Abstract
Background
Meaning and purpose in life are associated with cancer patients’ and survivors’ mental and physical health and also constitute highly valued outcomes in themselves. Because meaning and purpose are often threatened by cancer diagnosis and treatment, interventions have been developed to promote meaning and purpose. The present meta-analysis of randomized controlled trials (RCTs) evaluated effects of psychosocial interventions on meaning/purpose in adults with cancer and tested potential moderators of intervention effects.
Methods
Six literature databases were systematically searched to identify RCTs of psychosocial interventions in which meaning or purpose was an outcome. Rater pairs extracted and evaluated data for quality using PRISMA guidelines. Findings were synthesized across studies using standard meta-analytic methods, including meta-regression with robust variance estimation and risk-of-bias sensitivity analysis.
Results
Twenty-nine RCTs were identified, encompassing 82 treatment effects among 2,305 patients/survivors. Psychosocial interventions were associated with significant improvements in meaning/purpose (g = 0.37, 95% CI: [0.22, 0.52], p < .0001). Interventions designed to enhance meaning/purpose (g = 0.42, 95% CI: [0.24, 0.60]) demonstrated significantly higher effect sizes than those targeting other primary outcomes (g = 0.18, 95% CI: [0.09, 0.27]; p = .009). Few other intervention, clinical, or demographic characteristics tested were significant moderators.
Conclusion
Results suggest psychosocial interventions are associated with small-to-medium effects in enhancing meaning/purpose among cancer patients, comparable benefits to interventions designed to reduce depression, pain, and fatigue in patients with cancer. Methodological concerns include small samples and ambiguity regarding allocation concealment. Future research should focus on explicitly meaning-centered interventions and identify optimal treatment or survivorship phases for implementation.
Keywords: meta-analysis, cancer, meaning, purpose, interventions
Precis:
The present meta-analysis of randomized controlled trials (RCTs) evaluated effects of psychosocial interventions on meaning/purpose in adults with cancer and tested potential moderators of intervention effects.
Results suggest psychosocial interventions are associated with small-to-medium effects in enhancing meaning/purpose among cancer patients, comparable benefits to interventions designed to reduce depression, pain, and fatigue in patients with cancer.
Cancer diagnosis and treatment often disrupt many aspects of daily life, as patients experience unwelcome changes in their roles and responsibilities, perceptions of control, and expectations for the future. As a result, existential distress may become pronounced. Recently, interest has intensified in perceptions of meaning or purpose in life and their associations with health outcomes among cancer patients and survivors1, 2, 3. A sense of meaning and purpose in life refers to the extent to which people perceive the world to be understandable, feel committed to and motivated by valued goals, and experience their existence as significant in the larger scheme of the world—that they matter4.
Maintaining a sense that life is meaningful may help manage distress and enhance quality of life and physical health. Indeed, myriad investigations among cancer patients suggest that greater meaning in life is associated with more favorable psychological outcomes (e.g., less depression, hopelessness, and anxiety)5, 6, 7, 8, 9, 10, 11 and is also—more modestly—associated with positive physical health outcomes12, 13, 14. Moreover, meaning in life itself represents an important aspect of patient-reported outcomes inherently valued by patients15, 16, 17
A recent wave of interventions for cancer patients has been specifically designed to address existential/spiritual concerns or questions of personal meaning18, 19, 20, 21, 22, 23, 24, 25, 26. Psychosocial interventions designed to influence a wide array of psychological and even physical health outcomes might also affect meaning-related endpoints, even if these are not their singular or primary emphasis (e.g., coping skills, health education, or creative arts programs). A large and growing research base has evaluated psychosocial interventions for patients with various malignancies, and many of these trials have included outcomes concerning meaning or purpose. However, whether these interventions contribute to patients’ or survivors’ meaning in life remains unclear. Thus, we conducted a meta-analytic review to synthesize knowledge regarding psychosocial interventions to promote meaning and to identify areas needing further research.
Specifically, we synthesized findings from randomized trials evaluating effects of psychosocial interventions on meaning or purpose among oncology patients. Our primary study aim was to determine the magnitude of treatment effects on meaning-related outcomes. A secondary aim was to examine potential moderating effects of treatment, clinical, and demographic factors.
Method
Search Strategy
Studies were identified by searching electronic databases (Ovid MEDLINE, PsycInfo, CINAHL, EMBASE, Cochrane Central, and Web of Science), emailing professional listservs, and contacting study authors. Electronic searches were performed through September 14, 2018. For the MEDLINE search, we used the McMaster multi-term filters with the best balance of sensitivity and specificity for retrieving randomized controlled trials (RCTs)27 and systematic reviews28. Detailed search strategies for all databases are available in the supporting information online (Table A). Unpublished studies were requested from professional listservs (Society of Behavioral Medicine, American Psychosocial Oncology Society, and American Psychological Association). We attempted to acquire missing information from recently published papers by contacting 29 study authors; 10 responded and 6 of these provided additional information.
Eligibility Criteria
Studies were included if they: (1) evaluated a psychosocial intervention using an RCT design; (2) were written in English; (3) included an adult sample (≥18 years old) with a diagnosis of cancer; and (4) evaluated a meaning/purpose outcome (detailed below). Excluded studies focused on pharmacological or medical rather than psychosocial interventions; used qualitative assessments of the intervention; studied pediatric or caregiver samples; used a quasi-experimental design; or used a comparative treatment design with no control group.
Psychosocial interventions included those targeting thoughts, feelings, or behaviors. Psychosocial interventions were thus broadly defined and included (among others) existential or meaning-based therapies, cognitive-behavioral techniques, interpersonal or supportive-expressive interventions, coping skills or stress management, relaxation training, education, meditation, yoga, hypnosis, or other experiential techniques, provided in individual, group, or dyadic/family modalities. There were no restrictions on the type of psychosocial interventions included in the review.
Meaning Outcomes
Meaning is a complex construct that has been conceptualized in many different ways7, 29, 30. Several models construe “meaning in life” or personal meaning as encompassing core assumptions about life, hierarchically-ordered personal goals, and subjective perceptions of coherence, purpose, and significance29, 31. “Global meaning” (i.e., central beliefs and goals) has been distinguished from “situational meaning” (i.e., perceptions of specific experiences, such as cancer)32. Other investigators have differentiated “search for meaning” (i.e., efforts to derive understanding or purpose) from “found meaning” (i.e., resolution of those efforts)33, 34. The current investigation focused on measures encompassing facets of meaning in life or attained global meaning. We refer to these outcomes as “meaning/purpose,” “meaning in life,” or “perceived meaning.” We excluded measures more broadly assessing spiritual/religious wellbeing (e.g., the full FACIT-Sp Spiritual Wellbeing subscale35) or on perceived positive life changes (e.g., Posttraumatic Growth Inventory36, Benefit-Finding Scale37) because these measures assess conceptually distinct constructs. Measures ultimately retained in analyses included the meaning or meaning/peace subscales of the FACIT-Sp35, the existential wellbeing subscale of the McGill Quality of Life Scale38, the presence subscale of the Meaning in Life scale33, the meaningfulness subscale of the Sense of Coherence Scale39, the value of life subscale of the Quality of Life Concerns in the End of Life questionnaire40, the existential subscale of the Spiritual Wellbeing Scale41, the Self-Transcendence Scale42, the personal meaning index from the Life Attitude Profile (Revised)43, the Personal Meaning Profile44, and the purpose in life subscale from Ryff’s Scales of Psychological Well-Being45.
Study Selection
The review team included five raters, all with doctoral degrees and extensive experience coding psychosocial oncology studies for meta-analyses. Using the Cochrane technology platform Covidence (www.covidence.org), each abstract was reviewed by a rater pair to determine which articles merited full review. Studies possibly meeting inclusion criteria underwent full-text review by a pair of raters; each rater independently evaluated the study and abstracted data elements. Discrepancies were resolved by consensus within rater pairs.
Data Coding
Data extracted from each study included demographic and clinical information about the sample (average age, gender composition, cancer type, cancer stage, and phase of treatment/survivorship). We also coded RCTs based on several intervention characteristics: 1) intervention type using an adapted version of a framework developed to categorize psychosocial interventions46 (Meaning/Existential, Coping Skills-based, Meditation/Yoga, Education/Information, Creative Arts); 2) intervention modality (individual, dyad, group); 3) delivery format (in-person, audiovisual, print, telephone, Internet); 4) intervention target (i.e., whether an intervention was specifically designed to improve or “target” meaning or purpose); and 5) control condition type (waitlist, standard/usual care condition versus an active, attentional, educational, or component condition). If meaning or purpose was mentioned in the background of the paper as part of the theoretical orientation, in hypotheses/specific aims, or as a target in the intervention description, the intervention target variable was coded “yes”; if meaning or purpose was not mentioned in those key manuscript sections, the study was coded “no.” We extracted the specific measures used to assess target meaning and purpose outcomes and further coded these as primary, secondary, or unspecified outcomes based on authors’ descriptions of the relative importance of these measures to the study. Table 1 describes the demographic, clinical, and intervention characteristics of included studies.
Table 1.
Summary of demographic, clinical, and intervention characteristics
| Demographic or characteristic | M (SD) | Number of studies | Number of effect size estimates | Average ES [95% CI] | I2(%) | F (df1, df2) | P | |
|---|---|---|---|---|---|---|---|---|
| Average participant age | 57.2 (7.5) | 24 | 63 | 0.01 [−0.02, 0.03] | 0.37 | 78 | 0.59 (1, 7.9) | .465 |
| Percent female | 71.5 (25.8) | 25 | 67 | 0.00 [−0.01, 0.01] | 0.26 | 79 | 0.01 (1, 16.7) | .906 |
| Follow-up time (weeks from baseline) | 20.6 (7.5) | 29 | 82 | 0.00 [−0.01, 0.01] | 0.32 | 82 | 0.00 (1, 2.6) | .997 |
| Cancer typea | 70 | 0.01 (1, 20.4) | .925 | |||||
| Breast | 8 | 18 | 0.42 [0.18, 0.65] | 0.16 | ||||
| Other | 18 | 61 | 0.40 [0.16, 0.65] | 0.42 | ||||
| Not reported | 3 | 3 | 0.10 [−0.26, 0.46] | 0.00 | ||||
| Cancer stagea | 71 | 2.66 (2, 11.7) | .111 | |||||
| Early | 5 | 24 | 0.46 [0.13, 0.79] | 0.14 | ||||
| Advanced | 9 | 23 | 0.52 [0.14, 0.91] | 0.48 | ||||
| Mixed | 10 | 28 | 0.17 [−0.05, 0.39] | 0.17 | ||||
| Not reported | 5 | 7 | 0.27 [−0.13, 0.67] | 0.19 | ||||
| Cancer phasea | 70 | 1.50 (3, 8.9) | .281 | |||||
| Curative | 5 | 18 | 0.05 [−0.35, 0.44] | 0.22 | ||||
| Post-treatment | 5 | 20 | 0.34 [0.11, 0.57] | 0.00 | ||||
| Palliative | 6 | 18 | 0.65 [−0.05, 1.35] | 0.62 | ||||
| Mixed | 8 | 19 | 0.35 [0.09, 0.61] | 0.16 | ||||
| Not reported | 5 | 7 | 0.34 [−0.08, 0.77] | 0.25 | ||||
| Delivery format | 57 | 11.02 (1, 3.4) | .038 | |||||
| In-person | 27 | 78 | 0.40 [0.24, 0.56] | 0.32 | ||||
| Other | 2 | 4 | 0.09 [−0.60, 0.77] | 0.00 | ||||
| Intervention modalityb | 78 | 0.03 (2, 2.4) | .973 | |||||
| Individual | 17 | 45 | 0.37 [0.12, 0.62] | 0.42 | ||||
| Dyad | 2 | 4 | 0.32 [−2.38, 3.03] | 0.22 | ||||
| Group | 11 | 33 | 0.33 [0.14, 0.53] | 0.17 | ||||
| Control type | 85 | 0.00 (1, 13.2) | .965 | |||||
| Active/ attention/ education/ component | 9 | 19 | 0.38 [0.04, 0.71] | 0.38 | ||||
| Wait-list / standard care | 20 | 63 | 0.37 [0.19, 0.55] | 0.30 | ||||
| Intervention typeb,c | 75 | 2.57 (2, 14.0) | .112 | |||||
| Creative arts | 2 | 2 | 0.50 [−1.59, 2.59] | 0.00 | ||||
| Education/information | 1 | 3 | −0.0 [−0.21, 0.20] | 0.12 | ||||
| Meaning/existential | 13 | 32 | 0.56 [0.29, 0.84] | 0.38 | ||||
| Meditation/yoga | 8 | 23 | 0.19 [−0.09, 0.47] | 0.25 | ||||
| Coping skills-based | 8 | 22 | 0.28 [0.07, 0.48] | 0.16 | ||||
| Intervention targets meaning/purposeb | 74 | 8.63 (1, 17.8) | .009 | |||||
| No | 8 | 24 | 0.18 [0.09, 0.27] | 0.00 | ||||
| Yes | 24 | 58 | 0.42 [0.24, 0.60] | 0.34 | ||||
| Outcome measureb | 73 | 2.60 (2, 15.6) | .106 | |||||
| Primary | 13 | 33 | 0.52 [0.25, 0.80] | 0.39 | ||||
| Secondary | 7 | 21 | 0.19 [0.01, 0.38] | 0.08 | ||||
| Unspecified | 10 | 28 | 0.26 [−0.04, 0.55] | 0.30 | ||||
| Outcome scale | 78 | 1.28 (2, 9.5) | .323 | |||||
| FACIT-Sp meaning | 7 | 9 | 0.19 [−0.06, 0.45] | 0.13 | ||||
| FACIT-Sp meaning/peace | 9 | 15 | 0.48 [0.14, 0.81] | 0.36 | ||||
| McGill Quality of Life existential well-being | 6 | 22 | 0.28 [−0.29, 0.85] | 0.48 |
Notes:
a Test for between-group differences excludes “Not reported” group.
b Sum of number of studies is larger than 29 because some studies included effects from more than one category.
c Test for between-group differences excludes “Creative arts” and “Education/information” because these groups each contain fewer than 3 studies.
Assessment of Risk of Bias
Rater pairs independently reviewed each article and coded the following Risk of Bias categories relevant to our self-report outcomes: sequence generation, allocation concealment, attrition, and outcome reporting. Across all four categories, we used the coded values to inform a categorical assessment of bias risk as low, unclear, or high. Blinding of participants was not evaluated, because blinding is often not feasible for trials of psychosocial interventions, and blinding of outcome assessors was not considered because all studies used self-reported outcomes. Discrepancies were resolved by consensus within pairs of raters.
Effect Size Calculations and Meta-Analytic Procedures
For quantifying the effects of psychosocial interventions on meaning and purpose outcomes, we used standardized mean differences between treatment and control groups, estimated using Hedge’s g correction47. For the numerator of the effect size estimate, we used the estimated difference between treatment and control groups, adjusted for baseline differences (i.e., change-score adjustment or regression adjustment). We estimated the denominator of the effect size using pre-intervention standard deviations in the outcome, pooled across groups. For two studies lacking baseline data48, 49, we used unadjusted differences between groups at post-test and standardized based on the pooled variance at post-test. We calculated effect size estimates from reported mean and SD estimates by group if available; otherwise, we used reported statistical tests (e.g., t- or F-statistics, p-values) to calculate comparable effect size estimates.
An examination of the distribution of raw effect size estimates included in the meta-analysis revealed several positive outliers. We used Tukey’s50 definition of outliers as values below the 1st quartile minus 3 times the inter-quartile range (g = −1.05) or above the 3rd quartile plus 3 times the interquartile range (g=1.57). Two outlying effect size estimates (both from Xiao51) at the high end of the distribution were re-coded (i.e., winsorized) to the corresponding upper fence value52.
Many included studies reported intervention effects on multiple measures of meaning and purpose and/or at multiple follow-up time points. Effect size estimates for multiple measures or time points are correlated because they are based on a common sample, yet the information necessary to estimate the degree of correlation is seldom available from published sources. Such was the case with the included studies. Therefore, to synthesize effect size estimates across included studies, we used random effects meta-analysis in combination with robust variance estimation techniques53 to account for potential dependencies among effect size estimates from common samples. Specifically, we used a “correlated effects” working model, assuming a correlation of 0.7, as well as small-sample corrections to standard errors, hypothesis tests, and confidence intervals54, 55. We used restricted maximum likelihood estimates of the between-study standard deviation, denoted as , to measure the extent of heterogeneity among the effect sizes. We also report the I2 statistic, a relative measure of the extent to which heterogeneity among true effect sizes contributes to observed variation in effect size estimates56. To examine differences in effect size across moderating variables, we used random effects meta-regression models that allowed for both the average effect size and the between-study variance to differ across levels of the moderator.
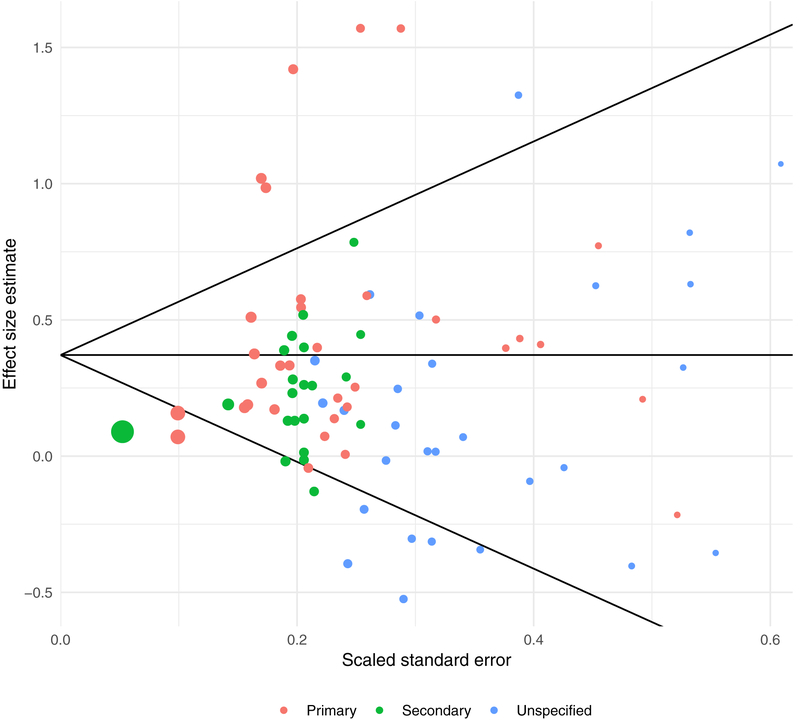
To investigate possible risks of bias due to incomplete outcome reporting, we examined a funnel plot of effect size estimates and conducted a modified version of Egger’s regression test for funnel plot asymmetry. The funnel plot asymmetry test examines the association between the magnitude of effect size estimates and a measure of their precision. To measure precision, we used the scaled standard error, calculated as the standard error of the numerator of the effect size estimate, scaled by the denominator of the effect size estimate; the scaled standard error was used to avoid artifactual association between the effect size estimate and its standard error57. The funnel plot asymmetry test also used robust variance estimation to account for dependence of effect size estimates nested within studies.
All analyses were conducted using the metafor package58 and clubSandwich package59 for the R statistical computing environment. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA60) was used to guide our reporting of results. Raw data (including effect size estimates, variance estimates, and moderator variables) and code for replicating all reported analyses are available in the accompanying supplementary materials.
Results
Study Selection
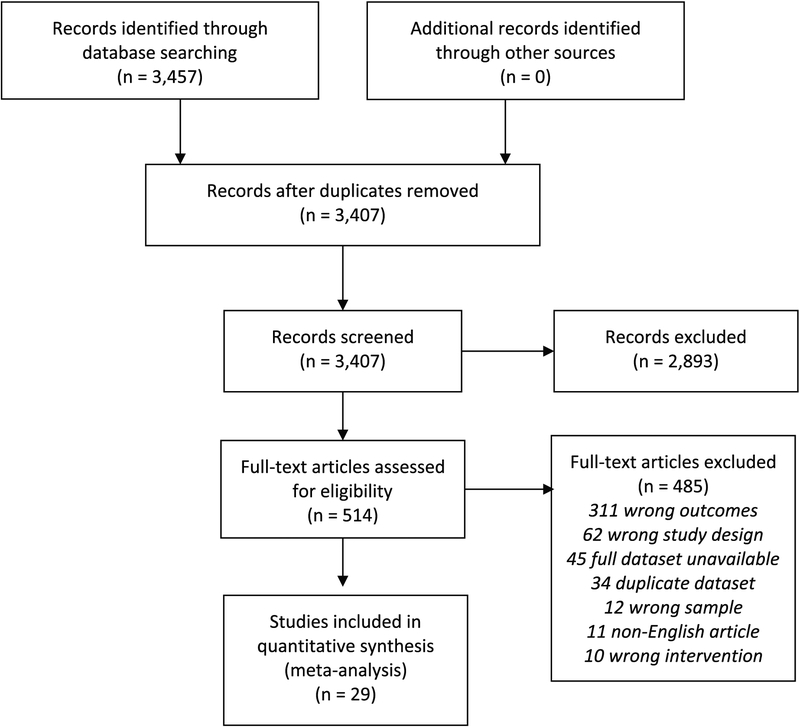
The electronic database search retrieved 3,457 citations (Figure 1). After removal of duplicates, 3,407 remained and were evaluated on the basis of title and abstract. Of these, 2,893 clearly did not meet the inclusion criteria and were discarded, and 514 were assessed further using full texts. Of these, 485 did not meet the inclusion criteria; 29 did and were included in analyses18, 21, 24, 48, 49, 51, 61–83. All studies included in the meta-analysis are denoted with **.
Figure 1.
PRISMA Flow Diagram
Overall Description of Studies and Effects
Meta-analysis included 29 RCTs encompassing 82 effect sizes (including between 1 and 12 per study, with a median of 2) and a combined sample of 2,305 participants. The weighted average effect of meaning and purpose outcomes was estimated as g = 0.371, 95% CI [0.221, 0.521], p < .0001, denoting significant intervention effects of small-to-moderate magnitude. The estimated between-study standard deviation was (I2 = 82%), indicating substantial heterogeneity of effects across studies.
Leave-one-out sensitivity analyses indicated that the estimated effect size distribution was influenced by two studies with outlying effect size estimates. Effect size estimates remained significant when these studies were eliminated from the analyses. More specifically, excluding the single eligible effect size estimate reported in Ando61 (g = 1.42, SE = 0.23) reduced the overall average effect estimate to g = 0.318, 95% CI [0.193, 0.443], p < .0003 and the between-study heterogeneity estimate to . Excluding the two effect size estimates reported in Xiao51 (both winsorized to g = 1.57, SEs = 0.34 and 0.38) reduced the overall average effect estimate to g = 0.333, 95% CI [0.197, 0.470], p < .0001 and the between-study heterogeneity estimate to .
Risk of Bias
A sensitivity analysis examined how study risk-of-bias affected estimates of the overall average effect size and extent of heterogeneity, with successively stronger inclusion criteria at each step (Table 2). The first row reports the estimated distribution of effect sizes across all included studies. Subsequent rows report estimates for subsets of studies, illustrating how the overall average effect estimate is altered by stringency of inclusion criteria. Thus, including only the 15 studies (47 effects) at low risk-of-bias for sequence generation and outcome reporting, the overall average effect was notably lower (g = 0.267, 95% CI [0.053, 0.481], These analyses indicated that most risk-of-bias factors were not strongly associated with effect magnitude.
Table 2.
Risk-of-bias analysis using successive inclusion criteria
| Criteria | Studies (Effects) | Average ES [95% CI] |
I2 | |
|---|---|---|---|---|
| All studies | 29 (82) | 0.371 [0.211, 0.521] | 0.317 | 82% |
| Studies with low ROB outcome reporting | 24 (70) | 0.403 [0.217, 0.589] | 0.364 | 85% |
| Studies with low ROB outcome reporting and low ROB sequence generation | 15 (47) | 0.267 [0.053, 0.481] | 0.309 | 85% |
| Studies with low ROB outcome reporting, sequence generation, and allocation concealment | 4 (19) | 0.301 [0.029, 0.573] | 0.000 | 0% |
Note: ROB = risk-of-bias.
To further investigate possible risks of bias due to incomplete outcome reporting, we examined a funnel plot of effect size estimates and conducted modified versions of Egger’s regression test for funnel plot asymmetry. Figure 2 displays a funnel plot of effect size estimates versus scaled standard errors. Although no asymmetry is visually apparent, Egger’s regression test was statistically significant, with an estimated slope for the scaled standard error of , 95% CI [0.227, 2.035], p = .021, indicating possible small-study effects.
Figure 2.
Funnel Plot
Moderator analyses
Table 1 reports estimates of average effect size disaggregated by intervention characteristics and study demographics, along with results of statistical tests for differences between moderator categories. In terms of intervention characteristics, there were no significant differences by intervention format (F(2,2.4) = 0.03, p=0.973) nor between studies that used active, attention, education, or component controls versus those that used wait-list or usual care controls (F(1, 13.2) = 0.002, p=0.965). Interventions delivered in-person had significantly higher effects (g=0.402, 95% CI [0.243, 0.562]) than those delivered through other modalities (g=0.089, 95% CI [−0.596, 0.774]); F(1,3.4)=11.02, p=.038. Importantly, interventions that specifically targeted a meaning/purpose outcome generated significantly higher effect sizes (g=0.419, 95% CI [0.242, 0.596]) than did interventions that did not (g=0.177, 95% CI [0.089, 0.265]; (F(1,17.8) = 8.63, p=0.009). Studies in which meaning/purpose was a primary outcome yielded higher average effect size estimates (g=0.523, 95% CI [0.248, 0.798]) than those in which it was secondary (g=0.192, 95% CI [0.006, 0.379]) or unspecified (g=0.255, 95% CI [−0.036, 0.545]); however, these differences were not statistically significant at conventional levels (F(2,15.6)= 2.60, p=0.106).
The most common outcome scales used to assess meaning/purpose were the meaning subscale of FACIT-Sp (used in 7 studies, 9 effect sizes), the meaning/peace subscale of FACIT-Sp (9 studies, 15 effect sizes), and the existential well-being subscale of the McGill Quality of Life Questionnaire (6 studies, 22 effect sizes). Average effect sizes were not statistically distinguishable across these three categories (F[2, 9.5]=1.28, p=.323).
Regarding demographic factors, effect size magnitude was not significantly associated with the sample’s average age (, 95% CI [−0.016, 0.033], p=.465) or proportion of women (, 95% CI [−0.007, 0.007], p=.906), or with number of weeks of post-intervention follow-up assessment (, 95% CI [−0.006, 0.006], p=.997). Clinical variables also failed to moderate intervention effects. Effects did not differ for studies of breast cancer patients versus all other types of cancer (F(1,20.4) = 0.01, p=.924) or for studies with patients at different phases of treatment (curative, post-treatment, or palliative; F(3,8.9) = 1.50, p=.281).
Exploratory analyses
We were puzzled to observe no differences in average effect size between studies that used active, attention, education, or component controls (g=0.376, 95% CI [0.037, 0.714], ) versus those that used usual care or wait-list controls (g=0.368, 95% CI [0.190, 0.546], ). To probe further, we conducted exploratory meta-regression analysis that controlled for outcome group (primary, secondary, or un-specified), intervention modality, and whether intervention targetted meaning/purpose, in addition to control group type; the model allowed the between-study heterogeneity to differ by outcome group. The first three covariates were chosen based on their statistical significance in the univariate moderator analyses. Controlling for these factors, studies that used usual care or wait-list control groups had larger average effect sizes than studies that used other types of control groups (, 95% CI [−0.022, 0.434]), although the difference is not statistically distinguishable from zero (p=.070). Estimated differences by type of control group were similar when controlling for outcome group alone, outcome group and intervention target, or outcome group and intervention modality. The supplementary materials include full numerical results from these exploratory analyses.
Discussion
Professional standards and practice guidelines require attention to psychosocial concerns as a core dimension of patient-centered care84, 85, 86, 87. Meaning and purpose are a salient aspect of well-being— patients identify these issues as important to them (15, 16, 17) and investigators have increasingly recognized their significance88, 88, 90. Struggles to maintain meaning or purpose are thus important concerns in their own right, as many writers have emphasized (e.g.,38, 88, 90, 91, 92). Difficulties with meaning or purpose may also have notable implications for other patient-reported and objective health outcomes among cancer patients4, 5, 6, 7, 8, 10, 93.
Given that meaning and purpose are highly valued patient-centered outcomes for cancer patients and survivors, relatively few studies have tested psychosocial interventions to promote these outcomes. We located only 29 relevant RCTs, and of these, only 83% explicitly targeted meaning/purpose. In comparison, a recent meta-analysis of interventions targeting cancer-related fatigue identified 113 eligible studies94. The variety of interventons included in our current analyses ranged from meaning-focused approaches to coping skills-based strategies, meditation, yoga, creative arts, and health education; not surprisingly, these varied interventions demonstrated a high degree of heterogeneity in their effects on meaning.
In spite of this heterogeneity, we found a moderate effect size (g=0.371) of interventions on meaning across the pool of included studies. This result indicates that, relative to control conditions, psychosocial interventions that assessed meaning demonstrated significant improvements in meaning. This overall benefit compares quite favorably with recent meta-analyses examining the efficacy of psychosocial intervention trials to treat depression (g=0.4395), pain (g=0.34 to 0.4096), and fatigue (g=0.27 to 0.3094) among cancer patients. When we focused only on studies with low risk of bias in subsequent analyses, the overall effect was notably lower, but still in the small-to-moderate effect size range.
Our results suggest that psychosocial interventions can increase a sense of meaning and purpose in cancer patient and survivors, especially if they are explicitly designed to do so and focus on enhancing patients’ sense of meaning and purpose26, 93. These interventions are generating growing interest18, 19, 20, 21, 23, 24, 25, and thus, we anticipate that development and testing of meaning-related interventions will increase fairly rapidly. Given that meaning and purpose have been conceptualized in different ways and encompass multiple distinct dimensions4, it will be important for future studies to consider carefully and delineate more clearly what aspects of meaning the intervention is intended to target, and to differentiate these endpoints from related concepts (such as spirituality or general well-being).
More research is needed to determine which meaning-focused interventions are most appropriate for whom. Different types of meaning-focused therapies (e.g., meaning-focused group psychotherapy, cognitive-existential therapy, supportive-expressive therapy, mindfulness-based stress reduction) may be differentially effective. Combination therapies that use mind-body techniques along with a specific focus on meaning might usefully create synergies across these modalities24, 91, 92. Moreover, different meaning-based approaches may be more beneficial for some individuals than for others. For example, patients in active treatment may have different existential concerns than those transitioning to longer-term survivorship or palliative care. We did not find strong evidence for clinical or demographic moderators, but clearly further research is needed to explore differential effects for distinct patient subgroups (e.g., phase of treatment, cancer stage, racial/cultural background). Additionally, in future investigations, it might be useful to select patients with low levels of meaning at enrollment, which may increase the effectiveness of these interventions. None of the studies included in this review screened patients in this manner. Of course, it is possible that even individuals presenting with moderate or high levels of meaning may derive benefits in other areas of functioning (e.g., positive affect, growth, treatment adherence, social functioning), and these questions merit further attention.
Studies utilizing more rigorous methods are also needed. Our review included a high proportion of studies at risk of bias due to attrition (7 studies) and uncertain risk of bias regarding sequence generation (12 studies) and allocation concealment (20 studies). Some investigations included clinically heterogeneous samples, which may obscure differential effects, or did not report basic clinical characteristics, which make findings hard to interpret (e.g., 14 studies included patients with highly diverse disease stage or did not report stage).
Conceptually, this area of intervention research would be enriched by more thoughtful consideration regarding which measures of meaning to employ. The majority of studies in our review (55%) used the meaning or meaning/peace subscale of the FACIT-Spirituality scale35. Many other well-validated measures of meaning in life or illness-specific meaning are available and may be more useful in differentiating important components of these constructs (e.g., comprehensibility, purpose, identity) as well as disambiguating meaning/purpose from related constructs such as spirituality. A more sophisticated understanding of these distinct dimensions of meaning/purpose, and appropriate selection of measures that are matched to intervention aims, is an important priority as this area of research begins to mature. Finally, interventions designed to improve meaning/purpose might be expected in turn to have saluatary effects on other clinically relevant endpints, such as treatment adherence, decision making, clincal trials participation, hospice utilization, and so on; these outcomes have yet to be evaluated.
Promoting a stronger sense of meaning is an important endeavor warranting clinical investment; meaning is associated favorably with mental and physical well-being and is also highly valued in its own right. Our analysis suggests that such investment can pay off for patients and survivors, providing them with a greater sense of meaning and purpose. Additional work is needed to evaluate these interventions using more rigorous methodology and more refined outcome measures.
Supplementary Material
Funding:
Supported by National Cancer Institute Grant R03 CA184560 (PI: Salsman).
Footnotes
Conflict of Interest: No author has a conflict of interest to declare.
References
- 1. Posluszny DM, Dew AM, Beckjord E, et al. : Existential challenges experienced by lymphoma survivors: results from the 2010 LIVESTRONG survey. J Health Psychol 21:2357–2366, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee V, Loiselle CG: The salience of existential concerns across the cancer control continuum. Palliat Support Care10:123–133, 2012 [DOI] [PubMed] [Google Scholar]
- 3. Henoch I, Strang S, Browall M, et al. : Development of an existential support training program for healthcare professionals. Palliat Support Care 13:1701–1709, 2015 [DOI] [PubMed] [Google Scholar]
- 4. George LS, Park CL: Meaning in life as comprehension, purpose, and mattering: Toward integration and new research questions. Rev Gen Psychol 20: 205–220, 2016 [Google Scholar]
- 5. Mehnert A, Koch U: Psychometric evaluation of the German version of the Life Attitude Profile-Revised (LAP-R) in prostate cancer patients. Palliat Support Care 6:119–124, 2008 [DOI] [PubMed] [Google Scholar]
- 6. Park CL, Edmondson D, Fenster JR, et al. : Meaning making and psychological adjustment following cancer: the mediating roles of growth, life meaning, and restored just-world beliefs. J Consult Clin Psychol 76:863–875, 2008 [DOI] [PubMed] [Google Scholar]
- 7. Sherman AC, Simonton S, Latif U, et al. : Effects of global meaning and illness-specific meaning on health outcomes among breast cancer patients. J Behav Med 33;364–377, 2010 [DOI] [PubMed] [Google Scholar]
- 8. Sherman AC, Simonton S: Effects of personal meaning among patients in primary and specialized care: associations with psychosocial and physical outcomes. Psychol Health 27:475–490, 2012 [DOI] [PubMed] [Google Scholar]
- 9. Vehling S, Lehmann C, Oechsle K, et al. : Global meaning and meaning-related life attitudes: exploring their role in predicting depression, anxiety, and demoralization in cancer patients. Support Care Cancer 19:513–520, 2010 [DOI] [PubMed] [Google Scholar]
- 10. Vickberg SMJ, Bovbjerg DH, DuHamel KN, et al. : Intrusive thoughts and psychological distress among breast cancer survivors: global meaning as a possible protective factor. Behav Med 25:152–160, 2000 [DOI] [PubMed] [Google Scholar]
- 11. Vickberg SMJ, Duhamel KN, Smith MY, et al. : Global meaning and psychological adjustment among survivors of bone marrow transplant. Psycho-Oncol 10:29–39, 2001 [DOI] [PubMed] [Google Scholar]
- 12. Jim HS, Andersen BL: Meaning in life mediates the relationship between social and physical functioning and distress in cancer survivors. Brit J Health Psychol 12:363–381, 2007 [DOI] [PubMed] [Google Scholar]
- 13. Simonelli LE, Fowler JG. Maxwell L, et al. : Physical sequelae and depressive symptoms in gynecologic cancer survivors: meaning in life as a mediator. Ann Behav Med 35:275–284, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tomich PL, Helgeson V: Five years later: a cross-sectional comparison of breast cancer survivors with healthy women. Psycho-Oncol 11:154–169, 2002 [DOI] [PubMed] [Google Scholar]
- 15. Moadel A, Morgan C, Fatone A, et al. : Seeking meaning and hope: self-reported spiritual and existential needs among an ethnically diverse cancer patient population. Psychooncol 8:378–385, 1999 [DOI] [PubMed] [Google Scholar]
- 16. Strang S, Strang P. Questions posed to hospital chaplains by palliative care patients. J Palliat Med. 5:857–864, 2002 [DOI] [PubMed] [Google Scholar]
- 17. Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliat Med 18:39–45, 2004 [DOI] [PubMed] [Google Scholar]
- 18.**. Breitbart W, Poppito S, Rosenfeld B, et al. : Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol 30:1304–1309, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Breitbart W, Rosenfeld B, Pessin H, et al. : Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol 33:749–754, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chochinov HM, Kristjanson LJ, Breitbart W, et al. : Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol 12:753–762, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.**. Gagnon P, Fillion L, Robitaille MA, et al. : A cognitive-existential intervention to improve existential and global quality of life in cancer patients: a pilot study. Palliat Support Care 13:981–990, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee V, Cohen RS, Edgar L, et al. : Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Soc Sci Med 62:3133–3145, 2006 [DOI] [PubMed] [Google Scholar]
- 23. Steinhauser KE, Alexander SC, Byock IR, et al. : Do preparation and life completion discussions improve functioning and quality of life in seriously ill patients? Pilot randomized controlled trial. J Palliat Med 11:1234–1240, 2008 [DOI] [PubMed] [Google Scholar]
- 24.**. van der Spek N, Vos J, van Uden-Kraan CF, et al. : Efficacy of meaning-centered group psychotherapy for cancer survivors: a randomized controlled trial. Psychol Med 247:1990–2001, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang CW, Chow AY, Chan CL: The effects of life review interventions on spiritual well-being, psychological distress, and quality of life in patients with terminal or advanced cancer: A systematic review and meta-analysis of randomized controlled trials. Palliat Med 31:883–894, 2017 [DOI] [PubMed] [Google Scholar]
- 26. Bauereiß N, Obermaier S, Özünal, SE, Baumeister H: Effects of existential interventions on spiritual, psychological, and physical well-being in adult patients with cancer: Systematic review and meta-analysis of randomized controlled trials. Psycho-Oncology, 27(11), 2531–2545, 2018 [DOI] [PubMed] [Google Scholar]
- 27. Haynes RB, McKibbon KA, Wilczynski NL, et al. : Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. BMJ 330(7501), 1179, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Montori VM, Wilczynski NL, Morgan D, et al. : Optimal search strategies for retrieving systematic reviews from Medline: analytical survey. BMJ 330(7482), 68, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Park CL: Making sense of the meaning literature: an integrated review of meaning making and its effects on adjustment to stressful life events. Psychological Bull 136:257–301, 2010 [DOI] [PubMed] [Google Scholar]
- 30. George LS, Park CL: Meaning in life as comprehension, purpose, and mattering: toward integration and new research questions. Rev Gen Psychol 20:205–220, 2016 [Google Scholar]
- 31. Reker GT, Wong PTP: Aging is an individual process: toward a theory of personal meaning, in Birren JE, Bengtson VL, (eds.), Emerging Theories of Aging (pp. 214–246). New York: Springer, 1988, pp 214–246 [Google Scholar]
- 32. Park CL, Folkman S. Meaning in the context of stress and coping. Rev Gen Psychol 2:115–144, 1997 [Google Scholar]
- 33. Steger MF, Frazier P, Oishi S, et al. : The Meaning in Life Questionnaire: assessing the presence of and search for meaning in life. J Consult Psychol 2006; 53:80–93, 2006 [Google Scholar]
- 34. Thompson SC, Janigian AS: Life schemes: a framework for understanding the search for meaning. J Soc Clin Psychol 7:260–280, 1988 [Google Scholar]
- 35. Peterman AH, Fitchett G, Brady MJ, et al. : Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 24:49–58, 2002 [DOI] [PubMed] [Google Scholar]
- 36. Tedeschi RG, Calhoun LG: The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Traum Str, 9:455–471, 1996 [DOI] [PubMed] [Google Scholar]
- 37. Carver CS, Antoni MH: Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychology 23:595–598, 2004 [DOI] [PubMed] [Google Scholar]
- 38. Cohen SR, Mount BM, Strobel MG, et al. : The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. Palliative Medicine 9:207–219, 1995 [DOI] [PubMed] [Google Scholar]
- 39. Antonovsky A: The structure and properties of the sense of coherence scale. Social Science & Medicine 36:725–733, 1993 [DOI] [PubMed] [Google Scholar]
- 40. Pang S, Chan KS, Chung M, et al. : Assessing the quality of life of persons with advanced COPD in the end of life. J Palliat Care 21:180–187, 2005 [PubMed] [Google Scholar]
- 41. Bufford R, Paloutzian R, Ellison C: Spiritual Well-Being Scale. J Psychology and Theology 19:56–70, 1991 [Google Scholar]
- 42. Haugan G, Rannestad T, Garåsen H, et al. : The self-transcendence scale: an investigation of the factor structure among nursing home patients. J Holistic Nursing 30:147–159, 2012 [DOI] [PubMed] [Google Scholar]
- 43. Reker GT. Manual of the Life Attitude Profile–Revised (LAP-R): Peterborough, Canada: Student Psychologists Press; 1992 [Google Scholar]
- 44. Jaarsma TA, Pool G, Ranchor AV, Sanderman R: The concept and measurement of meaning in life in Dutch cancer patients. Psycho-Oncology 16, 241–248, 2007 [DOI] [PubMed] [Google Scholar]
- 45. van Dierendonck D: The construct validity of Ryff’s scales of psychological well-being and its extension with spiritual well-being. Personality and Individual Differences 36, 629–643, 2004 [Google Scholar]
- 46. Moyer A, Sohl SJ, Knapp-Oliver SK, Schneider S: Characteristics and methodological quality of 25 years of research investigating psychosocial interventions for cancer patients. Cancer treatment reviews, 35(5), 475–484, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hedges L: Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational and Behavioral Statistics 6:107–128, 1981 [Google Scholar]
- 48.**. Cook EL, Silverman MJ: Effects of music therapy on spirituality with patients on a medical oncology/hematology unit: a mixed-methods approach. The Arts in Psychotherapy, 40(2), 239–244, 2013 [Google Scholar]
- 49.**. Fauver R: The healing wisdom within: A preliminary experimental trial of Psycho-Spiritual Integrative Therapy for people with cancer. Institute of Transpersonal Psychology, 2012 [Google Scholar]
- 50. Tukey JW: Exploratory Data Analysis. Addison-Wesley Publishing Company, 1977 [Google Scholar]
- 51.**. Xiao H, Kwong E, Pang S, et al. : Effect of a life review program for Chinese patients with advanced cancer: a randomized controlled trial. Cancer Nurs 36:274–83, 2013 [DOI] [PubMed] [Google Scholar]
- 52. Lipsey MW, Wilson DB: Practical Meta-Analysis. Thousand Oaks, CA, Sage Publications, 2001 [Google Scholar]
- 53. Hedges LV, Tipton E, Johnson MC: Robust variance estimation in meta-regression with dependent effect size estimates. Research Synthesis Methods, 1:39–65, 2010 [DOI] [PubMed] [Google Scholar]
- 54. Tipton E: Small sample adjustments for robust variance estimation with meta-regression. Psychological Methods 20:375–393, 2015 [DOI] [PubMed] [Google Scholar]
- 55. Tipton E, Pustejovsky JE: Small-sample adjustments for tests of moderators and model fit using robust variance estimation in meta-regression. J Educ and Behav Statistics 40:604–634, 2015 [Google Scholar]
- 56. Borenstein M, Higgins JPT, Hedges LV, et al. : Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods 8:5–18, 2017 [DOI] [PubMed] [Google Scholar]
- 57. Pustejovsky JE, Rodgers M: (2018). Testing for funnel plot asymmetry of standardized mean differences. Research Synthesis Methods. 10.1002/jrsm.1332 [DOI] [PubMed] [Google Scholar]
- 58. Viechtbauer W: Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36:1–48, 2010 [Google Scholar]
- 59. Pustejovsky JE: clubSandwich: Cluster-robust (sandwich) variance estimators with small-sample corrections, 2017. https://cran.r-project.org/package=clubSandwich
- 60. Shamseer L, Moher D, Clarke M, et al. : PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Brit Med J 350:g7647, 2015 [DOI] [PubMed] [Google Scholar]
- 61.**. Ando M, Morita T, Akechi T, et al. : Efficacy of short-term life-review interviews on the spiritual well-being of terminally ill cancer patients. J Pain and Symptom Management 39:993–1002, 2010 [DOI] [PubMed] [Google Scholar]
- 62.**. Bower JE, Crosswell AD, Stanton AL, et al. : Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer, 121(8), 1231–1240, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.**. Breitbart W, Rosenfeld B, Gibson C, et al. : Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-Oncology, 19(1), 21–28, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.**. Breitbart W, Pessin H, Rosenfeld B, et al. : Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: A randomized controlled trial in patients with advanced cancer. Cancer, 124(15), 3231–3239, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.**. Carlson LE, Tamagawa R, p J, et al. : Randomized-controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long-term follow-up results. Psycho-Oncology, 25(7), 750–759, 2016 [DOI] [PubMed] [Google Scholar]
- 66.**. Cole B, Broer K, Hopkins C, et al. : A Randomized controlled trial of spiritually-focused meditation in patients newly diagnosed with acute leukemia, Blood, 116:1519, 2010 [Google Scholar]
- 67.**. Cole BS, Hopkins CM, Spiegel J, et al. :A randomised clinical trial of the effects of spiritually focused meditation for people with metastatic melanoma. Mental Health, Religion & Culture, 15(2), 161–174, 2012 [Google Scholar]
- 68.**. Danhauer SC, Mihalko SL, Russell GB, et al. : Restorative yoga for women with breast cancer: findings from a randomized pilot study. Psycho-Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 18(4), 360–368, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.**. Djuric Z, Mirasolo J, Kimbrough L, Brown DR, Heilbrun LK, Canar L, … & Simon MS: A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. Journal of the National Medical Association, 101(6), 552, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.**. Duggleby WD, Degner L, Williams A, et al. : Living with hope: initial evaluation of a psychosocial hope intervention for older palliative home care patients. Journal of Pain and Symptom Management, 33(3), 247–257, 2007 [DOI] [PubMed] [Google Scholar]
- 71.**. Guthrey CR: An empirical study of the effect of Psycho-Spiritual Integrative Therapy on the spirituality of cancer patients (Doctoral dissertation, Institute of Transpersonal Psychology), 2016
- 72.**. Hawkes AL, Pakenham KI, Chambers SK, et al. : Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: a randomized controlled trial. Annals of Behavioral Medicine, 48(3), 359–370, 2014 [DOI] [PubMed] [Google Scholar]
- 73.**. Henderson VP, Clemow L, Massion AO, et al. : The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Research and Treatment, 131(1), 99–109, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.**. Henry M, Cohen SR, Lee V, et al. : The Meaning-Making intervention (MMi) appears to increase meaning in life in advanced ovarian cancer: A randomized controlled pilot study. Psycho-oncology, 19(12), 1340–1347, 2010 [DOI] [PubMed] [Google Scholar]
- 75.**. Hsiao FH, Jow GM, Kuo WH, et al. : The effects of psychotherapy on psychological well-being and diurnal cortisol patterns in breast cancer survivors. Psychotherapy and Psychosomatics, 81(3), 173–182, 2012 [DOI] [PubMed] [Google Scholar]
- 76.**. Jafari N, Farajzadegan Z, Zamani A, et al. : Spiritual therapy to improve the spiritual well-being of Iranian women with breast cancer: a randomized controlled trial. Evidence-Based Complementary and Alternative Medicine, 9 pages, ID 353262, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.**. Mok E, Lau KP, Lai T, Ching S: The meaning of life intervention for patients with advanced-stage cancer: development and pilot study. Oncology nursing forum, 39(6), 2012. [DOI] [PubMed] [Google Scholar]
- 78.**. Nidich SI, Fields JZ, Rainforth MV, et al. : A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integrative Cancer Therapies, 8(3), 228–234, 2009 [DOI] [PubMed] [Google Scholar]
- 79.**. Ownsworth T, Chambers S, Damborg E, et al. : Evaluation of the making sense of brain tumor program: a randomized controlled trial of a home-based psychosocial intervention. Psycho-Oncology, 24(5), 540–547, 2015 [DOI] [PubMed] [Google Scholar]
- 80.**. Pelekasis P, Zisi G, Koumarianou A, et al. : Forming a stress management and health promotion program for women undergoing chemotherapy for breast cancer: a pilot randomized controlled trial. Integrative Cancer Therapies, 15(2), 165–174, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.**. Piderman KM, Johnson ME, Frost MH, et al. : Spiritual quality of life in advanced cancer patients receiving radiation therapy. Psycho-Oncology, 23(2), 216–221, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.**. Wise M, Marchand LR, Roberts LJ, Chih MY: Suffering in Advanced Cancer: A randomized control trial of a narrative intervention. Journal of Palliative Medicine, 21(2), 200–207, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.**. Ye ZJ, Liang MZ, Qiu HZ, et al. : Effect of a multidiscipline mentor-based program, Be Resilient to Breast Cancer (BRBC), on female breast cancer survivors in mainland China—A randomized, controlled, theoretically-derived intervention trial. Breast Cancer Research and Treatment, 158(3), 509–522, 2016 [DOI] [PubMed] [Google Scholar]
- 84. American College of Surgeons. Cancer program standards 2012: Ensuring patient-centered care; Chicago, Illinois, 2012. http://www.facs.org/cancer/coc/cocprogramstandards2012.pdf [Google Scholar]
- 85. Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs, Washington, DC, National Academy Press, 2008 [PubMed] [Google Scholar]
- 86. National Comprehensive Care Network, Distress Management. NCCN Clinical Practice Guidelines in Oncology National Comprehensive Cancer Network; 2008. https://www.nccn.org/professoinals/physician_gls/pdf/distress.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Neuss MN, Polovich M, McNiff K, et al. : updated American Society of Clinical Oncology/Oncology Nursing Society chemotherapy administration safety standards including standards for the safe administration and management of oral chemotherapy. J Oncol Practice 9(2 Suppl): 5s–13s, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lethborg C, Aranda S, Kissane D: Meaning in adjustment to cancer: a model of care. Palliat Support Care 6:61–70, 2008 [DOI] [PubMed] [Google Scholar]
- 89. Vehling S, Philipp R. Existential distress and meaning-focused interventions in cancer survivorship. Curr Opin Support Palliat Care 12:46–51, 2018 [DOI] [PubMed] [Google Scholar]
- 90. Winger JG, Adams RN, Mosher CE. Relations of meaning in life and sense of coherence to distress in cancer patients: a meta-analysis. Psychooncol 25:2–10, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Simonton S, Sherman AC: An integrative model of group therapy for cancer patients. Intl J Group Psychother 50:487–506, 2000 [DOI] [PubMed] [Google Scholar]
- 92. Spira JL, ed. Group Therapy for Medically Ill Patients. New York: Guilford Press; 1997 [Google Scholar]
- 93. Rosenfeld B, Cham H, Pessin H, et al. : Why is Meaning Centered Group Psychotherapy (MCGP) effective? Enhanced sense of meaning as the mechanism of change for advanced cancer patients. Psycho-Oncol, 27(2), 654–660, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Mustian KM, Alfano CM, Heckler C, et al. : Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol. 3(7):961–968, 2017. doi: 10.1001/jamaoncol.2016.6914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Hart SL, Hoyt MA, Diefenbach M, et al. : Meta-analysis of efficacy of interventions for elevated depressive symptoms in adults diagnosed with cancer. J Natl Cancer Inst 104:990–1004, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Sheinfeld Gorin S, Krebs P, Badr H, et al. : Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol 30:539–547, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.