Abstract
Objective:
Dietary restraint refers to an individual’s intention to restrict food intake, measured via self-report questionnaires, whereas dietary restriction refers to actual reduction in caloric intake. The aim of this research was to investigate the association between dietary restraint scales and actual caloric restriction.
Method:
Data were collected from six previously published or two ongoing eating behavior studies in which participants (n = 183) completed the Three Factor Eating Questionnaire (TFEQ) and Eating Disorders Examination Questionnaire (EDE-Q) and participated in a laboratory-based research lunch meal. Participants were individuals with anorexia nervosa (AN), bulimia nervosa (BN), and healthy controls (HC). The primary analysis was the association between TFEQ Restraint subscale and caloric intake in the meal.
Results:
There was a significant negative correlation between total caloric intake and TFEQ Restraint scores (r = −.60, p < .001) and EDE-Q Restraint scores (r = −.54, p < .001). For TFEQ Restraint score, this relationship was significant within each diagnostic group (HC: r = −.32, p = .007; AN: r = −.38, p < .001; BN: r = −.43, p = .02).
Discussion:
These results suggest that the TFEQ Restraint scale is a useful measure of dietary restriction, especially among individuals with eating disorders.
Keywords: anorexia nervosa, bulimia nervosa, caloric restriction, dietary restraint, eating disorders
1 |. INTRODUCTION
Caloric restriction is a salient feature of eating disorders. This is most prominent in anorexia nervosa (AN) where the phrase, “restriction of energy intake relative to requirements,” begins the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) diagnostic criteria (American Psychiatric Association, 2013). Studies of eating behavior in bulimia nervosa (BN) have also shown that patients are prone to consuming fewer calories in a non-binge meal than healthy peers (Walsh, 2011). Dietary restraint differs from caloric restriction in that it refers to the intention to restrict the amount eaten for the purposes of maintaining or achieving a desired weight (Schaumberg & Anderson, 2016). Elevated dietary restraint has also been noted among individuals with eating disorders. How this cognitive measure of intent to restrict relates to actual restrictive eating is an empirical question the present study aimed to answer by comparing self-reported restraint with actual food intake in a laboratory meal among individuals with and without eating disorders.
Several instruments measure dietary restraint. Among the first historically was the Restraint Scale, a self-report instrument developed by Herman and Mack in 1975 (Herman & Mack, 1975) to identify chronic dieters. In an initial study, individuals who scored higher on the scale paradoxically consumed more ice cream after a milkshake preload, whereas individuals who scored lower consumed less ice cream. These counterintuitive findings provided support for their theory that individuals who exhibit high restraint may be more vulnerable to uncontrolled eating when restraint is abandoned. However, several shortcomings of the Restraint Scale were noted, including confounding of restraint with disinhibition and failure to predict behavior in obese individuals (Heatherton, Herman, Polivy, King, & McGree, 1988). Several other self-report scales were subsequently developed in hopes of addressing these limitations, including the Three Factor Eating Questionnaire (TFEQ; [Stunkard & Messick, 1985]), the Eating Disorder Examination Questionnaire (EDE-Q; [Fairburn, 2008]), and the Dutch Eating Behavior Questionnaire (Van Strien, Frijters, Bergers, & Defares, 1986).
It has been suggested that these scales, especially the TFEQ, may better identify individuals who can successfully restrict calories, while the Restraint Scale may be more likely to identify those who engage in relatively unsuccessful dieting (Heatherton et al., 1988; Laessle, Tuschl, Kotthaus, & Pirke, 1989). The TFEQ was designed to assess three parameters related to eating behavior: cognitive restraint of eating, disinhibition, and hunger. In a study of 103 women, those who scored higher on the TFEQ-Restraint scale (TFEQ-R) reported lower total caloric intake and less frequent consumption of sweets compared to women with lower TFEQ-R scores over a 6-month period (French, Jeffery, & Wing, 1994). In contrast, women who scored higher on the Restraint Scale in this study did not differ significantly on any measure of dietary intake from women who scored lower.
While numerous studies have found a relationship between restraint scales and self-reported intake (French et al., 1994; Moreira, de Almeida, & Sampaio, 2005; Neumark-Sztainer, Jeffery, & French, 1997; Van Strien, Frijters, Van Staveren, Defares, & Deurenberg, 1986; Wardle & Beales, 1987), the results of studies assessing the relationship between restraint and objectively measured food intake have not been consistent. The majority of such studies among healthy controls (HC) have found non-significant relationships between dietary restraint and total caloric intake (Anderson, Reilly, Schaumberg, Dmochowski, & Anderson, 2016; Bathalon et al., 2000; de Witt Huberts, Evers, & de Ridder, 2013; Epstein et al., 2004; Jansen, 1996; Jansen et al., 2003; Martin et al., 2005; Ouwens, van Strien, & van der Staak, 2003; Rolls et al., 1997; Stice, Cooper, Schoeller, Tappe, & Lowe, 2007; Stice, Fisher, & Lowe, 2004; Stice, Sysko, Roberto, & Allison, 2010; Sysko, Walsh, & Wilson, 2007). In the few studies that did detect a significant relationship, the amount of variance explained was generally small. Furthermore, although some studies found the intuitively expected inverse relationship between restraint and intake (Greenwood, Broadbent, & Fuller-Tyszkiewicz, 2014; Rideout, McLean, & Barr, 2004; Schoch & Raynor, 2012; Stice et al., 2004, 2010) other studies found a positive relationship (Jansen et al., 2009; Wardle & Beales, 1987).
Only three prior studies of restraint scales have included individuals with eating disorders and BED has been represented most prominently. In the first study (Stice et al., 2004), 151 participants, including 32 patients with BN, 60 patients with binge eating disorder (BED), and 59 healthy controls completed the TFEQ-R and EDEQ-R and participated in a laboratory breakfast consisting of cereal, fruit, a bread roll, and decaffeinated tea or coffee. The authors found no significant correlation between dietary restraint and caloric intake. The relatively limited foods provided during the laboratory meal may have restricted the range of eating behaviors, limiting the ability to detect an association; alternatively, a breakfast meal may be less prone to promoting restrictive food intake. In a later paper from this group (Stice et al., 2010), data from two studies were compiled to include 44 women with overweight or obesity (25 with BED and 19 with obesity) and 17 normal weight women, and caloric intake at a normal meal and a binge-instruction meal were averaged. The authors found a quadratic relationship between TFEQ restraint scores and caloric intake; those with highest and lowest restraint scores consumed fewest calories. These results again suggest that a different pattern between restraint and intake may emerge when binge eating occurs. Sysko, Walsh, Schebendach, and Wilson (2005) included 12 patients with AN before and after weight restoration in addition to 12 HC. None of the restraint scores measured (Dietary Intent Scale, TFEQ, EDE, and EDE-Q) were significantly correlated with intake in the laboratory meal that consisted of a strawberry yogurt shake. In this small study, participants were only offered one food item and the type and quantity of food were concealed. The meal was associated with high anxiety and very limited intake. Restraint was not a primary variable in this study and the design may have limited the ability to examine the relationship with intake.
The paucity of studies among patients with eating disorders (especially in AN and BN) (Stice et al., 2004, 2010; Sysko et al., 2005), small sample sizes, and mixed findings to date warrant additional research into this topic. Therefore, we conducted a retrospective analysis pooling data from eight studies, some previously published and some ongoing, in which dietary restraint was assessed and caloric intake in a laboratory meal was measured. Participants included individuals with AN and BN, in addition to HC across a weight spectrum. Our primary aim was to assess the relationship between the TFEQ-R and caloric intake. We hypothesized that TFEQ-R would be inversely related to caloric intake. Secondarily, we investigated the relationship between restraint scores on the EDE-Q Restraint scale (EDE-Q-R) and caloric intake, and explored associations with other subscales of the TFEQ, to assess whether relationships were specific to the restraint component of the TFEQ.
2 |. METHOD
2.1 |. Participants
Participants were 183 individuals who participated in one of six previously published (Foerde, Steinglass, Shohamy, & Walsh, 2015; Gianini et al., 2015; Mayer, Schebendach, Bodell, Shingleton, & Walsh, 2012; Steinglass et al., 2014, 2018; Sysko et al., 2017) or two ongoing eating behavior studies at the Columbia Center for Eating Disorders at the New York State Psychiatric Institute (NYSPI): 81 women and two men with AN, 30 women with BN, and 69 female and one male HC. HC were individuals with no current or prior eating disorder and included normal weight non-dieters, as well as those who endorsed dieting, and obese individuals, as well as individuals who had lost at least 30 lbs. (maintained for at least 12 months). Diagnosis was established via Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Janet, 1998), Eating Disorders Examination (Fairburn & Cooper, 1993) and/or Eating Disorders Assessment-5 (Sysko et al., 2015). The parent studies included the baseline assessment from two pilot interventional studies (Steinglass et al., 2014; Steinglass et al., 2018). Details available in prior publications.
2.2 |. Procedures
In each study, participants completed the TFEQ and EDE-Q and participated in a laboratory-based research lunch meal. Timing of administration of the TFEQ was not standardized. Laboratory meals consisted of either a multi-item meal (six studies) or a modified multi-item meal (two studies). All studies were approved by the Institutional Review Board of NYSPI and all participants provided written informed consent.
2.2.1 |. Laboratory meal
Participants consumed a standardized breakfast (~300 kcal) at 8 a.m. and did not eat or drink anything until the study lunch, which was at 1 p.m. for the multi-item meal and noon for the modified multi-item meal (Sysko, Steinglass, Schebendach, Mayer, & Walsh, 2018). All test meals occurred in the eating behavior laboratory at the Biological Studies Unit of NYSPI. For both meal types, participants were provided with a range of food options on a table. Each food item was weighed before and after the meal. Caloric intake was calculated based on grams consumed and the caloric density of the food item. Participants were instructed: “This is your lunch for today. Eat as much or as little as you like,” and to indicate when they were finished by ringing a bell on the table.
The multi-item meals included a range of foods of varying caloric and fat content, including items like: grilled chicken, fried chicken, tuna, white and wheat bread, macaroni and cheese, salad, pickles, chocolate sandwich cookies, ice cream, donuts, candy, fruit salad, condiments, water, diet cola, and iced tea (specific foods available varied slightly across studies). The modified multi-item meal (Gianini et al., 2015; Steinglass et al., 2014) consisted of a turkey submarine sandwich (600 kcal), a large bowl of potato chips (455 kcal), a jar of mayonnaise, and an 8 oz. bottle of water.
2.3 |. Instruments
2.3.1 |. Three Factor Eating Questionnaire (TFEQ)
The TFEQ is a valid and reliable 51-item self-report questionnaire assessing eating disorder symptoms in three domains: Cognitive Restraint of Eating, Disinhibition, and Hunger (Stunkard & Messick, 1985). A series of statements are rated either 0 or 1, with higher scores indicating greater eating disorder symptom severity. Internal consistency has been reported as Cronbach’s α > 0.7 (Cappelleri et al., 2009; Mostafavi et al., 2017).
2.3.2 |. The Eating Disorder Examination-Questionnaire (EDE-Q)
EDE-Q is a 36-item assessment of eating disorder symptoms, including number of objective and subjective bulimic episodes in the prior month (Fairburn & Beglin, 1994). The EDE-Q scores four symptom subscales on a scale of 0–6: Restraint, Eating Concern, Shape Concern, and Weight Concern. To obtain an overall “global” score, the subscales are averaged. The EDE-Q has established community norms for adolescents and adults. Internal consistency has been reported as Cronbach’s α > 0.8 (Luce & Crowther, 1999; Reas, Grilo, & Masheb, 2006).
2.4 |. Data analysis
Means and SDs were calculated for demographic and clinical variables, including age, BMI, TFEQ, EDE-Q, and caloric intake. One-way analysis of variance (anova) was used to compare differences between groups.
Association between TFEQ subscales and caloric intake was examined using Pearson correlation coefficients in the whole sample and within each diagnostic group after excluding binge meals (defined as consuming >2000 kcal, n = 5). Linear regression was used to assess the effect of meal type. Similar analyses were used to examine the association between the EDE-Q-R subscale and caloric intake. Analyses were repeated with binge meals included. Statistical analyses were performed with SPSS for Windows, version 24.0 (SPSS Inc., Chicago, IL). Significance level was set at .05. Our primary hypothesis was that the score on the TFEQ-R subscale would be inversely associated with caloric intake at the laboratory meal. We did not correct for multiple comparisons in the exploratory analyses.
3 |. RESULTS
Means and SDs of demographic and clinical variables are reported in Table 1. Age did not differ significantly among groups. As expected, BMI differed significantly. Among the patients with AN, 42 (50.6%) had restricting subtype and 41 (49.4%) had binge-eating/purging subtype. There were significant differences between groups in all TFEQ and EDE-Q scores and in caloric intake.
TABLE 1.
Demographic and clinical characteristics of participants. Groups with the same superscript (a and/or b) differ significantly in post-hoc Tukey HSD tests
| Healthy control (n = 70) | Anorexia nervosa (n = 83) | Bulimia nervosa (n = 30) | ||
|---|---|---|---|---|
| Age (years) | 27.31 ± 9.53 | 27.48 ± 8.36 | 25.07 ± 5.51 | F2,180 = 0.97, p = 0.38 |
| BMI (kg/m2) | 22.60 ± 3.00a | 16.93 ± 2.37a,b | 21.76 ± 2.47b | F2,180 = 96.3, p < 0.001 |
| TFEQ-Restraint | 6.28 ± 4.45a | 17.04 ± 3.83a | 13.70 ± 4.36a | F2,179 = 127.7, p < 0.001 |
| TFEQ-Disinhibition | 3.29 ± 2.33a | 6.07 ± 4.43a | 13.17 ± 1.86a | F2,179 = 87.9, p < 0.001 |
| TFEQ-Hunger | 3.36 ± 2.47a | 5.07 ± 3.78a | 8.57 ± 2.89a | F2,179 = 8.0, p < 0.001 |
| EDE-Q Restraint | 0.62 ± 1.12a | 4.29 ± 1.68a | 3.30 ± 1.24a | F2,163 = 120.3, p < 0.001 |
| EDE-Q Eating Concern | 0.12 ± 0.29a,b | 3.74 ± 1.43a | 3.61 ± 1.26b | F2,163 = 216.7, p < 0.001 |
| EDE-Q Weight Concern | 0.52 ± 0.91a,b | 4.50 ± 1.52a | 4.01 ± 1.58b | F2,163 = 165.9, p < 0.001 |
| EDE-Q Shape Concern | 0.58 ± 1.04a,b | 4.73 ± 1.35a | 4.45 ± 1.28b | F2,163 = 218.1, p < 0.001 |
| Caloric intake (kcal)* | 784 ± 279a | 389 ± 259a | 542 ± 413a | F2,175 = 33.1, p < 0.001 |
Note. BMI = body mass index; TFEQ = Three-Factor Eating Questionnaire; EDE-Q = Eating Disorder Examination Questionnaire.
Data are missing for: one HC for TFEQ; four HC and 13 AN for EDE-Q Restraint and EDE-Q Eating; five HC and 14 AN for EDE-Q Weight and EDE-Q Shape.
Caloric intake is reported with binge meals excluded. Tukey HSD test indicated significant differences between all groups.
There was a significant negative correlation between TFEQ-R and caloric intake (r = −0.598, p = <0.001). Associations were significant within each diagnostic group, as well as the total sample (Figure 1). Regression analysis (including diagnosis, TFEQ-R and modified vs. non-modified multi-item meal type) indicated that meal type did not have a significant effect on caloric intake (Beta = −201.6 ± 122.5 SE, p = 0.10). In linear regression analysis (including caloric intake, TFEQ-R, and time between TFEQ and MIM), the time between TFEQ administration and the MIM did not approach statistical significance (Beta = 0.267 ± 1.12 SE, p = 0.881). There was a significant association between EDE-Q-R and caloric intake across the total sample and within the AN group, though not within the other groups (Table 2).
FIGURE 1.
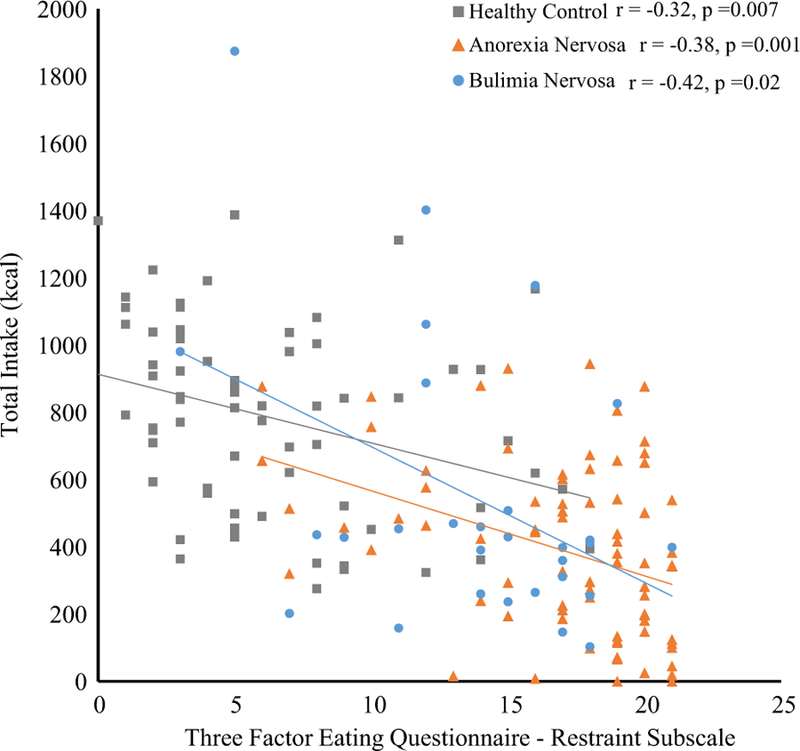
Pearson’s correlation between TFEQ Restraint subscale and caloric intake in the laboratory meal, with binge meals excluded. The association is statistically significant across the total sample (r = −0.598, p < 0.001) and within each diagnostic group, as shown [Color figure can be viewed at wileyonlinelibrary.com]
TABLE 2.
Pearson’s correlations between caloric intake and selfreport measures
| n | r | 95% CI | p | |
|---|---|---|---|---|
| Total sample | ||||
| TFEQ-Restraint | 177 | −.598 | −0.685, −0.511 | <0.001 |
| TFEQ-Disinhibition | 177 | −.004 | −0.153, 0.145 | 0.96 |
| TFEQ-Hunger | 177 | .031 | −0.124, 0.186 | 0.68 |
| EDE-Q-Restraint | 162 | −.538 | −0.647, −0.429 | <0.001 |
| Healthy control | ||||
| TFEQ-Restraint | 69 | −.322 | −0.545, −0.099 | 0.007 |
| TFEQ-Disinhibition | 69 | .207 | −0.014, 0.428 | 0.088 |
| TFEQ-Hunger | 69 | .196 | −0.020, 0.412 | 0.107 |
| EDE-Q-Restraint | 66 | −.232 | −0.474, 0.010 | 0.061 |
| Anorexia nervosa | ||||
| TFEQ-Restraint | 79 | −.380 | −0.562, −0.199 | <0.001 |
| TFEQ-Disinhibition | 79 | .314 | 0.120, 0.507 | 0.005 |
| TFEQ-Hunger | 79 | .218 | 0.040, 0.395 | 0.054 |
| EDE-Q-Restraint | 67 | −.370 | −0.583, −0.156 | 0.002 |
| Bulimia nervosa | ||||
| TFEQ-Restraint | 29 | −.425 | −0.784, −0.065 | 0.022 |
| TFEQ-Disinhibition | 29 | .343 | 0.098, 0.589 | 0.068 |
| TFEQ-Hunger | 29 | .253 | −0.024, 0.527 | 0.189 |
| EDE-Q-Restraint | 29 | −.130 | −0.399, 0.139 | 0.502 |
Note. TFEQ = Three-Factor Eating Questionnaire; EDEQ = Eating Disorder Examination Questionnaire; CI = Confidence Interval.
We explored the associations between intake and the other TFEQ subscales. There were no significant associations between TFEQ-Disinhibition or TFEQ-Hunger and caloric intake, except that both the subscales were positively associated with intake in the AN group (Table 2). Within a subsample (n = 127), we found no significant association between TFEQ-R and gram weight of food consumed (r = 0.10, p = 0.28).
We conducted the same analyses with binge meals (n = 5) included (the participants who binge ate at the meal included one individual with BN and four with AN binge-eating/purging subtype). Mean caloric intake did not differ significantly between groups: HC = 784 ± 280 kcal, AN = 562 ± 843 kcal, and BN = 617 ± 577 kcal (F2, 180 = 2.36, p = 0.097). The pattern of a relationship between TFEQ-R and caloric intake remained significant for all groups, except those with AN (Total r = −0.247, p = 0.001; HC r = −0.322, p = 0.007; AN r = −0.131, p = 0.24; BN −0.437, p = 0.016). The pattern of a relationship between EDE-Q-R and caloric intake remained significant for the total sample, but not within any diagnostic group (Total r = −0.192, p = 0.013; HC: r = −0.232, p = 0.061, AN: r = −0.099, p = 0.413, BN: r = 0.007, p = 0.969). For the other subscales of the TFEQ, the pattern of associations with caloric intake was similar to above: no significant associations in the total sample (ps > .19); among BN, no association with TFEQ-Hunger (r = 0.33, p = 0.07) and a significant association with TFEQ-Disinhibition (r = 0.37, p = 0.04). The only change was that among AN, with the binge meals included there was no significant association between intake and TFEQ-Disinhibition (r = 0.142, p = 0.20) or TFEQHunger (r = 0.137, p = 0.22).
4 |. DISCUSSION
In this large secondary analysis, higher dietary restraint measured by the TFEQ-R was associated with lower calorie intake in a laboratorybased multi-item meal. This relationship was significant within each diagnostic group (HC, AN, and BN) during non-binge meals. Across the total sample, the EDE-Q-R was also significantly associated with caloric intake. While the TFEQ-R was significantly related to intake within each group, the EDE-Q-R was significantly associated with caloric intake only within the AN group. This study provides useful information about the relationship between dietary restraint and restriction among individuals with eating disorders.
This study adds to the existing literature on the relationship between dietary restraint and food intake and helps address some mixed findings. Many studies in healthy individuals have shown small or non-significant correlations between restraint and intake. Of note, the few studies that showed a positive correlation between restraint and intake provided snack-like, “junk food” options in the eating laboratory (Jansen et al., 2009; Wardle & Beales, 1987). It is possible that the availability of these highly palatable foods triggers overeating (Herman & Mack, 1975), which may obscure the relationship between restraint and food intake in normal meals. Studies that included a wider variety of food options (similar to the multi-item meal in the current study) were more likely to show a negative correlation between restraint and intake, consistent with our findings (Greenwood et al., 2014; Rideout et al., 2004; Schoch & Raynor, 2012; Stice et al., 2004, 2010). Our finding that restraint score was not related to grams consumed suggests that a critical feature of restriction is the selection of low energy-dense foods, not a reduction in the total weight of food consumed.
The present study has several advantages. First, this study pooled data from eight separate studies, which provided a large sample size (n = 183). Second, this study included the largest sample of patients with eating disorders that are associated with high levels of dietary restriction (83 patients with AN and 30 patients with BN). As a result, the study benefited from a diverse group of participants who exhibited a wide range of dietary restraint and eating behavior and increased statistical power compared with prior studies. Finally, unlike several previous studies that focused on a limited range of food items, the current report provides data from multi-item meals with a variety of food options.
It is important to note several limitations of the present study. First, the data were obtained from several studies conducted over a number of years, and the multi-item meals were not entirely identical. Second, these studies examined a single eating episode. It would be useful to determine whether restraint scores predict behavior over a longer duration of time, as longer-term limitation of intake is more likely to result in physical and psychological repercussions. In addition, the present study focused on meals conducted in a laboratory, which differs from eating in the natural environment. For example, participants were presented with a large buffet of food items, which may not be representative of their typical meal settings. In addition, knowing they were being observed via closed-circuit television may have influenced the participants’ behavior. This study also did not include any participants with BED. The exploratory findings need to be considered in light of the limitation that we did not correct for multiple comparisons. Finally, our primary analyses excluded meals in which binge eating occurred, and it is possible that the relationship between dietary restraint and eating behavior differs during binge, compared to non-binge, meals. It will be useful to further investigate this phenomenon in the future with larger samples of patients who engage in binge eating. In particular, future research should seek to identify individual characteristics or environmental factors that predict which highly restrained individuals are likely to engage in restrictive versus binge eating and under what circumstances these different behaviors may emerge.
This study helps address gaps in our knowledge about the relationship between dietary restraint and restriction, particularly among patients with eating disorders. The results suggest that the TFEQRestraint scale is a useful measure of dietary restriction in individuals who exhibit pathological eating behavior, such as patients with AN and BN. Further research will be necessary to replicate these findings and extend them to understand restraint and restriction outside of a laboratory setting and over longer periods of time.
ACKNOWLEDGMENTS
The authors would like to acknowledge Yuanjia Wang PhD for her review of statistical analyses and Fiona Angel for her contribution to this work.
Funding information
Irving Institute for Clinical and Translational Research, Grant/Award Numbers: Clinical Trials Pilot Award, Irving Scholars Program; National Alliance for Research on Schizophrenia and Depression, Grant/Award Number: Young Investigator Award; National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: DK088532; National Institute of Mental Health, Grant/Award Numbers: MH082736, MH105452
REFERENCES
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 Arlington,VA: American Psychiatric Publishing. [Google Scholar]
- Anderson LM, Reilly EE, Schaumberg K, Dmochowski S, & Anderson DA (2016). Contributions of mindful eating, intuitive eating, and restraint to BMI, disordered eating, and meal consumption in college students. Eating and Weight Disorders, 21(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Bathalon GP, Tucker KL, Hays NP, Vinken AG, Greenberg AS, McCrory MA, & Roberts SB (2000). Psychological measures of eating behavior and the accuracy of 3 common dietary assessment methods in healthy postmenopausal women. The American Journal of Clinical Nutrition, 71(3), 739–745. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Lowe MR, & Karlsson J (2009). Psychometric analysis of the threefactor eating questionnaire-R21: Results from a large diverse sample of obese and non-obese participants. International Journal of Obesity, 33(6), 611–620. [DOI] [PubMed] [Google Scholar]
- de Witt Huberts JC, Evers C, & de Ridder DTD (2013). Double trouble: Restrained eaters do not eat less and feel worse. Psychology & Health, 28(6), 686–700. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wright SM, Paluch RA, Leddy J, Hawk LW Jr., Jaroni JL, … Lerman C (2004). Food hedonics and reinforcement as determinants of laboratory food intake in smokers. Physiology & Behavior, 81(3), 511–517. [DOI] [PubMed] [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders New York: Guilford Press. [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self-report questionnaire? The International Journal of Eating Disorders, 16(4), 363–370. [PubMed] [Google Scholar]
- Fairburn CG, & Cooper PJ (1993). The eating disorder examination. In Fairburn CG & Wilson GT (Eds.), Binge eating: Nature, assessment, and treatment (pp. 317–360). New York: Guilford Press. [Google Scholar]
- First M, Spitzer RL, Gibbon M, & Janet BW (1998). Structured clinical interview for DSM-IV disorders Washington, DC: American Psychiatric Press. [Google Scholar]
- Foerde K, Steinglass JE, Shohamy D, & Walsh BT (2015). Neural mechanisms supporting maladaptive food choices in anorexia nervosa. Nature Neuroscience, 18(11), 1571–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Jeffery RW, & Wing RR (1994). Food intake and physical activity: A comparison of three measures of dieting. Addictive Behaviors, 19(4), 401–409. [DOI] [PubMed] [Google Scholar]
- Gianini L, Liu Y, Wang Y, Attia E, Walsh BT, & Steinglass J (2015). Abnormal eating behavior in video-recorded meals in anorexia nervosa. Eating Behaviors, 19, 28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood J, Broadbent J, & Fuller-Tyszkiewicz M (2014). Restrained eaters consume more food only if they are impulsive and male. Eating Behaviors, 15(4), 582–585. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Herman CP, Polivy J, King GA, & McGree ST (1988). The (mis)measurement of restraint: An analysis of conceptual and psychometric issues. Journal of Abnormal Psychology, 97(1), 19–28. [DOI] [PubMed] [Google Scholar]
- Herman CP, & Mack D (1975). Restrained and unrestrained eating. Journal of Personality, 43(4), 647–660. [DOI] [PubMed] [Google Scholar]
- Jansen A (1996). How restrained eaters perceive the amount they eat. The British Journal of Clinical Psychology, 35(Pt 3), 381–392. [DOI] [PubMed] [Google Scholar]
- Jansen A, Nederkoorn C, van Baak L, Keirse C, Guerrieri R, & Havermans R (2009). High-restrained eaters only overeat when they are also impulsive. Behaviour Research and Therapy, 47(2), 105–110. [DOI] [PubMed] [Google Scholar]
- Jansen A, Theunissen N, Slechten K, Nederkoorn C, Boon B, Mulkens S, & Roefs A (2003). Overweight children overeat after exposure to food cues. Eating Behaviors, 4(2), 197–209. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, & Pirke KM (1989). A comparison of the validity of three scales for the assessment of dietary restraint. Journal of Abnormal Psychology, 98(4), 504–507. [DOI] [PubMed] [Google Scholar]
- Luce KH, & Crowther JH (1999). The reliability of the eating disorder examination—Self-report questionnaire version (EDE-Q). The International Journal of Eating Disorders, 25, 349–351. [DOI] [PubMed] [Google Scholar]
- Martin CK, Williamson DA, Geiselman PJ, Walden H, Smeets M, Morales S, & Redmann S Jr. (2005). Consistency of food intake over four eating sessions in the laboratory. Eating Behaviors, 6(4), 365–372. [DOI] [PubMed] [Google Scholar]
- Mayer LE, Schebendach J, Bodell LP, Shingleton RM, & Walsh BT (2012). Eating behavior in anorexia nervosa: Before and after treatment. The International Journal of Eating Disorders, 45(2), 290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira P, de Almeida MD, & Sampaio D (2005). Cognitive restraint is associated with higher intake of vegetables in a sample of university students. Eating Behaviors, 6(3), 229–237. [DOI] [PubMed] [Google Scholar]
- Mostafavi S, Mohammadi RM, Eshraghian MR, Hosseini S, Moghadam FA, Hosseinzadeh P, et al. (2017). Psychometric properties, reliability and validity of Persian version of the three-factor eating questionnaire-R18 (TFEQ-R18) in overweight and obese women and its relationship with some body composition and dietary intake variables. Iranian Journal of Psychiatry, 12(2), 100–108.28659982 [Google Scholar]
- Neumark-Sztainer D, Jeffery RW, & French SA (1997). Self-reported dieting: How should we ask? What does it mean? Associations between dieting and reported energy intake. The International Journal of Eating Disorders, 22(4), 437–449. [DOI] [PubMed] [Google Scholar]
- Ouwens MA, van Strien T, & van der Staak CP (2003). Tendency toward overeating and restraint as predictors of food consumption. Appetite, 40(3), 291–298. [DOI] [PubMed] [Google Scholar]
- Reas DL, Grilo CM, & Masheb RM (2006). Reliability of the eating disorder examination-questionnaire in patients with binge eating disorder. Behaviour Research and Therapy, 44, 43–51. [DOI] [PubMed] [Google Scholar]
- Rideout CA, McLean JA, & Barr SI (2004). Women with high scores for cognitive dietary restraint choose foods lower in fat and energy. Journal of the American Dietetic Association, 104(7), 1154–1157. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Castellanos VH, Shide DJ, Miller DL, Pelkman CL, Thorwart ML, & Peters JC (1997). Sensory properties of a nonabsorbable fat substitute did not affect regulation of energy intake. The American Journal of Clinical Nutrition, 65(5), 1375–1383. [DOI] [PubMed] [Google Scholar]
- Schaumberg K, & Anderson D (2016). Dietary restraint and weight loss as risk factors for eating pathology. Eating Behaviors, 23, 97–103. [DOI] [PubMed] [Google Scholar]
- Schoch AH, & Raynor HA (2012). Social desirability, not dietary restraint, is related to accuracy of reported dietary intake of a laboratory meal in females during a 24-hour recall. Eating Behaviors, 13(1), 78–81. [DOI] [PubMed] [Google Scholar]
- Steinglass JE, Albano AM, Simpson HB, Wang Y, Zou J, Attia E, & Walsh BT (2014). Confronting fear using exposure and response prevention for anorexia nervosa: A randomized controlled pilot study. The International Journal of Eating Disorders, 47(2), 174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Glasofer DR, Walsh E, Guzman G, Peterson CB, Walsh BT, … Wonderlich SA (2018). Targeting habits in anorexia nervosa: A proof-of-concept randomized trial. Psychological Medicine, 48(15), 2584–2591. [DOI] [PubMed] [Google Scholar]
- Stice E, Cooper JA, Schoeller DA, Tappe K, & Lowe MR (2007). Are dietary restraint scales valid measures of moderateto - long-term dietary restriction? Objective biological and behavioral data suggest not. Psychological Assessment, 19(4), 449–458. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, & Lowe MR (2004). Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment, 16(1), 51–59. [DOI] [PubMed] [Google Scholar]
- Stice E, Sysko R, Roberto CA, & Allison S (2010). Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite, 54(2), 331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJ, & Messick S (1985). The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research, 29(1), 71–83. [DOI] [PubMed] [Google Scholar]
- Sysko R, Glasofer DR, Hildebrandt T, Klimek P, Mitchell JE, Berg KC, … Walsh BT (2015). The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. The International Journal of Eating Disorders, 48(5), 452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sysko R, Ojserkis R, Schebendach J, Evans SM, Hildebrandt T, & Walsh BT (2017). Impulsivity and test meal intake among women with bulimia nervosa. Appetite, 112, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sysko R, Steinglass J, Schebendach J, Mayer LES, & Walsh BT (2018). Rigor and reproducibility via laboratory studies of eating behavior: A focused update and conceptual review. The International Journal of Eating Disorders, 51(7), 608–616. [DOI] [PubMed] [Google Scholar]
- Sysko R, Timothy Walsh B, & Terence Wilson G (2007). Expectancies, dietary restraint, and test meal intake among undergraduate women. Appetite, 49(1), 30–37. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, & Wilson GT (2005). Eating behavior among women with anorexia nervosa. The American Journal of Clinical Nutrition, 82(2), 296–301. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Frijters JE, Bergers GP, & Defares PB (1986). Dutch eating behaviour questionnaire for assessment of restrained, emotional and external eating behavior. The International Journal of Eating Disorders, 5, 295–315. [Google Scholar]
- Van Strien T, Frijters JE, Van Staveren WA, Defares PB, & Deurenberg P (1986). The predictive validity of the Dutch restrained eating scale. The International Journal of Eating Disorders, 5(4), 747–755. [Google Scholar]
- Walsh BT (2011). The importance of eating behavior in eating disorders. Physiology & Behavior, 104(4), 525–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J, & Beales S (1987). Restraint and food intake: An experimental study of eating patterns in the laboratory and in normal life. Behaviour Research and Therapy, 25(3), 179–185. [DOI] [PubMed] [Google Scholar]


