Abstract
Copious research exists regarding ankle instability, yet lateral ankle sprains (LASs) persist in being among the most common recurrent musculoskeletal injuries. Key anatomical structures of the ankle include a triform articulating structure that includes the inferior tibiofibular, talocrural, and subtalar joints. Functionally, force absorption and propulsion through the ankle complex are necessary for any task that occurs in weight bearing. For optimal ankle performance and avoidance of injury, an intricate balance between stability and mobility is necessary to ensure that appropriate force transfer occurs during sports and activities of daily living. Consideration for the many structures that may be directly or indirectly involved in LASs will likely translate into advancements in clinical care. In this clinical review, we present the structure, function, and relevant pathologic states of the ankle complex to stimulate a better understanding of the prevention, evaluation, and treatment of LASs.
Keywords: anatomy, biomechanics, joint injury, lower extremity
Lateral ankle sprains (LASs) are the scourge of sport participation. As the most common lower extremity orthopaedic injury, approximately 23 000 ankle sprains occur daily in the United States.1,2 The LAS is the most frequent injury during athletic participation, affecting an estimated 1.5 to 2.0 million people in the United States each year.2–4 Athletes and other stakeholders also incur substantial costs from these injuries. Lost time from sport participation, school, or work5 and the associated monetary costs6 are markers of resource depletion directly related to LASs. Furthermore, LASs account for up to 1.6 million physician office visits,7 approximately 600 000 emergency department visits,8 and more than 8000 hospitalizations per year.9 Associated annual health care costs in the United States are estimated to be $4.2 billion.7,10 In addition, LASs often progress and become long-term problems, with residual symptoms, early-onset posttraumatic ankle osteoarthritis, and long-term deficits.11–16 These residual effects often lead to decreased physical activity,17 with the resultant increased health care costs and effects on quality of life.
One of the most common long-term consequences of LAS is chronic ankle instability (CAI), affecting 30% to 70% of those who experience a first-time LAS.18,19 The manifestation of CAI is a result of an LAS; the initial LAS is a criterion for diagnosis of CAI.20 Included in the clinical presentation of CAI are pain, the perception of ankle instability, and recurrent episodes of giving way, with these characteristics lasting at least 1 year after the initial injury.21 Various combinations of these key characteristics and other signs and symptoms have been included in models for 3 presentations of CAI (mechanical insufficiency,22 functional instability,22 and perceived instability23) and the updated model of CAI23 that includes individuals who do not have obvious structural or functional deficits but still experience recurrent sprains. Although often viewed as mild injuries, LASs represent an important public health problem.7,15 Based on the high and persistent recurrence rate and frequency of subsequent comorbidities, current care and education concerning LASs are inadequate.24
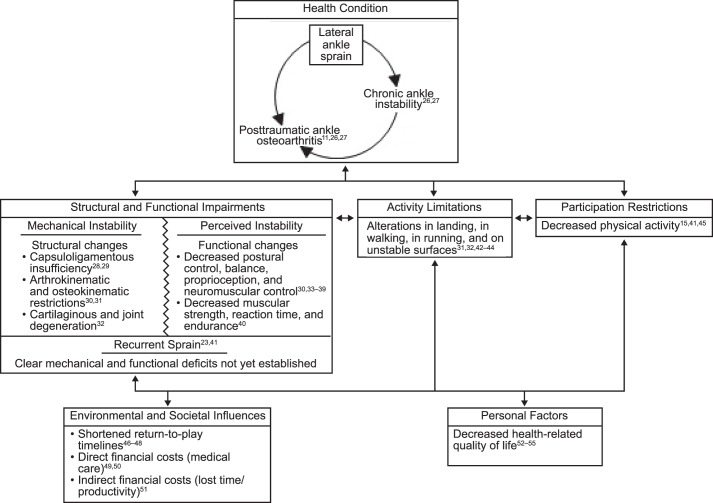
The International Classification of Functioning, Disability, and Health (ICF), adopted by the World Health Organization in 2001, is a model that supports the scientific basis for studying health and health-related conditions.25 This model allows for a comprehensive biopsychosocial approach to understanding how a disease state affects an individual patient while considering that personal and environmental factors provide the contextual influences on the perceptions of health and disability.25 Briefly, within the ICF, domains of deficits are related to (1) body structures and functions (ie, pertaining to anatomic, neurologic, and physiological processes), (2) activities (eg, walking, running, or throwing), and (3) participation in life situations and the ability to perform in the individual's role (eg, an athlete's full participation in the sports of choice). Mitigating factors include personal influences (somatic, cognitive, and psychological factors, such as age, weight, self-efficacy, lifestyle, and personal traits) and environmental influences (sociologic and ecologic factors, such as support network, stakeholders, work environment, and access to health care).
A health condition, such as LAS, can result in a pathologic state for (1) body structures and functions, which is termed an impairment and defined as a specific disruption to anatomic or functional processes; (2) activity, which is termed a limitation and is defined as the inability to execute a task; and (3) participation, which is termed a restriction and is defined as the limited capacity for involvement in life situations. The contextual influences of personal and environmental factors can affect or be affected by impairments, limitations, and restrictions that a patient is experiencing.25 The effects of LAS, including CAI and posttraumatic ankle osteoarthritis, in the context of the ICF domains are presented in Figure 1. Although this is not an exhaustive representation of all the literature on LASs, it is evident that LAS and highly likely that the consequent morbidities of CAI and posttraumatic ankle osteoarthritis can affect all aspects of life and the perceptions of health and disability. Therefore, the purpose of our clinical review was to present the structure, function, and relevant pathologic states of the ankle-joint complex (ankle complex) to promote a better understanding of the prevention, evaluation, and treatment of LASs.
Figure 1.
The effect of lateral ankle sprain in the context of the International Classification of Functioning, Disability, and Health.25
Simply put, the ankle complex is formed by the compound articulations of the talocrural, distal tibiofibular, and subtalar joints. Although the structures and functions of these 3 joints are often described separately, an intricate relationship exists among them, and they cannot be disconnected. Before discussing the relevant anatomy and biomechanics of the ankle complex, we describe its function from the position of the foot on the ground, which is often loosely termed the closed kinetic chain (CKC) position. We will use this term with the understanding that, strictly speaking, it may not be entirely biomechanically accurate in every instance. For our article, this term will help to simplify the descriptions that follow and more accurately describe the position of the foot when the ankle is injured.
BONY ANATOMY
Talocrural Joint
Overall, the bony stability of the talocrural joint is very good. Superiorly, the talocrural joint includes the tibia (medial) and fibula (lateral), and inferiorly, the talus. The tibia and fibula create the ankle mortise, an inverted U-shaped structure that forms the proximal segment of the talocrural joint. The articulating surfaces on the inner surfaces of the medial and lateral malleoli are convex, and the inferior surface of the tibia is concave.
Inferior to the ankle mortise sits the talus, with a wedge-shaped body and the neck and spherical head extending anteriorly at approximately 90° to the tibia. The body of the talus is wider anteriorly than posteriorly and has 1 convex facet superiorly. Two concave facets on the outer walls extend approximately halfway down the sides of the talar body. These 3 facets articulate with those on the tibia and fibula. More surface area of the talus is dedicated to articulation with the tibia than the fibula. However, the fibula extends inferiorly at the lateral side of the talocrural joint compared with the medial malleolus, allowing for increased contact surface area. The reciprocating convex-concave features facilitate tracking and motion of the talocrural joint, and together, these 3 structures provide considerable bony congruity that gives stability to the talocrural joint. Finally, an articular surface covers the head of the talus.
Subtalar Joint
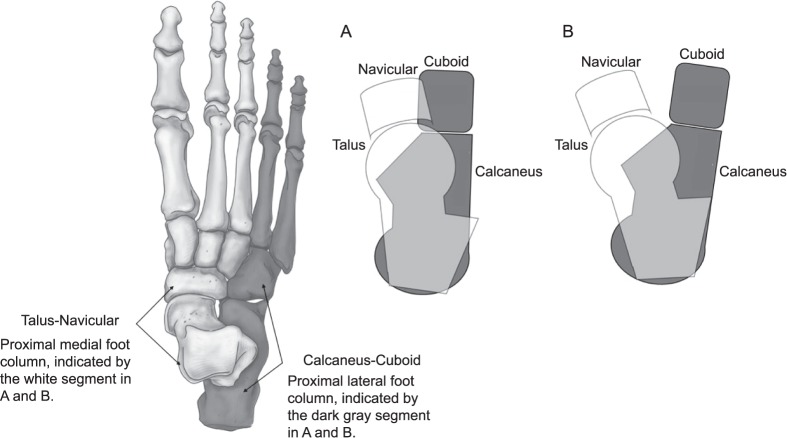
Although often mentioned, the subtalar joint and its relevant structures are less well understood.56–58 Three separate articulations exist between the talus and the calcaneus. The inferior surface of the talus has 3 facets (anterior, middle, and posterior calcaneal facets), whereas the calcaneus has 3 corresponding surfaces (anterior, middle, and posterior talar facets).59 The posterior and middle facets of the talus are on the body, and the anterior facet is on the underside of the talar head. The primary and largest articulation, which is formed by the posterior facets, is concave at the talus and convex at the calcaneus. The remaining 2 are flatter; more gliding than rotation occurs between these surfaces (Figure 2).
Figure 2.
The functional subtalar joint. The functional subtalar-joint complex is divided into the 2 compartments: the posterior compartment (talocalcaneal joint) and the anterior compartment (talocalcaneonavicular joint). Stability is provided by the extrinsic ligaments (the calcaneofibular and deltoid ligaments) and a series of broad, thick intrinsic ligaments situated in the tarsal canal.
Between the articulated middle and posterior facets, a gap that spans the medial to the lateral side of the subtalar joint is called the tarsal canal. As it expands laterally, the space becomes the sinus tarsi. A fourth subtalar articulation exists between the talus and navicular. Although not typically considered part of the true subtalar joint, this articulation has an important role in normal subtalar motion.
Among these 4 articulations, the subtalar joint is divided into 2 compartments (Figure 2).60 The posterior compartment, comprising the talocalcaneal articulations at the posterior facets, is sometimes considered the anatomic or true subtalar joint. The anterior compartment also includes the junctions between the talocalcaneal middle and anterior facets, as well as the articulation of the talus with the navicular (the talocalcaneonavicular joint). Together, the anterior and posterior compartments are considered the functional subtalar joint, as the motions that occur between them cannot be separated during CKC functional tasks.
Other Bony Anatomy of the Foot
Even though they are perhaps less relevant to the direct biomechanics of the ankle complex, the other bony structures of the foot have functional roles during CKC tasks. Distal to the navicular are cuneiforms 1 through 3, which articulate with the first, second, and third metatarsals, respectively. Lateral to the navicular and distal to the calcaneus sits the cuboid, a large tarsal that articulates with the fourth and fifth metatarsals. Fourteen phalanges articulate distally with the metatarsals.
Medial and Lateral Foot Columns
With all of the bony anatomy now described, we can highlight the larger functional division of the foot into 2 columns, which encompass all the bones of the foot (Figure 3). The medial foot column includes the talus, navicular, cuneiforms, and metatarsals and phalanges of the first, second, and third rays. The lateral foot column comprises the calcaneus and the fourth and fifth cuboid rays. A discussion of the roles of the medial and lateral foot columns during normal supination and pronation, as well as with LAS, follows.
Figure 3.
The foot columns and subtalar-joint motion in the closed kinetic chain. These combined frontal-plane and transverse-plane motions occur simultaneously, resulting in a multiplanar rotation. This is different from single-plane, noncardinal motion and is a multiplanar rotary motion that is similar to the motion occurring at the knee. A, Supination. “Stacking” of the medial foot column laterally and vertically over the lateral foot column results in a higher, narrower foot. B, Pronation. “Unstacking” of the medial foot column medially away from the lateral foot column results in a wider, flatter foot.
ANKLE COMPLEX DURING WALKING
A primary functional task of the lower extremity is walking and, as an extension, running. For each of these tasks, a gait pattern is adopted. Gait is an oscillating pattern of force accommodation and generation designed for locomotion.61 Throughout the gait cycle, a cyclical pattern of absorption and propulsion occurs. Absorption decelerates and controls forward progression, and propulsion continues that forward progression. Many musculoskeletal injuries occur because of improper force absorption, such as from poor mechanics, a bad landing, or a stumble on a slippery surface.
During gait, the leg and foot move around 3 primary axes of rotation, termed rockers: the heel rocker, ankle rocker, and forefoot rocker (Figure 4).62,63 In the stance phase of walking gait, initial contact begins with the heel landing on the ground. With the heel on the ground, the foot is lowered to the ground and rotation occurs around the heel. This is the heel rocker.62,63 With the foot flat on the ground, the leg advances anteriorly over the foot, with the axis of rotation occurring at the talocrural joint; this is the ankle rocker.62,63 After leg progression and moving into terminal stance, the heel and midfoot lift off the ground, with rotation occurring around the metatarsophalangeal joints.62,63 This is the forefoot rocker. Next, the toes leave the ground, ending the stance phase for that limb. Tying this to force absorption and propulsion, force absorption occurs during the heel rocker. The ankle rocker is transitional, moving from absorption to propulsion, and the individual's center of gravity advances over the stance foot. Finally, the forefoot rocker is associated with propulsion. When shifting from walking to running, the heel rocker will be eliminated first to minimize absorption and increase propulsion.61 To move into sprinting, the ankle rocker will be diminished to maximize the efficiency of the most propulsive rocker.61
Figure 4.
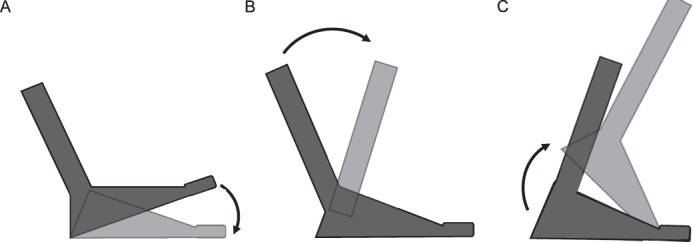
The rockers. The 3 rockers of gait describe the foot and leg rotational motions during the absorption and propulsions stages of the stance phase of gait. A, Heel rocker. The foot is lowered to the ground around the calcaneus (heel). B, Ankle rocker. The leg advances over the foot around the talocrural joint. C, Forefoot rocker. The heel lifts off the ground around the metatarsophalangeal joints.
BIOMECHANICS
Talocrural Joint
At the talocrural joint, the primary osteokinematics are dorsiflexion and plantar flexion, which occur in the approximate cardinal sagittal plane (<10° off axis). In the anatomic position with the foot positioned at 90° to the tibia, the talocrural joint typically has more available plantar flexion than dorsiflexion. Throughout the walking-gait cycle, the talocrural joint moves through 2 phases of alternating dorsiflexion and plantar flexion: 2 plantar-flexion cycles and 1 dorsiflexion cycle occur during the CKC stance phase,61,64 and 1 dorsiflexion cycle occurs during the swing phase of gait.61,64
The first plantar-flexion phase occurs during the heel rocker and allows for force absorption at the beginning of the stance phase.63 This is a controlled deceleration to assist in maintaining a consistent walking speed and allow for accurate foot placement in preparation for full weight acceptance. The second plantar-flexion phase occurs during the forefoot rocker,63 propelling the body forward during the final stage of the stance phase. During this motion, the hindfoot lifts off the ground followed by the forefoot and toes. During the stance phase between the 2 plantar-flexion cycles, the ankle rocker causes stance-phase dorsiflexion.61 This locks the talocrural joint into the closed-packed position65 and allows the leg to become a more rigid beam for efficient energy transfer. The Table provides a summary of the motions of the talocrural and subtalar joints during the gait cycle.
Table.
Motions and Muscular Actions of the Talocrural and Subtalar Joints During Walking
| Gait Phase |
||||||||
| Swing |
Stance |
|||||||
| Talocrural motion | Dorsiflexion | Plantar flexion | Dorsiflexion | Plantar flexion | ||||
| Rocker | Heel | Ankle | Forefoot | |||||
| Muscle group | Concentric anterior compartmenta | Eccentric anterior compartmenta | Eccentric posterior compartmentsb | Concentric posterior compartmentsb,c | ||||
| Action | Active dorsiflexion | Controlled plantar flexion | Controlled dorsiflexion | Active plantar flexion | ||||
| Subtalar motion | ||||||||
| Hindfoot | Supination | Supination | Supination | Pronation | Pronation | Pronation | Pronation | Supination |
| Midfoot and forefoot | Supination | Supination | Supination | Supination | Pronation | Pronation | Pronation | Pronation |
| Foot columns | Stacked | Transition | Unstacked | Transition | ||||
The anterior compartment of the leg includes the tibialis anterior, extensor hallucis longus, and extensor digitorum longus.
The posterior compartments of the leg include the superficial posterior compartment (gastrocnemius, soleus, and plantaris) and the deep posterior compartment (tibialis posterior, flexor hallucis longus, and flexor digitorum longus).
Some controversy exists about whether this is a concentric or isometric contraction.
At the joint surfaces, the talocrural joint is in the closed-packed position during dorsiflexion65 based on the wedge shape of the superior aspect of the talar body, which maximizes contact between the talar dome and the mortise.66 Furthermore, the talus puts stress on the ligamentous structures of the tibia and fibula, increasing compression while the ankle is dorsiflexed. In plantar flexion, the posterior talus, which is the narrower part of the wedge, is in more contact with the mortise, decreasing the bony stability of the talocrural joint (open-packed position), and the inferior tibiofibular ligaments are more slack. In this position, reliance on the ligamentous contributions to stabilize the talocrural joint is increased. The arthrokinematics of the talocrural joint are generally understood, but we will note these in the context of the CKC. With the calcaneus and, therefore, talus fixed to the ground, the concave surface of the ankle mortise rolls and glides anteriorly on the talus during the dorsiflexion motion that occurs throughout the ankle rocker.66 Therefore, for dorsiflexion to occur in the CKC, the tibia must progress anteriorly over the talus and the talus must glide posteriorly within the ankle mortise. Familiarity with the osteokinematics and arthrokinematics at the talocrural joint is important to the subsequent discussion of the pathomechanics of LAS.
Subtalar Joint
The osteokinematics of the subtalar joint are more complex when described in the CKC. It is well established that inversion and eversion occur at the anatomic subtalar joint (the posterior subtalar compartment).67 A clinician can manually reproduce this motion when the patient is in a non–weight-bearing position. However, this cannot be isolated during physiological motion, and the actions at the anterior and posterior compartments must be considered together when the foot is on the ground and the calcaneus is fixed.68
During CKC supination, calcaneal inversion occurs at the anatomic subtalar joint; however, motion at the navicular and cuboid also occurs. In this position, inversion becomes supination, which is a combination of plantar flexion, inversion, adduction, and external rotation69 of the tibia and the medial foot column.68 Eversion becomes pronation, which is a combination of dorsiflexion, eversion, abduction, and internal rotation of the tibia and medial foot column. For supination and pronation, the talus-navicular and calcaneus-cuboid act as joined segments of the medial and lateral columns, respectively (Figure 3). During supination, the talus-navicular elevates (dorsiflexes) and rotates externally (abducts) on the fixed calcaneus-cuboid. External rotation of the talus-navicular is initiated by the tibia, resulting in a higher, narrower foot. In this position, the medial column stacks vertically on the lateral foot column, resulting in a more parallel alignment of the 2 foot columns (Figure 3).
During pronation, the reverse occurs. The talus-navicular lowers (plantar flexes) and rotates medially (adducts) on the fixed calcaneus-cuboid. Internal rotation of the talus-navicular comes from internal rotation of the tibia during this motion. This results in a wider and flatter foot, with the medial and lateral foot columns unstacked and positioned in an off-parallel, intersecting alignment (Figure 3). During supination and pronation, the frontal-plane and transverse-plane motions occur in an approximate 1 : 1 ratio and cannot be separated during CKC tasks. Therefore, the resultant motion of the functional subtalar joint is multiplanar with integrated rotary motion and not single-planar motion in a noncardinal-plane direction. During walking gait, pronation begins during the heel rocker and continues throughout the ankle rocker when the foot reaches its lowest position with respect to the ground. With the transition into propulsion during the forefoot rocker, the foot begins to elevate and stack in a more supinated position, creating a rigid foot for push-off (Table).
The arthrokinematics of the functional subtalar joint during the CKC movement are complex66, which directly results from the joint-surface anatomy of the anterior and posterior compartments. At the anterior compartment, the talus is convex, and the navicular is concave.60,70 At the posterior compartment, the talus is concave at its inferior surface, and the corresponding surface of the calcaneus is convex.60,70 This reciprocating convexity and concavity help produce the rotary motion at the subtalar joint. During CKC supination, the medial roll of the talus (inversion) that occurs with supination is coupled with a medial glide for the posterior compartment but a lateral glide for the anterior compartment. For pronation, this is reversed. The lateral roll (eversion) of the talus at the posterior compartment is coupled with lateral glide and at the anterior compartment is coupled with medial glide. To summarize the biomechanics of the inversion mechanism21,71–77 in the CKC (the position of LAS injury), the pathomechanics actually involve a multiplanar-supination motion and not strict inversion as this mechanism is often described.
STRUCTURES
Tibiofibular Joint
The tibia and the fibula are tightly bound together by an interosseous membrane. Strong anterior and posterior tibiofibular ligaments located superiorly and inferiorly (anterosuperior, posterosuperior, anteroinferior, and posteroinferior tibiofibular ligaments) also stabilize the proximal and distal joints. Normal stability and motion at both joints are important for function of the ankle complex.78,79 Hypomobility of the proximal tibiofibular joint can limit or alter motion at the talocrural joint.80
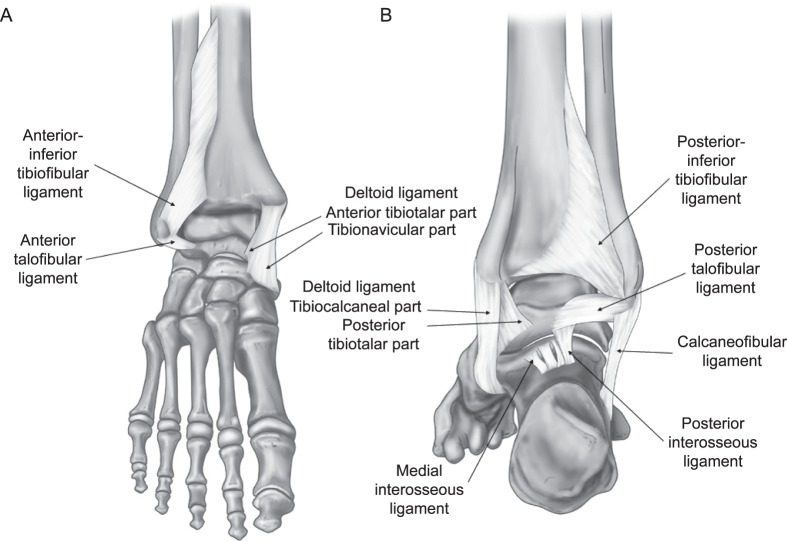
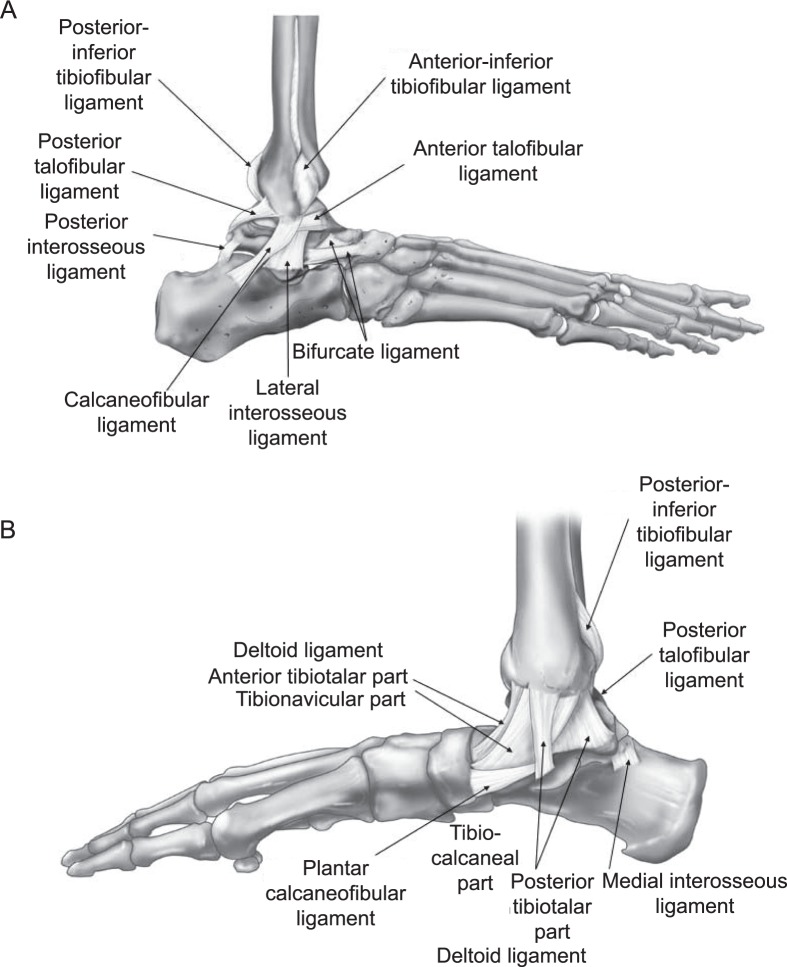
Distally, the anteroinferior and posteroinferior tibiofibular ligaments originate from the fibula and travel medially and superiorly to insert on the tibia. Relative to the ankle mortise, these 2 ligaments are situated at the lateral one-third of the entire width of the tibia and fibula (Figures 5 and 6). At the distal tibiofibular joint, the anteroinferior and posteroinferior tibiofibular ligaments do not directly stabilize the lateral ankle; however, compromise to the distal tibiofibular ligaments can indirectly destabilize the talocrural joint by decreasing compressive forces between the tibia and fibula.
Figure 5.
Ligaments relevant to stability of the ankle complex. A, Anterior view. B, Posterior view.
Figure 6.
Ligaments relevant to stability of the ankle complex. A, Lateral view. B, Medial view.
Talocrural Joint
The ligamentous stabilizers of the talocrural joint are extrinsic, as they are part of, or lie outside of, the joint capsule. Three primary ligaments are specific to the talocrural joint, crossing the joint space between the ankle mortise and the talus. However, other structures provide further static stability (Figures 5 and 6). Probably the most easily recognized are the anterior talofibular ligament (ATFL) and posterior talofibular ligament (PTFL), which provide stability to the lateral joint.81 The ATFL is oriented 90° to the lateral malleolus, traveling anteriorly to insert on the talus. In contrast, the PTFL extends approximately 180° in the opposite direction to insert on the posterior talus. The PTFL extends around the talus to nearly the most medial part on the posterior side. Originating between the ATFL and the PTFL, the calcaneofibular ligament (CFL) extends from the lateral malleolus at approximately 45° inferiorly and posteriorly past the talus to insert on the calcaneus. This ligament is often grouped with the ATFL and PTFL and provides stability to the lateral talocrural joint, but it does not directly stabilize this joint. Although not typically damaged during LAS, portions of the tibial-side deltoid ligament (in particular, the anterior and posterior tibiotalar bands) are direct stabilizers of the talocrural joint.82 The 2 central bands of the deltoid ligament, the tibionavicular ligament and the tibiocalcaneal ligament, provide secondary stability to the talocrural joint.
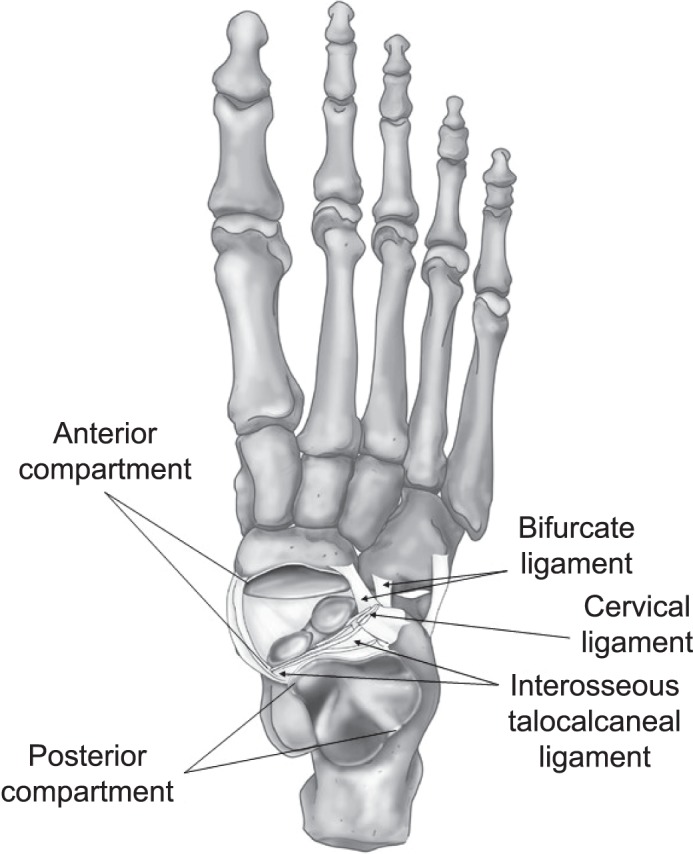
Capsuloligamentous Stability of the Subtalar Joint (Extrinsics and Intrinsics)
The subtalar joint is stabilized by extrinsic and intrinsic ligaments (Figures 2, 5, and 6). The 2 primary extrinsic ligaments are the lateral CFL, which is an important subtalar stabilizer, and the 2 central bands of the deltoid ligament (tibionavicular and tibiocalcaneal ligaments) on the medial side, which provide stability to the subtalar joint.81 As a lateral extrinsic stabilizer of the subtalar joint, the CFL is a stabilizer primarily as the talocrural joint moves into dorsiflexion. It is up to 3.5 times stronger than the ATFL.83 Three smaller extrinsic ligaments are also specific to the subtalar joint: the medial talocalcaneal (posterior aspect of the medial talar tubercle to the posterior aspect of the sustentaculum tali), the posterior talocalcaneal (posterior aspect of the lateral talar tubercle to the superior aspect of the posteromedial calcaneus), and the lateral talocalcaneal (anterior and deep to the CFL with parallel fibers).59 Although these 3 interosseous perimeter ligaments are small, they are a potential source of pain in chronic subtalar instability.
The intrinsic subtalar ligaments include a series of broad, thick ligaments situated in the tarsal canal that separate the anterior and posterior compartments (Figures 2, 5, and 6).59,84 Located centrally in the subtalar joint is the interosseous talocalcaneal ligament (ITCL). This broad, thick ligament extends from the inferior surface of the anterolateral talar neck to the superior surface of the talus. Although the specific direction of stabilization for the ITCL is controversial, it likely has a multiplanar role in stabilization similar to that of the anterior cruciate ligament at the knee. Moving medially from the ITCL and across from the tarsal canal sit the cervical ligament (dorsolateral aspect of the anterior calcaneus to the dorsolateral talus, adjacent to the sinus tarsi) and the bifurcate ligament with its 2 bands (dorsolateral aspect of the anterior calcaneus to the dorsolateral navicular and the dorsomedial cuboid). Fibrous bands also extend from the inferior extensor retinaculum and enter the tarsal canal, merging with these structures to further enhance stability. Although these are separate structures, the close proximity and tight articulation make it difficult to separate these structures even in cadaveric dissection. Collectively, these intrinsic ligaments are called the subtalar-joint complex. An increasing body of evidence supports the role of the ITCL as the primary stabilizer of the functional subtalar-joint complex85–88 and provider of a crucial source of somatosensory information.89–91
MUSCULAR AND NEURAL ANATOMY
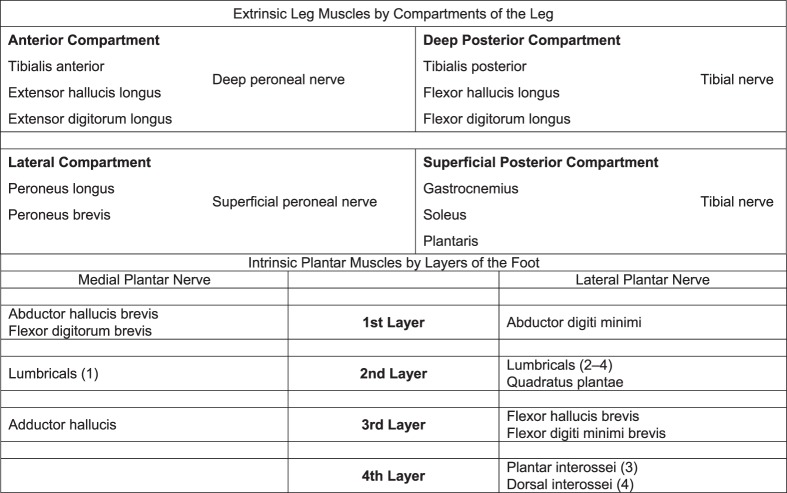
Extrinsic Foot Muscles
The extrinsic foot muscles are the primary movers of the ankle and foot. These muscles, which originate proximal to the talocrural joint, are separated by strong intermuscular septa into 4 compartments: the anterior, lateral, superficial posterior, and deep posterior compartments (Figure 7). The roles of these muscle groups are described in the CKC as they function in the gait cycle. The anterior compartment (tibialis anterior, extensor hallucis longus, extensor digitorum longus) is innervated by the deep peroneal nerve. The primary roles of this compartment are to eccentrically lower the foot to the ground during the heel rocker, which we will describe, and to dorsiflex the talocrural joint to assist with foot clearance during the swing phase of gait (second dorsiflexion arc). The lateral compartment (peroneus longus and peroneus brevis) is innervated by the superficial peroneal nerve and helps to move the ankle and foot into pronation through the ankle rocker. The peroneus longus also helps to drive the first ray into the ground to assist with the transition to propulsion. The superficial posterior compartment (gastrocnemius, soleus, plantaris), innervated by the tibial nerve, acts during the ankle rocker and then the forefoot rocker. These muscles contract eccentrically to slow tibial progression over the ankle and foot and then concentrically to initiate the plantar flexion needed for the final propulsive action during the forefoot rocker. The Table provides a summary of the muscular actions of the extrinsic foot muscles during the gait cycle.
Figure 7.
The relevant neuromuscular structures of the ankle complex.
Intrinsic Plantar Muscles
The intrinsic plantar muscles originate and insert within the foot to provide local stability and active support to the foot arches. These muscles are typically described as separated into 4 layers based on their depth from the plantar surface (Figure 7). Although each intrinsic plantar muscle has a unique action, this muscle group acts collectively to promote dynamic foot stability.92 In weight bearing, coordinated contraction of the intrinsic plantar muscles can be observed through a shortening of the distance between the metatarsal heads and calcaneus and a narrowing of the foot width in the region of the metatarsal heads. The synergistic action of these muscles supports the medial longitudinal and transverse arches of the foot, working with the bones, ligaments, and joint capsules to create a functional half dome at the underside of the foot.92 In addition to the motor action of the intrinsic plantar muscles, these structures provide a neural contribution to foot stability when in a weight-bearing position. Innervation for the intrinsic plantar muscles comes from the medial and lateral plantar nerves, which originate from the tibial nerve and can be initially identified in the tarsal tunnel near the inferior border of the flexor retinaculum. In addition to innervating the intrinsic plantar muscles, the medial and lateral plantar nerves innervate the skin overlying the medial and lateral aspects of the plantar surface of the foot and digits. Collectively, the intrinsic plantar muscles and plantar surface provide valuable somatosensory information regarding the environment, movement, and perturbation.92
LATERAL ANKLE SPRAIN
Mechanisms
The mechanisms of LASs can be characterized as direct contact, indirect contact, or noncontact.83,93 A direct-contact mechanism involves contact, often from another player, to the medial leg just before or during foot placement, resulting in forced inversion.93 An indirect-contact mechanism involves contact from an obstacle or individual that alters the way the foot is brought to the ground during weight acceptance.83,93 For example, this mechanism could include stepping on another player's foot while landing from a jump or into a divot while running on uneven terrain. Noncontact injuries are characterized by landing inappropriately when no other external forces or obstacles are apparent.22,93 Indirect-contact and noncontact mechanisms typically occur during rapid changes of direction (cutting) or when stopping quickly. In sports such as basketball, football, lacrosse, soccer, and volleyball, it is not surprising that LAS is one of the most common injuries.2,4,12,94–96 What takes place while abruptly changing direction in athletic activity needs to be considered.
For most LASs, particularly noncontact injuries, the mechanism includes talocrural plantar flexion, subtalar inversion, and external rotation of the medial foot column. As described, in the transition from walking to running, the heel rocker is nearly eliminated.61 By reducing the absorption that occurs during the heel-rocker plantar-flexion arc of motion, the individual accelerates and shifts into a running gait. When decelerating, the heel rocker is reincorporated to absorb forward momentum, and the individual shifts back to a walking gait. During cutting, the directional momentum must be rapidly reduced (absorption) and then reversed to propel the individual into a new direction (propulsion). With this rapid shift from absorption to propulsion, the body may respond with inappropriate force-attenuating strategies, and a musculoskeletal injury in the form of a noncontact ankle-sprain event can theoretically occur. The heel-rocker plantar-flexion arc is used to absorb the directional momentum and bring the foot to the ground.61 When this plantar-flexion arc is combined with the laterally directed force of a cutting maneuver, an LAS can result. However, LAS mechanisms may vary based on sport. For example, in their recent study of LAS mechanisms in men's and women's volleyball, Skazalski et al97 determined that rapid inversion without plantar flexion due to contact with another player was the primary mechanism for most injuries. Although a plantar-flexed position is often involved in LASs, other positions can also stress the lateral joint structures.
Pathomechanics
Talocrural Joint
A concrete understanding of LAS pathomechanics is crucial. Most clinicians are familiar with the standard descriptions of injury mechanisms related to LAS. However, a clear understanding of how these injuries occur during sport participation is important for improving evaluation. Athletes tend to describe how they were hurt while participating. In other words, careful consideration should be given to how the injury occurred with the foot on the ground, the associated osteokinematics and arthrokinematics, and the resulting force transmission through the ankle complex.
Lateral ankle sprains most commonly occur after initial foot contact during functional activities, such as running, cutting, or landing from a jump.22,83,98 The injury mechanism has been theorized to take place in as little as 40 milliseconds and move through an arc of motion greater than 700°/s.69 Given the explosive nature of an LAS, insufficient time is available to develop the muscle force capable of controlling this excessive supination. Of note, no muscles directly insert onto the talus. Therefore, motion at the talus is restricted directly by ligaments and the bony congruency between the talus and mortise.
As discussed, during CKC plantar flexion, the talus is positioned anteriorly in the ankle mortise. The primary restraint for excessive anterior talar glide is the ATFL. Based on its anatomic orientation and size, it is considered the weakest of the 3 lateral ligaments, which contributes to the high injury rate of the ATFL.22,81,83,98 The PTFL is rarely injured during an LAS; however, a direct relationship appears to exist between the magnitude of force applied during an ankle sprain and the number of ligaments damaged.83,98 A larger force results in more lateral extrinsic ligaments being damaged, with the damage occurring in a pattern that moves from anterior to posterior. Therefore, damage to the PTFL is most often accompanied by a fracture or dislocation (ie, with very high-force events). From the perspective of the rockers, indirect and noncontact LASs occur from incorrect foot placement during the heel rocker or poor transition into propulsion during the forefoot rocker. The AFTL is injured, and further damage occurs to the more posterolateral extrinsic ligaments as the body transitions through the ankle rocker during tibial progression over an inappropriately placed foot.
Alternatively, a reverse forefoot rocker can occur. In the reverse forefoot rocker, the toes are in contact with the ground first, as when landing from a jump. The midfoot and hindfoot rock down to the ground around the metatarsophalangeal joints, and the heel is brought into contact with the ground. Given that this is an absorption motion, injury can occur. Therefore, regardless of the heel or reverse forefoot rocker, the typical transition toward absorption of body weight as the individual approaches the ankle rocker is altered, and force absorption may be transferred to the ligaments. For both indirect and noncontact mechanisms, incorrect foot placement and force absorption prohibit the foot from moving into eversion during foot contact with the ground, whether on the heel (heel rocker) or with forefoot landing (ie, reverse forefoot rocker).
Subtalar Joint
As discussed, CKC inversion is actually supination; the classic inversion ankle pathomechanics are also a supination mechanism.21,71–77 With inversion on the fixed calcaneus, concurrent forefoot adduction and external rotation of the medial foot column occur. During excessive CKC supination, the ATFL, and possibly the CFL, can be injured. The CFL is damaged approximately 25% of the time in combination with the ATFL but is almost never damaged in isolation.83 However, this same mechanism can damage the subtalar intrinsic ligaments. The ITCL and potentially the other subtalar intrinsic ligaments are damaged in an estimated 25% to 80% of all LASs, especially when the CFL is involved.99 With excessive inversion force, the subtalar ligaments are disrupted in a logical order, beginning with the CFL. When the CFL is disrupted, the lateral talocalcaneal ligament, cervical ligament, bifurcate ligament, and ITCL ligaments may be damaged.100 Therefore, if damage to the CFL is suspected, further damage to the subtalar ligaments often follows and must be evaluated systematically. Concurrent injury to the lateral extrinsic and subtalar intrinsic ligaments results in anterolateral instability of the subtalar joint.87,101 This is particularly problematic during the stance phase of gait, resulting in persistent pain, bouts of giving way, and a general feeling of instability during functional tasks and activities of daily living.102,103
Talocrural and Subtalar Arthrokinematic and Osteokinematic Impairments
After LAS, a decrease in dorsiflexion range of motion (ROM) is common.104,105 In many patients with LASs, dorsiflexion ROM improves in 4 to 6 weeks with the standard of care.104 However, residual dorsiflexion ROM impairments can persist and are frequent in individuals with CAI. Approximately 30% to 74% of individuals with unilateral CAI exhibit at least a 5° deficit in the involved limb,106,107 which may be due to restrictions in posterior talar glide. Restricted posterior talar glide has been documented using the posterior talar glide test in collegiate athletes with a history of LAS108 and has been identified as a clinical indicator of CAI at 12-month follow-up.109
Another positional fault at the ankle is an anterior shift in talar positioning relative to the ankle mortise. This shift may create anterior impingement and alter the ability of the tibia to progress normally over the talus when attempting to dorsiflex in the CKC. As with decreased posterior glide, anterior positional shift of the talus has been identified in individuals with CAI.110 These limitations in dorsiflexion ROM have been correlated with impaired dynamic balance,111 lateral step-down test performance,112 and landing biomechanics31 among individuals with CAI. Therefore, arthrokinematic and osteokinematic deficiencies are important considerations in the evaluation and rehabilitation strategy after LAS.
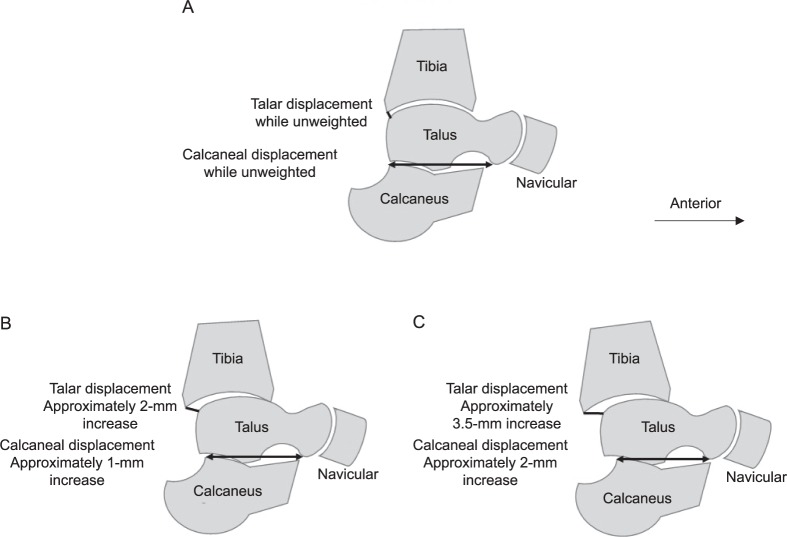
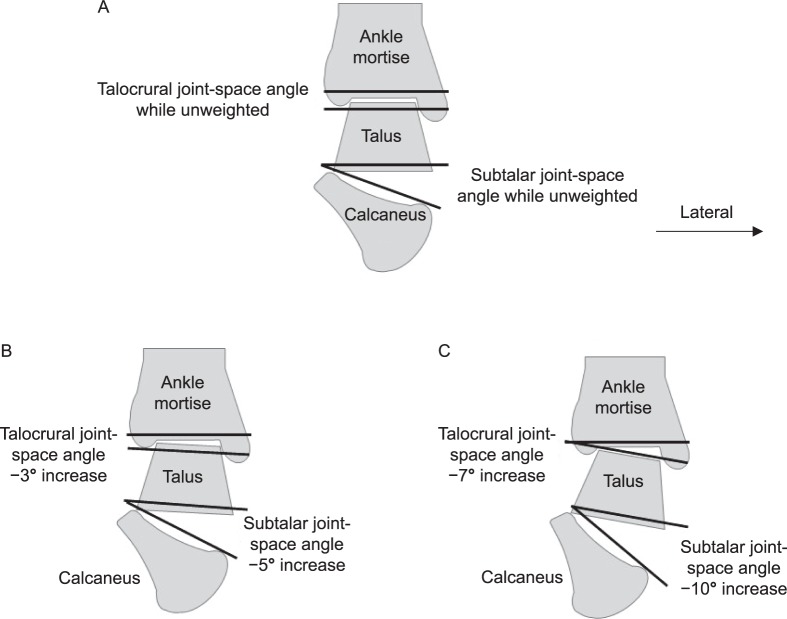
Finally, increased instability is common after LAS. Whether this instability is acute or chronic, increased displacement can occur at the talocrural joint or the subtalar joint, or both. Inversion stress to the ankle complex tends to be more definitive for instability of the subtalar joint, whereas the anterior drawer test better targets the talocrural joint.113 Figures 8 and 9 depict the increased opening up of the talocrural and subtalar joints under anterior drawer and inversion stresses, respectively.
Figure 8.
Sagittal-plane (medial) view of the talocrural and subtalar joints. A, Unweighted ankle. B, Displacement under stress of the stable ankle. C, Displacement under stress of the unstable ankle. Unstable ankles can have an average of 2 times the displacement of the talus on the mortise and the calcaneus on the talus. The anterior drawer stress test tends to be more specific to increased motion at the talocrural joint than the subtalar joint.113
Figure 9.
Frontal-plane (posterior) view of the talocrural and subtalar joints. A, Unweighted ankle. B, Joint displacement under the stress of the stable ankle. C, Joint displacement under the stress of the unstable ankle. Unstable ankles can have an average of twice the displacement of the talus on the mortise and the calcaneus on the talus. An inversion stress test tends to be more specific to increased motion at the subtalar joint than the talocrural joint.113
Intrinsic Plantar Muscle Function, LAS, and CAI and LAS
Intrinsic plantar-muscle function has not been thoroughly investigated regarding the cause or pathomechanics of LAS. However, individuals with CAI exhibit several impairments in foot function that may contribute to a vulnerable base of support. For instance, Feger et al114 reported that people with CAI had decreased total volume of the intrinsic plantar and extrinsic foot muscles based on magnetic resonance imaging measurements. The atrophy of these muscles in the active subsystem may affect local stability and global mobility of the foot. Individuals with CAI have also demonstrated decreased sensory perception over the plantar aspect of the foot, namely at the heel, first metatarsal head, and fifth metatarsal base.115–117 These neural deficits associated with the tibial distribution may impede perturbation detection and delay motor coordination to avoid injury. Finally, patients with CAI who have displayed a pronated static foot posture have also displayed decreased dynamic balance.118 Cumulatively, structure and function of the foot, including the intrinsic plantar muscles, may have a role in LAS and associated sequelae. Based on the retrospective nature of the research to this point, it is difficult to determine whether intrinsic plantar-muscle function contributes to the index LAS or at what point in the recurrent injury cycle foot function may begin to decline.
CLINICAL CONSIDERATIONS AND SUMMARY
Lateral ankle sprains are common, and a clear understanding of the relevant structures and clinical function of the ankle complex needs to extend beyond the talocrural joint. We believe several considerations should be included in the clinical evaluation and rehabilitation process centered on the structure and function of the ankle complex.
The foot- and ankle-rocker system provides a systematic evaluation strategy for understanding injury mechanisms and postinjury impairments based on the fundamental functional demands of the joints and muscles throughout the ankle complex.
In addition to having a thorough understanding of the ligamentous structures that are typically involved at the talocrural joint after LAS, clinicians should be competent in describing the anatomy associated with the subtalar joint. Damage to these structures may be implicated in a large proportion of LASs but be undetected during clinical examination. Refining the evaluation techniques for the subtalar-joint stabilizers may assist with identifying additional sources of residual instability and impairment after LAS. Accurate evaluation and treatment selection rely on correctly identifying all involved structures and biomechanical deficits.
With LAS, particularly in recurrent cases, arthrokinematic changes may occur in the talocrural joint. This has implications for the performance of several functional tasks. Therefore, a thorough understanding of normal talocrural arthrokinematics is needed to identify possible restrictions after injury.
Finally, fully understanding the structure and function of the extrinsic and intrinsic muscles that support the ankle and foot is important. Although certain muscles, such as the peroneals, have a logical connection to LAS, others, such as the tibialis posterior and the intrinsic plantar muscles, play a large role in dynamic foot stability. These structures and functions likely have ramifications for the ankle complex.
From an anatomic perspective, LASs are much more complex than simple damage to the ATFL. A complete working knowledge of the anatomy, biomechanics, and pathomechanics of both the talocrural joint and subtalar joint is necessary. Consideration for the many structures that may be directly or indirectly involved in LAS will likely translate into advances in clinical care.
ACKNOWLEDGMENTS
We thank Tom Dolan, MS, medical illustrator at the University of Kentucky, for his detailed anatomical images (Figures 2, 3, 5, and 6).
REFERENCES
- 1.Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle: operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73(2):305–312. [PubMed] [Google Scholar]
- 2.Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641–645. doi: 10.1197/j.aem.2007.03.1354. [DOI] [PubMed] [Google Scholar]
- 3.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 4.Swenson DM, Collins CL, Fields SK, Comstock RD. Epidemiology of U.S. high school sports-related ligamentous ankle injuries, 2005/06–2010/11. Clin J Sport Med. 2013;23(3):190–196. doi: 10.1097/JSM.0b013e31827d21fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Bie RA, de Vet HC, van den Wildenberg FA, Lenssen T, Knipschild PG. The prognosis of ankle sprains. Int J Sports Med. 1997;18(4):285–289. doi: 10.1055/s-2007-972635. [DOI] [PubMed] [Google Scholar]
- 6.Shah S, Thomas AC, Noone JM, Blanchette CM, Wikstrom EA. Incidence and cost of ankle sprains in United States emergency departments. Sports Health. 2016;8(6):547–552. doi: 10.1177/1941738116659639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984;183:160–168. [PubMed] [Google Scholar]
- 8.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 9.Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 10.Curtis CK, Laudner KG, McLoda TA, McCaw ST. The role of shoe design in ankle sprain rates among collegiate basketball players. J Athl Train. 2008;43(3):230–233. doi: 10.4085/1062-6050-43.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 12.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 13.Swenson DM, Yard EE, Fields SK, Comstock RD. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009;37(8):1586–1593. doi: 10.1177/0363546509332500. [DOI] [PubMed] [Google Scholar]
- 14.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am Med J. 2008;121(4):324–331. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Verhagen RA, de Keizer G, van Dijk CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114(2):92–96. doi: 10.1007/BF00422833. [DOI] [PubMed] [Google Scholar]
- 16.Hiller CE, Nightingale EJ, Raymond J, et al. Prevalence and impact of chronic musculoskeletal ankle disorders in the community. Arch Phys Med Rehabil. 2012;93(10):1801–1807. doi: 10.1016/j.apmr.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 17.Bahr R, Lian O, Bahr IA. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7(3):172–177. doi: 10.1111/j.1600-0838.1997.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 18.Peters JW, Trevino SG, Renstrom PA. Chronic lateral ankle instability. Foot Ankle. 1991;12(3):182–191. doi: 10.1177/107110079101200310. [DOI] [PubMed] [Google Scholar]
- 19.Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14(6):465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- 20.Gribble PA, Delahunt E, Bleakley CM, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Athl Train. 2014;49(1):121–127. doi: 10.4085/1062-6050-49.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 22.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 23.Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. J Athl Train. 2011;46(2):133–141. doi: 10.4085/1062-6050-46.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKeon PO, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med. 2008;27(3):371–382. doi: 10.1016/j.csm.2008.02.004. viii. [DOI] [PubMed] [Google Scholar]
- 25.How to use the ICF: a practical manual for using the International Classification of Functioning, Disability, and Health (ICF). Exposure draft for comment. World Health Organization Web site. 2018 http://www.who.int/classifications/drafticfpracticalmanual2.pdf Accessed November 10.
- 26.Golditz T, Steib S, Pfeifer K, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthritis Cartilage. 2014;22(10):1377–1385. doi: 10.1016/j.joca.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 27.Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–1806. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6(3):180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- 29.Brown CN, Rosen AB, Ko J. Ankle ligament laxity and stiffness in chronic ankle instability. Foot Ankle Int. 2015;36(5):565–572. doi: 10.1177/1071100714561057. [DOI] [PubMed] [Google Scholar]
- 30.Hoch MC, Staton GS, Medina McKeon JM, Mattacola CG, McKeon PO. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15(6):574–579. doi: 10.1016/j.jsams.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Hoch MC, Farwell KE, Gaven SL, Weinhandl JT. Weight-bearing dorsiflexion range of motion and landing biomechanics in individuals with chronic ankle instability. J Athl Train. 2015;50(8):833–839. doi: 10.4085/1062-6050-50.5.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011;45(8):660–672. doi: 10.1136/bjsm.2010.077404. [DOI] [PubMed] [Google Scholar]
- 33.Wikstrom EA, Naik S, Lodha N, Cauraugh JH. Balance capabilities after lateral ankle trauma and intervention: a meta-analysis. Med Sci Sports Exerc. 2009;41(6):1287–1295. doi: 10.1249/MSS.0b013e318196cbc6. [DOI] [PubMed] [Google Scholar]
- 34.Arnold BL, De La Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41(5):1048–1062. doi: 10.1249/MSS.0b013e318192d044. [DOI] [PubMed] [Google Scholar]
- 35.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing. J Athl Train. 2008;43(4):293–304. doi: 10.4085/1062-6050-43.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13(1):2–12. doi: 10.1016/j.jsams.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 37.Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bagherian S, Rahnama N, Wikstrom EA, Clark MA, Rostami F. Characterizing lower extremity movement scores before and after fatigue in collegiate athletes with chronic ankle instability. Int J Athl Ther Train. 2018;23(1):27–32. [Google Scholar]
- 39.Medina McKeon JM, McKeon PO. Evaluation of joint position recognition measurement variables associated with chronic ankle instability: a meta-analysis. J Athl Train. 2012;47(4):444–456. doi: 10.4085/1062-6050-47.4.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoch MC, McKeon PO. Peroneal reaction time after ankle sprain: a systematic review and meta-analysis. Med Sci Sports Exerc. 2014;46(3):546–556. doi: 10.1249/MSS.0b013e3182a6a93b. [DOI] [PubMed] [Google Scholar]
- 41.Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 42.Caffrey E, Docherty CL, Schrader J, Klossner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39(11):799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- 43.Fransz DP, Huurnink A, Kingma I, Verhagen EA, van Dieën JH. A systematic review and meta-analysis of dynamic tests and related force plate parameters used to evaluate neuromusculoskeletal function in foot and ankle pathology. Clin Biomech (Bristol, Avon) 2013;28(6):591–601. doi: 10.1016/j.clinbiomech.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 44.Moisan G, Descarreaux M, Cantin V. Effects of chronic ankle instability on kinetics, kinematics and muscle activity during walking and running: a systematic review. Gait Posture. 2017;52:381–399. doi: 10.1016/j.gaitpost.2016.11.037. [DOI] [PubMed] [Google Scholar]
- 45.Hubbard-Turner T, Wikstrom EA, Guderian S, Turner MJ. An acute lateral ankle sprain significantly decreases physical activity across the lifespan. J Sports Sci Med. 2015;14(3):556–561. [PMC free article] [PubMed] [Google Scholar]
- 46.Reed A, Medina McKeon JM, Uhl T, Bush HM. Estimated survival probabilities for return to play outcomes for ankle sprains, knee sprains, and concussions in high school athletes [abstract] J Athl Train. 2009;44(suppl 3):S-25–S-53. [Google Scholar]
- 47.Medina McKeon JM, Bush HM, Reed A, Whittington A, Uhl TL, McKeon PO. Return-to-play probabilities following new versus recurrent ankle sprains in high school athletes. J Sci Med Sport. 2014;17(1):23–28. doi: 10.1016/j.jsams.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 48.Clanton TO, Matheny LM, Jarvis HC, Jeronimus AB. Return to play in athletes following ankle injuries. Sports Health. 2012;4(6):471–474. doi: 10.1177/1941738112463347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Verhagen EA, van Tulder M, van der Beek AJ, Bouter LM, van Mechelen W. An economic evaluation of a proprioceptive balance board training programme for the prevention of ankle sprains in volleyball. Br J Sports Med. 2005;39(2):111–115. doi: 10.1136/bjsm.2003.011031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hupperets MD, Verhagen EA, Heymans MW, Bosmans JE, van Tulder MW, van Mechelen W. Potential savings of a program to prevent ankle sprain recurrence: economic evaluation of a randomized controlled trial. Am J Sports Med. 2010;38(11):2194–2200. doi: 10.1177/0363546510373470. [DOI] [PubMed] [Google Scholar]
- 51.Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev. 2007;13(6):416–421. doi: 10.1136/ip.2006.014720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Houston MN, Hoch JM, Hoch MC. Patient-reported outcome measures in individuals with chronic ankle instability: a systematic review. J Athl Train. 2015;50(10):1019–1033. doi: 10.4085/1062-6050-50.9.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–763. doi: 10.4085/1062-6050-49.3.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simon JE, Docherty CL. Current health-related quality of life is lower in former Division I collegiate athletes than in non-collegiate athletes. Am J Sports Med. 2014;42(2):423–429. doi: 10.1177/0363546513510393. [DOI] [PubMed] [Google Scholar]
- 55.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jastifer JR, Gustafson PA. The subtalar joint: biomechanics and functional representations in the literature. Foot (Edinb) 2014;24(4):203–209. doi: 10.1016/j.foot.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 57.Maceira E, Monteagudo M. Subtalar anatomy and mechanics. Foot Ankle Clin. 2015;20(2):195–221. doi: 10.1016/j.fcl.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 58.Piazza SJ. Mechanics of the subtalar joint and its function during walking. Foot Ankle Clin. 2005;10(3):425–442. doi: 10.1016/j.fcl.2005.04.001. v. [DOI] [PubMed] [Google Scholar]
- 59.Schuenke M, Schulte E, Schumacher U, et al. General Anatomy and Musculoskeletal System: Latin Nomenclature Vol 1. New York, NY: Thieme Medical Publishers; 2006. 374–377, 402–419, 452–461. [Google Scholar]
- 60.Sarrafian SK. Biomechanics of the subtalar joint complex. Clin Orthop Relat Res. 1993;290:17–26. [PubMed] [Google Scholar]
- 61.Perry J, Burnfield J. Gait Analysis: Normal and Pathological Function 2nd ed. Vol. 23. Thorofare, NJ: SLACK Inc; 2010. pp. 33–38. [Google Scholar]
- 62.Norkus SA, Floyd RT. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36(1):68–73. [PMC free article] [PubMed] [Google Scholar]
- 63.Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma. 2016;30(3):232–238. doi: 10.1016/j.mporth.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saunders JB, Inman VT, Eberhart HD. The major determinants in normal and pathological gait. J Bone Joint Surg Am. 1953;35(3):543–558. [PubMed] [Google Scholar]
- 65.Smith RW, Reischl S. The influence of dorsiflexion in the treatment of severe ankle sprains: an anatomical study. Foot Ankle. 1988;9(1):28–33. doi: 10.1177/107110078800900106. [DOI] [PubMed] [Google Scholar]
- 66.Loudon JK, Bell SL. The foot and ankle: an overview of arthrokinematics and selected joint techniques. J Athl Train. 1996;31(2):173–178. [PMC free article] [PubMed] [Google Scholar]
- 67.Krähenbühl N, Horn-Lang T, Hintermann B, Knupp M. The subtalar joint: a complex mechanism. EFORT Open Rev. 2017;2(7):309–316. doi: 10.1302/2058-5241.2.160050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Usuelli FG, Mason L, Grassi M, Maccario C, Ballal M, Molloy A. Lateral ankle and hindfoot instability: a new clinical based classification. Foot Ankle Surg. 2014;20(4):231–236. doi: 10.1016/j.fas.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 69.Fong DT, Ha SC, Mok KM, Chan CW, Chan KM. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: five cases from televised tennis competitions. Am J Sports Med. 2012;40(11):2627–2632. doi: 10.1177/0363546512458259. [DOI] [PubMed] [Google Scholar]
- 70.Barg A, Tochigi Y, Amendola A, Phisitkul P, Hintermann B, Saltzman CL. Subtalar instability: diagnosis and treatment. Foot Ankle Int. 2012;33(2):151–160. doi: 10.3113/FAI.2012.0151. [DOI] [PubMed] [Google Scholar]
- 71.Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33(10):1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 72.Dubin JC, Comeau D, McClelland RI, Dubin RA, Lateral Ferrel E. and syndesmotic ankle sprain injuries: a narrative literature review. J Chiropr Med. 2011;10(3):204–219. doi: 10.1016/j.jcm.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15(3):267–270. doi: 10.1249/00005768-198315030-00014. [DOI] [PubMed] [Google Scholar]
- 74.Osbahr DC, Drakos MC, O'Loughlin PF, et al. Syndesmosis and lateral ankle sprains in the National Football League. Orthopedics. 2013;36(11):e1378–e1384. doi: 10.3928/01477447-20131021-18. [DOI] [PubMed] [Google Scholar]
- 75.Andersen TE, Floerenes TW, Arnason A, Bahr R. Video analysis of the mechanisms for ankle injuries in football. Am J Sports Med. 2004;32(suppl 1):69S–79S. doi: 10.1177/0363546503262023. [DOI] [PubMed] [Google Scholar]
- 76.Giza E, Fuller C, Junge A, Dvorak J. Mechanisms of foot and ankle injuries in soccer. Am J Sports Med. 2003;31(4):550–554. doi: 10.1177/03635465030310041201. [DOI] [PubMed] [Google Scholar]
- 77.Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 78.Rasmussen O, Tovborg-Jensen I, Boe S. Distal tibiofibular ligaments: analysis of function. Acta Orthop Scand. 1982;53(4):681–686. doi: 10.3109/17453678208992276. [DOI] [PubMed] [Google Scholar]
- 79.Norkin CC, Levangie PK. Joint Structure and Function: A Comprehensive Analysis. Philadelphia, PA: FA Davis; 1983. pp. 380–383. [Google Scholar]
- 80.Bozkurt M, Yavuzer G, Tönük E, Kentel B. Dynamic function of the fibula. Gait analysis evaluation of three different parts of the shank after fibulectomy: proximal, middle and distal. Arch Orthop Trauma Surg. 2005;125(10):713–720. doi: 10.1007/s00402-005-0054-9. [DOI] [PubMed] [Google Scholar]
- 81.Bozkurt M, Doral MN. Anatomic factors and biomechanics in ankle instability. Foot Ankle Clin. 2006;11(3):451–463. doi: 10.1016/j.fcl.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 82.Rasmussen O, Kromann-Andersen C, Boe S. Deltoid ligament: functional analysis of the medial collateral ligamentous apparatus of the ankle joint. Acta Orthop Scand. 1983;54(1):36–44. doi: 10.3109/17453678308992867. [DOI] [PubMed] [Google Scholar]
- 83.Fong DT, Chan YY, Mok KM, Yung P, Chan KM. Understanding acute ankle ligamentous sprain injury in sports. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:14. doi: 10.1186/1758-2555-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mittlmeier T, Wichelhaus A. Subtalar joint instability. Eur J Trauma Emerg Surg. 2015;41(6):623–629. doi: 10.1007/s00068-015-0588-7. [DOI] [PubMed] [Google Scholar]
- 85.Choisne J, Ringleb SI, Samaan MA, Bawab SY, Naik D, Anderson CD. Influence of kinematic analysis methods on detecting ankle and subtalar joint instability. J Biomech. 2012;45(1):46–52. doi: 10.1016/j.jbiomech.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 86.Tochigi Y, Amendola A, Rudert MJ, et al. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004;25(8):588–596. doi: 10.1177/107110070402500813. [DOI] [PubMed] [Google Scholar]
- 87.Tochigi Y, Takahashi K, Yamagata M, Tamaki T. Influence of the interosseous talocalcaneal ligament injury on stability of the ankle-subtalar joint complex: a cadaveric experimental study. Foot Ankle Int. 2000;21(6):486–491. doi: 10.1177/107110070002100607. [DOI] [PubMed] [Google Scholar]
- 88.Ringleb SI, Dhakal A, Anderson CD, Bawab S, Paranjape R. Effects of lateral ligament sectioning on the stability of the ankle and subtalar joint. J Orthop Res. 2011;29(10):1459–1464. doi: 10.1002/jor.21407. [DOI] [PubMed] [Google Scholar]
- 89.Larsen E. Tendon transfer for lateral ankle and subtalar joint instability. Acta Orthop Scand. 1988;59(2):168–172. [PubMed] [Google Scholar]
- 90.Pisani G, Pisani PC, Parino E. Sinus tarsi syndrome and subtalar joint instability. Clin Podiatr Med Surg. 2005;22(1):63–77. doi: 10.1016/j.cpm.2004.08.005. vii. [DOI] [PubMed] [Google Scholar]
- 91.Weindel S, Schmidt R, Rammelt S, Claes L, van Campe A, Rein S. Subtalar instability: a biomechanical cadaver study. Arch Orthop Trauma Surg. 2010;130(3):313–319. doi: 10.1007/s00402-008-0743-2. [DOI] [PubMed] [Google Scholar]
- 92.McKeon PO, Hertel J, Bramble D, Davis I. The foot core system: a new paradigm for understanding intrinsic foot muscle function. Br J Sports Med. 2015;49(5):290. doi: 10.1136/bjsports-2013-092690. [DOI] [PubMed] [Google Scholar]
- 93.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 94.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 95.NCAA. 1981–82 – 2010–11 NCAA Sports Sponsorship and Participation Rates Report. Indianapolis, IN: National Collegiate Athletic Association; 2011. [Google Scholar]
- 96.Medina McKeon JM, Pommering TL. How does the incidence of lateral ankle sprains differ across sports and physical activities? In: McKeon PO, Wikstrom EA, editors. Quick Questions in Ankle Sprains. Thorofare, NJ: SLACK Inc; 2015. pp. 7–14. [Google Scholar]
- 97.Skazalski C, Kruczynski J, Bahr MA, Bere T, Whiteley R, Bahr R. Landing-related ankle injuries do not occur in plantarflexion as once thought: a systematic video analysis of ankle injuries in world-class volleyball. Br J Sports Med. 2018;52(2):74–82. doi: 10.1136/bjsports-2016-097155. [DOI] [PubMed] [Google Scholar]
- 98.Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69(1):17–26. [PubMed] [Google Scholar]
- 99.Meyer JM, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain: a roentgenographic study. Clin Orthop Relat Res. 1988;226:169–173. [PubMed] [Google Scholar]
- 100.Choisne J, Hoch MC, Bawab S, Alexander I, Ringleb SI. The effects of a semi-rigid ankle brace on a simulated isolated subtalar joint instability. J Orthop Res. 2013;31(12):1869–1875. doi: 10.1002/jor.22468. [DOI] [PubMed] [Google Scholar]
- 101.Wilkerson GB, Doty JF, Gurchiek LR, Hollis JM. Analysis of rotary ankle instability and taping restraint in a cadaver specimen. Athl Ther Today. 2010;15(4):9–12. [Google Scholar]
- 102.Keefe DT, Haddad SL. Subtalar instability: etiology, diagnosis, and management. Foot Ankle Clin. 2002;7(3):577–609. doi: 10.1016/s1083-7515(02)00047-5. [DOI] [PubMed] [Google Scholar]
- 103.Aynardi M, Pedowitz DI, Raikin SM. Subtalar instability. Foot Ankle Clin. 2015;20(2):243–252. doi: 10.1016/j.fcl.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 104.Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81(4):984–994. [PubMed] [Google Scholar]
- 105.Youdas JW, McLean TJ, Krause DA, Hollman JH. Changes in active ankle dorsiflexion range of motion after acute inversion ankle sprain. J Sport Rehabil. 2009;18(3):358–374. doi: 10.1123/jsr.18.3.358. [DOI] [PubMed] [Google Scholar]
- 106.Beazell JR, Grindstaff TL, Sauer LD, Magrum EM, Ingersoll CD, Hertel J. Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2012;42(2):125–134. doi: 10.2519/jospt.2012.3729. [DOI] [PubMed] [Google Scholar]
- 107.Wheeler TJ, Basnett CR, Hanish MJ, et al. Fibular taping does not influence ankle dorsiflexion range of motion or balance measures in individuals with chronic ankle instability. J Sci Med Sport. 2013;16(6):488–492. doi: 10.1016/j.jsams.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 108.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166–173. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- 109.Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Predicting chronic ankle instability following a first-time lateral ankle sprain using clinical assessment: a prospective cohort analysis. Br J Sports Med. 2017;51(suppl 1):A5–A6. [Google Scholar]
- 110.Wikstrom EA, Hubbard TJ. Talar positional fault in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010;91(8):1267–1271. doi: 10.1016/j.apmr.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 111.Hoch MC, Staton GS, McKeon PO. Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport. 2011;14(1):90–92. doi: 10.1016/j.jsams.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 112.Grindstaff TL, Dolan N, Morton SK. Ankle dorsiflexion range of motion influences Lateral Step Down Test scores in individuals with chronic ankle instability. Phys Ther Sport. 2017;23:75–81. doi: 10.1016/j.ptsp.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 113.Seebauer CJ, Bail HJ, Rump JC, Hamm B, Walter T, Teichgräber UK. Ankle laxity: stress investigation under MRI control. AJR Am J Roentgenol. 2013;201(3):496–504. doi: 10.2214/AJR.12.8553. [DOI] [PubMed] [Google Scholar]
- 114.Feger MA, Snell S, Handsfield GG, et al. Diminished foot and ankle muscle volumes in young adults with chronic ankle instability. Orthop J Sports Med. 2016;4(6):2325967116653719. doi: 10.1177/2325967116653719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Burcal CJ, Wikstrom EA. Plantar cutaneous sensitivity with and without cognitive loading in people with chronic ankle instability, copers, and uninjured controls. J Orthop Sports Phys Ther. 2016;46(4):270–276. doi: 10.2519/jospt.2016.6351. [DOI] [PubMed] [Google Scholar]
- 116.Hoch MC, McKeon PO, Andreatta RD. Plantar vibrotactile detection deficits in adults with chronic ankle instability. Med Sci Sports Exerc. 2012;44(4):666–672. doi: 10.1249/MSS.0b013e3182390212. [DOI] [PubMed] [Google Scholar]
- 117.Powell MR, Powden CJ, Houston MN, Hoch MC. Plantar cutaneous sensitivity and balance in individuals with and without chronic ankle instability. Clin J Sport Med. 2014;24(6):490–496. doi: 10.1097/JSM.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 118.Hogan KK, Powden CJ, Hoch MC. The influence of foot posture on dorsiflexion range of motion and postural control in those with chronic ankle instability. Clin Biomech (Bristol, Avon. 2016;38:63–67. doi: 10.1016/j.clinbiomech.2016.08.010. [DOI] [PubMed] [Google Scholar]