To the Editor:
I read with interest the study by Roca and coworkers (1) on the ROX index, which combines the oxygen saturation as measured by pulse oximetry (SpO2)/FiO2 ratio and the respiratory rate, and predicts the outcome of nasal high-flow (NHF) therapy in patients with acute respiratory failure caused by pneumonia. The index is based on two well-known facts: sicker patients require more oxygen and have higher respiratory rates. The study demonstrated that a ROX index of ≥4.88 at 2, 6, or 12 hours determines the success of the therapy. The authors noted that “among components of the index, SpO2/FiO2 had a greater weight than respiratory rate.” This highlights the role of FiO2 requirements in the success of NHF therapy for unstable patients with respiratory failure.
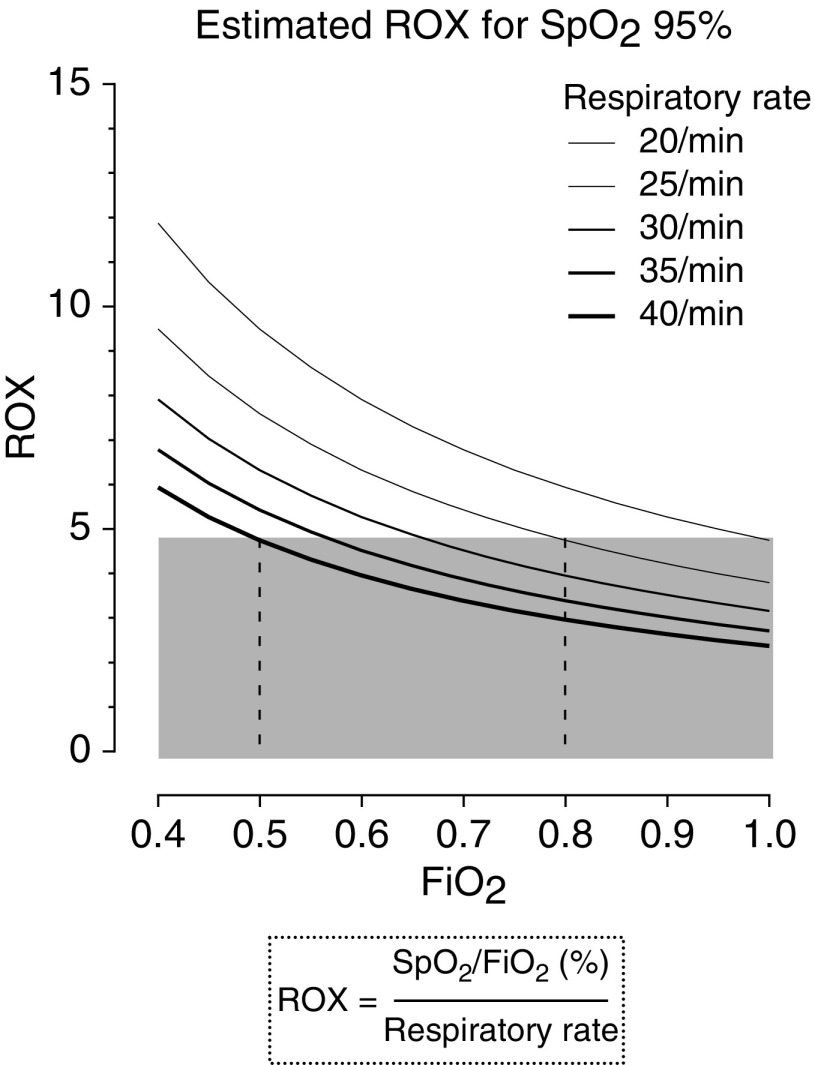
The figure of the calculated ROX index presented here may be complementary to the study (Figure 1) and may help to elucidate the index’s value and the relationship between FiO2 and respiratory rates.
Figure 1.
Relationship between FiO2 and the ROX index at SpO2 95% for a range of respiratory rates between 20 and 40 breaths/min. Respiratory rates are shown in the same order as in the key. The gray area indicates ROX < 4.88. FiO2 values of 0.5 and 0.8 are marked with dashed vertical lines. SpO2 = oxygen saturation as measured by pulse oximetry.
The ROX index was calculated for SpO2 of 95% and respiratory rates of 20–40 breaths/min using a range of FiO2 values from 0.4 to 1.0. The gray area indicates ROX values below a cutoff point of 4.88 (1).
Respiratory rates in oxygen-dependent patients are expected to be increased. The figure reveals that the ROX index is unlikely to drop below 4.88 with FiO2 values of up to 0.5, and it would be under the cutoff point with FiO2 values of 0.8 or higher for the anticipated range of respiratory rates. FiO2 values of 0.5 and 0.8 are marked with interrupted vertical lines. If SpO2 is under or above 95%, all of the presented curves of the calculated ROX will shift slightly downward or upward, respectively.
The index is very simple and has the potential to become a routine parameter in clinical practice when supplemental oxygen is used with NHF therapy. The presented figure may help to predict when a patient is expected to fail and could be considered for escalation of care.
Supplementary Material
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.201902-0376LE on March 21, 2019
Author disclosures are available with the text of this letter at www.atsjournals.org.
Reference
- 1.Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high flow therapy. Am J Respir Crit Care Med. doi: 10.1164/rccm.201803-0589OC. [online ahead of print] 21 Dec 2018; DOI: 10.1164/rccm.201803-0589OC. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.