Abstract
Background
Atmospheric electrical discharge is an extremely powerful natural phenomenon which can have dangerous and lethal effects on the human body. However, there is no evidence to indicate whether and, if so, to what extent the electric current travelling through the body can affect proper pacemaker function.
Case summary
An 80-year-old patient admitted to emergency department after being struck by a lightning bolt while riding a bike. The patient had a DDD pacemaker implanted 4 years prior to the incident. The ECG on admission depicted pacemaker spikes and native sinus rhythm at 50–60 b.p.m. On the 3rd day after admission the patient developed recurrent pacing-induced tachycardia. Pacemaker interrogation showed high pacing thresholds (failure to pace in the atrial channel). When the patient’s condition stabilized she was transferred to the tertiary hospital for transcutaneous lead extraction. The extracted pacing system was sent to Biotronik for thorough evaluation.
Discussion
Injuries due to a lightning strike are considered a rare occurrence but being struck by lightning with a pacemaker or an ICD is even less common. In the present case, the cause of cardiac arrhythmia was most probably electrical burn at the endocardial-electrode interface and a sudden elevation of the pacing threshold leading to transient pacing failure in both PM channels. To the best of our knowledge, in this case presentation we first described permanent lightning-induced pacemaker dysfunction.
Keywords: Case report, Pacemaker, Transcutaneous lead extraction, Lightning, Lightning in pacemaker carrier , Lightning-induced takotsubo cardiomyopathy
Learning points
Dysfunction of PM due to being struck by lightning may be caused by an electrical damage of endocardial-electrode interface.
After being struck by lightning pacing system may require transvenous lead extraction due to its dysfunction.
Introduction
Atmospheric electrical discharge is an extremely powerful natural phenomenon which can have a devastating effect on the body, if not fatal. Mortality due to lightning is estimated to be 0.2–1.7 deaths per million people and it is the second leading cause of weather-related death.1 Lightning strikes can be associated with multi-organ injuries, involving mainly the skin and internal organs (such as the liver and gastrointestinal tract) getting in the way of the current flowing through the body.2–4 The most common cause of storm-related death are complications related to the cardiovascular system and the central nervous system.5–11 However, there is no evidence to indicate whether and, if so, to what extent the electric current travelling through the body can affect proper pacemaker function.
Timeline
| 5 years before the incident | Arterial hypertension, anterolateral myocardial infarction, PTCA of LAD wit bare metal stent implantation |
| 4 years before the incident | Implantation of a DDD pacemaker due to sinus node disease |
| The incident | Struck by lightning, admission to hospital with symptoms of shock. Lack of pacing in both pacemaker channels. DDD pacing with high impulse amplitude in both channels |
| 3 days after admission | Development of pacing-induced tachycardia (140–160 b.p.m.). Reprogramming from DDD to VVI pacing mode |
| 18 days after admission | Transfer to a tertiary centre for lead extraction |
| 19 days after admission | Transcutaneous lead extraction and a new DDD system implantation performed without complications |
| 24 days after admission | The patient was discharged home in good general condition |
| 2 years after discharge | The patient was contacted by telephone, she remained in good general condition |
Case presentation
We present a case of an 80-year-old woman who was struck by lightning. The past medical history included a diagnosis of arterial hypertension, coronary artery disease, anterolateral myocardial infarction 5 years earlier treated by primary coronary angioplasty of left anterior descending coronary artery with stent placement (bare metal stent), implantation of a DDD pacemaker 4 years earlier due to sick sinus syndrome (Talos DR, Biotronik; Selox JT53 endocardial lead in RAA and Selox ST 60 in RVA with passive fixation). She was struck by a lightning bolt while she was standing by a bike, with one hand resting on the handlebar and the other holding up an umbrella with a metal frame and a mobile phone (the patient does not remember in which hand she was holding the phone). As a result she experienced a transient loss of consciousness. The undamaged phone was found by a witness 10 m away from her and her wristwatch had stopped at the moment of strike. The patient in grave general condition with the symptoms of shock was admitted to the intensive care unit (ICU) of a district hospital. First- and second-degree burns were visible on a line going from the left shoulder along the entire torso to the lower right extremity (Figure 1). The ECG on admission depicted pacemaker spikes and native sinus rhythm at 50–60 b.p.m. (Figure 2). Vasopressors (dopamine and dobutamine) were used in the treatment of shock. Laboratory investigation revealed an increased level of hsTn to 640 pg/ml and NT-pro-BNP to 1557 pg/ml. Levels of electrolytes, creatinine, urea, and aminotransferases were within normal limits. Bedside echocardiogram examination in the ICU with the diagnostic conclusion of ‘very poor contractility’. Pacemaker interrogation showed high pacing thresholds (failure to pace in the atrial channel) even if impulse energy was increased. On the 3rd day after admission the patient developed recurrent pacing-induced tachycardia at rates of 140–160 b.p.m. (Figure 2). The pacing mode was then changed to VVI. The symptoms of shock disappeared and the patient gradually improved. When the patient’s condition stabilized [ejection fraction (EF) was over 40%] she was transferred to the tertiary hospital for transcutaneous lead extraction (TLE). At 10 days after the index event she was in good general state, with burn wounds still not healed, especially in the region of the right nipple and the right thigh. Pacemaker interrogation revealed slightly elevated pacing thresholds of both leads (∼3.5 V with 1.0 ms impulse duration). Pacemaker memory data had been entirely erased upon lightning strike and during the consecutive programming changes. TLE was performed at 19 days after the strike. In the hybrid operating room with on-site cardiac surgery standby, the pacing system was removed from the patient under general anaesthesia using Cook mechanical telescoping sheaths under the guidance of transoesophageal echocardiography (TOE).
Figure 1.
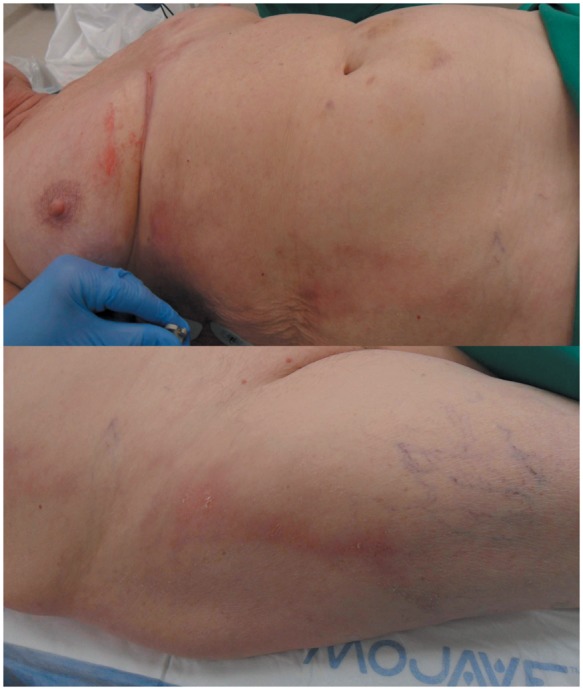
First- and second-degree burns were visible on a line going from the left shoulder along the entire torso to the lower right extremity.
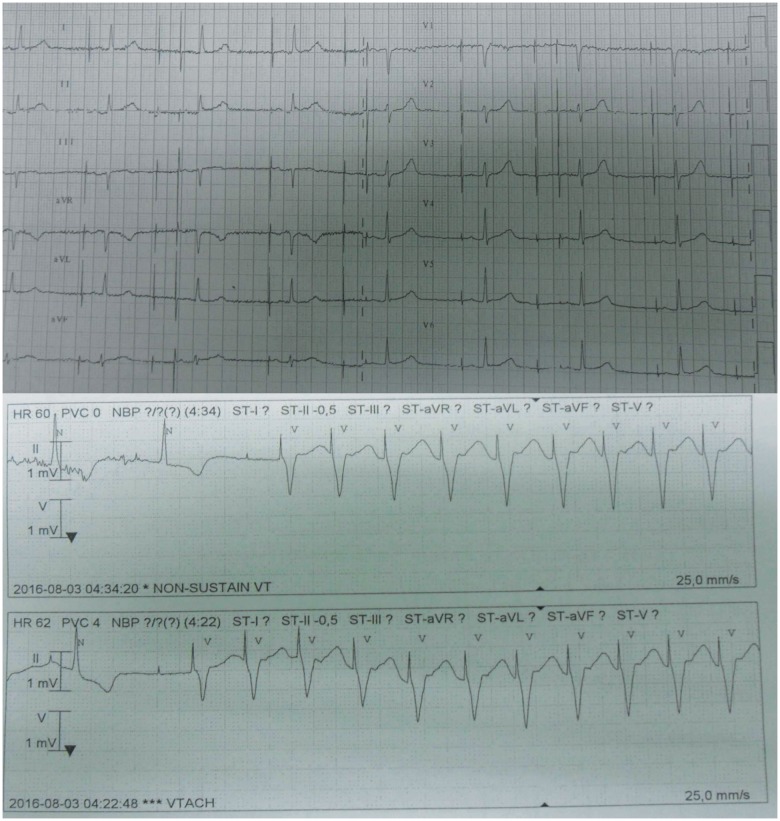
Figure 2.
The ECG on admission depicted pacemaker spikes and native sinus rhythm at 50–60 b.p.m. On the 3rd day after admission the patient developed recurrent pacing-induced tachycardia at the rates of 140–160 b.p.m.
Pre-procedural ECHO examination showed an EF of 55% without significant abnormalities in the heart. TOE imaging during the procedure did not show any pathologic structures on pacemaker leads. The extracted pacing system was sent to Biotronik (Germany) for thorough evaluation. At the same time the patient received a new DDD unit (Figure 3). Deep vein thrombosis of the left upper extremity developed after the procedure. The patient was treated with low molecular weight heparin and arm elevation and a few days later the symptoms of thrombosis resolved. The further post-operative course was uneventful and at 24 days after the index event she was discharged home in good general condition. Pre-discharge ECHO examination showed an EF of 60% and no morphological abnormalities in the heart. A follow-up phone call revealed that the patient was still doing well until the day of preparation of the manuscript for publication (exactly 2 years ago).
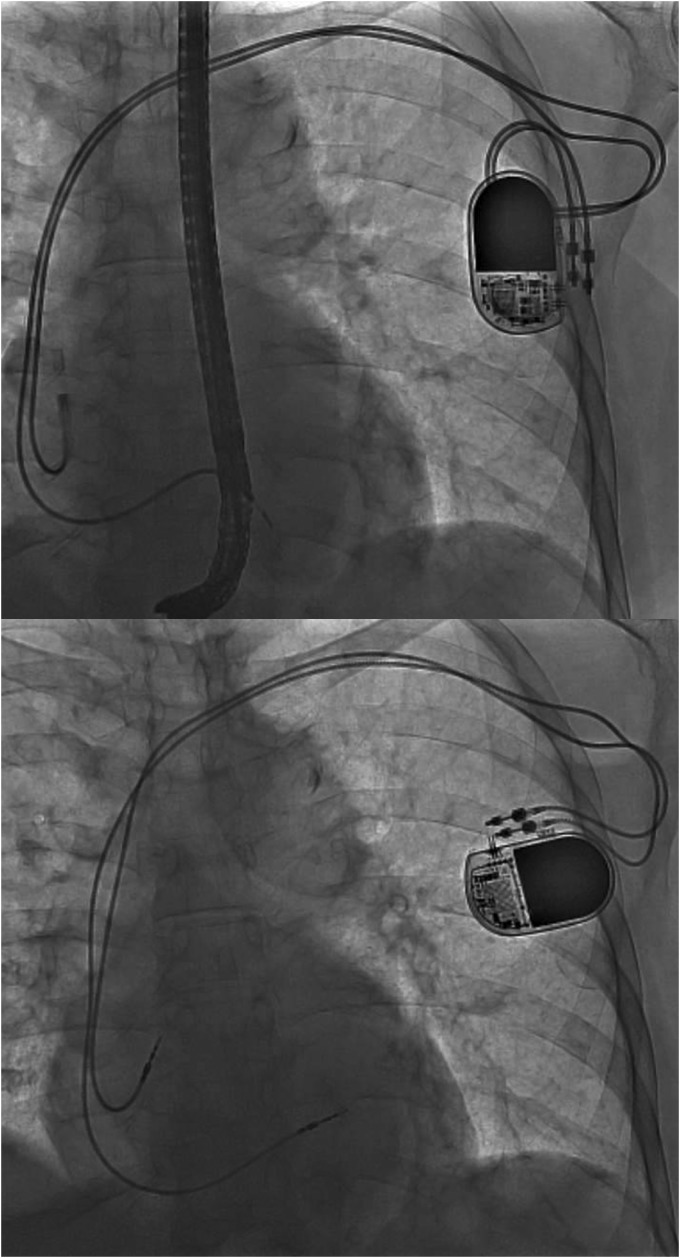
Figure 3.
The old and a new DDD pacing system (before and after replacement of the whole system).
The manufacturer’s (Biotronik) evaluation of the device did not show any significant damage either to the pacemaker or the extracted leads. Pacemaker battery status was as expected. Evaluation of the pacemaker memory did not show any abnormalities. The ability of the device to pace was checked. Antibradycardia pacing capabilities were in accordance with the programmed criteria, there were no changes with respect both to amplitude and rate. Pacemaker function was found to be normal. A long-term test to check for pacing ability was additionally performed. Every pacing impulse was recorded during the test. An in-depth analysis of the recorded pacing impulses confirmed normal pacemaker function. No temporary or permanent loss of capacity of the battery was noted. The pacemaker appeared to function properly. There were no deviations from technical standard. The extracted leads also conformed to the technical specification. By signing the consent form the patient agreed to use her anonymous medical data for research purposes and publication.
Discussion
Injuries due to a lightning strike are considered a rare occurrence but being struck by lightning with a pacemaker or an ICD is even less common.12,13
Cardiac manifestations in patients with storm-related injuries may include asystole, followed by sinus tachycardia, atrial fibrillation, although ventricular tachycardia and ventricular fibrillation are equally probable.6–11 Other complications are associated with transient regional wall motion abnormalities to a varying degree.9 Burns after lightning strikes are typical and occur at the border between dry and wet skin and around metal items in the clothes.14 In our patient it was a metal part of her bra.
In the present case, the cause of cardiac arrhythmia was most probably electrical burn at the endocardial-electrode interface and a sudden elevation of the pacing threshold leading to transient pacing failure in both PM channels. An increase in impulse amplitude resulted in paced ventricular beats and secondary endless loop tachycardia. Because endocardial injury under the electrode was irreversible, it was necessary to remove the lead. In our patient shock after being struck by lightning could have resulted from left ventricular dysfunction and takotsubo cardiomyopathy.
To the best of our knowledge, in this case presentation we first described permanent lightning-induced pacemaker dysfunction.
Lead author biography

Dr Bogdan Obszaijki graduated from Collegium Medicum of The Jagiellonian University in Krakow. He specialized in Internal Medicine and Cardiology. Dr Obszaijki is employed as senior assistant in the cardiology ward of The Pope John Paul II Hospital in Zamosc. For many years his main areas of work have been heart stimulation and lead extraction. The institution, Dr Obszaijki is employed in, is the largest lead extraction center in Poland where around 300 procedures of this type are performed every year.
Supplementary Material
Funding
All interventions and lab test were done in The Pope John Paul II Province Hospital of Zamosc. The Pope John Paul II Province Hospital of Zamosc provided all funding.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
References
- 1. Sumangala CN, Pradeep Kumar MP.. Lightning death: a case report. J Indian Acad Forensic Med 2015;37:93–95. [Google Scholar]
- 2. Pedersen ML, Uslu B, Lind MN, Carl P.. Survival following lightning strike and treatment of sequelae. Ugeskr Laeger 2011;173:1138–1139. [PubMed] [Google Scholar]
- 3. Eyerly-Webb S, Solomon R, Lee S, Sanchez R, Carrillo E, Davare D, Kiffin C, Rosenthal A.. Lightning burns and electrical trauma in a couple simultaneously struck by lightning. Clin Pract Cases Emerg Med 2017;1:246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fahmy FS, Brinsden MD, Smith J, Frame JD.. Lightning: the multisystem group injuries. J Trauma 1999;46:937–940. [DOI] [PubMed] [Google Scholar]
- 5. Alyan O, Ozdemir O, Tufekcioglu O, Geyik B, Aras D, Demirkan D.. Myocardial injury due to lightning strike-a case report. Angiology 2006;57:219–223. [DOI] [PubMed] [Google Scholar]
- 6. Saglam H, Yavuz Y, Yurumez Y, Ozkececi G, Kilit C.. A case of acute myocardial infarction due to indirect lightning strike. J Electrocardiol 2007;40:527–530. [DOI] [PubMed] [Google Scholar]
- 7. Lichtenberg R, Dries D, Ward K, Marshall W, Scanlon P.. Cardiovascular effects of lightning strikes. J Am Coll Cardiol 1993;21:531–536. [DOI] [PubMed] [Google Scholar]
- 8. McIntyre WF, Simpson CS, Redfearn DP, Adbollah H, Baranchuk A.. The lightning heart: a case report and brief review of the cardiovascular complications of lightning injury. Indian Pacing Electrophysiol J 2010;10:429–434. [PMC free article] [PubMed] [Google Scholar]
- 9. Dundon BK, Puri R, Leong DP, Worthley MI.. Takotsubo cardiomyopathy following lightning strike. BMJ Case Reports 2009;2009:bcr0320091646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Altalhi A, Al-Manea W, Alqweai N, Alothman M.. Cardiac rhythm recorded by implanted loop recorder during lightning strike. Ann Saudi Med 2017;37:401–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, Jeejeebhoy FM, Gabrielli A.. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S829–S861. [DOI] [PubMed] [Google Scholar]
- 12. Anderson DR, Gillberg JM, Torrey JW, Koneru JN.. Lightning induced inappropriate ICD shock: an unusual case of electromagnetic interference. Pacing Clin Electrophysiol 2012;35:e159–e162. [DOI] [PubMed] [Google Scholar]
- 13. Kondur AK, Afonso LC, Berenbom LD, Lakkireddy DR.. Implantable cardioverter defibrillators save lives from lightning-related electrocution too! Pacing Clin Electrophysiol 2008;31:256–257. [DOI] [PubMed] [Google Scholar]
- 14. Herrero F, Garcia-Morato V, Salinas V, Alonso S.. An unusual case of lightning injury: a melted silver necklace causing a full thickness linear burn. Burns 1995;21:308–309. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.