Abstract
Background
Rates of influenza hospitalizations differ by age, but few data are available regarding differences in laboratory-confirmed rates among adults aged ≥65 years.
Methods
We evaluated age-related differences in influenza-associated hospitalization rates, clinical presentation, and outcomes among 19 760 older adults with laboratory-confirmed influenza at 14 FluSurv-NET sites during the 2011–2012 through 2014–2015 influenza seasons using 10-year age groups.
Results
There were large stepwise increases in the population rates of influenza hospitalization with each 10-year increase in age. Rates ranged from 101–417, 209–1264, and 562–2651 per 100 000 persons over 4 influenza seasons in patients aged 65–74 years, 75–84 years, and ≥85 years, respectively. Hospitalization rates among adults aged 75–84 years and ≥85 years were 1.4–3.0 and 2.2–6.4 times greater, respectively, than rates for adults aged 65–74 years. Among patients hospitalized with laboratory-confirmed influenza, there were age-related differences in demographics, medical histories, and symptoms and signs at presentation. Compared to hospitalized patients aged 65–74 years, patients aged ≥85 years had higher odds of pneumonia (aOR, 1.2; 95% CI, 1.0–1.3; P = .01) and in-hospital death or transfer to hospice (aOR, 2.1; 95% CI, 1.7–2.6; P < .01).
Conclusions
Age-related differences in the incidence and severity of influenza hospitalizations among adults aged ≥65 years can inform prevention and treatment efforts, and data should be analyzed and reported using additional age strata.
Keywords: adult, epidemiology, influenza, human, hospitalization
Rates of hospitalization and risk of death from seasonal influenza increase with age among persons aged ≥65 years; influenza surveillance data from older adults should be analyzed and reported using additional age strata.
Adults aged ≥65 years suffer the most severe health effects of seasonal influenza. Approximately 90% of influenza-related deaths and 50%–70% of influenza-related hospitalizations occur in in this age group [1–3]. Adults aged ≥65 years have more medical comorbidities and age-related reductions in immunity that contribute to an increased risk of severe influenza [4–7]. Many older adults also have exposure to influenza in congregate settings, such as nursing homes, where outbreaks commonly occur [8, 9]. Because of their increased risk, older adults are a priority group for vaccination [10].
For surveillance purposes, adults aged ≥65 years often are treated as a single age group [11]. However, adults aged ≥65 years include a large and heterogeneous group of approximately 46 million people in the United States [12]. The prevalence of chronic diseases changes as age increases beyond 65 years, as does frailty and functional status [13, 14]. In order to better inform surveillance, prevention, and treatment efforts for adults aged ≥65 years, we evaluated age-related differences in influenza-associated hospitalization rates, clinical presentation, and outcomes among older adults using 10-year age strata and population-based surveillance data from the Centers for Disease Control and Prevention’s (CDC) U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
METHODS
We conducted a cross-sectional study of patients aged ≥65 years hospitalized with laboratory-confirmed influenza at 14 FluSurv-NET sites during the 2011–2012 through 2014–2015 influenza seasons. FluSurv-NET has a total catchment of >27 million persons (~9% of the US population) [15]. FluSurv-NET conducted population-based surveillance for influenza-associated hospitalizations at sites in California, Colorado, Connecticut, Georgia, Maryland, Michigan, Minnesota, New Mexico, New York-Albany, New York-Rochester, Ohio, Oregon, Tennessee, and Utah. Cases of laboratory-confirmed influenza hospitalization were identified from laboratory reports and active review of hospital records. Laboratory testing was ordered at the discretion of the healthcare provider and included viral culture, direct or indirect fluorescent antibody staining, rapid antigen testing, or real-time reverse transcription polymerase chain reaction [15]. Patients were included if they were admitted to the hospital within 14 days after and 3 days before a positive influenza test result during October 1–April 30.
FluSurv-NET staff conducted medical record reviews of all cases using standardized case reporting forms. Detailed demographic and medical history was collected, including age, sex, nursing home residence, medical comorbidities, current influenza vaccination status, and antiviral therapy. Specific outcomes of interest included community-acquired pneumonia and in-hospital death or transfer to hospice. We used a standard FluSurv-NET definition of pneumonia, which included a combination of radiographic findings of bronchopneumonia, air space opacity, consolidation, lobar or interstitial infiltrate within 3 days of hospital admission, and either a discharge diagnosis of pneumonia by ICD-10 codes (481–487, 510, 513, or 997.31, International Statistical Classification of Diseases and Related Health Problems, 10th Revision) or documentation of pneumonia on the hospital discharge summary [16, 17]. Acute symptoms and signs were available for the 2014–2015 influenza season only.
For statistical analyses, we categorized patients by age groups 65–74, 75–84, and ≥85 years old. Age-group-specific population denominators were obtained from the National Centers for Health Statistics. Influenza-associated hospitalization rates were adjusted for under-detection related to influenza testing frequency and diagnostic sensitivity at participating hospitals, as previously described [3]. We calculated 95% confidence intervals (95% CI) using Monte Carlo simulations.
Among patients hospitalized with influenza, differences in demographic and medical history covariates and acute symptoms and signs by age group were evaluated using Cochran-Armitage Χ2 test for trend. We used multivariable logistic regression to evaluate the odds of each outcome associated with age after adjusting for sex, nursing home residence, morbid obesity, smoking, neurologic disorder, cardiovascular disease, renal disease, asthma, chronic lung disease, immunosuppression, influenza vaccination, season, and study site. Receipt of antiviral therapy was included in the model for in-hospital death or transfer to hospice, but not for pneumonia, because we could not determine whether antiviral therapy preceded development of pneumonia in time. These potential confounders were defined a priori as known risk factors for severe influenza [10]. In a secondary analysis, we modeled the crude association of age as a continuous variable with the probability of pneumonia or in-hospital death or transfer to hospice using logistic regression. Model parameters for age were chosen using the likelihood ratio test and plots of observed versus expected values to determine best model fit. P-values ≤0.05 were considered statistically significant. Analyses were completed using SAS for Windows version 9.4 (SAS, Cary, NC).
FluSurv-NET activities were considered nonresearch for public health purposes by the institutional review board at CDC, and FluSurv-NET sites obtained human subjects and ethics approvals from their respective state health department and academic partner institutional review boards.
RESULTS
Across 4 influenza seasons, there were 19 760 patients aged ≥65 years with laboratory-confirmed influenza hospitalization identified by FluSurv-NET surveillance. These included 5956 (30.1%) patients aged 65–74 years, 6998 (35.4%) aged 75–84 years, and 6806 (34.4%) aged ≥85 years (Table 1). By season, 921 (4.7%), 5526 (28.0%), 2765 (14.0%), and 10 548 (53.4%) patients were hospitalized during the 2011–2012, 2012–2013, 2013–2014, and 2014–2015 influenza seasons, respectively. Influenza A(H1N1) was the predominant circulating virus during the 2013–2014 season, whereas influenza A(H3N2) was the predominant circulating virus during other seasons.
Table 1.
Demographics and Medical History of Older Adult Patients Hospitalized With Laboratory-Confirmed Influenza—FluSurv-NET, 2011–2012 Through 2014–2015 Influenza Seasons (n = 19 760), by Age Group
| 65–74 Years Old | 75–84 Years Old | ≥85 Years Old | ||
|---|---|---|---|---|
| (n = 5956) | (n = 6998) | (n = 6806) | ||
| no. (%) | no. (%) | no. (%) | P a | |
| Season | <.01 | |||
| 2011–2012 | 281 (4.7) | 348 (5.0) | 292 (4.3) | |
| 2012–2013 | 1596 (26.8) | 1969 (28.1) | 1961 (28.8) | |
| 2013–2014 | 1283 (21.5) | 940 (13.4) | 542 (8.0) | |
| 2014–2015 | 2796 (46.9) | 3741 (53.5) | 4011 (58.9) | |
| Female sex | 3114 (42.3) | 3733 (53.3) | 4056 (59.6) | <.01 |
| Non-white raceb | 1297 (24.9) | 1150 (18.8) | 734 (12.3) | <.01 |
| Hispanic ethnicityb | 369 (8.0) | 386 (7.3) | 227 (4.5) | <.01 |
| Nursing home residentb | 666 (11.3) | 1303 (18.8) | 2695 (40.0) | <.01 |
| Morbid obesityb | 580 (10.4) | 330 (5.0) | 105 (1.7) | <.01 |
| Current smoking | 1195 (20.0) | 556 (8.0) | 156 (2.3) | <.01 |
| Current alcohol | 177 (3.0) | 96 (1.4) | 57 (0.8) | <.01 |
| Neurologic disorder | 987 (16.6) | 1777 (25.4) | 2501 (36.8) | <.01 |
| Chronic cardiovascular disease | 3055 (52.3) | 4328 (61.9) | 4500 (66.1) | <.01 |
| Renal disease | 1218 (20.5) | 1764 (25.2) | 1769 (26.0) | <.01 |
| Asthma | 1081 (18.2) | 870 (12.4) | 618 (9.1) | <.01 |
| Chronic lung disease | 2429 (40.8) | 2366 (33.8) | 1683 (24.7) | <.01 |
| Chronic metabolic disease | 2989 (50.2) | 3464 (49.5) | 2947 (43.3) | <.01 |
| Immunosuppressive condition | 1214 (20.4) | 939 (13.4) | 603 (8.9) | <.01 |
| Hemoglobinopathy | 343 (5.8) | 430 (6.1) | 418 (6.1) | .38 |
| Neuromuscular disorder | 373 (6.3) | 462 (6.6) | 409 (6.0) | .52 |
| History of Guillain-Barre Syndrome | 11 (0.2) | 19 (0.3) | 18 (0.3) | .37 |
| Influenza vaccineb | 3135 (57.8) | 4058 (64.8) | 4236 (70.1) | <.01 |
| Antiviral therapyb | 5009 (84.6) | 6059 (87.1) | 5906 (87.5) | <.01 |
| Pneumonia | 1233 (20.7) | 1472 (21.0) | 1576 (23.2) | <.01 |
| In-Hospital death or transfer to hospiceb | 225 (3.8) | 370 (5.3) | 588 (8.7) | <.01 |
aCochran-Armitage Χ2 test for trend except for season for which a standard Χ2 test was used.
bMissing data excluded from % (non-white race: 12% missing, no association with age; Hispanic ethnicity: 24% missing, increase from 23% to 26% with age; morbid obesity: 6% missing, no association with age; influenza vaccine: 10% missing, increase from 9% to 11% with age; antiviral therapy: <1% missing, no association with age; in-hospital death or transfer to hospice: 1% missing, no association with age).
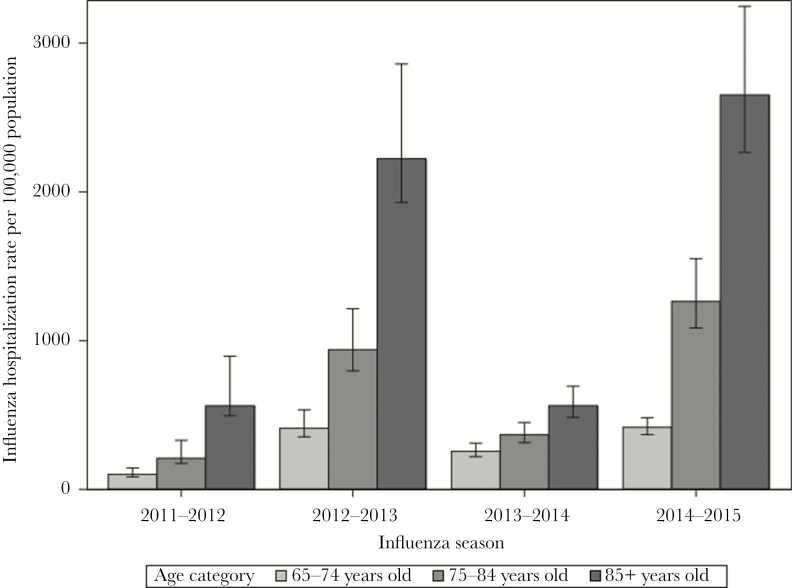
There were stepwise increases in estimated population rates of influenza-associated hospitalization with age during each influenza season (Figure 1), with the highest rates occurring in adults aged ≥85 years (Supplemental Table). Depending on the season, the rate of influenza-associated hospitalization for adults aged 75–84 years was 1.4 to 3.0 times higher than the rate for adults aged 65–74 years, and the rate for adults aged ≥85 years was 2.2 to 6.4 times higher than the rate for adults aged 65–74 years. Hospitalization rates were highest during the 2012–2013 and 2014–2015 influenza seasons. Differences in hospitalization rates by age group did not appear to be as great during the H1N1 predominant season (Figure 1).
Figure 1.
Estimated population rates of influenza-associated hospitalization with 95% confidence intervals by influenza season and age group—U.S Influenza Hospitalization Surveillance Network (FluSurv-NET). Influenza A(H3N2) was the predominant circulating virus during the 2011–2012, 2012–2013, and 2014–2015 seasons. Influenza A(H1N1) predominated during the 2013–2014 season.
Among patients with laboratory-confirmed influenza hospitalization, older patients were more likely to be female, white, and non-Hispanic (P < .01) (Table 1). Of note, the frequency of nursing home residence increased with age from 11.3% of patients aged 65–74 years to 40.0% of patients aged ≥85 years-old (P < .01). Increasing age was associated with increasing frequency of neurologic disorder, cardiovascular disease, and renal disease. The frequency of morbid obesity, smoking, alcohol use, asthma, chronic lung disease, chronic metabolic disease, and immunosuppression decreased with increasing age (P < .01 for each). Finally, the frequency of seasonal influenza vaccination increased with age (P < .01), as did receipt of antivirals (P < .01).
Among the 10 548 (53.4%) patients from the 2014–2015 influenza season for which we had data about symptoms and signs at admission, cough was common in all age groups (~80%) (Table 2). The frequency of altered mental status increased with age (14.3% of patients aged 65–74 years, 20.7% of patients aged 75–84 years, and 23.0% of patients aged ≥85 years, P < .01). Conversely, the frequency of fever, shortness of breath, nasal congestion or rhinitis, myalgia, nausea or vomiting, wheezing, chest pain, diarrhea, sore throat, and headache decreased with age (<0.01). Many of these trends, though statistically significant, were associated with relatively small absolute differences in symptom or sign frequency between the youngest and oldest age groups, on the order of 5%–10%.
Table 2.
Acute Signs or Symptoms at Admission of Older Adult Patients Hospitalized With Laboratory-Confirmed Influenza—FluSurv-NET, 2014–2015 Influenza Season (n = 10 548), by Age Group
| 65–74 Years Old | 75–84 Years Old | ≥85 Years Old | ||
|---|---|---|---|---|
| (n = 2796) | (n = 3741) | (n = 4011) | ||
| no. (%) | no. (%) | no. (%) | P a | |
| Cough | 2234 (79.9) | 3041 (81.3) | 3213 (80.1) | .97 |
| Fever | 1754 (63.0) | 2202 (59.1) | 2197 (55.1) | <.01 |
| Shortness of breath/respiratory distress | 1662 (59.4) | 2011 (53.8) | 1970 (49.1) | <.01 |
| Congested/runny nose | 708 (25.3) | 896 (24.0) | 902 (22.5) | .01 |
| Myalgia/muscle aches | 685 (24.5) | 708 (18.9) | 558 (13.9) | <.01 |
| Nausea/vomiting | 621 (22.2) | 691 (18.5) | 611 (15.2) | <.01 |
| Wheezing | 583 (20.9) | 706 (18.9) | 646 (16.1) | <.01 |
| Chest pain | 441 (15.8) | 457 (12.2) | 310 (7.7) | <.01 |
| Altered mental status/confusion | 401 (14.3) | 773 (20.7) | 921 (23.0) | <.01 |
| Diarrhea | 363 (13.0) | 402 (10.8) | 376 (9.4) | <.01 |
| Sore throat | 345 (12.3) | 387(10.3) | 311 (7.8) | <.01 |
| Headache | 334 (12.0) | 286 (7.7) | 195 (4.9) | <.01 |
| Rash | 10 (0.4) | 16 (0.4) | 10 (0.3) | .38 |
| Conjunctivitis/pink eye | 9 (0.3) | 10 (0.3) | 13 (0.3) | .94 |
| Seizures | 3 (0.1) | 8 (0.2) | 5 (0.1) | .96 |
aCochran-Armitage Χ2 test for trend.
Pneumonia occurred in 1233 (20.7%) patients aged 65–74 years, 1472 (21.0%) patients aged 75–84 years, and 1576 (23.2%) patients aged ≥85 years (Table 1). In univariate analysis, compared to 65–74 year old patients, ≥85 year old patients had a 20% increased odds of pneumonia (OR, 1.2; 95% CI, 1.1–1.3; P < .01) (Table 3). The relative odds of pneumonia were similar after adjusting for sex, medical comorbidities, influenza vaccination, season, and study site (aOR, 1.2; 95% CI, 1.0–1.3; P = .01). In the multivariable model, male sex, nursing home residence, chronic lung disease, and immunosuppression also were associated with the occurrence of pneumonia, while asthma was inversely associated with this outcome (P < .01 for each).
Table 3.
Odds Ratios for Pneumonia And Death or Transfer to Hospice Among Older Adult Patients Hospitalized With Laboratory-Confirmed Influenza, Univariate and Multivariable Analyses—FluSurv-NET, 2011–2012 Through 2014–2015 Influenza Seasons
| Pneumoniaa | In-hospital Death or Transfer to Hospiceb | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariable Analysis | Univariate Analysis | Multivariable Analysis | |||||
| ORc | 95% CI | aORc | 95% CI | ORc | 95% CI | aORc | 95% CI | |
| Age, years | ||||||||
| 65–74 | — | — | — | — | — | — | — | — |
| 75–84 | 1.0 | 0.9, 1.1 | 1.0 | 0.9, 1.1 | 1.4 | 1.2, 1.7 | 1.4 | 1.2, 1.7 |
| ≥85 | 1.2 | 1.1, 1.3 | 1.2 | 1.0, 1.3 | 2.4 | 2.1, 2.8 | 2.1 | 1.7, 2.6 |
| Male sex | 1.2 | 1.2, 1.3 | 1.2 | 1.1, 1.3 | 0.9 | 0.8, 1.1 | 1.0 | 0.9, 1.1 |
| Nursing home resident | 1.3 | 1.2, 1.4 | 1.3 | 1.2, 1.5 | 2.8 | 2.5, 3.2 | 2.4 | 2.0, 2.7 |
| Morbid obesity | 0.8 | 0.7, 0.9 | 0.9 | 0.7, 1.1 | 0.9 | 0.6, 1.1 | 1.1 | 0.8, 1.5 |
| Current smoking | 1.0 | 0.9, 1.1 | 0.9 | 0.8, 1.1 | 0.7 | 0.6, 0.9 | 0.9 | 0.7, 1.2 |
| Neurologic disorder | 1.1 | 1.0, 1.2 | 1.0 | 0.9, 1.1 | 2.0 | 1.8, 2.3 | 1.5 | 1.3, 1.8 |
| Cardiovascular disease | 1.1 | 1.0, 1.2 | 1.0 | 0.9, 1.1 | 1.5 | 1.4, 1.7 | 1.3 | 1.1, 1.5 |
| Renal disease | 1.2 | 1.1, 1.3 | 1.1 | 1.0, 1.2 | 1.5 | 1.3, 1.7 | 1.4 | 1.2, 1.7 |
| Asthma | 0.8 | 0.7, 0.9 | 0.8 | 0.7, 0.9 | 0.6 | 0.5, 0.7 | 0.7 | 0.5, 0.8 |
| Chronic lung disease | 1.1 | 1.0, 1.2 | 1.1 | 1.0, 1.2 | 1.3 | 1.1, 1.5 | 1.5 | 1.3, 1.8 |
| Chronic metabolic disease | 1.0 | 0.9, 1.0 | 1.0 | 0.9, 1.1 | 1.0 | 0.9, 1.1 | 0.9 | 0.8, 1.1 |
| Immunosuppression | 1.2 | 1.1, 1.4 | 1.2 | 1.1, 1.4 | 1.4 | 1.2, 1.6 | 1.9 | 1.6, 2.2 |
| Vaccinated | 1.0 | 0.9, 1.1 | 1.0 | 0.9, 1.1 | 0.9 | 0.8, 1.1 | 0.8 | 0.7, 0.9 |
| Antiviral therapy | NA | NA | NA | NA | 0.7 | 0.6, 0.9 | 0.6 | 0.5, 0.8 |
| Season | ||||||||
| 2011–2012 | — | — | — | — | — | — | — | — |
| 2012–2013 | 0.9 | 0.7, 1.1 | 1.1 | 0.9, 1.4 | 1.1 | 0.8, 1.6 | 1.3 | 0.9, 1.9 |
| 2013–2014 | 1.6 | 1.3, 1.9 | 1.9 | 1.5, 2.3 | 1.4 | 1.0, 2.0 | 1.9 | 1.2, 2.8 |
| 2014–2015 | 1.2 | 1.0, 1.4 | 1.4 | 1.2, 1.7 | 1.3 | 0.9, 1.7 | 1.4 | 1.0, 2.1 |
Abbreviations: 95% CI, 95% confidence interval, aOR, adjusted odds ratio; OR, odds ratio; NA, not applicable.
aFor univariate analyses of pneumonia, n varies by characteristic (see Table 1). For the multivariable analysis, n = 16 644. The multivariable analysis included adjustment for study site. A Hosmer and Lemeshow goodness-of-fit test indicated no evidence of lack of model fit (P = .90).
bFor univariate analyses of in-hospital death or transfer to hospice, N varies by characteristic (see Table 1). For the multivariable analysis, N = 16 561. The multivariable analysis included adjustment for study site. A Hosmer–Lemeshow goodness-of-fit test indicated no evidence of lack of model fit (P = .40).
cThe reference categories for age and season are indicated by “—”. The reference category for other characteristics is absence of the characteristic.
In-hospital death or transfer to hospice occurred in 225 (3.8%) patients aged 65–74 years, 370 (5.3%) patients aged 75–84 years, and 588 (8.7%) patients aged ≥85 years (Table 1). In univariate analysis, compared to 65–74 year-old patients, the odds of in-hospital death or transfer to hospice increased with age (patients aged 75–84 years: OR, 1.4; 95% CI, 1.2–1.7; P < .01; patients aged ≥85 years: OR, 2.4; 95% CI, 2.1–2.8; P < .01) (Table 3). In multivariable analysis, compared to patients aged 65–74 years, patients aged 75–84 years had a 40% increased odds of in-hospital death or transfer to hospice (aOR, 1.4; 95% CI, 1.2–1.7; P < .01) and patients aged ≥85 years had a 110% increased odds of in-hospital death or transfer to hospice (aOR, 2.1; 95% CI, 1.7–2.6; P < .01) after adjusting for sex, medical comorbidities, influenza vaccination, receipt of antiviral therapy, season, and study site. In the multivariable model, nursing home residence, neurologic disorder, cardiovascular disease, renal disease, chronic lung disease, and immunosuppression were associated with in-hospital death or transfer to hospice, while asthma, receipt of influenza vaccine, and receipt of antiviral therapy were inversely associated (P < .01 for each).
When patient outcomes were plotted against age as a continuous variable, the slope of the association steepened with age, most notably for in-hospital death or transfer to hospice (Supplemental Figure A–B). A quadratic model of age best fit this nonlinear association. According to the model, probability of pneumonia increased after the age of 80–85 years. The probability of in-hospital death or transfer to hospice increased exponentially throughout the age range (Supplemental Figure C–D).
DISCUSSION
Using data from a large network of hospitals, we demonstrated important age-related differences in the epidemiology, clinical presentation, and outcomes of laboratory-confirmed influenza hospitalization among adults aged ≥65 years. This group of older patients is traditionally reported on together in influenza surveillance. However, there were large stepwise increases in the population rates of influenza hospitalization with each 10-year increase in age, with rates ranging from 101–417, 209–1264, and 562–2651 per 100 000 persons in patients aged 65–74 years, 75–84 years, and ≥85 years, respectively. Influenza hospitalization rates for patients aged ≥85 years were 2.2–6.4 times greater than the hospitalization rates for patients 65–74 years. Among patients hospitalized with laboratory-confirmed influenza, ≥85 year-old patients had a 20% increased odds of pneumonia and more than a 2-fold increased odds of death or transfer to hospice compared to 65–74 year-old patients. Although we chose to stratify patients according to 10-year age strata a priori, our findings of an exponential increase in probability of death or transfer to hospice when age was modeled as a continuous variable suggest that use of age-strata smaller than 10 years may useful for influenza surveillance or research among older adults.
Previous studies have evaluated the relationship between older age and rates of respiratory hospitalization in the United States using diagnostic codes from administrative records. In an analysis of data from the Centers for Medicare and Medicaid Services (CMS), the average annual rate of pneumonia and influenza hospitalizations increased from 17.9 per 1000 people to 95.5 per 1000 people as age increased from 65–74 years to ≥85 years, respectively [18]. More recently, in a time series analysis using data from the U.S. Nationwide Inpatient Sample and nationwide laboratory-based virus surveillance, the rate of respiratory hospitalization attributable to influenza was estimated to be 157 per 100 000 persons aged ≥75 years compared to 49 per 100 000 persons aged 65–74 years during 1997–2009 [19]. Other studies using a variety of methods have demonstrated analogous age-related trends among older adults hospitalized for influenza and related outcomes, including influenza-associated respiratory failure and pneumonia [20–23]. Using data from FluSurv-NET allowed us to evaluate the relationship of older age with rates of laboratory-confirmed influenza hospitalization and the clinical epidemiology of severe influenza in older adults, which studies based on administrative coding are unable to do.
We found age-related differences in demographics and the medical histories of patients hospitalized with laboratory-confirmed influenza. These included increased frequency of neurologic, cardiovascular, and renal disease; decreased frequency of chronic lung disease, chronic metabolic disease, and immunosuppression; and decreased frequency of risk factors for chronic disease such as morbid obesity, smoking, and alcohol use with age. The increasing frequency of neurologic disorder with age from 17% to 37% in our study is similar to the trend of increasing frequency of dementia from 5% to 21% among patients hospitalized for pneumonia and influenza in the CMS study noted above [18]. To some extent, our findings of age-related differences reflect the underlying prevalence of chronic disease [13]. Nevertheless, the above medical conditions are risk factors for hospitalization and other severe outcomes of influenza [5]. We further demonstrated their relative importance to these endpoints by age.
The increase in frequency of nursing home residence from 11% among patients aged 65–74 years to 40% among patients aged ≥85 years was notable. In the United States, over 4 million persons are admitted to or reside in nursing homes each year [24]. Nursing home residence is both a marker of vulnerability to influenza and an opportunity for exposure. Nursing home residents often are frail, have multiple medical comorbidities and functional impairments, share living space and care givers, and transfer between healthcare settings [8, 9]. Nursing home outbreaks are common during influenza seasons and are associated with high attack rates [8, 9]. In our study, nursing home residence was the strongest independent risk factor for pneumonia and in-hospital death or transfer to hospice.
Consistent with prior studies, most older patients hospitalized with laboratory-confirmed influenza presented with cough, while fewer (55%–65%), presented with fever [25, 26]. The frequency of fever and several other typical symptoms of influenza decreased in frequency with age beyond 65 years. In addition, we found that older patients were more likely to have altered mental status upon admission. Others have documented that compared to patients aged <65 years hospitalized with influenza, patients aged ≥65 years less often report fever and systemic symptoms [26]. Although influenza infection may manifest differently in older adults as they age, selection biases related to healthcare provider admission and testing practices may account for some of our findings. Practices may change with age and underlying conditions, such that older adults may be hospitalized with fewer signs and symptoms. This is the case for pneumonia, where older age alone is a strong criterion for hospital admission [27]. The oldest patients may have had cognitive deficits or communication challenges that may have led them to underreport symptoms [8]. It is worthwhile to note that we were able to identify relatively small age-related differences in clinical presentation that may be difficult to incorporate into guidance for clinical practice.
The increasing risk of in-hospital death or transfer to hospice with age among patients hospitalized with laboratory-confirmed influenza in our study emphasizes the importance of existing recommendations to vaccinate older adults and their contacts for primary prevention and to promptly initiate antiviral therapy in older adult patients for chemoprophylaxis or treatment influenza infection [10, 28, 29]. Although we found a reduced odds of in-hospital death or transfer to hospice associated with influenza vaccination and receipt of antiviral therapy, our study was not designed to assess these effects. We did not account for timing of administration or type of vaccine or antiviral therapy received. Nor did we address competing risks that may have biased our results [16]. Other studies have looked at the efficacy and effectiveness of influenza vaccination and antiviral therapy in older adults in more detail [10, 28]. Also of note, frequency of influenza vaccination among the hospitalized patients in this study increased with age and was lower than the coverage estimate for the noninstitutionalized U.S. population aged ≥65 years, which was estimated to be 73.5% during the 2014–2015 influenza season [30]. Although antiviral therapy is generally underutilized [31, 32], a high proportion of patients in this study received antiviral therapy, likely due in part to the exclusion of influenza patients without laboratory confirmation of diagnosis.
Similar to the findings here, other analyses of FluSurv-NET data prior to the 2009 pandemic indicated that older age (≥75 years) was associated with an 30% increased risk of pneumonia compared to younger patients [33]. The current study suggests that the increased risk of pneumonia is evident only in patients aged ≥85 years when compared to patients aged 65–74 years (aOR, 1.2; 95% CI, 1.0–1.3; P = .01). Of interest, both our current study and a prior FluSurv-NET study found a negative association between asthma and pneumonia [33]. This may be a reflection of biases in testing and admission practices of patients with certain underlying conditions as previously described [33, 34]. Because influenza infection and older age increase a person’s susceptibility to secondary bacterial pneumonia [21, 22, 35, 36], vaccination of older adults with pneumococcal conjugate and polysaccharide vaccines is an important preventive measure [37]. Management of bacterial pneumonia should include prompt initiation of antibiotic therapy as recommended by practice guidelines [27].
This study has several strengths. First, the study included a large, multi-site, multi-season population-based sample of adults hospitalized with influenza in the United States. Second, our study of laboratory-confirmed influenza evaluated influenza in older adults in a more specific fashion with a lower likelihood of diagnosis misclassification than prior studies that may have relied on diagnostic codes or symptoms. Finally, detailed clinical data from patients allowed us to evaluate important demographic and clinical features, epidemiologic exposures, and specific clinical outcomes.
There are several potential limitations to our study. First, we were unable to formally assess how differences in provider testing and admission practices across sites, over time, or with patient age may have influenced our findings [38]. Second, the findings that older age was an independent risk factor for pneumonia and in-hospital death or transfer to hospice suggests that there were unmeasured age-related factors (eg, frailty or functional status) that may account for these associations [39, 40]. We did not have data on frailty or functional status and relied on nursing home residence as a marker for frailty in our analyses. Finally, the cross-sectional study design did not allow us to determine causality of association, nor was our study designed to evaluate the roles of vaccination or antiviral therapy. Despite these potential limitations, our findings add to the knowledge base of influenza in older adults.
In summary, there are age-related differences in the epidemiology, clinical presentation, and outcomes of adults aged ≥65 years hospitalized with influenza. Of these, a significant increase in rate of hospitalization and increased mortality following hospitalization with age are of the greatest public health concern. Our findings emphasize the importance of existing recommendations for the use of influenza vaccine and antiviral therapies [10, 28, 29, 37]. Newer high-dose and adjuvented influenza vaccines available for persons aged ≥65 years may provide additional protection for this age group [10]. Public health epidemiologists should analyze and report influenza surveillance data using additional age strata for older adults to demonstrate increasing vulnerability of the aging population and to identify opportunities to improve preventive care.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
Deborah Aragon, Mary Kohrman, Jillian Jaskunas, Chelsea Stacy, and Samie Stephens, Colorado Department of Public Health and Environment, Denver, Colorado; Alissa O’Halloran and Carrie Reed, Centers for Disease Control and Prevention, Atlanta, Georgia; Kyle Openo and Monica M. Farley, Georgia Emerging Infections Program, Atlanta, Georgia; Christina Felsen and Maria Gaitan, University of Rochester School of Medicine and Dentistry, Rochester, New York; Krista Lung and Nicholas Fisher, Ohio Department of Health, Columbus, Ohio; Pam Daily Kirley and Art Reingold, California Emerging Infections Program, Oakland, California; Kathy Angeles, Lisa Butler, and Sarah Khanlian, New Mexico Emerging Infections Program, Albuquerque, New Mexico; Ruth Lynfield, Craig Morin, and Anna Strain, Minnesota Department of Health, St. Paul, Minnesota; Patricia Ryan, Brian Bachaus, Emily Blake, Amanda Palmer, Rebecca Perlmutter, Shaylee Mehta, and Molly Hyde, Maryland Department of Health, Baltimore, Maryland; Nancy Spina, New York State Department of Health, Albany, New York; Karen Leib and Katie Dyer, Vanderbilt University School of Medicine, Nashville, Tennessee; Matt Laidler, Oregon Public Health Division, Portland, Oregon; Tamara Rissman and James Meek, Connecticut Emerging Infections Program, Yale School of Public Health, New Haven, Connecticut.
Financial support. This work was supported by the Centers for Disease Control and Prevention (cooperative agreements CDC-RFA-CK17-1701 and 5U38OT000143).
Potential conflicts of interest. N.A. reports grants from the Centers for Disease Control and Prevention Emerging Infections Program Cooperative Agreement; E.J.A. reports personal fees from AbbVie, grants from Merck, Pfizer, Regeneron, Sanofi Pasteur, Novavax, Micron, and PaxVax; W.S. reports personal fees from Merck, Pfizer, Seqirus, Dyanavax, SutroVax, and Shionogi; and R.K.H. reports grants from the Centers for Disease Control and Prevention. All other authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. Estimates of deaths associated with seasonal influenza — United States, 1976–2007. MMWR Morb Mortal Wkly Rep 2010; 59:1057–62. [PubMed] [Google Scholar]
- 2. Zhou H, Thompson WW, Viboud CG, et al. . Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis 2012; 54:1427–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Reed C, Chaves SS, Daily Kirley P, et al. . Estimating influenza disease burden from population-based surveillance data in the United States. PLOS ONE 2015; 10:e0118369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Quandelacy TM, Viboud C, Charu V, et al. . Age- and sex-related risk factors for influenza-associated mortality in the United States between 1997–2007. Am J Epidemiol 2014; 179:156–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mertz D, Kim TH, Johnstone J, et al. . Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ 2013; 347:f5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pop-Vicas A, Gravenstein S. Influenza in the elderly: a mini-review. Gerontology 2011; 57:397–404. [DOI] [PubMed] [Google Scholar]
- 7. Poland GA, Ovsyannikova IG, Kennedy RB, et al. . A systems biology approach to the effect of aging, immunosenescence and vaccine response. Curr Opin Immunol 2014; 29:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lansbury LE, Brown CS, Nguyen-Van-Tam JS. Influenza in long-term care facilities. Influenza Other Respir Viruses 2017; 11:356–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strausbaugh LJ, Sukumar SR, Joseph CL. Infectious disease outbreaks in nursing homes: an unappreciated hazard for frail elderly persons. Clin Infect Dis 2003; 36:870–6. [DOI] [PubMed] [Google Scholar]
- 10. Grohskopf LA, Sokolow LZ, Broder KR, et al. . Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices - United States, 2017-18 Influenza Season. MMWR Recomm Rep 2017; 66:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. FluView https://www.cdc.gov/flu/weekly/. Accessed May 3, 2019.
- 12. United States Census Bureau. American Community Survey https://www.census.gov/programs-surveys/acs/. Accessed May 3, 2019.
- 13. Schoenborn CA, Heyman KM. Health characteristics of adults aged 55 years and over: United States, 2004–2007. Natl Health Stat Report 2009, 16. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 14. Clegg A, Young J, Iliffe S, et al. . Frailty in elderly people. Lancet 2013; 381:752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chaves SS, Lynfield R, Lindegren ML, et al. . The US influenza hospitalization surveillance network. Emerg Infect Dis 2015; 21:1543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Arriola CS, Garg S, Anderson EJ, et al. . Influenza vaccination modifies disease severity among community-dwelling adults hospitalized with influenza. Clin Infect Dis 2017; 65:1289–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bramley AM, Chaves SS, Dawood FS, et al. . Utility of keywords from chest radiograph reports for pneumonia surveillance among hospitalized patients with influenza: the CDC influenza hospitalization surveillance network, 2008–2009. Public Health Rep 2016; 131:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Naumova EN, Parisi SM, Castronovo D, et al. . Pneumonia and influenza hospitalizations in elderly people with dementia. J Am Geriatr Soc 2009; 57:2192–9. [DOI] [PubMed] [Google Scholar]
- 19. Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of hospitalization attributable to influenza and RSV in the US during 1997–2009, by age and risk status. BMC Public Health 2017; 17:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ortiz JR, Neuzil KM, Rue TC, et al. . Population-based incidence estimates of influenza-associated respiratory failure hospitalizations, 2003 to 2009. Am J Respir Crit Care Med 2013; 188:710–5. [DOI] [PubMed] [Google Scholar]
- 21. Jain S, Self WH, Wunderink RG, et al. ; for the CDC EPIC Study Team. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med 2015; 373:415–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Storms AD, Chen J, Jackson LA, et al. . Rates and risk factors associated with hospitalization for pneumonia with ICU admission among adults. BMC Pulm Med 2017; 17:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Curns AT, Holman RC, Sejvar JJ, et al. . Infectious disease hospitalizations among older adults in the United States from 1990 through 2002. Arch Intern Med 2005; 165:2514–20. [DOI] [PubMed] [Google Scholar]
- 24. Centers for Disease Control and Prevention. Nursing Homes and Assisted Living (Long-Term Care Facilities [LTCFs]) https://www.cdc.gov/longtermcare/. Accessed January 18, 2019.
- 25. Walsh EE, Cox C, Falsey AR. Clinical features of influenza A virus infection in older hospitalized persons. J Am Geriatr Soc 2002; 50:1498–503. [DOI] [PubMed] [Google Scholar]
- 26. Falsey AR, Baran A, Walsh EE. Should clinical case definitions of influenza in hospitalized older adults include fever? Influenza Other Respir Viruses 2015; 9(Suppl 1):23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mandell LA, Wunderink RG, Anzueto A, et al. ; Infectious Diseases Society of America; American Thoracic Society Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44(Suppl 2):S27–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fiore AE, Fry A, Shay D, et al. ; Centers for Disease Control and Prevention Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011; 60:1–24. [PubMed] [Google Scholar]
- 29. Uyeki TM, Bernstein HH, Bradley JS, et al. . Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis 2019; 68:e1–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams WW, Lu PJ, O’Halloran A, et al. . Surveillance of vaccination coverage among adult populations - United States, 2015. MMWR Surveill Summ 2017; 66:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lindegren ML, Griffin MR, Williams JV, et al. . Antiviral treatment among older adults hospitalized with influenza, 2006–2012. PLOS ONE 2015; 10:e0121952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Garg S, Chaves SS, Perez A, et al. . Reduced influenza antiviral treatment among children and adults hospitalized with laboratory-confirmed influenza infection in the year after the 2009 pandemic. Clin Infect Dis 2012; 55:e18–21. [DOI] [PubMed] [Google Scholar]
- 33. Garg S, Jain S, Dawood FS, et al. . Pneumonia among adults hospitalized with laboratory-confirmed seasonal influenza virus infection-United States, 2005–2008. BMC Infect Dis 2015; 15:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Collins JP, Campbell AP, Openo K, et al. . Clinical features and outcomes of immunocompromised children hospitalized with laboratory-confirmed influenza in the United States, 2011–2015 [published online ahead of print October 25, 2018]. J Pediatric Infect Dis Soc ; doi:10.1093/jpids/piy101. [DOI] [PubMed] [Google Scholar]
- 35. Shrestha S, Foxman B, Berus J, et al. . The role of influenza in the epidemiology of pneumonia. Sci Rep 2015; 5:15314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shrestha S, Foxman B, Weinberger DM, et al. . Identifying the interaction between influenza and pneumococcal pneumonia using incidence data. Sci Transl Med 2013; 5:191ra84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tomczyk S, Bennett NM, Stoecker C, et al. ; Centers for Disease Control and Prevention Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2014; 63:822–5. [PMC free article] [PubMed] [Google Scholar]
- 38. Su S, Fry AM, Kirley PD, et al. . Survey of influenza and other respiratory viruses diagnostic testing in US hospitals, 2012-2013. Influenza Other Respir Viruses 2016; 10:86–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Andrew MK, Shinde V, Ye L, et al. ; Serious Outcomes Surveillance Network of the Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) and the Toronto Invasive Bacterial Diseases Network (TIBDN) The importance of frailty in the assessment of influenza vaccine effectiveness against influenza-related hospitalization in elderly people. J Infect Dis 2017; 216:405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jackson LA, Nelson JC, Benson P, et al. . Functional status is a confounder of the association of influenza vaccine and risk of all cause mortality in seniors. Int J Epidemiol 2006; 35:345–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.