Abstract
Background
Alcohol and other drug (AOD) problems are commonly depicted as chronically relapsing, implying multiple recovery attempts are needed prior to remission. Yet, although a robust literature exists on quit attempts in the tobacco field, little is known regarding patterns of cessation attempts related to alcohol, opioid, stimulant, or cannabis problems. Greater knowledge of such estimates and the factors associated with needing fewer or greater attempts may have utility for health policy and clinical communication efforts and approaches.
Methods
Cross‐sectional, nationally representative survey of U.S. adults (N = 39,809) who reported resolving a significant AOD problem (n = 2,002) and assessed on number of prior serious recovery attempts, demographic variables, primary substance, clinical histories, and indices of psychological distress and well‐being.
Results
The statistical distribution of serious recovery attempts was highly skewed with a mean of 5.35 (SD = 13.41) and median of 2 (interquartile range [IQR] = 1 to 4). Black race, prior use of treatment and mutual‐help groups, and history of psychiatric comorbidity were associated with higher number of attempts, and more attempts were associated independently with greater current distress. Number of recovery attempts did not differ by primary substance (e.g., opioids vs. alcohol).
Conclusions
Estimates of recovery attempts differed substantially depending on whether the mean (5.35 recovery attempts) or median (2 recovery attempts) was used as the estimator. Implications of this are that the average may be substantially lower than anticipated because cultural expectations are often based on AOD problems being “chronically relapsing” disorders implicating seemingly endless tries. Depending on which one of these estimates is reported in policy documents or communicated in public health announcements or clinical settings, each may elicit varying degrees of help‐seeking, hope, motivation, and the use of more assertive clinical approaches. The more fitting, median estimate of attempts should be used in clinical and policy communications given the distribution.
Keywords: Recovery, Opioid Use Disorder, Quit Attempts, Alcohol Use Disorder, Remission
Introduction
Substance use disorders are often described as “chronically relapsing”—an assertion confirmed from common anecdote, clinical observation, and myriad systematic clinical and epidemiological studies (Dennis and Scott, 2007; McKay and Hiller‐Sturmhofel, 2011; McLellan et al., 2000; White and McClellan, 2008; White et al., 2003). Although the “chronic disease” designation has been challenged (Brown, 1998; Heyman, 2010), there is broad support for the central notion that changing addictive behavior is difficult and more a stage‐dependent process than an event—facts confirmed by the percentage of people who fail to complete addiction treatment in the United States (more than 50%; Substance Abuse and Mental Health Services Administration, 2014), the 58% of people entering addiction treatment with 1 or more prior treatment admissions (Substance Abuse and Mental Health Services Administration, 2014), and the high rate of posttreatment recurrence of alcohol and other drug (AOD) use (more than 50%; White, 2008a, 2012), most often within 90 days of treatment discharge (Hubbard et al., 2003).
There are a number of biopsychosocial challenges for those seeking to recover from compulsive AOD use and psychological and physical dependence. Theories of incentive salience (Bindra, 1974; Robinson and Berridge, 1993), negative emotionality (Heilig et al., 2010; Sinha et al., 2009), and executive function deficits (Bickel et al., 2012; Koob and Le Moal, 2001) all help explain some of these challenges, with incentive salience representing use for reward (positive reinforcement), negative emotionality representing use for relief (negative reinforcement), and executive functioning theories reflecting changes in inhibitory control impairing ability to stop (Koob and Le Moal, 1997). These empirically grounded theories help explain the formidable challenges faced by people making serious attempts to cease deeply imbedded and harmful patterns of substance use. Although compulsive AOD use is commonly depicted as chronically relapsing, very little is known regarding the actual number of serious recovery attempts that people make prior to successfully resolving a significant AOD problem. Such research efforts on quit attempts have been made in the tobacco addiction field (Borland et al., 2010; Chaiton et al., 2016), with estimates of the number of quit attempts prior to successful quitting ranging very broadly from an average somewhere between 6 and 30 or more, depending on the study design and methods used (Chaiton et al., 2016). Yet, little is known regarding patterns of cessation attempts related to opioid, alcohol, stimulant, or cannabis use disorders. Greater knowledge of these estimates of AOD recovery attempts prior to problem resolution, and the factors associated with needing fewer or greater attempts to resolve an AOD problem (e.g., demographic and clinical predictors), has utility for health administrations and health policy communication efforts. Also, such data can inform and shape clinical approaches and the nature of communication in treatment settings; findings might be used, for example, to help patients stay engaged following initial cessation failures (Chaiton et al., 2016; McQuaid et al., 2017) and help inform patients and families about what to expect as they prepare for change. In contrast, if the mean and median recovery attempt numbers are very high, this could decrease motivation and diminish hope that salutary change is possible, especially for certain patient subgroups, while simultaneously alerting sufferers, families, clinicians, and health systems of the need for perhaps more assertive efforts given the probable challenges that lie ahead.
Available data on recovery attempt patterns and outcomes reside primarily within clinical follow‐up studies of addiction treatment, studies of professional assistance programs, and recent “Life in Recovery” surveys. Dennis and colleagues (2005) conducted a 5‐year follow‐up of more than 1,200 predominately minority patients admitted to publicly funded addiction treatment in a large U.S. metropolitan area. Among those achieving 1 or more years of abstinence, the median time from first use to last use was 27 years and from first treatment episode to last use was 9 years, indicating multiple recovery attempts without reporting this specifically. Laudet and White (2004) conducted a 5‐year follow‐up of 354 people in recovery living in New York City, most of whom reported both prior addiction treatment and mutual‐help group participation. Seventy‐one percent of respondents reported earlier periods of 1 or more months of abstinence and 50% reported 4 or more periods of 1 or more months of abstinence before achieving stable recovery. The time between recurrences ranged from 1 month to 5+ years, with two‐thirds of those reporting recurring use having resumed AOD use for a year or more. DuPont and colleagues (2009) followed 904 physicians treated for substance use disorder as part of their involvement in a Physician Health Program (PHP). Over a 5‐year period, nearly 90% of program participants had no positive drug tests and only 18% of those with a positive drug test had a subsequent positive drug test. PHP studies consistently show high rates of continuous recovery without recurrences of AOD use and related consequences (Skipper and DuPont, 2011). The 3 clinical studies profiled illustrate wide divergence in patterns of recovery attempts but are limited by the selectiveness of the samples. Most clinical studies report a pre‐ and postintervention recovery status, but not transitions in status between these points of evaluation. Multiple‐year studies of clinical populations (Scott et al., 2005) and the general population (Dawson et al., 2007) that use numerous time points of evaluation report frequent shifts in recovery status between points of follow‐up, but such studies have not reported the total mean and median number of recovery attempts preceding sustained recovery.
Life in Recovery Surveys have been recently conducted in the United States (Laudet, 2013), Canada (McQuaid et al., 2017), the U.K. (Best et al., 2015), and Australia (Best and Savic, 2015). These studies report long prerecovery addiction careers (20.4 mean years in the U.S. survey and 18.6 mean years in the Australian survey) and dramatic improvements in health and quality of life following recovery initiation and stabilization, but only the Canadian study collected data on the number of recovery attempts prior to sustained recovery stabilization. Canadians (N = 855) who self‐identified as being in recovery reported the pattern of recovery attempts as follows: no recurrence of AOD use following initial recovery initiation (51.2%), 1 recurrence (14.3%), 2 to 5 recurrences (19.4%), and 6 or more AOD recurrence episodes (15%) prior to recovery stability. These clinical and Life in Recovery surveys may not be applicable to broader general population samples containing significant numbers of people who have resolved an AOD problem but have not necessarily embraced a recovery identity (Kelly et al., 2018a).
To help fill this knowledge gap in the field, the current study uses a national sample of U.S. adults who have successfully resolved a significant AOD problem to (1) estimate the average number of recovery attempts and the variability of such attempts prior to AOD problem resolution; (2) explore demographic and clinical predictors of the number of recovery attempts needed prior to successfully entering recovery; and (3) characterize the relationship between number of recovery attempts and indices of quality of life and psychological well‐being after AOD problem resolution.
Materials and Methods
Participants and Procedure
The present study uses data from the National Recovery Study, as described elsewhere (Kelly et al., 2017b). In brief, the internationally recognized survey company GfK screened 39,809 individuals from their “KnowledgePanel,” comprised of adults (18 and older), randomly selected using address‐based sampling. Eligible individuals were those who answered “yes” to the screening question “Did you use to have a problem with drugs or alcohol, but no longer do?”
Of the 39,809 individuals screened, 25,229 responded to the screening question (63.4%). The sample consisted of 2,002 individuals who self‐reported a resolved AOD problem from the 25,229 survey respondents (Kelly et al., 2017b).
IRB Statement
All study procedures were approved by the Partners HealthCare Institutional Review Board.
Measures
Demographic Characteristics
Participants reported the following: (a) age (in years); (b) level of education (less than college; bachelor's degree or higher), race/ethnicity (White/non‐Hispanic; Black/non‐Hispanic; other/non‐Hispanic; 2+ races/non‐Hispanic; Hispanic), sex (male; female), household income (less than 50,000 USD; 50,000 USD or greater), and marital status (married or living with partner; not married).
Problem Resolution/Recovery History
Participants reported the number of “serious attempts” made to resolve their AOD problem before they “overcame” it and time (in years/months) since they resolved their problem: “Approximately how many serious attempts did you make to resolve your alcohol/drug problem before you overcame it?”
Substance Use History
Participants answered a series of questions about 15 substances/classes of substances (hereafter simply referred to as substances) based on items from the Global Appraisal of Individual Needs (Dennis et al., 2002): (1) alcohol, (2) marijuana, (3) cocaine, (4) heroin, (5) narcotics other than heroin (e.g., pharmaceutical opioids), (6) methadone, (7) buprenorphine and its formulations (e.g., “Suboxone”), (8) amphetamines (including methylenedioxymethamphetamine, or MDMA), (9) methamphetamine (“crystal meth”), (10) benzodiazepines, (11) barbiturates, (12) hallucinogens, (13) synthetic drugs (e.g., synthetic cannabinoids such as “K2,” and synthetic cathinones such as “bath salts”), (14) inhalants, and (15) steroids, as well as other (specified by participant). First, participants reported which of these substances they used 10 or more times in their life. Then for each substance endorsed, they provided information on the following: (i) age of first use; (ii) age of first regular use (i.e., at least once per week); (iii) whether the substance was a perceived problem for them (yes/no); (iv) whether they were still using the substance (yes/no); and (v) if they were no longer using the substance, age at which they stopped using it. Finally, from the list of substances they deemed to be a problem, participants chose their primary substance (“drug of choice”) (Charney et al., 2002).
Medical/Psychiatric History
The Kessler‐6 (Kessler et al., 2003) is a 6‐item scale assessing psychiatric symptoms (also referred to as psychological distress) that asks participants to rate how often, from 0 = none of the time to 4 = all of the time, they felt each of the 6 symptoms (e.g., nervousness and depression) during the past 30 days (current sample, α = 0.93). Also regarding psychiatric functioning, the survey assessed whether participants had ever been diagnosed with one or more of the following non‐AOD psychiatric disorders (Dennis et al., 2002): anxiety disorders, depressive disorders, eating disorders (e.g., anorexia), or psychotic disorders (e.g., schizophrenia).
Treatment and Other Recovery Support Services
The questionnaire assessed history of participation in 9 psychosocial treatment and recovery support services (Institute of Behavioral Research, 2002): (1) inpatient or residential treatment; (2) outpatient addiction treatment; (3) state or local recovery community organization; (4) faith‐based recovery services (e.g., addiction recovery support group provided by a church, synagogue, or mosque); (5) recovery community center; (6) collegiate recovery program/community; (7) recovery high school; (8) sober living environment; and (9) mutual‐help organizations (MHOs).
Recovery Capital
The survey included the Brief Assessment of Recovery Capital (BARC) (Vilsaint et al., 2016), a 10‐item abridged version of the Addiction Recovery Capital Scale (Groshkova et al., 2013). For this measure, participants reported their level of agreement, on a Likert scale from 1 = strongly disagree to 6 = strongly agree, with statements on their recovery, environmental support, and well‐being (e.g., “I regard my life as challenging and fulfilling without the need for using drugs or alcohol”). The BARC has demonstrated excellent concurrent validity with the original measure of recovery capital (r = 0.92) as well as excellent internal consistency (α = 0.95), and measurement invariance between treatment and nontreatment recovery samples. Its internal consistency in the current sample was also excellent (α = 0.93)
Quality of Life
The European Health Interveiw Surveys‐Quality of Life (Schmidt et al., 2006) is a widely used 8‐item measure of quality of life, adapted from the World Health Organization Quality of Life—Brief Version. Item responses are on Likert scales from 1 to 5 (e.g., “How satisfied are you with your personal relationships?”; 1 = very dissatisfied to 5 = very satisfied). The measure has strong psychometric properties, including good‐to‐excellent predictive validity (i.e., significant discrimination between individuals with and without a health condition), convergent validity with other measures of health and wellness (rs = 0.4 to 0.6), and internal consistency (α = 0.83). Its internal consistency was excellent in the current sample (α = 0.90).
Happiness and Self‐Esteem
Participants rated their happiness on a Likert scale from 1 = completely unhappy to 5 = completely happy (Meyers and Smith, 1995). They also rated the extent to which “I have high self‐esteem” is true on a Likert scale from 1 = not very true to 5 = very true (Robins et al., 2016).
Statistical Analysis
We calculated the mean, median, and measures of variation (standard deviation, interquartile range, minimum, maximum) of the number of recovery attempts in the full sample. We then characterized this distribution stratified by demographic (i.e., sex, education, race/ethnicity, household income, and marital status) and clinical factors (i.e., primary substance, psychiatric diagnoses, outpatient treatment history, inpatient treatment history, mutual‐help attendance, and utilization of any treatment or recovery support services). We evaluated whether the number of recovery attempts was associated with these factors or continuous (age, age of onset) demographic and clinical correlates by regressing these factors with number of recovery attempts. In these models, number of recovery attempts was transformed using the negative reciprocal transformation to fulfill the assumption of normality. These variables were selected based on prior research and stress and coping theory (Folkman and Lazarus, 1980) with the supposition that those with greater substance use severity and service use histories would have required a greater number of serious recovery attempts.
Also, given that it is quite probable that at least some of those in the current sample are likely to suffer a future recurrence of AOD problems—particularly those in the early phases of recovery (e.g., <5 years; White, 2012), recovery from which would likely add to their current tally of prior serious recovery attempts—we conducted a sensitivity analysis whereby we restricted the sample to those who had 5 or more years in recovery in order to see whether the estimate of prior serious recovery attempts differed in this subset of more stable remitters.
Finally, to examine the relationship between number of recovery attempts and quality of life, we ran a series of 3 models for each of the 5 quality‐of‐life outcomes (current quality of life, happiness, self‐esteem, psychological distress, and recovery capital). The first model examined the relationship between number of recovery attempts and each of the quality‐of‐life outcomes modeled separately. The second set of models similarly examined the association between number of recovery attempts and quality‐of‐life outcomes controlling for years since problem resolution. The final set of models examined the association between number of recovery attempts and quality of life controlling for years since problem resolution and clinical correlates that were found to be significantly associated with number of recovery attempts. In these models, psychological distress and recovery capital were transformed using natural log and square root transformations, respectively. All models incorporated survey weights and were conducted using Stata, version 14 (College Station, TX, USA).
Results
Distribution of Number of Recovery Attempts Among Adults Who Have Resolved a Problem With Alcohol or Other Drugs
The number of serious recovery attempts made among adults who have resolved a problem with alcohol or other drugs in the United States ranged from 0 to 100 attempts. The mean number of recovery attempts was 5.35 (SD = 13.41); however, the data were substantially positively skewed and kurtotic (Fig. 1 A; skewness = 5.89, SE = 0.57; kurtosis = 50.27, SE = 9.66). As shown in Fig. 1 B, the median number of recovery attempts was 2 (IQR = 1 to 4; Fig. 1 B). The modal number of serious attempts was 1. In Fig. 1 B, the middle 50% of the distribution (i.e., 25th–75th percentile) are represented by the values covered by the gray box (i.e., 1–4 recovery attempts). The midline shown in the gray box represents the median (i.e., 50th percentile). The upper and lower fence, calculated as 1.5 multiplied by the interquartile range, represent the maximum and minimum value beyond which the data are considered to be outliers, as indicated by circles. Both the histograms and box plots confirm that the data are positively skewed and required a negative reciprocal transformation in order to be included in linear models assuming normality, the results of which are described below.
Figure 1.
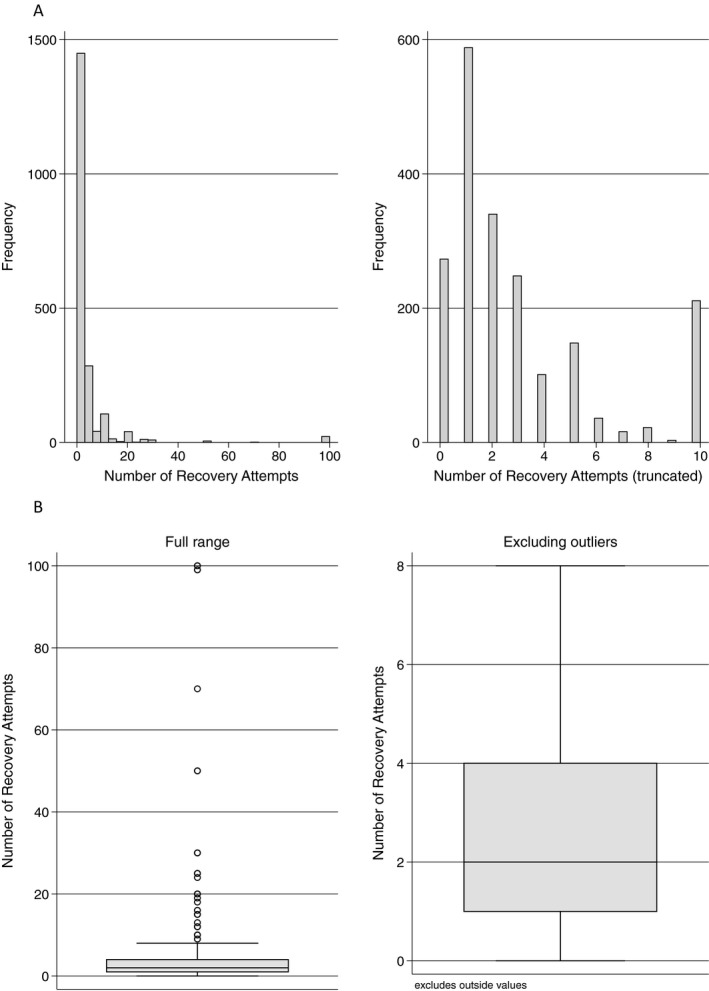
(A) Distribution of number of recovery attempts (histogram). (B). Distribution of number of recovery attempts (box plot).
Of note, approximately 13% of the sample (n = 260) reported not making any serious recovery attempts. Sensitivity analyses were conducted excluding those who did not report something that constituted a “serious” recovery attempt. Results revealed that among participants reporting at least 1 serious recovery attempt (n = 1,742), the mean and median number of recovery attempts were slightly higher—6.14 (SD = 14.20) and 3 (IQR = 1 to 5) recovery attempts, respectively.
An additional sensitivity analysis examining only those with 5+ years of recovery (see the Analysis section) found that this more stable group of individuals in recovery reported a very similar pattern of serious recovery attempts compared to the sample in general (i.e., mean = 5.02, SD = 13.61; median = 2, IQR = 1 to 4).
Distribution of Number of Recovery Attempts by Demographic and Clinical Correlates
As shown in Fig. 2, individuals who were non‐Hispanic Black (vs. non‐Hispanic White) and not married (vs. married or living with a partner) reported a greater number of recovery attempts. There was no statistically significant association between number of recovery attempts and age, sex, education, or household income. Individuals who reported having been diagnosed with depressive or anxiety disorders or who had received treatment or recovery support services, including inpatient, outpatient mutual help, or any support service, reported a greater number of recovery attempts (Fig. 3). Age of onset and primary substance were not significantly associated with number of recovery attempts (Table 1). As shown in Fig. 4 and Table 1, there were apparent differences in the distribution of number of recovery attempts by primary substance; however, these did not reach statistical significance likely due to the large amount of variability, particularly within alcohol and opioid groups.
Figure 2.
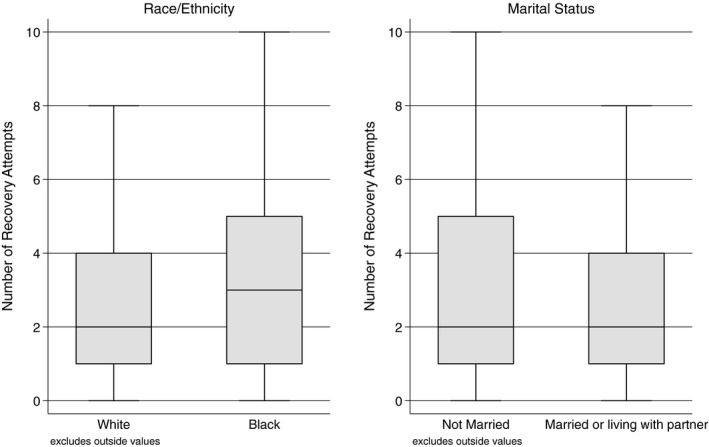
Demographic factors significantly associated with number of recovery attempts.
Figure 3.
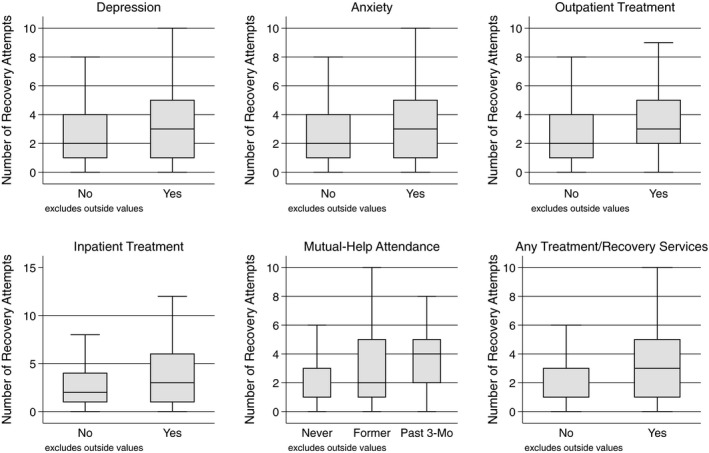
Clinical factors significantly associated with number of recovery attempts.
Table 1.
Distribution of Number of Recovery Attempts and Associations With Demographic and Clinical Correlates (N = 2,002)
| Mean (SD) | Median (IQR) | Min, max | t | p | |
|---|---|---|---|---|---|
| Full sample | 5.35 (13.41) | 2 (1, 4) | 0, 100 | – | – |
| Age (in years) | – | – | – | −1.53 | 0.127 |
| Sex | |||||
| Female | 4.18 (9.16) | 2 (1, 4) | 0, 100 | REF | REF |
| Male | 6.12 (15.56) | 2 (1, 5) | 0, 100 | −0.32 | 0.748 |
| Education | |||||
| Less than college | 5.47 (13.64) | 2 (1, 4) | 0, 100 | REF | REF |
| Bachelor's degree or higher | 4.80 (12.32) | 2 (1, 4) | 0, 100 | −1.55 | 0.122 |
| Race/ethnicity | |||||
| White, non‐Hispanic | 5.33 (14.51) | 2 (1, 4) | 0, 100 | REF | REF |
| Black, non‐Hispanic | 4.60 (8.10) | 3 (1, 5) | 0, 99 | 2.96 | 0.003 |
| Other, non‐Hispanic | 6.60 (16.14) | 3 (1, 5) | 0, 100 | 1.90 | 0.058 |
| Hispanic | 5.67 (11.92) | 2 (1, 5) | 0, 100 | 1.42 | 0.154 |
| 2+ races, non‐Hispanic | 4.36 (11.81) | 2 (1, 4) | 0, 100 | 0.58 | 0.561 |
| Marital status | |||||
| Not married | 6.07 (14.82) | 2 (1, 5) | 0, 100 | REF | REF |
| Married or living with partner | 4.68 (11.95) | 2 (1, 4) | 0, 100 | −2.56 | 0.011 |
| Household income | |||||
| <50,000 USD | 5.46 (13.71) | 2 (1, 5) | 0, 100 | REF | REF |
| 50,000 USD or greater | 5.22 (13.09) | 2 (1, 4) | 0, 100 | 0.18 | 0.859 |
| Age of onset (in years) | – | – | – | −1.47 | 0.143 |
| Primary substance | |||||
| Alcohol | 5.38 (13.45) | 2 (1, 4) | 0, 100 | REF | REF |
| Cannabis | 4.62 (8.41) | 2 (1, 4) | 0, 100 | 0.29 | 0.771 |
| Opioids | 8.48 (21.08) | 3 (1, 6) | 0, 100 | 0.90 | 0.368 |
| Stimulants | 4.64 (8.03) | 2 (1, 5) | 0, 100 | 0.35 | 0.725 |
| Other drugs | 3.00 (4.01) | 1 (1, 6) | 0, 20 | −0.86 | 0.392 |
| Depressive disorder | |||||
| No | 5.27 (13.86) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 5.84 (10.52) | 3 (1, 5) | 0, 100 | 3.30 | 0.001 |
| Anxiety disorder | |||||
| No | 5.14 (13.33) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 6.08 (13.76) | 3 (1, 5) | 0, 100 | 3.14 | 0.002 |
| Psychotic disorder | |||||
| No | 5.17 (13.11) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 12.22 (21.59) | 3 (0, 10) | 0, 100 | 0.44 | 0.662 |
| Eating disorder | |||||
| No | 5.31 (13.43) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 7.53 (13.73) | 2 (1, 6) | 0, 50 | 1.41 | 0.159 |
| Outpatient treatment | |||||
| No | 5.17 (13.32) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 6.22 (13.83) | 3 (2, 5) | 0, 100 | 4.40 | <0.001 |
| Inpatient/residential treatment | |||||
| No | 5.12 (13.23) | 2 (1, 4) | 0, 100 | REF | REF |
| Yes | 6.65 (14.38) | 3 (1, 6) | 0, 100 | 5.10 | <0.001 |
| Mutual‐help attendance | |||||
| Never | 4.21 (11.12) | 1 (1, 3) | 0, 100 | REF | REF |
| Former | 5.56 (12.87) | 2 (1, 5) | 0, 100 | 4.84 | <0.001 |
| Past 3 months | 9.86 (21.31) | 4 (2, 5) | 0, 100 | 8.25 | <0.001 |
| Any treatment or recovery services | |||||
| No | 4.20 (11.35) | 1 (1, 3) | 0, 100 | REF | REF |
| Yes | 6.42 (15.03) | 3 (1, 5) | 0, 100 | 7.01 | <0.001 |
IQR, interquartile range.
Figure 4.
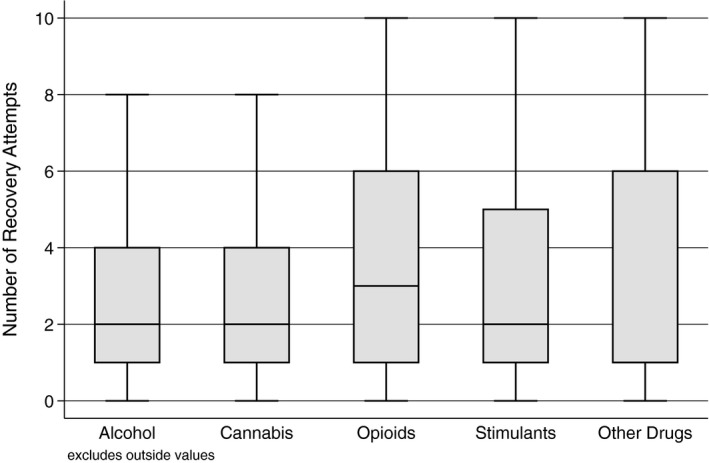
Number of recovery attempts by primary substance.
Relationship Between Number of Recovery Attempts and Quality of Life After Problem Resolution
In the unadjusted models, number of recovery attempts was associated with quality of life across all 5 indicators (i.e., quality of life, happiness, self‐esteem, psychological distress, and recovery capital). More specifically, a greater number of recovery attempts was significantly associated with lower quality of life, happiness, and self‐esteem, and higher psychological distress and recovery capital (Model 1). When the models also controlled for the number of years since problem resolution, the negative association between number of recovery attempts and lowered happiness, self‐esteem, and recovery capital was nullified (Model 2), suggesting this relationship in part may be explained by time in recovery. Upon addition of significant clinical correlates (depression, anxiety, and utilization of any treatment/recovery services), only the relationship between greater number of recovery attempts and higher current psychological distress remained statistically significant (Model 3; p = 0.002; Table 2), suggesting that regardless of how long one has been in recovery, a history of mood and anxiety disorders, and use of treatment services, a greater number of recovery attempts was still associated with greater current distress.
Table 2.
Relationship Between Number of Recovery Attempts and Quality of Life
| Dependent variable | Model 1 | Model 2 | Model 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | p | B | SE | t | p | B | SE | t | p | |
| Quality of life | −5.80 | 1.65 | −3.52 | <.001 | −4.29 | 1.63 | −2.63 | 0.009 | −2.34 | 1.63 | −1.44 | 0.150 |
| Happiness | −0.63 | 0.22 | −2.88 | 0.004 | −0.37 | 0.23 | −1.65 | 0.100 | −0.12 | 0.22 | −0.56 | 0.578 |
| Self‐esteem | −0.78 | 0.29 | −2.65 | 0.008 | −0.49 | 0.30 | −1.65 | 0.100 | −0.19 | 0.29 | −0.67 | 0.504 |
| Psychological distress | 1.47 | 0.26 | 5.65 | <.001 | 1.14 | 0.26 | 4.38 | <.001 | 0.81 | 0.26 | 3.15 | 0.002 |
| Recovery capital | 0.85 | 0.35 | 2.42 | 0.016 | 0.56 | 0.35 | 1.60 | 0.110 | 0.38 | 0.35 | 1.11 | 0.268 |
Model 1: coefficients for number of recovery attempts (transformed), unadjusted.
Model 2: coefficients for number of recovery attempts (transformed), controlling for time since problem resolution.
Model 3: coefficients for number of recovery attempts (transformed), controlling for time since problem resolution, depression diagnosis, anxiety diagnosis, and utilization of treatment and recovery support services.
Discussion
Estimates of the number of “quit attempts” have been reported and described extensively in the tobacco cessation literature, yet few studies have reported on the number of recovery attempts among those suffering from AOD problems. This study found the distribution of attempts to be very heavily positively skewed and kurtotic producing very different estimates of central tendency, depending on whether the mean or median is used as the estimator. Specifically, there was a much higher mean and much lower median, typical of positively skewed distributions. This type of skewed distribution is also indicative of the presence of subgroups of individuals who need many more attempts than most to resolve their AOD problem. Related to this notion, there were substantial differences in the median number of recovery attempts needed depending on psychiatric diagnoses, treatment use, and MHO participation. Findings highlight the broad variability in the reported number of recovery attempts prior to resolving an AOD problem and perhaps a surprisingly low average (median), number, in general, with certain subgroups needing substantially more attempts. This low median held true even when examining the more stably remitted subsample (i.e., those with 5+ years of recovery), who are statistically much less likely to add to their future tally of serious recovery attempts given they are much less likely to relapse (White, 2012).
The overall distribution was broad, fairly platykurtic, and positively skewed. The median and mean differed substantially. In the research field, there is a tendency to more often use parametric rather than nonparametric statistical models to estimate relationships among variables of interest, and thus, there is a tradition of computing and reporting the arithmetic mean rather than the median. This is in part because many researchers are not trained to use nonparametric models to estimate effects and thus tend to transform data sets so that the mean and standard deviations/errors can be calculated and parametric models tested (Erceg‐Hurn and Mirosevich, 2008). Findings here highlight a need to report the median in addition to, or as opposed to, the mean, as the most fitting measure of central tendency, as the mean is influenced by outliers and extreme values and thus likely produces biased estimates of central tendency. The difference in our nationally representative sample was large depending on whether the mean (5.35 recovery attempts made) or median (2 recovery attempts made) is used as the estimate. This has obvious relevance in communication efforts given the large difference. Depending on which one of these estimates is reported in policy documents or communicated in public health announcements or clinical settings, each is likely to elicit varying degrees of hope and motivation as well as a cue to action.
As noted by Tukey (1977), the basic data distribution is informative and tells its own story regarding the phenomena under investigation. Here, we observed a positively skewed distribution and generally large standard deviations, reflecting high variability, and fairly wide confidence intervals, when using parametric estimators (i.e., the mean and SD). This is suggestive that there are subgroups of individuals within the sample who may be quite different. This is what we would expect given the nature of this sample of individuals who have resolved a significant AOD problem who exhibit a wide range of impairment and distress (Kelly et al., 2017a, 2018b).
Notably, those who required a significantly greater number of serious recovery attempts prior to resolving their AOD problem were single, more likely to be of Black race, and those who had used prior treatment and recovery support services, particularly MHOs. Given the cross‐sectional nature of the data, it is currently unclear whether relationship status (e.g., married, living with partner) at the time of those serious recovery attempts had any bearing on them as this variable reflected current status rather than historical status. It is unclear also why those of Black race compared to White race may have required significantly more recovery attempts. Future research is needed to understand more about such racial differences. The association of a greater number of recovery attempts among those who had used more treatment and MHOs may be indicative of greater severity and AOD‐related impairment that could have negatively impacted inhibitory control regions of the brain requiring greater degrees of focused and intensive support that treatment services and ongoing MHO participation can provide, in order to resolve a significant AOD problem. These findings of help‐seeking with greater severity are similar to the large set of findings on natural recovery (e.g., Klingemann et al., 2001). Finally, in terms of the relationship between recovery attempts and indices of quality of life and well‐being, our models suggest that a higher number of recovery attempts needed prior to successful AOD problem resolution is independently related to greater psychological distress, but not other indices (e.g., quality of life, happiness; self‐esteem), regardless of how long one has been in recovery, prior service use, or the presence of other psychiatric comorbidity. This may be indicative of a subgroup of individuals who have suffered from either a greater burden of or sensitivity to stress, and who found recovery‐related changes more challenging, or perhaps represents those who have found a way to stay in recovery despite a greater burden of sensitivity to stress. It may reflect stress‐related central nervous system sequelae from longer, harmful, levels of AOD exposure that has resulted in greater stress sensitivity (Quadros et al., 2016). Alternatively, it could reflect life contexts that were, and are, stressful, so that despite entering recovery, actual levels of stress remain high.
Of note, 13% of the sample, although reporting that they had resolved a significant AOD problem, nevertheless reported they had never made a serious recovery attempt prior to overcoming their problem. It is possible that they misinterpreted the question or perhaps did not consider any of their attempts “serious.” Regarding the first possibility of question misinterpretation, it is possible that because the question asked about serious recovery attempts “prior to overcoming” their AOD problem, they did not count the current attempt, even though it may have been regarded as a serious attempt. Regarding the second possibility, in subsidiary analyses (not shown) we found that about 34% of this group (of n = 260) who reported zero prior serious recovery attempts also reported use of some kind of treatment or mutual‐help recovery support service, indicative of perhaps a more “serious” concerted effort to resolve their problem (Kelly et al., 2018a). In this scenario, it is also possible that they may have misinterpreted the question to mean not including the current recovery attempt or that use of such services still did not surpass their own subjective threshold of what constitutes a “serious” attempt. From our prior research with this sample (Kelly et al., 2018a), however, it is quite possible that at least some people found it very straightforward to resolve their AOD problem as it was reported as not severe and not resulting in substantial impairment. Regardless, even when assuming everyone in this zero group did indeed have at least 1 serious recovery attempt, it did not make a large absolute difference in increasing the average number of recovery attempts as our sensitivity analyses revealed the absolute median number of recovery attempts needed prior to AOD problem resolution remained low, moving from 2 to 3, and with the mean moving from 5.35 to 6.14.
It is also possible that individuals who never encounter MHOs or treatment services never perceive their problem to be bad enough to warrant a “serious recovery attempt” merely because they have little reference or context for such an appraisal. In contrast, exposure to MHOs or treatment may enhance the perceived gravity of the situation and serious nature of their condition—independent of AOD problem severity—such that this implicitly “raises the stakes” making any future appraisal of recovery attempts more “serious.” This could also be another explanation—beyond severity—that would create an association between number of serious attempts and use of external recovery support services, and should be investigated further.
Implications of Study Findings
The median number of recovery attempts prior to successful AOD problem resolution may be substantially lower than most people might have guessed. This may be surprising to many because, arguably, our cultural psyche regarding how AOD problems are resolved is infused with the stereotyped notion that such problems constitute “chronically relapsing brain diseases” and thus success in changing AOD use is perceived to involve seemingly endless tries (e.g., possibly predicated on clinical samples alone and reporting of a biased higher mean number of recovery attempts, such as that found in this study). Relatedly, many may believe—again based on cultural stereotype—that changing AOD use is so difficult that it inevitably involves going to “rehab” and/or “AA.” Although it is certainly true that some do need that level of care and ongoing recovery support to achieve long‐term remission, this stereotype may have the unintended consequence of reducing hope and recovery self‐efficacy for many less severely affected individuals, preventing help‐seeking, because the threshold for successful change is perceived to be too high. Both the Canadian study on people who self‐identify as being in recovery (McQuaid et al., 2017) and this broad nationally representative sample of Americans resolving a significant AOD problem (Kelly et al., 2017b) suggest that for most people (based on the median), the number of serious recovery attempts needed is actually quite low, but with certain subgroups (i.e., likely those with higher severity/chronicity/comorbidity and lower recovery capital), requiring more attempts to achieve success. Yet, it is these more severe subgroups that are perceived as the norm, when the opposite is in fact true.
There are several treatment implications of the current findings. First, if AOD problems do not represent a singular clinical entity with a narrow developmental pathway and course treatable through a fixed “program” for all patients, but rather a spectrum disorder characterized by heterogeneous etiological pathways, diverse clinical profiles, highly variable courses, and diverse pathways and styles of problem resolution (e.g., Kelly et al., 2017a; White, 2012), then one would expect to see the wide range of recovery attempts found in the present study. Such diversity requires highly individualized approaches to addressing AOD problems. If clinical outcomes are highly influenced by the interaction of problem severity/complexity/chronicity and available personal/family/community recovery capital as some suggest (Kelly and Hoeppner, 2015; White and Cloud, 2008), then a treatment system designed around the mean clinical profile would have 2 unforeseen consequences: overtreating those persons with lower severity patterns and high recovery capital and undertreating those with high problem severity patterns but minimal recovery capital. The former would result in people receiving unneeded treatment or treatment at more intense levels of care than clinically indicated. The latter would provide insufficient care to initiate recovery that, like inadequate doses or durations of antibiotics, would temporarily suppress symptoms but inevitably result in a return of symptoms in a potentially more intractable form as well as a revolving door of acute treatment (White, 2008b). Homogenized approaches to treatment based on the mean of these 2 diverse patterns risk iatrogenic treatment effects for both populations and give rise to unnecessary personal and system expenditure. These findings once again underscore the notion that “one size does not fit all” and calls for perhaps more time to be invested in more accurate assessment of the full nature and impact of AOD problems and their sequelae as well as available recovery capital in order to enhance the efficiency and effectiveness of treatment efforts. More sophisticated assessment protocols that focus, for example, on the ratio of problem severity to recovery capital might result in significantly improved recovery outcomes and improved stewardship of system resources. Efforts to develop treatment models for people with low‐to‐moderate AOD problem severity (Kaner et al., 2018), and efforts to extend acute care models of addiction treatment to models of sustained recovery management for those with high problem severity and limited recovery capital (Dennis and Scott, 2007; Kelly and White, 2011), hold promise for the future of expanded choices across diverse populations within addiction treatment.
Limitations
Study findings should be interpreted cautiously in light of important limitations. First, although nationally representative, the study design was cross‐sectional and thus any longitudinal inferences should be made cautiously pending future longitudinal investigations. Estimates also relied on participants’ retrospective recall, which could be prone to bias, either over‐ or underestimating recovery attempts. Also, the stem question used to inquire into the number of serious recovery attempts was left to participants to decide for themselves regarding what a “serious” attempt was. Consequently, future estimates may vary depending on how such assessments in this area are made. A further limitation is the fact that the survey did not include adolescents, who may exhibit recovery attempt patterns quite different than those summarized in the present study.
Conclusions
Substance‐related problems and conditions are often referred to as chronically relapsing, conferring a prodigious, frequently lethal, burden on individual sufferers, their families, and society at large. Although more is known about estimates of prior quit attempts in the tobacco cessation field, little is known regarding the number of recovery attempts prior to successful problem resolution in the AOD field. This study is among the first to provide estimates of central tendency and spread (i.e., mean/median; standard deviations/interquartile ranges) in such recovery attempts that demonstrated large differences between mean and median recovery attempts in a large sample designed and weighted to be representative of the U.S. population. These differences reflect a highly positively skewed distribution. This variability, in turn, is suggestive of subgroups of individuals within the general population of those who have resolved significant AOD problems, who undertake several more serious recovery attempts prior to resolving their problem. In this study, a greater number of recovery attempts was associated most notably with use of external treatment and recovery support services that may be necessary for those most seriously impaired by AOD use. The median number of recovery attempts, however, was perhaps surprisingly low and may offer hope to those struggling with AOD problems.
Funding
Funding for this study was provided by the MGH Recovery Research Institute.
Conflict of interest
The authors report no conflicts of interest.
References
- Best D, Albertson K, Irving J, Lightowlers C, Mama‐Rudd A, Chaggar A (2015) UK Life in Recovery Survey 2015. The First National UK Survey of Addiction Recovery Experiences, in Series UK Life in Recovery Survey 2015. The First National UK Survey of Addiction Recovery Experiences Sheffield Hallam University and Helena Kennedy Centre for International Justice, Sheffield. [Google Scholar]
- Best D, Savic M (2015) The Australian Life in Recovery Survey, in Series The Australian Life in Recovery Survey Turning Point, Victoria, Australia. [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM, McClure SM (2012) Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology 221:361–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bindra D (1974) A motivational view of learning, performance, and behavior modification. Psychol Rev 81:199–213. [DOI] [PubMed] [Google Scholar]
- Borland R, Yong H‐H, Balmford J, Cooper J, Cummings KM, O'connor RJ, McNeill A, Zanna MP, Fong GT (2010) Motivational factors predict quit attempts but not maintenance of smoking cessation: findings from the International Tobacco Control Four country project. Nicotine Tob Res 12:S4–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BS (1998) Drug use–chronic and relapsing or a treatable condition? Subst Use Misuse 33:2515–2520. [DOI] [PubMed] [Google Scholar]
- Chaiton M, Diemert L, Cohen JE, Bondy SJ, Selby P, Philipneri A, Schwartz R (2016) Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open 6:e011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charney DS, Nemeroff CB, Lewis L, Laden SK, Gorman JM, Laska EM, Borenstein M, Bowden CL, Caplan A, Emslie GJ, Evans DL, Geller B, Grabowski LE, Herson J, Kalin NH, Keck PE Jr, Kirsch I, Krishnan KR, Kupfer DJ, Makuch RW, Miller FG, Pardes H, Post R, Reynolds MM, Roberts L, Rosenbaum JF, Rosenstein DL, Rubinow DR, Rush AJ, Ryan ND, Sachs GS, Schatzberg AF, Solomon S (2002) National depressive and manic‐depressive association consensus statement on the use of placebo in clinical trials of mood disorders. Arch Gen Psychiatry 59:262–270. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF (2007) Rates and correlates of relapse among individuals in remission from DSM‐IV alcohol dependence: a 3‐year follow‐up. Alcohol Clin Exp Res 31:2036–2045. [DOI] [PubMed] [Google Scholar]
- Dennis M, Scott CK (2007) Managing addiction as a chronic condition. Addict Sci Clin Pract 4:45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R, Foss MA (2005) The duration and correlates of addiction and treatment careers. J Subst Abuse Treat 28(Suppl 1):S51–S62. [DOI] [PubMed] [Google Scholar]
- Dennis M, Titus J, White M, Unsicker J, Hodkgins D (2002) Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures, in Series Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures Chestnut Health Systems, Bloomington, IL. [Google Scholar]
- DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE (2009) How are addicted physicians treated? A national survey of physician health programs. J Subst Abuse Treat 37:1–7. [DOI] [PubMed] [Google Scholar]
- Erceg‐Hurn DM, Mirosevich VM (2008) Modern robust statistical methods: an easy way to maximize the accuracy and power of your research. Am Psychol 63:591–601. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS (1980) An analysis of coping in a middle-aged community sample. J Health Soc Behav 21:219–239. [PubMed] [Google Scholar]
- Groshkova T, Best D, White WL (2013) The assessment of recovery capital: properties and psychometrics of a measure of addiction recovery strengths. Drug Alcohol Rev 32:187–194. [DOI] [PubMed] [Google Scholar]
- Heilig M, Egli M, Crabbe JC, Becker HC (2010) Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addict Biol 15:169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman GM (2010) Addiction: A Disorder of Choice. Cambridge, MA: Harvard University Press. [Google Scholar]
- Hubbard RL, Craddock SG, Anderson J (2003) Overview of 5‐year followup outcomes in the drug abuse treatment outcome studies (DATOS). J Subst Abuse Treat 25:125–134. [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research (2002) TCU Comprehensive Intake (TCU CI), Texas Christian University, Institute of Behavioral Research. Available at https://ibr.tcu.edu, Fort Worth.
- Kaner EF, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B (2018) Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2 :CD004148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Abry AW, Milligan CM, Bergman BG, Hoeppner BB (2018a) On being “in recovery”: A national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychol Addict Behav 32:595–604. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Bergman BG, Hoeppner BB, Vilsaint CL, White WL (2017a) Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend 181:162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, Bergman BG (2018b) Beyond abstinence: changes in indices of quality of life with time in recovery in a Nationally Representative Sample of U.S. adults. Alcohol Clin Exp Res 42:770–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner BB (2015) A biaxial formulation of the recovery construct. Addict Res Theory 23:5–9. [Google Scholar]
- Kelly JF, Hoeppner BB, Bergman BG, Vilsaint CL (2017b) Recovery from substance use disorder in the United States: prevalence, characteristics, and pathways from the first national probability‐based sample. Alcohol Clin Exp Res 41:179A.28019652 [Google Scholar]
- Kelly JF, White WL (2011) Recovery management and the future of addiction treatment and recovery in the USA, in Addiction Recovery Management: Theory, Research and Practice (Kelly JF, White WL. eds), pp. 303–316. Humana Press, Totowa, NJ. [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60:184–189. [DOI] [PubMed] [Google Scholar]
- Klingemann H, Sobell L, Barker J, Blomqvist J, Cloud W, Ellinstad T, Finfgeld D, Granfield R, Hodgings D, Hunt G, Junker C, Moggi F, Peele S, Smart R, Sobell M, Tucker J (2001) Promoting Self‐Change From Problem Substance Use Practical Implications for Policy, Prevention and Treatment New York, NY: Springer; 10.1007/978-94-010-0922-5 Kluwer Academic Publishers [DOI] [Google Scholar]
- Koob GF, Le Moal M (1997) Drug abuse: hedonic homeostatic dysregulation. Science 278:52–58. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M (2001) Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 24:97–129. [DOI] [PubMed] [Google Scholar]
- Laudet A (2013) “Life in Recovery”: Report on the Survey Findings. in Series “Life in Recovery”: Report on the Survey Findings Faces & Voices of Recovery, Washington, DC. [Google Scholar]
- Laudet A, White WL (2004) An Exploration of Relapse Patterns Among Former Poly‐Substance Users, in Series An Exploration of Relapse Patterns Among Former Poly‐substance Users, 132nd Annual Meeting of the American Public Health Association. [Google Scholar]
- McKay JR, Hiller‐Sturmhofel S (2011) Treating alcoholism as a chronic disease: approaches to long‐term continuing care. Alcohol Res Health 33:356–370. [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD (2000) Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 284:1689–1695. [DOI] [PubMed] [Google Scholar]
- McQuaid RJ, Malik A, Morrisey M, Baydack N (2017) Life in Recovery From Addiction in Canada, in Series Life in Recovery from Addiction in Canada Canadian Centre on Substance Abuse, Ottawa, ON. [Google Scholar]
- Meyers RJ, Smith JE (1995) Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach Guilford Press, New York, NY. [Google Scholar]
- Quadros IMH, Macedo GC, Domingues LP, Favoretto CA (2016) An update on CRF mechanisms underlying alcohol use disorders and dependence. Front Endocrinol (Lausanne) 7:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins RW, Hendin HM, Trzesniewski KH (2016) Measuring global self‐esteem: construct validation of a single‐item measure and the Rosenberg self‐esteem scale. Pers Soc Psychol Bull 27:151–161. [Google Scholar]
- Robinson TE, Berridge KC (1993) The neural basis of drug craving: an incentive‐sensitization theory of addiction. Brain Res Brain Res Rev 18:247–291. [DOI] [PubMed] [Google Scholar]
- Schmidt S, Muhlan H, Power M (2006) The EUROHIS‐QOL 8‐item index: psychometric results of a cross‐cultural field study. Eur J Public Health 16:420–428. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, Foss MA (2005) Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug Alcohol Depend 78:325–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM (2009) Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology 34:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skipper GE, DuPont RL (2011) The Physician Health Program: A replicable model of sustained recovery management, in Addiction Recovery Management: Theory, Research and Practice (Kelly JF, White WL. eds), pp 281–302. Humana Press, Totowa, NJ. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2014) Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, Substance Abuse and Mental Health Services Administration, NSDUH Series H‐48, HHS Publication No. (SMA) 14‐4863. Rockville, MD. [Google Scholar]
- Tukey JW (1977) Exploratory Data Analysis Addison‐Wesley, Reading, MA. [Google Scholar]
- Vilsaint CL, Kelly JF, Groshkova T, Best D, White WL (2016) Development of a 10‐Item Assessment of Alcohol and Drug use Disorder Recovery Capital (arc‐10) Using Item Response Theory., in Series Development of a 10‐Item Assessment of Alcohol and Drug use Disorder Recovery Capital (arc‐10) Using Item Response Theory Research Society on Alcoholism, New Orleans, LA. [Google Scholar]
- White WL (2008a) Recovery Management and Recovery‐Oriented Systems of Care: Scientific Rationale and Promising Practices, in Series Recovery Management and Recovery‐Oriented Systems of Care: Scientific Rationale and Promising Practices Northeast Addiction Technology Transfer Center, Great Lakes Addiction Technology Transfer Center, Philadelphia Department of Behavioral Health/Mental Retardation Services, Pittsburgh, PA. [Google Scholar]
- White WL (2008b) Recovery: old wine, flavor of the month or new organizing paradigm? Subst Use Misuse 43:1987–2000. [DOI] [PubMed] [Google Scholar]
- White WL (2012) Recovery/remission from substance use disorders: An analysis of reported outcomes in 415 scientific reports, 1868‐2011, in Series Recovery/Remission From Substance use Disorders: An Analysis of Reported Outcomes in 415 Scientific Reports, 1868‐2011, Philadelphia Department of Behavioral Health and Intellectual Disability Services [Google Scholar]
- White WL, Boyle M, Loveland D (2003) Recovery management: transcending the limitations of addiction treatment. Behav Health Manag 23:38–44. [Google Scholar]
- White WL, Cloud W (2008) Recovery capital: a primer for addictions professionals. Counselor 9:22–27. [Google Scholar]
- White WL, McClellan AT (2008) Addiction as a chronic disorder. Counselor: The Magazine for Addiction Professionals 8.


