Abstract
Prior research has shown associations between opioid misuse and suicidal behaviors, but the relationship between medical opioid use and suicidal behaviors is not known. We assessed associations of opioid use and misuse with suicidal ideation, suicide plans, and suicide attempts among adults aged 18–64 years (n = 86,186) using nationally representative cross-sectional data from the 2015 and 2016 administrations of the National Survey on Drug Use and Health. We used logistic regression to estimate associations between opioid use/misuse and suicidal behaviors and propensity score–weighted logistic regression analysis to examine the counterfactual scenario in which persons with misuse had instead not misused opioids. In propensity score–weighted analyses, compared with opioid misuse, opioid use without misuse was associated with lower odds of suicidal ideation (odds ratio (OR) = 0.57, 95% confidence interval (CI): 0.45, 0.72) and suicide plans (OR = 0.53, 95% CI: 0.35, 0.80), and no use was associated with lower odds of suicidal ideation (OR = 0.62, 95% CI: 0.49, 0.80), suicide plans (OR = 0.56, 95% CI: 0.39, 0.79), and suicide attempts (OR = 0.54, 95% CI: 0.33, 0.89). These findings suggest that opioid misuse is associated with greater odds of suicidal behaviors, but opioid use without misuse is not. Compared with persons with opioid misuse, similar persons without misuse have a reduced risk of suicidal behaviors. Clinical and public health interventions should focus on preventing misuse of opioids.
Keywords: attempted suicide, nonmedical medication use, opioid abuse, opioids, prescription drug misuse, suicidal ideation, suicide
For the first time in decades, US life expectancy declined 2 years in a row from 2014 to 2016 (1, 2). While mortality from 7 of the 10 leading causes of death decreased, mortality from suicide and unintentional injuries—including drug overdoses—increased. Unintentional opioid overdose is now a leading public health and clinical concern, and evidence further suggests that the national opioid epidemic has also contributed to the recent increase in suicide. The proportion of suicides directly attributable to opioids approximately doubled from 1999 to 2014 (3). Suicide also contributes to excess mortality among persons with opioid use disorder (OUD) (4, 5) and among persons who die within 1 year of experiencing a nonfatal opioid overdose (6).
These national trends focus attention on the complex relationships between opioid use and suicidal behaviors. One study using nationally representative epidemiologic data found no association between suicide attempts and opioid misuse but revealed a positive association between suicidal ideation and former misuse, persistent misuse, and prescription OUD (7). However, persons who began misusing opioids in the past 2 years were not at increased risk of suicidal ideation (7). Another study showed an association between suicidal ideation and past-year opioid misuse (8), and a third study found that more frequent opioid misuse was associated with suicidal ideation, suicide plans, and suicide attempts (9).
To our knowledge, no studies have examined the association between opioid use without misuse (i.e., medical opioid use as directed by a physician) and suicidal behaviors, yet this relationship is potentially important because of the strong association between suicidal behavior and chronic pain, which is the primary clinical indication for use of prescription opioids. Surveys of US (10), Canadian (11), Australian (12), and multinational (13) samples have demonstrated a relationship between chronic pain conditions and increased risk of past-year and lifetime suicidal behaviors. Prospective research has also revealed that pain is strongly associated with suicide death (14). However, little is known about the relationship between medical opioid use and suicidal behaviors. In a 2015 national survey, among adults with suicidal ideation who had used opioids in the past year, nearly 70% were medical opioid users who did not misuse opioids (15), but it is unclear whether and to what extent medical use of opioids independently contributes to risk of suicidal behaviors. We addressed this knowledge gap by analyzing risk factors associated with suicidal behaviors in adults with no past-year opioid use, adults with past-year use but no misuse (i.e., medical use as directed by a physician), and adults with past-year misuse (i.e., use in any way not directed by a physician). Our goal was to inform efforts to prevent suicidal behaviors within the opioid-using population by evaluating whether the increased risk of suicidal behaviors associated with opioids extends to opioid use without misuse (16).
METHODS
We analyzed cross-sectional data from the 2015 and 2016 administrations of the National Survey on Drug Use and Health (NSDUH), conducted annually among noninstitutionalized persons in the United States (17, 18). The NSDUH samples persons in all 50 states and the District of Columbia to obtain nationally representative estimates of drug use and mental health problems, collecting data from over 60,000 people each year using computer-assisted interviewing methods. Weighted interview response rates were 69.7% in 2015 and 68.4% in 2016. Detailed information regarding NSDUH methods can be found in the 2015 and 2016 NSDUH methodological resource books (19, 20).
Respondents were asked about any past-year use of prescription drugs, including opioids, and then about past-year misuse for each prescription drug used. Our sample included adults aged 18–64 years, categorized into 3 groups: 1) no past-year opioid use, 2) past-year opioid use without misuse, and 3) past-year opioid misuse.
Measures
Outcome: suicidal behaviors
Suicidal behaviors included any past-year suicidal ideation, plans, or attempts. Respondents were first asked, “At any time in the past 12 months . . . did you seriously think about trying to kill yourself?” Respondents reporting suicidal ideation were then asked 2 additional questions about suicidal behaviors in the past 12 months: 1) whether they had made any plans to kill themselves and 2) whether they had tried to kill themselves. Outcomes for suicidal ideation, plans, and attempts were dichotomous (1 = yes, 0 = no), and respondents could answer “yes” to multiple questions.
Exposure: opioid use/misuse
The opioid screener displays digital pill images and asks respondents, “In the past 12 months, which, if any, of these pain relievers have you used?” Persons reporting no prescription opioid use in the past 12 months were included in the group with no past-year opioid use. Respondents reporting past-year prescription opioid use were prompted to respond to additional questions, including measures of misuse. Misuse was defined as use “in any way a doctor did not direct you to use it/them,” and respondents were provided with examples, including: 1) use without a prescription of one’s own; 2) use in greater amounts, more often, or longer than directed; and 3) use in any other way not directed by a physician. Persons reporting only medical opioid use in the past 12 months (i.e., use only as directed by a physician) were included in the group with past-year opioid use without misuse. Persons reporting any opioid use in the past 12 months that was in any way not directed by a physician were included in the group with past-year opioid misuse.
Additional measures
To control for potential confounding, we included additional measures associated with opioid use/misuse and suicidal behaviors in prior studies. To capture illicit drug use, we included binary measures for past-year use of heroin, cocaine, or methamphetamine. We also included binary measures for any use of simulants or sedatives/tranquilizers because their use may indicate treatment for mental health conditions that are not otherwise captured by NSDUH but have an established relationship to suicidal behaviors and because previous research has shown a relationship between use (with or without misuse or dependence) and suicidal behaviors (21, 22).
We also included binary measures of past-year behavioral health comorbidity. Nicotine dependence was based on responses to questions from the Nicotine Dependence Syndrome Scale (23) and the Fagerström Test of Nicotine Dependence among past-month smokers (24). Depression, alcohol use disorder, and cannabis use disorder were determined by responses to questions based on symptom criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (25). We included a categorical variable for persons with chronic medical conditions (0, 1, or >1 condition) based on responses to a question asking respondents to report “all of the conditions that a doctor or health professional has ever told you that you had.” Conditions included high blood pressure, heart disease, diabetes, cancer, asthma, chronic obstructive pulmonary disease, human immunodeficiency virus/acquired immunodeficiency syndrome, hepatitis B or C, liver cirrhosis, and kidney disease. We included a measure of self-rated health on a 5-point scale from excellent to poor.
In addition, we included sociodemographic measures for sex, age, race/ethnicity, education, employment, income, marital status, parental status (≥1 child or none), health insurance, and residence in an urban area.
Statistical analysis
To examine the counterfactual scenario in which persons with past-year opioid misuse had instead not misused opioids, we used propensity score (PS) weighting to account for differences in observed sociodemographic characteristics (sex, age, race/ethnicity, education, employment, income, marital status, insurance, urban/rural residence, parental status), past-year drug use (heroin, cocaine, methamphetamine, stimulants, sedatives/tranquilizers), comorbidity (depression, nicotine dependence, alcohol use disorder, cannabis use disorder, number of chronic medical conditions), and self-rated health across opioid use/misuse groups.
We calculated propensity scores from separate logistic regression models predicting the probability of opioid misuse in comparison with 1) opioid use without misuse and 2) no opioid use. The PS models were weighted using survey sampling weights (26). This method of using separate logistic regressions performs similarly to or better than calculating PS weights using multinomial logistic regression for multiple study groups (27). We used the propensity scores to calculate weights based on the odds of past-year opioid misuse for each comparison group member and multiplied these weights by the survey sampling weights to obtain new weights to equate each comparison group to the group with past-year opioid misuse with respect to sociodemographic characteristics, past-year drug use, comorbidity, and self-rated health (26). We assessed balance between the group with past-year opioid misuse and each comparison group by calculating the standardized difference in mean values for each covariate before and after PS weighting (28).
We then examined the association between suicidal behaviors and past-year opioid misuse using separate logistic regression models weighted by the combined survey and PS weights and accounting for the complex survey design to obtain nationally representative estimates for each outcome (ideation, plans, and attempts). We calculated the predicted probability of each outcome across the population to display differences in the adjusted rates across opioid use/misuse groups. All 3 PS-weighted models also adjusted for sociodemographic characteristics, past-year drug use, comorbidity, and self-rated health to obtain doubly robust estimates of the association between opioid misuse and suicidal behaviors.
To examine how the relationship between opioid use with and without misuse is potentially modified by past-year drug use and health, we repeated the estimation process for the single outcome of any suicidal behaviors (ideation, plans, or attempts) in each subgroup defined by levels of the potential effect moderators (past-year drug use and self-rated health). We then calculated the predicted probability of any suicidal behaviors from each model to display differences in the adjusted rates for each subgroup with medical opioid use compared with past-year opioid misuse.
Finally, we conducted a sensitivity analysis excluding persons who met criteria for OUD to ensure that associations between each suicidal behavior and past-year opioid misuse were not driven by persons with misuse severe enough to meet OUD criteria.
RESULTS
Unweighted and weighted sample characteristics
The sample included 86,186 adults. Most had no past-year opioid use (n = 55,118), a large minority had past-year opioid use but no misuse (n = 26,085), and 4,983 had past-year opioid misuse. Before PS weighting, adults with past-year opioid misuse differed from adults with use but no misuse and from adults with no use in terms of sociodemographic characteristics, past-year drug use, comorbidity, and self-rated health (Table 1). Compared with those with past-year opioid misuse, greater proportions of persons with no use and persons with use but no misuse were female, older, married, college-educated, and higher-income, while smaller proportions were unemployed, were uninsured, or had past-year drug use or behavioral health comorbidity.
Table 1.
Characteristics (%) of Adults Aged 18–64 Years Before and After Propensity Score Weighting as Compared With Those With Past-Year Opioid Misuse, National Survey on Drug Use and Health, 2015–2016
| Variable | Opioid Misuse (n = 4,983) | Unweighted Samplea | Weighted Sampleb | ||
|---|---|---|---|---|---|
| Opioid Use Without Misuse (n = 26,085) | No Opioid Use (n = 55,118) | Opioid Use Without Misuse (n = 26,085) | No Opioid Use (n = 55,118) | ||
| Suicidal behaviorsc | |||||
| Ideation | 14.1 | 4.5d | 3.0d | 10.9e | 13.5 |
| Plans | 5.2 | 1.3d | 0.7d | 3.5e | 4.3 |
| Attempts | 2.7 | 0.6d | 0.4d | 2.5 | 4.0 |
| Sociodemographic characteristics | |||||
| Sex | |||||
| Female | 44.4 | 56.7d | 49.8d | 44.1 | 46.0 |
| Male | 55.6 | 43.3d | 50.2d | 55.9 | 54.0 |
| Age group, years | |||||
| 18–25 | 24.3 | 10.8d | 15.3d | 25.4 | 29.6e |
| 26–34 | 25.4 | 14.3d | 15.9d | 26.3 | 24.9 |
| 35–49 | 25.4 | 24.6 | 24.9 | 24.8 | 22.7e |
| 50–64 | 19.9 | 28.6d | 24.5d | 18.7 | 18.2 |
| ≥65 | 5.1 | 21.7d | 19.4d | 4.8 | 4.6 |
| Race/ethnicity | |||||
| White | 67.6 | 68.7 | 62.2d | 68.4 | 65.0 |
| Black | 10.5 | 12.5f | 11.5 | 10.6 | 11.3 |
| Hispanic | 15.9 | 12.4d | 17.3 | 15.7 | 17.5 |
| Other | 5.9 | 6.3 | 9.0d | 5.3 | 6.2 |
| Education | |||||
| Less than high school | 15.7 | 12.6d | 13.8e | 16.3 | 15.9 |
| High school graduation | 26.8 | 26.1 | 24.9 | 26.9 | 27.9 |
| Some college | 35.0 | 34.0 | 28.7d | 34.0 | 34.6 |
| College graduation | 22.5 | 27.4d | 32.6d | 22.8 | 21.6 |
| Employment | |||||
| Full-time | 51.2 | 44.9d | 51.0 | 50.7 | 51.3 |
| Part-time | 15.2 | 12.3f | 13.6 | 15.5 | 17.9 |
| No work | 8.7 | 4.2d | 4.6d | 9.1 | 7.2 |
| Other work | 24.9 | 38.6d | 30.9d | 24.8 | 23.6 |
| Annual income, dollars | |||||
| <20,000 | 23.6 | 18.3d | 16.5d | 24.3 | 23.2 |
| 20,000–49,999 | 32.0 | 31.1 | 29.3f | 31.1 | 32.9 |
| 50,000–74,999 | 15.1 | 16.1 | 16.4e | 15.7 | 14.7 |
| ≥75,000 | 29.3 | 34.5d | 37.7d | 28.9 | 29.2 |
| Marital status | |||||
| Single | 45.5 | 23.3d | 28.9d | 47.3 | 49.6 |
| Married | 35.2 | 53.0d | 53.0d | 33.1 | 31.7e |
| Divorced | 15.7 | 16.9 | 12.3d | 16.1 | 15.0 |
| Widowed | 3.6 | 6.8d | 5.8d | 3.5 | 3.6 |
| Health insurance | |||||
| Private | 50.0 | 47.5e | 54.0d | 49.5 | 47.7 |
| Medicaid/SCHIP | 18.3 | 12.3d | 9.8d | 18.6 | 21.0 |
| Medicare | 8.8 | 24.2d | 18.2d | 8.6 | 8.6 |
| Military | 3.1 | 6.5d | 4.6d | 2.8 | 2.8 |
| Other | 3.4 | 2.0d | 2.5e | 3.1 | 3.3 |
| None | 16.5 | 7.5d | 10.9d | 17.4 | 16.6 |
| Urban/rural residence | |||||
| Urban | 54.6 | 51.1f | 55.2 | 55.8 | 58.6e |
| Not urban | 45.4 | 48.9f | 44.8 | 44.2 | 41.4e |
| Parental status | |||||
| No children | 60.4 | 62.8f | 62.6e | 61.8 | 59.1 |
| ≥1 child | 39.6 | 37.2f | 37.4e | 38.2 | 40.9 |
| Past-year drug use | |||||
| Heroin use | 5.6 | 0.2d | 0.1d | 7.6 | 9.3 |
| Cocaine use | 14.5 | 1.5d | 1.3d | 18.3f | 23.0f |
| Methamphetamine use | 5.5 | 0.5d | 0.3d | 7.5 | 7.5 |
| Stimulant use | 25.8 | 8.4d | 4.4d | 28.2 | 31.0 |
| Sedative/tranquilizer use | 50.6 | 31.9d | 10.6d | 50.5 | 53.1 |
| Comorbidity and health | |||||
| Behavioral health conditions | |||||
| Nicotine dependence | 22.5 | 6.0d | 5.1d | 26.1e | 28.5e |
| Alcohol use disorder | 9.1 | 1.1d | 1.0d | 12.6e | 16.2e |
| Cannabis use disorder | 17.1 | 9.0d | 4.7d | 19.9 | 21.9 |
| Depression | 30.8 | 14.7d | 9.0d | 31.9 | 33.3 |
| No. of chronic medical conditions | |||||
| 0 | 62.3 | 49.2d | 63.2 | 62.9 | 61.6 |
| 1 | 24.8 | 29.2d | 25.6 | 24.6 | 25.8 |
| >1 | 12.9 | 21.6d | 11.2 | 12.5 | 12.6 |
| Self-rated health | |||||
| Excellent | 15.0 | 14.7 | 25.2d | 14.8 | 14.7 |
| Very good | 33.3 | 32.4 | 37.2f | 33.1 | 31.5 |
| Good | 33.5 | 32.4 | 27.3d | 32.4 | 32.5 |
| Fair | 14.6 | 15.3 | 8.8d | 15.9 | 17.4 |
| Poor | 3.6 | 5.2f | 1.5d | 3.8 | 3.9 |
Abbreviations: PS, propensity score; SCHIP, State Children’s Health Insurance Program.
a “Unweighted” refers only to PS weighting. Percentages were survey-weighted to be nationally representative and may not add up to 100.
b “Weighted” refers to PS weighting. Percentages were weighted using the product of survey weights and weights derived from propensity scores.
c Suicidal behavior outcomes were not included in PS estimation.
dP < 0.001.
eP < 0.05.
fP < 0.01.
PS weighting achieved good balance across groups for each covariate (see Web Figure 1, available at https://academic.oup.com/aje). After weighting, all groups had similar distributions of sex, race/ethnicity, education, employment, income, health insurance, parental status, chronic medical conditions, and self-rated health compared with those with past-year opioid misuse. Some differences between groups remained but were diminished after weighting. A greater proportion of persons with no use and with use but no misuse had past-year cocaine use, nicotine dependence, and alcohol use disorder compared with those with past-year opioid misuse. In addition, greater proportions of those with no past-year opioid use than those with past-year opioid misuse were 18–25 years of age and lived in urban areas, while a smaller proportion was married (Table 1).
Suicidal ideation, plans, and attempts
Table 2 shows PS-adjusted results for suicidal ideation, suicide plans, and suicide attempts after weighting persons with no use and persons with use but no misuse to resemble those with past-year opioid misuse in terms of sociodemographic characteristics, drug use, comorbidity, and self-rated health and after adjusting for any remaining differences across groups. Compared with persons with past-year opioid misuse, those with past-year opioid use without misuse had lower odds of suicidal ideation (odds ratio (OR) = 0.57, 95% confidence interval (CI): 0.45, 0.72) and suicide plans (OR = 0.53, 95% CI: 0.35, 0.80), and those with no past-year opioid use had lower odds of suicidal ideation (OR = 0.62, 95% CI: 0.49, 0.80), suicide plans (OR = 0.56, 95% CI: 0.39, 0.79), and suicide attempts (OR = 0.54, 95% CI: 0.33, 0.89).
Table 2.
Adjusted Propensity Score–Weighted Logistic Regression Estimates of Past-Year Suicidal Ideation, Suicide Plans, and Suicide Attempts (n = 86,186), National Survey on Drug Use and Health, 2015–2016a,b
| Past-Year Opioid Use/Misuse | Suicidal Ideation | Suicide Plans | Suicide Attempts | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| No opioid use | 0.62 | 0.49, 0.80 | 0.56 | 0.39, 0.79 | 0.54 | 0.33, 0.89 |
| Opioid use without misuse | 0.57 | 0.45, 0.72 | 0.53 | 0.35, 0.80 | 0.71 | 0.46, 1.10 |
| Opioid misuse | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
Abbreviations: CI, confidence interval; OR, odds ratio.
a All models controlled for sociodemographic characteristics (sex, age, race/ethnicity, education, employment, income, marital status, insurance, urban/rural residence, parental status), past-year drug use (heroin, cocaine, methamphetamine, stimulants, sedatives/tranquilizers), comorbidity (depression, nicotine dependence, alcohol use disorder, cannabis use disorder, number of chronic medical conditions), and self-rated health.
b ORs and CIs were computed with propensity score–weighted data.
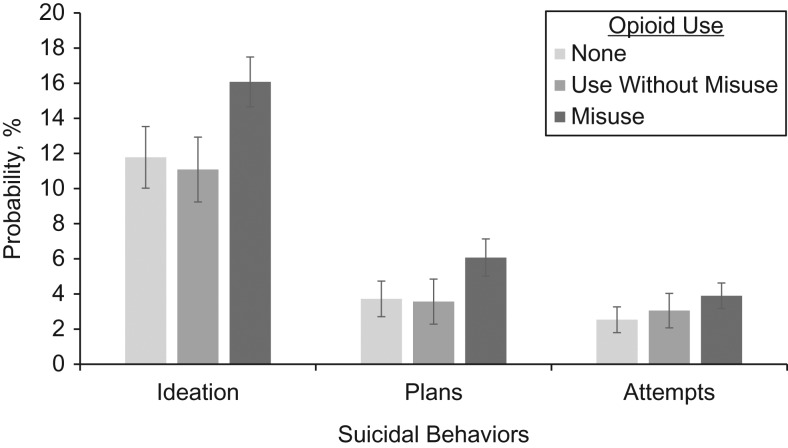
Figure 1 shows the predicted probability of each suicidal behavior calculated from PS-weighted logistic regression analyses for each outcome. In addition, Figure 1 shows the significance level for the predicted difference in the probability of each suicidal behavior for persons with opioid use without misuse and persons with no opioid use compared with the reference group of persons with past-year opioid misuse. Compared with past-year opioid misuse, opioid use without misuse was associated with a 31% relative reduction in the probability of ideation (−5.0 percentage points; 95% CI: −7.0, −3.0) and a 41% reduction in the probability of plans (−2.5 percentage points; 95% CI: −3.9, −1.1). Similarly, no opioid use was associated with a 27% relative reduction in the probability of ideation (−4.3 percentage points; 95% CI: −6.5, −2.1), a 39% reduction in the probability of plans (−2.4 percentage points; 95% CI: −3.7, −1.0), and a 22% reduction in the probability of attempts (−1.4 percentage points; 95% CI: −2.4, −0.3).
Figure 1.
Adjusted differences in the probabilities of past-year suicidal ideation, suicide plans, and suicide attempts for persons with no opioid use, persons with opioid use without misuse, and persons with opioid misuse, National Survey on Drug Use and Health, 2015–2016. Predicted probabilities and differences in predicted probabilities compared with the reference group of persons with past-year opioid misuse were derived from propensity score–weighted logistic regression analyses estimating results for each suicidal behavior (ideation, plans, and attempts). All models controlled for sociodemographic characteristics (sex, age, race/ethnicity, education, employment, income, marital status, insurance, urban/rural residence, parental status), past-year drug use (heroin, cocaine, methamphetamine, stimulants, sedatives/tranquilizers), comorbidity (depression, nicotine dependence, alcohol use disorder, cannabis use disorder, number of chronic medical conditions), and self-rated health. Compared with opioid misuse, no opioid use was associated with significantly lower probability of suicidal ideation (P < 0.001), plans (P = 0.001), and attempts (P = 0.01), and opioid use without misuse was associated with significantly lower probability of suicidal ideation (P < 0.001) and plans (P < 0.001). Bars, 95% confidence intervals.
Effect modification of the association between opioid use/misuse and suicidal behaviors by past-year drug use and health
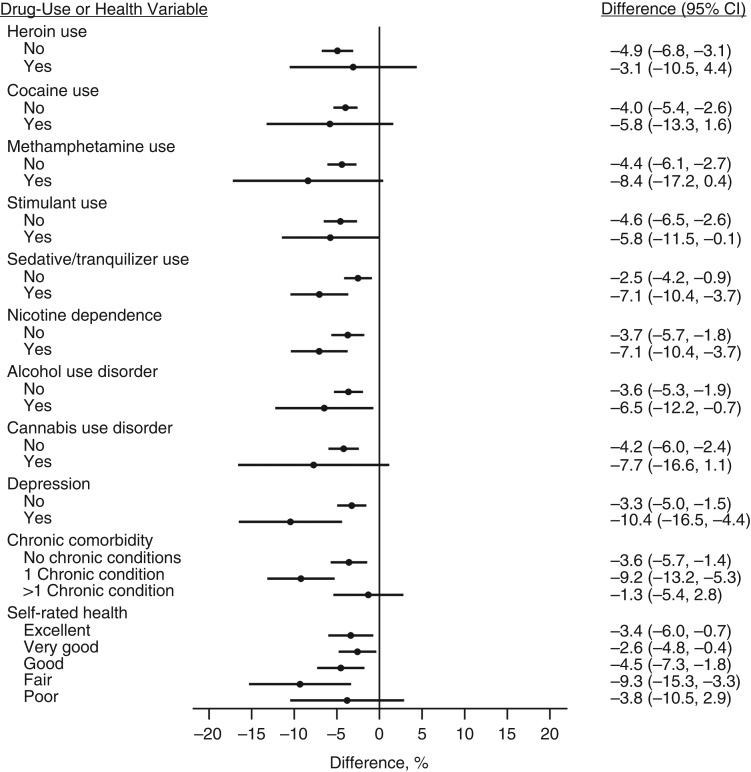
Figure 2 shows differences in the predicted probability of any suicidal behavior (ideation, plans, or attempts) calculated from PS-weighted logistic regression analyses for each subgroup level. Compared with past-year opioid misuse, opioid use without misuse was associated with significant reductions in the probability of suicidal behaviors among those with no past-year use of other drugs (heroin, cocaine, methamphetamine, stimulants, or sedatives/tranquilizers). However, there were no significant differences in the risk of suicidal behaviors for opioid use without misuse as compared with past-year opioid misuse among persons with past-year use of heroin (−3.1 percentage points; 95% CI: −10.5, 4.4), cocaine (−5.8 percentage points; 95% CI: −13.3, 1.6), or methamphetamine (−8.4 percentage points; 95% CI: −17.2, 0.4). Compared with past-year opioid misuse, opioid use without misuse was associated with significant reductions in the probability of suicidal behaviors among persons with no comorbidity. However, there were no significant differences in the risk of suicidal behaviors for opioid use without misuse compared with past-year opioid misuse among those who met criteria for a cannabis use disorder (−7.7 percentage points; 95% CI: −16.6, 1.1) or those with more than 1 chronic medical condition (−1.3 percentage points; 95% CI: −5.4, 2.8). Among those with self-rated health ranging from “fair” to “excellent,” opioid use without misuse was associated with significant reductions in the probability of suicidal behaviors compared with past-year opioid misuse. However, among those with “poor” self-rated health, opioid use without misuse was not associated with a significantly different risk of suicidal behaviors compared with past-year opioid misuse (−3.8 percentage points; 95% CI: −10.5, 2.9).
Figure 2.
Adjusted difference (percentage points) in the probability of any past-year suicidal ideation, plans, or attempts among persons with past-year opioid use without misuse versus those with past-year opioid misuse, by past-year drug use and health, National Survey on Drug Use and Health, 2015–2016. Differences in predicted probabilities were derived from propensity score–weighted logistic regression analyses estimating the risk of any suicidal behaviors (ideation, plans, or attempts) within each subgroup of each covariate, compared with the reference group of persons with past-year opioid misuse. All models controlled for sociodemographic characteristics (sex, age, race/ethnicity, education, employment, income, marital status, insurance, urban/rural residence, parental status), past-year drug use (heroin, cocaine, methamphetamine, stimulants, sedatives/tranquilizers), comorbidity (depression, nicotine dependence, alcohol use disorder, cannabis use disorder, number of chronic medical conditions), and self-rated health. Bars, 95% confidence intervals (CIs).
Sensitivity analyses
Results of sensitivity analyses carried out among persons who did not meet criteria for OUD (n = 85,376) resembled the main findings, indicating that the association between suicidal behaviors and opioid use/misuse was not driven by persons with misuse severe enough to meet OUD criteria (Web Table 1).
DISCUSSION
Findings
To our knowledge, this is the first study to have examined relationships between opioid use with and without misuse and suicidal behaviors. We found no evidence that opioid use without misuse is associated with suicidal ideation, plans, or attempts after controlling for sociodemographic characteristics, past-year drug use, comorbidity, and self-rated health. However, opioid misuse is independently associated with increased risk of suicidal ideation, plans, and attempts. These findings suggest that if persons with opioid misuse had instead not misused opioids, their risk of suicidal behaviors would be lower. The magnitudes of these decreases were similar for persons with no use and persons with use but no misuse, suggesting that interventions should focus on preventing misuse.
Guidelines for opioid prescribing recommend risk assessment prior to initiation and periodically throughout treatment, including screening for opioid misuse and ensuring safe use with validated screening tools, urinalysis, and prescription monitoring (29, 30). Screening tools focus on predicting and measuring opioid misuse, but those with a stronger evidence base also include measures to detect emotional problems, including thoughts of self-harm (31). As research on opioid misuse screening tools grows, future studies should examine the extent to which they effectively identify high-risk individuals as part of a suicide prevention strategy.
Effective medical care may also help address clinical characteristics that are associated with risk of suicidal behaviors. Prior studies examining opioid misuse (8, 9) and studies outside the context of opioid use (32) have shown that chronic medical comorbidity and self-rated health are associated with suicidal behaviors. In this study, risk of suicidal behaviors was lower for opioid use without misuse than for opioid misuse among persons with 1 or fewer chronic medical conditions and among persons with fair-to-excellent self-rated health. However, risks of suicidal behaviors were similar for opioid use with misuse and opioid use without misuse among persons with more than 1 chronic medical condition and persons with poor self-rated health.
Since persons with multiple chronic medical conditions or poor self-rated health have similarly elevated risks of suicidal behaviors with medical opioid use or opioid misuse, this finding, along with previous research, raises the possibility that unmeasured symptoms, such as pain, may mediate the relationship between general health and suicidal behaviors (32). The NSDUH data do not include measures of pain or indicators for chronic pain conditions, though pain has been related to both opioid use/misuse (33) and suicidal behavior (10–14), highlighting the importance of continuously monitoring patients’ pain symptoms and functional status (29, 30). Recommendations for opioid prescribing include clinical assessment and treatment of chronic medical conditions that may be related to patients’ pain symptoms, in addition to regular review of current comorbidity (e.g., substance use disorder, sleep-disordered breathing, pregnancy) and treatments (e.g., sedatives) that may be associated with increased risk of opioid-related harms (29, 30).
Risk of suicidal behaviors was lower for opioid use without misuse than for opioid misuse among persons without past-year use of heroin, cocaine, or methamphetamine and among persons who did not meet criteria for a cannabis use disorder. However, risks of suicidal behaviors were similar for opioid misuse and opioid use without misuse among persons with past-year use of heroin, cocaine, or methamphetamine and among those who met criteria for cannabis use disorder. These findings could indicate that these groups have similarly elevated risks of suicidal behaviors with medical opioid use or misuse. Alternatively, the lower risk estimates observed in each group may have failed to reach statistical significance because of the relatively small number of persons with past-year cannabis use disorder and past-year use of heroin, cocaine, and methamphetamine. While clinical recommendations suggest urine screening for current substance use (29) and evaluating patients’ substance use history (30) to assess risk of opioid misuse and overdose, screening specifically for suicidal behaviors may be the most direct approach for identifying at-risk individuals.
Overall, opioid misuse is associated with increased risk of suicidal behaviors, and this higher risk is relatively consistent across levels of past-year drug use and self-rated health. Interventions should aim to reduce and prevent opioid misuse in a supportive health-care environment capable of providing or referring high-risk individuals to accessible health and social services. Offering suicide or depression screening and adopting effective brief intervention strategies may be particularly useful in general medical settings (34).
Limitations
The NSDUH data are cross-sectional, and we could not determine whether opioid use and misuse preceded suicidal behaviors. Longitudinal research is needed to evaluate whether opioid use/misuse leads to suicidal behaviors. In addition, although we adjusted for a wide range of individual characteristics, residual confounding could have resulted from unobserved factors. Finally, the NSDUH survey employs a self-reporting format, which is subject to 2 main limitations. First, the survey questions cover sensitive material about drug use and health that could lead to over- or underreporting of some symptoms and behaviors, including opioid misuse. To minimize social desirability bias, computer-assisted interviewing is used to enhance the privacy and confidentiality of responses. Second, responses depend on participants’ memory of past experiences, which could result in some inaccurate reporting. To minimize recall bias, the NSDUH surveys incorporate procedures to enhance recall, but drug use that results in cognitive impairment may be particularly susceptible to this bias.
Conclusions
Overall, our findings suggest that reducing and preventing opioid misuse may prevent suicidal behavior. At the same time, explicit suicide prevention efforts and practices aimed at reducing other opioid-related problems may also be helpful. Clinical and public health interventions should focus on reducing and preventing opioid misuse while adopting strategies that are sensitive to potential differences in the level of risk observed across clinical characteristics, particularly those related to chronic medical conditions.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York (Hillary Samples); Department of Mental Health, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland (Elizabeth A. Stuart); and Department of Psychiatry, Columbia University Irving Medical Center, New York, New York (Mark Olfson).
This work was funded by the National Institute on Drug Abuse (grant T32 DA031099) and the Institute of Education Sciences, US Department of Education (grant R305D150001).
H.S. has received consulting fees from the American Society of Addiction Medicine.
Abbreviations
- CI
confidence interval
- NSDUH
National Survey on Drug Use and Health
- OR
odds ratio
- OUD
opioid use disorder; PS, propensity score.
REFERENCES
- 1. Kochanek KD, Murphy SL, Xu J, et al. . Mortality in the United States, 2016. (NCHS Data Brief no. 293). Hyattsville, MD: National Center for Health Statistics; 2017. https://www.cdc.gov/nchs/data/databriefs/db293.pdf. Accessed May 24, 2018. [Google Scholar]
- 2. Xu J, Murphy SL, Kochanek KD, et al. . Mortality in the United States, 2015. (NCHS Data Brief no. 267). Hyattsville, MD: National Center for Health Statistics; 2016. https://www.cdc.gov/nchs/data/databriefs/db267.pdf. Accessed May 24, 2018. [Google Scholar]
- 3. Braden JB, Edlund MJ, Sullivan MD. Suicide deaths with opioid poisoning in the United States: 1999–2014. Am J Public Health. 2017;107(3):421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76(suppl):S11–S19. [DOI] [PubMed] [Google Scholar]
- 5. Bohnert KM, Ilgen MA, Louzon S, et al. . Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112(7):1193–1201. [DOI] [PubMed] [Google Scholar]
- 6. Olfson M, Crystal S, Wall M, et al. . Causes of death after nonfatal opioid overdose. JAMA Psychiatry. 2018;75(8):820–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kuramoto SJ, Chilcoat HD, Ko J, et al. . Suicidal ideation and suicide attempt across stages of nonmedical prescription opioid use and presence of prescription opioid disorders among US adults. J Stud Alcohol Drugs. 2012;73(2):178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ford JA, Perna D. Prescription drug misuse and suicidal ideation: findings from the National Survey on Drug Use and Health. Drug Alcohol Depend. 2015;157:192–196. [DOI] [PubMed] [Google Scholar]
- 9. Ashrafioun L, Bishop TM, Conner KR, et al. . Frequency of prescription opioid misuse and suicidal ideation, planning, and attempts. J Psychiatr Res. 2017;92:1–7. [DOI] [PubMed] [Google Scholar]
- 10. Braden JB, Sullivan MD. Suicidal thoughts and behavior among adults with self-reported pain conditions in the National Comorbidity Survey Replication. J Pain. 2008;9(12):1106–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ratcliffe GE, Enns MW, Belik S-L, et al. . Chronic pain conditions and suicidal ideation and suicide attempts: an epidemiologic perspective. Clin J Pain. 2008;24(3):204–210. [DOI] [PubMed] [Google Scholar]
- 12. Campbell G, Darke S, Bruno R, et al. . The prevalence and correlates of chronic pain and suicidality in a nationally representative sample. Aust N Z J Psychiatry. 2015;49(9):803–811. [DOI] [PubMed] [Google Scholar]
- 13. Scott KM, Hwang I, Chiu WT, et al. . Chronic physical conditions and their association with first onset of suicidal behavior in the World Mental Health Surveys. Psychosom Med. 2010;72(7):712–719. [DOI] [PubMed] [Google Scholar]
- 14. Juurlink DN, Herrmann N, Szalai JP, et al. . Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164(11):1179–1184. [DOI] [PubMed] [Google Scholar]
- 15. Han B, Compton WM, Blanco C, et al. . Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293–301. [DOI] [PubMed] [Google Scholar]
- 16. Oquendo MA, Volkow ND. Suicide: a silent contributor to opioid-overdose deaths. N Engl J Med. 2018;378(17):1567–1569. [DOI] [PubMed] [Google Scholar]
- 17. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services National Survey on Drug Use and Health (NSDUH-2015). https://datafiles.samhsa.gov/study/national-survey-drug-use-and-health-nsduh-2015-nid16893. Accessed January 4, 2018.
- 18. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services National Survey on Drug Use and Health (NSDUH-2016). https://datafiles.samhsa.gov/study/national-survey-drug-use-and-health-nsduh-2016-nid17184. Accessed January 4, 2018.
- 19. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services 2015 National Survey on Drug Use and Health. Methodological Resource Book Section 8: Data Collection Final Report Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. https://www.samhsa.gov/data/sites/default/files/NSDUHmrbDCFR2015.pdf. Accessed January 10, 2018.
- 20. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services 2016 National Survey on Drug Use and Health. Methodological Resource Book Section 8: Data Collection Final Report Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. https://www.samhsa.gov/data/sites/default/files/NSDUHmrbDCFR2016.pdf. Accessed January 10, 2018.
- 21. Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am J Epidemiol. 2000;151(8):781–789. [DOI] [PubMed] [Google Scholar]
- 22. Goodwin RD, Hasin DS. Sedative use and misuse in the United States. Addiction. 2002;97(5):555–562. [DOI] [PubMed] [Google Scholar]
- 23. Shiffman S, Waters A, Hickcox M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327–348. [DOI] [PubMed] [Google Scholar]
- 24. Heatherton TF, Kozlowski LT, Frecker RC, et al. . The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 25. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 26. Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McCaffrey DF, Griffin BA, Almirall D, et al. . A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. 2013;32(19):3388–3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci 2010;25(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sehgal N, Manchikanti L, Smith HS. Prescription opioid abuse in chronic pain: a review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician. 2012;15(3 suppl):ES67–ES92. [PubMed] [Google Scholar]
- 31. Butler SF, Budman SH, Fernandez KC, et al. . Development and validation of the Current Opioid Misuse Measure. Pain. 2007;130(1-2):144–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Druss B, Pincus H. Suicidal ideation and suicide attempts in general medical illnesses. Arch Intern Med. 2000;160(10):1522–1526. [DOI] [PubMed] [Google Scholar]
- 33. Chou R, Turner JA, Devine EB, et al. . The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention workshop. Ann Intern Med. 2015;162(4):276–286. [DOI] [PubMed] [Google Scholar]
- 34. Hargraves D, White C, Frederick R, et al. . Implementing SBIRT (screening, brief intervention and referral to treatment) in primary care: lessons learned from a multi-practice evaluation portfolio. Public Health Rev. 2017;38:Article 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.