Abstract
Context
Given the frequency of ankle sprains, especially in the athletic population, prevention is a primary task of athletic trainers and other sports health care professionals.
Objective
To discuss the current evidence as it relates to prophylactic programs for the prevention of ankle sprains and to provide critical interpretation of the evidence supporting and refuting the implementation of preventive programs.
Conclusions
External prophylactic supports and preventive exercise programs are effective for reducing the risk of ankle sprains in both uninjured and previously injured populations. Ankle bracing appears to offer the best outcomes in terms of cost and risk reduction. However, there remains a paucity of well-designed, prospective randomized controlled trials relevant to the primary prevention of lateral ankle sprains, especially across a range of sport settings.
Keywords: taping, bracing, prophylactic supports, proprioception, neuromuscular function
The public health burden of ankle sprains across athletic, physically active, and general populations is well established.1 Beyond the widespread prevalence of these injuries, lateral ankle sprains are associated with deleterious outcomes secondary to common sequelae, such as chronic ankle instability (CAI) and posttraumatic osteoarthritis.2,3 Subsequently, patients with this spectrum of injury—originating from a single ankle sprain—experience deficits in health-related quality of life4 and potential decreases in physical activity,5 which negatively affect overall health and produce an economic burden on global health care systems.6 Although researchers continue to explore rehabilitation techniques capable of optimizing outcomes in patients with these injuries, we must also address both primary prevention and secondary prevention of recurrent damage.
When considering the long-term effects of ankle conditions, such as CAI and posttraumatic osteoarthritis, it is important to consider that the origin of this cascade of events is the initial lateral ankle sprain.7,8 Consistently, the most common risk factor for lateral ankle sprains is a previous history of that injury.9,10 Multiple hypotheses exist to explain this relationship, but it is generally accepted that damage to the ligament initiates changes to the joint's biomechanics and modifies neural control of the joint.11 Subsequently, these patients exhibit kinematics that place the joint at risk of reinjury,12 while concurrently demonstrating altered neuromuscular control and functional performance that diminish the ability of the dynamic stabilizers to adequately stress shield the joint.13,14 Therefore, these patients enter a negative feedback loop by which each injury leaves the joint more vulnerable to subsequent injury, exposing the joint to atypical forces that contribute to degenerative changes. Because as many as 70% of patients with ankle sprains experience recurrent injury and enter this negative feedback loop, primary prevention is paramount to diminishing the global burden of this common condition.2,15 With nearly continuous access to their patient populations, athletic trainers (ATs) and other sports health care professionals often have a unique advantage in implementing prevention programs among athletes and the physically active. These prevention programs may include screening of participants for risk factors; however, which interventions are most effective in eliminating those risk factors and subsequently decreasing the injury risk has not been determined.
Similar to the deficits observed after injury, prophylactic interventions to minimize the risk of ankle sprains can often be stratified into interventions capable of affecting mechanical function and those designed to improve proprioceptive ability and neuromuscular function about the joint. The former often involves the use of external supports, such as taping and bracing, with the intent of preventing the joint from exceeding the physiological range of motion, thereby minimizing stress on the static joint stabilizers.16 Conversely, proprioceptive and neuromuscular risk factors are addressed via exercise programs designed to optimize the ability of the dynamic stabilizers to protect the joint.17 Although commonly implemented in athletic settings, both types of prevention programs often require significant time and financial resources that may deter clinicians from maximizing their use. The purpose of this review is to discuss the current evidence as it relates to prophylactic programs for the prevention of ankle sprains and to provide critical interpretation of the evidence supporting and refuting various preventive programs.
EVIDENCE SEARCH
Our intent was to provide an evidence review regarding current practice as it relates to the primary and secondary prevention of ankle sprains. Even though our goal was not to conduct a systematic review, we used certain similar methods to ensure a comprehensive search for the available evidence. Systematic searches of the literature were implemented to identify evidence relating to intervention strategies in the prevention of ankle sprains. The search was split into evidence regarding taping and the application of external prophylactic supports and that addressing prophylactic exercise programs. With regard to external support (ie, taping and bracing), our initial search strategy revealed several systematic reviews whose authors had thoroughly explored this topic, and therefore, we limited our systematic search in MEDLINE (PubMed) and the Cumulative Index for Nursing and Allied Health Literature (CINAHL) to systematic reviews discussing this intervention. For intervention programs, a similar initial exploratory search was implemented, and we conducted a search of the literature in MEDLINE and CINAHL for randomized controlled trials of preventive programs in athletic populations. For both topics, we included only articles that provided information directly related to ankle injury rates. More detailed information on our search strategy and article inclusion can be found in Appendices 1 and 2. We purposefully included several tables to summarize the importance of this literature related to ankle-sprain prevention and, whenever available, supplied associated odds or risk ratios for interpretation by the clinical sports medicine practitioner.
EXTERNAL PROPHYLACTIC SUPPORT
Because ankle sprains are so common, especially in the athletic population, prevention is a primary task of ATs and other sports health care professionals. Ankle bracing can be traced back to the 1880s, with the advent of the lace-up ankle brace patented to Frederick Hackey on May 24, 1887, and most likely used for general medical purposes and not sport.18 Gibney19 introduced the concept of ankle taping as a treatment for ankle sprains in 1895, and for more than a century, ankle taping has been advocated as a means of protecting the ankle ligaments from excessive strain. To this day, ankle taping and bracing remain popular ankle injury-prevention modalities at all levels of athletic competition, although some have questioned their effectiveness in preventing both first-time ankle sprains and subsequent sprains in those with a history of injury. The purpose of this section of the review is to share the most current evidence examining the effectiveness of ankle taping and bracing in preventing ankle sprains.
The 2013 “National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes”20 devoted a section to taping and bracing considerations and yet failed to make any succinct recommendations regarding the effectiveness of taping and bracing or the superiority of 1 method over the other. Despite the obvious advantages of ankle bracing related to self-application, reuse, and adjustments, taping is well known to be more expensive than bracing, especially over the long term.21 A plethora of ankle-taping techniques is available; selection is typically based on the clinician's familiarity with the strapping technique and the athlete's preference. Ankle braces are divided into 3 primary categories: soft, semirigid, and rigid. The effectiveness of taping and bracing depends on the material properties, application method, and whether the athlete has ankle instability or a history of a previous sprain.22 The greater acceptance of ankle bracing and evolving design technology over the years has narrowed the gap between bracing and taping. The prevailing early opinion of most sports medicine clinicians and athletes was that taping provided superior benefits related to comfort, perception of greater support, and less interference with normal function.23
Rationale for Taping and Bracing
Although many variations of ankle taping applications and brace designs are available, the obvious question is “what exactly is the rationale for prophylactic ankle taping and bracing?” Zwiers et al22 best summarized the effects of ankle taping and bracing in a recent review paper using 3 categories: (1) mechanical, (2) neuromuscular, and (3) psychological.
Mechanical Support
Mechanical support is thought to be the primary benefit of ankle taping and bracing, preventing extreme and abnormal variants in range of motion. Restricted are all 4 directions of ankle motion (inversion, eversion, plantar flexion, and dorsiflexion) as well as accessory motions such as anteroposterior translation of the talus.16 Some have argued that taping and bracing may lose mechanical effectiveness during exercise or activity, but their restraining effect on extreme ankle motion is not eliminated completely during prolonged athletic activities.16,23
Neuromuscular Effects
Taping and bracing both have profound neuromuscular influences. Neuromuscular control in and around the ankle joint is achieved via a combination of improved proprioception, peroneal muscle activity, reflexive action, reaction time, and postural stability.22 Taping or a brace is theorized to increase stimulation of the cutaneous mechanoreceptors, which enhances proprioception by modifying the sensitivity of the musculotendinous mechanoreceptors surrounding the joint.24 The peroneal muscles are important evertors of the ankle joint and thought to counter violent inversion moments that typically occur during an ankle sprain. Peroneal muscle function and latency have both been studied extensively, but evidence of benefits provided by ankle taping and bracing is inconclusive.25 However, postural control—the act of maintaining, achieving, or restoring a state of balance during any posture or activity—seems to improve with taping and bracing.22,26
Psychological Benefits
Although not usually considered a benefit of ankle taping or bracing prescribed to prevent ankle sprains, the potential psychological aspects of this intervention strategy may be helpful.27 Investigators28 reported enhanced perceptions of stability, confidence, and reassurance during activity and a level of comfort enabling participants to think that they would not sprain their ankles. This benefit was not directly linked to ankle stability, yet key psychosocial risk factors for musculoskeletal injury have recently been identified.29
Effectiveness of Taping and Bracing in Preventing Ankle Sprains
The prevention of an initial ankle sprain is the goal of any ankle prophylaxis. It is important to understand that prevention is the key word here and should not be confused with ankle-sprain treatments that may involve taping or bracing. We did not include the latter studies in our search for evidence on preventing ankle sprains. Since 1990, published studies of varying methodologic quality have addressed taping and bracing for preventing ankle sprains. In addition, authors of a number of systematic reviews (and meta-analyses) have tried to offer generalizations and recommendations based on the best available evidence (Table 1). In 2016, Zwiers et al22 summarized their review of the current literature on taping and bracing for preventing ankle sprains by concluding that (1) taping and bracing were valid prophylactic measures for preventing first-time and recurrent sprains, especially among athletes who played high-risk sports such as basketball, football, and volleyball; (2) the number needed to treat was lower for braces than for tape; (3) taping and bracing lost their restrictive properties during exercise; and (4) taping and bracing minimally affected performance. As a practical note, the affordability of ankle bracing, especially over the long term, is a concern; readers are directed to a 2004 article by Olmsted et al21 for details on how taping and bracing compared from a cost standpoint. Evans and Clough30 provided a thorough systematic review in 2013 and determined that bracing was the best and least expensive intervention for preventing ankle sprains. Dizon and Reyes,31 in their 2010 systematic review on the effectiveness of external supports in the prevention of inversion ankle sprains, also noted that ankle sprains were reduced by approximately 70% when ankle braces were worn. Many more researchers have examined the effect of taping on laboratory measurements, such as proprioception, balance, and structural support, than in preventing sprains.30 Verhagen and Bay,32 in their 2010 critical review and practical appraisal of the ankle-sprain literature, reported that, among the few studies involving taping prophylaxis, the sprain rate was 2-fold to 4-fold lower in participants with taped ankles versus those opting for no preventive intervention. The number of studies demonstrating the preventive effects of taping on first-time ankle sprains25,30,31 is limited, due mostly to the difficulty of developing and executing randomized controlled trials that would involve the same clinician applying the tape and carefully monitoring athlete-exposure rates over time.27,35,36 The seminal 1973 work of Garrick and Requa35 examining ankle-sprain prevention has shockingly never been replicated. Their findings supported the use of ankle taping in preventing both primary and recurrent sprains among basketball players, yielding a 55% risk reduction.35 In 1988, Rovere et al37 concluded that lace-up ankle braces resulted in a lower risk of ankle sprain than ankle taping among football players. In 2006, Mickel et al36 observed reductions in the incidence of ankle sprains among their select group of high school athletes using ankle taping and bracing. We carefully examined these studies and determined that the researchers all used a closed basket-weave technique involving a figure-of-8 heel lock. Additionally, all used 1.5-in (3.8-cm) adhesive tape, pretape underwrap, and heel and lace pads with skin lubricant. For the sake of completeness, we also mention early, limited reviews of ankle-sprain prevention by Handoll et al33 in 2001 and Thacker et al34 in 1999; they determined that both taping and bracing were effective means of preventing ankle sprains. Considering that ankle taping is perhaps the most time-honored tradition in the athletic training profession, it is alarming that only a handful of well-designed randomized, controlled trials have been carried out to investigate the effectiveness of such prophylaxis. Our report should serve notice that such studies are necessary.
Table 1.
Summary of Review Articles Examining Taping and Bracing in the Prevention of Ankle Sprains
| Study |
Title |
Number of Studies Included |
Conclusions |
| Zwiers et al22 (2016) | “Taping and bracing in the prevention of ankle sprains: current concepts” | 17 | Taping and bracing have a preventive effect on ankle sprains during sports and minimally affect sport-specific performance. No clear distinction can be made for taping versus bracing; therefore, the athlete's personal preference should be heeded. |
| Evans and Clough30 (2013) | “Prevention of ankle sprain: a systematic review” | 3 | Only bracing has been proven to limit ankle sprains in a controlled sport trial. Taping, while effective in empirical trials, may or may not have a preventive effect in sports or ordinary daily activities. Studies involving orthotic interventions lacked evidence for or against ankle-sprain prevention. |
| Dizon and Reyes31 (2010) | “A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players” | 7 | Reduction of ankle sprain by 69% (odds ratio = 0.31) with an ankle brace and reduction of ankle sprain by 71% (odds ratio = 0.29) with ankle taping among previously injured athletes. |
| Verhagen and Bay32 (2010) | “Optimizing ankle sprain prevention: a critical review and practical appraisal of the literature” | 8 | Compared with no intervention, ankle-sprain rates were 2-fold to 4-fold lower in taped ankles. Taping seemed particularly effective for previously sprained ankles. Bracing was effective in preventing ankle sprains, with risk ratios from 0.15 to 0.50 in favor of bracing. Bracing was also effective in preventing recurrent ankle sprains. |
| Handoll et al33 (2001) | “Interventions for preventing ankle ligament injuries” | 4 | Reduced number of ankle sprains in people allocated external supports (risk ratio = 0.53). The reduction was greatest in those with a history of previous ankle sprains but still possible for those without prior sprain. |
| Thacker et al34 (1999) | “The prevention of ankle sprains in sports: a systematic review of the literature” | 6 | Taping can prevent ankle sprains, especially in those with previous ankle injuries. |
Alternative Taping Therapies and Foot Orthoses
Alternative taping therapies have become more mainstream over the last decade as health care professionals, including ATs, seek better ways to prevent injuries among athletes. For preventing ankle sprains, 2 such alternative therapies that have been introduced: Kinesio taping (Kinesio Co, Ltd, Tokyo, Japan) and fibular-repositioning taping (FRT). Kinesio taping for the ankle is a large deviation from the traditional taping method and involves the precise placement of 3 to 4 strips of Kinesio tape across the ankle joint, in line with the ankle-stabilizing muscles (Figure 1).38–40 Although Kinesio tape is commonly advertised as improving proprioception and neuromuscular control, as well as providing external support that can be worn over several days and with minimal discomfort, its effectiveness in preventing injury is largely unfounded. Very few well-controlled studies examining its effectiveness in injury prevention have been carried out, with authors instead identifying the effect of Kinesio taping on risk factors associated with ankle sprains. These studies have provided equivocal evidence regarding the tape's proprioceptive effects39–42 but promise in modifying stiffness characteristics and improving joint stability during functional movements.42,43 In fact, in their 2012 meta-analysis of Kinesio taping for the treatment and prevention of sports injuries, Williams et al44 noted that little quality evidence supported the use of Kinesio taping over other types of elastic taping for managing or preventing sports injuries.
Figure 1.
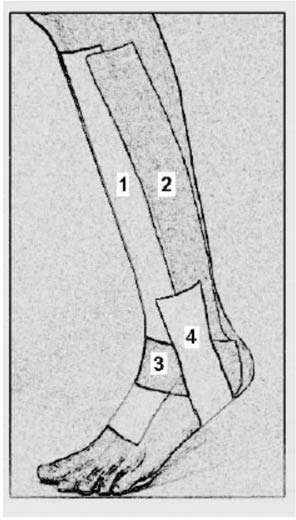
Kinesio taping for the ankle. (Reprinted with permission from Halseth et al [2004]).39
The FRT technique was introduced by Mulligan45 and purported to correct an anterior positional fault of the fibula while maintaining correct fibular alignment (Figure 2). The only examination of the effectiveness of the FRT technique in preventing ankle sprains was carried out in 2006 by Moiler et al.46 Among Australian basketball players, the FRT method provided a prophylactic benefit over the no-intervention control group.
Figure 2.

Fibular-repositioning taping by Mulligan. (Reprinted with permission from Moiler et al [2006]).46
As high-top shoe designs became popular in sports (especially basketball) in the 1970s, Garrick and Requa35 examined their contribution in the prevention of ankle sprains. Interestingly, they concluded that a combination of high-top shoes and ankle taping decreased the frequency of ankle sprains, especially among those with previous injuries. Very little research into shoe design for preventing ankle sprains has been carried out. Verhagen and Bay32 performed a critical review and concluded that the effect of shoe type and design on sprain incidence remains speculative. Curtis et al47 assessed the role of shoe design in the incidence of lateral ankle sprains among collegiate basketball players. They hypothesized that collegiate basketball players wearing the cushioned-column shoe design would have a higher incidence of lateral ankle sprains than those not wearing this shoe type and were surprised when neither group experienced an increase in sprains.47
Foot orthotics are sports medicine treatments for a variety of lower extremity ailments; however, their use as a prophylactic intervention for ankle sprains has been limited. The 2013 systematic review by Evans and Clough30 included orthotics together with taping and bracing as an intervention for ankle-sprain prevention. However, few authors performed empirical research using traditional foot orthotics, and of those, none examined the ankle-sprain risk. Some limited evidence supports the use of custom orthotics to control inversion perturbations in those with previously sprained ankles, yet no investigators have addressed their use in preventing first-time ankle sprains.48
PROPHYLACTIC PREVENTION PROGRAMS
An alternate method of addressing ankle-sprain prevention and avoiding the initiating event contributing to a lifetime of negative sequelae is implementing preventive exercise programs to improve dynamic ankle stability. These programs are arguably more labor intensive than prophylactic support options, typically requiring 15 to 30 minutes of time on multiple days per week, and thereby potentially affecting compliance.49 However, these programs also highlight cooperation among the sports medicine team members, as the exercises are often integrated into prepractice treatments, warmups, or team conditioning sessions. Furthermore, their utility extends beyond the prevention of ankle sprains, as the exercises include stretching, balancing, power, and agility techniques that may prevent injuries to multiple joints and contribute to improved athletic performance.17,49 Yet the utility of these programs in decreasing the incidence of ankle sprains largely depends on their ability to enable individuals to better control the position of the joint and optimize neuromuscular control to appropriately stress shield the joint in preparation for and in reaction to potentially injurious joint loading.13,50
Rationale for Preventive Programs
Exercise programs to prevent ankle sprains and other lower extremity injuries often incorporate similar components, such as stretching, strengthening, balancing, and sport-specific hopping and agility motions.32,51 Each component may highlight an important role in the prevention of these injuries. Stretching, specifically of the triceps surae, improves dorsiflexion range of motion about the ankle. Given the frequency of range-of-motion deficits among patients with CAI, improving this motion was hypothesized to allow the joint to function in a more stable position.52 The suggested role of strengthening was to allow the joint to better withstand injurious loads; however, given the high loads associated with ankle-sprain mechanisms, strengthening of the ankle stabilizers does not seem likely to contribute to injury prevention.53 Many prevention programs emphasize strengthening about the hip and knee joints rather than the ankle, which may place the lower extremity at decreased risk of injury.54,55 Squats, planks, and lateral hip-strengthening exercises are often incorporated with the intent of optimizing neuromuscular control about the proximal musculature to allow adaptation to unstable surfaces.55
Balancing and proprioceptive exercises are the core components of many of these programs and are the most common prevention techniques in exercise programs.32 These exercises include single-limb balancing on stable and unstable surfaces, often with perturbations such as throwing or kicking a ball, using a wobble board, or manipulating the task (ie, adding a reach). These subsequently serve to enhance both the static and dynamic postural control necessary for athletic performance by optimizing the body's ability to sense and correct mild deviations in joint motion.50,56 Similar to strengthening, static and dynamic balance exercises incorporate corrections not only of the ankle joint but the proximal joint systems. Proprioceptive exercises often continuously progress and merge into sport-specific exercises that emphasize neuromuscular training through hopping and agility-based tasks. As the speed of contraction increases during hopping and cutting tasks, so does neuronal firing, facilitating rapid force development that may be crucial in preventing impending rollover events.57,58
Effectiveness of Intervention Programs in Preventing Ankle Sprains
Although each of these components has been individually demonstrated to improve the outcome it directly targets (ie, stretching improves range of motion, balancing improves postural control),52,59,60 several limitations affect the effectiveness of these changes in preventing ankle sprains. First, the authors of investigations into the effects of each individual training component have largely addressed subsets of healthy or injured participants, without directly looking at the component's influence on injury risk. Second, those researchers who quantified the effects of these training techniques on primary ankle-injury prevention often combined the interventions, making it difficult to determine the direct risk reduction from individual components. As the purpose of our review was to audit the direct effectiveness of current prevention techniques on injury risk, we identified studies that implemented training programs and subsequently quantified the rates of ankle sprains or injuries among those receiving an intervention compared with a control group. Articles implementing primary prevention programs and quantifying rates of ankle sprains or injuries are presented in Table 2. Although limited in number, these examinations offered excellent insight into the effectiveness of the programs across a range of high-risk populations. Nearly all investigations were performed across sports with known high rates of ankle sprains: soccer,61–65 basketball,65–68 and volleyball,69 along with 2 involving European handball,70,71 and 1 among military recruits.72 A broad range of ages and both sexes were included; however, only 3 studies65,66,71 had the primary purpose of preventing ankle sprains; the remainder quantified injuries throughout the lower extremity. As such, these prevention programs often focus on exercises at the hip and knee and have unknown effects on the ankle. Furthermore, only 4 studies64–66,69 quantified ankle sprain as a specific outcome aside from general ankle injuries.
Table 2.
Articles Implementing Primary Prevention Programs and Quantifying Ankle-Injury or -Sprain Rates
| Study |
Population |
Intervention |
Ankle Specific? |
Outcome |
Risk Ratio (95% CI) |
Number Needed to Treat |
| Emery and Meeuwisse (2010)61 | Adolescent male and female soccer teams | Strengthening for core, hip, and knees | No | Ankle injuries | 0.46 (0.24, 0.87) | 26.8 |
| SL static balancing with perturbations | ||||||
| Engebretsen et al (2008)62 | Adult male soccer teams | Strengthening for groin and knee | No | Ankle injuries | 0.66 (0.34, 1.28) | 11.3 |
| SL hopping in multiple planes | ||||||
| Static and dynamic balancing tasks with perturbations | ||||||
| Labella et al (2011)63 | Adolescent female soccer teams | Coach-implemented program consisting of strengthening, plyometric, balance, and agility exercises. | No | Ankle sprain | 0.43 (0.18, 1.04) | 76.8 |
| Soligard et al (2008)64 | Adolescent female soccer teams | FIFA-11 program consisting of lower extremity strengthening, SL balancing, and DL and SL hopping | No | Ankle sprain | 0.85 (0.57, 1.26) | 63.6 |
| McGuine and Keene (2006)65 | Adolescent male and female basketball and soccer athletes | Static and dynamic balancing tasks with perturbations | Yes | Ankle sprain | 0.62 (0.38, 1.02) | 26.4 |
| Eils et al (2010)66 | Adolescent and adult male basketball athletes | Static and dynamic balancing tasks | Yes | Ankle injuries | 0.35 (0.16, 0.80) | 5.5 |
| SL hopping exercises | ||||||
| Emery et al (2007)67 | Adolescent male and female basketball teams | SL static balancing with perturbations | No | Ankle injuries | 0.70 (0.52, 0.96) | 18.9 |
| Longo et al (2012)68 | Adolescent male elite basketball teams | FIFA-11 program consisting of lower extremity strengthening, SL balancing, and DL and SL hopping | No | Ankle injuries | 0.77 (0.13, 4.42) | 88.6 |
| Verhagen et al (2004)69 | Adult male and female volleyball players | SL balancing with perturbations | No | Ankle sprain | 0.54 (0.34, 0.85) | 21.5 |
| Olsen et al (2005)70 | Adolescent male and female handball teams | Hip and knee strengthening and plyometric exercises | No | Ankle injuries | 0.60 (0.38, 0.93) | 59.7 |
| Agility exercises | ||||||
| DL and SL static and dynamic balance | ||||||
| Wedderkopp et al (1999)71 | Adolescent female handball players | SL balancing exercises with perturbations | Yes | Ankle injuries | 0.30 (0.13, 0.70) | 7.8 |
| Goodall et al (2013)72 | Male and female army recruits | Dynamic SL and DL balance tasks | No | Ankle injuries | 1.11 (0.77, 1.59) | 75.0a |
| SL and DL hopping exercises | ||||||
| Overall effect—ankle sprain | 0.72 (0.61, 0.85) | 37.4 | ||||
| Overall effect—ankle injuries | 0.53 (0.40, 0.70) | 39.0 | ||||
Abbreviations: CI, confidence interval; DL, double legged; FIFA, Fédération Internationale de Football Association; SL, single-legged.
a Indicates number needed to harm.
The effectiveness of these programs varies across the range of sports, ages, training, and outcome measures, yet prevention programs have been associated with a 30% to 45% decrease in the ankle-sprain or -injury risk. A numbers-needed-to-treat analysis revealed that 5.5 to 89 individuals would need to undergo training to prevent a single ankle sprain, demonstrating the variability of program effectiveness. Given the variety of interventions, populations, and outcome measures, it is difficult to determine the factors that contributed to better outcomes in some studies compared with others. No obvious advantage occurred from a program designed to target ankle injuries as opposed to an array of lower extremity injuries, nor were notable differences observed between studies that targeted ankle sprains as the primary outcome versus all ankle injuries. However, the researchers who demonstrated the greatest risk reduction commonly incorporated single-limb static balancing with perturbations, often including the use of either perturbation platforms (eg, wobble boards) or a sport-specific task such as catching, throwing, kicking, or dribbling a ball.62,66,71 Thus, exercises to improve proprioception and neuromuscular control seemed to be the primary component decreasing the ankle-sprain risk across broad populations.
These data should be considered with some caution. The interventions in most studies were delivered by either a coach or AT as a dynamic warmup before practice among cohorts of teams that were randomly selected to receive them. However, the control groups in these studies participated in team warmups that might have naturally incorporated exercises designed to improve range of motion, strength, hopping, or agility, which may identify balancing exercises as the key difference between these groups. Further work may be required to attempt to modify the best components of a dynamic warmup and delivery method (ie, from the AT or coach) for improving outcomes with a primary prevention program. Additionally, it is important to note that these studies primarily focused on adolescent and young adults, leaving some question regarding the effectiveness of the interventions among older and younger populations.
Comparing Prophylactic Support and Exercise Programs
Each external prophylactic support and exercise program for the prevention of ankle sprains has its pros and cons. Currently, no investigators have directly compared the benefits of each in a primary prevention setting, making it difficult to determine which is more effective. When comparing the risk ratios associated with taping and bracing versus those of preventive programs, an external prophylactic support appears to be slightly more effective in preventing ankle sprains. Additionally, reusable ankle braces are a demonstrated cost-effective method of preventing ankle injury that can be used in the absence of an AT or other practitioner.21 Such braces are also time effective, typically requiring less than 5 minutes per day, and athletes can apply them concurrently (as opposed to taping).
However, several additional factors must be considered when determining the most effective method of preventing ankle sprains in a given setting. Prevention programs are generally cost effective, as minimal equipment is necessary, and balance perturbations can be applied with equipment typically used for that sport.17,32,49 Although more time intensive, these programs can be incorporated into a team or individual's dynamic warmup routine; many studied programs were led by team coaches who received standardized information regarding the exercises to include and were given feedback. Furthermore, as previously mentioned, these techniques not only benefit injury prevention but also potentially improve performance.49 This is in stark contrast to emerging evidence regarding the use of prophylactic support that indicates associated decreases in speed and jump height.73
The clinician need not decide between using external supports or preventive programs, as both could aid in the reduction of injuries among athletes in high-risk sports. Yet in accordance with current models of evidence-based medicine, it would be paramount to consider the values of patients and coaches regarding the time and financial resources dedicated to prevention, sport-specific activities that may be impeded by the support, and individual preferences.
SECONDARY PREVENTION OF ANKLE SPRAIN
The focus of our review has been the primary prevention of ankle sprains: an attempt to avert the initial injury that predisposes individuals to reinjury and further disability. However, given the prevalence of ankle sprains and the consistency with which a history of ankle sprain predisposes an individual to subsequent injury, the secondary prevention of these injuries should also be of interest to practicing clinicians.74 Unsurprisingly, among the most commonly identified recommendations for preventing secondary injury is conservative treatment of the initial ankle injury. Multiple investigators7,8 have proposed that the subacute phase of injury (2–4 weeks), when inflammation is subsiding and musculoskeletal and nervous systems are adapting to imposed constraints, may be the most crucial in determining whether individuals will experience recurrent problems. Incorporating targeted rehabilitation exercises and optimizing joint loading through the use of dynamic immobilization devices may allow for optimal healing, enabling a safer return-to-play progression.75–77
After recovery from the initial injury, the question remains whether similar prophylactic external supports or exercise programs can modify the risk of subsequent injuries. The authors of earlier meta-analyses provided cumulative odds ratios for reinjury with the use of prophylactic supports or exercise programs among individuals with previous ankle injury. Regarding external prophylactic support, Doherty et al78 reported a cumulative odds ratio of 0.40 (95% confidence interval [CI] = 0.29, 0.56), favoring bracing for preventing recurrent ankle sprains.78 Although this result is in line with odds ratios for the primary prevention of ankle sprain via taping and bracing, it is important to note that these investigators did not separate the times of brace application (acute versus after recovery), and all included studies took place before 2000. Given the developments in brace technology since this work, further research should be conducted to determine the effectiveness of external supports in preventing recurrent ankle sprains.
Risk reduction from proprioceptive training or exercise programs for patients with a history of ankle sprain yields similar values as observed for primary prevention. Meta-analyses by Doherty et al78 and Schiftan et al17 showed odds ratios of 0.57 (95% CI = 0.49, 0.66) and 0.64 (95% CI = 0.51, 0.81), respectively. Interestingly, many of the higher-quality randomized controlled trial designs65,69,79 demonstrated nonsignificant effects of proprioceptive training; however, when they were pooled, an effect was apparent. These investigations included proprioceptive programs with an emphasis on single-limb balancing progressions performed as part of a warmup routine several times per week. Although this training certainly works to restore proprioception and improve neuromuscular control and is effective in rehabilitative protocols, continuing these exercises through an athletic season is likely the factor that contributes to the risk reduction.
Although no authors directly compared external supports and exercise programs in the primary prevention of ankle sprain, Janssen et al80 conducted a randomized controlled trial of semirigid bracing, unsupervised proprioceptive training, and both combined in reducing recurrent ankle injuries across a broad range of athletes. Despite high levels of participant attrition, bracing was more effective than training for reducing recurrent ankle injuries (risk ratio [RR] = 0.52, 95% CI = 0.28, 0.95). This reduction was greater than the combination of bracing and training program versus training alone (RR = 0.71, 95% CI = 0.41, 1.22). Despite several methodologic concerns (eg, high levels of attrition and noncompliance, self-reports of injury and compliance, and an unsupervised intervention80), these findings provide insight into the potential real-world limitations and moderate effectiveness of these interventions for preventing recurrent injuries. A previous report21 highlighted the cost- and time-effectiveness of bracing, which perhaps contributed to this intervention being better in preventing recurrent injuries among these populations. To our knowledge, no prospective randomized controlled trials have yet addressed the simultaneous or comparative effect of external supports versus exercise programs on the primary prevention of ankle injury. Also needed are studies assessing patient-perceived barriers to optimizing injury prevention.
EMERGING PREVENTION TECHNIQUES
In the constantly evolving health care system, techniques, technologies, and scientific theories have emerged that may affect ankle-sprain prevention practices in the coming years. For instance, the designs of ankle braces have continued to advance, with lighter, semirigid materials that improve comfort and provide multiplane stability.18,81 Technological advances have also facilitated the implementation of exercise programs via the Internet and smartphone apps. These technologies have made it easier to educate coaches, athletes, and staff regarding preventive exercises, providing cueing for proper and improper techniques, and progression options. These interventions can improve the feedback provided by coaches during warmup routines and supply athletes with take-home exercises to improve ankle stability. Furthermore, Van Reijen et al82 demonstrated that smartphone app-based interventions could be effective in decreasing the ankle-sprain risk among patients with a history of ankle sprain. However, limitations of these interventions include less compliance with e-health–based interventions and the lack of personal feedback. As technology advances, e-health–based prevention techniques may become increasingly prevalent throughout sports medicine.
A final emerging area to consider for ankle-sprain prevention is incorporating dual-task and cognitive loading in intervention techniques. Increasing evidence8,83 has attributed an increased risk of ankle and other joint injuries to attentional changes related to external events. This is based on the theory that injuries are most likely to occur when individuals are physically and mentally fatigued, thinking about multiple items (eg, where to run or pass the ball, what play is next), startled, or otherwise distracted.84–86 As cognitive resources are dedicated to other tasks, individuals often lose the concentration that may be needed to stabilize the lower extremity. New evidence84,86 supported the use of cognitive training in prevention and rehabilitation programs, such as performing cognitive tasks during balancing exercises or incorporating choices and decision making into dynamic-stabilization tasks.
CONCLUSIONS
Overall, our findings indicate that, although both external prophylactic supports and preventive exercise programs are effective for reducing the risk of ankle sprains, both in uninjured and previously injured populations, external support in the form of bracing appears to offer the best outcomes in terms of cost and risk reduction. However, both external supports and preventive programs are effective in decreasing ankle-sprain risk and can be used together for the best outcomes. Furthermore, preventive programs protect multiple joint systems from injury. In these scenarios, athletes in high-risk sports may be taped or braced before practices and competitions. A neuromuscular warmup that implements static and dynamic balancing 3 or more days per week supplies an added dimension of protection. In this context, the AT should work with coaches, strength and conditioning specialists, and other members of the sports health care team to determine the time and expense that can be dedicated to preventing these common injuries.
Despite the evidence from which these conclusions were drawn, we still have a pressing need to further develop evidence relevant to the prevention of lateral ankle sprains. For instance, although many authors have studied the mechanical and proprioceptive benefits of ankle taping and bracing, contemporary prospective research aimed at identifying the level of risk reduction using various types of external prophylactic supports is lacking. Similarly, given the high levels of variability in injury-risk reduction from prophylactic programs, further investigation may be necessary to determine which program elements improve injury-related outcomes. Moreover, researchers should aim to better identify the barriers to implementation of these preventive programs across a range of physically active populations. These programs seem to be empirically effective, yet epidemiologic investigations have not indicated any changes in trends related to injury rates, suggesting that the use of these programs is not being optimized.
Appendix 1.
Search Strategy for Systematic Reviews Related to Taping and Bracing (Search Performed in October 2017 and Updated January 2018)
| Step |
Search Term(s) |
PubMed Results |
CINAHL Results |
| 1 | Ankle OR lower limb | 24 012 | 34 862 |
| 2 | Injur* | 1 072 540 | 243 396 |
| 3 | Prevent* | 2 217 819 | 619 699 |
| 4 | Tape OR tapin* OR brac* OR support | 8 680 903 | 337 995 |
| 5 | 1 AND 2 AND 3 AND 4 | 1849 | 309 |
| 6 | 5 AND filter: systematic review | 51 | 22 |
Appendix 2.
Search Strategy for Systematic Reviews Related to Injury-Prevention Programs (Search Performed in October 2017 and Updated in January 2018)
| Step |
Search Term(s) |
PubMed Results |
CINAHL Results |
| 1 | Ankle OR lower limb | 24 012 | 34 862 |
| 2 | Injur* | 1 072 540 | 243 396 |
| 3 | Prevent* | 2 217 819 | 619 699 |
| 4 | #1 AND #2 AND #3 | 1595 | 1615 |
| 5 | #5 AND filter: randomized control trial | 108 | 70 |
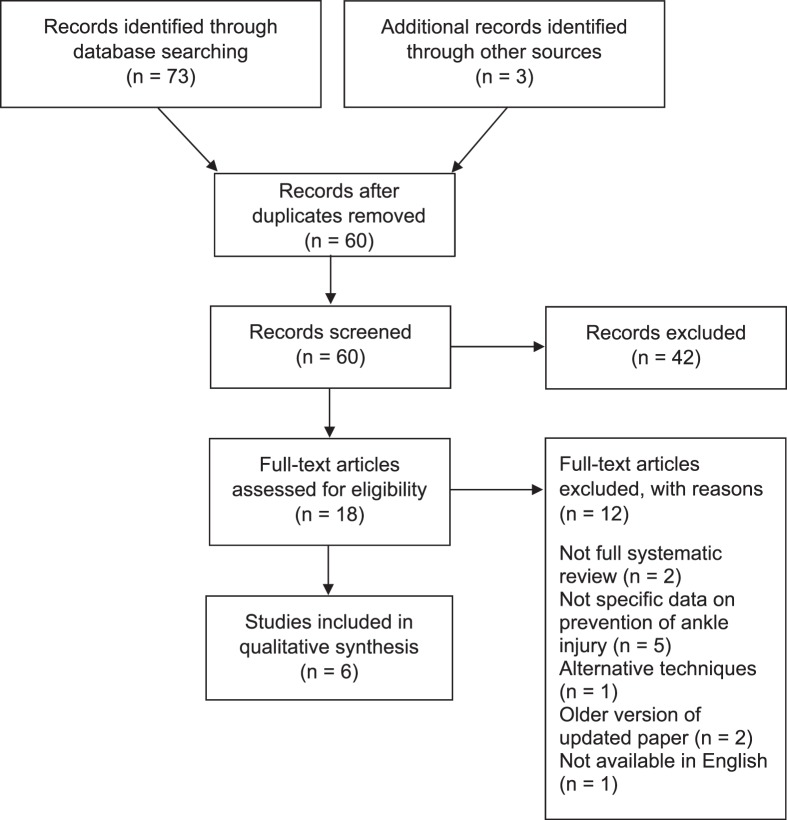
Appendix Figure 1.
Search strategy for systematic review papers related to taping and bracing.
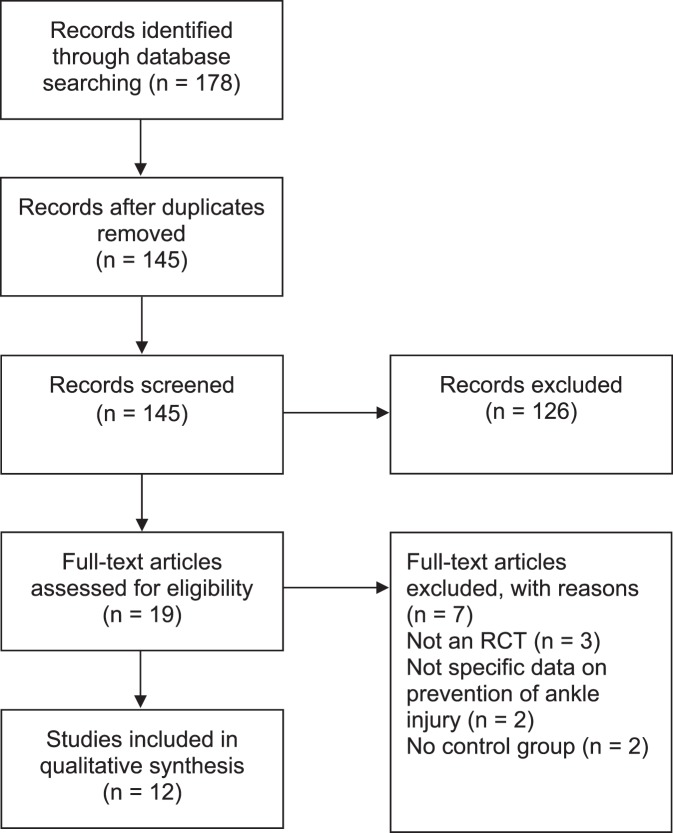
Appendix Figure 2.
Search strategy for systematic review papers related to prevention programs. Abbreviation: RCT, randomized controlled trial.
REFERENCES
- 1.Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 2.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. discussion e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golditz T, Steib S, Pfeifer K, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthritis Cartilage. 2014;22(10):1377–1385. doi: 10.1016/j.joca.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 4.Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–763. doi: 10.4085/1062-6050-49.3.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hubbard-Turner T, Turner MJ. Physical activity levels in college students with chronic ankle instability. J Athl Train. 2015;50(7):742–747. doi: 10.4085/1062-6050-50.3.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah S, Thomas AC, Noone JM, Blanchette CM, Wikstrom EA. Incidence and cost of ankle sprains in United States emergency departments. Sports Health. 2016;8(6):547–552. doi: 10.1177/1941738116659639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wikstrom EA, Brown CN. Minimum reporting standards for copers in chronic ankle instability research. Sports Med. 2014;44(2):251–268. doi: 10.1007/s40279-013-0111-4. [DOI] [PubMed] [Google Scholar]
- 8.Needle AR, Lepley AS, Grooms DR. Central nervous system adaptation after ligamentous injury: a summary of theories, evidence, and clinical interpretation. Sports Med. 2017;47(7):1271–1288. doi: 10.1007/s40279-016-0666-y. [DOI] [PubMed] [Google Scholar]
- 9.Baumhauer JF, Alosa DM, Renstrom AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 10.Beynnon BD, Renström PA, Alosa DM, Baumhauer JF, Vacek PM. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19(2):213–220. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 11.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. vii. [DOI] [PubMed] [Google Scholar]
- 12.Chinn L, Dicharry J, Hertel J. Ankle kinematics of individuals with chronic ankle instability while walking and jogging on a treadmill in shoes. Phys Ther Sport. 2013;14(4):232–239. doi: 10.1016/j.ptsp.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Needle AR, Baumeister J, Kaminski TW, Higginson JS, Farquhar WB, Swanik CB. Neuromechanical coupling in the regulation of muscle tone and joint stiffness. Scand J Med Sci Sports. 2014;24(5):737–748. doi: 10.1111/sms.12181. [DOI] [PubMed] [Google Scholar]
- 14.Rosen AB, Needle AR, Ko J. Ability of functional performance tests to identify individuals with chronic ankle instability: a systematic review with meta-analysis. Clin J Sport Med. In press. [DOI] [PubMed]
- 15.Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller HE, Needle AR, Swanik CB, Gustavsen G, Kaminski TW. Role of external prophylactic support in restricting accessory ankle motion after exercise. Foot Ankle Int. 2012;33(10):862–869. doi: 10.3113/FAI.2012.0862. [DOI] [PubMed] [Google Scholar]
- 17.Schiftan GS, Ross LA, Hahne AJ. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: a systematic review and meta-analysis. J Sci Med Sport. 2015;18(3):238–244. doi: 10.1016/j.jsams.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Peters R. The evolution and future of ankle bracing. Ultra Ankle Web site. 2017 http://blog.ultraankle.com/ankle-tech/evolution-future-ankle-bracing Accessed September 10.
- 19.Gibney VP. Sprained ankle: a treatment that involves no loss of time, requires no crutches, and is not attended with an ultimate impairment in function. NY Med J. 1895;61:193–197. [Google Scholar]
- 20.Kaminski TW, Hertel J, Amendola N, et al. National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528–545. doi: 10.4085/1062-6050-48.4.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olmsted LC, Vela LI, Denegar CR, Hertel J. Prophylactic ankle taping and bracing: a numbers-needed-to-treat and cost-benefit analysis. J Athl Train. 2004;39(1):95–100. [PMC free article] [PubMed] [Google Scholar]
- 22.Zwiers R, Vuurberg G, Blankevoort L, Kerkhoffs GMMJ. Taping and bracing in the prevention of ankle sprains: current concepts. J ISAKOS Jt Disord Orthop Sports Med. 2016;1(6):304–310. [Google Scholar]
- 23.Wilkerson GB. Biomechanical and neuromuscular effects of ankle taping and bracing. J Athl Train. 2002;37(4):436–445. [PMC free article] [PubMed] [Google Scholar]
- 24.Miralles I, Monterde S, Montull S, Salvat I, Fernández-Ballart J, Beceiro J. Ankle taping can improve proprioception in healthy volunteers. Foot Ankle Int. 2010;31(12):1099–1106. doi: 10.3113/FAI.2010.1099. [DOI] [PubMed] [Google Scholar]
- 25.Raymond J, Nicholson LL, Hiller CE, Refshauge KM. The effect of ankle taping or bracing on proprioception in functional ankle instability: a systematic review and meta-analysis. J Sci Med Sport. 2012;15(5):386–392. doi: 10.1016/j.jsams.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Pollock AS, Durward BR, Rowe PJ, Paul JP. What is balance? Clin Rehabil. 2000;14(4):402–406. doi: 10.1191/0269215500cr342oa. [DOI] [PubMed] [Google Scholar]
- 27.Simon J, Donahue M. Effect of ankle taping or bracing on creating an increased sense of confidence, stability, and reassurance when performing a dynamic-balance task. J Sport Rehabil. 2013;22(3):229–233. doi: 10.1123/jsr.22.3.229. [DOI] [PubMed] [Google Scholar]
- 28.Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010;91(9):1383–1389. doi: 10.1016/j.apmr.2010.06.023. [DOI] [PubMed] [Google Scholar]
- 29.Cagle JA, Overcash KB, Rowe DP, Needle AR. Trait anxiety as a risk factor for musculoskeletal injury in athletes: a critically appraised topic. Int J Athl Ther Train. 2017;22(3):26–31. [Google Scholar]
- 30.Evans LJ, Clough A. Prevention of ankle sprain: a systematic review. Int Musculoskelet Med. 2013;34(4):146–158. [Google Scholar]
- 31.Dizon JM, Reyes JJ. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport. 2010;13(3):309–317. doi: 10.1016/j.jsams.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Verhagen EA, Bay K. Optimising ankle sprain prevention: a critical review and practical appraisal of the literature. Br J Sports Med. 2010;44(15):1082–1088. doi: 10.1136/bjsm.2010.076406. [DOI] [PubMed] [Google Scholar]
- 33.Handoll HH, Rowe BH, Quinn KM, de Bie R. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2001;(3):CD000018. doi: 10.1002/14651858.CD000018. [DOI] [PubMed] [Google Scholar]
- 34.Thacker SB, Stroup DF, Branche CM, Gilchrist J, Goodman RA, Weitman EA. The prevention of ankle sprains in sports: a systematic review of the literature. Am J Sports Med. 1999;27(6):753–760. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- 35.Garrick JG, Requa RK. Role of external support in the prevention of ankle sprains. Med Sci Sports. 1973;5(3):200–203. [PubMed] [Google Scholar]
- 36.Mickel TJ, Bottoni CR, Tsuji G, Chang K, Baum L, Tokushige KA. Prophylactic bracing versus taping for the prevention of ankle sprains in high school athletes: a prospective, randomized trial. J Foot Ankle Surg. 2006;45(6):360–365. doi: 10.1053/j.jfas.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Rovere GD, Clarke TJ, Yates CS, Burley K. Retrospective comparison of taping and ankle stabilizers in preventing ankle injuries. Am J Sports Med. 1988;16(3):228–233. doi: 10.1177/036354658801600305. [DOI] [PubMed] [Google Scholar]
- 38.Kase K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Method Vol 2. Albuquerque, NM: Kinesio Taping Association; 2003. [Google Scholar]
- 39.Halseth T, McChesney JW, DeBeliso M, Vaughn R, Lien J. The effects of Kinesio (TM) taping on proprioception at the ankle. J Sports Sci Med. 2004;3(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 40.Shields CA, Needle AR, Rose WC, Swanik CB, Kaminski TW. Effect of elastic taping on postural control deficits in subjects with healthy ankles, copers, and individuals with functional ankle instability. Foot Ankle Int. 2013;34(10):1427–1435. doi: 10.1177/1071100713491076. [DOI] [PubMed] [Google Scholar]
- 41.Seo HD, Kim MY, Choi JE, et al. Effects of Kinesio taping on joint position sense of the ankle. J Phys Ther Sci. 2016;28(4):1158–1160. doi: 10.1589/jpts.28.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fayson SD, Needle AR, Kaminski TW. The effects of ankle Kinesio taping on ankle stiffness and dynamic balance. Res Sports Med. 2013;21(3):204–216. doi: 10.1080/15438627.2013.792083. [DOI] [PubMed] [Google Scholar]
- 43.Fayson SD, Needle AR, Kaminski TW. The effect of ankle Kinesio tape on ankle muscle activity during a drop landing. J Sport Rehabil. 2015;24(4):391–397. doi: 10.1123/jsr.2014-0221. [DOI] [PubMed] [Google Scholar]
- 44.Williams S, Whatman C, Huma PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med. 2012;42(2):153–164. doi: 10.2165/11594960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 45.Mulligan BR. Manual Therapy: NAGS, SNAGS, MWMS, etc 6th ed. Wellington, NZ: Plane View Services, LTD; 2010. [Google Scholar]
- 46.Moiler K, Hall T, Robinson K. The role of fibular tape in the prevention of ankle injury in basketball: a pilot study. J Orthop Sports Phys Ther. 2006;36(9):661–668. doi: 10.2519/jospt.2006.2259. [DOI] [PubMed] [Google Scholar]
- 47.Curtis CK, Laudner KG, McLoda TA, McCaw ST. The role of shoe design in ankle sprain rates among collegiate basketball players. J Athl Train. 2008;43(3):230–233. doi: 10.4085/1062-6050-43.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guskiewicz KM, Perrin DH. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23(5):326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- 49.Hübscher M, Zech A, Pfeifer K, Hänsel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: a systematic review. Med Sci Sports Exerc. 2010;42(3):413–421. doi: 10.1249/MSS.0b013e3181b88d37. [DOI] [PubMed] [Google Scholar]
- 50.Gutierrez GM, Kaminski TW, Douex AT. Neuromuscular control and ankle instability. PM R. 2009;1(4):359–365. doi: 10.1016/j.pmrj.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 51.McKeon PO, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med. 2008;27(3):371–382. doi: 10.1016/j.csm.2008.02.004. viii. [DOI] [PubMed] [Google Scholar]
- 52.McKeon PO, Wikstrom EA. Sensory-targeted ankle rehabilitation strategies for chronic ankle instability. Med Sci Sports Exerc. 2016;48(5):776–784. doi: 10.1249/MSS.0000000000000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gehring D, Wissler S, Mornieux G, Gollhofer A. How to sprain your ankle—a biomechanical case report of an inversion trauma. J Biomech. 2013;46(1):175–178. doi: 10.1016/j.jbiomech.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 54.Lentell G, Katzman LL, Walters MR. The relationship between muscle function and ankle stability. J Orthop Sports Phys Ther. 1990;11(12):605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- 55.Beckman SM, Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch Phys Med Rehabil. 1995;76(12):1138–1143. doi: 10.1016/s0003-9993(95)80123-5. [DOI] [PubMed] [Google Scholar]
- 56.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing? J Athl Train. 2008;43(3):293–304. doi: 10.4085/1062-6050-43.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kollock R, Van Lunen BL, Ringleb SI, Oñate JA. Measures of functional performance and their association with hip and thigh strength. J Athl Train. 2015;50(1):14–22. doi: 10.4085/1062-6050-49.3.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Doherty C, Bleakley C, Hertel J, et al. Lower extremity coordination and symmetry patterns during a drop vertical jump task following acute ankle sprain. Hum Mov Sci. 2014;38:34–46. doi: 10.1016/j.humov.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 59.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 60.Wright CJ, Linens SW, Cain MS. A randomized controlled trial comparing rehabilitation efficacy in chronic ankle instability. J Sport Rehabil. 2017;26(4):238–249. doi: 10.1123/jsr.2015-0189. [DOI] [PubMed] [Google Scholar]
- 61.Emery CA, Meeuwisse WH. The effectiveness of a neuromuscular prevention strategy to reduce injuries in youth soccer: a cluster-randomised controlled trial. Br J Sports Med. 2010;44(8):555–562. doi: 10.1136/bjsm.2010.074377. [DOI] [PubMed] [Google Scholar]
- 62.Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008;36(6):1052–1060. doi: 10.1177/0363546508314432. [DOI] [PubMed] [Google Scholar]
- 63.LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 64.Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. doi: 10.1136/bmj.a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 66.Eils E, Schröter R, Schröder M, Gerss J, Rosenbaum D. Multistation proprioceptive exercise program prevents ankle injuries in basketball. Med Sci Sports Exerc. 2010;42(11):2098–2105. doi: 10.1249/MSS.0b013e3181e03667. [DOI] [PubMed] [Google Scholar]
- 67.Emery CA, Rose MS, McAllister JR, Meeuwisse WH. A prevention strategy to reduce the incidence of injury in high school basketball: a cluster randomized controlled trial. Clin J Sport Med. 2007;17(1):17–24. doi: 10.1097/JSM.0b013e31802e9c05. [DOI] [PubMed] [Google Scholar]
- 68.Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V. The FIFA 11+ program is effective in preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med. 2012;40(5):996–1005. doi: 10.1177/0363546512438761. [DOI] [PubMed] [Google Scholar]
- 69.Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 70.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wedderkopp N, Kaltoft M, Lundgaard B, Rosendahl M, Froberg K. Prevention of injuries in young female players in European team handball. A prospective intervention study. Scand J Med Sci Sports. 1999;9(1):41–47. doi: 10.1111/j.1600-0838.1999.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 72.Goodall RL, Pope RP, Coyle JA, Neumayer R. Balance and agility training does not always decrease lower limb injury risks: a cluster-randomised controlled trial. Int J Inj Contr Saf Promot. 2013;20(3):271–281. doi: 10.1080/17457300.2012.717085. [DOI] [PubMed] [Google Scholar]
- 73.Fu T, Wong AMK, Pei YC, Wu KP, Chou SW, Lin YC. Effect of kinesio taping on muscle strength in athletes: a pilot study. J Sci Med Sport. 2008;11(2):198–201. doi: 10.1016/j.jsams.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 74.Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50(24):1493–1495. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 75.Hubbard TJ, Hicks-Little CA. Ankle ligament healing after an acute ankle sprain: an evidence-based approach. J Athl Train. 2008;43(5):523–529. doi: 10.4085/1062-6050-43.5.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW. Collaborative Ankle Support Trial (CAST Group). Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. The Lancet. 2009;373(9663):575–581. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 77.Stirling AM, McBride JM, Merritt EK, Needle AR. Nervous system excitability and joint stiffness following short-term dynamic ankle immobilization. Gait Posture. 2018;59:46–52. doi: 10.1016/j.gaitpost.2017.09.028. [DOI] [PubMed] [Google Scholar]
- 78.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51(2):113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 79.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35(6):922–926. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]
- 80.Janssen KW, van Mechelen W, Verhagen EA. Bracing superior to neuromuscular training for the prevention of self-reported recurrent ankle sprains: a three-arm randomised controlled trial. Br J Sports Med. 2014;48(16):1235–1239. doi: 10.1136/bjsports-2013-092947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Janssen K, Van Den Berg A, Van Mechelen W, Verhagen E. User survey of 3 ankle braces in soccer, volleyball, and running: which brace fits best? J Athl Train. 2017;52(8):730–737. doi: 10.4085/1062-2050-52.4.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Van Reijen M, Vriend I, Zuidema V, van Mechelen W, Verhagen EA. Increasing compliance with neuromuscular training to prevent ankle sprain in sport: does the ‘Strengthen your ankle' mobile app make a difference? A randomised controlled trial. Br J Sports Med. 2016;50(19):1200–1205. doi: 10.1136/bjsports-2015-095290. [DOI] [PubMed] [Google Scholar]
- 83.Burcal CJ, Needle AR, Custer L, Rosen AB. The effects of cognitive loading on motor behavior in injured individuals: a systematic review. Sports Med. 2019 doi: 10.1007/s40279-019-01116-7. [DOI] [PubMed]
- 84.Grooms D, Appelbaum G, Onate J. Neuroplasticity following anterior cruciate ligament injury: a framework for visual-motor training approaches in rehabilitation. J Orthop Sports Phys Ther. 2015;45(5):381–393. doi: 10.2519/jospt.2015.5549. [DOI] [PubMed] [Google Scholar]
- 85.Rosen AB, Than NT, Smith WZ, et al. Attention is associated with postural control in those with chronic ankle instability. Gait Posture. 2017;54:34–38. doi: 10.1016/j.gaitpost.2017.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Needle AR, Rosen AB. Ligament injury changes brain function: now let's think about it. Athl Train Sports Health Care. 2017;9(5):198–199. [Google Scholar]