Abstract
Background
Percutaneous atrial septal defect (ASD) closure carries a not negligible burden of complications, such as the erosion of cardiac structures surrounding the device. Complications related to erosion are rare and often occur during the first 6 months after implantation.
Case summary
A 40-year-old female patient underwent percutaneous ASD closure in 2006. After 12 years of uneventful follow-up, in March 2018, a device dislodgement causing atrial shunting was incidentally discovered and was attributed to device-induced atrial septal erosion. The patient successfully underwent surgical removal of the device and correction of the interatrial defect.
Discussion
Our purpose is to underline the importance of staged long-term imaging follow-up, even many years after a successful procedure and to highlight the possible risk factors leading to this worrisome condition. In addition, we sought to underline the possible risks associated with deficient aortic rim and explain pros and cons of different approaches.
Keywords: Atrial septal defect, Atrial septal erosion, Aortic rim, Septal occlude, Device dislodgement, Late complications, Case report
Learning points
A yearly diagnostic imaging follow-up should be always performed after successful atrial septal device closure over a very long-term period.
In case of deficient aortic rim, the straddling aorta technique should be considered as it could reduce the risk of subsequent septal erosion at the price of increasing the risk of aortic erosions. However, the surgical option should be considered in cases of very large or multi-perforated ASDs associated with deficient rims.
Introduction
Mounting evidence established atrial septal defect (ASD) percutaneous closure as the preferred strategy over surgery for ASD management, whenever the anatomy is favourable.
Noteworthy, ASD device closure carries a not negligible burden of complications, namely atrial fibrillation, haematoma at puncture site, device embolization, device-related erosion, and device thrombosis.
Erosions in surrounding cardiac structures are rare (0.2–0.3% of cases) after closure of ASDs and in most cases occur during the first 6 months after implantation.1 Nonetheless, late erosions, even many years after device implantation, have been described. Erosion of the atrial wall can lead to cardiac perforation with pericardial effusion and cardiac tamponade. Aortic erosion results in fistula formation.2 When the septum is eroded, this can cause device dislodgement and potential late embolization or recurrence of atrial shunting.
We present one of the few known latest cases of device dislodgment due to atrial septal erosion and subsequent development of shunting, 12 years after placement.
Timeline
| 2006 | The patient underwent percutaneous closure of an atrial septal defect. |
| Every year | The patient underwent cardiac ultrasonography to confirm the well placement of the device. |
| April 2017 | Last unremarkable cardiac ultrasonography. No shunt is present and the device is well placed. |
| March 2018: day of the admission (9 a.m.) | Incidental finding at transthoracic ultrasonography of severe shunt and atrial septal erosion. |
| Day of the admission (11 a.m.) | Transoesophageal ultrasound confirms this finding. |
| Day after the admission (4 p.m.) | The patient is brought to surgery. |
| Five days after the admission | The patient is discharged without complications. |
Case presentation
In 2006 a 40-year-old woman, whose medical history was unremarkable, except for sideropenic anaemia, was incidentally diagnosed an ASD at transthoracic echocardiography (TTE). The exam showed an ostium secundum ASD (2.1 × 1.7 cm in diameters) with severe left to right shunt (Qp/Qs = 2.1/1); moderate right atrium enlargement and increased pulmonary pressures (PAPs 35 mmHg) were documented. There was a good sized posterior atrial rim (15 mm), but only a 3.5 mm anterior aortic rim. The indications for closure in adults are echocardiographic finding of right ventricular volume overloading and/or catheterization findings of Qp:Qs greater than 1.5:1.0. Additional reasons are to prevent heart failure, prevent functional deterioration, improve myocardial function, and prevent paradoxical embolism. Therefore, after stretching balloon sizing, the patient underwent successful percutaneous ASD closure with a 34-mm Amplatzer Septal Occluder (Figure 1A), under intracardiac echo-guidance. Her clinical course was uneventful and adequate device positioning was confirmed by TTEs performed yearly, until April 2017.
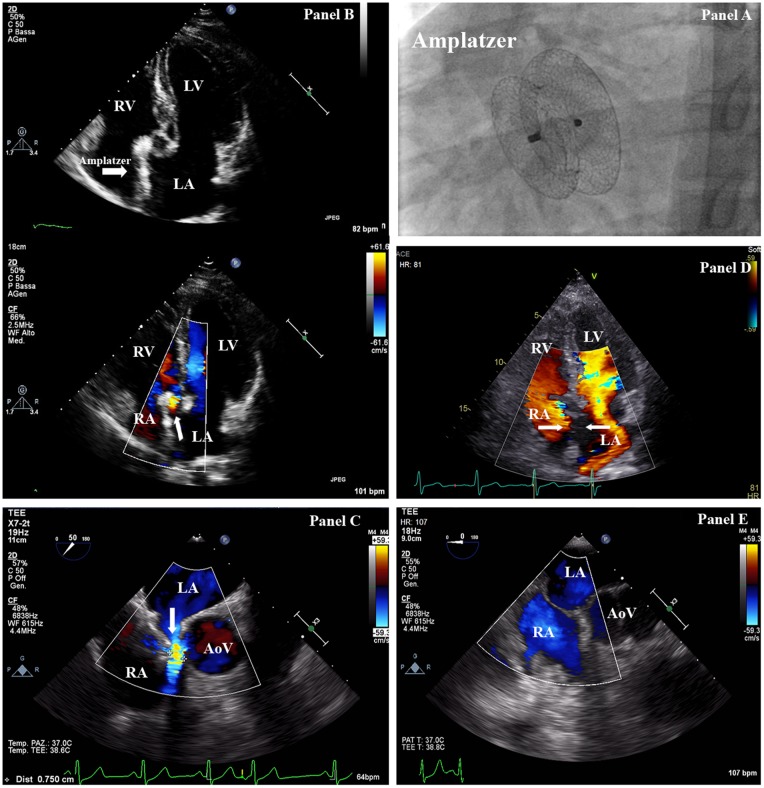
Figure 1.
(A) Fluoroscopy (antero-posterior projection) exhibiting correct placement of 34-mm Amplatzer Septal Occluder device. (B) Transthoracic echocardiography (four-chamber projection) showing malalignment of the septal occluder device (arrow) with the interatrial septum. (C) Transoesophageal echocardiography demonstrating left to right interatrial shunt. (D) Transoesophageal echocardiography after removal of the atrial septal defect septal occluder device and patch closure of the secundum atrial septal defect. AO, aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
In March 2018, 12 years after device implantation, the patient was evaluated for her annual TTE, fully healthy and asymptomatic. Her labs and physical examination were unremarkable. Her lungs were clear, she had no peripheral oedema and a soft mid-systolic murmur was detectable at the upper left sternal border with wide and fixed splitting of the second heart sound. At TTE, a displacement of the left disk to the right atrium at the retro-aortic rim was detected (Figure 1B, Supplementary material online, Video S1), causing severe left to right shunt (Qp/Qs = 1.7/1). This finding was confirmed by transoesophageal echocardiography (TOE) (Figure 1C, and Supplementary material online, Video S2). The patient was therefore referred to urgent surgery. The next day open surgery confirmed device dislodgement secondary to partial erosion of the aortic rim. Removal of the device and correction of the ASD with an autologous pericardial patch was then successfully performed. No shunt was evident thereafter at TOE (Figure 1D).
Discussion
This case demonstrates that late atrial septal occluder (ASO) device erosions can occur and cause late device dislodgement.
Our case illustrates the importance of a long-term follow-up after device implantation as late complications may occur. Erosions of the aortic wall and the atrial roof have been described previously.3,4 However, only few cases have been published demonstrating late erosions, mostly involving the atrial wall or the aortic wall.5 Our case is unique as it involves the atrial septum. Atrial septal erosion seems rare but could result in device dislodgement and possible device late embolization. The risk of device erosion with ASO is low and complications can be decreased by identifying high‐risk patients and following them closely. Patients with deficient aortic rim and/or superior rim may be at higher risk for device erosion. Another technical issue increasing the late risk of erosion is the ASO oversizing. Another possible explanation of the adverse event occurred, lays in overstretching the defect at the time of balloon sizing thus leading to a larger device size choice. Therefore, in these cases with a deficient aortic rim, an accurate heart team evaluation including the echocardiographist, the interventionalist, and the surgeon could better evaluate risks and benefits of both the percutaneous and the surgical procedure for a more appropriate decision making strategy.
This case illustrates the need for a thoroughly performed very long-term follow-up. The most accurate timing for a less frequent diagnostic follow-up has not yet been assessed and, according to our experience, should be carried on yearly. Together with a diagnostic echocardiographic follow-up, clinical patients evaluation focused on symptoms (i.e. dyspnoea on exertion, fatigue, and fainting) as well as new onset arrhythmias suggesting in- and out-flow disturbances should be considered.
The second interesting point arising from our case is how to approach ASD device closure when dealing with a deficient aortic rim. According to current literature, aortic straddling has to be achieved when aortic rim is deficient or absent, as it could reduce the risk of subsequent septal erosion at the price of increasing the risk of aortic erosion.6 In our case, no aortic straddling was evident at intracardiac ultrasonography evaluation at the time of device placement (Supplementary material online, Figure S1). This may be a possible explanation for the late erosion, as the constant motion of the device could cause damage to the septal rims.
Conclusion
Atrial septal defect closure-related complications rarely occur many years after implantation. However the long-term risk is not negligible and the clinician should never drop his guard down, even in asymptomatic patients.
Moreover, when dealing with deficient aortic rim, weight possible risks and benefits associated with the percutaneous technique compared to the surgical intervention.
Lead author biography

Marco Bergonti graduated in Medicine in 1992 and board in Cardiology at the University of Milan in 1997. She was a Visiting fellow in the Intravascular Ultrasound Laboratory, Catheterization Lab, Washington Hospital Center (1997-1998). In 1998 she becomes staff member of the Cath Lab at the Centro Cardiologico Monzino and she was elected as Chief of the Invasive Cardiology Unit at the same Institute in October 2017 and Director of the Women Heart Center, focused on cardiovascular prevention in women. She is teaching clinical cardiology at the postgraduate cardiology school, University of Milan. She is fellow of the European Society of Cardiology and American College of Cardiology.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Moore J, Hegde S, El-Said H, Beekman R, Benson L, Bergersen L, Holzer R, Jenkins K, Ringel R, Rome J, Vincent R, Martin G; ACC IMPACT Steering Committee . Transcatheter device closure of atrial septal defects: a safety review. JACC Cardiovasc Interv 2013;6:433–442. [DOI] [PubMed] [Google Scholar]
- 2. Tobis JM. Addressing the needs of treating congenital heart disease: the influence of deficient retro-aorticrim on technical success and early adverse events following device closure of secundum atrial septal defects: An analysis of the IMPACT registry®. Catheter Cardiovasc Interv 2017;89:112–113. [DOI] [PubMed] [Google Scholar]
- 3. Amin Z, Hijazi ZM, Bass JL, Cheatham JP, Hellenbrand WE, Kleinman CS.. Erosion of Amplatzer septal occluder device after closure of secundum atrial septal defects: review of registry of complications and recommendations to minimize future risk. Catheter Cardiovasc Interv 2004;63:496–502. [DOI] [PubMed] [Google Scholar]
- 4. Lapierre C, Hugues N, Dahdah N, Déry J, Raboisson MJ, Miró J.. Long-term follow-up of large atrial septal occluder (Amplatzer device) with cardiac MRI in a pediatric population. Am J Roentgenol 2012;199:1136–1141. [DOI] [PubMed] [Google Scholar]
- 5. Guelker JE, Jansen R, Sievert K, Sievert H, Bertog S.. Very late erosion of Amplatzer occluder device resulting in Cardiac tamponade after 15 years. Clin Res Cardiol 2018;107:527.. [DOI] [PubMed] [Google Scholar]
- 6. El-Said HG, Moore JW.. Erosion by the Amplatzer Septal Occluder: experienced operator opinions at odds with manufacturer recommendations? Cathet Cardiovasc Intervent 2009;73:925–930. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.