Abstract
The next step in reestablishing credibility seams to us honesty and recognizing we all share a common goal of the health and wellness of the human community and the planet. Everyone agrees that the current healthcare system, despite its many incredible successes, is also showing its limitations and is no longer sustainable. We believe the solution starts with us the researchers and editors. A good first step might be formally recognizing the errors and showing how we can and intend to get better.
Evidence-based medicine—by definition—requires objective, reliable and accurate research and reviews from which to make the best decisions in patient care and public policy. The causes of inaccurate information, ranging from presumably innocent mistakes all the way to apparently intentional fraud, affect all scientific and biomedical disciplines.1 While these accidental and intentional errors can derail our understanding of diseases and impact tens of thousands of affected patients, such inaccuracies in the field of nutrition can impact hundreds of millions of people worldwide.2 While fractions of the population succumb to a specific disease that may need drug therapy, the entire human population eats food and is directly affected by nutrition research. Further, the science of nutrition is particularly contentious and territorial. A great irony of nutrition research is that most of it is conducted by healthcare professionals with little to no formal training in nutrition. Clinical therapeutic nutrition is not taught in the vast majority of medical schools3-5 nor in post-graduate medical training programs6, including those specialties that are obviously impacted by dietary intake such as gastroenterology7 and cardiology.8,9 Despite this absence of training in clinical nutrition, the medical profession proclaims itself authoritative on all health-related topics, including the entire territory of clinical nutrition.10 A major and serious problem arises when unskilled and invalid research is published by authors (including nonphysician journalists11) in major journals which mischaracterizes the validity of nutrition interventions (e.g., essentially always concluding that nutritional interventions are inefficacious or potentially hazardous) and then such research is used politically and in the media to disparage, restrict and regulate practitoners and nutrition supplement industry12 to the detriment of human health.
Several factors disrupting the integrity of nutrition research are commonly found in studies published by “elite” universities in “top-tier” journals, which are then republished and distributed as “headlining news” in newspapers, magazines, and television via which they ultimately influence patient care, government policy and health outcomes for tens/hundreds of millions of people. This editorial provides several recent examples of questionable nutrition research and publications, lists possible causes and suggests some proposed solutions. Given that all aspects of healthcare are dependent upon the integrity of the educational, investigative and publication processes, the advancements of clinical medicine and population-wide health improvements are hindered by accidental and intentional ignorance in nutrition education and research.
Recent examples of questionable nutrition publications from major journals
In the following subsection, we review recent examples of questionable or inaccurate publications related to nutrition. Perceived shortcomings are documented with both citations here and links to more detailed and authoritative reviews and video presentations. In some instances, speculations regarding the cause and consequences of identified errors are provided.
Vitamin and Mineral Supplements: What Clinicians Need to Know (JAMA—Journal of the American Medical Association 2018 Mar). In this recent publication, authors Manson and Bassuk10 attempt to review “what clinicians need to know” about “vitamin and mineral supplements” within a span of two pages. Such a publication apparently attempts to simplify the entire field of clinical nutrition to a ridiculous diminution and by such brevity must contain oversimplifications that are ultimately misleading. Oddly and clearly discordant with most reviews on pharmacotherapeutics, such nutrition reviews in medical journals commonly start with overtures reviewing the popularity of nutritional supplements (“52% of US adults reported use of at least one supplement product”), the financial size of the market (“$30 billion industry in the United States”), sweeping generalizations that claim inefficacy of the entire genre (“most randomized clinical trials of vitamin and mineral supplements have not demonstrated clear benefits”), and allusions to “harmful effects” and the need to “curb inappropriate use of such supplements except that “clinicians may wish to favor prescription products.” Revealingly, the authors make several mentions of “folic acid” but without any mention of the other and clinically preferred forms of the nutrient as folinic acid and methylfolate; likewise, “vitamin B12” is discussed without differentiation of its various forms: cyanocobalamin, hydroxocobalamin, adenosylcobalamin and methylcobalamin. “Vitamin D” is referenced without distinction of ergocalciferol from cholecalciferol as if these are equipotent when in fact the latter is generally considered more potent and has some important physiological differences.13-15 Further, inaccurate dosage recommendations are made despite overwhelming evidence that the cited doses are inadequate by an order of magnitude.16-20 This is further aggravated by the foundational misperception that a nutrient can be studied as an isolated molecule like a drug, but in reality nutrients always function within biochemical networks of interaction and inderdependency that require multiple nutrients and affect multiple pathways and physiologic systems. Studying supplemental vitamin D without paying attention to the status of magnesium, vitamins A and K2 is an effective way to ensure negative results and adverse reactions. Citing clinical trials that failed to assess baseline nutrient intake is akin to a drug trial that failed to inquire about and document baseline pharmacotherapy and polypharmacy. “Vitamin K” is mentioned without distinction of important dosing and effect differences among K1 (phylloquinone), K2 (menaquinone-4), K3 (menadione), and K7 (menaquinone-7).21 As a final example, the authors state that “calcium supplements may increase the risk for kidney stones” but make no mention whatsoever of mitigating this risk with diet modification, magnesium, citrate or urinary alkalinization.22 In short, their review is impressively lacking in important details that clinicians legitimately need to know regarding vitamin and mineral supplements; as such we consider it a misleading representation of the field, especially given that the publication is directed to an audience of medical physicians with no formal training and thus no background information nor evaluative perspective on the topic.
Associations of Omega-3 Fatty Acid Supplement Use With Cardiovascular Disease Risks: Meta-analysis of 10 Trials Involving 77917 Individuals (JAMA Cardiology 2018 Mar). Conclusions from this meta-analysis23 were echoed (See illustration 1: The pharmaceutical-journal-news echo chamber.) in newspapers, magazines, and throughout the internet, thereby ultimately influencing hundreds of millions of healthcare recipients.24 Per video critique by Vasquez25, important shortcomings of this review include (1) unjustified selective exclusion of data, (2) non-therapeutic dosing, (3) use of unnatural/semisynthetic form of fish oil, (4) conclusions at odds with data, (5) pro-pharma conflicts of interest among authors, publication, and supporting organizations, and—related to critique #2 aforementioned—(6) no mention anywhere in the article of the importance of the omega-3 index, the concept and use of which is highly important as documented more than 20 years previously26 and repeatedly validated and widely published in leading scientific27 and cardiology specialty journals.28
Supplemental Vitamins and Minerals for CVD Prevention and Treatment (Journal of the American College of Cardiology 2018 Jun). Problems with this publication29 include (1) paid conflicts of interest among the journal’s editorial/review staff30, (2) conflicts of interest with the drug and processed food industries, (3) unscientific exclusion of data, (4) removal of data that countered the overall narrative of the article, eg, “Studies containing selenium were removed from the analysis of antioxidants due to the high percentage of these studies of the left side of the unity line versus the right side of the unity line in the antioxidant forest plot. This is compared to other components of antioxidant mixtures. Removal of the selenium studies resulted in a significant increase in all-cause mortality”, (5) failure to maintain basic clinical and pharmacologic standards, and (6) confusion and equivocation with regard to details of nutritional interventions.31
Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus (New England Journal of Medicine 2018 Aug/Oct). Known as the ASCEND study32, this large long-term clinical trial compared effects of low-dose fish oil against low-dose olive oil, looking for a difference in effect on cardiovascular outcomes. Per critiques by Vasquez33, major shortcomings of this trial include (1) erroneous description and use of olive oil as “placebo”, and (2) conflicts of interest with the pharmaceutical industry, including supervision of key meetings by drug industry sponsors. In one of the most bizarre statements we have ever read in our 60+ years of reviewing medical literature, this article notes, “Mylan, Solvay and Abbott had nonvoting representation at meetings of the steering committee of the study and provided comments regarding the trial design and draft manuscript…” Olive oil cannot be considered a placebo given the well-established facts that it is one of the most potent anti-inflammatory and cardioprotective foods ever discovered; in fact, a short review published 15 years ago in the self-same New England Journal of Medicine noted that olive oil consumption in the Mediterranean diet provides such consumers with “very low rates of coronary heart disease and certain types of cancer and [had] a long life expectancy.”34 Cardioprotective, anti-inflammatory and antioxidant components of olive oil include squalene, oleic acid, and the numerous and abundant phytochemicals. The metabolic and cardioprotective benefits of olive oil are realized with consumption of low doses.35 In fact, the antiinflammatory benefits of olive oil are so potent that a clinical trial36 published in 1991 stated, “Olive oil can no longer confidently be used as a placebo control.” Further, 10% of ASCEND subjects were already taking fish oil (n3) supplementation at baseline, with corresponding omega-3 indexes of 6.6% and 7.1%, remarkably higher than the average 4% typical of Western societies.37 Consistent with the post-publication peer-review process, Vasquez38 punctually submitted a guideline-conforming critique of this research; but the critique was rejected by the New England Journal of Medicine with the excuse that the journal did not have sufficient print space for a critique of less than 175 words despite the original article length of roughly 7,000 words.
Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia (New England Journal of Medicine 2019 Jan) and Prescription-strength omega-3 fatty acids to prevent heart disease?“A drug made from a highly purified fat from fish reduced cardiovascular events in people with heart disease or diabetes” (Harvard Heart Letter 2019 Feb): The original article39 and related publication by Harvard Medical School/Harvard Heart Letter40 both report a trial sponsored by the prescription drug manufacturer wherein 4 grams per day of “prescription-strength omega-3 fatty acids” from fish oil were compared against “a placebo that contains mineral oil.” As noted by Vasquez41, 4 grams per day of concentrated fish oil would be expected to produce more robust benefits than did the previously mentioned articles that used only 25% of this dose; as one would expect from the study of pharmacology, fish oil is similar to any other therapeutic in that its distribution and effects demonstrate a dose-response relationship Furthermore, the mineral oil purportedly used as a “placebo” is very clearly not an inert substance, as has been well known and documented, for example in the Journal of the American Medical Association, for more than 70 years.42-45 Mineral oil is known to block absorption of fat-soluble antiinflammatory, anti-oxidant, and cardioprotective nutrients, specifically but not exclusively vitamin A, vitamin D, and beta-carotene. Mineral oil may also reduce absorption of cardioprotective drugs, as noted in the original study by Bhatt et al, who questioned the possibility “if mineral oil in the placebo affected statin absorption in some patients, this might have contributed to differences in outcomes between the groups”; the authors made no attempt to assess for this possibility nor for iatrogenic malabsorption of nutrients. Not surprisingly, and perhaps also due to pro-inflammatory stimulation of the immune system, administration of mineral oil causes significant and measurable adverse effects on markers of cardiovascular disease risk, as noted in a remarkably insightful article by Herper46 published in Forbes. Mineral oil is absorbed from the intestines and is deposited in skin, subcutaneous tissues, intestinal wall, regional lymph nodes, liver, spleen, lungs, and bone marrow.47-49 The paradoxical use of a high-dose fish oil product against metabolically adverse/deleterious mineral oil would be expected to greatly favor the fish oil product, as noted by Herper.
Why Is So Much Of The Nutritional Medicine Research So Flawed?
Trying to think through why these obviously erroneous studies where published, we see basically only two options: ignorance or medical/financial priorities.
Ignorance
We are willing to consider that the following are due to lack of adequate education in nutrition.
Olive Oil Is Not Inert
Comparing two compounds that are both effective is obviously not going to show much difference in outcomes. Some of the studies critiqued above used fish oil VS olive oil. The authors and editors should have been aware that olive oil is cardioprotective and antiinflammatory since the data has been consistently published for almost 60 years, including in the NEJM.
Mineral Oil Is Not Inert
On the other hand, plenty of research shows multiple adverse physiological effects of mineral oil, making it a profoundly inappropriate placebo. Relative to long-term administration of mineral oil, almost anything “not too toxic” will look good by comparison. Examples of the ill effects of mineral oil are noted above.
Ignorance of Previous Standards For Assessing Omega-3 Status
The omega-3 index was validated some 20 years ago. Why wasn’t it used to assess both initial status and impact of intervention? How can a major review of fish oil trials—especially in a cardiology specialty journal—fail to make any mention whatsoever about appropriate dosing, adjustments for body size (especially given that many subjects were overweight or obese), and the objectively measurable (for compliance and treatment effect) and consistently validated omega-3 index?
Medical/Financial Political
Obviously, research integrity is jeopardized when it becomes dependent or overly close with funding sources or political organizations. “Research for profit” is often hidden or obfuscated.
Pay-To-Play Research
The Oxford study ASCEND claimed that all authors were “independent scientists” but the online documents showed that the majority of authors were rewarded by drug companies; and the article itself stated that the drug company supervised key meetings where their paid consultants were working; several drug companies “had nonvoting representation at meetings of the steering committee of the study and provided comments regarding the trial design and draft manuscript…” Could the financial conflicts of interest or potential for industry influence be more obvious? Why weren’t the conflicts of interest printed within the same publication wherein the authors called themselves “independent investigators.” Why were university and nonprofit affiliations listed so clearly whereas drug industry connections were omitted from the printed article and available only in separate documents online?
Hidden Data
The 2018 NEJM “fish oil vs mineral oil” study obscured the identity of the placebo and also hid the adverse effects in the online materials separate from the main publication. This means very few researchers or busy doctors saw the adverse effects by reading the published study. Separating key data from the main publication by the inconvenient or unsuspected use of cumbersome online “supplemental materials” surely prevents many if not most readers from seeing important information and making appropriate and contextualized interpretations of the data. Why was important information separated from the primary publication? When physicians are given a reprint of the study, most of them will not have immediate access to the accessory online documents that contain important information.
Common Problem of Inaccuracy In Published Abstracts
The reading of any study begins with the reading of the title and abstract of the article. Many and perhaps most busy healthcare professionals, among those who are even willing to independently keep up with the research, read only the abstracts, not the full study. “Abstract-only” reading is usually due to time limitations, but many major journals require a fee to access the full study, while the abstract is available for free either at the publisher’s website or within a cataloged database. Unless they are part of an academic health center or a clinical organization that is large enough to afford the huge subscription fees, most clinicians never see the actual research. Many studies of clinical trial abstract quality have been published, consistently showing multiple types of problems. A review study published a full 20 years ago found that 18%-68% of the abstracts in 5 major medical journals (Annals of Internal Medicine, BMJ, JAMA, Lancet, and New England Journal of Medicine) contain multiple factual inaccuracies.50 Another example study looked at major journals like NEGM, JAMA, BMJ and Lancet and found less than 10% clearly defined blinding, less than 15% reported numbers lost to follow up and only half reported ADRs.51 In our extensive reading of medical research, we have found multiple examples of abstracts that report the exact opposite of the actual data in the study (See IMCJ editorial 14.4 for an example). We are admonished to practice evidence-based medicine. But what happens when the “evidence” presented in the published abstract is exactly wrong?
Now, with the growing and strategic popularity of separating key findings and authors’ financial ties in online “supplementary materials”, has medical publishing yet further and paradoxically obscured and encumbered the proper evaluation of scientific publications?
Problem Of Drug Advertising Distorting Publication Of Stuides On Dietary Supplements
Readers of research articles assume, appropriately but not accurately, total separation of a journal’s editorial and marketing divisions. Unfortunately, such separation of scientific content from industry payments (and thus influence) does not appear to be the norm in many major journals. One study looked at the correlation between the number of pharmaceutical advertisements in 11 major medical journals and their publication of articles on dietary supplements. They found that journals with the most pharmaceutical ads published: (1) fewer major articles about dietary supplements, (2) when such articles were published they were far more likely to conclude that dietary supplements were unsafe, and (3) were 50% more likely to publish studies showing dietary supplements were clinically ineffective. All these findings of bias were statistically significant.52
Pay-To-Publish
The authors are not the only ones with conflicts of interests. With the huge surge in “open-access journals”, authors commonly pay journals (and thus editors) for publication. The potential for conflict of interest is obvious and substantial: editors of such journals have a financial incentive to accept articles, likely including those that they might have otherwise rejected. Several studies have documented predatory behaviors by editors to recruit fees, high susceptibility to falsified credentials in editorial board members, and little to no rigor in their review processes.53 We are not saying that all open-access journals are problematic, but rather that the potential for conflict of interest, ie, “incentivized acceptance”, is especially high.
Thoughts on How to Improve Nutrition Research
The flaws we documented and exemplified above are clearly preventable by researchers making better study design decisions. Equally clear is that editors should not accept papers until such obvious problems are resolved. We propose the following for consideration by both authors and editors.
Micromanagement
We can develop formal rules and governing bodies to certify and monitor editors. In turn, the editors in a very formalized and rigorous manner micromanage authors to prevent problems such as: systematic bias, nutrients being studied at inappropriate dosages, in ineffective forms, or with no attention to the full matrix in which they function, etc. We are not advocating for this authoritarian solution, but must admit it is a pathway.
Improve the Quality of Abstracts
The CONSORT reporting guidelines for the abstracts of randomized clinical trials is a good starting point. It provides clear guidelines and a checklist. Unfortunately, virtually no journals are following these guidelines. One study evaluated the abstracts of 395 randomized clinical trials published in anesthesia journals in 2010 and in 2016 to determine adherence to CONSORT and trend using a 16 point scale. The good news is that there was a statistically significant improvement. The bad news is that the average rating increased from only 4 to only 6 points out of a total of 16 possible quality points. Not a single abstract scored 16 and 75% met fewer than ½ the guidelines.54
Competence in Nutrition
We can teach editors, researchers and doctors to be nutritionally competent (which they should have learned in medical school) so that when they evaluate or use nutrition research, they hold it to a higher level of intellectual and scientific competence so that junk research is not published in the first place nor thereafter accepted by medical professionals.
Reestablish Integrity
We need to think more broadly about how we teach ethics. Medical students commonly receive training in “medical ethics”, but most of the exercises are specific to clinical situations appropriate for inexperienced and naïve medical students. We as educators need to teach broader conceptualizations of ethics that serve to create and maintain a healthy and empowered healthcare community making clinical decisions based on the best real research. In addition, journals themselves need to be more accepting and responsive to post-publication critiques. They must be willing to retract, or at least bring substantial attention, to previously published articles that are shown to be problematic.
Update Education of Current Practitioners and Reform Licensing Bodies
Clinicians who want to independently stay up with the research need to be better taught to recognize and combat unreliable research. However, in this authoritarian age we also need to curtail overzealous licensing boards from restricting a practitioner from exercising his or her best clinical judgment.
Summary
The next step in reestablishing credibility seams to us honesty and recognizing we all share a common goal of the health and wellness of the human community and the planet. Everyone agrees that the current healthcare system, despite its many incredible successes, is also showing its limitations and is no longer sustainable. We believe the solution starts with us the researchers and editors. A good first step might be formally recognizing the errors and showing how we can and intend to get better.
Full disclosure
JP: As fully detailed in Editorial 8.6, JP is a scientific consultant to Bioclinic Naturals, a bioceuticals company. No studies using any of their proprietary products have been published in IMCJ. AV: In addition to having authored approximately 100 articles and letters in a wide range of disciplines and peer-reviewed journals, AV is the author of the 1200-page Inflammation Mastery, 4th Edition (2016), also published in two volumes as Textbook of Clinical Nutrition and Functional Medicine with sections excerpted as Human Microbiome and Dysbiosis in Clinical Disease, Antiviral Nutrition, and Brain Inflammation in Chronic Pain, Migraine, and Fibromyalgia. Dr Vasquez has served as a consultant to Biotics Research Corporation.
In This Issue
We start this issue with appreciation for Associate Editor David Riley, MD who set up and lead the excellent Case Report series for IMCJ. With great sadness we announce that David is retiring from his editorial position. Thank you David for your excellent work demonstrating that carefully and rigorously designed patient reports are a credible way of providing scientific documentation of efficacy of the personalized medicine we advocate.
As usual, Associate Editor Jeffrey Bland, PhD kicks off this issue. His very interesting Commentary dives deeply into the fasting and para-fasting research. Having myself supervised hundreds of 4- to 30-day water-only fasts, I’ve substantial experience in this area. This is a good example of how using PubMed-indexed research totally misses the hundreds of years of successful clinical fasting expertise that is found in natural medicine books and clinicians. A good example to the non-MD community of the importance of documenting our work. Those interested in learning more about this very useful therapeutic modality will find the fasting chapter (first published in 1985) in my Textbook of Natural Medicine very helpful, as well as the patient handouts in the Appendix.
George W. Cody, JD, MA, continues his series on the origins of integrative medicine. In this article he covers some of the key contributions from the chiropractic profession.
Regular contributor John Weeks discusses the huge challenge facing doctors of integrative medicine who use compounding pharmacists to personalize drug prescriptions for their patients. This problem is fully addressed by attorney Alan Dumoff, JD, MSW who has lead the fight to protect this important resource for our patients. The article he wrote for IMCJ can be found in issue 17.3. As usual, he has many other interesting briefs about the politics and business of this medicine. The results of the poll assessing the percent of cancer patients who believe alternative medicine has a cure are quite surprising.
Tom Blue has written two interesting articles on public interest in this medicine and the many challenges facing clinicians trying to make this work financially. His several suggestions are worth serious consideration. His considerable experience with concierge medicine provides useful insights.
One of the most fun and gratifying responsibilities as editor is being able to interview the special people who have created and practice this medicine. Managing Editor Craig Gustafson interviewed expert functional medicine neurologist and my friend David Haase, MD. His insightful ideas on stress, pain, and addiction are very helpful, especially in this era of prescription pain medication abuse.
Original research by David S. Riley, MD; Viktor G. Lizogub, PhD; Marianne Heger, MD; Petra Funk, PhD;Heiko Mueller, Walter Lehmacher evaluates the efficacy of Pelargonium sidoides root in the treatment of the common cold. This multi-center, randomized, double-blind phase III clinical trial with 105 adults showed clear efficacy. Having personally used Umcka for over 10 years, I can attest that these results are consistent with my experience.
Self-insured corporations have, in my experience, been the most receptive to health promotion. Corporate wellness programs are a great way to demonstrate the efficacy of the concepts of our medicine. Managing editor Craig Gustafson interviewed Richard E. Johnson, JD, a health strategy expert. Those interested in working in this area will find a lot of value here.
Remarkable serendipity that Associate Editor Bill Benda, MD finishes the issue with the same concerns with which we started: Time to get back to the Truth. Journals of science are published as part of our community efforts to objectively understand the world. The truth decay in research which Alex and I addressed seems a sad symptom apparently escalating throughout our society.

Joseph Pizzorno, ND, Editor in Chief
drpizzorno@innovisionhm.com
Figure 1.
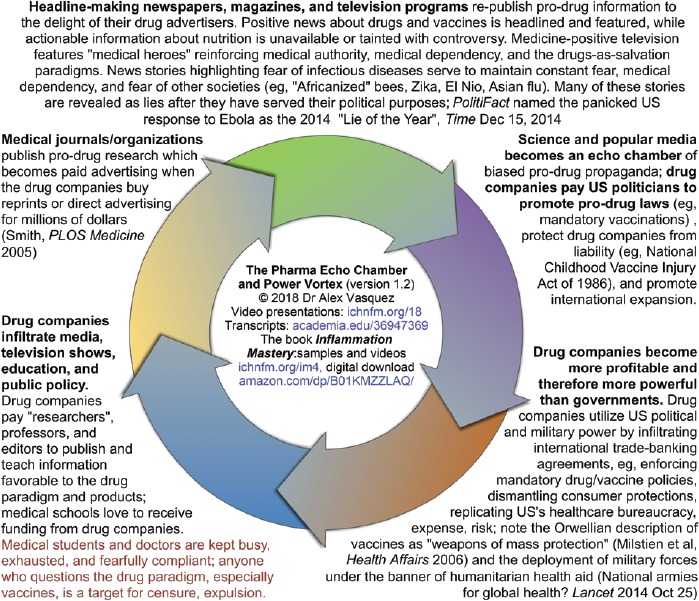
The pharmaceutical-journal-news echo chamber: Medical journals have inherent biases to publish pro-drug and anti-nutrition articles, both to please their pharmaceutical sponsors and to maintain their pharmacocentric paradigms. Newspapers and television repeat the conclusions from medical journals, thereby dispersing the information to hundreds of millions of persons. Television shows also glorify medicine and drugs in programs featuring “medical heroes” ranging from Doogie Howser MD to MASH to House MD. As the drug paradigm is strengthened financially and socially, drug companies have more money to buy more political influence (ie, transitioning from “echo chamber” to “power vortex”), including directly paying politicians to pass drug-friendly protective laws and mandatory drug requirements. Influence from the pharmaceutical and processed food industries is noted in international policies determining use of (for example) vaccines, genetically modified foods, and breast feeding. Meanwhile, medical professionals are kept overly busy, burnt-out, and untrained in nutrition, thereby leaving them vulnerable to misinformation, especially in nutrition. Drug companies pay for and “supervise” research via universities, while also paying textbook authors, journal editors, and medical societies that publish treatment guidelines.
Biography
References
- 1.Byrne J. We need to talk about systematic fraud. Nature. 2019. Feb;566(7742):9 doi: 10.1038/d41586-019-00439-9. [DOI] [PubMed] [Google Scholar]
- 2.Bowman L, Mafham M, Stevens W, et al. ASCEND: A Study of Cardiovascular Events In Diabetes: Characteristics of a randomized trial of aspirin and of omega-3 fatty acid supplementation in 15,480 people with diabetes. Am Heart J. 2018. Apr;198:135-144. doi: 10.1016/j.ahj.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010. Sep;85(9):1537-42. doi: 10.1097/ACM.0b013e3181eab71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halsted CH. The relevance of clinical nutrition education and role models to the practice of medicine. Eur J Clin Nutr. 1999. May;53 Suppl 2:S29-34. [DOI] [PubMed] [Google Scholar]
- 5.Adams KM, Lindell KC, Kohlmeier M, Zeisel SH. Status of nutrition education in medical schools. Am J Clin Nutr. 2006. Apr;83(4):941S-944S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vetter, et al. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr. 2008. Apr;27(2):287-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raman M, Violato C, Coderre S. How much do gastroenterology fellows know about nutrition? J Clin Gastroenterol. 2009. Jul;43(6):559-64. [DOI] [PubMed] [Google Scholar]
- 8.Devries S, Freeman AM. Nutrition Education for Cardiologists: The Time Has Come. Curr Cardiol Rep. 2017. Sep;19(9):77 doi: 10.1007/s11886-017-0890-6. [DOI] [PubMed] [Google Scholar]
- 9.Devries S, Agatston A, Aggarwal M. A Deficiency of Nutrition Education and Practice in Cardiology. Am J Med. 2017. Nov;130(11):1298-1305. doi: 10.1016/j.amjmed.2017.04.043. [DOI] [PubMed] [Google Scholar]
- 10.Manson JE, Bassuk SS. Vitamin and Mineral Supplements: What Clinicians Need to Know. JAMA. 2018. Mar 6;319(9):859-860. doi: 10.1001/ jama.2017.21012. [DOI] [PubMed] [Google Scholar]
- 11.Abbasi J. Another Nail in the Coffin for Fish Oil Supplements. JAMA. 2018. May 8;319(18):1851-1852. doi: 10.1001/jama.2018.2498. See also commentary: Vasquez A. Perpetuating Nutritional Ignorance among Doctors and Recycling Bad Science at JAMA and AMA https://vimeo.com/265987272 and https://www.academia.edu/36470484 [DOI] [PubMed] [Google Scholar]
- 12.“The take-home to me is that from a primary prevention standpoint in this older population there appears to be no role for vitamin D or fish oil supplementation. These are supplements that many people use. They are generally over-the-counter supplements that can be as cheap as $10 per month or as much as $50 or $60 per month…. To go further, I think regulating the mass marketing of multivitamins is also warranted.” Gulati M. VITAL: Mixed findings for vitamin D, omega-3s in CVD, cancer prevention. American Heart Association Scientific Sessions, Nov 10-12 [2018] Chicago. Cardiology Today, December 2018 https://www.healio.com/cardiology/chd-prevention/news/print/cardiology-today/%7B0970820c-ebb7-4525-b9e9-1b8006af4805%7D/vital-mixed-findings-for-vitamin-d-omega-3s-in-cvd-cancer-prevention/.
- 13.Logan VF, Gray AR, Peddie MC, Harper MJ, Houghton LA. Long-term vitamin D3 supplementation is more effective than vitamin D2 in maintaining serum 25-hydroxyvitamin D status over the winter months. Br J Nutr. 2013. Mar 28;109(6):1082-8. doi: 10.1017/S0007114512002851. [DOI] [PubMed] [Google Scholar]
- 14.Armas LA, Hollis B W, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004. Nov;89(11):5387-91 DOI: 10.1210/jc.2004-0360. [DOI] [PubMed] [Google Scholar]
- 15.Daroux M, Shenouda M, Bacri JL, Lemaitre V, Vanhille P, Bataille P. Vitamin D2 versus vitamin D3 supplementation in hemodialysis patients: a comparative pilot study. J Nephrol. 2013. Jan-Feb;26(1):152-7. doi: 10.5301/ jn.5000123. [DOI] [PubMed] [Google Scholar]
- 16.Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003. Jan;77(1):204-10. [DOI] [PubMed] [Google Scholar]
- 17.Vasquez A, Manso G, Cannell J. The clinical importance of vitamin D (cholecalciferol): a paradigm shift with implications for all healthcare providers. Altern Ther Health Med. 2004. Sep-Oct;10(5):28-36. [PubMed] [Google Scholar]
- 18.Veugelers PJ, Ekwaru JP. A statistical error in the estimation of the recommended dietary allowance for vitamin D. Nutrients. 2014. Oct 20;6(10):4472-5. doi: 10.3390/nu6104472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heaney R1, Garland C2, Baggerly C3, French C4, Gorham E5. Letter to Veugelers, P.J. and Ekwaru J.P., A statistical error in the estimation of the recommended dietary allowance for vitamin D. Nutrients 2014, 6, 4472-4475; doi:10.3390/nu6104472. Nutrients. 2015. Mar 10;7(3):1688-90. doi: 10.3390/ nu7031688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimball SM, Mirhosseini N, Holick MF. Evaluation of vitamin D3 intakes up to 15,000 international units/day and serum 25-hydroxyvitamin D concentrations up to 300 nmol/L on calcium metabolism in a community setting. Dermatoendocrinol 2017. Apr 13;9(1):e1300213 doi: 10.1080/19381980.2017.130021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Personal communication between AV and Alan Gaby MD on 11 Feb 2019. See also: Gaby AR. Chapter 15. Vitamin K. In Gaby AR. Nutritional Medicine, 2nd edition Concord, NH, 2017. doctorgabycom. [Google Scholar]
- 22. Recently reviewed in: Vasquez A. “Urinary Alkalinization against Mild Metabolic Acidosis: Obesity, Pain, Diabetes, Kidney Protection” (July 29, 2018). https://www.academia.edu/37138783 and “Importance of acid-base balance, serum bicarbonate, potassium citrate, urine pH” video presentation available online https://vimeo.com/282027203. See also: “Introduction to Cardiovascular Nutrition (cardionutrition #1): Ketogenic Diet and Potassium Citrate” video presentation available online https://vimeo.com/277472451.
- 23.Aung T, Halsey J, Kromhout D, et al. Associations of Omega-3 Fatty Acid Supplement Use with Cardiovascular Disease Risks: Meta-analysis of 10 Trials Involving 77 917 Individuals. JAMA Cardiol. 2018. Mar 1;3(3):225-234. doi: 10.1001/jamacardio.2017.5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicholas Bakalar Omega-3 Supplements Don’t Protect Against Heart Disease. New York Times Jan. 31, 2018. https://www.nytimes.com/2018/01/31/well/ live/omega-3-supplements-dont-protect-against-heart-disease.html. See also: Omega-3 Fatty Acid Supplements Do Not Reduce Cardiovascular Disease Risks. February 09, 2018. https://www.practiceupdate.com/content/omega-3-fatty-acid-supplements-do-not-reduce-cardiovascular-disease-risks/63830. See also: Lisa Rapaport. Omega-3 supplements may not cut heart disease risk. Reuters. Feb 3, 2018 https://www.reuters.com/article/us-health-heart-omega3-supplements/omega-3-supplements-may-not-cut-heart-disease-risk-idUSKBN1FM2UR
- 25.Vasquez A. Review of “Associations of Omega-3 Fatty Acid Supplement Use with Cardiovascular Disease Risks. JAMA. doi: 10.1001/jamacardio.2017.5205. Cardiology 2018” Video: https://vimeo.com/255648523 PDF: http://www.academia.edu/35935996. [DOI] [PMC free article] [PubMed]
- 26.Harris WS. Omega-3 fatty acids and cardiovascular disease: a case for omega-3 index as a new risk factor. Pharmacol Res. 2007. Mar;55(3):217-23 PMCID: PMC1899522 DOI: 10.1016/j.phrs.2007.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Albert BB, Derraik JG, Brennan CM, et al. Higher omega-3 index is associated with increased insulin sensitivity and more favourable metabolic profile in middle-aged overweight men. Sci Rep. 2014. Oct 21;4:6697 doi: 10.1038/srep06697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris WS, Del Gobbo L, Tintle NL. The Omega-3 Index and relative risk for coronary heart disease mortality: Estimation from 10 cohort studies. Atherosclerosis. 2017. Jul;262:51-54. doi: 10.1016/j.atherosclerosis.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Jenkins DJA, Spence JD, Giovannucci EL, et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J Am Coll Cardiol. 2018. Jun 5;71(22):2570-2584. doi: 10.1016/j.jacc.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 30.Liu JJ, Bell CM, Matelski JJ, Detsky AS, Cram Payments by US pharmaceutical and medical device manufacturers to US medical journal editors: retrospective observational study. BMJ. 2017; 359 doi: https://doi.org/10.1136/bmj.j4619. See also: “Worst on that list is the Journal of the American College of Cardiology (JACC), where 19 of its editors received, on average, US$475,072 personally and another US$119,407 for ‘research’.” Macdonald F. This Is the Sickening Amount Pharmaceutical Companies Pay Top Journal Editors. 12 Apr 2018 https://www.sciencealert.com/how-much-top-journal-editors-get-paid-by-big-pharma-corrupt [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vasquez A. Brief Critique of “Supplemental Vitamins and Minerals for CVD Prevention and Treatment” in Journal of the American College of Cardiology 2018: Video presentation https://vimeo.com/273402598 and transcript academia.edu/36790803 2018 Jun.
- 32.ASCEND Study Collaborative Group. Bowman L, Mafham M, Wallendszus K, et al. Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus. N Engl J Med. 2018. Oct 18;379(16):1540-1550. doi: 10.1056/NEJMoa1804989 [DOI] [PubMed] [Google Scholar]
- 33.Vasquez A. Brief Critique of “Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus: ASCEND Study” N Engl J Med 2018. Aug https://vimeo.com/287650812 and Critique of “Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus: ASCEND Study” N Engl J Med. 2018 Aug https://vimeo.com/287266715. [DOI] [PubMed]
- 34.Hu FB. The Mediterranean diet and mortality—olive oil and beyond. N Engl J Med. 2003. Jun 26;348(26):2595-6. [DOI] [PubMed] [Google Scholar]
- 35.Gammelmark A, Madsen T, Varming K, et al. Low-dose fish oil supplementation increases serum adiponectin without affecting inflammatory markers in overweight subjects. Nutr Res. 2012. Jan;32(1):15-23. doi: 10.1016/j. nutres.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 36.Brzeski M, Madhok R, Capell HA. Evening primrose oil in patients with rheumatoid arthritis and side-effects of non-steroidal anti-inflammatory drugs. Br J Rheumatol. 1991. Oct;30(5):370-2. [DOI] [PubMed] [Google Scholar]
- 37.Stark KD, Van Elswyk ME, Higgins MR, Weatherford CA, Salem N., Jr Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog Lipid Res. 2016. Jul;63:132-52. doi: 10.1016/j.plipres.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 38.Vasquez A. Comment on Effects of n-3 Fatty Acid Supplements in Diabetes Mellitus: ASCEND Study. N Engl J Med. 2018. Aug [rejected] https://www.academia.edu/37964035. [DOI] [PubMed]
- 39.Bhatt DL, Steg PG, Miller M, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019. Jan 3;380(1):11-22. doi: 10.1056/NEJMoa1812792. [DOI] [PubMed] [Google Scholar]
- 40.Harvard Heart Letter. Prescription-strength omega-3 fatty acids to prevent heart disease? A drug made from a highly purified fat from fish reduced cardiovascular events in people with heart disease or diabetes. Published: February, 2019 https://www.health.harvard.edu/heart-health/prescription-strength-omega-3-fatty-acids-to-prevent-heart-disease.
- 41.Vasquez A. Bad Science in Medical Nutrition: Politics of Fish Oil. 2019. Feb. Video presentation https://vimeo.com/314997927 and PDF “Critique of “Prescription-strength omega-3 fatty acids to prevent heart disease” by Harvard Medical School 2019 Feb” (in preparation): https://www.academia.edu/38289348.
- 42.The effects of mineral oil. JAMA. 1947. Oct;135(8):512-513. doi:10.1001/ jama.1947.02890080042011 [Google Scholar]
- 43.Robertson WE. The effects of mineral oil. JAMA 1947. Nov;135(12):790 doi:10.1001/jama.1947.02890120044023 [Google Scholar]
- 44.McDonald RF. The effects of mineral oil. JAMA 1947. Nov;135(12):790 doi:10.1001/jama.1947.02890120044024 [Google Scholar]
- 45.Morgan JW. The harmful effects of mineral oil (liquid petrolatum) purgatives. JAMA 1941. Oct;117(16):1335-1336. doi:10.1001/jama.1941.02820420027008 [Google Scholar]
- 46.Herper M. Amarin’s Fish-Oil-Derived Drug Shows Great Promise—With Big Caveats. Forbes 2018. (Nov 10) https://www.forbes.com/sites/ matthewherper/2018/11/10/fish-oil-derived-drug-shows-great-promise--with-big-caveats/
- 47.Cruickshank B. Follicular (mineral oil) lipidosis: I. Epidemiologic studies of involvement of the spleen. Hum Pathol. 1984. Aug;15(8):724-30 [DOI] [PubMed] [Google Scholar]
- 48.Cruickshank B, Thomas MJ. Mineral oil (follicular) lipidosis: II. Histologic studies of spleen, liver, lymph nodes, and bone marrow. Hum Pathol. 1984. Aug;15(8):731-7. [DOI] [PubMed] [Google Scholar]
- 49.Nochomovitz LE, Uys CJ, Epstein S. Massive deposition of mineral oil after prolonged ingestion. S Afr Med J. 1975. Dec 13;49(53):2187-90. [PubMed] [Google Scholar]
- 50.Pitkin RM, Branagan MA, Burmeister LF. Accuracy of data in abstracts of published research articles. JAMA. 1999. Mar 24-31;281(12):1110-1. [DOI] [PubMed] [Google Scholar]
- 51.Berwanger O, Ribeiro RA, Finkelsztejn A, et al. The quality of reporting of trial abstracts is suboptimal: survey of major general medical journals. J Clin Epidemiol. 2009. Apr;62(4):387-92. [DOI] [PubMed] [Google Scholar]
- 52.Kemper KJ, Hood KL. Does pharmaceutical advertising affect journal publication about dietary supplements? BMC Complement Altern Med. 2008. Apr 9;8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sorokowski P, Kulczycki E, Sorokowska A, Pisanski K. Predatory journals recruit fake editor. Nature. 2017. Mar 22;543(7646):481-483. [DOI] [PubMed] [Google Scholar]
- 54.Chow JTY, Turkstra TP, Yim E, Jones PM. The degree of adherence to CONSORT reporting guidelines for the abstracts of randomised clinical trials published in anaesthesia journals: A cross-sectional study of reporting adherence in 2010 and 2016. Eur J Anaesthesiol. 2018. Sep 17:942-948. [DOI] [PubMed] [Google Scholar]


