Abstract
Few studies have explored sexual orientation disparities in mental health and substance use outcomes among racial minorities. This study examined sexual orientation disparities in depression, suicidality, and substance use among Black American young people in the USA, and the mediating role of cyber and bias-based victimisation in accounting for these disparities. Secondary analyses were performed on data from a probability sample of young people (N = 1,129) collected in a school district in the south-eastern USA. Participants reported socio-demographics, depressive symptoms, suicidality, substance use, and experiences of bias-based and cyber victimisation. With some exceptions, Black participants who were lesbian, gay, bisexual, or mostly heterosexual reported higher rates of depression, suicidal ideation, suicide planning, and substance use than Black heterosexual participants. Black lesbian, gay, bisexual, and mostly heterosexual participants reported more cyber and bias-based victimisation than Black heterosexual participants. Sexual orientation disparities in mental health and, to some extent, substance use were partially explained by both forms of victimisation. Further research is needed address the role of bias-based and cyber victimisation in disparities in mental health and substance use among Black sexual minority young people. The present study carries implications for prevention and treatment efforts for racially diverse sexual minorities.
Keywords: sexual minority; Black; adolescents; youth; cyber victimisation; bias-based victimisation; depression; suicide; substance use, USA
Introduction
Sexual minority (e.g., lesbian, gay, bisexual and queer) young people report higher rates of depressive symptoms, suicidal ideation, and suicide attempts compared to their heterosexual peers (Marshal et al. 2011; Almeida et al. 2009). Reporting of substance use is also greater among sexual minority young people than their heterosexual counterparts (Marshal et al. 2008). Although prior research has highlighted important public health concerns, sexual orientation disparities in mental health and substance use among Black youth have not been sufficiently addressed. Limited research has indicated that Black sexual minority young people report higher levels of depression and suicidality compared to their Black heterosexual counterparts (Consolacion, Russell and Sue 2004; Bostwick et al. 2014). Black sexual minority young people also have higher rates of substance use compared to their Black heterosexual peers (Talley et al. 2014). In the light of this, this study explored sexual orientation disparities in mental health and substance use among Black young people and tested factors that may account for these inequities.
Victimisation and sexual orientation disparities in health
One factor that contributes to disparities in mental health and substance use is victimisation. Victimisation can take several forms, including in person and online (e.g., social media) (Slonje and Smith 2008), and can be general or bias-based (e.g., homophobic victimisation). Victimisation has been associated with increased depression, suicidality and substance use (Luk, Wang and Simons-Morton 2010; Geoffroy et al. 2016). Overall, sexual minority young people experience higher rates of victimisation than their heterosexual peers (Bouris et al. 2016).
As young people spend much of their day in digital spaces (e.g., social media, texting, computer use), it is perhaps not surprising that cyber victimisation has dramatically increased (Eaton and Elaine 2017). Experiences of cyber victimisation and online harassment are higher among sexual minorities compared to heterosexuals (GLSEN; Aboujaoude et al. 2015). Cyber victimisation is associated with poor mental health among sexual minority young people, including depression and suicidality (Cooper and Blumenfeld 2012; Abreu and Kenny 2018). In the youth population more generally, cyber victimisation is also associated with increased substance use (Fisher, Gardella and Teurbe-Tolon 2016). Therefore, it is plausible that sexual orientation disparities in mental health and substance use may be explained by cyber victimisation among Black young people.
In addition to general forms of victimisation, some young people experience bias-based forms of victimisation in which their identities or aspects of their lived experiences are targeted (e.g., gender, race and sexual orientation) (Seals and Young 2003; D’Augelli, Pilkington and Hershberger 2002). Bias-based victimisation may also take several forms, including in person and in cyber spaces (Rubin and McClelland 2015). Sexual minority young people report higher rates of bias-based victimisation, such as homophobic victimisation (i.e., verbal and physical harassment specific to their sexual orientation) compared to their heterosexual peers (Almeida et al. 2009; Savin-Williams 1994). These types of targeted victimisation experiences, which can be considered minority stressors, may be associated with adverse health outcomes above and beyond general stressors (Meyer 2003). Minority stressors lead to poor mental health and substance use through compromised stress pathways, such as maladaptive cognitions, emotional dysregulation and disrupted interpersonal processes (Hatzenbuehler 2009). Sexual minority young people are more likely to report bias-based victimisation specific to their gender than their heterosexual peers (Collier et al. 2013). Furthermore, given the higher prevalence of poor mental and physical health outcomes, they may also experience bias-based victimisation specific to their mental or physical status.
Black sexual minority young people may experience additional minority stressors or forms of bias-based victimisation specific to their marginalised and intersecting identities (Parks 2001; Pingel and Bauermeister 2018). Sexual minorities who are members of racial minorities may experience race- or language-based victimisation (Ryan 2003; Holmes and Cahill 2004). Minority stress and intersectionality frameworks suggest that these multiple and intersecting forms of bias-based victimisation may account for disparities among sexual minorities with multiple minority identities; however, researchers have yet to examine their effects. Furthermore, considering these multiple forms of victimisation as additive has produced mixed results in the research literature (Almeida et al. 2009; Consolacion, Russell and Sue 2004); thus, in this study we considered and combined multiple forms of bias-based victimisation without favouring one identity over another in understanding disparities.
Current study
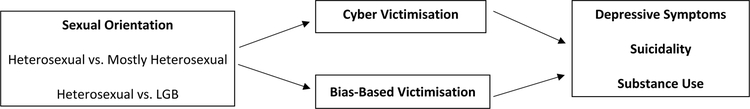
To our knowledge, no studies to date have tested the effects of cyber victimisation or multiple forms of bias-based victimisation in accounting for sexual orientation disparities in mental health and substance use for Black sexual minority young people in the USA. The present study therefore investigated sexual orientation disparities in mental health and substance use outcomes and tested whether cyber victimisation and bias-based victimisation account for these disparities among Black young people (see Figure 1). We hypothesised that Black sexual minority young people would have poorer mental health—specifically, greater depressive symptoms, suicidality, and substance use—compared to their heterosexual peers from similar racial and ethnic backgrounds. Given higher rates of cyber victimisation and bias-based victimisation among sexual minority young people, we also hypothesised that these forms of victimisation would uniquely account for disparities in depressive symptoms, suicidality and substance use among Black sexual minority young people.
Figure 1.
Conceptual model of the mediating effects of two types of victimisation on the associations between sexual orientation and mental health and substance use outcomes among Black young people.
Methods
Procedures
Secondary analyses were conducted using a dataset from the 2014 Youth Development Survey, a comprehensive cross-sectional survey of the primary school district of a large county in North Carolina in the USA using random cluster sampling. Survey covered topics included relationships, bullying, substance use, and health. The original study was approved by the University of Southern California’s institutional review board. More detailed procedures are described elsewhere (Goldbach, Mereish and Burgess 2017; Mereish et al. 2017).
Surveyed young people returned 4,259 surveys (94.5% response rate). Prior to modelling, the data were prepared and cleaned. Respondents who appeared dishonest or responded incorrectly to validity checks were removed. These included individuals who endorsed use of a fictitious drug, daztrex, reported 30-day but not lifetime use of any substance, or reported an age of substance initiation greater than their reported current age. Of the remaining, 187 surveys were returned blank, 238 did not report their sexual orientation, and 25 did not report their race and ethnicity and were removed. Due to the focus of our study on Black young people, the sub-sample of Black participants was selected for this study from the remaining data, which comprised a final analytic sample of 1,129 participants. Multiple imputation with chained equations was performed using IVEware (version 0.2) to create 20 datasets with no missing values for all outcome variables (Raghunathan et al. 2001).
Participants
Participants were 1,129 young people (51.7% female, 47.2% male, 1.1% transgender or other) who identified as straight or heterosexual (74.3%), mostly heterosexual (19.8%), bisexual (3.5%), mostly gay or lesbian (1.2%), or gay, lesbian, or homosexual (1.2%). They ranged in age from 10 years old or younger (0.1%), 11 (14.1%), 12 (11.2%), 13 (10.9%), 14 (8.9%), 15 (15.3%), 16 (13.1%), 17 (18.4%), to 18 (5.8%). The mode was 17 years of age, and 2.2% did not provide their age. Participants spanned several grades: sixth (26.2%; ages 11 to 12), eighth (21.6%; ages 13 to 14), 10th (27.8%; ages 15–16), and 12th (22.1%; ages 17 and older); 2.2% did not report their grade level.
Measures
Demographic and control variables.
Participants reported their age, gender, grade, race and ethnicity, and sexual orientation. Participants’ sexual orientation identity was assessed with one item (“How do you identify?”) with the following response options: straight or heterosexual; mostly straight; bisexual; mostly gay or lesbian; or gay, lesbian, or homosexual.
Depressive symptoms.
We assessed depressive symptoms using two measures: (a) the 10-item Center for Epidemiological Studies Depression Scale (CES-D-10) and (b) a 1-item depression measure. The CES-D-10 is a shortened version of the 20-item CES-D (Radloff 1977). Response options ranged from 0 = rarely or none of the time (less than 1 day) to 3 = all of the time (5–7 days), with scores ranging from 0 to 30. A cut-off score of 10 or higher indicates risk of clinical symptoms of depression (Andresen et al. 1994). The CES-D-10 has demonstrated good reliability with young people (Bradley, Bagnell and Brannen 2010) and in the present study (α = .71). Participants were also asked, “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some of your usual activities?” Response options were no or yes, coded as 0 and 1, respectively.
Suicidality.
We assessed two domains of suicidality: suicidal ideation and suicide planning during the past year. Suicidal ideation was assessed by asking: “During the past 12 months did you ever seriously consider attempting suicide?” Suicide planning was assessed by asking: “During the past 12 months, did you make a plan about how you would attempt suicide?” Response options were no or yes, coded as 0 and 1, respectively.
Substance use.
Participants indicated whether they had smoked cigarettes in their lifetime (lifetime use) and the past 30 days (recent use). Response choices were: never, once or twice, once in a while but not regularly, or regularly. Participants were also asked if in their lifetime and the past 30 days they had “drank one or more drinks of alcohol,” “used marijuana or hashish,” and “used prescription drugs not prescribed.” Response choices were 0, 1 or 2, 3–5, 6–9, or 10+ times. Response choices were dichotomised as 0 (never) and 1 (once or more). The substance use variables were coded as 0 (no use) or 1 (use).
Cyber victimisation.
Experiences of cyber victimisation were assessed with one item: “During the past 12 months, how often have you been electronically bullied by someone? (Include being bullied through e-mail, chat rooms, instant messaging, websites, or texting).” Response options ranged from never to every day, coded from 0 to 4, respectively. For descriptive purposes, response options were recoded as 0 (never) and 1 (experienced cyber victimisation), but the continuous item was included in the main analyses.
Bias-based victimisation.
Experiences with bias-based victimisation were assessed with one question: “During the past 12 months, how often were you bullied for any of the following reasons?” They received the following seven reasons for being bullied: race, ethnicity, or national origin; religion; gender; because you are gay, lesbian, or bisexual, or someone thought you were; a physical or mental disability; because of your language or accent; and any other reason. Because it is unclear if the “any other reason” option was bias specific, we did not include it in our study. Response options ranged from never to every day, coded from 0 to 4, respectively. The scale demonstrated good reliability in the present study (α = .71). For descriptive purposes, response options were recoded as 0 (never) and 1 (experienced victimisation) for each type of bias-based victimisation. A sum score of all six reasons was computed to represent an index of multiple forms of bias-based victimisation, and the index was included in the main analyses.
Analytic plan
Descriptive and regression analyses were conducted using IBM SPSS Statistics 25. Sexual orientation was coded into three groups: (a) heterosexual (n = 839), (b) mostly heterosexual (n = 224) and (c) bisexual, mostly gay or lesbian, or gay, lesbian, or homosexual (LGB; n = 66). Because too few participants identified as lesbian or gay, they were aggregated with bisexual participants. For all analyses, the reference group was heterosexual participants, coded as 0, and the target group were sexual minorities (mostly heterosexual or LGB), coded as 1. Similarly, due to few participants who identified as a sexual minority, we also aggregated across genders. Furthermore, due to the low prevalence of recent and lifetime substance for each of the substance, we computed a substance use variable indicating any recent or lifetime substance use rather than use of a specific substance (e.g., alcohol).
We first conducted a multivariate analysis of variance to test for sexual orientation and gender differences in bias-based and cyber victimisation. We conducted logistic regression analyses to examine differences between Black heterosexual and Black sexual minority young people (mostly heterosexual or LGB) in their likelihood of reporting depressive symptoms, suicidal ideation, suicide plans, and recent and lifetime substance use. Regression analyses accounted for age, grade and gender. We then used multiple mediation models to test the relationships among sexual orientation (heterosexual versus mostly heterosexual; heterosexual versus LGB), mediators (cyber and bias-based victimisation), and mental health and substance use outcomes, while accounting for socio-demographics. The mediation models tested sexual orientation and sociodemographic variables in Step 1 and the two victimisation mediators in Step 2; as such, the mediators were tested concurrently. The PROCESS macro (Hayes 2013) as used to conduct a bias-corrected bootstrapping procedure using 1,000 samples with 95% confidence intervals and to obtain indirect effects to test for mediation.
Results
Depressive symptoms, suicidality, substance use, and victimisation
As reported in Table 1, the highest rates of depressive symptoms, suicidality, and substance use were reported by LGB participants, followed by mostly heterosexual and then heterosexual participants. LGB participants also reported the highest rates of bias-based victimisation, followed by mostly heterosexual and then heterosexual participants. LGB and mostly heterosexual participants reported comparable rates of cyber victimisation, and both sexual minority groups reported more cyber victimisation than heterosexual participants.
Table 1.
Sample demographic characteristics
| Total | Heterosexual | Mostly Heterosexual | LGB | |
|---|---|---|---|---|
| (N = 1,129) | (n = 839) | (n = 224) | (n = 66) | |
| % (n) | % (n) | % (n) | % (n) | |
| Gender | ||||
| Male | 47.2 (522) | 46.6 (382) | 48.0 (106) | 53.1 (34) |
| Female | 51.7 (571) | 52.7 (432) | 50.2 (111) | 43.8 (28) |
| Transgender | 1.1 (12) | 0.8 (6) | 1.8 (4) | 3.1 (2) |
| Grade | ||||
| 6 | 26.2 (296) | 27.7 (227) | 28.2 (62) | 10.9 (7) |
| 8 | 21.6 (244) | 21.3 (175) | 25.9 (57) | 18.8 (12) |
| 10 | 27.8 (314) | 28.5 (234) | 25.0 (55) | 39.1 (25) |
| 12 | 22.1 (250) | 22.4 (184) | 20.9 (46) | 31.3 (20) |
| Depression | ||||
| CES-D-10 | 32.1 (362) | 28.4 (238) | 38.8 (87) | 56.1 (37) |
| Sad or hopeless | 28.1 (317) | 24.2 (203) | 34.4 (77) | 56.1 (37) |
| Suicidality | ||||
| Ideation | 13.6 (153) | 11.2 (94) | 15.2 (34) | 37.9 (25) |
| Plan | 10.6 (120) | 8.2 (69) | 12.5 (28) | 34.8 (23) |
| Cigarettes | ||||
| Recent | 4.1 (46) | 3.5 (29) | 5.4 (12) | 7.7 (5) |
| Lifetime | 12.7 (143) | 10.8 (91) | 13.8 (31) | 31.8 (21) |
| Alcohol | ||||
| Recent | 8.9 (100) | 8.6 (72) | 6.3 (14) | 21.2 (14) |
| Lifetime | 29.6 (334) | 28.4 (238) | 25.4 (57) | 59.1 (39) |
| Marijuana | ||||
| Recent | 9.9 (112) | 9.1 (76) | 7.6 (17) | 28.8 (19) |
| Lifetime | 20.5 (231) | 18.6 (156) | 18.8 (42) | 50.0 (33) |
| Prescription drugs | ||||
| Recent | 3.2 (36) | 2.7 (23) | 3.1 (7) | 9.1 (6) |
| Lifetime | 7.6 (86) | 6.9 (58) | 6.3 (14) | 21.2 (14) |
| Substance use | ||||
| Recent | 16.3 (184) | 14.9 (125) | 16.1 (36) | 34.8 (23) |
| Lifetime | 37.1 (419) | 35.0 (294) | 35.3 (79) | 69.7 (46) |
| Bias-based victimisation | ||||
| Race and ethnicity | 16.3 (184) | 15.1 (127) | 20.1 (45) | 18.2 (12) |
| Religion | 7.5 (85) | 7.0 (59) | 9.4 (21) | 7.6 (5) |
| Gender | 7.9 (89) | 6.3 (53) | 12.5 (28) | 12.1 (8) |
| LGB | 10.9 (123) | 6.9 (58) | 16.1 (36) | 43.9 (29) |
| Disability | 5.6 (63) | 4.4 (37) | 9.4 (21) | 7.6 (5) |
| Language and accent | 11.9 (134) | 10.1 (85) | 17.9 (40) | 13.6 (9) |
| Cyber victimisation | 15.9 (179) | 13.5 (113) | 22.8 (51) | 22.7 (15) |
| Bias-based victimisation | 27.6 (312) | 23.4 (196) | 35.3 (79) | 56.1 (37) |
Note. LGB = lesbian, gay, or bisexual.
Associations among sexual orientation, mental health, and substance use
The results of the logistic regression analyses indicated that after accounting for sociodemographic characteristics, mostly heterosexual participants had higher odds than heterosexual participants of depressive symptoms, suicidality and recent substance use, but not lifetime substance use. Results are presented in Table 2 (see Step 1). After accounting for sociodemographic characteristics, LGB participants had higher odds than heterosexual participants of depressive symptoms, suicidality and recent and lifetime substance use. The results are presented in Table 2 (see Step 1).
Table 2.
Logistic regression analysis of depression, suicidality, and substance use outcomes among heterosexual, mostly heterosexual, and LGB Black young people.
| CES-D-10 | Sad or Hopeless | CES-D-10 | Sad or Hopeless | ||
|---|---|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | ||
| Step 1 | Step 1 | ||||
| H vs MH | 1.63 (1.19, 2.22)** | 1.61 (1.17, 2.22)** | H vs LGB | 3.06 (1.81, 5.16)*** | 3.62 (2.14, 6.13)*** |
| Step 2 | Step 2 | ||||
| H vs MH | 1.37 (0.98, 1.91) | 1.36 (0.97, 1.92) | H vs LGB | 2.40 (1.37, 4.19)** | 2.90 (1.67, 5.02)*** |
| Cyber. | 1.87 (1.49, 2.35)*** | 1.72 (1.39, 2.14)*** | Cyber | 1.95 (1.51, 2.52)*** | 1.54 (1.22, 1.95)*** |
| Bias-based | 1.42 (1.27, 1.59)*** | 1.40 (1.25, 1.56)*** | Bias-based | 1.46 (1.27, 1.67)*** | 1.45 (1.27, 1.66)*** |
| Suicidal Ideation | Suicide Plan | Suicidal Ideation | Suicide Plan | ||
| Step 1 | Step 1 | ||||
| H vs MH | 1.42 (0.92, 2.18) | 1.65 (1.03, 2.64)* | H vs LGB | 4.41 (2.52, 7.73)*** | 5.85 (3.26, 10.49)*** |
| Step 2 | Step 2 | 3.70 (2.05, 6.68)*** | 4.78 (2.59, 8.82)*** | ||
| H vs MH | 1.22 (0.78, 1.91) | 1.36 (0.83, 2.23) | H vs LGB | ||
| Cyber | 1.63 (1.30, 2.04)*** | 1.44 (1.12, 1.85)** | Cyber | 1.73 (1.35, 2.20)*** | 1.49 (1.14, 1.95)** |
| Bias-based | 1.24 (1.10, 1.41)** | 1.40 (1.23, 1.59)*** | Bias-based | 1.14 (0.98, 1.34) | 1.30 (1.10, 1.53)** |
| Recent Substance Use | Lifetime Substance Use | Recent Substance Use | Lifetime Substance Use | ||
| Step 1 | Step 1 | ||||
| H vs MH | 1.20 (0.79, 1.81) | 1.04 (0.75, 1.43) | H vs LGB | 2.53 (1.43, 4.46)** | 3.39 (1.93, 5.94)*** |
| Step 2 | Step 2 | ||||
| H vs MH | 1.09 (0.72, 1.67) | 0.99 (0.72, 1.37) | H vs LGB | 2.21 (1.23, 3.96)** | 3.18 (1.80, 5.63)*** |
| Cyber | 1.10 (0.85, 1.42) | 1.06 (0.86, 1.30) | Cyber | 0.96 (0.72, 1.29) | 1.10 (0.88, 1.38) |
| Bias-based | 1.22 (1.08, 1.39)** | 1.10 (0.99, 1.23) | Bias-based | 1.29 (1.11, 1.50)** | 1.08 (0.95, 1.23) |
Note. H vs MH = heterosexual vs. mostly heterosexual; H vs LGB = heterosexual vs. lesbian, gay, or bisexual; cyber = cyber victimisation; bias-based = bias-based victimisation; AOR = adjusted odds ratio; CI = confidence interval.
p < .05.
p < .01.
p < .001.
Accounting for socio-demographics and sexual orientation, results in Table 2 (see Step 2) demonstrate that cyber and bias-based victimisation were associated with more depressive symptoms, suicidality, and substance use among all participants. However, there were some inconsistent associations between victimisation and suicidal ideation and recent and lifetime substance use.
Mediation results
Depression outcomes.
Cyber and bias-based victimisation had significant mediation effects on the association between sexual orientation (heterosexual versus mostly heterosexual and heterosexual versus LGB) and both depression outcomes (see Table 3 for indirect effects).
Table 3.
Mediation of cyber and bias-based victimisation on sexual orientation disparities in depressive symptoms, suicidality, and substance use among Black young people.
| H v. MH | H vs. LGB | |||
|---|---|---|---|---|
| b (SE) | CI | b (SE) | CI | |
| CES-D-10 | ||||
| Cyber | .07 (.04) | .015, .154 | .18 (.09) | .048, .421 |
| Bias based | .13 (.04) | .059, .234 | .22 (.08) | .101, .455 |
| Sad or hopeless | ||||
| Cyber | .06 (.03) | .011, .153 | .11 (.07) | .026, .292 |
| Bias based | .12 (.04) | .057, .222 | .22 (.07) | .095, .389 |
| Suicidal ideation | ||||
| Cyber | .06 (.03) | .009, .129 | .14 (.08) | .024, .327 |
| Bias based | .08 (.04) | .021, .163 | .08 (05) | −.011, .209 |
| Suicide plan | ||||
| Cyber | .04 (.03) | .003, .110 | .11 (.07) | .015, .288 |
| Bias based | .12 (.05) | .044, .244 | .16 (.06) | .049, .308 |
| Recent substance use | ||||
| Cyber | .01 (.02) | −.014, .053 | −.01 (.05) | −.135, .064 |
| Bias based | .07 (.03) | .020, .156 | .15 (.07) | .041, .294 |
| Lifetime substance use | ||||
| Cyber | .01 (.01) | −.018, .045 | .03 (.04) | −.025, .130 |
| Bias based | .04 (.02) | .000, .094 | .05 (.05) | −.031, .154 |
Note. H = heterosexual; MH = mostly heterosexual; LBG = lesbian, gay, or bisexual; b = unstandardised beta; CI = confidence interval.
Suicidality outcomes.
Cyber and bias-based victimisation had significant mediation effects on sexual orientation (heterosexual versus mostly heterosexual) and both suicidal ideation and suicide planning. For models comparing heterosexual and LGB participants, cyber victimisation had significant mediation effects on the relationships between sexual orientation (heterosexual versus LGB) and both suicidality outcomes. However, bias-based victimisation had significant mediation effects for suicidal planning but not suicidal ideation.
Substance use outcomes.
Bias-based victimisation had significant mediation effects on the association between sexual orientation (heterosexual vs. mostly heterosexual) and recent substance use, but not lifetime substance use. Cyber victimisation did not have significant mediation effects on the relationship between sexual orientation and either substance use outcome. For models comparing LGB and heterosexual participants, bias-based victimisation had a significant mediation effect on sexual orientation and recent substance use, but cyber victimisation did not. Cyber and bias-based victimisation did not have significant meditation effects on the relationship between sexual orientation and lifetime substance use.
Discussion
To our knowledge, this is the first study to document sexual orientation disparities in depressive symptoms, suicidality and substance use in a large sample of Black young people. We explored whether cyber and bias-based victimisation may account for these disparities. With some exceptions for mostly heterosexual participants, we found that Black sexual minority young people had higher rates of depressive symptoms, suicidal ideation, suicide plans and recent and lifetime substance use than their heterosexual counterparts. We also documented higher rates of cyber and bias-based victimisation among sexual minority participants compared to their heterosexual peers. Additionally, our results indicate that disparities in depressive symptoms and suicidality and, to some extent, substance use can be explained through Black sexual minority young people’s increased risk of both forms of victimisation. These findings have implications for minority stress theory, research and clinical intervention among Black sexual minority young people.
Our findings document high rates of depressive symptomology and suicidality among all young people in the sample, but in particular among Black sexual minority youth, with Black LGB participants exhibiting the highest rates (over half reported depressive symptoms and over a third reported suicidality). Elevated rates of recent and lifetime substance among LGB participants were also documented in our sample, but less so for mostly heterosexual participants. Mostly heterosexual participants were not at higher risk of recent or lifetime substance use compared to heterosexual participants. Our results are noteworthy because there is a dearth of research documenting sexual orientation disparities among Black young people. They are also important because research is limited regarding the experiences of mostly heterosexual young people (Balsam et al. 2015). Future research needs to examine the heterogeneity of sexual orientation identification among Black young people and its association with differing elevated rates of health risks.
Black sexual minority young people were significantly more likely than their Black heterosexual peers to experience bias-based victimisation. Our findings also document that multiple forms of bias-based victimisation are associated with more depressive symptoms and suicidality, and to some extent more substance use. This is consistent with the literature documenting the negative effects of homophobic victimisation on both sexual minority and heterosexual young people’s mental health (Poteat et al. 2014; Poteat et al. 2011). We also found that bias-based victimisation partially accounted for sexual orientation disparities in depressive symptoms and suicidality, but less so for disparities in substance use. Our results build on the existing literature, which has primarily focused on homophobic victimisation, to document the effects of other forms of bias-based victimisation for Black young people. Bias-based victimisation may have deleterious effects on mental health and contribute to substance use through compromised minority stress processes, such as maladaptive cognitions, emotional dysregulation, or social isolation (Hatzenbuehler 2009; Mereish and Poteat 2015). Given that these are all health risk factors, future research should examine mechanisms in the associations between bias-based victimisation and sexual minorities’ increased risk of negative health outcomes.
These findings are novel in terms of underscoring the negative effects of cyber victimisation. We found that Black sexual minority young people experience higher rates of cyber victimisation than their heterosexual peers. Moreover, cyber victimisation was associated with greater depression symptoms, suicidality and to some extent substance use for most participants, regardless of sexual orientation. This builds on limited literature documenting the negative effects of cyber victimisation on both sexual minority and heterosexual peers’ mental health (Sinclair et al. 2012). We also found that cyber victimisation accounted for sexual orientation disparities in mental health but not substance use. Because the digital space provides young people with anonymity, it is plausible that they feel freer to act on their biases and stigmatising attitudes and target individuals with minority identities. As young people become more digitally connected, future research and interventions should focus on the role of cyber victimisation in sexual minorities’ health.
Bias-based victimisation, but not cyber victimisation, was associated with more recent substance use and partially accounted for sexual orientation disparities in substance use. This may be an artefact of reduced statistical power. Alternatively, research has shown that Black young people develop resilience resources due to their experiences of racism (Dupree, Spencer and Spencer 2015), which may allow them to cope with victimisation in the context of substance use. It is also plausible that Black young people have differing social norms around substance use or motives to use substances (Zapolski et al. 2014; Terry-McElrath, O’Malley and Johnston 2009); thus, they may not use substances to cope with victimisation. Moreover, increased substance use may be a distal health outcome for victimisation that unfolds over time among Black sexual minorities, which might explain the inconsistent associations; victimisation may be internalised more proximally and quickly and result in increased depressive symptoms and suicidality among sexual minority young people. Future research should examine these issues as well as avenues of resilience among sexual minority young people of colour (Schmitz, Sanchez and Lopez 2018).
Limitations
Although this study makes a number of novel contributions, several limitations need considering. The cross-sectional design limited the causal and temporal understanding of the relationships between victimisation and our outcomes. For example, it is also plausible that participants who are feeling suicidal or depressed may go online but might end up experiencing cyber victimisation. Longitudinal research is needed to test how multiple forms of victimisation may lead to sexual orientation disparities across developmental trajectories in adolescence. Due to the small subgroups of participants (e.g., specific gender groups, participants who identified as lesbian or gay), we aggregated several subgroups into larger groups. This limited understanding of nuances and sensitivity to the varying genders and sexual orientations of sexual minority young people and limited the generalisability of our results to many of these subgroups. Our analyses were not clustered at the school level; future research should consider the effects of school differences in understanding the documented disparities.
The measures used in this study also had limitations. Specifically, the cyber victimisation measure was only one item; therefore, it did not comprehensively assess types of cyber victimisation and whether cyber victimisation was more generic or targeted (i.e., bias based). This limitation might have led to potential overlap between cyber and bias-based victimisation. Additionally, neither victimisation measure assessed appraisals of the experience or the source or context of the victimisation. Future research should identify the source, context, and content of victimisation as well as the individuals’ appraisals of the victimisation (e.g., intensity) and coping responses. These factors are essential to informing prevention efforts and clinical interventions. Although we had multiple measures of depressive symptoms and suicidality, similar to national health surveys of youth and young people, future research should examine more comprehensive and diagnostic criteria of these mental health concerns. Similarly, due to limited frequency of differing forms of recent and lifetime substance (i.e., tobacco, alcohol, marijuana and prescription drugs) in our sample, we had to compute an index of overall substance use. Future research is needed to examine disparities and effects of victimisation on differing substances.
Conclusion
Our findings document sexual orientation disparities in depressive symptoms, suicidality and substance use among Black young people, with alarmingly high rates of poor mental health outcomes among Black sexual minority youth. These disparities can be explained in part by multiple forms of minority stress (e.g., multiple forms of bias-based victimisation) and general victimisation (e.g., cyber victimisation). Given the high rates of depression, suicide, and substance use among Black sexual minority young people and lack of empirically tested interventions, it is important to develop culturally informed interventions and clinical care for Black sexual minorities. Structural and systematic interventions that target multiple forms of oppression are needed to address disparities for Black sexual minority young people. Clinical research should engage with the unique experiences of sexual minorities belonging to multiple minority groups to develop culturally affirming interventions for Black sexual minority young people. Moreover, given the role of cyber victimisation in the lives of young people, future research and interventions should target and help decrease cyber victimisation and generate digital interventions to help those affected to cope with these experiences.
Acknowledgements
Ethan Mereish was supported in part by a grant from the US National Institutes of Health under Grant K08-AA025011.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- Aboujaoude Elias, Savage Matthew W., Starcevic Vladan, and Salame Wael O.. 2015. “Cyberbullying: Review of an Old Problem Gone Viral.” Journal of Adolescent Health 57 (1): 10–8. [DOI] [PubMed] [Google Scholar]
- Abreu Roberto L., and Kenny Maureen C.. 2018. “Cyberbullying and LGBTQ Youth: A Systematic Literature Review and Recommendations for Prevention and Intervention.” Journal of Child & Adolescent Trauma 11 (1): 81–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida Joanna, Johnson Renee M., Corliss Heather L., Molnar Beth E., and Azrael Deborah. 2009. “Emotional Distress among LGBT Youth: The Influence of Perceived Discrimination Based on Sexual Orientation.” Journal of Youth and Adolescence 38 (7): 1001–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen Elena M., Judith A Malmgren William B. Carter, and Patrick Donald L.. 1994. “Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D.” American Journal of Preventive Medicine 10: 77–84. [PubMed] [Google Scholar]
- Balsam Kimberly F., Molina Yamile, Blayney Jessica A., Dillworth Tiara, Zimmerman Lindsey, and Kaysen Debra. 2015. “Racial/Ethnic Differences in Identity and Mental Health Outcomes among Young Sexual Minority Women.” Cultural Diversity and Ethnic Minority Psychology 21 (3): 380–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick Wendy B., Meyer Ilan, Aranda Frances, Russell Stephen, Hughes Tonda, Birkett Michelle, and Mustanski Brian. 2014. “Mental Health and Suicidality among Racially/Ethnically Diverse Sexual Minority Youths.” American Journal of Public Health 104 (6): 1129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouris Alida, Everett Bethany G., Heath Ryan D., Elsaesser Caitlin E., and Neilands Torsten B.. 2016. “Effects of Victimization and Violence on Suicidal Ideation and Behaviors among Sexual Minority and Heterosexual Adolescents.” LGBT Health 3 (2): 153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley Kristina L., Bagnell Alexa L, and Brannen Cyndi L.. 2010. “Factorial Validity of the Center for Epidemiological Studies Depression 10 in Adolescents.” Issues in Mental Health Nursing 31 (6): 408–12. [DOI] [PubMed] [Google Scholar]
- Collier Kate L., Gabriël van Beusekom, Henny M.W. Bos, and Theo G.M. Sandfort. 2013. “Sexual Orientation and Gender Identity/Expression Related Peer Victimization in Adolescence: A Systematic Review of Associated Psychosocial and Health Outcomes.” Journal of Sex Research 50 (3–4): 299–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolacion Theodora B., Russell Stephen T., and Sue Stanley. 2004. “Sex, Race/Ethnicity, and Romantic Attractions: Multiple Minority Status Adolescents and Mental Health.” Cultural Diversity and Ethnic Minority Psychology 10 (3): 200–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Robyn M., and Blumenfeld Warren J.. 2012. “Responses to Cyberbullying: A Descriptive Analysis of the Frequency of and Impact on LGBT and Allied youth.” Journal of LGBT Youth 9 (2): 153–77. [Google Scholar]
- D’Augelli Anthony R., Pilkington Neil W., and Hershberger Scott L.. 2002. “Incidence and Mental Health Impact of Sexual Orientation Victimization of Lesbian, Gay, and Bisexual Youths in High School.” School Psychology Quarterly 17 (2): 148–67. [Google Scholar]
- Dupree Davido, Spencer Tirzah R., and Beale Spencer Margaret. 2015. “Stigma, Stereotypes and Resilience Identities: The Relationship between Identity Processes and Resilience Processes among Black American Adolescents.” In Youth Resilience and Culture, edited by Theron Linda, Liebenberg Linda, and Ungar Michael, 117–129. Dordrecht: Springer. [Google Scholar]
- Eaton Sarah E. 2017. “Cyberbullying among Children and Teens: A Pervasive Global Issue.” Calgary: University of Calgary. [Google Scholar]
- Fisher Benjamin W., Gardella Joseph H., and Teurbe-Tolon Abbie R.. 2016. “Peer Cybervictimization among Adolescents and the Associated Internalizing and Externalizing Problems: a Meta-analysis.” Journal of Youth and Adolescence 45 (9): 1727–1743. [DOI] [PubMed] [Google Scholar]
- Geoffroy Marie-Claude, Boivin Michel, Arseneault Louise, Turecki Gustavo, Vitaro Frank, Brendgen Mara, Renaud Johanne, Séguin Jean R., Tremblay Richard E., and Côté Sylvana M.. 2016. “Associations between Peer Victimization and Suicidal Ideation and Suicide Attempt During Adolescence: Results from a Prospective Population-based Birth Cohort.” Journal of the American Academy of Child & Adolescent Psychiatry 55 (2): 99–105. [DOI] [PubMed] [Google Scholar]
- GLSEN, CiPHR, and CCRC. (2013) Out Online: The Experiences of Lesbian, Gay, Bisexual and Transgender Youth on the Internet. New York: GLSEN. [Google Scholar]
- Goldbach Jeremy T., Mereish Ethan H., and Burgess Claire. 2017. “Sexual Orientation Disparities in the Use of Emerging Drugs.” Substance Use & Misuse 52 (2): 265–271. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler Mark L. 2009. “How Does Sexual Minority Stigma “Get Under the Skin”? A Psychological Mediation Framework.” Psychological bulletin 135 (5): 707–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes Andrew F. 2013. “PROCESS Macro Package for SPSS.” Retrieved on February 10, 2013 from: http://www.processmacro.org
- Holmes Sarah E., and Cahill Sean. 2004. “School Experiences of Gay, Lesbian, Bisexual and Transgender Youth.” Journal of Gay & Lesbian Issues in Education 1 (3): 53–66. [Google Scholar]
- Luk Jeremy W., Wang Jing, and Simons-Morton Bruce G.. 2010. “Bullying Victimization and Substance Use among US Adolescents: Mediation by Depression.” Prevention Science 11 (4): 355–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal Michael P., Dietz Laura J., Friedman Mark S., Stall Ron, Smith Helen A., James McGinley Brian C. Thoma, Murray Pamela J., D’Augelli Anthony R., and Brent David A.. 2011. “Suicidality and Depression Disparities between Sexual Minority and Heterosexual Youth: A Meta-Analytic Review.” Journal of Adolescent Health 49 (2): 115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal Michael P., Friedman Mark S., Stall Ron, King Kevin M., Miles Jonathan, Gold Melanie A., Bukstein Oscar G., and Morse Jennifer Q.. 2008. “Sexual Orientation and Adolescent Substance Use: A Meta‐analysis and Methodological Review.” Addiction 103 (4): 546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish Ethan H., and Paul Poteat V. 2015. “A Relational Model of Sexual Minority Mental and Physical Health: The Negative Effects of Shame on Relationships, Loneliness, and Health.” Journal of Counseling Psychology 62 (3): 425–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish Ethan H., Goldbach Jeremy T., Burgess Claire, and DiBello Angelo M.. 2017. “Sexual Orientation, Minority Stress, Social Norms, and Substance Use among Racially Diverse Adolescents.” Drug and Alcohol Dependence 178: 49–56. doi: 10.1016/j.drugalcdep.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer Ilan H. 2003. “Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence.” Psychological Bulletin 129 (5): 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks Carlton W. 2001. “African-American Same-gender-loving Youths and Families in Urban Schools.” Journal of Gay & Lesbian Social Services 13 (3): 41–56. [Google Scholar]
- Pingel Emily S., and Bauermeister José A.. 2018. “‘Church Hurt can be the Worst Hurt’: Community Stakeholder Perceptions of the Role of Black Churches in HIV Prevention among Young Black Gay and Bisexual Men.” Culture, Health & Sexuality 20 (2): 218–31. doi: 10.1080/13691058.2017.1338756. [DOI] [PubMed] [Google Scholar]
- Poteat V. Paul, Mereish Ethan H., DiGiovanni Craig D., and Koenig Brian W.. 2011. “The Effects of General and Homophobic Victimization on Adolescents’ Psychosocial and Educational Concerns: The Importance of Intersecting Identities and Parent support.” Journal of Counseling Psychology 58 (4): 597–609. [DOI] [PubMed] [Google Scholar]
- Poteat V. Paul, Scheer Jillian R., DiGiovanni Craig D., and Mereish Ethan H.. 2014. “Short-term Prospective Effects of Homophobic Victimization on the Mental Health of Heterosexual Adolescents.” Journal of Youth and Adolescence 43 (8): 1240–1251. [DOI] [PubMed] [Google Scholar]
- Radloff Lenore Sawyer. 1977. “The CES-D Scale: A Self-Report Depression Scale for Research in the General Population.” Applied Psychological Measurement 1 (3): 385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Raghunathan TE, Lepkowski JM, Van Hoewyk J, and Solenberger P. 2001. “A Multivariate Technique for Multiply Imputing Missing Values using a Sequence of Regression Models.” Survey Methodology 27: 85–96. [Google Scholar]
- Rubin Jennifer D., and McClelland Sara I.. 2015. “‘Even Though it’s a Small Checkbox, It’s a Big Deal’: Stresses and Strains of Managing Sexual Identity(s) on Facebook.” Culture, Health & Sexuality 17 (4): 512–526. doi: 10.1080/13691058.2014.994229. [DOI] [PubMed] [Google Scholar]
- Ryan Caitlin. 2003. “Lesbian, Gay, Bisexual, and Transgender Youth: Health Concerns, Services, and Care.” Clinical Research and Regulatory Affairs 20 (2): 137–158. [Google Scholar]
- Savin-Williams Ritch C. 1994. “Verbal and Physical Abuse as Stressors in the Lives of Lesbian, Gay Male, and Bisexual Youths: Associations with School Problems, Running Away, Substance Abuse, Prostitution, and Suicide.” Journal of Consulting and Clinical Psychology 62 (2): 261–269. [DOI] [PubMed] [Google Scholar]
- Schmitz Rachel M., Sanchez Julissa, and Lopez Bianca. 2018. “LGBTQ+ Latinx Young Adults’ Health Autonomy in Resisting Cultural Stigma.” Culture, Health & Sexuality: 1–15. doi: 10.1080/13691058.2018.1441443. [DOI] [PubMed] [Google Scholar]
- Seals Dorothy, and Young Jerry. 2003. “Bullying and Victimization: Prevalence and Relationship to Gender, Grade Level, Ethnicity, Self-esteem, and Depression.” Adolescence 38 (152): 735–747. [PubMed] [Google Scholar]
- Sinclair Katerina O., Bauman Sheri, Paul Poteat V, Koenig Brian, and Russell Stephen T.. 2012. “Cyber and Bias-based Harassment: Associations with Academic, Substance Use, and Mental Health Problems.” Journal of Adolescent Health 50 (5): 521–523. [DOI] [PubMed] [Google Scholar]
- Slonje Robert, and Smith Peter K.. 2008. “Cyberbullying: Another Main Type of Bullying?” Scandinavian Journal of Psychology 49 (2): 147–54. [DOI] [PubMed] [Google Scholar]
- Talley Amelia E., Hughes Tonda L., Aranda Frances, Birkett Michelle, and Marshal Michael P.. 2014. “Exploring Alcohol-use Behaviors among Heterosexual and Sexual Minority Adolescents: Intersections with Sex, Age, and Race/Ethnicity.” American Journal of Public Health 104 (2): 295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath Yvonne M., O’Malley Patrick M., and Johnston Lloyd D.. 2009. “Reasons for Drug Use among American Youth by Consumption Level, Gender, and Race/Ethnicity: 1976–2005.” Journal of Drug Issues 39 (3): 677–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski Tamika C.B., Sarah L. Pedersen, Denis M. McCarthy, and Gregory T. Smith. 2014. “Less Drinking, Yet More Problems: Understanding African American Drinking and Related Problems.” Psychological Bulletin 140 (1): 188–223. [DOI] [PMC free article] [PubMed] [Google Scholar]