We thank Dott. Girleanu and coauthors for the comments and the interest in our article. We agree with the authors that patients with decompensated cirrhosis are a different population compared with patients with compensated liver disease (i.e., Child A class) when they develop portal vein thrombosis (PVT) (1). In fact, a recently published article that demonstrated that the occurrence of PVT does not influence the natural history of cirrhosis included only very stable patients with almost normal liver tests (2).
In this article, although the group of patients in Child C class was not very numerous, we were able to demonstrate for the first time that patients with cirrhosis with decompensated liver disease who do not resolve PVT are characterized by a higher risk of death at 2 years of follow-up; this was not the case in Child A patients.
This study was not interventional, and the therapeutic choice was left to the clinician's judgment. Actually, in the present cohort, the patients experienced the same number of bleeding episodes if PVT was not treated and during anticoagulation treatment, but significantly less after withdrawal of anticoagulation. We interpreted this finding in relation to the possible decrease in portal pressure in those who resolved PVT. The period of anticoagulation was shorter than that in the study by Villa et al. (3), and the dose was mostly therapeutic, which can justify the higher percentage of bleeding during treatment.
Moreover, the best therapeutic approach in patients with PVT and decompensated liver disease with severe portal hypertension may not be anticoagulation as first-line treatment in all the cases.
We agree that acute PVT is difficult to catch, especially in patients with cirrhosis, probably because collateralization of the splanchnic venous system is already present, and the acute occlusion of PVT may be less symptomatic in the short term. We agree with the authors that classification of the PVT should not be merely anatomical, but based on the chance of response to anticoagulation (4), underlying the stage of cirrhosis, presence or complications of portal hypertension, and eventual candidacy of the patient to liver transplant (5).
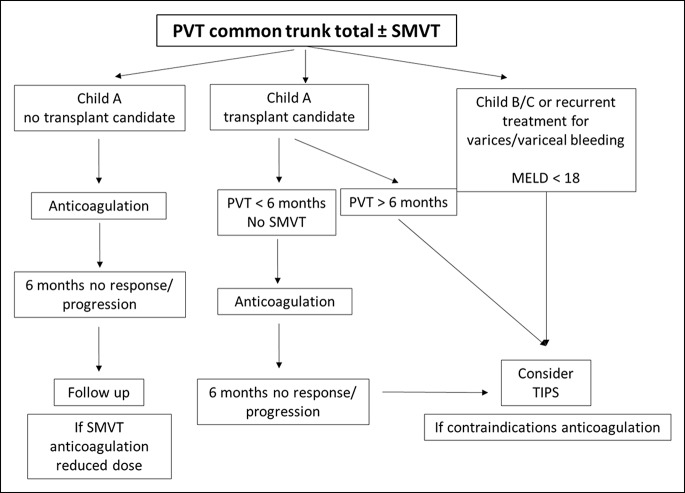
A new classification was recently proposed (6), which may be the base to create a treatment algorithm. Probably, a transjugular intrahepatic portosystemic shunt should be considered early in the course of PVT in some patients, in particular in liver transplant candidates. A proposal of treatment algorithm for complete PVT incorporating radiological intervention is represented in Figure 1.
Figure 1.
Treatment algorithm for complete PVT.
CONFLICTS OF INTEREST
Guarantor of the article: Marco Senzolo, MD, PhD.
Specific author contributions: All authors contributed to the letter.
Financial support: None.
Potential competing interests: None.
REFERENCES
- 1.Senzolo M. Liver: PVT in cirrhosis, not always an innocent bystander. Nat Rev Gastroenterol Hepatol 2015;12(1):11–3. [DOI] [PubMed] [Google Scholar]
- 2.Nery F, Chevret S, Condat B, et al. ; Groupe d'Etude et de Traitement du Carcinome Hépatocellulaire. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: Results of a longitudinal study. Hepatology 2015;61(2):660–7. [DOI] [PubMed] [Google Scholar]
- 3.Villa E, Cammà C, Marietta M, et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology 2012;143(5):1253–60.e4. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Castro KI, Vitale A, Fadin M, et al. A prediction model for successful anticoagulation in cirrhotic portal vein thrombosis. Eur J Gastroenterol Hepatol 2019;31:34–42. [DOI] [PubMed] [Google Scholar]
- 5.Zanetto A, Rodriguez-Kastro KI, Germani G, et al. Mortality in liver transplant recipients with portal vein thrombosis: An updated meta-analysis. Transpl Int 2018;31(12):1318–29. [DOI] [PubMed] [Google Scholar]
- 6.Sarin SK, Philips CA, Kamath PS, et al. Toward a comprehensive new classification of portal vein thrombosis in patients with cirrhosis. Gastroenterology 2016;151(4):574–77.e3. [DOI] [PubMed] [Google Scholar]