ABSTRACT
Background
Many updates to young child feeding recommendations have been published over the past decade, but concurrent intake trends have not been assessed.
Objective
The aim of this study was to evaluate adequacy and trends in energy and nutrient intakes of US infants and children aged 0–47.9 mo through use of Feeding Infants and Toddlers Study (FITS) data from 2002, 2008, and 2016.
Methods
FITS are cross-sectional surveys of parents/caregivers of infants and young children (FITS 2002, n = 2962; FITS 2008, n = 3276; FITS 2016, n = 3235). Dietary intakes were assessed by telephone with trained interviewers using the Nutrition Data System for Research. Mean ± SE nutrient intakes were calculated. Diet adequacy was assessed with the nutrient adequacy ratio (NAR) for 17 nutrients and the corresponding mean adequacy ratio.
Results
Energy and macronutrient intakes were generally stable across surveys, but significant decreases for saturated fat and total sugars and an increase in fiber were observed among 6–11.9-mo-olds and 12–23.9-mo-olds (P-trend < 0.0001). Mean sodium intakes exceeded Adequate Intakes (AI) for all ages, whereas fiber intakes were universally below the AI. Nutrients with the lowest NAR values were vitamin D (range 0.41–0.67/1.00) and vitamin E (range 0.60–0.79/1.00 for 2008 and 2016). For iron, infants aged 6–11.9 mo had the lowest NAR values at 0.77–0.88/1.00, compared to 0.85–0.89/1.00 for 12–47.9-mo-olds. Potassium was low from 12 to 47.9 mo (NAR range 0.55–0.63/1.00 across survey years). The nutrients with the greatest decline in mean intakes were iron and vitamins D and E among 6–11.9-mo-olds, and vitamin D and potassium among 12–23.9-mo-olds in 2016 compared to 2002.
Conclusions
The diets of US infants and young children were generally adequate for most micronutrients and stable over time, but sodium intakes were too high, and nutrient gaps still existed, especially for vitamins D, E, and fiber across ages and for iron among infants.
Keywords: nutrient intake, Feeding Infants and Toddlers Study, infants, young children, nutrient adequacy ratio, pediatric nutrition
Introduction
The transition from breast milk and/or infant formula to a more diverse diet is needed to meet infants’ changing nutritional and developmental requirements (1, 2). This period is important for developing food preferences and eating behaviors that may have lasting impacts on dietary patterns and later body weight status (3–5). Early exposure to a variety of foods, flavors, and textures leads to greater acceptance of foods comprising a diverse diet (4, 6, 7). Current feeding guidelines focus on what is consumed, when different foods are introduced, and how to feed infants and toddlers to help them develop food preferences and eating patterns that are consistent with long-term health (2, 8, 9). In the United States, work is currently under way in the Birth to 24 mo (B-24) Project to gather and evaluate the evidence base for feeding practices and their associations with growth and development of infants and young children (9, 10). The project is being used in the preparation of the 2020–2025 Dietary Guidelines for Americans that will include specific B-24 recommendations for the first time (9).
Over the last decade, there have been several important updates to feeding recommendations for young children, and more will likely emerge with the 2020–2025 Dietary Guidelines. The American Academy of Pediatrics has issued 2 editions to its Pediatric Nutrition Handbook, encouraging offering new foods multiple times (about 10 exposures) to promote acceptance of new foods in 2009, and in 2014, focusing on diet quality and variety, and encouraging responsive feeding (1, 11). The Food and Nutrition Board of the National Academy of Sciences released new dietary reference values for calcium and vitamin D in 2011 (12), and the Academy of Nutrition and Dietetics published Nutritional Guidance for Healthy Children Ages 2 to 11 Years in 2014 (13), identifying high intakes of sugar and sodium as problems for children of these ages. Implementation of these guidelines into nutrition recommendations may have contributed to changes in nutrient intakes for infants and young children.
Monitoring the dietary intakes of infants and young children is necessary to determine whether they are meeting recommendations (12), and to identify changes in nutrient intakes over time. In the United States, the 2 largest population-based national surveys evaluating nutrient intakes in infants and young children are the NHANES (14–20) and the Feeding Infants and Toddlers Study (FITS) (21–26). Until now, only 2 studies from these surveys have examined trends in nutrient intakes over time. The NHANES compared intakes of 2–19-y-olds from 1999–2000 through 2009–2010, but data were not available among infants and toddlers aged <24 mo (14). The FITS trend data focused only on the prevalence of inadequate and excessive nutrient intakes among 6–11-mo-olds and 12–23-mo-olds from 2002 and 2008 (24). Therefore, the objective in this study was to evaluate trends in nutrient intakes, prevalence of adequacy/excess, and nutrient density over time through use of FITS data from 2002, 2008, and 2016. We also investigated whether intakes of key dietary components (energy, protein, total fat, saturated fat, total carbohydrate, total and added sugars, fiber, and micronutrients including sodium) have changed in infants and toddlers. Finally, we explored which food groups were most associated with dietary adequacy in infants and young children by comparing the impact of tertiles of nutrient adequacy, estimated from the mean adequacy ratio, on consumption of key food groups.
Methods
FITS survey methods
The FITS are cross-sectional surveys of national samples of infants and young children in the United States (27–29). The 2002 sample included infants and toddlers aged 4–24 mo. In 2008 and 2016, the sample was extended from birth up to age 48 mo. In all cases, national sampling plans were designed to reflect the geographic and sociodemographic diversity of households with young children (1–4 y) across the 50 states in the United States.
The samples in 2002 and 2008 were drawn from targeted lists of prenatal and postnatal records from the New Parent Database from Experian Information Solutions, Inc, and were weighted to be representative to the US population. In 2016, samples were drawn from a combination of the New Parent Database, address-based and cellphone sampling frames, and a web panel. To minimize potential bias for nonresponse, sampling weights were calibrated to the 2014 US population distributions for age, sex, race/ethnicity, and educational attainment. Further details of the sampling and methodology are available in methods publications from each FITS (27–29).
A total of 9473 infants and young children were included in these analyses, 3235 from FITS 2016, 3276 from FITS 2008, and 2962 from FITS 2002 (Supplemental Table 1). Because of the timing of recruitment questionnaires and the subsequent 24-h recalls, 59 children from 2002 were older than 24 mo by the time they had their dietary interview. We excluded them from our analysis because there were too few children in this age group to draw any conclusions.
Structured telephone interviews were conducted with the mother or primary caregiver of the selected child (1 child per household). Age-specific recruitment and feeding practices questionnaires were developed to assess household demographics, characteristics of the child, feeding practices, and eating behaviors, with separate questionnaires for infants and young children aged <24 mo and for children aged ≥24 mo. After completion of the recruitment and feeding practices questionnaires, a 24-h recall was conducted. A second 24-h recall was collected at least 1 wk later (mean = 12 d; 95% within 30 d) on a random subset of respondents to estimate usual nutrient intakes, 23% in 2002 (27), 21% in 2008 (28), and 25% in 2016 (29), but only mean intakes and standard errors are presented in this paper.
Dietary intakes
In all FITS, multiple-pass 24-h recalls were collected by telephone with trained interviewers using the Nutrition Data System for Research. For each study, a review of baby food products available on the market at the time was conducted, and these were added to the Nutrition Data System for Research database to facilitate the interviews. For example, 358 baby-specific foods were added for FITS 2008 (28), and 351 were added for FITS 2016 (29). Before the interviews, a package of food measurement aids was sent to the household, including a measuring cup and tape, a list of commonly forgotten foods, and a booklet showing common sippy cups, spoons, bowls, wedges, and grids to assist the parent or caregiver in estimating portion sizes for their child (30).
Breast milk volumes were estimated consistently across the surveys with procedures developed for FITS (22), based on age-specific volumes derived from Dewey et al. (31, 32), and Kent et al. (33). This strategy has been further supported by systematic review and modeling (34), and adopted by the Centers for Disease Control and Prevention for the NHANES (15). For breastfeeding infants from birth to 5.9 mo, we assumed 780 mL/day, and for those 6–11.9 mo, 600 mL/d was used. If other milks were fed in addition to breast milk, these amounts were subtracted from the daily totals. A volume of 89 mL or 59 mL per feeding was assigned for 12–17.9-mo-olds or 18–41.9-mo-olds, respectively (28).
Statistical methods and analyses
Statistical analyses were performed with SAS (version 9, SAS Institute Inc.) and SAS-callable SUDAAN (version 11, RTI International) software. Age-specific means and SE for intakes of 17 nutrients were compared between survey years through use of linear regression. Nutrient intakes were re-estimated for all previous FITS survey years. The food composition table appropriate for each year of the survey was used because values for the nutritional content of foods may have changed over time. Dietary supplements were excluded from these analyses.
Diet adequacy was assessed with the nutrient adequacy ratio (NAR) and the corresponding mean adequacy ratio (MAR). NAR is obtained by expressing the individual's intake of a nutrient as a percentage (capped at 100%) of the corresponding RDA for that nutrient for the individual's age and sex (35). NAR values were based on mean nutrient intakes from each subject's first recall day. For many nutrients among infants, only an Adequate Intake (AI) was available, and these were used instead of the RDA. The mean of these values provides some indication of the extent to which the intakes of the group under study met the standard. If everyone in the group met the standard then the NAR for the group would be 1.00, and if none did so, it would be 0. In general, the higher the NAR, the more likely it is that many of those in the group had intakes at or close to the RDA/AI. Similarly, the MAR is a summary measure that expresses the mean of all the NARs for different nutrients measured to provide insight into the adequacy of the diet as a whole. For the MAR in this study, a NAR was calculated for 17 vitamins and minerals from food and beverage sources only; not including nutrients from dietary supplements if they were consumed by the infant. All NARs were truncated at 1.00, and then the MAR was calculated by summing the NARs and dividing by 17. Statistical analyses were conducted with use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age.
To evaluate the food groups consumed, we first classified the MAR values into tertiles by age. We then calculated the intakes (g/d) for the following food group categories: milk and milk products, fruit, meats, and protein foods, grains and grain products, mixed dishes, sweets/sweetened beverages/desserts, and vegetables. Data for the food groups are presented in radar plots by MAR tertile to visualize the impact of consumption of different food groups on diet adequacy.
Results
Reported energy and macronutrient intakes were generally stable across the FITS survey years (Table 1). Energy intakes increased with increasing age, but within age groups, there were no significant differences in energy intakes across the survey years. The sole exception was for toddlers aged 12–23.9 mo in 2002 whose intakes were slightly higher in energy compared to the later survey years (overall P-trend = 0.0002). Carbohydrate intakes were also slightly higher among the 12–23.9-mo-olds in 2002 compared to later survey years (overall P-trend = 0.0006). As with energy and macronutrients, intake in grams of saturated fat, total sugars, added sugars, and sodium increased with age. Significant decreases across survey years (overall P-trend < 0.0001) were observed for saturated fat and for total sugars among 6–11.9-mo-olds and 12–23.9-mo-olds (Table 1). Mean sodium intakes exceeded AI for all age categories (AI = 370 mg/d for 6–12 mo, and 1000 mg/d for 1–3 y). Dietary fiber significantly increased among 6–11.9-mo-olds and 12–23.9-mo-olds across the 3 FITS (overall P-trend < 0.0001). Although AIs have not been determined for fiber in children aged <1 y, the mean intakes we observed for those aged ≥12 mo were well below the AI of 19 g/d established for 1–3-y-olds in the United States, with mean intakes from 8.0 to 10.0 g/d among 12–23.9-mo-olds and 10.3–11.9 g/d among 24–47.9-mo-olds across survey years.
TABLE 1.
Energy, saturated fat, total sugars, added sugars, sodium, and fiber intakes for infants and young children from the Feeding Infants and Toddlers Studies 2002, 2008, and 20161
| 6–11.9 mo | 12–23.9 mo | 24–47.9 mo | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2002 | 2008 | 2016 | 2002 | 2008 | 2016 | 2008 | 2016 | ||
| Nutrient | n = 1464 | n = 509 | n = 902 | n = 1031 | n = 924 | n = 1133 | 2002 | n = 1461 | n = 600 |
| Energy (kcal/d) | 857 ± 9 | 836 ± 23 | 855 ± 14 | 1228 ± 16 | 1139 ± 18 | 1172 ± 16 | — | 1306 ± 17 | 1396 ± 24 |
| Protein (g/d) | 20.4 ± 0.3 | 21.8 ± 1.3 | 21.5 ± 0.6 | 46.2 ± 0.7 | 42.4 ± 0.8 | 46.1 ± 0.7 | — | 49.3 ± 0.9 | 52.0 ± 1.0 |
| Total fat (g/d) | 34.7 ± 0.3 | 35.1 ± 1.1 | 37.5 ± 0.6 | 45.1 ± 0.7 | 41.6 ± 0.8 | 44.0 ± 0.7 | — | 44.8 ± 0.9 | 50.2 ± 1.2 |
| Saturated fat (g/d) | 15.8 ± 0.2a | 14.3 ± 0.4b | 14.8 ± 0.3b | 20.0 ± 0.3a | 16.9 ± 0.4b | 17.6 ± 0.3b | — | 17.0 ± 0.4 | 18.0 ± 0.5 |
| Carbohydrate (g/d) | 117.8 ± 1.3 | 111.0 ± 3.0 | 111.7 ± 2.1 | 164.3 ± 2.4 | 153.0 ± 2.8 | 152.6 ± 2.3 | — | 181.8 ± 2.4 | 190.3 ± 3.5 |
| Total sugars (g/d) | 78.2 ± 0.8a | 72.0 ± 1.7b | 69.6 ± 1.1b | 98.2 ± 1.6a | 85.3 ± 1.8b | 80.7 ± 1.3b | — | 96.2 ± 1.6 | 96.4 ± 2.1 |
| Added sugars (g/d) | — | 25.6 ± 1.6 | 24.2 ± 1.0 | — | 26.7 ± 1.1 | 22.3 ± 0.9 | — | 37.1 ± 1.2 | 37.2 ± 1.3 |
| Sodium (mg/d) | 434 ± 16.2 | 525 ± 50.8 | 469 ± 22.3 | 1580 ± 29.7 | 1481 ± 38.8 | 1439 ± 26.8 | — | 1855 ± 31.5 | 1978 ± 49.2 |
| Dietary fiber (g/d) | 5.3 ± 0.1a | 5.6 ± 0.3a,b | 6.5 ± 0.2b | 8.0 ± 0.2a | 8.7 ± 0.2b | 10.0 ± 0.2c | — | 10.3 ± 0.2 | 11.9 ± 0.3 |
Statistical tests were computed with use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age. Data are presented as means ± SE. Mean intakes with different superscripts (a,b,c) represent an overall difference at P ≤ 0.0001 and a year-to-year difference of P ≤ 0.005 within each age grouping.
Nutrient adequacy was assessed with use of the NAR for individual nutrients and the MAR as a summary measure to assess the adequacy of the entire diet based on those same micronutrients (Tables 2–5). For the most part, NARs for individual nutrients were >0.85. Mean vitamin D intakes were lower than the RDA/AI for many individuals and therefore they had the lowest NAR values across survey years and across all ages (birth–47.9 mo), ranging from 0.41 to 0.67, with lowest values among 24–47.9-mo-olds. Vitamin E was also below the standard for a relatively large number of individuals, with NAR values ranging from 0.60 to 0.79 in the last 2 cycles of FITS, a significant decline from 2002 among infants aged 0–5.9 mo and aged 6–11.9 mo. Another nutrient of concern was potassium, but intakes were low compared to the AI only among toddlers and young children (12–47.9 mo), with NAR values ranging from 0.55 to 0.63. For iron, infants aged 6–11.9 mo had the lowest NAR values compared to other age groups (ranging from 0.77–0.88 for 6–11.9-mo-olds to 0.85–0.89 for 12–23.9-mo-olds and 0.91–0.93 for 24–47.9-mo-olds over the survey years). Overall, MAR values ranged from 0.88 to 0.94 across all age categories for FITS 2002, 2008, and 2016 indicating that the diets of US infants and young children were generally adequate for most micronutrients.
TABLE 2.
Comparison of nutrient intakes and nutrient adequacy for infants aged 0–5.9 mo from the Feeding Infants and Toddlers Studies 2002, 2008, and 20161
| Mean intakes ± SE2 | Nutrient adequacy ratio | ||||||
|---|---|---|---|---|---|---|---|
| 2002 | 2008 | 2016 | 2002 | 2008 | 2016 | ||
| Nutrient | AI2 | n = 467 | n = 382 | n = 600 | n = 467 | n = 382 | n = 600 |
| Vitamin A (μg RAE/d) | 400 | 631 ± 11.7 | 519 ± 8.5 | 574 ± 9.4 | 0.99 | 0.98 | 0.99 |
| Thiamin (mg/d) | 0.2 | 0.5 ± 0.0 | 0.4 ± 0.0 | 0.4 ± 0.0 | 0.85 | 0.83 | 0.85 |
| Riboflavin (mg/d) | 0.3 | 0.8 ± 0.0a | 0.6 ± 0.0b | 0.7 ± 0.0b | 1.00 | 0.99 | 0.99 |
| Niacin (mg/d) | 2 | 6.0 ± 0.2a | 4.6 ± 0.2b | 4.9 ± 0.2b | 0.94 | 0.90 | 0.91 |
| Vitamin B-6 (mg/d) | 0.1 | 0.4 ± 0.0 | 0.3 ± 0.0 | 0.3 ± 0.0 | 0.96 | 0.96 | 0.97 |
| Folate (μg DFE/d) | 65 | 111 ± 5.1 | 100.9 ± 5.4 | 116 ± 4.1 | 0.89 | 0.86 | 0.87 |
| Vitamin B-12 (mg/d) | 0.4 | 1.3 ± 0.0a | 1.2 ± 0.1b | 1.3 ± 0.1b | 0.95 | 1.00 | 1.00 |
| Vitamin C (mg/d) | 40 | 67.1 ± 1.6 | 56.2 ± 1.6 | 61.6 ± 1.5 | 1.00 | 0.99 | 0.99 |
| Vitamin D (μg/d) | 10 | 6.1 ± 0.2 | 5.0 ± 0.3 | 5.7 ± 0.3 | 0.55 | 0.48 | 0.51 |
| Vitamin E (mg/d) | 4 | 9.1 ± 0.2a | 4.0 ± 0.3b | 4.2 ± 0.2b | 1.00 | 0.62 | 0.63 |
| Vitamin K (μg/d) | 2 | 36.2 ± 1.7 | 27.8 ± 1.9 | 31.7 ± 1.6 | 1.00 | 1.00 | 1.00 |
| Calcium (mg/d) | 200 | 470 ± 10.7 | 421 ± 14.8 | 451 ± 11.8 | 1.00 | 1.00 | 1.00 |
| Iron (mg/d) | 0.27 | 9.9 ± 0.5 | 7.2 ± 0.6 | 7.6 ± 0.4 | 0.97 | 0.96 | 0.97 |
| Magnesium (mg/d) | 30 | 57.5 ± 1.6a | 42.9 ± 1.5b | 49.7 ± 1.5b | 0.98 | 0.92 | 0.93 |
| Phosphorus (mg/d) | 100 | 302 ± 8.7 | 224 ± 9.5 | 245 ± 8.7 | 1.00 | 1.00 | 1.00 |
| Potassium (mg/d) | 400 | 704 ± 15.5 | 568 ± 123.7 | 647 ± 14.9 | 1.00 | 0.99 | 0.99 |
| Zinc (mg/d) | 2 | 4.0 ± 0.1 | 3.7 ± 0.2 | 4.0 ± 0.2 | 0.91 | 0.88 | 0.89 |
| Mean adequacy ratio | 0.94 | 0.90 | 0.91 | ||||
Statistical tests were computed through use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age. Mean intakes with different superscripts (a,b) represent an overall difference at P ≤ 0.0001 and a year-to-year difference of P ≤ 0.005 within each age grouping. AI, Adequate Intake; DFE, dietary folate equivalent; RAE, retinol activity equivalent.
There are no RDA values for this age group.
TABLE 5.
Comparison of nutrient intakes and nutrient adequacy for young children 24–47.9 mo from the Feeding Infants and Toddlers Studies 2002, 2008, and 20161
| Mean intakes ± SE | Nutrient adequacy ratio | ||||||
|---|---|---|---|---|---|---|---|
| 2008 | 2016 | 2008 | 2016 | ||||
| Nutrient | RDA2/AI | 2002 | n = 1461 | n = 600 | 2002 | n = 1461 | n = 600 |
| Vitamin A (μg RAE/d) | 3002 | — | 618 ± 24 | 594 ± 18 | — | 0.94 | 0.93 |
| Thiamin (mg/d) | 0.52 | — | 1.2 ± 0.0 | 1.2 ± 0.0 | — | 0.99 | 0.99 |
| Riboflavin (mg/d) | 0.52 | — | 1.7 ± 0.0 | 1.7 ± 0.0 | — | 1.00 | 1.00 |
| Niacin (mg/d) | 62 | — | 13.3 ± 0.3 | 13.9 ± 0.3 | — | 0.98 | 0.99 |
| Vitamin B-6 (mg/d) | 0.52 | — | 1.2 ± 0.0 | 1.3 ± 0.0 | — | 0.99 | 1.00 |
| Folate μg (DFE/d) | 1502 | — | 368 ± 8.4 | 364 ± 10.2 | — | 0.98 | 0.98 |
| Vitamin B-12 (mg/d) | 0.92 | — | 4.1 ± 0.1 | 3.8 ± 0.1 | — | 0.99 | 0.98 |
| Vitamin C (mg/d) | 152 | — | 66.5 ± 2.5 | 73.7 ± 3.8 | — | 0.95 | 0.96 |
| Vitamin D (μg/d) | 152 | — | 6.7 ± 0.2 | 6.3 ± 0.2 | — | 0.44 | 0.41 |
| Vitamin E (mg/d) | 62 | — | 4.5 ± 0.1a | 5.6 ± 0.2b | — | 0.65 | 0.75 |
| Vitamin K (μg/d) | 30 | — | 42.5 ± 3.8a | 48.2 ± 2.6b | — | 0.77 | 0.86 |
| Calcium (mg/d) | 7002 | — | 937 ± 19.4 | 932 ± 27.8 | — | 0.89 | 0.88 |
| Iron (mg/d) | 72 | — | 9.5 ± 0.3 | 9.7 ± 0.3 | — | 0.91 | 0.93 |
| Magnesium (mg/d) | 802 | — | 186 ± 3.1 | 196 ± 4.1 | — | 0.99 | 1.00 |
| Phosphorus (mg/d) | 4602 | — | 959 ± 15.9 | 979 ± 20.7 | — | 0.99 | 0.99 |
| Potassium (mg/d) | 3000 | — | 1787 ± 28.3 | 1890 ± 39.2 | — | 0.59 | 0.62 |
| Zinc (mg/d) | 32 | — | 7.3 ± 0.2 | 7.4 ± 0.2 | — | 0.99 | 1.00 |
| Mean adequacy ratio | — | 0.89 | 0.90 | ||||
Statistical tests were computed through use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age. Mean intakes with different superscripts (a,b) represent an overall difference at P ≤ 0.0001 and a year-to-year difference of P ≤ 0.005 within each age grouping. AI, Adequate Intake; DFE, dietary folate equivalent; RAE, retinol activity equivalent.
Values with a superscript are RDA values; AI values do not have a superscript.
We observed significant declines in mean intakes across FITS survey years for many micronutrients among infants aged 6–11.9 mo (overall P-trend < 0.0001) (Table 3). The largest differences were seen for iron, and vitamins D and E, but significant declines were also observed for vitamin C, thiamin, riboflavin, niacin, magnesium, and phosphorus. Calcium was the only nutrient in this age group that showed an increase over time. Among 12–23.9-mo-olds, mean intakes of vitamin D, potassium, and vitamin C were lower in 2016 (overall P-trend < 0.0001) (Table 4). The only significant trends in mean intakes among 24–47.9-mo-olds were for vitamin E and vitamin K, both of which were higher in 2016 (Table 5).
TABLE 3.
Comparison of nutrient intakes and nutrient adequacy for infants 6–11.9 mo from the Feeding Infants and Toddlers Studies 2002, 2008, and 20161
| Mean intakes ± SE | Nutrient adequacy ratio | ||||||
|---|---|---|---|---|---|---|---|
| 2002 | 2008 | 2016 | 2002 | 2008 | 2016 | ||
| Nutrient | RDA2/AI | n = 1464 | n = 509 | n = 902 | n = 1464 | n = 509 | n = 902 |
| Vitamin A (μg RAE/d) | 500 | 761 ± 11 | 668 ± 22 | 793 ± 17 | 0.96 | 0.93 | 0.95 |
| Thiamin (mg/d) | 0.3 | 0.8 ± 0.0a | 0.7 ± 0.0a,b | 0.7 ± 0.0b | 0.97 | 0.95 | 0.93 |
| Riboflavin (mg/d) | 0.4 | 1.2 ± 0.0a | 1.0 ± 0.0b | 1.0 ± 0.0b | 0.99 | 0.98 | 0.97 |
| Niacin (mg/d) | 4 | 9.9 ± 0.2a | 9.4 ± 0.4a,b | 8.9 ± 0.3b | 0.96 | 0.95 | 0.92 |
| Vitamin B-6 (mg/d) | 0.3 | 0.7 ± 0.0 | 0.7 ± 0.0 | 0.7 ± 0.0 | 0.96 | 0.95 | 0.94 |
| Folate μg (DFE/d) | 80 | 182 ± 7.4 | 220 ± 10.2 | 211 ± 9.2 | 0.96 | 0.96 | 0.95 |
| Vitamin B-12 (mg/d) | 0.5 | 1.8 ± 0.0 | 2.2 ± 0.1 | 2.1 ± 0.1 | 0.96 | 0.98 | 0.96 |
| Vitamin C (mg/d) | 50 | 100 ± 1.5a | 86.0 ± 3.4b | 85 ± 2.4b | 0.98 | 0.95 | 0.94 |
| Vitamin D (μg/d) | 10 | 7.6 ± 0.1a | 6.1 ± 0.3b | 6.7 ± 0.2b | 0.67 | 0.58 | 0.59 |
| Vitamin E (mg/d) | 5 | 9.6 ± 0.2a | 5.6 ± 0.2b | 5.9 ± 0.2b | 0.98 | 0.79 | 0.77 |
| Vitamin K (μg/d) | 2.5 | 53.1 ± 1.4 | 54.6 ± 5.4 | 50.0 ± 1.7 | 1.00 | 0.99 | 1.00 |
| Calcium (mg/d) | 260 | 606 ± 8.2a | 608 ± 19.2a,b | 629 ± 15.7b | 0.99 | 0.98 | 0.98 |
| Iron (mg/d) | 112 | 15.6 ± 0.3a | 15.1 ± 0.6a,b | 13.4 ± 0.4b | 0.88 | 0.84 | 0.77 |
| Magnesium (mg/d) | 75 | 106 ± 1.5a | 100 ± 3.8a,b | 102 ± 2.3b | 0.93 | 0.90 | 0.89 |
| Phosphorus (mg/d) | 275 | 482 ± 7.5a | 448 ± 18.9a,b | 421 ± 11.2b | 0.95 | 0.92 | 0.90 |
| Potassium (mg/d) | 700 | 1174 ± 14.9 | 1086 ± 34.1 | 1139 ± 22.8 | 0.97 | 0.95 | 0.95 |
| Zinc (mg/d) | 32 | 5.4 ± 0.1 | 6.2 ± 0.3 | 6.0 ± 0.2 | 0.94 | 0.94 | 0.92 |
| Mean adequacy ratio | 0.94 | 0.91 | 0.90 | ||||
Statistical tests were computed through use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age. Mean intakes with different superscripts (a,b) represent an overall difference at P ≤ 0.0001 and a year-to-year difference of P ≤ 0.005 within each age grouping. AI, Adequate Intake; DFE, dietary folate equivalent; RAE, retinol activity equivalent.
Values with a superscript are RDA values; AI values do not have a superscript.
TABLE 4.
Comparison of nutrient intakes and nutrient adequacy for toddlers 12–23.9 mo from the Feeding Infants and Toddlers Studies 2002, 2008, and 20161
| Mean intakes ± SE | Nutrient adequacy ratio | ||||||
|---|---|---|---|---|---|---|---|
| 2002 | 2008 | 2016 | 2002 | 2008 | 2016 | ||
| Nutrient | RDA2/AI | n = 1031 | n = 924 | n = 1133 | n = 1031 | n = 924 | n = 1133 |
| Vitamin A (μg RAE/d) | 3002 | 684 ± 16 | 602 ± 17 | 590 ± 12.7 | 0.96 | 0.97 | 0.95 |
| Thiamin (mg/d) | 0.52 | 1.2 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 0.99 | 0.99 | 0.99 |
| Riboflavin (mg/d) | 0.52 | 1.8 ± 0.0 | 1.6 ± 0.0 | 1.6 ± 0.0 | 1.00 | 1.00 | 0.99 |
| Niacin (mg/d) | 62 | 12.4 ± 0.3 | 10.8 ± 0.2 | 11.5 ± 0.2 | 0.96 | 0.97 | 0.96 |
| Vitamin B-6 (mg/d) | 0.52 | 1.2 ± 0.0 | 1.1 ± 0.0 | 1.1 ± 0.0 | 0.99 | 0.99 | 0.98 |
| Folate μg (DFE/d) | 1502 | 307 ± 8.1 | 309 ± 7.7 | 294 ± 6.4 | 0.96 | 0.97 | 0.96 |
| Vitamin B-12 (mg/d) | 0.92 | 3.6 ± 0.1 | 3.9 ± 0.1 | 3.6 ± 0.1 | 0.98 | 0.99 | 0.98 |
| Vitamin C (mg/d) | 152 | 90.0 ± 2.7a | 64.8 ± 3.2b | 65.0 ± 2.2b | 0.98 | 0.93 | 0.95 |
| Vitamin D (μg/d) | 152 | 8.6 ± 0.2a | 7.4 ± 0.2b | 7.1 ± 0.2b | 0.54 | 0.49 | 0.46 |
| Vitamin E (mg/d) | 62 | 5.2 ± 0.1 | 4.0 ± 0.1 | 4.7 ± 0.1 | 0.67 | 0.60 | 0.65 |
| Vitamin K (μg/d) | 30 | 35.5 ± 2.7 | 39.1 ± 3.0 | 42.5 ± 3.1 | 0.72 | 0.73 | 0.76 |
| Calcium (mg/d) | 7002 | 926 ± 15.6 | 913 ± 19.9 | 889 ± 15.6 | 0.90 | 0.91 | 0.89 |
| Iron (mg/d) | 72 | 9.9 ± 0.2 | 9.1 ± 0.2 | 8.6 ± 0.2 | 0.89 | 0.88 | 0.85 |
| Magnesium (mg/d) | 802 | 181 ± 2.4 | 163 ± 2.7 | 170 ± 2.9 | 0.99 | 1.00 | 0.99 |
| Phosphorus (mg/d) | 4602 | 949 ± 13.8 | 856 ± 17.8 | 873 ± 13.4 | 0.98 | 0.98 | 0.97 |
| Potassium (mg/d) | 3000 | 1935 ± 25.3a | 1654 ± 31.8b | 1738 ± 25.9b | 0.63 | 0.55 | 0.57 |
| Zinc (mg/d) | 32 | 6.8 ± 0.1 | 6.6 ± 0.1 | 6.5 ± 0.1 | 0.99 | 0.99 | 0.98 |
| Mean adequacy ratio | 0.89 | 0.88 | 0.88 | ||||
Statistical tests were computed through use of regression models with each nutrient as a dependent variable and year as the independent variable, stratified by age. Mean intakes with different superscripts (a,b) represent an overall difference at P ≤ 0.0001 and a year-to-year difference of P ≤ 0.005 within each age grouping. A, Adequate Intake; DFE, dietary folate equivalent; RAE, retinol activity equivalent.
Values with a superscript are RDA values; AI values do not have a superscript.
Lastly, we examined the intake (mean, g/d) of different food categories by tertile of MAR to obtain information about the food groups that contributed the most to intakes of key nutrients (Figure 1). If intake of the food group rose dramatically with the MAR tertile, it was considered that the food group must have contributed to the adequacy of the diet. From this perspective, it is clear that milk and milk products is the primary food group consumed by infants, toddlers, and young children. Across all of the age groups, increasing dietary adequacy, measured by increasing MAR tertile, was associated with increased consumption of milk and milk products (P < 0.0001). Increasing dietary adequacy was also associated with increased fruit, vegetable, and grain intakes across age groups, although those differences were smaller in magnitude than milk (P < 0.0001). Higher MAR tertiles were also significantly associated with meat/protein intake among toddlers and young children and with mixed dishes intakes among infants aged 6–11.9 mo and toddlers aged 12–23.9 mo (P < 0.0001). In fact, only the categories of sweets/sweetened beverages/desserts and savory snacks were unaffected by diet adequacy, showing no association with the MAR tertile and presumably with micronutrient adequacy.
FIGURE 1.
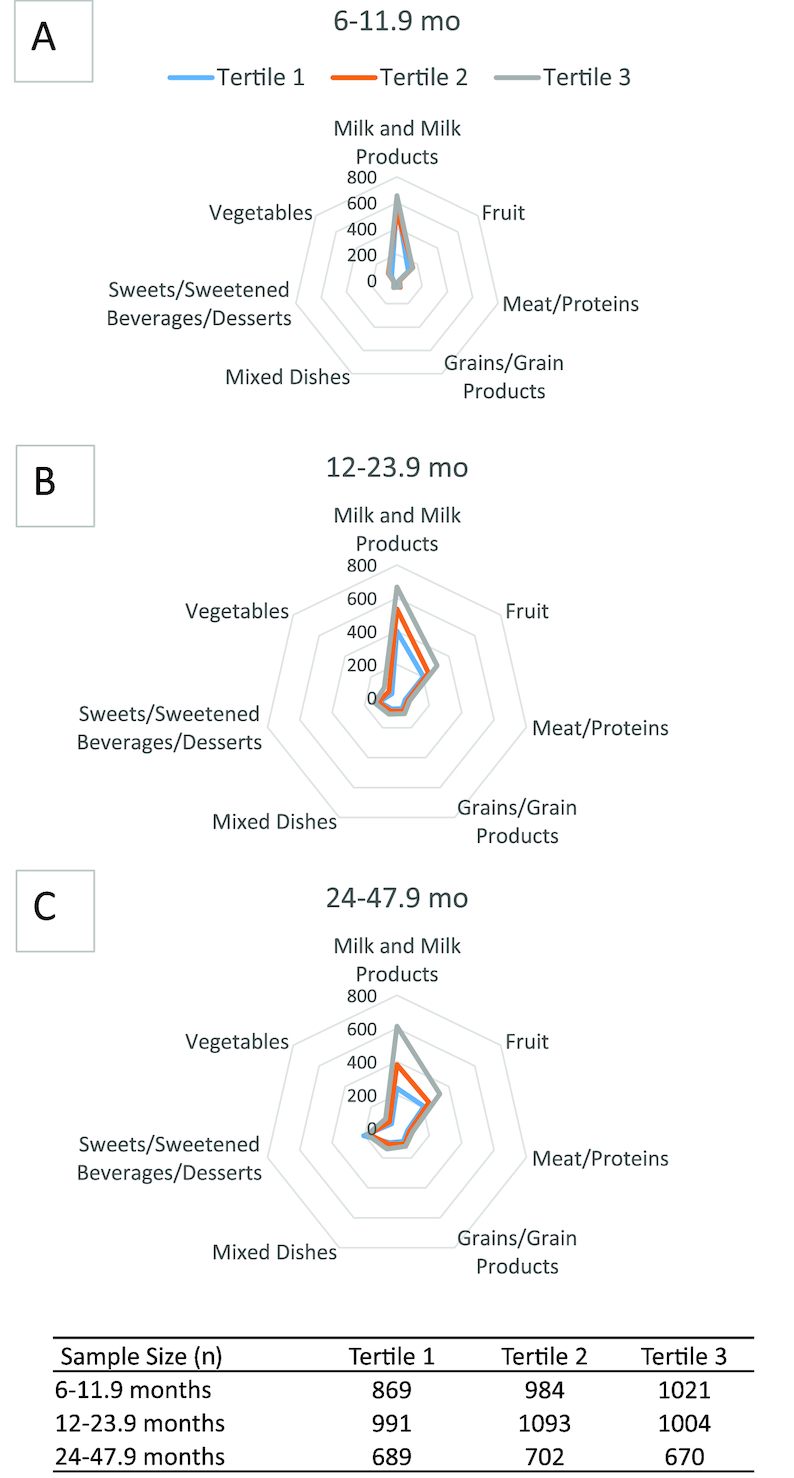
Food groups consumed (mean, g/d) among US infants and young children by age group and tertile of mean adequacy ratio (MAR) values. (A) 6–11.9-mo-olds (2002–2016). (B) 12–23.9-mo-olds (2002–2016). (C) 24–47.9-mo-olds (2008–2016).
Discussion
Diets are homogenous in very young infants, and among young infants under the age of about 6 mo, breast milk is the preferred sole feeding. Because breast milk is low in vitamin D and iron, the American Academy of Pediatrics recommends 400 IU/d of vitamin D supplementation from the first few days of life, and supplemental iron after age 4 mo (1). Iron-fortified infant formulas are an appropriate substitute when breast milk is not available (1).
A healthful and diverse diet provides the basis for satisfactory nutritional status beyond infancy. A more diverse diet starts with the introduction of complementary foods at about 6 mo and becomes more pronounced at age 12 mo. Several nutrients including iron, vitamin D, and fiber, have been identified in recent population-based surveys as warranting emphasis for increased consumption among older infants and young children to ensure dietary adequacy (15). Therefore, early complementary foods should include a source of iron either from fortified infant cereal or meat (rich in heme iron), because by about age 6 mo, breastfeeding is no longer adequate to meet the nutritional needs of infants, and innate iron stores are depleted (36). As with young infants, the American Academy of Pediatrics recommends 400 IU/d vitamin D supplementation for all breastfed infants and children who consume <1 L (33.8 fl oz)/d of formula or fortified milk (37). Official standards for fiber intakes are not available for infants and toddlers aged <1 y, but these too appear to be quite low in comparison to existing recommendations for older children. Meeting required amounts of key nutrients and fiber is challenging in infants and young children who have a small gastric capacity, and is best accommodated by consuming foods that are nutrient-dense relative to energy content (7).
The NAR and MAR values provide an interesting perspective on nutrient adequacy, because with the MAR, it is possible to evaluate general adequacy of the diet from food and beverage intakes. We found that overall dietary adequacy with the MAR was relatively high and quite stable for infants and young children over time. It should be noted that the MAR provides a conservative estimate of adequacy because it is based on the RDA and not the estimated average requirement (EAR), and so a low MAR or NAR does not necessarily indicate dietary inadequacy (e.g., intakes below the EAR). There are few trend data with which to compare our FITS findings in these respects, but NHANES data with combined data sets from 2003–2012 for food and beverage intakes alone also show low percentages of children aged 12–23 mo below the EAR for iron (0.4%), calcium (2.0%), and zinc (0.0%) (16). Among 12–35-mo-olds from NHANES 2011–2012, only vitamins D and E were found to be inadequate in a large portion of the population (86% and 62% below EAR for vitamin D and vitamin E, respectively) (19), similar to our findings. Among infants aged 6–11 mo, NHANES 2009–2012 identified intakes of iron and zinc below the EAR for 10% and 5%, respectively (15). In FITS 2016, 18% of infants aged 6–11.9 mo were below the EAR for iron and 3.5% were below the EAR for zinc (25). Mean nutrient intakes for vitamins (vitamins C, A, D, E) and for minerals (calcium, iron, potassium, and sodium) among 1–3-y-olds from NHANES 2009–2012 from foods and beverages alone (17) were very similar to those we observed in toddlers and young children in FITS.
Our assessment focused on food and beverage sources of nutrients; dietary supplements would likely improve nutrient adequacy among consumers. We have previously reported that 15% of 6–11.9-mo-olds, 21% of 12–23.9-mo-olds, and approximately 40% of 24–47.9-mo-olds took some type of dietary supplement on the day of their recall (25). For example, vitamin D is the most commonly consumed dietary supplement in this age group with 20% of 12–23.9-mo-olds and approximately 40% of 24–47.9-mo-olds consuming supplemental vitamin D. It is important to note that the RDA for vitamin D was established assuming minimal exposure to sunlight. Whether the low dietary intakes of vitamin D in infants and toddlers pose a risk for deficiency would need to be confirmed by blood tests measuring the biomarker of nutritional status 25-hydroxyvitamin D to fully examine the endogenous production from sun exposure. Iron supplements, on the other hand, were consumed by fewer than 10% of the infant and young child population (25). Potassium intakes fell below the AI from the age of 12 mo when the AI increased from 700 to 3000 mg/d, and no infants or children were given potassium supplements. Dietary reference intakes for potassium are currently under review in the United States by the Food and Nutrition Board.
Energy intakes from FITS are similar to those previously shown in NHANES, although differences in time frame and age categorizations makes direct comparisons challenging. Mean energy intakes for age 0–11 mo, 12–23 mo, and 2–3 y were reported as 805 kcal/d, 1253 kcal/d, and 1461 kcal/d, respectively, in NHANES 2011–2014 (20), and 1335 kcal/d for 12–35-mo-olds in NHANES 2011–2012 (19). Energy intakes of 978 kcal/d were reported for 0–24-mo-olds in a combined data set from 2003–2012 NHANES (18), but we have found that energy intakes increase significantly across these ages, so we cannot compare them directly to our findings. We did not observe decreases in energy intake over time as was reported for 2–5-y-olds from NHANES between 1999–2000 and 2009–2010 (14). Instead, reported energy intakes from FITS were quite stable over the period of 2002–2016.
We observed very little difference in MAR across the 3 survey years of FITS. By plotting dietary adequacy, estimated by tertiles of MAR values, by food groups, differences in intakes of milk and milk products, meats and proteins, grains and grain foods, fruits and vegetables were evident. These findings indicate that those food categories were driving the differences in tertiles of MAR values, and underscore an opportunity for developing future dietary guidelines around these categories. Increased consumption of meats and fortified cereals could increase iron intakes, and increased consumption of vegetables could address nutrient shortfalls for potassium, vitamin A, and dietary fiber. Because iron intake is also a concern among 6–11-mo-olds, increased consumption of meats and fortified cereals designed for infants may also be warranted.
This paper compares results from 3 cross-sectional studies of infants and young children from 2002 to 2016. Because of the cross-sectional design, we were unable to evaluate the impact of dietary changes within the same children over time, and the FITS lack data on biomarkers or anthropometrics. FITS are not national probability samples, but sampling weights were calibrated to population distributions for age, sex, race/ethnicity, and educational attainment of the parents to help to remove bias resulting from selection, nonresponse, and coverage. The dietary intake data reported here are based on self-report by mothers or caregivers, and although self-report methods have limitations, they are still considered to be useful for estimations of group-level dietary intakes (38, 39). However, our estimates do not include micronutrient intakes from dietary supplements, but those from food sources only. Although current dietary guidance recommends obtaining nutrients from food sources, our analysis points to important areas for improvement, but it must be recognized that by omitting dietary supplements, the intakes of some infants and children were underestimated. Also, vitamin D can also be obtained from UV light exposure. Another limitation is that breast milk volumes were estimated, not measured.
Despite these limitations, we observed that the adequacy of infant and child diets was quite consistent over time, and the nutrients of concern from FITS are largely consistent with those identified from other national surveys in the United States. However, vitamin D and possibly vitamin E could be considered nutrients of need for infants and young children (depending on supplement use, and sun-exposure in the case of vitamin D), and potassium intakes were low from age 12 mo. Population intakes of iron were low for infants aged 6–11.9 mo. Rather than an expected increase in nutrient intakes, mean intakes among 6–11.9-mo-olds appeared to be lower for several nutrients in 2016 compared to 2002. In contrast, estimated energy intakes and macronutrients were quite stable over the survey years, differing only by age, as would be expected. Because nutrients are optimally obtained from a diverse diet, we will evaluate food intake patterns, and how these patterns have changed over time in future research through use of the FITS. The establishment of Dietary Guidelines for infants and young children will also provide a framework for developing a Healthy Eating Index for these ages, to target guidance to more specific food sources of nutrients.
Supplementary Material
Acknowledgments
We thank Ronette R. Briefel and Mary Kay Fox (Mathematica Policy Research, Washington, DC and Cambridge, MA) as the research coordinating center for FITS 2002 and 2008, and Andrea S. Anater, Principal Investigator (RTI International, Research Triangle Park, NC), research coordinating center for FITS 2016. We also thank Lisa J. Harnack, University of Minnesota and the staff at the Nutrition Coordinating Center for dietary data collection in all 3 surveys (Minneapolis, MN). In addition, we thank Emma Jacquier, Nestlé Research, for helpful comments and review during the development of this manuscript. We are grateful to the thousands of mothers and caregivers who have provided data about their infants and children over the 3 cycles of FITS. The authors’ responsibilities were as follows—ALE, DJC, and RLB: designed the research; DJC and JCH: created the data sets and performed the statistical analyses; all co-authors: participated in the interpretation of findings; all authors: contributed to writing and review; ALE: primary responsibility for final content; and all authors: read and approved the final paper.
Notes
Supported by Nestlé Research, Lausanne, Switzerland.
Author disclosures: ALE is an employee of Nestlé Research (the funding source); DJC and JCH are employees and RLB has consulted for RTI International, the research coordinating center for FITS 2016; JTD is a member of the Scientific Advisory Boards of Conagra Foods and McCormick Spice, and served as a consultant for Nestlé Research until December 2017. RLB currently serves as a consultant for Gerber/Nestlé.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Abbreviations used: AI, Adequate Intake; EAR, estimated average requirement; FITS, Feeding Infants and Toddlers Study; MAR, mean adequacy ratio; NAR, nutrient adequacy ratio.
References
- 1. American Academy of Pediatrics Committee on Nutrition. Pediatric nutrition. 7th ed Elk Grove Village (IL): American Academy of Pediatrics; 2014. [Google Scholar]
- 2. Butte N, Cobb K, Dwyer J, Graney L, Heird W, Rickard K. The Start Healthy Feeding Guidelines for infants and toddlers. J Am Diet Assoc. 2004;104:442–54. [DOI] [PubMed] [Google Scholar]
- 3. Schwartz C, Scholtens PA, Lalanne A, Weenen H, Nicklaus S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite. 2011;57:796–807. [DOI] [PubMed] [Google Scholar]
- 4. Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clin Nutr. 2014;99:723S–8S. [DOI] [PubMed] [Google Scholar]
- 5. Luque V, Escribano J, Closa-Monasterolo R, Zaragoza-Jordana M, Ferre N, Grote V, Koletzko B, Totzauer M, Verduci E, ReDionigi A et al.. Unhealthy dietary patterns established in infancy track to mid-childhood: the EU Childhood Obesity Project. J Nutr. 2018;148:752–9. [DOI] [PubMed] [Google Scholar]
- 6. Mennella JA, Trabulsi JC. Complementary foods and flavor experiences: setting the foundation. Ann Nutr Metab. 2012;60:(Suppl 2):40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Young BE, Krebs NF. Complementary feeding: critical considerations to optimize growth, nutrition, and feeding behavior. Curr Pediatr Rep. 2013;1:247–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pérez-Escamilla R, Segura-Pérez S, Lott M. Feeding guidelines for infants and young toddlers: a responsive parenting approach. Nutr Today. 2017;52:223–31. [Google Scholar]
- 9. Raiten DJ, Raghavan R, Porter A, Obbagy JE, Spahn JM. Executive summary: evaluating the evidence base to support the inclusion of infants and children from birth to 24 mo of age in the Dietary Guidelines for Americans—“the B-24 Project”. Am J Clin Nutr. 2014;99:663S–91S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahluwalia N, Herrick K, Paulose-Ram R, Johnson C. Data needs for B-24 and beyond: NHANES data relevant for nutrition surveillance of infants and young children. Am J Clin Nutr. 2014;99:747S–54S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kleinman RE, Coletta FA.. Historical overview of transitional feeding recommendations and vegetable feeding practices for infants and young children. Nutr Today. 2016;51:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for calcium and vitamin D, Ross AC et al. ed., Washington (DC): National Academies Press; 2011. [PubMed] [Google Scholar]
- 13. Ogata BN, Hayes D.. Position of the Academy of Nutrition and Dietetics: nutrition guidance for healthy children ages 2 to 11 years. J Acad Nutr Diet. 2014;114:1257–76. [DOI] [PubMed] [Google Scholar]
- 14. Ervin RB, Ogden CL.. Trends in intake of energy and macronutrients in children and adolescents from 1999–2000 through 2009–2010. NCHS Data Brief, 2013;113:1–8. [PubMed] [Google Scholar]
- 15. Ahluwalia N, Herrick KA, Rossen LM, Rhodes D, Kit B, Moshfegh A, Dodd KW. Usual nutrient intakes of US infants and toddlers generally meet or exceed Dietary Reference Intakes: findings from NHANES 2009–2012. Am J Clin Nutr. 2016;104:1167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hamner HC, Perrine CG, Scanlon KS. Usual intake of key minerals among children in the second year of life, NHANES 2003–2012. Nutrients. 2016;8:468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Storey ML, Anderson PA.. Nutrient intakes and vegetable and white potato consumption by children aged 1 to 3 years. Adv Nutr. 2016;7:241S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Davis KE, Li X, Adams-Huet B, Sandon L. Infant feeding practices and dietary consumption of US infants and toddlers: National Health and Nutrition Examination Survey (NHANES) 2003–2012. Public Health Nutr. 2018;21:711–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moshfegh AJ, Rhodes DG, Goldman JD, Clemens JC. Characterizing the dietary landscape of children, 12 to 35 months old. Nutr Today. 2017;52:S52–9. [Google Scholar]
- 20. Demmer E, Cifelli CJ, Houchins JA, Fulgoni VL 3rd. The pattern of complementary foods in American infants and children aged 0–5 years old—a cross-sectional analysis of data from the NHANES 2011–2014. Nutrients. 2018;10:(7):827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Devaney B, Kalb L, Briefel R, Zavitsky-Novak T, Clusen N, Ziegler P. Feeding Infants and Toddlers Study: overview of the study design. J Am Diet Assoc. 2004;104:8–13. [DOI] [PubMed] [Google Scholar]
- 22. Ponza M, Devaney B, Ziegler P, Reidy K, Squatrito C. Nutrient intakes and food choices of infants and toddlers participating in WIC. J Am Diet Assoc. 2004;104:71–9. [DOI] [PubMed] [Google Scholar]
- 23. Briefel R, Ziegler P, Novak T, Ponza M. Feeding Infants and Toddlers Study: characteristics and usual nutrient intake of Hispanic and non-Hispanic infants and toddlers. J Acad Nutr Diet. 2006;106:S84–95. [DOI] [PubMed] [Google Scholar]
- 24. Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, Reidy KC. Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed Dietary Reference Intakes. J Am Diet Assoc. 2010;110:S27–37. [DOI] [PubMed] [Google Scholar]
- 25. Bailey RL, Catellier DJ, Jun S, Dwyer JT, Jacquier EF, Anater AS, Eldridge AL. Total usual nutrient intakes of US children (under 48 months): findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr. 2018;148:1557s–66s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jun S, Catellier DJ, Eldridge AL, Dwyer JT, Eicher-Miller HA, Bailey RL. Usual nutrient intakes from the diets of US children by WIC participation and income: findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr. 2018;148:1567s–74s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Briefel RR, Reidy K, Karwe V, Devaney B. Feeding Infants and Toddlers Study: improvements needed in meeting infant feeding recommendations. J Am Diet Assoc. 2004;104:31–7. [DOI] [PubMed] [Google Scholar]
- 28. Briefel RR, Kalb LM, Condon E, Deming DM, Clusen NA, Fox MK, Harnack L, Gemmill E, Stevens M, Reidy KC. The Feeding Infants and Toddlers Study 2008: study design and methods. J Am Diet Assoc. 2010;110:S16–26. [DOI] [PubMed] [Google Scholar]
- 29. Anater AS, Catellier DJ, Levine BA, Krotki KP, Jacquier EF, Eldridge AL, Bronstein KE, Harnack LJ, Lorenzana Peasley JM, Lutes AC. The Feeding Infants and Toddlers Study (FITS) 2016: study design and methods. J Nutr. 2018;148:1516S–24S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nutrition Coordinating Center [Internet]. Food Measurement Aids for Infants and Toddlers. 2016; [accessed 26 October 2018]. Available from: http://www.ncc.umn.edu/wp-content/uploads/2018/10/Food-Measurement-Aids-for-Infants-and-Toddlers-Bilingual.pdf. [Google Scholar]
- 31. Dewey KG, Lonnerdal B.. Milk and nutrient intake of breast-fed infants from 1 to 6 months: relation to growth and fatness. J Pediatr Gastroenterol Nutr. 1983;2:497–506. [DOI] [PubMed] [Google Scholar]
- 32. Dewey KG, Finley DA, Lonnerdal B. Breast milk volume and composition during late lactation (7–20 months). J Pediatr Gastroenterol Nutr. 1984;3:713–20. [DOI] [PubMed] [Google Scholar]
- 33. Kent JC, Mitoulas L, Cox DB, Owens RA, Hartmann PE. Breast volume and milk production during extended lactation in women. Exp Physiol. 1999;84:435–47. [PubMed] [Google Scholar]
- 34. da Costa TH, Haisma H, Wells JC, Mander AP, Whitehead RG, Bluck LJ. How much human milk do infants consume? Data from 12 countries using a standardized stable isotope methodology. J Nutr. 2010;140:2227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guthrie HA, Scheer JC. Nutritional adequacy of self-selected diets that satisfy the four food groups guide. J Nutr Educ. 1981;13:46–9. [Google Scholar]
- 36. Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008;122:(Suppl 2):S36–42. [DOI] [PubMed] [Google Scholar]
- 37. Wagner CL, Greer FR.. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–52. [DOI] [PubMed] [Google Scholar]
- 38. U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans 2015–2020. Washington (DC): 2015. [Google Scholar]
- 39. Subar AF, Freedman LS, Tooze JA, Kirkpatrick SI, Boushey C, Neuhouser ML, Thompson FE, Potischman N, Guenther PM, Tarasuk V et al.. Addressing current criticism regarding the value of self-report dietary data. J Nutr. 2015;145:2639–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


