic fields modulate opioid peptide gene expression in myocardial cells. Cardiovasc Res. 2000;45:1054–1064. doi: 10.1016/s0008-6363(99)00408-3. [DOI] [PubMed] [Google Scholar]
- 102.Ventura C, Spurgeon H, Lakatta EG, Guarnieri C, Capogrossi MC. Kappa and delta opioid receptor stimulation affects cardiac myocyte function and Ca2+ release from an intracellular pool in myocytes and neurons. Circ Res. 1992;70:66–81. doi: 10.1161/01.res.70.1.66. [DOI] [PubMed] [Google Scholar]
- 103.Ventura C, Capogrossi MC, Spurgeon HA, Lakatta EG. Kappa-opioid peptide receptor stimulation increases cytosolic pH and myofilament responsiveness to Ca2+ in cardiac myocytes. Am J Physiol. 1991;261:H1671–H1674. doi: 10.1152/ajpheart.1991.261.5.H1671. [DOI] [PubMed] [Google Scholar]
- 104.Ventura C, Pintus G, Fiori MG, Bennardini F, Pinna G, Gaspa L. Opioid peptide gene expression in the primary hereditary cardiomyopathy of the Syrian hamster. I. Regulation of prodynorphin gene expression by nuclear protein kinase C. J Biol Chem. 1997;272:6685–6692. doi: 10.1074/jbc.272.10.6685. [DOI] [PubMed] [Google Scholar]
- 105.Ventura C, Pintus G, Tadolini B. Opioid peptide gene expression in the primary hereditary cardiomyopathy of the Syrian hamster. II. Role of intracellular calcium loading. J Biol Chem. 1997;272:6693–6698. doi: 10.1074/jbc.272.10.6693. [DOI] [PubMed] [Google Scholar]
- 106.Ventura C, Pintus G. Opioid peptide gene expression in the primary hereditary cardiomyopathy of the Syrian hamster. III. Autocrine stimulation of prodynorphin gene expression by dynorphin B. J Biol Chem. 1997;272:6699–6705. doi: 10.1074/jbc.272.10.6699. [DOI] [PubMed] [Google Scholar]
- 107.Ventura C, Maioli M. Opioid peptide gene expression primes cardiogenesis in embryonal pluripotent stem cells. Circ Res. 2000;87:189–194. doi: 10.1161/01.res.87.3.189. [DOI] [PubMed] [Google Scholar]
- 108.Ventura C, Zinellu E, Maninchedda E, Fadda M, Maioli M. Protein kinase C signaling transduces endorphin-primed cardiogenesis in GTR1 embryonic stem cells. Circ Res. 2003;92:617–622. doi: 10.1161/01.RES.0000065168.31147.5B. [DOI] [PubMed] [Google Scholar]
- 109.Ventura C, Zinellu E, Maninchedda E, Maioli M. Dynorphin B is an agonist of nuclear opioid receptors coupling nuclear protein kinase C activation to the transcription of cardiogenic genes in GTR1 embryonic stem cells. Circ Res. 2003;92:623–629. doi: 10.1161/01.RES.0000065169.23780.0E. [DOI] [PubMed] [Google Scholar]
- 110.Ventura C, Maioli M, Asara Y, Santoni D, Mesirca P, Remondini D, Bersani F. Turning on stem cell cardiogenesis with extremely low frequency magnetic fields. FASEB J. 2005;19:155–157. doi: 10.1096/fj.04-2695fje. [DOI] [PubMed] [Google Scholar]
- 111.Maioli M, Rinaldi S, Santaniello S, Castagna A, Pigliaru G, Gualini S, Fontani V, Ventura C. Radiofrequency energy loop primes cardiac, neuronal, and skeletal muscle differentiation in mouse embryonic stem cells: a new tool for improving tissue regeneration. Cell Transplant. 2012;21:1225–1233. doi: 10.3727/096368911X600966. [DOI] [PubMed] [Google Scholar]
- 112.Maioli M, Rinaldi S, Santaniello S, Castagna A, Pigliaru G, Delitala A, Bianchi F, Tremolada C, Fontani V, Ventura C. Radioelectric asymmetric conveyed fields and human adipose-derived stem cells obtained with a nonenzymatic method and device: a novel approach to multipotency. Cell Transplant. 2014;23:1489–1500. doi: 10.3727/096368913X672037. [DOI] [PubMed] [Google Scholar]
- 113.Maioli M, Rinaldi S, Santaniello S, Castagna A, Pigliaru G, Gualini S, Cavallini C, Fontani V, Ventura C. Radio electric conveyed fields directly reprogram human dermal skin fibroblasts toward cardiac, neuronal, and skeletal muscle-like lineages. Cell Transplant. 2013;22:1227–1235. doi: 10.3727/096368912X657297. [DOI] [PubMed] [Google Scholar]
- 114.Baal N, Reisinger K, Jahr H, Bohle RM, Liang O, Münstedt K, Rao CV, Preissner KT, Zygmunt MT. Expression of transcription factor Oct-4 and other embryonic genes in CD133 positive cells from human umbilical cord blood. Thromb Haemost. 2004;92:767–775. doi: 10.1160/TH04-02-0079. [DOI] [PubMed] [Google Scholar]
- 115.Goodell MA. Stem-cell "plasticity": befuddled by the muddle. Curr Opin Hematol. 2003;10:208–213. doi: 10.1097/00062752-200305000-00003. [DOI] [PubMed] [Google Scholar]
- 116.Lang KC, Lin IH, Teng HF, Huang YC, Li CL, Tang KT, Chen SL. Simultaneous overexpression of Oct4 and Nanog abrogates terminal myogenesis. Am J Physiol Cell Physiol. 2009;297:C43–C54. doi: 10.1152/ajpcell.00468.2008. [DOI] [PubMed] [Google Scholar]
- 117.Park SB, Seo KW, So AY, Seo MS, Yu KR, Kang SK, Kang KS. SOX2 has a crucial role in the lineage determination and proliferation of mesenchymal stem cells through Dickkopf-1 and c-MYC. Cell Death Differ. 2012;19:534–545. doi: 10.1038/cdd.2011.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rinaldi S, Maioli M, Pigliaru G, Castagna A, Santaniello S, Basoli V, Fontani V, Ventura C. Stem cell senescence. Effects of REAC technology on telomerase-independent and telomerase-dependent pathways. Sci Rep. 2014;4:6373. doi: 10.1038/srep06373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Maioli M, Rinaldi S, Pigliaru G, Santaniello S, Basoli V, Castagna A, Fontani V, Ventura C. REAC technology and hyaluron synthase 2, an interesting network to slow down stem cell senescence. Sci Rep. 2016;6:28682. doi: 10.1038/srep28682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Choudhary M, Zhang X, Stojkovic P, Hyslop L, Anyfantis G, Herbert M, Murdoch AP, Stojkovic M, Lako M. Putative role of hyaluronan and its related genes, HAS2 and RHAMM, in human early preimplantation embryogenesis and embryonic stem cell characterization. Stem Cells. 2007;25:3045–3057. doi: 10.1634/stemcells.2007-0296. [DOI] [PubMed] [Google Scholar]
- 121.Camenisch TD, Spicer AP, Brehm-Gibson T, Biesterfeldt J, Augustine ML, Calabro A, Jr, Kubalak S, Klewer SE, McDonald JA. Disruption of hyaluronan synthase-2 abrogates normal cardiac morphogenesis and hyaluronan-mediated transformation of epithelium to mesenchyme. J Clin Invest. 2000;106:349–360. doi: 10.1172/JCI10272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Deb TB, Datta K. Molecular cloning of human fibroblast hyaluronic acid-binding protein confirms its identity with P-32, a protein co-purified with splicing factor SF2. Hyaluronic acid-binding protein as P-32 protein, co-purified with splicing factor SF2. J Biol Chem. 1996;271:2206–2212. doi: 10.1074/jbc.271.4.2206. [DOI] [PubMed] [Google Scholar]
- 123.Zhang S, Chang MC, Zylka D, Turley S, Harrison R, Turley EA. The hyaluronan receptor RHAMM regulates extracellular-regulated kinase. J Biol Chem. 1998;273:11342–11348. doi: 10.1074/jbc.273.18.11342. [DOI] [PubMed] [Google Scholar]
- 124.Florian MC, Geiger H. Concise review: polarity in stem cells, disease, and aging. Stem Cells. 2010;28:1623–1629. doi: 10.1002/stem.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ventura C, Maioli M, Asara Y, Santoni D, Scarlata I, Cantoni S, Perbellini A. Butyric and retinoic mixed ester of hyaluronan. A novel differentiating glycoconjugate affording a high throughput of cardiogenesis in embryonic stem cells. J Biol Chem. 2004;279:23574–23579. doi: 10.1074/jbc.M401869200. [DOI] [PubMed] [Google Scholar]
- 126.Ventura C, Cantoni S, Bianchi F, Lionetti V, Cavallini C, Scarlata I, Foroni L, Maioli M, Bonsi L, Alviano F, Fossati V, Bagnara GP, Pasquinelli G, Recchia FA, Perbellini A. Hyaluronan mixed esters of butyric and retinoic Acid drive cardiac and endothelial fate in term placenta human mesenchymal stem cells and enhance cardiac repair in infarcted rat hearts. J Biol Chem. 2007;282:14243–14252. doi: 10.1074/jbc.M609350200. [DOI] [PubMed] [Google Scholar]
- 127.Maioli M, Santaniello S, Montella A, Bandiera P, Cantoni S, Cavallini C, Bianchi F, Lionetti V, Rizzolio F, Marchesi I, Bagella L, Ventura C. Hyaluronan esters drive Smad gene expression and signaling enhancing cardiogenesis in mouse embryonic and human mesenchymal stem cells. PLoS One. 2010;5:e15151. doi: 10.1371/journal.pone.0015151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Simioniuc A, Campan M, Lionetti V, Marinelli M, Aquaro GD, Cavallini C, Valente S, Di Silvestre D, Cantoni S, Bernini F, Simi C, Pardini S, Mauri P, Neglia D, Ventura C, Pasquinelli G, Recchia FA. Placental stem cells pre-treated with a hyaluronan mixed ester of butyric and retinoic acid to cure infarcted pig hearts: a multimodal study. Cardiovasc Res. 2011;90:546–556. doi: 10.1093/cvr/cvr018. [DOI] [PubMed] [Google Scholar]
- 129.Lionetti V, Cantoni S, Cavallini C, Bianchi F, Valente S, Frascari I, Olivi E, Aquaro GD, Bonavita F, Scarlata I, Maioli M, Vaccari V, Tassinari R, Bartoli A, Recchia FA, Pasquinelli G, Ventura C. Hyaluronan mixed esters of butyric and retinoic acid affording myocardial survival and repair without stem cell transplantation. J Biol Chem. 2010;285:9949–9961. doi: 10.1074/jbc.M109.087254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cheng J, Türkel N, Hemati N, Fuller MT, Hunt AJ, Yamashita YM. Centrosome misorientation reduces stem cell division during ageing. Nature. 2008;456:599–604. doi: 10.1038/nature07386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cicalese A, Bonizzi G, Pasi CE, Faretta M, Ronzoni S, Giulini B, Brisken C, Minucci S, Di Fiore PP, Pelicci PG. The tumor suppressor p53 regulates polarity of self-renewing divisions in mammary stem cells. Cell. 2009;138:1083–1095. doi: 10.1016/j.cell.2009.06.048. [DOI] [PubMed] [Google Scholar]
- 132.Maioli M, Rinaldi S, Migheli R, Pigliaru G, Rocchitta G, Santaniello S, Basoli V, Castagna A, Fontani V, Ventura C, Serra PA. Neurological morphofunctional differentiation induced by REAC technology in PC12. A neuro protective model for Parkinson's disease. Sci Rep. 2015;5:10439. doi: 10.1038/srep10439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.McGuff PE, Deterling RA, Jr, Gottlieb LS. Tumoricidal effect of laser energy on experimental and human malignant tumors. N Engl J Med. 1965;273:490–492. doi: 10.1056/NEJM196508262730906. [DOI] [PubMed] [Google Scholar]
- 134.Maiman TH. Stimulated optical radiation in ruby. Nature. 1960;187:493–494. [Google Scholar]
- 135.Mester E, Ludany G, Selyei M, Szende B, Total J. The simulating effect of low power laser rays on biological systems. Laser Rev. 1968:1: 3. [Google Scholar]
- 136.Mester E, Szende B, Gärtner P. The effect of laser beams on the growth of hair in mice. Radiobiol Radiother (Berl) 1968;9:621–626. [PubMed] [Google Scholar]
- 137.Mester E, Mester AF, Mester A. The biomedical effects of laser application. Lasers Surg Med. 1985;5:31–39. doi: 10.1002/lsm.1900050105. [DOI] [PubMed] [Google Scholar]
- 138.Mester E, Nagylucskay S, Döklen A, Tisza S. Laser stimulation of wound healing. Acta Chir Acad Sci Hung. 1976;17:49–55. [PubMed] [Google Scholar]
- 139.Albrecht-Buehler G. Rudimentary form of cellular "vision". Proc Natl Acad Sci U S A. 1992;89:8288–8292. doi: 10.1073/pnas.89.17.8288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Albrecht-Buehler G. A long-range attraction between aggregating 3T3 cells mediated by near-infrared light scattering. Proc Natl Acad Sci U S A. 2005;102:5050–5055. doi: 10.1073/pnas.0407763102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang Y, Huang YY, Wang Y, Lyu P, Hamblin MR. Photobiomodulation (blue and green light) encourages osteoblastic-differentiation of human adipose-derived stem cells: role of intracellular calcium and light-gated ion channels. Sci Rep. 2016;6:33719. doi: 10.1038/srep33719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Venkatachalam K, Montell C. TRP channels. Annu Rev Biochem. 2007;76:387–417. doi: 10.1146/annurev.biochem.75.103004.142819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature. 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- 144.Wang L, Zhang D, Schwarz W. TRPV Channels in Mast Cells as a Target for Low-Level-Laser Therapy. Cells. 2014;3:662–673. doi: 10.3390/cells3030662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Martins D, Tavares I, Morgado C. "Hotheaded": the role OF TRPV1 in brain functions. Neuropharmacology. 2014;85:151–157. doi: 10.1016/j.neuropharm.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 146.Kumbalasiri T, Provencio I. Melanopsin and other novel mammalian opsins. Exp Eye Res. 2005;81:368–375. doi: 10.1016/j.exer.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 147.Terakita A. The opsins. Genome Biol. 2005;6:213. doi: 10.1186/gb-2005-6-3-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nussbaumer B, Kaminski-Hartenthaler A, Forneris CA, Morgan LC, Sonis JH, Gaynes BN, Greenblatt A, Wipplinger J, Lux LJ, Winkler D, Van Noord MG, Hofmann J, Gartlehner G. Light therapy for preventing seasonal affective disorder. Cochrane Database Syst Rev. 2015:CD011269. doi: 10.1002/14651858.CD011269.pub2. [DOI] [PubMed] [Google Scholar]
- 149.van Maanen A, Meijer AM, van der Heijden KB, Oort FJ. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med Rev. 2016;29:52–62. doi: 10.1016/j.smrv.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 150.Oldham MA, Ciraulo DA. Bright light therapy for depression: a review of its effects on chronobiology and the autonomic nervous system. Chronobiol Int. 2014;31:305–319. doi: 10.3109/07420528.2013.833935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wang Y, Huang YY, Wang Y, Lyu P, Hamblin MR. Red (660 nm) or near-infrared (810 nm) photobiomodulation stimulates, while blue (415 nm), green (540 nm) light inhibits proliferation in human adipose-derived stem cells. Sci Rep. 2017;7:7781. doi: 10.1038/s41598-017-07525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Leung MC, Lo SC, Siu FK, So KF. Treatment of experimentally induced transient cerebral ischemia with low energy laser inhibits nitric oxide synthase activity and up-regulates the expression of transforming growth factor-beta 1. Lasers Surg Med. 2002;31:283–288. doi: 10.1002/lsm.10096. [DOI] [PubMed] [Google Scholar]
- 153.Peplow PV. Neuroimmunomodulatory effects of transcranial laser therapy combined with intravenous tPA administration for acute cerebral ischemic injury. Neural Regen Res. 2015;10:1186–1190. doi: 10.4103/1673-5374.162687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Oron A, Oron U, Chen J, Eilam A, Zhang C, Sadeh M, Lampl Y, Streeter J, DeTaboada L, Chopp M. Low-level laser therapy applied transcranially to rats after induction of stroke significantly reduces long-term neurological deficits. Stroke. 2006;37:2620–2624. doi: 10.1161/01.STR.0000242775.14642.b8. [DOI] [PubMed] [Google Scholar]
- 155.Zhang L, Chen J, Li Y, Zhang ZG, Chopp M. Quantitative measurement of motor and somatosensory impairments after mild (30 min) and severe (2 h) transient middle cerebral artery occlusion in rats. J Neurol Sci. 2000;174:141–146. doi: 10.1016/s0022-510x(00)00268-9. [DOI] [PubMed] [Google Scholar]
- 156.Meyer DM, Chen Y, Zivin JA. Dose-finding study of phototherapy on stroke outcome in a rabbit model of ischemic stroke. Neurosci Lett. 2016;630:254–258. doi: 10.1016/j.neulet.2016.06.038. [DOI] [PubMed] [Google Scholar]
- 157.Lapchak PA, Salgado KF, Chao CH, Zivin JA. Transcranial near-infrared light therapy improves motor function following embolic strokes in rabbits: an extended therapeutic window study using continuous and pulse frequency delivery modes. Neuroscience. 2007;148:907–914. doi: 10.1016/j.neuroscience.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 158.Lampl Y, Zivin JA, Fisher M, Lew R, Welin L, Dahlof B, Borenstein P, Andersson B, Perez J, Caparo C, Ilic S, Oron U. Infrared laser therapy for ischemic stroke: a new treatment strategy: results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1) Stroke. 2007;38:1843–1849. doi: 10.1161/STROKEAHA.106.478230. [DOI] [PubMed] [Google Scholar]
- 159.Huisa BN, Stemer AB, Walker MG, Rapp K, Meyer BC, Zivin JA NEST-1 and -2 investigators. Transcranial laser therapy for acute ischemic stroke: a pooled analysis of NEST-1 and NEST-2. Int J Stroke. 2013;8:315–320. doi: 10.1111/j.1747-4949.2011.00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zivin JA, Albers GW, Bornstein N, Chippendale T, Dahlof B, Devlin T, Fisher M, Hacke W, Holt W, Ilic S, Kasner S, Lew R, Nash M, Perez J, Rymer M, Schellinger P, Schneider D, Schwab S, Veltkamp R, Walker M, Streeter J NeuroThera Effectiveness and Safety Trial-2 Investigators. Effectiveness and safety of transcranial laser therapy for acute ischemic stroke. Stroke. 2009;40:1359–1364. doi: 10.1161/STROKEAHA.109.547547. [DOI] [PubMed] [Google Scholar]
- 161.Oron A, Oron U, Streeter J, de Taboada L, Alexandrovich A, Trembovler V, Shohami E. low-level laser therapy applied transcranially to mice following traumatic brain injury significantly reduces long-term neurological deficits. J Neurotrauma. 2007;24:651–656. doi: 10.1089/neu.2006.0198. [DOI] [PubMed] [Google Scholar]
- 162.Wu Q, Xuan W, Ando T, Xu T, Huang L, Huang YY, Dai T, Dhital S, Sharma SK, Whalen MJ, Hamblin MR. Low-level laser therapy for closed-head traumatic brain injury in mice: effect of different wavelengths. Lasers Surg Med. 2012;44:218–226. doi: 10.1002/lsm.22003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Karu TI, Pyatibrat LV, Afanasyeva NI. Cellular effects of low power laser therapy can be mediated by nitric oxide. Lasers Surg Med. 2005;36:307–314. doi: 10.1002/lsm.20148. [DOI] [PubMed] [Google Scholar]
- 164.Ando T, Xuan W, Xu T, Dai T, Sharma SK, Kharkwal GB, Huang YY, Wu Q, Whalen MJ, Sato S, Obara M, Hamblin MR. Comparison of therapeutic effects between pulsed and continuous wave 810-nm wavelength laser irradiation for traumatic brain injury in mice. PLoS One. 2011;6:e26212. doi: 10.1371/journal.pone.0026212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Xuan W, Vatansever F, Huang L, Wu Q, Xuan Y, Dai T, Ando T, Xu T, Huang YY, Hamblin MR. Transcranial low-level laser therapy improves neurological performance in traumatic brain injury in mice: effect of treatment repetition regimen. PLoS One. 2013;8:e53454. doi: 10.1371/journal.pone.0053454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Xuan W, Agrawal T, Huang L, Gupta GK, Hamblin MR. Low-level laser therapy for traumatic brain injury in mice increases brain derived neurotrophic factor (BDNF) and synaptogenesis. J Biophotonics. 2015;8:502–511. doi: 10.1002/jbio.201400069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Xuan W, Vatansever F, Huang L, Hamblin MR. Transcranial low-level laser therapy enhances learning, memory, and neuroprogenitor cells after traumatic brain injury in mice. J Biomed Opt. 2014;19:108003. doi: 10.1117/1.JBO.19.10.108003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Dong T, Zhang Q, Hamblin MR, Wu MX. Low-level light in combination with metabolic modulators for effective therapy of injured brain. J Cereb Blood Flow Metab. 2015;35:1435–1444. doi: 10.1038/jcbfm.2015.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Naeser MA, Martin PI, Lundgren K, Klein R, Kaplan J, Treglia E, Ho M, Nicholas M, Alonso M, Pascual-Leone A. Improved language in a chronic nonfluent aphasia patient after treatment with CPAP and TMS. Cogn Behav Neurol. 2010;23:29–38. doi: 10.1097/WNN.0b013e3181bf2d20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Naeser MA, Zafonte R, Krengel MH, Martin PI, Frazier J, Hamblin MR, Knight JA, Meehan WP, 3rd, Baker EH. Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study. J Neurotrauma. 2014;31:1008–1017. doi: 10.1089/neu.2013.3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Henderson TA, Morries LD. SPECT Perfusion Imaging Demonstrates Improvement of Traumatic Brain Injury With Transcranial Near-infrared Laser Phototherapy. Adv Mind Body Med. 2015;29:27–33. [PubMed] [Google Scholar]
- 172.De Taboada L, Yu J, El-Amouri S, Gattoni-Celli S, Richieri S, McCarthy T, Streeter J, Kindy MS. Transcranial laser therapy attenuates amyloid-β peptide neuropathology in amyloid-β protein precursor transgenic mice. J Alzheimers Dis. 2011;23:521–535. doi: 10.3233/JAD-2010-100894. [DOI] [PubMed] [Google Scholar]
- 173.Saltmarche AE, Naeser MA, Ho KF, Hamblin MR, Lim L. Significant Improvement in Cognition in Mild to Moderately Severe Dementia Cases Treated with Transcranial Plus Intranasal Photobiomodulation: Case Series Report. Photomed Laser Surg. 2017;35:432–441. doi: 10.1089/pho.2016.4227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Maksimovich IV. Dementia and cognitive impairment reduction after laser transcatheter treatment of Alzheimer's disease. World J Neurosci. 2015;5:188–202. [Google Scholar]
- 175.Shaw VE, Spana S, Ashkan K, Benabid AL, Stone J, Baker GE, Mitrofanis J. Neuroprotection of midbrain dopaminergic cells in MPTP-treated mice after near-infrared light treatment. J Comp Neurol. 2010;518:25–40. doi: 10.1002/cne.22207. [DOI] [PubMed] [Google Scholar]
- 176.Purushothuman S, Nandasena C, Johnstone DM, Stone J, Mitrofanis J. The impact of near-infrared light on dopaminergic cell survival in a transgenic mouse model of parkinsonism. Brain Res. 2013;1535:61–70. doi: 10.1016/j.brainres.2013.08.047. [DOI] [PubMed] [Google Scholar]
- 177.Abstracts of the American Society for Laser Medicine and Surgery 30th Annual Conference. Phoenix, Arizona, USA. April 16-18, 2010. Lasers Surg Med Suppl. 2010;22:1–125. doi: 10.1002/lsm.20916. [DOI] [PubMed] [Google Scholar]
- 178.Blatt A, Elbaz-Greener GA, Tuby H, Maltz L, Siman-Tov Y, Ben-Aharon G, Copel L, Eisenberg I, Efrati S, Jonas M, Vered Z, Tal S, Goitein O, Oron U. Low-Level Laser Therapy to the Bone Marrow Reduces Scarring and Improves Heart Function Post-Acute Myocardial Infarction in the Pig. Photomed Laser Surg. 2016;34:516–524. doi: 10.1089/pho.2015.3988. [DOI] [PubMed] [Google Scholar]