Abstract
Background
Driving a motor vehicle is an important aspect of mobility for older adults. Limited lower extremity functioning performance, as measured by the Short Physical Performance Battery (SPPB), has been associated with various negative health outcomes, but little is known about the association of SPPB scores with driving status.
Objective
The purpose of this study was to evaluate whether lower (poorer) SPPB scores are associated with an increased rate for being a current nondriver among a nationally representative sample of community-dwelling older adults.
Design
The National Health and Aging Trends Study is a longitudinal cohort study.
Methods
A population of 5935 participants, surveyed annually from 2011 to 2014 for the National Health and Aging Trends Study, was used to examine the relationship between SPPB and driving status. Using weighted data, multivariable Poisson regression with generalized estimating equations was used to calculate the rate ratios, adjusting for covariates and clustering due to the complex survey design.
Results
Participants with a low (poor) SPPB score (0–5) had a rate for being a current nondriver 2.01 times the rate (or 101% increase) of those with a high (good) SPPB score (10–12) (adjusted 95% confidence interval = 1.78–2.26).
Limitations
Current nondrivers were not asked whether they planned to resume driving if they had not driven in the previous year.
Conclusions
Unlike other factors, such as cognitive decline, lower SPPB scores (poorer lower extremity functioning) are significantly associated with an increased rate of being a current nondriver and are a modifiable risk factor. Further research is needed to examine whether optimum exercises and other physical therapist interventions focused on improving lower extremity strength and balance ultimately improve driving outcomes.
In the United States and other industrialized countries, driving is an important component of independent mobility for adults.1 Driving connects adults with many fundamental aspects of daily life such as employment, social engagements, and personal care.2 As the number of older adult drivers increases, health professionals play an important role in keeping older drivers safely on the road, for example, by providing rehabilitative and prevention services for correctable problems such as musculoskeletal strength.3 If the physical therapy profession is going to “transform society by optimizing movement to improve the human experience,”4,5 it is arguable that maintaining independent and safe driving mobility is a goal for physical therapy.
Although it is commonly known that the frequency of driving declines as people get older, there is a growing amount of literature that focuses on other risk factors for driving cessation in older adults besides aging.6–9 Driving cessation is associated with various negative consequences for older adults, including an increase in depressive symptoms, and is independently associated with entering long-term care facilities.10,11 Previous research supports the association between health-related factors and driving cessation among older adults. The most notable ones include: cognitive factors, such as memory, processing speed, and verbal reasoning; poorer self-rated health; and visual impairment.12,13 Research has shown a modest association between physical functioning measures (ie, grip strength, the Turn 360 test) and driving cessation.12,14
Physical functioning is an important factor to consider for understanding driving behavior because it is modifiable. In their comprehensive review, Anstey and colleagues proposed a conceptual framework of factors enabling safe driving behavior, with cognition, vision, and physical function determining an individual's capacity to drive safely.15 Individuals use knowledge of their own physical and cognitive capabilities and deficits to form beliefs about their driving abilities; as a result, physical functioning directly affects both driving capacity and beliefs about driving capacity.15 Driving capacity, in combination with individuals’ self-monitoring and beliefs about their own driving capacity, is what ultimately determines individuals’ driving behavior.15
Since 1994, when the Short Physical Performance Battery (SPPB) was developed by Guralnik and colleagues as a measure of lower extremity functioning, the SPPB has been associated with a variety of health outcomes such as disability, hospitalization and length of hospital stay, poorer health outcomes after discharge, health and function declines, and mortality.16–22 The SPPB is frequently used in studies of older adults and has shown good reliability and validity in this population.16,18,21,23,24
The SPPB has been assessed previously in studies of driving in older adults, including those that have focused on driving exposure and driving cessation, but not in any large, nationally representative samples.25–28 We recently published a systematic review on this topic.28 In brief, Davis and colleagues found in their cross-sectional study that the amount of car trips made per week declined with declining SPPB scores, indicating that lower SPPB scores are associated with limited driving exposure.25 Further, 2 prospective cohort studies found that lower SPPB scores were significantly associated with decreased driving.26,27 One of those studies focused on individuals who reported at 18-month follow-ups across a 12-year span that they had not driven over a 6-month period (“long-term disability in driving a car”).27 The other specified driving cessation as the outcome of interest, which was determined by a prior driver reporting no longer driving 2 years after baseline.27 Notably, the SPPB was modified in 1 of these driving cessation studies on 2 of the 3 physical performance measures included in the battery.26
The present study uses measures collected annually by the National Health and Aging Trends Study (NHATS), a large and nationally representative cohort, to evaluate the hypothesis that poorer lower extremity physical functioning levels (lower scores on the standard SPPB) will be associated with an increased rate for being a current nondriver among a sample of community-dwelling older adults.
Methods
This article adheres to the reporting standards laid out in the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement.29
Data Source and Study Sample
NHATS is a nationally representative, age-stratified longitudinal study of US Medicare beneficiaries aged 65 years and older who reside in the community in their own or another's home or in a residential care setting.30 Data have been collected from 2011 (T1 or baseline) to 2014 (T4) on the same participants. The study oversampled individuals from older age groups and black individuals. NHATS aims to understand trends and trajectories in functioning and disability as older individuals age by conducting 90-minute in-person interviews every year in participants’ homes. Physical and performance-based assessments, including chair and balance stands and a walking speed test, were collected along with self-reported data.31 If a participant was unable to respond to the interview questions, a proxy respondent could provide the necessary information. For proxy interviews, participants eligible for performance-based assessments were given the opportunity to participate.
At baseline, 8245 persons participated in NHATS and the response rate was 71%.31 Our study sample consisted of 5935 persons who were in community or nonnursing home residential care settings, had an SPPB score for at least 1 wave of the study (T1–T4), and were current or previous drivers at baseline (Figure). Participants reporting that they had never driven in their lifetime were excluded from the study.
Figure.
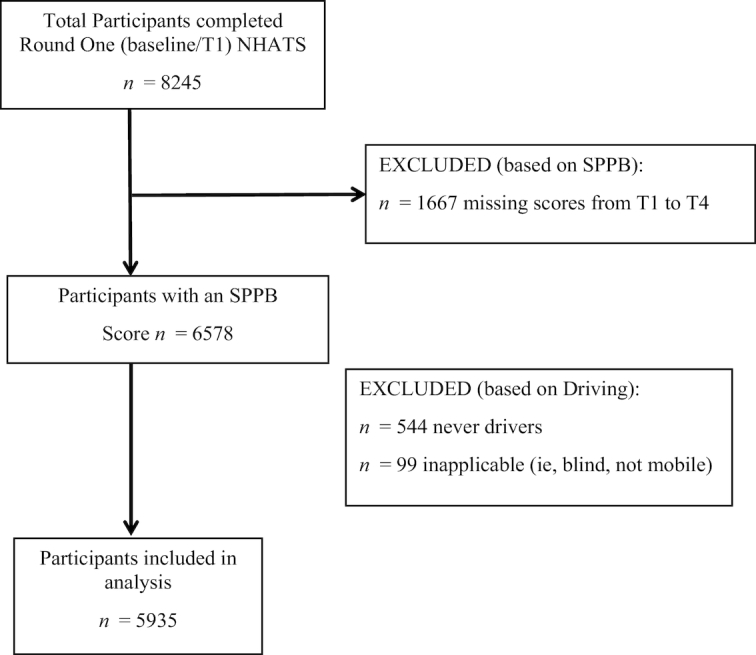
Flow diagram of study participant inclusion. NHATS = National Health and Aging Trends Study; SPPB = Short Physical Performance Battery.
Measures
Physical functioning
Physical functioning data were collected at each wave (T1–T4) using SPPB. The SPPB measures lower extremity physical function and has 3 components: standing balance, gait speed, and repeated chair stands. Standing balance evaluates an individual's ability to stand with feet together in the side-by-side, semitandem, and tandem positions for up to 10 seconds. Usual gait speed is timed and measured from a standing start over a 3-m course. Repeated chair stands reflect time to rise from a chair and return to a seated position 5 times as quickly as possible with the arms folded across the chest. Each measurement (balance, gait speed, and repeated chair stands) is scored from 0 (inability to carry out task) to 4 (best score), and each score is then summed to determine the total SPPB score (0 to 12).18
Scoring for the balance stands test was defined as: 0 (unable to attempt or complete the side-by-side stand); 1 (participant completed the side-by-side stand and did not complete or did not attempt the semitandem stand for safety reasons); 2 (participant completed the semitandem stand and held the full tandem stand for 0 to 2.99 seconds or did not attempt the full tandem stand for safety reasons); 3 (participant completed the semitandem stand and held the full tandem stand for 3 to 9.99 seconds); and 4 (participant completed the semitandem stand and held the full tandem stand for 10 seconds). Scoring for the walking speed test was as follows: 0 (not attempted for safety reasons, or attempted but not completed); 1 (≤ 0.441 m/s); 2 (0.442–0.624 m/s); 3 (0.625–0.798 m/s); and 4 (≥ 0.799 m/s). Finally, the scoring for the repeated chair stands was defined as: 0 (not attempted for safety reasons, or attempted but not completed); 1 (≥ 16.70 seconds); 2 (13.70–16.69 seconds); 3 (11.20–13.69 seconds); and 4 (≤ 11.19 seconds).32
The cut-points used in this study for each test are from the “original SPPB.”18 Details on the scoring are available elsewhere.32 Individuals with missing or inapplicable SPPB total scores for all 4 waves (T1–T4) of data collection were excluded from this study (n = 1667). Total scores on the SPPB were categorized as poor (0–5), fair (6–9), and good (10–12).33,34
Driving status
Baseline (T1) driving status was derived by using participant responses to a question regarding the last time the participant had driven. Driving status at follow-up visits (T2–T4) was derived based on the participants’ responses to how often they had driven in the past year (every day, most days, some days, rarely, or never). Those who had reported driving in the past year were considered current drivers. Current nondrivers were defined as individuals who reported never driving in the last year. Participants who reported that they had never driven in their lifetime (n = 544) or those who reported being blind or never leaving their residence (n = 99) were not included in the analysis.35 Although rare, it was possible for nondrivers at 1 time point to resume driving at the next follow-up point (eg, after recovery from an injury). Of the included sample, 1.8% were resumed drivers from T1 at T2; 0.8% were resumed drivers from T2 at T3; and 0.9% were resumed drivers from T3 at T4.
Covariates
Demographic characteristics previously associated with driving cessation among older adults were included as covariates in our analyses.6,12,33,36,37 These covariates include age, sex, race/ethnicity, living arrangement, a comorbidity scale, and dementia. Age was categorized as 65 to 69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, and 90 years or older. Sex was defined as female or male. Race/ethnicity was defined as white non-Hispanic, black non-Hispanic, Hispanic, and other non-Hispanic. Living arrangement was defined as either living alone in a household or not living alone in a household. Participants with an unreported race/ethnicity or living arrangement were added to the majority response group for that covariate. The comorbidity scale includes the following chronic conditions that have been used in previous physical functioning and driving cessation research: diabetes mellitus, lung disease, heart disease, osteoporosis, non–skin cancer, stroke, and arthritis.38,39 Values reported in the comorbidity scale were a sum of all the diagnoses reported by the participant that were categorized as 0, 1, 2, 3, or 4 or more. Dementia was categorized into probable dementia and possible or no dementia; a description of this classification is described elsewhere.40
Statistical Analysis
Descriptive analyses of baseline demographic characteristics and driving status by baseline SPPB total score were examined with χ2 tests. To investigate the association of time-varying SPPB total score on a categorical scale (0–5, 6–9, 10–12) and the rate of being a current nondriver, a generalized estimating equation analysis was employed, specifying the log link function with a Poisson distribution.41,42
A generalized estimating equation was chosen to account for the correlated data resulting from the within-subjects repeated measures from T1 to T4.41 A generalized estimating equation further allowed the analyses to account for participants that were missing 1 or more of the follow-up time points, at which driving status was assessed (T2, T3, and T4), and to account for a small proportion of participants who were resumed drivers, meaning that they had once been nondrivers and had resumed driving in a follow-up round.41
The adjusted model included a priori participant- and time-dependent covariates (age, living arrangement, and comorbidity scale).43 Age categories and the comorbidity scale were assessed for linearity with driving status. Both age and comorbidity were included in the models as ordinal variables. Living arrangement, age, and the comorbidity scale were modeled as time-variant covariates, whereas all other variables were modeled as time-invariant. Clustering was accounted for in unadjusted and adjusted models. To estimate the rate ratios and confidence intervals (CIs), a log link and exchangeable working correlation matrix were specified in the models because using an exchangeable structure with our data provided us with a more efficient inference.44 Robust SEs for the parameter estimates were used to control for mild violation of the distribution assumption.42 All statistical analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC, USA), and the final models were run in STATA Version 14.0 (STATA Corp, College Station, TX, USA).
NHATS collected data from participants using a complex sampling design. We used the T4 (or 2014) replicate weights developed by NHATS to produce nationally representative estimates of the older Medicare population.31 These weights used the modified balance repeated replication method to adjust for variance estimates. All means, proportions, and measures of association are based on the weighted data, and sample sizes are unweighted.
Results
Our analyses were performed on a study cohort of 5935 NHATS participants with an SPPB total score for at least 1 wave of the study (T1–T4) who were former or current drivers at baseline. Individuals who reported never having driven in their lifetime were excluded. At baseline, 18.9% of older Medicare beneficiaries had a poor SPPB total score, 28.5% had a fair SPPB total score, and 52.6% had a good SPPB total score, after adjustment using NHATS-provided study weights (Tab. 1). When independently tested, all covariates were significantly associated with SPPB total score. Approximately 17% of the participants were nondrivers at baseline.
Table 1.
Characteristics of Medicare Beneficiaries by SPPB Total Score at Baseline, NHATS, 2011a
| Variables, % (n) | Total | Total SPPB Score: Poor (0–5) | Total SPPB Score: Fair (6–9) | Total SPPB Score: Good (10–12) | P |
|---|---|---|---|---|---|
| Total | (5935) | 24.7 (1465) | 31.3 (1856) | 44.0 (2614) | |
| Driving status | <.0001 | ||||
| Current driver | 83.2 | 46.2 | 84.0 | 96.1 | |
| Nondriver | 16.8 | 53.8 | 16.0 | 3.9 | |
| Age group, y | <.0001 | ||||
| 65–69 | 29.5 | 12.7 | 20.9 | 40.3 | |
| 70–74 | 25.7 | 16.5 | 25.0 | 29.3 | |
| 75–79 | 19.2 | 17.9 | 22.5 | 17.8 | |
| 80–84 | 14.0 | 20.5 | 18.7 | 9.2 | |
| 85–89 | 8.0 | 19.8 | 9.8 | 2.8 | |
| 90+ | 3.6 | 12.6 | 3.1 | 0.6 | |
| Sex | <.0001 | ||||
| Female | 54.5 | 63.4 | 59.6 | 48.6 | |
| Male | 45.5 | 36.6 | 40.4 | 51.4 | |
| Race/ethnicity | <.0001 | ||||
| White, NH | 84.4 | 80.5 | 81.0 | 87.7 | |
| Black, NH | 7.1 | 10.6 | 9.1 | 4.7 | |
| Hispanic | 5.7 | 7.1 | 7.1 | 4.5 | |
| Other | 2.8 | 1.9 | 2.8 | 3.1 | |
| Living arrangement | <.0001 | ||||
| Alone | 28.1 | 38.9 | 33.1 | 21.5 | |
| Not alone | 71.9 | 61.1 | 66.9 | 78.5 | |
| Dementia | <.0001 | ||||
| Possible or no | 92.7 | 73.9 | 94.5 | 98.4 | |
| Probable | 7.3 | 26.1 | 5.5 | 1.6 | |
| Comorbidity scale | <.0001 | ||||
| 0 | 19.6 | 9.4 | 14.9 | 25.9 | |
| 1 | 31.5 | 23.3 | 28.2 | 36.2 | |
| 2 | 26.6 | 29.0 | 30.2 | 23.8 | |
| 3 | 14.3 | 22.1 | 16.0 | 10.5 | |
| 4 or more | 8.0 | 16.2 | 10.7 | 3.7 |
Analyses of weighted data from the National Health and Aging Trends Study (NHATS). Sample totals provided along with weighted percentages. NH = non-Hispanic; SPPB = Short Physical Performance Battery.
Participants with a poor SPPB total score (0–5) (poor physical functioning performance) had a 133% increase in rate (unadjusted rate ratio = 2.33) for being a current nondriver when compared with participants with a good SPPB total score (10–12) (unadjusted 95% CI = 2.11–2.58). Additionally, participants with a fair SPPB total score (6–9) had a rate for being a current nondriver 1.34 times the rate (a 34% increase) of those with a good SPPB total score (10–12) (unadjusted 95% CI = 1.25–1.44). This association remained after adjusting for sex, age, living arrangement, dementia, comorbidities, and clustering (P < .001). After adjusting for covariates, participants with a poor SPPB total score (0–5) (poor physical functioning performance) had a rate for being a nondriver 2.01 times the rate (a 101% increase) of those with a good SPPB total score (10–12) (adjusted 95% CI = 1.78–2.26). Additionally, participants with a fair SPPB total score (6–9) had a rate for being a nondriver 1.31 times the rate (a 31% increase) of those with a good SPPB total score (10–12), when adjusting for the same covariates (adjusted 95% CI = 1.19–1.45) (Tab. 2).
Table 2.
Total SPPB Score and Rate of Being a Current Nondriver, NHATS, 2011–2014a
| Variables | Unadjusted Rate Ratio (95% CI) | Adjusted Rate Ratiob (95% CI) |
|---|---|---|
| Total SPPB score (0–5) | 2.33 (2.11–2.58)c | 2.01 (1.78–2.26)c |
| Total SPPB score (6–9) | 1.34 (1.25–1.44)c | 1.31 (1.19–1.45)c |
| Total SPPB score (10–12) | Reference | Reference |
Analyses of weighted data from the National Health and Aging Trends Study (NHATS). CI = confidence interval; SPPB = Short Physical Performance Battery.
Multivariable Poisson regression generalized estimating equation model adjusted for age, sex, race, living arrangement, dementia, and comorbidity accounting for clustering.
P < .001.
Discussion
Driving cessation can have significant implications for mobility, safety, and health among older adults. Identification of the modifiable risk factors, such as physical functioning, associated with driving cessation is important to target individuals who might benefit from physical therapist interventions to continue driving as they age. Physical therapists can provide rehabilitation and/or prevention services that can target muscle strength of the lower extremities.
The SPPB is a lower extremity physical functioning measurement that has been used extensively in aging research.18 Our study examined whether SPPB score, treated as a time-dependent variable, is associated with driving status (ie, is the participant currently a driver or a nondriver?) in a nationally representative, older adult population that was followed for 4 years. Our findings indicate that there is a significant relationship between SPPB total score and driving status in older adults. We found that participants with poor and fair SPPB total scores had an increased rate for being nondrivers when compared with participants with a good SPPB total score, both before and after adjustment for covariates.
These results are consistent with previous smaller, non–nationally representative cohort studies that found poorer SPPB scores to be associated with decreased driving.26,27 Gill and colleagues followed a cohort of 507 individuals in Connecticut for 12 years to determine if a poor SPPB score was a significant risk factor of driving cessation or “long-term disability in driving a car.”26 Further, Sims and colleagues found that every 1-point decline in SPPB scores was associated with a 16% increase in odds of driving cessation in their cohort of 646 participants followed for 2 years in Alabama.27 However, these studies were limited by size, generalizability of the study population, and, in the case of Gill et al, a modified version of the SPPB.26,28
Our study is strengthened by using 4 years of data from the nationally representative NHATS longitudinal cohort. The SPPB was administered in the NHATS cohort by a strict protocol, thus maintaining the fidelity of the battery. Administration of an unmodified SPPB is important for comparability between studies in order to maintain standardization across the field, and yet some studies use their own modified version of the SPPB, making results more difficult to generalize.26 Further, the use of total SPPB score as a time-dependent variable over 4 years emphasizes the dynamic nature of lower extremity mobility.
This study has some limitations. Due to the nature of the survey, the exact date when individuals stopped driving was not provided except for the first round. It is possible that some individuals who were no longer driving at the time of the annual survey were misclassified as current drivers, when in fact they could have driven at some point in the past year but were no longer driving at the time of the interview. Participants were also not asked whether they ever planned on resuming driving if they had not driven in the past year.
Although every effort was made to include relevant covariates in the analyses that were available in the NHATS dataset, we do recognize that the models could have been strengthened with the availability of additional variables that could have impacted driving status. For example, there is a trend toward greater involvement with driving among more affluent socioeconomic groups, and low income has been associated with older adults limiting or avoiding driving.38 Beyond medical and cognitive reasons for changing driving status, older adults who limit their driving also report driving-related fears, such as concerns about being in an accident or about crime.38 We posit that “fear of driving” could be a variable worth investigating in the future in relation to driving status; it is a fear that physical therapists are well positioned to address.
The present study found a significant association between time-dependent SPPB total score and driving status over 4 years of follow-up. Our results can be generalized to an older adult population who reside in the community in their own or another's home or a residential care setting in the United States. If the SPPB were more routinely administered as part of physical examinations in health care settings, physical performance scores could be a useful modifiable determinant for identifying older adults who are at risk for being a nondriver. Finding this association is the first step; future studies need to examine this association on the individual level. Previous research has found that exercise training in older adults can improve physical functioning, including balance and strength.45,46 Research indicates that a structured physical therapist intervention can improve SPPB scores for older adults, suggesting that an intervention that improves SPPB performance could offer benefits for more distal health outcomes, including driving outcomes or performance.47 More specifically, a systematic review concluded that there is moderate evidence—1 high-quality and 1 fair-quality randomized controlled trial—that physical therapist–guided exercises improve driving outcomes.48 A recent study from Antin and colleagues confirmed the low mileage bias hypothesis, namely, that older adults driving fewer miles per year have an increased crash rate; this suggests that overall fitness could be a mediating factor underlying this phenomenon (ie, older adult drivers with poor fitness drive less but have a higher risk per mile).49,50 This is further evidence that warrants more studies with rigorous designs, physical therapist–designed interventions, and measurement of direct driving outcomes. Perhaps physical therapists have more of a role to play in keeping older adults safely on the road and mobile than previously thought.
Author Contributions
Concept/idea/research design: J.A. Cisewski, L.L. Durbin, J.M. Guralnik, J. Kasper, T.J. Mielenz
Writing: J.A. Cisewski, L.L. Durbin, E.G. Bond, J.M. Guralnik, J. Kasper, T.J. Mielenz
Data collection: L.L. Durbin, J.M. Guralnik, J. Kasper
Data analysis: J.A. Cisewski, L.L. Durbin, T.J. Mielenz
Project management: T.J. Mielenz
Fund procurement: T.J. Mielenz
Providing facilities/equipment: T.J. Mielenz
Providing institutional liaisons: T.J. Mielenz
Clerical/secretarial support: T.J. Mielenz
Consultation (including review of manuscript before submitting): J.A. Cisewski, L.L. Durbin, E.G. Bond, J.M. Guralnik, J. Kasper, T.J. Mielenz, M. Qian
Ethics Approval
The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging and conducted by Johns Hopkins University. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved this study. Written informed consent was obtained from all participants or their proxy respondents. The results reported here are from secondary analysis of downloadable, deidentified, and publicly available NHATS data. The authors did not collect data and/or obtain consent from participants. This project was reviewed by and found exempt under 45 CFR 46 (not human participants research) by the Institutional Review Board of Columbia University Medical Center.
Funding
This work was supported by the AAA Foundation for Traffic Safety's Longitudinal Research on Aging Drivers (LongROAD) Project. It was supported in part by a grant from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, to the Center for Injury Epidemiology and Prevention at Columbia University (Grant No. R49 CE002096-01). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention. NHATS is sponsored by the US Department of Health and Human Services, National Institutes of Health, National Institute on Aging (Grant No. NIA U01AG032947) through an agreement with the Johns Hopkins Bloomberg School of Public Health.
Disclosures and Presentations
This project was funded by the AAA Foundation for Traffic Safety's (AAAFTS) Longitudinal Research on Aging Drivers (LongROAD) Project. A brief report including this topic and the frailty phenotype were published on the AAAFTS website: Durbin LL, Bond EG, Cisewski, JA, Qian M, Guralnik JM, Kasper JD, Mielenz TJ. Frailty phenotype, physical function, and driving status in older adults: LongROAD analysis of the National Health and Aging Trends Study. Washington, DC: AAA Foundation for Traffic Safety; 2017. Research Brief.
J.A. Cisewski presented the first draft of the manuscript as her Master's student thesis for Columbia University's Mailman School of Public Health. T.J. Mielenz was her first reader at the Mailman School of Public Health.
References
- 1. Choi NG, DiNitto DM. Depressive symptoms among older adults who do not drive: association with mobility resources and perceived transportation barriers. Gerontologist. 2016;56:432–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barr RA. More road to travel by: implications for mobility and safety in late life. Gerontechnology. 2002;2:50–54. [Google Scholar]
- 3. Underwood M. The older driver clinical assessment and injury prevention. Arch Intern Med. 1992;152:735–740. [DOI] [PubMed] [Google Scholar]
- 4. Jette AM. A bold vision for physical therapy. Phys Ther. 2017;97:946–947. [DOI] [PubMed] [Google Scholar]
- 5. American Physical Therapy Association; Vision statement for the physical therapy profession and guiding principles to achieve the vision. http://www.apta.org/Vision/ 2013. Accessed April 2, 2018. [Google Scholar]
- 6. Campbell MK, Bush TL, Hale WE. Medical conditions associated with driving cessation in community-dwelling, ambulatory elders. J Gerontol. 1993;48:S230–S234. [DOI] [PubMed] [Google Scholar]
- 7. Chihuri S, Mielenz TJ, DiMaggio CJ et al.. Driving cessation and health outcomes in older adults. J Am Geriatr Soc. 2016;64:332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dellinger AM, Sehgal M, Sleet DA, Barrett-Connor E. Driving cessation: what older former drivers tell us. J Am Geriatr Soc. 2001;49:431–435. [DOI] [PubMed] [Google Scholar]
- 9. Marottoli RA, Ostfeld AM, Merrill SS et al.. Driving cessation and changes in mileage driven among elderly individuals. J Gerontol. 1993;48:S255–S260. [DOI] [PubMed] [Google Scholar]
- 10. Windsor TD, Anstey KJ, Butterworth P, Luszcz MA, Andrews GR. The role of perceived control in explaining depressive symptoms associated with driving cessation in a longitudinal study. Gerontologist. 2007;47:215–223. [DOI] [PubMed] [Google Scholar]
- 11. Freeman EE, Gange SJ, Munoz B, West SK. Driving status and risk of entry into long-term care in older adults. Am J Public Health. 2006;96:1254–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Anstey KJ, Windsor TD, Luszcz MA, Andrews GR. Predicting driving cessation over 5 years in older adults: psychological well-being and cognitive competence are stronger predictors than physical health. J Am Geriatr Soc. 2006;54:121–126. [DOI] [PubMed] [Google Scholar]
- 13. Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and time to driving cessation in older adults. Optom Vis Sci. 2005;82:765–773. [DOI] [PubMed] [Google Scholar]
- 14. Edwards JD, Ross LA, Ackerman ML et al.. Longitudinal predictors of driving cessation among older adults from the ACTIVE clinical trial. J Gerontol B Psychol Sci Soc Sci. 2008;63:P6–P12. [DOI] [PubMed] [Google Scholar]
- 15. Anstey KJ, Wood J, Lord S, Walker JG. Cognitive, sensory and physical factors enabling driving safety in older adults. Clin Psychol Rev. 2005;25:45–65. [DOI] [PubMed] [Google Scholar]
- 16. Cesari M, Onder G, Zamboni V et al.. Physical function and self-rated health status as predictors of mortality: results from longitudinal analysis in the ilSIRENTE study. BMC Geriatr. 2008;8:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guralnik JM, Simonsick EM, Ferrucci L et al.. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- 19. Rolland Y, Lauwers-Cances V, Cesari M, Vellas B, Pahor M, Grandjean H. Physical performance measures as predictors of mortality in a cohort of community-dwelling older French women. Eur J Epidemiol. 2006;21:113–122. [DOI] [PubMed] [Google Scholar]
- 20. Studenski S, Perera S, Wallace D et al.. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. [DOI] [PubMed] [Google Scholar]
- 21. Volpato S, Cavalieri M, Guerra G et al.. Performance-based functional assessment in older hospitalized patients: feasibility and clinical correlates. J Gerontol A Biol Sci Med Sci. 2008;63:1393–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Volpato S, Cavalieri M, Sioulis F et al.. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kwon S, Perera S, Pahor M et al.. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging. 2009;13:538–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ostir GV, Volpato S, Fried LP, Chaves P, Guralnik JM. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the Women's Health and Aging Study. J Clin Epidemiol. 2002;55:916–921. [DOI] [PubMed] [Google Scholar]
- 25. Davis MG, Fox KR, Hillsdon M et al.. Getting out and about in older adults: the nature of daily trips and their association with objectively assessed physical activity. Int J Behav Nutr Phys Act. 2011;8:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012;156:131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sims RV, Ahmed A, Sawyer P, Allman RM. Self-reported health and driving cessation in community-dwelling older drivers. J Gerontol A Biol Sci Med Sci. 2007;62:789–793. [DOI] [PubMed] [Google Scholar]
- 28. Mielenz TJ, Durbin L, Cisewski JA, Guralnik JM, Li G. Select physical performance measures and driving outcomes in older adults. Inj Epidemiol. 2017;4:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. von Elm E, Altman DG, Egger M et al.. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. [DOI] [PubMed] [Google Scholar]
- 30. Montaquila J, Freedman VA, Edwards B, Kasper JD. National Health and Aging Trends Study: Round 1 Sample Design and Selection. Baltimore, MD: Johns Hopkins School of Public Health; 2012. [Google Scholar]
- 31. Kasper JD, Freedman VA. National Health and Aging Trends Study User Guide: Rounds 1-6 Final Release. Baltimore, MD: Johns Hopkins School of Public Health; 2017. [Google Scholar]
- 32. Kasper JD, Freedman VA, Niefeld MR. Construction of Performance-Based Summary Measures of Physical Capacity in the National Health and Aging Trends Study. Baltimore, MD: Johns Hopkins School of Public Health; 2012. [Google Scholar]
- 33. Chen CM, Chang WC, Lan TY. Identifying factors associated with changes in physical functioning in an older population. Geriatr Gerontol Int. 2015;15:156–164. [DOI] [PubMed] [Google Scholar]
- 34. Guralnik JM, Ferrucci L, Pieper CF et al.. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Skehan ME, Kasper JD, Freedman VA. Driving and Transportation Measures in the National Health and Aging Trends Study. Baltimore, MD: Johns Hopkins School of Public Health; 2014. [Google Scholar]
- 36. Ackerman ML, Edwards JD, Ross LA, Ball KK, Lunsman M. Examination of cognitive and instrumental functional performance as indicators for driving cessation risk across 3 years. Gerontologist. 2008;48:802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Herrmann N, Rapoport MJ, Sambrook R, Hebert R, McCracken P, Robillard A. Predictors of driving cessation in mild-to-moderate dementia. CMAJ. 2006;175:591–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ragland DR, Satariano WA, MacLeod KE. Reasons given by older people for limitation or avoidance of driving. Gerontologist. 2004;44:237–244. [DOI] [PubMed] [Google Scholar]
- 39. Samuel LJ, Glass TA, Thorpe RJ Jr, Szanton SL, Roth DL. Household and neighborhood conditions partially account for associations between education and physical capacity in the National Health and Aging Trends Study. Soc Sci Med. 2015;128:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kasper JD, Freedman VA, Spillman B. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Baltimore, MD: Johns Hopkins School of Public Health; 2013. [Google Scholar]
- 41. Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. [DOI] [PubMed] [Google Scholar]
- 42. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 43. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 44. Wacholder S. Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol. 1986;123:174–184. [DOI] [PubMed] [Google Scholar]
- 45. Fiatarone MA, O'Neill EF, Ryan ND et al.. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330:1769–1775. [DOI] [PubMed] [Google Scholar]
- 46. Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures: a randomized controlled trial. JAMA. 1994;272:1909–1914. [DOI] [PubMed] [Google Scholar]
- 47. Pahor M, Blair SN, Espeland M et al.. Effects of a physical activity intervention on measures of physical performance. Results of the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. [DOI] [PubMed] [Google Scholar]
- 48. Korner-Bitensky N, Kua A, von Zweck C, Van Benthem K. Older driver retraining: an updated systematic review of evidence of effectiveness. J Safety Res. 2009;40:105–111. [DOI] [PubMed] [Google Scholar]
- 49. Antin JF, Guo F, Fang Y, Dingus TA, Perez MA, Hankey JM. A validation of the low mileage bias using naturalistic driving study data. J Safety Res. 2017;63:115–120. [DOI] [PubMed] [Google Scholar]
- 50. Hakamies-Blomqvist L, Raitanen T, O'Neill D. Driver ageing does not cause higher accident rates per km. Trans p Res Part F. Traffic Psychol Behav. 2002;5:271–274. [Google Scholar]


