Abstract
Medical cannabis has been touted as a solution to the US opioid overdose crisis since Bachhuber et al. [M. A. Bachhuber, B. Saloner, C. O. Cunningham, C. L. Barry, JAMA Intern. Med. 174, 1668–1673] found that from 1999 to 2010 states with medical cannabis laws experienced slower increases in opioid analgesic overdose mortality. That research received substantial attention in the scientific literature and popular press and served as a talking point for the cannabis industry and its advocates, despite caveats from the authors and others to exercise caution when using ecological correlations to draw causal, individual-level conclusions. In this study, we used the same methods to extend Bachhuber et al.’s analysis through 2017. Not only did findings from the original analysis not hold over the longer period, but the association between state medical cannabis laws and opioid overdose mortality reversed direction from −21% to +23% and remained positive after accounting for recreational cannabis laws. We also uncovered no evidence that either broader (recreational) or more restrictive (low-tetrahydrocannabinol) cannabis laws were associated with changes in opioid overdose mortality. We find it unlikely that medical cannabis—used by about 2.5% of the US population—has exerted large conflicting effects on opioid overdose mortality. A more plausible interpretation is that this association is spurious. Moreover, if such relationships do exist, they cannot be rigorously discerned with aggregate data. Research into therapeutic potential of cannabis should continue, but the claim that enacting medical cannabis laws will reduce opioid overdose death should be met with skepticism.
Keywords: medical cannabis, opioid overdose, public policy
A 2014 study by Bachhuber et al. (1) created a sensation by showing that state medical cannabis laws were associated with lower-than-expected opioid overdose mortality rates from 1999 to 2010. Cited by more than 350 scientific articles to date, the study attracted national and international media attention and was hailed by many activists and industry representatives as proof that expanding medical cannabis would reverse the opioid epidemic (1). Despite the authors’ cautions about drawing firm conclusions from ecological correlations, and similar warnings from other scientists (2), many such conclusions were drawn, to the point where medical cannabis has now been approved by several states as a treatment for opioid use disorder (3, 4). Subsequently published papers also found that cannabis access and indices of opioid-related harm were negatively correlated in the aggregate, with some attributing this less to medical cannabis laws per se than to increased access to any form of cannabis (including recreational) (5–7).
Given mounting deaths from opioid overdose, replicating the Bachhuber et al. (1) finding is a worthy task, especially in light of the changing policy landscape. Between 2010 and 2017, 32 states enacted medical cannabis laws, including 17 that allowed only medical cannabis with low levels of the psychoactive tetrahydrocannabinol (THC) and high levels of the nonpsychoactive component cannabidiol. Eight states enacted recreational cannabis laws during this period. Opioid overdose deaths have also increased dramatically over that time period (8). Using the same methods as Bachhuber et al. (1), we revisited the question with seven more years of data. To investigate how newer cannabis laws may be associated with changes in the association between cannabis laws and opioid overdose mortality, we also created a model with additional terms to account for presence of a recreational cannabis law or a low-THC restriction. Because none of the states with low-THC laws operate medical dispensaries and many limit access to a small number of indications, the levels of access can be approximated as highest for recreational, then “comprehensive” medical with dispensaries, and lowest for states with low-THC only. If broader access to cannabis writ large, rather than medical cannabis specifically, is the latent factor associated with lower opioid overdose mortality, we would expect to see the most negative association in states with recreational laws and the least negative association (or even positive) association in states with low-THC-only laws.
Results
For the original 1999–2010 time period, we obtained estimates similar to Bachhuber et al. (1), with slight differences likely due to missing values for 30 state/year combinations. Whereas Bachhuber et al. (1) estimated a 24.8% reduction in deaths per 100,000 population associated with a medical cannabis law’s introduction, we estimated a statistically indistinguishable 21.1% decrease. As in the original model, none of the four time-varying covariates (annual state unemployment rate and presence of the following: prescription drug monitoring program, pain management clinic oversight laws, and law requiring or allowing pharmacists to request patient identification) were significantly associated with opioid overdose mortality (Table 1). Using the full 1999–2017 dataset, we found that the sign reversed for medical cannabis laws, such that states passing a medical cannabis law experienced a 22.7% increase, 95% CI (2.0, 47.6) in overdose deaths. As an additional robustness test, we estimated models including state-specific linear time trends as well as state and year fixed effects. As with the analysis reported above, the sign of the effect of medical cannabis law switched from negative to positive once the data were extended to 2017; however, the magnitude was diminished and in neither specification was the estimate statistically significant.
Table 1.
Age-adjusted opioid overdose death rate per 100,000 population
| Independent variables | Bachhuber et al. (1999–2010) | Replication (1999–2010) | Extension (1999–2017) | Expanded model (1999–2017) |
| Medical cannabis law | −24.8 (−37.5 to −9.5) | −21.1 (−35.7, −3.0) | 22.7 (2.0, 47.6) | N/A |
| Prescription drug monitoring program | 3.7 (−12.7 to 23.3) | −2.8 (−16.7, 13.3) | −2.7 (−15.9, 12.5) | −4.0 (−17.1, 11.1) |
| Law requiring or allowing pharmacists to request patient identification | 5.0 (−10.4 to 23.1) | 2.8 (−12.6, 20.9) | 11.8 (−7.7, 35.5) | 8.8 (−10.2, 31.9) |
| Increased state oversight of pain management clinics | −7.6 (−19.1 to 5.6) | −6.9 (−18.4, 6.2) | 9.0 (−15.6, 40.8) | 13.7 (−11.2, 45.5) |
| Annual state unemployment rate | 4.4 (−0.3 to 9.3) | 4.4 (−0.3, 9.3) | 1.4 (−2.7, 5.5) | 0.7 (−3.1, 4.6) |
| Types of cannabis laws | ||||
| Recreational and medical cannabis law | N/A | N/A | N/A | −14.7 (−43.6, 29.0) |
| Medical cannabis only | N/A | N/A | N/A | 28.2 (1.2, 62.4) |
| Low-THC–only medical cannabis law | N/A | N/A | N/A | −7.1 (−29.1, 21.7) |
All models also included year and state fixed effects. N/A denotes not applicable because variable was not included in model.
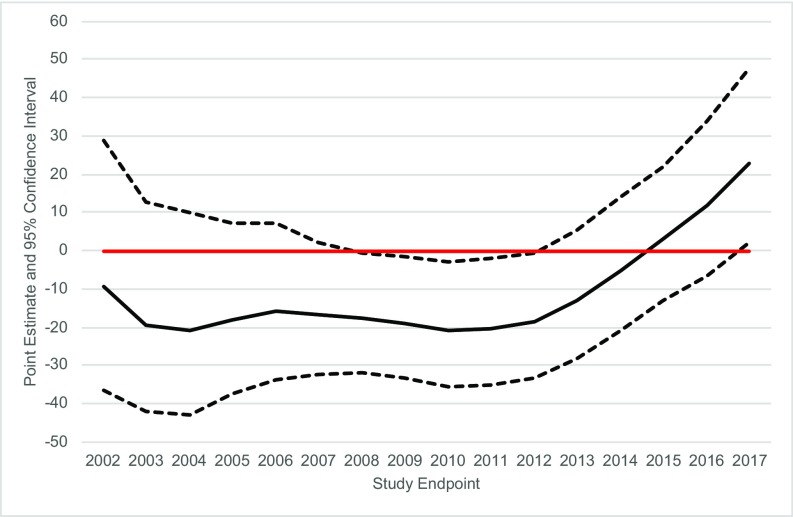
The direction of the association between medical cannabis laws and opioid overdose mortality was sensitive to the study’s endpoint (Fig. 1). For end dates between 2008 and 2012, the association was negative as reported in Bachhuber et al. (1). Subsequently, the association became statistically indistinguishable from zero before turning positive in 2017.
Fig. 1.
Changes in point estimate and 95% CI of association between medical cannabis law and age-adjusted opioid overdose death rate by the last year included in the analysis since 1999. Fixed (year and state) and time-varying effects (prescription drug monitoring program, state unemployment, pain management clinic oversight laws, and prescription drug identification laws) were also adjusted for.
In the expanded model with indicators for different types of cannabis laws, having a comprehensive medical cannabis law was associated with a 28.2%, 95% CI (1.2, 62.4) higher opioid overdose mortality, while estimates for other laws were nonsignificant. The association between having a recreational cannabis law and opioid overdose mortality was −14.7%, 95% CI (−43.6, 29.0). Having a low-THC-only medical cannabis law was associated with −7.1%, 95% CI (−29.1, 21.7) lower opioid overdose mortality. For both of these laws, the wide CIs include strong positive, strong negative, and null associations, indicating compatibility with a large range of true associations.
Discussion
We replicated Bachhuber et al.’s (1) finding of a negative association between medical marijuana and opioid overdose deaths from 1999 to 2010. However, the association did not hold when more extensive data through 2017 were analyzed. Had the analysis’ endpoint been between 2008 and 2012, the results would have been comparable to those obtained by Bachhuber et al. (1). However, the association became equivocal in 2013; by 2017 it had reversed such that a study conducted in that year might lead some to conclude that medical cannabis laws were compounding opioid overdose mortality.
The mechanism theorized to describe a causal relationship between medical cannabis laws and opioid overdose mortality rests on several premises: (i) Cannabis is more available in states with medical cannabis laws; (ii) people in these states substitute cannabis for opioids, whether for pain management, intoxication, or both; and (iii) this substitution occurs on a large enough scale to impact the population-level overdose mortality estimates. Under this model, states with highly restrictive medical cannabis laws limited to low-THC products would be expected to have a weaker association than states with comprehensive medical cannabis, while states with recreational cannabis would be expected to have a stronger association. Our results do not support this, as after adjusting for more and less restrictive types of cannabis law (recreational and medical or low-THC only), states with comprehensive medical cannabis laws still had a positive association with opioid overdose mortality.
The Bachhuber et al. (1) study is one of several that find the rate of cannabis access and some index of opioid-related harm are negatively correlated in the aggregate (1, 5–7). Policy that expands access to cannabis based on these findings assumes that (i) the same negative relationship is present at the individual level and (ii) the relationship is causal. The first conclusion is frequently incorrect across many research fields owing to the ecological fallacy (9). Ecological correlations cannot establish individual-level relationships and indeed may run in the directly opposite direction (e.g., higher rates of smoking in French regions with lower rates of esophageal cancer should not be interpreted as evidence of a protective effect of smoking) (10). In this case, compelling evidence exists that violates the first assumption: A study of a nationally representative sample of individuals shows that use of medical cannabis is positively correlated both with use and misuse of prescription pain relievers (11). This positive correlation does not at all prove that medical cannabis causes individuals to use opioids because correlation of nonexperimentally gathered data does not establish causation, a general principle that all parties to the current debate should bear in mind.
When multiple studies using similar methods generate a particular result, and for the first time one of those studies fails to replicate with more extensive data, there are multiple ways to explain the discrepancy. It could be that by bad luck the only one of those studies whose initial findings would not stand up to reanalysis with more recent data happened to be the one that was reexamined and every other similar study in that area would survive such an analysis (even though, as in this case, they explicitly build on the nonreplicated finding). However, we think a nonreplication should at least raise the possibility in the minds of scientists that the similar findings of other, similar studies in this area might also not replicate with a longer time series.
We are more cautious than others have been in drawing causal conclusions from ecological correlations and conclude that the observed association between these two phenomena is likely spurious rather than a reflection of medical cannabis saving lives 10 y ago and killing people today. Medical cannabis users are about 2.5% of the population, making it unlikely that they can significantly alter population-wide indices (12). Unmeasured variables likely explain both associations (e.g., state incarceration rates and practices, naloxone availability, and the extent of insurance and services) (2).
Our expanded analysis does not support the interpretation that broader access to cannabis is associated with lower opioid overdose mortality. The CIs for both recreational cannabis laws and low-THC laws are wide due to the comparatively small number of state/year combinations with these laws. Importantly, the CIs are compatible with a strong positive or strong negative correlation, as well as no correlation. Future estimates may be more precise (i.e., have narrower CIs) as data accumulate over time, and we caution scientists who conduct these analyses to note that, at present, states with recreational cannabis laws (Alaska, California, Colorado, Massachusetts, Maine, Oregon, Washington, Vermont, and the District of Columbia) form a group that is qualitatively different from the rest of the United States on a number of metrics that may confound estimates.
The nonrobustness of the earlier findings also highlights the challenges of controlling scientific messages in controversial policy areas. Corporate actors (e.g., the medical cannabis industry) with deep pockets have substantial ability to promote congenial results, and suffering people are desperate for effective solutions. Cannabinoids have demonstrated therapeutic benefits (13), but reducing population-level opioid overdose mortality does not appear to be among them.
Materials and Methods
Opioid analgesic overdose deaths were extracted from Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) and independent variables were obtained from the sources cited in the original paper and are included in the associated dataset for ref. 1. For rates with 95% CIs in CDC WONDER but no point estimate (those with 10 to 20 deaths in a state and year) we smoothed the data by averaging the confidence limits. Medical cannabis laws were coded as 0 for years preimplementation and 1 for years postimplementation. As applicable, we included a fraction for the year the law went into effect (e.g., 0.5 for a law implemented on July 1). A generalized linear model with robust standard errors was specified with year and state as fixed effects. We reviewed the legal literature to assess the effects of potential inaccuracies in the original sources (14); coefficient of the independent variable was insensitive to these differences. We ran the main model with end years from 2002 to 2017 and plotted the adjusted association. To assess the association between new cannabis laws implemented since 2010, we specified a model that included indicator variables for three kinds of cannabis laws: (i) presence of a recreational cannabis law and medical cannabis law, (ii) medical cannabis only with no restriction on THC content, and (iii) medical cannabis but only low-THC. Data are available in Dataset S1.
Supplementary Material
Acknowledgments
C.L.S. was supported by National Institute on Drug Abuse of the National Institutes of Health Award T32 DA035165 and the Wu Tsai Neurosciences Institute. K.H. was supported by a Senior Career Research Scientist Award from the Veterans Health Administration, Wu Tsai Neurosciences Institute, and the Esther Ting Memorial Professorship at Stanford University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the authors’ employers.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1903434116/-/DCSupplemental.
References
- 1.Bachhuber M. A., Saloner B., Cunningham C. O., Barry C. L., Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern. Med. 174, 1668–1673 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall W., et al. , It is premature to expand access to medicinal cannabis in hopes of solving the us opioid crisis. Addiction 113, 987–988 (2018). [DOI] [PubMed] [Google Scholar]
- 3.Humphreys K., Saitz R., Should physicians recommend replacing opioids with cannabis? JAMA 321, 639–640 (2019). [DOI] [PubMed] [Google Scholar]
- 4.New York State Department of Health , New York State Department of Health announces opioid replacement now a qualifying condition for medical marijuana. https://www.health.ny.gov/press/releases/2018/2018-07-12_opioid_replacement.htm. Accessed 24 February 2019.
- 5.Powell D., Pacula R. L., Jacobson M., Do medical marijuana laws reduce addictions and deaths related to pain killers? J. Health Econ. 58, 29–42 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradford A. C., Bradford W. D., Medical marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Aff. 36, 945–951 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Wen H., Hockenberry J. M., Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Intern. Med. 178, 673–679 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scholl L., Seth P., Mbabazi K., Wilson N., Baldwin G., Drug and opioid-involved overdose deaths, United States, 2013-2017. Morb. Mortal. Weekly Rep. 67, 1419–1427 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson W., Ecological correlations and the behavior of individuals. Am. Sociol. Rev. 15, 351–357 (1950). [Google Scholar]
- 10.Finney J. W., Humphreys K., Kivlahan D. R., Harris A. H., Why health care process performance measures can have different relationships to outcomes for patients and hospitals: Understanding the ecological fallacy. Am. J. Public Health 101, 1635–1642 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caputi T. L., Humphreys K., Medical marijuana users are more likely to use prescription drugs medically and nonmedically. J. Addict. Med. 12, 295–299 (2018). [DOI] [PubMed] [Google Scholar]
- 12.Caputi T. L., Medical marijuana, not miracle marijuana: Some well-publicized studies about medical marijuana don’t pass a reality check. Addiction 114, 1128–1129 (2019). [DOI] [PubMed] [Google Scholar]
- 13.National Academies of Sciences, Engineering, and Medicine , The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research (The National Academies Press, Washington, DC, 2017). [PubMed] [Google Scholar]
- 14.Horwitz J., Davis C. S., McClelland L. S., Fordon R. S., Meara E., The problem of data quality in analyses of opioid regulation: The case of prescription drug monitoring programs, NBER Working Paper 24947 (National Bureau of Economic Research, Cambridge, MA, 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.