Abstract
Background:
The significance of the timing and chronicity of childhood adversity for depression outcomes later in life is unclear. Identifying trajectories of adversity throughout childhood would allow classification of children according to the accumulation, timing, and persistence of adversity and may provide unique insights into the risk of subsequent depression.
Methods:
Using data from the Avon Longitudinal Study of Parents and Children (ALSPAC), we created a composite adversity score comprised of ten prospectively assessed domains (e.g., violent victimization; inter-parental conflict; financial hardship) for each of eight time points from birth through age 11.5 years. We used semi-parametric group-based trajectory modeling to derive childhood adversity trajectories and examined the association between childhood adversity and depression outcomes at age 18 years.
Results:
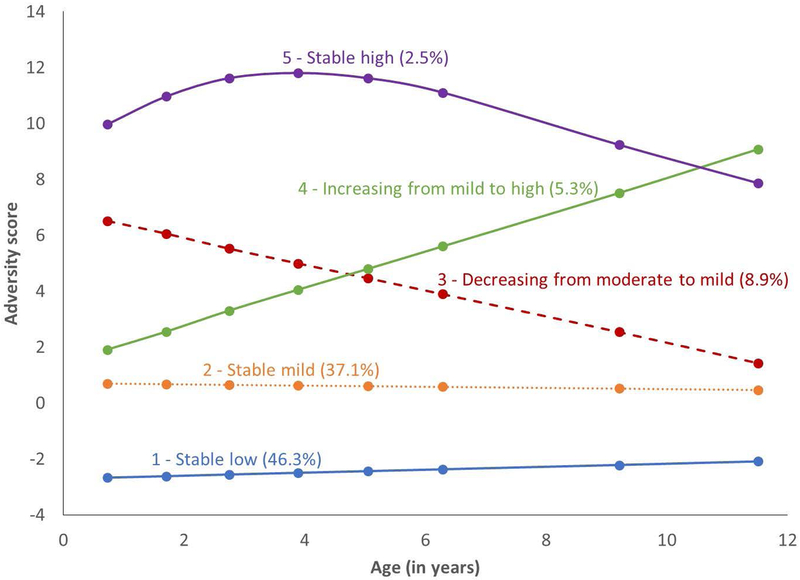
Among 9,665 participants, five adversity trajectories were identified, representing stable-low levels (46.3%), stable-mild levels (37.1%), decreasing levels (8.9%), increasing levels (5.3%), and stable-high levels of adversity (2.5%) from birth through late childhood. Approximately 8% of the sample met criteria for probable depression at 18 years and the mean depression severity score was 3.20 (SD=3.95, range 0–21). The risk of depression in young adulthood was elevated in the decreasing (OR=1.72, 95% CI=1.19–2.48), increasing (OR=1.81, 95% CI=1.15–2.86), and stable-high (OR=1.80, 95% CI=1.00–3.23) adversity groups, compared to those with stable-low adversity, when adjusting for potential confounders.
Conclusions:
Children in trajectory groups characterized by moderate or high levels of adversity at some point in childhood exhibited consistently greater depression risk and depression severity, regardless of the timing of adversity.
Keywords: ALSPAC, depression, mental health, childhood adversity, adverse childhood experiences, trajectories
INTRODUCTION
Childhood adversity, including maltreatment, financial hardship, and parental separation, is reported by more than half of many adult populations (Felitti et al., 1998; Green et al., 2010). Evidence from numerous studies has illustrated the negative consequences of childhood adversity (Brown et al., 2009; Chartier, Walker, & Naimark, 2010; Felitti et al., 1998; Green et al., 2010), including increased risk for mental health problems in adolescence and adulthood (Benjet, Borges, & Medina-Mora, 2010; Björkenstam, Pebley, Burström, & Kosidou, 2017; Gilman, Kawachi, Fitzmaurice, & Buka, 2003; Mersky, Topitzes, & Reynolds, 2013; Schilling, Aseltine, & Gore, 2007, 2008). Since childhood adversities tend to cluster together, measures of “cumulative adversity” are often derived as counts of events occurring during a specified time period (Atkinson et al., 2015; Evans, Li, & Whipple, 2013; Raposa, Hammen, Brennan, O’Callaghan, & Najman, 2014; Turner & Lloyd, 1995), with greater numbers of events associated with greater severity of mental health problems (Björkenstam et al., 2017; Chapman et al., 2004; Edwards, Holden, Felitti, & Anda, 2003; Fergusson, Woodward, & Horwood, 2000; Mersky et al., 2013; Schilling et al., 2007). However, many studies of cumulative adversity rely on retrospective self-reports of childhood events and circumstances (Benjet et al., 2010; Lloyd & Turner, 2008; Whitesell et al., 2007), use simple counts of dichotomized items (Slopen, Koenen, & Kubzansky, 2014; Slopen, Kubzansky, McLaughlin, & Koenen, 2013), and fail to account for the timing or persistence of adversity throughout childhood (Appleton, Holdsworth, Ryan, & Tracy, 2017; Slopen et al., 2014) when examining its effects on health later in life.
The timing and persistence of childhood adversity may be particularly important for the development of mental health problems (Dunn, Nishimi, Powers, & Bradley, 2017; Dunn et al., 2018; Schalinski et al., 2017, 2016). Some prospective studies have found adverse experiences in early childhood (e.g., before age five) to have long-term effects on depression (Kaplow & Widom, 2007; Manly, Kim, Rogosch, & Cicchetti, 2001; Thornberry, Henry, Ireland, & Smith, 2010), while others have found stronger effects of adverse events occurring at later times (e.g., middle childhood or adolescence) (Harpur, Polek, & van Harmelen, 2015; Najman et al., 2010; Thornberry, Ireland, & Smith, 2001). It is difficult to untangle timing and chronicity in some of this prior work, as individuals experiencing adversity at earlier ages often have the longest durations of exposure, while mental health outcomes reported in adolescence or early adulthood may be more sensitive to recent events. Identifying trajectories of adversity throughout childhood allows for classification of individuals according to the accumulation, timing, and duration of their adverse experiences (Bøe et al., 2017). This may provide unique insights into the etiology of mental health problems according to the patterning and timing of childhood adversity, and may also suggest novel avenues for intervention.
Given the dramatic increase in depression prevalence during adolescence and young adulthood and the many negative consequences associated with depression in this phase of life (Costello, Swendsen, Rose, & Dierker, 2008; Glied & Pine, 2002), we aimed to identify trajectories of adversity from birth through late childhood and to examine long-term effects on depression outcomes in young adulthood across these trajectory groups.
MATERIALS AND METHODS
Study participants
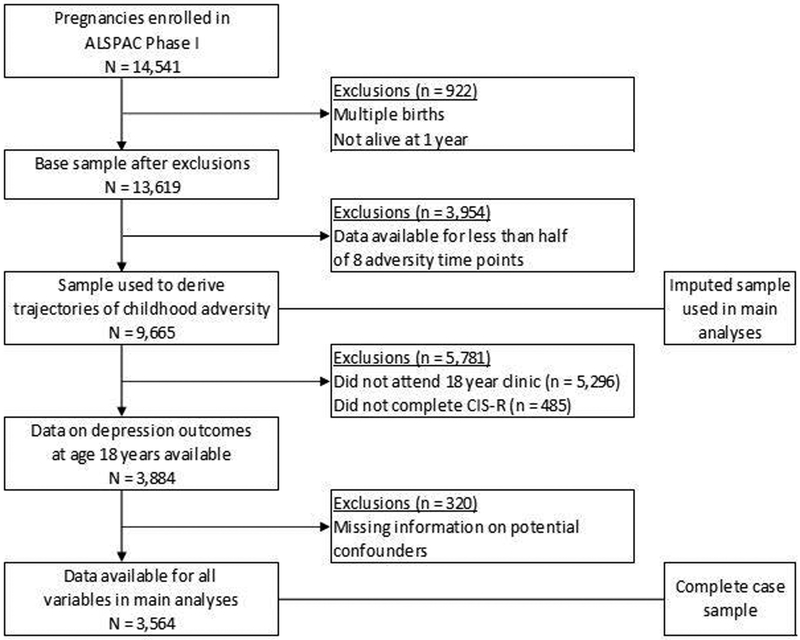
The Avon Longitudinal Study of Parents and Children (ALSPAC) is an ongoing population-based prospective cohort study that enrolled pregnant women with expected delivery dates between April 1, 1991 and December 31, 1992 who were residing in the former Avon Health Authority in southwestern England (Boyd et al., 2013; Fraser et al., 2013). Participating mothers, their partners, and their study offspring have been assessed repeatedly since pregnancy, with both in-person visits and mailed questionnaires. Of the 14,062 live births resulting from 14,541 pregnancies, 13,619 were singletons and alive at age 12 months (Figure 1). The ALSPAC study website contains details of all the data that are available, through a fully searchable data dictionary and variable search tool (http://www.bris.ac.uk/alspac/researchers/our-data). Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees, including the University at Albany Institutional Review Board.
Figure 1.
Flow chart of participation in the Avon Longitudinal Study of Parents and Children
Study measures
Depression outcomes.
Depressive symptoms were assessed using the Clinical Interview Schedule – Revised (CIS-R) (Lewis, 1994; Lewis, Pelosi, Araya, & Dunn, 1992), which was self-administered via a computerized questionnaire during the 18-year clinic visit (Bowes, Joinson, Wolke, & Lewis, 2015). The CIS-R has been used extensively in community-based surveys (Jenkins et al., 2003; Meltzer, Gill, Petticrew, & Hinds, 1995) to generate International Statistical Classification of Diseases, 10th Revision (ICD-10) diagnoses of mental disorders including depression. A total depression score ranging from 0–21 can also be created by summing scores on five depression-related domains (fatigue, concentration problems, sleep problems, depression, and depressive thoughts). We used the ICD-10 diagnosis of depression as an indicator of probable depression and the total depression score as an indicator of depression severity. For a supplemental analysis of shorter-term depression outcomes, we also examined depressive symptoms assessed with the Short Moods and Feelings Questionnaire (SMFQ) (Angold, Costello, Messer, & Pickles, 1995) during in-person clinic visits at ages 12.5 and 13.5 years.
Childhood adversity.
Mothers and fathers completed questionnaires regularly throughout the study period, reporting on their own experiences of life events, behaviors, and social circumstances as well as those of the study child during the time since the last assessment (or since the child’s birth, at the earliest assessment) (Slopen et al., 2013). In order to identify trajectories of childhood adversity, we created summary measures of adversities reported at each of eight time points when children were, on average, aged 8 months, 1.5 years, 2.5 years, 3.5 years, 5 years, 6.5 years, 9 years, and 11.5 years. Ten adversity domains were included, reflecting both acute and chronic adverse exposures, consistent with previous work on childhood adversity (Benjet et al., 2010; Felitti et al., 1998; Nobile et al., 2013; Schilling et al., 2007; Slopen et al., 2014) (see eTable 1 in the Online Supplement for a complete list of items included in each domain): (1) death or illness in family, (2) child’s experience of violent victimization (e.g., physical or sexual abuse), (3) inter-parental conflict, (4) family disruption (e.g., mother got divorced or separated), (5) parental employment difficulties, (6) parental legal difficulties, (7) parental psychopathology (e.g., mother or father reported high levels of depression or anxiety symptomatology), (8) parental substance use (e.g., mother or father reported heavy alcohol consumption or illegal drug use), (9) financial hardship, and (10) housing inadequacies or instability. Since the number of items available varied for each adversity domain, we created a standardized score (with mean of zero and standard deviation of one) for each domain at each time point; these scores were then summed to create a composite measure of adversity at each of the eight time points. This approach allowed each domain to contribute equally to the composite adversity measure and took full advantage of all of the data collected. We conducted sensitivity analyses using two alternate approaches to creating composite adversity measures: (1) restricting to items that were measured consistently across all time points, and (2) weighting each domain by its factor loading before summing (see Online Supplement for details).
Other covariates.
Potential confounders of the association between childhood adversity and depression included mother’s age at delivery and highest level of education for the child’s mother or father (reported at 32 weeks gestation). Mother’s mental health was assessed using the Crown-Crisp Experiential Index (CCEI) (Crown & Crisp, 1979) and the Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, & Sagovsky, 1987) completed by the mother around 18 weeks gestation. Probable maternal depression or anxiety during pregnancy was identified by a score > 10 on the CCEI anxiety scale, > 9 on the CCEI depression scale, or > 12 on the EPDS (Slopen et al., 2014), and was included as a potential confounder given possible familial transmission of mental health risk (Gilman et al., 2003; Weissman et al., 2016); postnatal parental mental health was assessed in the same manner and was included directly in the childhood adversity measure. The incidence of depression in adolescence varies substantially by sex (Piccinelli & Wilkinson, 2000) and may be more common among girls than boys after exposure to childhood adversity (Bouma, Ormel, Verhulst, & Oldehinkel, 2008; Gallo, Munhoz, Loret de Mola, & Murray, 2018; Oldehinkel & Ormel, 2015). Therefore, we adjusted for the child’s sex in our primary analyses, but also conducted sex-stratified sensitivity analyses.
Statistical analyses
We used PROC TRAJ in SAS to conduct semi-parametric group-based trajectory modeling to identify trajectories of adversity from birth through age 11.5 years (Cerda, Vlahov, Tracy, & Galea, 2008; Jones, Nagin, & Roeder, 2001; Nagin, 2005; Wiesner, Weichold, & Silbereisen, 2007), including the dropout extension to account for non-random attrition among those with non-missing adversity data for at least four time points (Haviland, Jones, & Nagin, 2011). The Bayesian Information Criterion (BIC) was used to select the best-fitting model, along with consideration of the interpretation and size of each trajectory group (Andruff, Carraro, Thompson, Gaudreau, & Louvet, 2009). Once the optimal number of trajectory groups was established, statistical significance of higher-order parameters (i.e., p<0.05 of linear, quadratic, and cubic terms) was then used to determine the appropriate shape of each trajectory. Individuals in the sample were assigned to the trajectory group for which their probability of group membership was highest.
Given our interest in measures collected over an 18-year period, there was considerable missing data among our sample owing both to loss to follow-up and failure to participate in specific assessments (Figure 2). We compared the study participants with (n=3,564) and without (n=10,055) complete data for our outcomes, exposure, and potential confounders (Figure 1) and found that missing data were related to both childhood adversity and child mental health; a complete case analysis would thus likely produce biased estimates (see the Online Supplement and eTable 2 for details). We therefore conducted multiple imputation of missing data using fully conditional specification implemented in SAS (version 9.4, SAS Institute Inc., Cary, NC, USA). This method uses an iterative approach to imputation that can flexibly accommodate different variable distributions (Berglund, 2015; van Buuren, 2007) and has been used in several previous studies of the ALSPAC cohort with similar amounts of missing information (Bowes et al., 2015; Culpin, Stapinski, Miles, Araya, & Joinson, 2015; Hammerton et al., 2015; Stapinski et al., 2014). The imputed sample were those with data for at least four of the eight adversity time points from birth through age 11.5 years (n = 9,665; Figure 1); this sample was highly similar to the larger base sample (eTable 3). Only covariate and outcome data were imputed (not childhood adversity information). Variables included in the imputation model were those known to be associated with depression in young adulthood (e.g., child behavior problems and depression assessed at earlier ages) (Angold et al., 1995; A. Goodman, Heiervang, Collishaw, & Goodman, 2011; R. Goodman, 1997, 2001; R. Goodman, Ford, Richards, Gatward, & Meltzer, 2000; R Goodman, Ford, Simmons, Gatward, & Meltzer, 2000) as well as those associated with missingness (e.g., socio-demographics) and all other variables included in the main analyses (see Online Supplement). Using logistic regression, multinomial logistic regression, linear regression, and predictive mean matching as appropriate, 60 imputed datasets were created, each with 25 burn-in iterations, producing a relative efficiency close to one (> 0.99) for all effects, with a maximum fraction of missing information of 0.55, thus indicating an adequate number of imputed datasets (Berglund, 2015).
Figure 2.
Participation in each assessment, among the ALSPAC sample included in analyses (n = 9,665)
Logistic regression models were then used to predict probable depression and negative binomial regression models were used to predict depression severity at age 18 years (given the skewed distribution of this symptom count) (Tracy, Hobfoll, Canetti-Nisim, & Galea, 2008). The association between childhood adversity trajectory group membership and depressive symptoms at ages 12.5 and 13.5 years was also assessed using negative binomial regression models in supplemental analyses.
RESULTS
In this sample of 9,665 ALSPAC participants, the five-group model proved optimal for describing their trajectories of adversity from birth through age 11.5 years (Figure 3); in the six-group model, although the BIC was significantly improved over that for the five-group model, the stable-high group appeared to be split into two groups, each comprising less than 2% of the sample. The five trajectory groups reflect stable-low levels of adversity throughout childhood (Group 1, 46.3%); stable-mild levels of adversity (Group 2, 37.1%); adversity decreasing from moderate levels after birth to mild levels by late childhood (Group 3, 8.9%); adversity increasing from mild levels after birth to high levels by late childhood (Group 4, 5.3%); and relatively stable-high levels of adversity throughout childhood (Group 5, 2.5%). Probabilities of group membership were high (>0.85) for all groups (eTable 4). Parents of children in trajectory groups characterized by higher levels of adversity generally had lower education, more mental health problems during pregnancy, and younger age at the time of delivery (eTable 5).
Figure 3.
Trajectories of adversity from birth through age 11.5 years (n = 9,665)
Approximately 8% of the sample met criteria for ICD-10-based depression at age 18 years and the mean depression severity score was 3.20 (SD=3.95, IQR=0–5) (Table 1). Adversity trajectory group membership was strongly associated with depression in bivariate analyses, with a higher prevalence of probable depression and higher mean depression severity in groups with higher levels of adversity. Female sex, maternal anxiety or depression during pregnancy, and younger maternal age at the time of delivery were also associated with higher risk of depression at age 18 years.
Table 1.
Bivariate associations between covariates of interest and depression outcomes at 18 years (n = 9,665)a
| Total | Probable depression at 18 years |
Depression severity at 18 years |
|||
|---|---|---|---|---|---|
| n (%) | (%)b | p-valuec | Mean (SD) | p-valuec | |
| Total | 9665 (100.0) | 767 (7.9) | 3.20 (3.95) | ||
| Adversity trajectory group | |||||
| 1 - Stable low | 4472 (46.3) | 289 (6.5) | <0.001 | 2.67 (3.55) | <0.001 |
| 2 - Stable mild | 3589 (37.1) | 287 (8.0) | 3.31 (3.98) | ||
| 3 - Decreasing from moderate to mild | 856 (8.9) | 100 (11.7) | 4.46 (4.56) | ||
| 4 - Increasing from mild to high | 508 (5.3) | 61 (12.0) | 4.39 (4.53) | ||
| 5 - Stable high | 240 (2.5) | 30 (12.3) | 4.58 (4.60) | ||
| Child sex | |||||
| Male | 4983 (51.6) | 234 (4.7) | <0.001 | 2.49 (3.38) | <0.001 |
| Female | 4682 (48.4) | 533 (11.4) | 3.97 (4.34) | ||
| Highest level of parental education | |||||
| Below O-level | 1546 (16.0) | 126 (8.1) | 0.360 | 3.22 (3.98) | 0.117 |
| O-level | 2607 (27.0) | 214 (8.2) | 3.12 (3.95) | ||
| A-level | 3238 (33.5) | 273 (8.4) | 3.34 (4.03) | ||
| University degree or higher | 2274 (23.5) | 155 (6.8) | 3.10 (3.78) | ||
| Maternal depression or anxiety during pregnancyd | |||||
| No | 8133 (84.2) | 605 (7.4) | 0.007 | 3.01 (3.81) | <0.001 |
| Yes | 1532 (15.8) | 162 (10.6) | 4.22 (4.45) | ||
| Maternal age at child’s birth | |||||
| 15–24 years | 1728 (17.9) | 186 (10.8) | 0.002 | 3.53 (4.23) | 0.016 |
| 25–39 years | 3859 (39.9) | 302 (7.8) | 3.13 (3.91) | ||
| 30–34 years | 3007 (31.1) | 206 (6.8) | 3.12 (3.84) | ||
| 35–44 years | 1071 (11.1) | 73 (6.9) | 3.18 (3.86) | ||
Depression outcomes were assessed with the Clinical Interview Schedule-Revised (CIS-R)
Percentages reflect the prevalence of probable depression in each category
p-values from Chi-square tests, t-tests, or ANOVA
Crown-Crisp Experiential Index (CCEI) anxiety scale score > 10, CCEI depression scale score > 9, or Edinburgh Postnatal Depression Scale (EPDS) score > 12 at 18 weeks gestation
Using logistic regression models, adversity trajectory group membership remained associated with a probable diagnosis of depression at age 18 when adjusting for child sex, parental education, maternal mental health during pregnancy, and maternal age at birth (Table 2). The decreasing adversity (Odds Ratio [OR]=1.72, 95% Confidence Interval [CI]=1.19–2.48), increasing adversity (OR=1.81, 95% CI=1.15–2.86), and stable-high adversity groups (OR=1.80, 95% CI=1.00–3.23) exhibited similarly elevated risk of probable depression at age 18 years, compared to those with stable-low adversity. Results of negative binomial regression models of depression severity were similar to those of probable depression, with increasing depression severity across trajectory groups defined by higher levels of adversity at one or more time points. Female sex remained associated with both probable depression and depression severity in adjusted models, and maternal anxiety or depression during pregnancy remained associated with depression severity in the adjusted model (Table 2).
Table 2.
Results of unadjusted and adjusted models predicting depression outcomes at 18 years (n = 9,665)a
| Probable depression at 18 years | Depression severity at 18 years | |||
|---|---|---|---|---|
| Unadjustedb | Adjustedb | Unadjustedc | Adjustedc | |
| OR (95% CI) | OR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Adversity trajectory group | ||||
| 1 - Stable low | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| 2 - Stable mild | 1.26 (0.98–1.61) | 1.22 (0.94–1.58) | 1.24 (1.14–1.35) | 1.21 (1.11–1.32) |
| 3 - Decreasing from moderate to mild | 1.91 (1.37–2.68) | 1.72 (1.19–2.48) | 1.67 (1.46–1.90) | 1.54 (1.34–1.78) |
| 4 - Increasing from mild to high | 1.96 (1.26–3.06) | 1.81 (1.15–2.86) | 1.64 (1.37–1.95) | 1.55 (1.29–1.86) |
| 5 - Stable high | 2.01 (1.19–3.40) | 1.80 (1.00–3.23) | 1.71 (1.37–2.13) | 1.54 (1.22–1.95) |
| Child sex | ||||
| Male | 1.00 (ref) | 1.00 (ref) | ||
| Female | 2.61 (2.07–3.29) | 1.60 (1.48–1.72) | ||
| Highest level of parental education | ||||
| Below O-level | 1.01 (0.64–1.59) | 0.97 (0.84–1.11) | ||
| O-level | 1.05 (0.73–1.49) | 0.95 (0.85–1.06) | ||
| A-level | 1.14 (0.85–1.54) | 1.04 (0.94–1.14) | ||
| University degree or higher | 1.00 (ref) | 1.00 (ref) | ||
| Maternal depression or anxiety during pregnancyd | ||||
| No | 1.00 (ref) | 1.00 (ref) | ||
| Yes | 1.17 (0.85–1.62) | 1.22 (1.09–1.37) | ||
| Maternal age at child’s birth | ||||
| 15–24 years | 1.45 (0.96–2.20) | 1.03 (0.89–1.20) | ||
| 25–39 years | 1.11 (0.79–1.55) | 0.97 (0.87–1.09) | ||
| 30–34 years | 0.98 (0.70–1.36) | 0.98 (0.88–1.10) | ||
| 35–44 years | 1.00 (ref) | 1.00 (ref) | ||
Depression outcomes were assessed with the Clinical Interview Schedule-Revised (CIS-R)
Using logistic regression; OR = odds ratio; CI = confidence interval
Using negative binomial regression; IRR = incident rate ratio
Crown-Crisp Experiential Index (CCEI) anxiety scale score > 10, CCEI depression scale score > 9, or Edinburgh Postnatal Depression Scale (EPDS) score > 12 at 18 weeks gestation
Trajectory groupings were similar when using alternate measures of adversity, and for both males and females when examining sex-stratified samples (eFigures 1–4 and eTable 9). Associations between these alternate and stratified trajectory groups and depression outcomes were similar to the main results provided here (eTables 6–7), as were results when examining depressive symptoms at younger ages (eTable 8). Finally, results of the complete case analysis were similar to the results when using the imputed sample (eFigure 5 and eTables 10–11).
DISCUSSION
Using prospectively collected information on ten different domains of childhood adversity among a large sample of young adults, we identified five major trajectories of adversity from birth through late childhood. Although the majority of study participants experienced consistently low or mild levels of adversity, membership in trajectory groups with higher adversity was positively associated with depression risk. Unexpectedly, participants who experienced decreases from or increases to moderate or high levels of adversity at some point in childhood exhibited similar depression risk and severity in young adulthood to those who experienced consistently high levels of adversity.
Young adults in the trajectory groups characterized by moderate levels of adversity at one or more time points (i.e., the increasing, decreasing, and stable-high groups) experienced more adverse depression outcomes than those with consistently low levels of adversity throughout childhood, reflecting the well-established association between childhood adversity and poorer mental health (Benjet et al., 2010; Björkenstam et al., 2017; Dunn et al., 2017, 2018; Gilman et al., 2003; Mersky et al., 2013; Oldehinkel & Ormel, 2015; Schilling et al., 2007, 2008). These findings highlight the importance of considering adverse exposures at multiple time points throughout childhood to capture the potential for health risks as a result of childhood circumstances. Even though adverse exposures steadily declined in our decreasing adversity group (Group 3), risk for depression in young adulthood remained elevated. This finding is consistent with several studies that have found increased depressive symptoms in adolescence and adulthood among those with maltreatment, higher cumulative adversity, or poverty in early childhood (Atkinson et al., 2015; Dunn, McLaughlin, Slopen, Rosand, & Smoller, 2013; Dunn et al., 2017; Kaplow & Widom, 2007; Manly et al., 2001; Shanahan, Copeland, Costello, & Angold, 2011; Teicher, Samson, Polcari, & Andersen, 2009; Thornberry et al., 2010), although some of these studies failed to distinguish between childhood-limited and persistent adversity that began in early childhood. Adversity during early childhood may disrupt the development of critical brain structures and stress response systems or may initiate a chain of other stressors and adjustment difficulties that in turn influence mental health risk (Culpin et al., 2015; English, Graham, Litrownik, Everson, & Bangdiwala, 2005; McLaughlin et al., 2010; Rutter, Kim-Cohen, & Maughan, 2006; Schalinski et al., 2017).
We also found evidence for an elevated risk of depression among individuals who experienced increases in adversity as they reached late childhood (Group 4), consistent with previous studies finding increased risk of depression in adolescence and young adulthood among those experiencing poverty or maltreatment in late childhood or early adolescence (Harpur et al., 2015; Najman et al., 2010; Schalinski et al., 2016; Thornberry et al., 2001). These associations may represent stronger effects of events occurring closer in time to the assessment of mental health outcomes than events occurring earlier (Dunn et al., 2018; Harpur et al., 2015; Shanahan et al., 2011) or may reflect particular vulnerability to adversity occurring as children transition into more independence and experience significant brain development during adolescence (Harpur et al., 2015; Schalinski et al., 2016; Thornberry et al., 2001).
The increasing, decreasing, and chronically high adversity trajectory groups (Groups 3–5) shared similar depression risk and severity, which was surprising given past findings that chronic childhood maltreatment and other adversities persisting across multiple developmental stages are associated with the highest risk of health problems later in life (Jaffee & Maikovich-Fong, 2011; Slopen et al., 2014), as is longer duration of adversity (Dunn et al., 2018). Bøe and colleagues derived trajectories of family income across middle childhood and adolescence in a large sample of Norwegian young adults and found consistent risks of many mental health outcomes including depression among those who were persistently poor and those who moved into or out of poverty (Bøe et al., 2017), similar to our results. Other studies have not found effects of the particular timing of adversities (Björkenstam et al., 2017). It is worth noting that we observed the same pattern of results when examining self-reported depressive symptoms across trajectory groups at ages 12.5 and 13.5 (eTable 8), suggesting that our results hold across both short- and longer-term measures of mental health, though analyses should be replicated among a higher risk sample with greater exposures to adversity. In particular, the stable-high adversity group was relatively small in our sample, limiting inferences and precision with respect to depression outcomes in this group. Taken together with previous work, however, our results indicate that moderate to high levels of adversity experienced at any time in childhood increase risk for subsequent depression, with relatively consistent risk associated with adversity in early or later childhood, regardless of duration of exposure.
Our group-based trajectory modeling approach to measuring childhood adversity incorporated the frequent co-occurrence of adverse experiences and simultaneously reflected the accumulation, timing, and chronicity of adversity. Like previous studies of childhood adversity in population-based samples (Björkenstam et al., 2017; Mersky et al., 2013; Perales et al., 2013; St Clair et al., 2015), although many of our study participants reported low levels of adversity throughout childhood, more than one third experienced mild levels and about one-sixth were exposed to moderate or higher levels of adversity at some time during childhood. Also similar to other studies generally finding stability among adversity measures assessed at multiple time points (Atkinson et al., 2015; Dunn et al., 2018), most of our study participants reported relatively stable adversity throughout childhood. However, we did identify small proportions of children who experienced decreasing and increasing adversity throughout childhood, highlighting the clinical and research importance of assessing adversity at multiple times throughout childhood in order to correctly classify children’s adversity experience. This is consistent with studies of economic trajectories, in which some households move into and out of poverty during childhood (Bøe et al., 2017; Shuey & Willson, 2014), and has also been observed in studies of maltreatment, in which abuse experiences are time-limited for some children (English et al., 2005; Jaffee & Maikovich-Fong, 2011; Manly et al., 2001; Thornberry et al., 2010).
This study has several limitations. Adverse exposures of study children were reported by their parents throughout childhood. Some types of exposures (e.g., child abuse, parental substance use) are likely under-reported and reporting may have been influenced by parental mental health. We combined information across ten domains to characterize childhood adversity; although our findings were robust to alternate specifications of this measure, other weighting schemes may have better accounted for the severity of different types of events. We were not able to assess adversity trajectories past age 11.5 years because of data limitations. Substantial attrition occurred over the 18 years of follow-up considered in this analysis, with differential loss to follow-up among those with greater childhood adversity and higher risk of mental health problems. We used multiple imputation to retain some of those lost to follow-up, including prior measures of mental health in our imputation model and restricting our analysis to those with adequate childhood adversity information. However, our imputed analysis may not reflect the true unbiased associations of interest given the large amount of missing data for our outcome measures; furthermore, childhood adversity and depression outcomes were likely underestimated in this analysis given our restriction to the sample with adequate non-missing adversity information. Finally, the ALSPAC cohort is predominantly white, with the majority of the cohort experiencing low or mild levels of adversity throughout childhood; these results may not be generalizable to more diverse populations with higher levels of adversity.
CONCLUSION
Despite these limitations, our findings extend previous work on cumulative adversity and specific childhood adversities among this birth cohort (Bowes et al., 2015; Bowes, Wolke, Joinson, Lereya, & Lewis, 2014; Dunn et al., 2018; Slopen et al., 2014, 2013; Stapinski et al., 2014) by identifying robust trajectories of childhood adversity and their effects on depression risk and severity in young adulthood. These results highlight the need for regular, periodic screening of adversity throughout childhood to identify children at greatest risk of depression. Future studies should aim to investigate the differential impact of specific types of adversities (Dunn et al., 2017, 2018) occurring during specific developmental periods (Schalinski et al., 2017, 2016) and to assess the effects of adversity trajectories on other mental health and behavioral outcomes (English et al., 2005; Kaplow & Widom, 2007) and on depression at later ages. Further work is also needed to better understand the biological, behavioral, and social mechanisms that may link these trajectories of childhood adversity to depression in young adulthood and beyond (Costello et al., 2008; Culpin et al., 2015; McLaughlin et al., 2010; McLaughlin & Sheridan, 2016; Shuey & Willson, 2014; Teicher et al., 2009; Wickrama, Conger, Lorenz, & Jung, 2008; Wickrama, Noh, & Elder, 2009), as well as protective factors that may promote resilience among children exposed to moderate or high levels of adversity at different stages of childhood (Hatch, 2005), in order to develop and target interventions to reduce the detrimental effects of childhood adversity.
Supplementary Material
ACKNOWLEDGEMENTS
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council and the Wellcome Trust (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. A comprehensive list of grant funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf); collection of outcome information was specifically funded by the Wellcome Trust (Grant ref: 08426812/Z/07/Z). This publication is the work of the authors, who will serve as guarantors for the contents of this paper. This work was partially supported by a grant to the Center for Social and Demographic Analysis (CSDA) from the National Institute of Child Health and Human Development of the National Institutes of Health [R24-HD044943]. Allison Appleton is supported by a JPB Environmental Health Fellowship award granted by the JPB Foundation and managed by the Harvard T.H. Chan School of Public Health.
REFERENCES
- Andruff H, Carraro N, Thompson A, Gaudreau P, & Louvet B (2009). Latent Class Growth Modelling: A Tutorial. Tutorials in Quantitative Methods for Psychology, 5(1), 11–24. [Google Scholar]
- Angold A, Costello EJ, Messer SC, & Pickles A (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5(4), 237–249. [Google Scholar]
- Appleton AA, Holdsworth E, Ryan M, & Tracy M (2017). Measuring childhood adversity in life course cardiovascular research: A systematic review. Psychosomatic Medicine, 79(4), 434–440. [DOI] [PubMed] [Google Scholar]
- Atkinson L, Beitchman J, Gonzalez A, Young A, Wilson B, Escobar M, … Villani V (2015). Cumulative risk, cumulative outcome: a 20-year longitudinal study. PloS One, 10(6), e0127650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Borges G, & Medina-Mora ME (2010). Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. Journal of Psychiatric Research, 44(11), 732–740. [DOI] [PubMed] [Google Scholar]
- Berglund PA (2015). Multiple imputation using the fully conditional specification method: a comparison of SAS, Stata, IVEware, and R. In Paper 2081–2015. Retrieved from http://support.sas.com/resources/papers/proceedings15/2081-2015.pdf [Google Scholar]
- Björkenstam E, Pebley AR, Burström B, & Kosidou K (2017). Childhood social adversity and risk of depressive symptoms in adolescence in a US national sample. Journal of Affective Disorders, 212, 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøe T, Skogen JC, Sivertsen B, Hysing M, Petrie KJ, Dearing E, & Zachrisson HD (2017). Economic volatility in childhood and subsequent adolescent mental health problems: a longitudinal population-based study of adolescents. BMJ Open, 7(9), e017030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouma EMC, Ormel J, Verhulst FC, & Oldehinkel AJ (2008). Stressful life events and depressive problems in early adolescent boys and girls: the influence of parental depression, temperament and family environment. Journal of Affective Disorders, 105(1–3), 185–193. [DOI] [PubMed] [Google Scholar]
- Bowes L, Joinson C, Wolke D, & Lewis G (2015). Peer victimisation during adolescence and its impact on depression in early adulthood: prospective cohort study in the United Kingdom. BMJ (Clinical Research Ed.), 350, h2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowes L, Wolke D, Joinson C, Lereya ST, & Lewis G (2014). Sibling bullying and risk of depression, anxiety, and self-harm: a prospective cohort study. Pediatrics, 134(4), e1032–1039. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, … Davey Smith G (2013). Cohort Profile: the ‘children of the 90s’--the index offspring of the Avon Longitudinal Study of Parents and Children. International Journal of Epidemiology, 42(1), 111–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, & Giles WH (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389–396. [DOI] [PubMed] [Google Scholar]
- Cerda M, Vlahov D, Tracy M, & Galea S (2008). Alcohol use trajectories among adults in an urban area after a disaster: evidence from a population-based cohort study. Addiction, 103(8), 1296–1307. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. [DOI] [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, & Naimark B (2010). Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse & Neglect, 34(6), 454–464. [DOI] [PubMed] [Google Scholar]
- Costello DM, Swendsen J, Rose JS, & Dierker LC (2008). Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. Journal of Consulting and Clinical Psychology, 76(2), 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry: The Journal of Mental Science, 150, 782–786. [DOI] [PubMed] [Google Scholar]
- Crown S, & Crisp AH (1979). Manual of the Crown-Crisp Experiential Index. London: Hodder and Staughton. [Google Scholar]
- Culpin I, Stapinski L, Miles ÖB, Araya R, & Joinson C (2015). Exposure to socioeconomic adversity in early life and risk of depression at 18 years: The mediating role of locus of control. Journal of Affective Disorders, 183, 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, & Smoller JW (2013). Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the National Longitudinal Study of Adolescent Health. Depression and Anxiety, 30(10), 955–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Powers A, & Bradley B (2017). Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? Journal of Psychiatric Research, 84, 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Soare TW, Raffeld MR, Busso DS, Crawford KM, Davis KA, … Susser ES (2018). What life course theoretical models best explain the relationship between exposure to childhood adversity and psychopathology symptoms: recency, accumulation, or sensitive periods? Psychological Medicine, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, & Anda RF (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. The American Journal of Psychiatry, 160(8), 1453–1460. [DOI] [PubMed] [Google Scholar]
- English DJ, Graham JC, Litrownik AJ, Everson M, & Bangdiwala SI (2005). Defining maltreatment chronicity: are there differences in child outcomes? Child Abuse & Neglect, 29(5), 575–595. [DOI] [PubMed] [Google Scholar]
- Evans GW, Li D, & Whipple SS (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342–1396. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ, & Horwood LJ (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine, 30(1), 23–39. [DOI] [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, … Lawlor DA (2013). Cohort Profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. International Journal of Epidemiology, 42(1), 97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo EAG, Munhoz TN, Loret de Mola C, & Murray J (2018). Gender differences in the effects of childhood maltreatment on adult depression and anxiety: A systematic review and meta-analysis. Child Abuse & Neglect, 79, 107–114. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, & Buka L (2003). Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychological Medicine, 33(8), 1341–1355. [DOI] [PubMed] [Google Scholar]
- Glied S, & Pine DS (2002). Consequences and Correlates of Adolescent Depression. Archives of Pediatrics & Adolescent Medicine, 156(10), 1009–1014. [DOI] [PubMed] [Google Scholar]
- Goodman A, Heiervang E, Collishaw S, & Goodman R (2011). The “DAWBA bands” as an ordered-categorical measure of child mental health: description and validation in British and Norwegian samples. Social Psychiatry and Psychiatric Epidemiology, 46(6), 521–532. [DOI] [PubMed] [Google Scholar]
- Goodman R (1997). The Strengths and Difficulties Questionnaire: a research note. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 38(5), 581–586. [DOI] [PubMed] [Google Scholar]
- Goodman R (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1337–1345. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Richards H, Gatward R, & Meltzer H (2000). The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 41(5), 645–655. [PubMed] [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, & Meltzer H (2000). Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. The British Journal of Psychiatry, 177(6), 534–539. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67(2), 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerton G, Mahedy L, Mars B, Harold GT, Thapar A, Zammit S, & Collishaw S (2015). Association between Maternal Depression Symptoms across the First Eleven Years of Their Child’s Life and Subsequent Offspring Suicidal Ideation. PloS One, 10(7), e0131885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpur LJ, Polek E, & van Harmelen A-L (2015). The role of timing of maltreatment and child intelligence in pathways to low symptoms of depression and anxiety in adolescence. Child Abuse & Neglect, 47, 24–37. [DOI] [PubMed] [Google Scholar]
- Hatch SL (2005). Conceptualizing and identifying cumulative adversity and protective resources: implications for understanding health inequalities. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60 Spec No 2, 130–134. [DOI] [PubMed] [Google Scholar]
- Haviland AM, Jones BL, & Nagin DS (2011). Group-based Trajectory Modeling Extended to Account for Nonrandom Participant Attrition. Sociological Methods & Research, 40(2), 367–390. [Google Scholar]
- Jaffee SR, & Maikovich-Fong AK (2011). Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 52(2), 184–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins R, Bebbington P, Brugha T, Farrell M, Gill B, Lewis G, … Petticrew M (2003). The National Psychiatric Morbidity Surveys of Great Britain--strategy and methods. International Review of Psychiatry (Abingdon, England), 15(1–2), 5–13. [DOI] [PubMed] [Google Scholar]
- Jones B, Nagin D, & Roeder K (2001). A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research, 29, 374–393. [Google Scholar]
- Kaplow JB, & Widom CS (2007). Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology, 116(1), 176–187. [DOI] [PubMed] [Google Scholar]
- Lewis G (1994). Assessing psychiatric disorder with a human interviewer or a computer. Journal of Epidemiology and Community Health, 48(2), 207–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G, Pelosi AJ, Araya R, & Dunn G (1992). Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychological Medicine, 22(2), 465–486. [DOI] [PubMed] [Google Scholar]
- Lloyd DA, & Turner RJ (2008). Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug and Alcohol Dependence, 93(3), 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: contributions of developmental timing and subtype. Development and Psychopathology, 13(4), 759–782. [PubMed] [Google Scholar]
- McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, & Koenen KC (2010). Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depression and Anxiety, 27(12), 1087–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond Cumulative Risk: A Dimensional Approach to Childhood Adversity. Current Directions in Psychological Science, 25(4), 239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer H, Gill B, Petticrew M, & Hinds K (1995). The OPCS Surveys of Psychiatric Morbidity. Report I: The prevalence of psychiatric morbidity among adults aged 16–64 living in private households in Great Britain. London: HMSO. [Google Scholar]
- Mersky JP, Topitzes J, & Reynolds AJ (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect, 37(11), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS (2005). Group-Based Modeling of Development. Harvard University Press. [Google Scholar]
- Najman JM, Hayatbakhsh MR, Clavarino A, Bor W, O’Callaghan MJ, & Williams GM (2010). Family poverty over the early life course and recurrent adolescent and young adult anxiety and depression: a longitudinal study. American Journal of Public Health, 100(9), 1719–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobile M, Colombo P, Bellina M, Molteni M, Simone D, Nardocci F, … Battaglia M (2013). Psychopathology and adversities from early- to late-adolescence: a general population follow-up study with the CBCL DSM-Oriented Scales. Epidemiology and Psychiatric Sciences, 22(1), 63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldehinkel AJ, & Ormel J (2015). A longitudinal perspective on childhood adversities and onset risk of various psychiatric disorders. European Child & Adolescent Psychiatry, 24(6), 641–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perales J, Olaya B, Fernandez A, Alonso J, Vilagut G, Forero CG, … Haro JM (2013). Association of childhood adversities with the first onset of mental disorders in Spain: results from the ESEMeD project. Social Psychiatry and Psychiatric Epidemiology, 48(3), 371–384. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, & Wilkinson G (2000). Gender differences in depression. Critical review. The British Journal of Psychiatry: The Journal of Mental Science, 177, 486–492. [DOI] [PubMed] [Google Scholar]
- Raposa EB, Hammen CL, Brennan PA, O’Callaghan F, & Najman JM (2014). Early adversity and health outcomes in young adulthood: the role of ongoing stress. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 33(5), 410–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Kim-Cohen J, & Maughan B (2006). Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 47(3–4), 276–295. [DOI] [PubMed] [Google Scholar]
- Schalinski I, Breinlinger S, Hirt V, Teicher MH, Odenwald M, & Rockstroh B (2017). Environmental adversities and psychotic symptoms: The impact of timing of trauma, abuse, and neglect. Schizophrenia Research. [DOI] [PubMed] [Google Scholar]
- Schalinski I, Teicher MH, Nischk D, Hinderer E, Müller O, & Rockstroh B (2016). Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry, 16, 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2007). Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health, 7, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2008). The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Social Science & Medicine, 66(5), 1140–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Costello EJ, & Angold A (2011). Child-, adolescent- and young adult-onset depressions: differential risk factors in development? Psychological Medicine, 41(11), 2265–2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuey KM, & Willson AE (2014). Economic hardship in childhood and adult health trajectories: An alternative approach to investigating life-course processes. Advances in Life Course Research, 22, 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Koenen KC, & Kubzansky LD (2014). Cumulative adversity in childhood and emergent risk factors for long-term health. The Journal of Pediatrics, 164(3), 631–638.e1–2. [DOI] [PubMed] [Google Scholar]
- Slopen N, Kubzansky LD, McLaughlin KA, & Koenen KC (2013). Childhood adversity and inflammatory processes in youth: a prospective study. Psychoneuroendocrinology, 38(2), 188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Clair MC, Croudace T, Dunn VJ, Jones PB, Herbert J, & Goodyer IM (2015). Childhood adversity subtypes and depressive symptoms in early and late adolescence. Development and Psychopathology, 27(3), 885–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapinski LA, Bowes L, Wolke D, Pearson RM, Mahedy L, Button KS, … Araya R (2014). Peer victimization during adolescence and risk for anxiety disorders in adulthood: a prospective cohort study. Depression and Anxiety, 31(7), 574–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, Polcari A, & Andersen SL (2009). Length of time between onset of childhood sexual abuse and emergence of depression in a young adult sample: a retrospective clinical report. The Journal of Clinical Psychiatry, 70(5), 684–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Ireland TO, & Smith CA (2010). The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 46(4), 359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Ireland TO, & Smith CA (2001). The importance of timing: the varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Development and Psychopathology, 13(4), 957–979. [PubMed] [Google Scholar]
- Tracy M, Hobfoll SE, Canetti-Nisim D, & Galea S (2008). Predictors of depressive symptoms among israeli jews and arabs during the Al aqsa intifada: a population-based cohort study. Annals of Epidemiology, 18(6), 447–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, & Lloyd DA (1995). Lifetime traumas and mental health: the significance of cumulative adversity. Journal of Health and Social Behavior, 36(4), 360–376. [PubMed] [Google Scholar]
- van Buuren S (2007). Multiple imputation of discrete and continuous data by fully conditional specification. Statistical Methods in Medical Research, 16(3), 219–242. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Gameroff MJ, Warner V, Pilowsky D, Kohad RG, … Talati A (2016). Offspring of Depressed Parents: 30 Years Later. The American Journal of Psychiatry, 173(10), 1024–1032. [DOI] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Keane EM, Spicer P, Turner RJ, & AI-SUPERPFP Team. (2007). The relationship of cumulative and proximal adversity to onset of substance dependence symptoms in two American Indian communities. Drug and Alcohol Dependence, 91(2–3), 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K. a. S., Conger RD, Lorenz FO, & Jung T (2008). Family antecedents and consequences of trajectories of depressive symptoms from adolescence to young adulthood: a life course investigation. Journal of Health and Social Behavior, 49(4), 468–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K. a. S., Noh S, & Elder GH (2009). An investigation of family SES-based inequalities in depressive symptoms from early adolescence to emerging adulthood. Advances in Life Course Research, 14(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner M, Weichold K, & Silbereisen RK (2007). Trajectories of alcohol use among adolescent boys and girls: identification, validation, and sociodemographic characteristics. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 21(1), 62–75. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.