Abstract
Ankle sprains are common injuries involving the lateral ankle ligaments and affect athletes of all levels. Most patients heal uneventfully, but those with symptoms persisting past 3 months should be evaluated for chronic ankle instability and its associated conditions as well as for the presence of varus malalignment. Chronic ankle instability is initially treated nonoperatively, with surgical management reserved for those who have failed to improve after 3 to 6 months of bracing and functional rehabilitation. Anatomic repair using a modification of the Broström procedure is the preferred technique for initial surgery. Anatomic reconstruction with tendon graft should be considered when repair is not possible, as it maintains physiological joint kinematics. Nonanatomic reconstructions are seldom indicated. Arthroscopic repair or reconstruction of the lateral ankle ligaments is a promising new technique with results similar to those of open surgery.
Keywords: ankle sprains, ankle ligaments, treatment, postoperative care
Ankle sprains are among the most common athletic injuries, comprising 50% of all lower extremity injuries in high school athletes.1 The National Collegiate Athlete Association's Injury Surveillance System has consistently placed ankle sprains among the most prevalent injuries experienced by athletes, accounting for 7% to 15% of all collegiate athletic injuries, with the highest rates among men's and women's basketball players.2,3 The true incidence may be even higher, as more than 50% of athletes with ankle sprains do not seek medical treatment.4
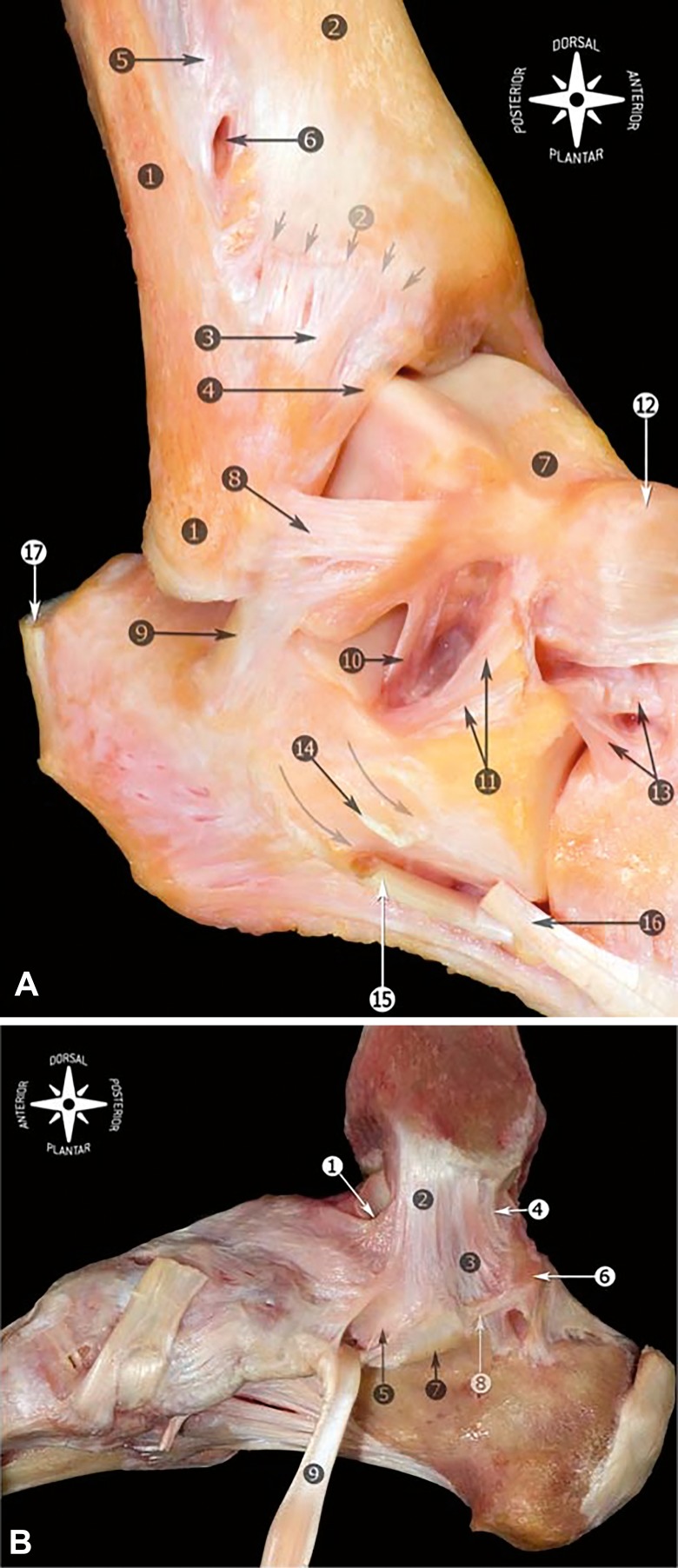
Ankle sprains most often involve injuries to the ligaments that stabilize the lateral ankle. The lateral ankle ligaments consist of a 3-part complex: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL; Figure 1). The ATFL originates at the distal anterior fibula and crosses the lateral ankle joint, often as a 2-band complex, where it inserts at an approximately 45° angle on the talus, anterior to the articular facet. From this position, the ATFL functions to restrict both internal rotation and adduction. The CFL originates below the ATFL along the anterior edge of the distal fibula; it then travels posteriorly and inferiorly to insert on the calcaneus, preventing adduction and inversion of the calcaneus. The PTFL travels horizontally, originating along the posterior talus and inserting on the medial surface of the lateral malleolus, limiting external rotation.
Figure 1.
Anatomy of the ankle ligaments. Right ankle. A, Fibula and tip of the fibula (1); tibia and anterior tubercle with arrows (2); anterior tibiofibular ligament (3); distal fascicle of the tibiofibular ligament (4); interosseous membrane (5); foramen for the perforating branch of the peroneal artery (6); talus (7); anterior talofibular ligament (8); calcaneofibular ligament (9); talocalcaneal interosseous ligament (10); inferior extensor retinaculum, cut (11); talonavicular ligament (12); bifurcate ligament (13); peroneal tubercle, arrows showing the peroneal tendons sulcus (14); peroneus longus tendon (15); peroneus brevis tendon (16); and calcaneal tendon (17). B, Medial view of the anatomic dissection of the main components of the medial collateral ligament. Tibionavicular ligament (1); tibiospring ligament (2); tibiocalcaneal ligament (3); deep posterior tibiotalar ligament (4); spring ligament complex, superomedial calcaneonavicular ligament (5); medial talar process (6); sustentaculum tali (7); medial talocalcaneal ligament (8); and tibialis posterior tendon (9). Reprinted from Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):944–956. Available through Open Access.
Lateral ankle sprains (LASs) typically occur from excessive inversion and internal rotation of the hindfoot while the leg is in external rotation. Injuries to the lateral ankle-ligament complex generally involve the ATFL and CFL, while sparing the PTFL. Midsubstance tears of the ATFL are the most frequent lateral ligament injury, but avulsion injuries can also occur.5,6 The susceptibility of the ATFL to injury may be due to both its orientation as it crosses from the distal fibula to the anterior talus and its lack of robustness. The ATFL has the smallest maximal load and lowest energy to failure of the 3 lateral ankle ligaments.7,8 Injuries to the ATFL can also occur with adduction while the ankle is in plantar flexion, whereas the CFL is injured by excessive inversion and a dorsiflexed ankle.9
The majority of ankle sprains resolve without sequelae; however, 30% of patients experience recurrent functional or mechanical instability.10 Functional instability is characterized by proprioceptive and strength deficits, changes in neuromuscular control, and impaired postural control and is identified from a patient's report of giving way, loss of strength, decreased functional performance, pain, swelling, and frank instability.11 In contrast, mechanical instability is characterized by laxity of the ankle joint due to structural damage of the ligaments and is diagnosed using physical examination and imaging. Chronic ankle instability (CAI) may be due to functional or mechanical instability (or both) and consists of episodes of giving way that lead to repeated ankle sprains, each of which is associated with a short period of pain and swelling and cumulatively lead to long-term decreases in ankle function and athletic performance. Accurate assessment and appropriate initial management of the acute ankle sprain may prevent the development of CAI.12,13
If left untreated, CAI can have severe consequences, as up to 78% of affected individuals will develop posttraumatic ankle osteoarthritis.14 Although not fully understood, this process is thought to be due either to the acute osteochondral lesion incurred during the initial sprain or to the chronic change in joint mechanics causing progressive cartilage degeneration.14,15 Surgical stabilization of the unstable ankle may help to slow or prevent the progression from CAI to posttraumatic ankle osteoarthritis.14
The goal of this review is to familiarize the reader with the evaluation and management of CAI and associated conditions from the perspective of the consultant surgeon. Our hope is that such understanding will aid in communication between athletic trainers and orthopaedic surgeons when treating patients with this common condition.
EVALUATION OF CAI
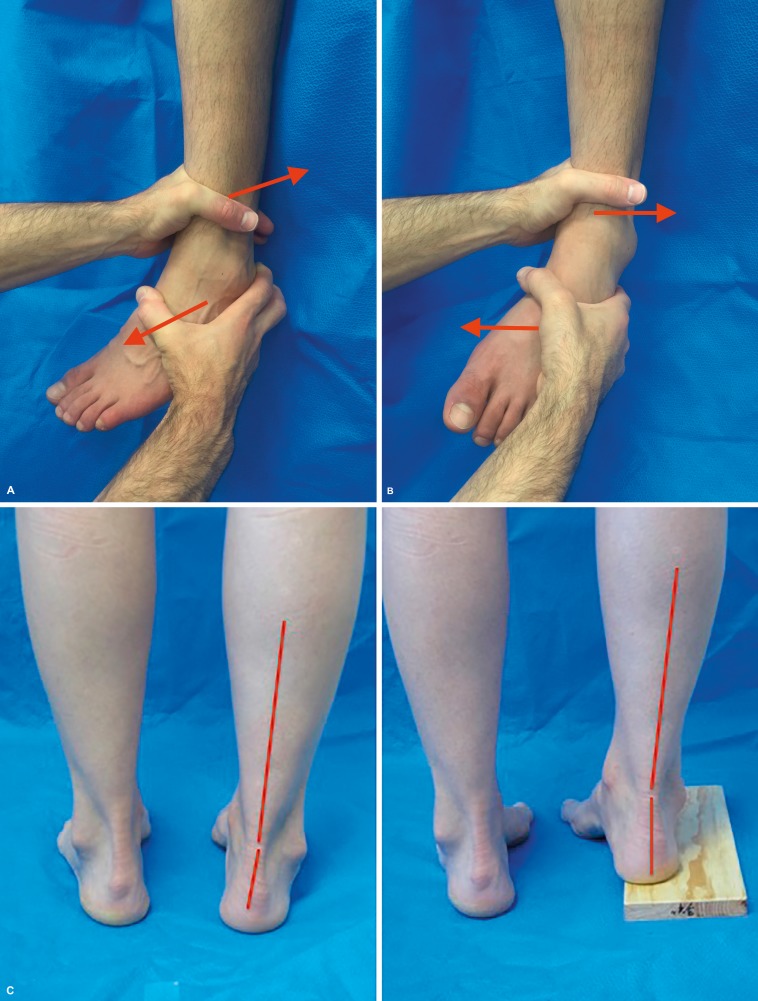
The assessment of the patient with CAI begins with a focused history and physical examination. The history should address the mechanism of the most recent injury, the ability to bear weight, the frequency of instability episodes and ankle sprains, and previous treatments. The physical examination includes an evaluation of gait and standing alignment during which the examiner looks for varus hindfoot alignment, which leads to lateral foot overload and can result in ankle instability, peroneal tendon injury, and fifth metatarsal stress fracture.16 Subtle hindfoot varus is often not recognized when viewing the foot from behind but instead can be recognized by the “peek-a-boo” heel sign, in which the medial border of the heel is seen from in front of the patient. Inspection and palpation of the hindfoot focuses on determining the degree of swelling, location of ecchymosis, point of maximal tenderness (ATFL, CFL, peroneal tendons, or syndesmosis), and whether the peroneal tendons click or are prominent. Range of motion of both the ankle and subtalar joints is assessed with the patient seated and the knee flexed to 90° to eliminate the pull of the gastrocnemius. A neurologic examination evaluates sensation in the distributions of the deep and superficial peroneal nerves and the sural, saphenous, and tibial nerves. The strength of the peroneus brevis is assessed by resisted eversion with the ankle in maximal plantar flexion to prevent the ankle extensors from assisting. The anterior drawer test (Figure 2A) addresses ATFL laxity: the examiner pulls the calcaneus anteriorly and internally, rotating it slightly with the ankle in 15° of plantar flexion. The test is positive when excessive anterior translation of the talus compared with the contralateral side occurs. The talar tilt test (Figure 2B) evaluates the integrity of both the ATFL and CFL: the examiner applies a varus moment to the calcaneus with the ankle in neutral position. As it can be difficult to differentiate physiological subtalar motion from varus tilting at the ankle joint, the test is often performed using fluoroscopy or radiography. A difference ≥15° in inversion of the hindfoot compared with the contralateral ankle is associated with complete rupture of both the ATFL and the CFL.17 The Coleman block test should be performed in patients exhibiting varus alignment to determine whether the hindfoot varus is forefoot driven (Figure 2C) and thus can be corrected by realigning the forefoot and accommodating the plantar-flexed first ray via an orthosis (such as the Arch Rival; DJO Global, Dallas, TX). The squeeze test (compression between the proximal tibia and fibula produces pain at the ankle) and the external-rotation stress test are used to evaluate syndesmosis injury (high ankle sprain).
Figure 2.
Special tests used in the examination of patients with lateral ankle instability. Left ankle. A, The anterior drawer test. B, The talar tilt test. C, The Coleman block test, which evaluates hindfoot flexibility and pronation of the forefoot.
The assessment of CAI also includes standing 3-view (anteroposterior, mortise, and lateral) radiographs of the ankle to evaluate alignment and identify the presence of arthritis, avulsion fracture, syndesmotic widening, or osteochondral lesion. Stress radiographs can be added to assess ligament function when the physical examination is equivocal. Magnetic resonance imaging or ultrasound should be obtained to assess the lateral ankle ligaments, peroneal tendons, peroneal retinacula, and syndesmotic ligaments. Magnetic resonance imaging is also used to determine the presence of an osteochondral lesion, whereas ultrasound is better for detecting transient subluxation or dislocation of the peroneal tendons.18
CONCOMITANT INJURIES
Lateral ankle pain that persists for more than 3 months after an acute inversion injury should lead to the search for not only CAI but also any of a number of other injuries that can occur concomitantly with LAS. Collectively, these disorders are often referred to as “the ankle sprain that will not heal”; they include peroneal tendinitis, peroneal tendon tear, peroneal subluxation, osteochondral lesion of the talus (OLT), high ankle sprain (syndesmotic injury), and ankle impingement.
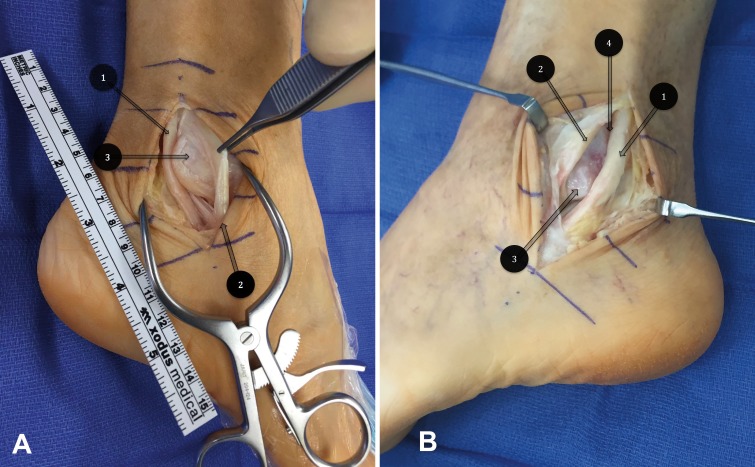
Peroneal tendon injuries occur commonly with LASs, as the peroneus brevis is an active stabilizer of the lateral ankle and fires reflexively to prevent excessive inversion of the ankle. Longitudinal-split tears of the peroneus brevis (Figure 3A) can occur when the brevis tendon pulls forcefully against the distal fibula, causing lateral translation within the fibular groove. This same mechanism is thought to lead to peroneal subluxation (Figure 3B) or dislocation due to tearing or avulsion of the superior peroneal retinaculum, which restrains the peroneal tendons within the fibular groove. Peroneal tendinitis and tenosynovitis occur from ineffective or incomplete healing of the overloaded peroneal tendons.
Figure 3.
Peroneal tendon injury often occurs in conjunction with lateral ankle ligament instability. Left ankle. A, A longitudinal split tear of the peroneus brevis: (1) peroneus longus, (2) peroneus brevis, and (3) lateral malleolus. B, Subluxation of the peroneal tendons due to a superior peroneal retinacular tear: (1) peroneus longus, (2) peroneus brevis, (3) lateral malleolus, and (4) fibular groove.
Osteochondral lesions of the talus also commonly occur with lateral ankle ligament injuries. The incidence has been reported19 to be as high as 89%; fortunately, the majority of these lesions are asymptomatic. The mechanism of OLT involves impaction of the shoulder of the centromedial talar dome on the tibial plafond with ankle inversion, leading to subchondral fracture and chondral compromise.
High ankle sprains involve injury to the syndesmotic ligaments, which bind the tibia to the fibula and maintain the stability of the ankle mortise. High ankle sprains often occur from excessive external rotation of the talus, which acts as a wedge to drive the ankle mortise apart.20 High ankle sprains are less common, take longer to heal, and have a higher morbidity than LASs. Untreated syndesmotic injury can lead to incongruity of the ankle joint and early arthritis.
The medial ankle ligaments are concomitantly injured in 2.8% of lateral ankle injuries.21 Medial-sided ecchymosis or tenderness should alert the examiner to the possibility of medial ankle-ligament injury. Medial ankle symptoms indicate a more severe injury, portend a poorer prognosis, and necessitate a longer healing time. Patients with medial-sided injuries are frequently immobilized in a cast for the first few weeks postinjury to prevent attenuation of the deltoid and spring ligaments during the healing process.
Ankle impingement can occur after ankle-ligament injury when synovial hypertrophy or fibrous bands form between the talus and tibia, resulting in pain or a feeling of giving way (or both) without ligamentous laxity. The diagnosis of impingement is made once other causes of the symptoms have been eliminated. The initial treatment for impingement should be directed at decreasing inflammation and relieving symptoms. Patients who do not respond to initial treatment may benefit from ankle arthroscopy with partial synovectomy.
These disorders should be suspected in any patient with an ankle sprain whose symptoms have persisted for 3 months or more. The workup for each disorder involves eliciting the characteristic physical examination findings and then confirming the diagnosis using magnetic resonance imaging or ultrasound. Treatment details for the associated disorders are beyond the scope of this review; however, a number of articles on these topics are available.20,22,23 The remainder of this review will focus on CAI treatment.
NONOPERATIVE TREATMENT
The initial management of CAI consists of functional rehabilitation and the use of bracing or taping. Rehabilitative exercises include proprioceptive training and eversion (peroneus brevis) strengthening. Ankle bracing or taping improves mechanical and functional stability in athletes with CAI.24 Both taping and bracing restrict range of motion, reduce reinjury rates, improve proprioception, have minimal negative effects on other joints, and do not affect athletic performance. Bracing with an ankle-stabilizing orthosis (a soft brace that provides compression and has straps crossing the ankle joint) limits varus angulation and provides proprioceptive feedback that helps to improve active stabilization by the peroneus brevis. Taping is less bulky than bracing and may cater to unusual anatomy; however, bracing has the advantage of being reusable and easily adjustable. Approximately 80% of patients improve with functional rehabilitation and bracing. Nonsteroidal anti-inflammatory drugs, either taken orally or applied topically, may be used to provided short-term (1–3 weeks) pain relief and a reduction in swelling, but they have no long-term effects on the symptoms of CAI. A detailed description of the nonoperative treatment of CAI is beyond the scope of this review.
OPERATIVE TREATMENT
Operative treatment of CAI is indicated in patients who have failed to improve on a 3- to 6-month trial of nonoperative management because of either persistent pain or mechanical instability. The operative treatments for lateral CAI include a variety of procedures ranging from simple repairs to complex reconstructions. Repairs consist of either reattaching or imbricating (shortening) the injured native tissues, whereas reconstructions involve replacing the ligaments with either autologous or allograft tissue. Furthermore, reconstructions may be either anatomic or nonanatomic. Anatomic reconstructions maintain the physiological orientation of the ATFL or CFL or both by attempting to preserve native ankle anatomy and normal joint kinematics. Nonanatomic reconstructions involve recreating the lateral ankle support using tissue that does not follow the physiological orientation of the ATFL and CFL.
Lateral ankle ligament surgery is generally performed as an outpatient procedure under general anesthesia and often supplemented with a popliteal nerve block. The patient is positioned in the lateral decubitus position. Laxity of the ATFL and CFL should be confirmed while the patient is under anesthesia by performing the anterior drawer and talar tilt tests under fluoroscopy. Equivocal results can be resolved by comparison with the contralateral side25; thus, the examination should be done before the surgical site is prepared.
Primary Repair (Broström and Its Modifications)
Anatomic repair of the lateral ligamentous complex remains the criterion standard for recurrent ankle instability, effectively restoring native ankle anatomy and joint kinematics while preserving motion. The Broström procedure and its modifications are the most common of the anatomic-repair procedures.
Broström Technique
First described in 1966, the Broström repair5 has evolved over the last 50 years to include several modifications, including those by Gould and Karlsson, and has recently been combined with ankle arthroscopy to identify and treat the concomitant osteochondral lesions.26
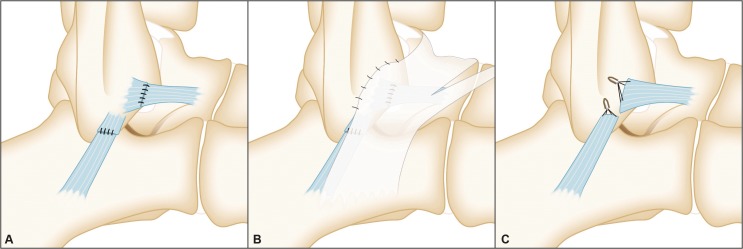
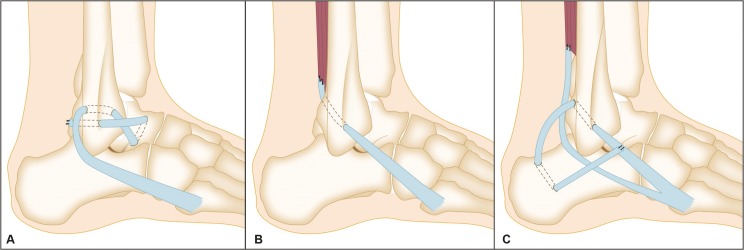
The Broström technique was designed to repair both the ATFL and CFL while retaining the anatomic relationship of the lateral ankle structures. The procedure can be performed using either a curved incision over the anterior border of the lateral malleolus (for isolated ligament repair) or an extensile longitudinal incision along the distal fibula (when concomitant tendon or retinacular repair is planned). The subcutaneous tissues are retracted anteriorly and the ATFL and CFL are identified as thickenings of the lateral aspect of the ankle-joint capsule (Figure 4A). The ATFL and CFL are then dissected free of the surrounding tissue, cut in the midsubstance, and repaired in a pants-over-vest fashion.5,25 After the repair has been completed, ankle stability should be reexamined using the anterior drawer and talar tilt tests. Once stability is confirmed, the ankle should be taken through a full range of plantar-flexion and dorsiflexion exercises to confirm that the repair has not limited the ankle range of motion.26
Figure 4.
Techniques for repair of the lateral ankle ligaments. A, Left-ankle Broström procedure. B, Left-ankle Gould modification of the Broström. C, Left-ankle Karlsson procedure.
The Broström is a highly effective and durable procedure. A long-term follow-up study27 identified 31 male patients who had undergone a Broström procedure for CAI as midshipmen enrolled in the US Naval Academy. The mean follow-up time in this study was 26.3 years. Using a self-report questionnaire, these patients were found to have high-functioning ankle joints with a mean numeric score for overall ankle function of 91.2 out of 100.27 Ninety-one percent of these patients also reported good or excellent results using the Good Ankle Function Scale.28 A total of 87% of the patients had full motion of the ankle joint restored postoperatively, and none cited ankle symptoms as affecting the length of their military career.29
In a recent study30 of patients with CAI, all had improved stability after the Broström procedure and reoperation rates were low. The mean follow-up time in this study was 3.6 years (range = 1–6.2 years). Among the 20 patients studied, only 3 had reoperations; 2 for probable subcutaneous nerve entrapment and 1 for posttraumatic osteoarthritis of the ankle joint.30 Overall, the Broström procedure has shown excellent results in restoring ankle stability, with relatively low reoperation rates and good longevity.31
Gould Modification
In 1980, Gould et al32 described a modification to the Broström technique in which the repair of the lateral ankle ligaments was reinforced by pulling the extensor retinaculum proximally and suturing it to the distal fibula (Figure 4B). This has the effect of both reinforcing the ATFL repair and limiting inversion to stabilize the subtalar joint.32 This modification has been shown to increase the strength of the repair by 50%.33
Karlsson Procedure
The Karlsson procedure34 is a variation of the Broström technique that was initially designed for late repair of LASs. The rationale behind this procedure was that the ATFL and CFL often heal after injury with increased length, which then causes laxity. This procedure eliminates the laxity by sectioning the ligaments 3 to 5 mm from their insertions on the fibula, excising the intervening scar tissue, and then reattaching the ligaments to the fibula using drill holes or, more recently, suture anchors34 (Figure 4C). The advantage of the Karlsson over the Broström procedure is its ligament-to-bone healing, as opposed to the ligament-to-ligament healing that occurs with the Broström procedure. A 3-year follow-up study of 60 patients who underwent the Karlsson procedure showed that functional results, including functional stability, pain, activity levels, and swelling, were good to excellent among 88% of patients. Commonly, both the ATFL and CFL are repaired, as 95% of patients undergoing repair of both had good to excellent results compared to 75% of those who underwent isolated ATFL repair.34
Secondary Reconstruction
Anatomic repairs (Broström and related procedures) address lateral ankle-ligament instability by shortening, tightening, or reattaching the native ligaments. Although these techniques are effective in most patients, they are not effective in those with severely attenuated or absent ligaments. In these situations, the surgeon must choose between nonanatomic and anatomic reconstruction using either local tendon transfer or free allograft- or autograft-tendon reconstruction.
Nonanatomic Reconstructions
Nonanatomic reconstructions stabilize the lateral ankle without repair of the native ligaments. These techniques involve rerouting the peroneus brevis tendon through bone tunnels in the distal fibula. Examples of nonanatomic reconstructions include the Watson-Jones,35 Evans,36 and Chrisman-Snook37 procedures (Figure 5). These procedures are included for historic interest as they alter hindfoot biomechanics, limit motion, and lead to the development of early arthritis. As a result, they have largely been supplanted by anatomic reconstructions.35–37
Figure 5.
The nonanatomic reconstructions. Right ankle. A, The Watson-Jones procedure. B, The Evans procedure. C, The Chrisman-Snook procedure.
Researchers in several long-term outcome studies have looked at the efficacy of these nonanatomic repairs for return of ankle function and performance. A 5-year follow-up study38 of a modified Evans procedure did not show promising results: only half of patients reported their ankles were fully recovered or much better than before surgery. Performance testing demonstrated even worse outcomes, with only 35% of the 48 ankles attaining a score of good to excellent. In addition, ankle range of motion was significantly impaired, and the incidence of ankle swelling and calf-muscle atrophy increased. Another study39 with a 14-year follow-up period also showed similar poor results for the Evans procedure: only 50% of patients endorsed satisfactory function and stability of the ankle. The majority of those with poor results complained of pain, instability, swelling, and restricted activity. In a prospective study40 comparing the modified Broström and Chrisman-Snook procedures among 40 patients with CAI, more than 80% had good to excellent stability. Patients who underwent the modified Broström procedure had better ankle-function scores with significantly fewer complications.
The long-term outcomes of nonanatomic reconstruction include alterations in ankle and hindfoot kinematics and the frequent loss of subtalar motion, leading to greater risks of progression to arthritis and further sequelae.41–43 Comparison studies with longer follow-ups mostly indicated that anatomic repair was favored over nonanatomic tenodesis reconstruction. Long-term studies of nonanatomic tenodesis have shown that these procedures resulted in ankle laxity, limited range of motion, decreased function, increased pain, increased need for revision procedures, and higher degrees of osteoarthritis compared with anatomic reconstruction.41 Their role as revision procedures when anatomic repair has failed has been replaced with anatomic graft–based reconstructions.
Anatomic Graft Reconstruction
For anatomic graft reconstructions, autogenous or allogenic tendon grafts are placed at the native ligament insertion sites to recreate both the anatomy and mechanics of the ATFL and CFL. These techniques are especially useful in patients with long-standing instability that has resulted in poor tissue quality, failed previous repair, generalized ligamentous laxity, and cavovarus foot deformity.44
A variety of reconstruction procedures have been described using different graft types, fixation methods, and materials.45–53 In these procedures, the graft is routed through tunnels in the distal fibula, the talus, and the calcaneus to recreate both the ATFL and CFL (Figure 6). The tendon grafts can be affixed either through sutures to themselves or by placing interference screws into the tunnels.
Figure 6.
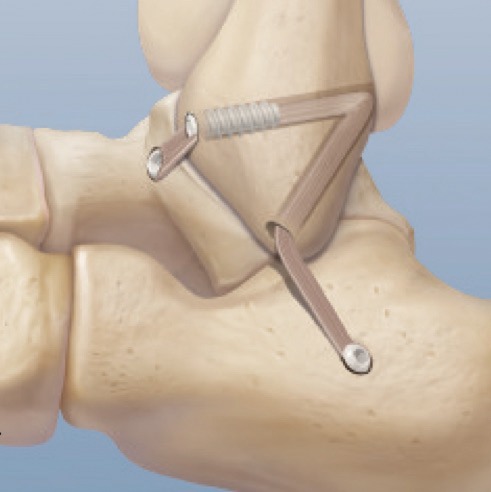
Right ankle. Anatomic reconstruction of the lateral ankle ligaments using Arthrex Lateral Ankle Reconstruction Implant System and VersaGraft. VersaGraft travels through tunnels in the distal fibula, talus, and calcaneus, and achieves anatomic reconstruction of the anterior talofibular and calcaneofibular ligaments with simple tensioning and rigid fixation. Reprinted with permission from VersaGraft presutured tendon for lateral ankle reconstruction. Arthrex Web site. https://www.arthrex.com/foot-ankle/lateral-ankle-ligament-reconstruction.
These procedures have demonstrated excellent results. One study45 of 28 patients undergoing gracilis autograft reconstruction showed that all patients rated their level of satisfaction as good to excellent. Seventy-nine percent of patients remained pain free at final follow-up, with a mean follow-up duration of 23 months. The remaining patients experienced mild pain, with morning stiffness among 24% and mild swelling postexercise in 21%. In another investigation53 of 38 patients who underwent reconstruction with semitendinosus allograft performed by a single surgeon over 8 years, all were satisfied with the procedure, mean Ankle-Hindfoot Scale scores increased by nearly 30 points, and overall pain scores decreased. A total of 71% of patients returned to preinjury or near preinjury activity levels; in addition, laxity improved among all patients. Other authors54 followed 19 patients for 30 months after allograft tendon reconstruction and observed that all had returned to activity without instability, pain, or decreased range of motion. One potential risk of these surgeries is fracture through the fibular tunnels, which are large (4–6 mm) in comparison with the tip of the fibula.55
Ankle Arthroscopic and Arthroscopic Ligament Repair
Ankle arthroscopy has commonly been performed in conjunction with open lateral ankle ligament reconstruction on patients who have concomitant lesions such as OLT, anterior ankle impingement, or a loose intra-articular body. Symptomatic OLT is treated with chondral debridement, microfracture, or retrograde drilling.
The arthroscopic Broström procedure was developed to address a number of challenges that arose when performing open repair after arthroscopy, such as soft tissue swelling from extravasated fluid that obscured tissue planes and the additional surgery time for patient repositioning between ankle arthroscopy and open lateral ankle-ligament repair. A number of techniques have been described for arthroscopic lateral ankle-ligament repair.56–58 These procedures are similar to the modified Broström procedure, except that the surgeon places the anchors while viewing the distal fibula through an arthroscope rather than through an open exposure of the distal fibula. The technical details of the arthroscopic Broström are beyond the scope of this review. Arthroscopic repair has been shown to restore equivalent function as open repair but with the advantages of smaller scars, less pain, less swelling, less disturbance of cutaneous sensation,56 and possibly faster recovery.57 Despite these reported advantages, arthroscopic repair has not yet gained widespread acceptance, perhaps because of the simplicity, reliability, and rapidity of the standard open-repair techniques.
Postoperative Management and Return to Sport
Postoperative protocols vary among surgeons and depend on the specific repair or reconstruction performed (Table). Generally, the postoperative protocol consists of an initial 2- to 6-week period of cast, splint, or boot immobilization to prevent stressing of the repaired or reconstructed tissue by inversion. Rehabilitative exercises are started after this initial period of immobilization. Initial therapy focuses on restoring ankle range of motion. Proprioceptive training and strength training begin once complete range of motion has been restored.
Table.
Surgical Management of Chronic Ankle Instability: Postoperative Protocols
| Study |
Weight-Bearing Status |
Immobilization |
Therapeutic Exercises |
Return to Play |
| Bell et al29 (2006) | Unspecified | Splint postoperatively for unspecified time period | Unspecified motion and activity | Return of ankle strength |
| Baraza et al30 (2017) | NWB for 6 wk before allowing WBAT in a MalleoLoca ankle splint | Cast for 6 wk postsurgery | PT involving gentle ROM exercises | Unspecified |
| Karlsson et al34 (1989) | Unspecified | Below-the-knee cast for 6 wk postsurgery | Peroneal strengthening exercises and coordination training using tilt boards for 6–12 wk | Ankle is functionally stable |
| Acevedo and Mangone56 (2015) | NWB for 2 wk postoperatively WBAT for wk 2–4 Full weight bearing for wk 4–6 | Short-leg splint for 2 wk postsurgery Boot walker for wk 2–4 Lace-up ankle brace for wk 4–6 Active ankle brace for 12 wk postsurgery and for 6 mo when participating in sports/high-impact physical activity | Gentle ROM exercises for wk 2–4 Continue dorsiflexion and plantar-flexion exercises for wk 4–6 PT involving peroneal muscle strengthening and proprioception at wk 6+ | Normal ankle strength and functional test performance at least 90% of opposite leg |
| Kaikkonen et al38 (1999) | Full weight bearing as soon as possible without pain | Below-knee plaster cast for 4–6 wk postsurgery | Isometric muscle exercises of the ankle, exercises of thigh muscle, and of knee joint while in cast | Unspecified |
| Active nonrestricted flexion-extension exercises after cast removal | ||||
| Karlsson et al39 (1988) | WBAT after 3 wk postsurgery | Below-the-knee plaster for 6 wk postsurgery | Unspecified | Unspecified |
| Hennrikus et al40 (1996) | Unspecified | Bulky compression dressing with ankle in neutral position for 2 wk postsurgery | Dorsiflexion and plantar-flexion exercises after cast removal | 3 mo after cast removal |
| Short-leg walking cast for wk 2–6 | ||||
| Sefton et al59 (1979) | WBAT after wound is healed | Below-the-knee plaster for 6 wk postsurgery | Graduated weight-bearing activities after plaster is removed | Unspecified |
| Li et al60 (2009) | NWB for 10–14 d postoperatively | Splint for 4 wk postsurgery Protective ankle brace starting at wk 4 | ROM exercises starting wk 4 Proprioception and strength training for wk 6–8 Plyometrics for wk 8–12 Straight running and functional activity starting at wk 12 Cutting and sports drills starting at wk 16 | Soon after cutting and sports drills |
Abbreviations: NWB, non–weight bearing; PT, physical therapy; ROM, range of motion; WBAT, weight bearing as tolerated.
a Bauerfeind AG, Zeulenroda-Triebes, Germany.
The timing of and specific criteria for return to activity and return to play have not been well defined but depend on the specific injury and the surgery performed. Patients may return to running on level ground once they demonstrate that 90% of their ankle strength has been restored, usually around 3 months after surgery. Cutting and jumping may then resume 4 to 6 months after surgery if balance and proprioception have been adequately restored.25
Return to play can be considered when an athlete no longer experiences pain or swelling; demonstrates normal ankle stability, strength, and neuromuscular control; and is able to perform a set of relevant functional tests. Ankle stability is assessed with the anterior drawer and talar tilt tests and by questioning the patient about episodes of giving way, swelling, or pain. The evaluation of neuromuscular control includes proprioception, balance, and postural control. Strength deficits in all muscle groups are assessed, but particular attention is paid to inversion and eversion.58 A large number of functional tests have been used to evaluate athletes with lateral ankle injuries, including lateral- and forward-hop tests, timed single-legged–stance tests, and heel-rocker tests to assess dorsiflexion of the ankle.24 However, because no consensus exists as to the specific functional tests an athlete would need to pass before returning to sport, many authors have suggested reasonable alternatives that accommodate individual athletes rather than a generalized population of athletes. For example, in 1 protocol, an athlete may be cleared to return to play simply by performing a full-speed figure of 8.56 Other protocols deem an athlete ready to return to sport if he or she can perform both cutting exercises and drills pertaining to the desired sport—for example, karaoke drills in soccer, double jumps in basketball, or burpees in football.60 Furthermore, some researchers40 who used casts for 6 weeks as their postoperative immobilization protocol suggested that an athlete may return to play 3 months after cast removal without mention of passing any functional tests. Ankle bracing or taping should be considered for all athletes returning to play, as these interventions were associated with a 70% decrease in recurrent ankle sprains.61 Ankle bracing or taping should be continued for at least 6 months after injury or surgery to allow time for ligamentous healing.
Our preferred postoperative protocol for lateral ligament reconstruction and repair involves cast placement in the operating room and the patient weight bearing as tolerated. At 3 weeks, the patient is seen for cast and suture removal. He or she is then placed in a removable boot for 3 weeks and asked to remove the boot 3 times a day for ankle range-of-motion exercises. At 6 weeks postsurgery, physical therapy and subtalar-joint range of motion may begin with proprioceptive training and eversion strengthening. Inversion stretching is not permitted until 3 months postsurgery. An ankle-stirrup splint is worn from 6 weeks to 3 months to prevent accidental inversion, which could injure the healing ligaments. At 3 months, the athlete is allowed to return to play in a functional brace.
SUMMARY
Lateral ankle instability is initially treated nonoperatively. Athletes who have failed to improve after 3 to 6 months of bracing and functional rehabilitation may benefit from surgery to restore ankle stability, reduce pain, and improve function. The preferred operative treatment is primary repair using a modified Broström technique because of its simplicity and strong reproducible outcomes. Anatomic reconstruction using tendon graft is performed when patients lack adequate tissue for repair. Nonanatomic reconstructions are performed infrequently, as they alter ankle mechanics and thus can lead to early arthritis. Postoperative protocols vary but generally involve a short period of immobilization followed by bracing and functional rehabilitation. Return to play should be considered when an athlete no longer experiences pain or swelling; demonstrates normal ankle stability, strength, and neuromuscular control; and is able to perform a set of relevant functional tests.
REFERENCES
- 1.Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among US high school athletes. Acad Emerg Med. 2007;14(7):641–645. doi: 10.1197/j.aem.2007.03.1354. [DOI] [PubMed] [Google Scholar]
- 2.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 3.Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(1):201–209. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 4.McKay GD, Goldie P, Payne WR, Oakes B. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Broström L. Sprained ankles, VI: surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132(5):551–565. [PubMed] [Google Scholar]
- 6.Hølmer P, Søndergaard L, Konradsen L, Nielsen PT, Jørgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15(2):72–74. doi: 10.1177/107110079401500204. [DOI] [PubMed] [Google Scholar]
- 7.Siegler S, Block J, Schneck CD. The mechanical characteristics of the collateral ligaments of the human ankle joint. Foot Ankle. 1988;8(5):234–242. doi: 10.1177/107110078800800502. [DOI] [PubMed] [Google Scholar]
- 8.Attarian DE, McCrackin HJ, DeVito DP, McElhaney JH, Garrett WE., Jr Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985;6(2):54–58. doi: 10.1177/107110078500600202. [DOI] [PubMed] [Google Scholar]
- 9.Stephens MM, Sammarco GJ. The stabilizing role of the lateral ligament complex around the ankle and subtalar joints. Foot Ankle. 1992;13(3):130–136. doi: 10.1177/107110079201300304. [DOI] [PubMed] [Google Scholar]
- 10.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–365. [PMC free article] [PubMed] [Google Scholar]
- 12.Peters JW, Trevino SG, Renstrom PA. Chronic lateral ankle instability. Foot Ankle. 1991;12(3):182–191. doi: 10.1177/107110079101200310. [DOI] [PubMed] [Google Scholar]
- 13.Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14(6):465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- 14.Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354–361. [PubMed] [Google Scholar]
- 15.Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–409. doi: 10.1177/03635465020300031601. [DOI] [PubMed] [Google Scholar]
- 16.Younger AS, Hansen ST., Jr Adult cavovarus foot. J Am Acad Orthop Surg. 2005;13(5):302–315. doi: 10.5435/00124635-200509000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Lynch SA. Assessment of the injured ankle in the athlete. J Athl Train. 2002;37(4):406–412. [PMC free article] [PubMed] [Google Scholar]
- 18.Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD, High-resolution US. and MR imaging of peroneal tendon injuries. Radiographics. 2015;35(1):179–199. doi: 10.1148/rg.351130062. [DOI] [PubMed] [Google Scholar]
- 19.Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury: an arthroscopic study. Am J Sports Med. 1993;21(1):120–127. doi: 10.1177/036354659302100120. [DOI] [PubMed] [Google Scholar]
- 20.Norkus SA, Floyd R. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36(1):68–73. [PMC free article] [PubMed] [Google Scholar]
- 21.Hintermann B, Valderrabano V, Boss A, Trouillier HH, Dick W. Medial ankle instability: an exploratory, prospective study of fifty-two cases. Am J Sports Med. 2004;32(1):183–190. doi: 10.1177/0095399703258789. [DOI] [PubMed] [Google Scholar]
- 22.Easley ME, Latt DL, Santangelo JR, Merian-Genast M, Nunley JA., II Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2010;18(10):616–630. doi: 10.5435/00124635-201010000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Philbin TM, Landis GS, Smith B. Peroneal tendon injuries. J Am Acad Orthop Surg. 2009;17(5):306–317. doi: 10.5435/00124635-200905000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Callaghan MJ. Role of ankle taping and bracing in the athlete. Br J Sports Med. 1997;31(2):102–108. doi: 10.1136/bjsm.31.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell SJ, Walthour CS, Provencher MT, Sitler D. Chronic lateral ankle instability: the Broström procedure. Op Tech Sports Med. 2005;13(3):176–182. [Google Scholar]
- 26.Hamilton WG, Thompson FM, Snow SW. The modified Brostrom procedure for lateral ankle instability. Foot Ankle. 1993;14(1):1–7. doi: 10.1177/107110079301400101. [DOI] [PubMed] [Google Scholar]
- 27.Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001;22(10):788–794. doi: 10.1177/107110070102201004. [DOI] [PubMed] [Google Scholar]
- 28.Good CJ, Jones MA, Livingstone BN. Reconstruction of the lateral ligament of the ankle. Injury. 1975;7(1):63–65. doi: 10.1016/0020-1383(75)90065-0. [DOI] [PubMed] [Google Scholar]
- 29.Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34(6):975–978. doi: 10.1177/0363546505282616. [DOI] [PubMed] [Google Scholar]
- 30.Baraza N, Hardy E, Shahban SA. Re-operation rates following Brostrom repair. JSM Foot Ankle. 2017;2(1):1019. [Google Scholar]
- 31.Maffulli N, Del Buono A, Maffulli GD, et al. Isolated anterior talofibular ligament Broström repair for chronic lateral ankle instability: 9-year follow-up. Am J Sports Med. 2013;41(4):858–864. doi: 10.1177/0363546512474967. [DOI] [PubMed] [Google Scholar]
- 32.Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1(2):84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 33.Aydogan U, Glisson RR, Nunley JA. Extensor retinaculum augmentation reinforces anterior talofibular ligament repair. Clin Orthop Rel Res. 2006;442:210–215. doi: 10.1097/01.blo.0000183737.43245.26. [DOI] [PubMed] [Google Scholar]
- 34.Karlsson J, Bergsten T, Lansinger O, Peterson L. Surgical treatment of chronic lateral instability of the ankle joint: a new procedure. Am J Sports Med. 1989;17(2):268–274. doi: 10.1177/036354658901700220. [DOI] [PubMed] [Google Scholar]
- 35.Watson-Jones R. Fractures and Joint Injuries Vol 2. 4th ed. Edinburgh, Scotland: E & S Livingstone Ltd; 1955. [Google Scholar]
- 36.Evans DL. Recurrent instability of the ankle: a method of surgical treatment. Proc R Soc Med. 1953;46(5):343–344. doi: 10.1177/003591575304600507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chrisman OD, Snook GA. Reconstruction of lateral ligament tears of the ankle: an experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969;51(5):904–912. [PubMed] [Google Scholar]
- 38.Kaikkonen A, Lehtonen H, Kannus P, Järvinen M. Long-term functional outcome after surgery of chronic ankle instability. A 5-year follow-up study of the modified Evans procedure. Scand J Med Sci Sports. 1999;9(4):239–244. doi: 10.1111/j.1600-0838.1999.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 39.Karlsson J, Bergsten T, Lansinger O, Peterson L. Lateral instability of the ankle treated by the Evans procedure: a long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988;70(3):476–480. doi: 10.1302/0301-620X.70B3.3372575. [DOI] [PubMed] [Google Scholar]
- 40.Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability: a prospective, randomized comparison. Am J Sports Med. 1996;24(4):400–404. doi: 10.1177/036354659602400402. [DOI] [PubMed] [Google Scholar]
- 41.Korkala O, Sorvali T, Niskanen R, Haapala J, Tanskanen P, Kuokkanen H. Twenty-year results of the Evans operation for lateral instability of the ankle. Clin Orthop Rel Res. 2002;405:195–198. doi: 10.1097/00003086-200212000-00025. [DOI] [PubMed] [Google Scholar]
- 42.Krips R, Van Dijk C, Halasi T, et al. Anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: a 2- to 10-year follow-up, multicenter study. Knee Surg Sports Traumatol Arthrosc. 2000;8(3):173–179. doi: 10.1007/s001670050210. [DOI] [PubMed] [Google Scholar]
- 43.Krips R, van Dijk CN, Halasi T, et al. Long-term outcome of anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: a multicenter study. Foot Ankle Int. 2001;22(5):415–421. doi: 10.1177/107110070102200510. [DOI] [PubMed] [Google Scholar]
- 44.Clanton TO, Viens NA, Campbell KJ, LaPrade RF, Wijdicks CA. Anterior talofibular ligament ruptures, part 2: biomechanical comparison of anterior talofibular ligament reconstruction using semitendinosus allografts with the intact ligament. Am J Sports Med. 2014;42(2):412–416. doi: 10.1177/0363546513509963. [DOI] [PubMed] [Google Scholar]
- 45.Coughlin MJ, Schenck RC, Jr, Grebing BR, Jr, Treme G. Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft. Foot Ankle Int. 2004;25(4):231–241. doi: 10.1177/107110070402500407. [DOI] [PubMed] [Google Scholar]
- 46.Horibe S, Shino K, Taga I, Inoue M, Ono K. Reconstruction of lateral ligaments of the ankle with allogeneic tendon grafts. J Bone Joint Surg Br. 1991;73(5):802–805. doi: 10.1302/0301-620X.73B5.1894670. [DOI] [PubMed] [Google Scholar]
- 47.Okuda R, Kinoshita M, Morikawa J, Jotoku T, Abe M. Reconstruction for chronic lateral ankle instability using the palmaris longus tendon: is reconstruction of the calcaneofibular ligament necessary? Foot Ankle Int. 1999;20(11):714–720. doi: 10.1177/107110079902001107. [DOI] [PubMed] [Google Scholar]
- 48.Hintermann B, Renggli P. Anatomic reconstruction of the lateral ligaments of the ankle using a plantaris tendon graft. Orthopäde. 1999;28(9):778–784. doi: 10.1007/PL00003667. [DOI] [PubMed] [Google Scholar]
- 49.Sugimoto K, Takakura Y, Kumai T, Iwai M, Tanaka Y. Reconstruction of the lateral ankle ligaments with bone-patellar tendon graft in patients with chronic ankle instability: a preliminary report. Am J Sports Med. 2002;30(3):340–346. doi: 10.1177/03635465020300030701. [DOI] [PubMed] [Google Scholar]
- 50.Schenck RC, Jr, Coughlin MJ. Lateral ankle instability and revision surgery alternatives in the athlete. Foot Ankle Clin. 2009;14(2):205–214. doi: 10.1016/j.fcl.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 51.Järvelä T, Weitz H, Järvelä K, Alavaikko A. A novel reconstruction technique for chronic lateral ankle instability: comparison to primary repair. Int Orthop. 2002;26(5):314–317. doi: 10.1007/s00264-002-0373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caprio A, Oliva F, Treia F, Maffulli N. Reconstruction of the lateral ankle ligaments with allograft in patients with chronic ankle instability. Foot Ankle Clin. 2006;11(3):597–605. doi: 10.1016/j.fcl.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 53.Dierckman BD, Ferkel RD. Anatomic reconstruction with a semitendinosus allograft for chronic lateral ankle instability. Am J Sports Med. 2015;43(8):1941–1950. doi: 10.1177/0363546515593942. [DOI] [PubMed] [Google Scholar]
- 54.Wang W, Xu GH. Allograft tendon reconstruction of the anterior talofibular ligament and calcaneofibular ligament in the treatment of chronic ankle instability. BMC Musculoskelet Disord. 2017;18(1):150. doi: 10.1186/s12891-017-1492-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Roward Z, Latt LD. Fracture through a distal fibular tunnel used for an anatomic lateral ankle ligament reconstruction. Foot Ankle Orthop. 2018;3(2) doi: 10.1177/2473011418763593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Acevedo JI, Mangone P. Arthroscopic Brostrom technique. Foot Ankle Int. 2015;36(4):465–473. doi: 10.1177/1071100715576107. [DOI] [PubMed] [Google Scholar]
- 57.Nery C, Raduan F, Del Buono A, Asaumi ID, Cohen M, Maffulli N. Arthroscopic-assisted Broström-Gould for chronic ankle instability: a long-term follow-up. Am J Sports Med. 2011;39(11):2381–2388. doi: 10.1177/0363546511416069. [DOI] [PubMed] [Google Scholar]
- 58.Vega J, Golanó P, Pellegrino A, Rabat E, Peña F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34(12):1701–1709. doi: 10.1177/1071100713502322. [DOI] [PubMed] [Google Scholar]
- 59.Sefton GK, George J, Fitton JM, McMullen H. Reconstruction of the anterior talofibular ligament for the treatment of the unstable ankle. J Bone Joint Surg Br. 1979;61(3):352–354. doi: 10.1302/0301-620X.61B3.113415. [DOI] [PubMed] [Google Scholar]
- 60.Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37(3):488–494. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
- 61.Dizon JMR, Reyes JJB. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport. 2010;13(3):309–317. doi: 10.1016/j.jsams.2009.05.002. [DOI] [PubMed] [Google Scholar]