Abstract
The use of hair samples in biomedical research is a rapidly growing field. High acceptability rates for hair collection have been demonstrated in multiple settings. Each setting may have unique issues and, to our knowledge, no previous study has assessed the acceptability of hair sampling for HIV-related research in Nigeria. This study aimed to assess the willingness to donate hair for research among people living with HIV (PLWH). A cross-sectional study was conducted among 381 PLWH in a tertiary institution in Southwest Nigeria, using convenience sampling. An interviewer-administered questionnaire was used to collect data from consenting participants, including a question on willingness to donate hair for research. The mean age of respondents was 42.1 ± 10.5 years and more than three-quarters of the respondents were females. Two hundred and eighty-eight (75.8%) respondents had at least a tertiary education. Only 51.4% of the respondents were willing to donate their hair for research. Possible sample diversion for rituals was the major (60.5%) reason cited for unwillingness to donate hair. In multivariate analysis, respondents with primary education or less exhibited a trend toward being more willing to donate hair than those with secondary education or more (p = .091). Muslims were 1.7 times more willing to donate hair than Christians even after adjusting for other demographic covariates (95% confidence interval: 1.11–2.72); p = .016. There is a moderate willingness to donate hair for research among our population of PLWH in Nigeria. These results underscore the importance of cultural sensitivity and community education when introducing innovative HIV research techniques to new settings.
Keywords: acceptability rate, adherence monitoring, antiretroviral drugs, beliefs, biomedical research, hair collection, HIV
Introduction
HIV-related research has led to massive improvements in morbidity and mortality from HIV infection worldwide. Biological specimens are frequently collected from participants in the conduct of HIV research, including plasma, dried blood spot (DBS), cerebrospinal fluid, and hair, among others. Each type of biospecimen has various rates of acceptability and feasibility when collected in the context of HIV research.
The use of hair samples in HIV-related research is a rapidly growing field. However, this important research area has received little or no attention in Nigeria. The concentration of medications in hair reflects drug uptake from the systemic circulation over weeks to months, enabling antiretroviral (ARV) levels in hair to serve as a useful and objective biomarker for evaluating adherence1–4 and drug exposure5,6 over time. Different methods used to assess ARV adherence and assays to analyze many ARVs in hair have also been developed and validated.7–10 Adherence monitoring using hair ARV levels has some advantages over other methods, such as pharmacy refills, pill counts, self-report, Medication Event Monitoring System (MEMS), and measuring ARV concentrations in plasma, DBS, or urine.
Self-report can be affected by recall ability and “social desirability bias” (i.e., answering questions to meet the researcher's expectation).8 Poor recording undermines the accuracy of pill count and pharmacy refill data, while MEMS can be affected by signal disruption and not all container cap openings result in drug consumption.9 In addition, interpretation of MEMS data may be challenging in patients on complex medication regimens.11 On the other hand, the use of some pharmacologic approaches to assess short-term adherence, like plasma or urine levels of ARV medications, may be limited by “white coat effects,”12 wherein patients increase their adherence a few days before their clinic visit. In that case, a single plasma level may not reflect long-term patterns of adherence. Compared to hair, DBS measures also reflect relatively short-term adherence for drugs that are not intracellularly processed (e.g., tenofovir).
Hair grows at an average rate of 1 cm per month,13 allowing for long-term adherence and exposure to medications to be assessed, and further allowing for segmental analysis to determine adherence at different points in time based on drug concentrations measured in different segments of hair from the proximal scalp.14–16 Hair levels provide additional advantages over blood/plasma and urine concentrations due to day-to-day (intraindividual) variation in plasma levels.17 Furthermore, hair sampling is painless and noninvasive, and may be particularly applicable to resource-limited settings since phlebotomy is not required and the sample can be stored and shipped at room temperature without biohazard concerns. ARV concentrations in home-collected hair samples are equivalent to those collected by field staff, indicative of the ease of hair sample collection.18 Hair ARV levels are one of the strongest predictors of virologic failure/success4,18–22 and have also been used to monitor ARV-related toxicities.23,24
However, the acceptability of hair collection among different groups has varied, ranging from the 60% level among men-who-have-sex-with-men in the United States24 to >95% in many African and Asian settings.3,19,20,24,25 Despite the benefits of using hair as a biomarker for adherence monitoring in resource-limited settings and the enormous burden of HIV infection in Nigeria,26,27 no research has been conducted to date in Nigeria on the acceptability of hair collection for research. In this report, we addressed this knowledge gap in the literature by assessing the willingness of people living with HIV (PLWH) in Southwest Nigeria to donate hair for biomedical research.
Materials and Methods
Study site and study population
The study site was the HIV Clinic of the Infectious Disease Institute (IDI), College of Medicine, University of Ibadan (UI), Nigeria. This clinic covers the entire Southwestern region of Nigeria and beyond. Most patients pick their drugs once every month. All PLWH receiving care at IDI were eligible to participate and those who gave their consent were recruited for this study from June 2017 to July 2017. This initial survey-based study was performed to determine the feasibility of a planned larger study, to determine adherence to antiretroviral therapy through hair levels in the clinic.
Sample size and sampling procedure
The sample size for this study was estimated using the formula for single proportions and we used an estimate of the proportion who would accept hair sampling (54.3%) from another study, which examined the proportion of respondents in a Southwestern Nigeria clinic willing to donate biological samples for future research.28 Assuming a precision of 5%, a type 1 error of 5%, and a population <10,000, we estimated a sample size of 381 and used this number as the target number for enrollment using convenience sampling. Patients in the waiting room of the HIV Clinic were approached each day and willing participants were then consented and asked to fill out the questionnaire until the required sample size was reached. Enrolment occurred over a period of 1 month and the requisite sample size was reached in that period.
Study instrument and data collection
An interviewer-administered quantitative survey was used to obtain information on respondents' demographic characteristics, willingness to donate biological samples (including hair) for research purpose, reasons for unwillingness to donate hair, and factors associated with the willingness to donate a hair sample. Multiple response questions were used to assess the willingness of the respondents to donate hair and the reasons for declining. The questionnaire was reviewed in-house among experts in epidemiology and medical sociology, and a medical statistician for face, construct, and content validity. The questionnaires were administered to consenting respondents one-on-one in a secluded area just off the waiting room, allowing for privacy.
Data analysis
Data were entered and analyzed using SPSS version 20.0 (IBM Corp., Chicago, IL). Descriptive statistics were used to describe the general characteristics of the sample. The chi-square test and multivariable logistic regression model were used to identify factors independently associated with willingness to donate hair for research purpose. The statistical significance of all tests was set at p < .05 (95% confidence interval).
Ethics statement
This study was approved by the joint UI/University College Hospital (UCH) ethics committee, UI. Approval was also obtained from the HIV clinic of the IDI, College of Medicine, UI. Participants provided written consent in English or the Yoruba Language before answering the questions provided in the questionnaire.
Results
Sociodemographic characteristic of respondents
Three hundred and eighty-one (381) PLWH receiving care at the IDI, College of Medicine, UI, participated in the study out of the 397 approached, giving a response rate of 96%. There were 295 females (77.4%) and 86 males (22.6%). The mean age of respondents was 42.1 ± 10.5 years and 201 (52.9%) of the respondents were older than 40 years. More than three-quarters of the respondents had at least a secondary education. Respondents were predominantly Christians (66.3%). Nearly three-quarters of the respondents were currently married (Table 1).
Table 1.
Sociodemographic Characteristic of Respondents (n = 381)
| Characteristic | N (%) |
|---|---|
| Sex | |
| Male | 86 (22.6) |
| Female | 295 (77.4) |
| Age (years) | |
| ≤30 | 44 (11.6) |
| 31–40 | 135 (35.5) |
| >40 | 201 (52.9) |
| Ethnicity | |
| Yoruba | 303 (79.5) |
| Igbo | 50 (13.1) |
| Hausa | 13 (3.4) |
| Othersa | 15 (3.9) |
| Marital status | |
| Never married | 50 (13.2) |
| Currently married | 276 (72.6) |
| Previously married | 54 (14.2) |
| Education | |
| Primary and below | 92 (24.2) |
| Secondary and above | 288 (75.8) |
| Religion | |
| Islam | 128 (33.7) |
| Christianity | 252 (66.3) |
| Occupation | |
| Unemployed | 32 (8.4) |
| Trading | 209 (54.9) |
| Skilled workers | 74 (19.4) |
| Professional | 66 (17.3) |
Ibibio = 5 (1.3%), Efik = 3 (0.8%), Tiv = 3 (0.8%), Non-Nigerians = 2 (0.5%), Idoma = 1 (0.3%), Igede = 1 (0.3%).
Factors associated with respondents' willingness to donate their hair for research
When asked as a Yes/No question, 196 individuals (51.4%) expressed a willingness to donate hair for biomedical research. In bivariate analysis, a higher percentage of younger respondents (≤30 years) than older ones were willing to donate their hair for research, but the difference was not statistically significant (p = .563). There was higher acceptability to donate hair for research among those with no formal education and primary education, or less compared to those with higher education. (p = .019). In addition, Muslims were more willing to donate hair for research than Christians (p = .004). Table 2 shows the association between the factors considered and the willingness to donate hair for research.
Table 2.
Factors Associated with Respondents' Willingness to Donate Their Hair for Research
| Independent variables | Cross tabulation | Logistic regression | |||
|---|---|---|---|---|---|
| Willingness to donate hair | p | OR | 95% CI OR | P | |
| Sex | |||||
| Male | 50 (58.1) | .158 | |||
| Female | 146 (49.5) | ||||
| Age (years) | |||||
| ≤30 | 26 (59.1) | ||||
| 31–40 | 69 (51.1) | .563 | |||
| >40 | 101 (50.2) | ||||
| Ethnicity | |||||
| Yoruba | 156 (51.5) | ||||
| Igbo | 24 (48.0) | .852 | |||
| Hausa | 8 (61.5) | ||||
| Othersa | 8 (53.3) | ||||
| Education | |||||
| ≤Primary | 57 (62.0) | .019* | 1.54 | .93–2.53 | .091 |
| ≥Secondary (Ref.) | 138 (47.9) | 1 | |||
| Religion | |||||
| Islam | 79 (61.7) | .004* | 1.73 | 1.11–2.72 | .016* |
| Christianity (Ref.) | 116 (46.0) | 1 | |||
| Occupation | |||||
| Unemployed | 18 (56.2) | ||||
| Trading | 110 (52.6) | .714 | |||
| Skilled workers | 38 (51.4) | ||||
| Professional | 30 (45.5) | ||||
| Marital status | |||||
| Never married | 26 (52.0) | ||||
| Currently married | 146 (52.9) | .523 | |||
| Previously married | 24 (44.4) | ||||
Other ethnic groups: Ibibio = 5 (1.3%), Efik = 3 (0.8%), Tiv = 3 (0.8%), Non-Nigerians = 2 (0.5%), Idoma = 1 (0.3%), Igede = 1 (0.3%).
Statistically significant at p < .05.
CI, confidence interval; OR, odds ratio; Ref., reference category.
In a multivariate regression model (Table 2), those with primary education or less were 1.54 times more willing to donate hair for research purpose than those who had higher qualifications, with a trend toward statistical significance (p = .091). The association between religion and willingness to donate hair remained significant in multivariate analysis. Specifically, Muslims had a 73% higher odds of willingness to donate hair samples for research than Christians (p = .016).
Respondents' willingness to donate biological samples for research and reasons for unwillingness
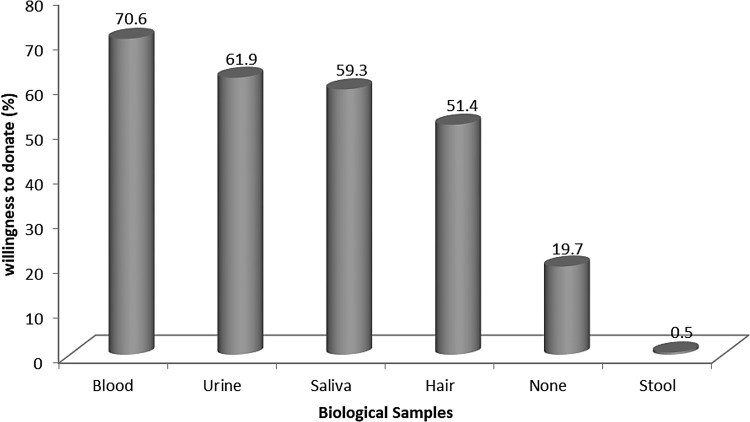
The majority (70.6%) of respondents were willing to donate blood. This was followed by urine (61.9%) as shown in Figure 1. Among the respondents, 19.7% were not willing to donate any biological specimen whatsoever for biomedical research.
FIG. 1.
Biological samples respondents were willing to donate for research purposes.
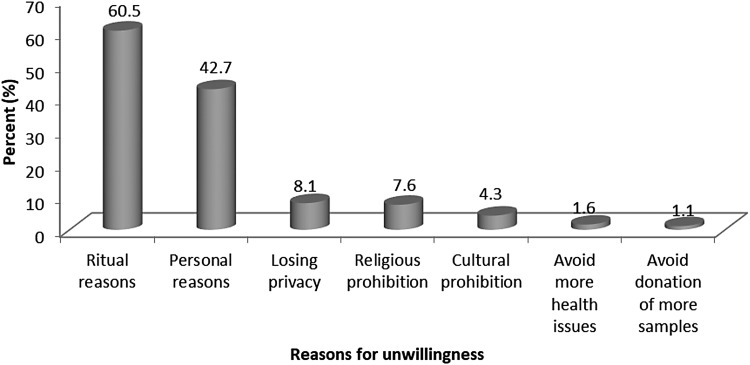
The most cited reasons by respondents for their unwillingness to donate hair for research purposes were the fear of their hair being used for ritual purposes (60.5%) and personal reasons (42.7%). Other reasons selected by respondents for not being willing to donate hair for research include losing privacy (8.1%), religious beliefs (7.6%), and cultural beliefs (4.3%), among others (Fig. 2).
FIG. 2.
Reasons for unwillingness to donate hair sample for research.
Discussion
In this study, we demonstrated moderate acceptability of hair collection for biomedical research among PLWH in Southwest Nigeria. To our knowledge, no previous study has assessed the acceptability of hair sampling for research in Nigeria. Most of the respondents in our sample were willing to donate blood with fewer reporting a willingness to donate other biospecimens (hair, urine, saliva, and stool). This may be because the use of blood for research is a common practice in this setting or because of other cultural beliefs associated with hair. The respondents (19.7%) not willing to donate any biospecimen whatsoever for research purpose additionally demonstrate a general unwillingness to provide specimens. The reason for the unwillingness to donate specimens for biomedical research, whether based on distrust of the medical system or a poor understanding of the importance of biomedical research, is a subject for further investigation and suggests the need for community education and sensitization within our setting.
There is need to adopt reliable means of monitoring ARV adherence in Nigeria as part of a strategy to improve treatment outcomes. The usefulness of hair ARV monitoring in modern HIV research, especially in resource-limited settings, considering the challenges associated with the storage of samples in these settings, has been demonstrated.3,20 Notwithstanding, disparities in belief systems and other cultural/traditional practices may influence people's beliefs and their acceptance of donating certain biospecimens for research considered “sensitive.” An example of such a biospecimen is hair.25 These “sensitive body parts” are believed to be metaphysically connected to each individual, thereby allowing for the possibility of manipulation to harm the person if not guarded. Certain tribes and cultures have different beliefs and perceptions about different parts of the body. In Tanzania, blood is believed to be sold for witchcraft purposes,29 while the Native American Diné perceive blood as a sacred fluid that moves the spirit of the Maker around a person's body30 and, as such, should be handled carefully. Similarly, several tribes, including some in Nigeria, believe that an individual's hair can be used for fetish or ritual purposes and consequently, cause harm to the individual whose hair has been collected.25,31 Further exploration of how such beliefs may have impacted patients in our study is indicated.
The 51.4% acceptability rate for hair sampling for research purposes in our study population of PLWH receiving treatment in a tertiary health facility in Ibadan, Southwest Nigeria, contrasts with acceptability rates in some Eastern African countries that were higher than 95%.3,32 In a study among HIV pregnant and breastfeeding women in Uganda,20 the acceptability rate was 84% and a randomized trial to assess adherence to pre-exposure prophylaxis involving Kenyan and Ugandan participants reported up to 96%–100% acceptability rates.32 Similarly, a study in non-HIV Asian populations to assess levels of organophosphates in hair reported a 96% acceptance rate despite their belief that hair may be used for sorcery.25 In contrast, in another study involving HIV-infected children in rural Uganda, there was a 61% acceptability rate. A study conducted among PLWH in South Africa33 reported a high level of unwillingness to donate repeated hair samples ranging from 57% to 97% across visits. “Volunteer effect” (a situation in which participants who have already volunteered to participate in a study before the request for hair sampling)3,20,31 may contribute to the high acceptability rate observed in the studies carried out in Eastern Africa. Patients already committed to a research study will likely have a more positive attitude toward hair sample donation compared to those who are not taking part in a predefined research study (as in our sample). Finally, another factor that may limit acceptability rates is the inability to get hair from some patients' heads. Some men and children in Africa shave their head as frequently as once or twice a month. Nevertheless, some patients in this category may volunteer to keep their hair uncut over a month, in which case, another visit can be scheduled for the hair sample collection.3 Some women may not be willing to provide hair after a weave. In general, variations in acceptance rates suggest that each setting in Africa or Asia may have unique issues, cultural beliefs, and superstitions, which are all important to address by participant and field staff education.
Sociodemographic factors associated with willingness to give hair for research
Bivariate and multivariate analyses showed that respondents with primary education or less were more willing to donate hair than those with secondary education or more. We speculate that this may be because some participants with lower education levels erroneously thought the donation of hair would personally benefit them compared to the more educated patients, who might have had a better understanding of the research concept. This possible gap in understanding can be avoided through comprehensive informed consent in studies that employ hair sampling. In one study involving Kenyan participants,3 the research procedure was framed to the volunteers as a “new hair test” that will enhance informed decision making in HIV treatment, a framing that may have led to a perception that the research would personally benefit them, unless detailed explanation was provided. Finally, in our study, Muslims were more willing to donate hair than Christians even when adjusting for other demographic covariates. The reason for this difference is not yet explained, although a moderating effect of religion on beliefs and behaviour may be postulated.
Reasons for unwillingness to donate hair for research
The most cited reason for not being willing to donate hair is the fear of hair being diverted for ritual purposes. In other words, the fear of being harmed. This is not surprising as this belief is common to many settings in Africa and Asia.25,31 In a qualitative assessment of people's concerns about donating hair for research among 21 Xhosa-speaking HIV-infected women in South Africa,31 different concerns were raised by participants, all centered on the possibility of being harmed if they donate hair. Participants in that study also mentioned the fact that hair can be used for witchcraft. One mentioned the concern that when their hair is blown away by the wind, animals may pick it up, build a nest with it, leading the patient to go mad. While belief systems are difficult to change, the research community could do more to help patients overcome the perception that samples donated for biomedical research may be used or diverted for other purposes. In our study, the second most cited reason for not being willing to donate hair was “personal.” This failure to comment suggests that further qualitative exploration on reasons for declining hair collection is indicated.
One of the main limitations of this study is that it was conducted at a single site and only on PLWH, which may limit the generalizability of our findings. However, the HIV clinic in the College of Medicine, UI, is one of the largest HIV clinics in Southwest Nigeria, drawing patients from several states. Hence, our sample serves as a good representation of the patients living with HIV in Southwestern Nigeria. In addition, the 51.4% willingness in this study may not translate to the actual level of willingness to donate hair in the context of a real-world study, since our study was not rooted in actual study procedures where hair sampling is involved, but asked as a theoretical concept.
Conclusion
In this single-site survey in Southwest Nigeria, there was a moderate level of willingness to donate hair for research among PLWH. This is in contrast to settings in Eastern Africa and Asia where acceptability rates of hair collection (in actual research studies collecting hair) were much higher. Divergent sociocultural factors may partially explain these disparate results. Further research is needed to unravel the reasons for this moderate willingness to donate hair in Nigeria and inform strategies to enhance its uptake given the benefits of hair concentrations of ARVs to assess adherence. Our results underscore the importance of cultural sensitivity and community education when introducing innovative HIV research techniques to new settings.
Acknowledgments
Research training for this publication was supported by the Fogarty International Center and National Institute of Mental Health (NIMH) of the National Institutes of Health (NIH) under award number D43TW009608. Support to M.G. was provided by the National Institute of Allergy and Infectious Diseases (NIAID)/NIH (2R01AI098472). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We acknowledge the HIV clinic, IDI, College of Medicine, UI, for permitting us to use the facility for this research. We also thank Centre for Drug Discovery Development and Production (CDDDP), Faculty of Pharmacy, UI, for their support.
Author Disclosure Statement
The authors declare no conflict of interests.
References
- 1. Liu AY, Yang Q, Huang Y, et al. : Strong relationship between oral dose and tenofovir hair levels in a randomized trial: Hair as a potential adherence measure for pre-exposure prophylaxis (PrEP). PLoS One 2014;9:e83736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Olds PK, Kiwanuka JP, Nansera D, et al. : Assessment of HIV antiretroviral therapy adherence by measuring drug concentrations in hair among children in rural Uganda. AIDS Care 2015;27:327–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hickey MD, Salmen CR, Tessler RA, et al. : Antiretroviral concentrations in small hair samples as a feasible marker of adherence in rural Kenya. J Acquir Immune Defic Syndr 2014;66:311–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gandhi M, Ameli N, Bacchetti P, et al. : Atazanavir concentration in hair is the strongest predictor of outcomes on antiretroviral therapy. Clin Infect Dis 2011;52:1267–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gandhi M, Greenblatt RM, Bacchetti P, et al. : A single-nucleotide polymorphism in CYP2B6 leads to >3-fold increases in efavirenz concentrations in plasma and hair among HIV-infected women. J Infect Dis 2012;206:1453–1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gandhi M, Mwesigwa J, Aweeka F, et al. : Hair and plasma data show that lopinavir, ritonavir, and efavirenz all transfer from mother to infant in utero, but only efavirenz transfers via breastfeeding. J Acquir Immune Defic Syndr 2013;63:578–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martin S, Elliott-DeSorbo DK, Calabrese S, et al. : A comparison of adherence assessment methods utilized in the United States: Perspectives of researchers, HIV-infected children, and their caregivers. AIDS Patient Care STDS 2009;23:593–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kagee A, Nel A: Assessing the association between self-report items for HIV pill adherence and biological measures. AIDS Care 2012;24:1448–1452 [DOI] [PubMed] [Google Scholar]
- 9. Gandhi M, Yang Q, Bacchetti P, Huang Y: Short communication: A low-cost method for analyzing nevirapine levels in hair as a marker of adherence in resource-limited settings. AIDS Res Hum Retroviruses 2014;30:25–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huang Y, Yang Q, Yoon K, et al. : Microanalysis of the antiretroviral nevirapine in human hair from HIV-infected patients by liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem 2011;401:1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wendel CS, Mohler MJ, Kroesen K, Ampel NM, Gifford AL, Coons SJ: Barriers to use of electronic adherence monitoring in an HIV clinic. Ann Pharmacother 2001;35:1010–1015 [DOI] [PubMed] [Google Scholar]
- 12. Podsadecki TJ, Vrijens BC, Tousset EP, Rode RA, Hanna GJ: “White coat compliance” limits the reliability of therapeutic drug monitoring in HIV-1-infected patients. HIV Clin Trials 2008;9:238–246 [DOI] [PubMed] [Google Scholar]
- 13. LeBeau MA, Montgomery MA, Brewer JD: The role of variations in growth rate and sample collection on interpreting results of segmental analyses of hair. Forensic Sci Int 2011;210:110–116 [DOI] [PubMed] [Google Scholar]
- 14. Thaden JT, Gandhi M, Okochi H, Hurt CB, McKellar MS: Seroconversion on preexposure prophylaxis: A case report with segmental hair analysis for timed adherence determination. AIDS 2018;32:F1–F4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beumer JH, Bosman IJ, Maes RA: Hair as a biological specimen for therapeutic drug monitoring. Int J Clin Pract 2001;55:353–357 [PubMed] [Google Scholar]
- 16. Cohen SE, Sachdev D, Lee SA, et al. : Acquisition of tenofovir-susceptible, emtricitabine-resistant HIV despite high adherence to daily pre-exposure prophylaxis: a case report. The Lancet HIV 2019;6:e43–e50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nettles RE, Kieffer TL, Parsons T, et al. : Marked intraindividual variability in antiretroviral concentrations may limit the utility of therapeutic drug monitoring. Clin Infect Dis 2006;42:1189–1196 [DOI] [PubMed] [Google Scholar]
- 18. Saberi P, Neilands TB, Ming K, et al. : Strong correlation between concentrations of antiretrovirals in home-collected and study-collected hair samples: Implications for adherence monitoring. J Acquir Immune Defic Syndr 2017;76:e101–e103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tabb ZJ, Mmbaga BT, Gandhi M, et al. : Antiretroviral drug concentrations in hair are associated with virologic outcomes among young people living with HIV in Tanzania. AIDS 2018;32.9:1115–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koss CA, Natureeba P, Mwesigwa J, et al. : Hair concentrations of antiretrovirals predict viral suppression in HIV-infected pregnant and breastfeeding Ugandan women. AIDS 2015;29:825–830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Prasitsuebsai W, Kerr SJ, Truong KH, et al. : Using lopinavir concentrations in hair samples to assess treatment outcomes on second-line regimens among Asian children. AIDS Res Hum Retroviruses 2015;31:1009–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baxi SM, Greenblatt RM, Bacchetti P, et al. : Nevirapine concentration in hair samples is a strong predictor of virologic suppression in a prospective cohort of HIV-infected patients. PLoS One 2015;10:e0129100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gandhi M, Glidden DV, Mayer K, et al. : Association of age, baseline kidney function, and medication exposure with declines in creatinine clearance on pre-exposure prophylaxis: An observational cohort study. Lancet HIV 2016;3:e521–e528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gandhi M, Murnane PM, Bacchetti P, et al. : Hair levels of preexposure prophylaxis drugs measure adherence and are associated with renal decline among men/transwomen. AIDS 2017;31:2245–2251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Knipe DW, Jayasumana C, Siribaddana S, et al. : Feasibility of hair sampling to assess levels of organophosphate metabolites in rural areas of Sri Lanka. Environ Res 2016;147:207–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Awofala AA, Ogundele OE: HIV epidemiology in Nigeria. Saudi J Biol Sci 2018;25:697–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. UNAIDS: UNAIDS/Nigeria. Available at www.unaids.org/en/regionscountries/countries/nigeria, accessed July14, 2018
- 28. Babatunde OA, Elegbede OE, Ayodele LM, et al. : Workers willingness to donate human biological sample for future research in a South Western Nigerian Tertiary Health Center. J Asian Sci Res 2013;3:57 [Google Scholar]
- 29. Vallely A, Shagi C, Kasindi S, et al. : The benefits of participatory methodologies to develop effective community dialogue in the context of a microbicide trial feasibility study in Mwanza, Tanzania. BMC Public Health 2007;7:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Davis SM, Reid R: Practicing participatory research in American Indian communities. Am J Clin Nutr 1999;69:755s–759s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coetzee B, Kagee A, Tomlinson M, Warnich L, Ikediobi O: Reactions, beliefs and concerns associated with providing hair specimens for medical research among a South African sample: A qualitative approach. Future Virol 2012;7:1135–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Baxi SM, Liu A, Bacchetti P, et al. : Comparing the novel method of assessing PrEP adherence/exposure using hair samples to other pharmacologic and traditional measures. J Acquir Immune Defic Syndr 2015;68:13–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Robbins R, Gouse H, Warne P, Mtingeni Y, Henry M, Lopez-Rios J: Feasibility and acceptability of hair-and dried blood spot-derived ARV biomarkers as objective measures of treatment adherence in South Africa. Paper presented at: IAPAC 10th International Conference on HIV Treatment and Prevention Adherence, Miami, Florida, June, 2015 [Google Scholar]