Abstract
Purpose
To explore the attitudes of reproductive endocrinology and infertility (REI) and maternal–fetal medicine (MFM) subspecialists regarding the necessity and appropriateness of body mass index (BMI) cutoffs for women seeking fertility treatment.
Methods
Members of the Society for Reproductive Endocrinology and Infertility (SREI) and the Society for Maternal Fetal Medicine (SMFM) were invited to participate in a survey querying their knowledge of existing institutional or clinic BMI policies and personal opinions regarding upper and lower BMI cutoffs for a range of fertility treatments, including oral ovulation agents, gonadotropins, and in vitro fertilization.
Results
Respondents included 398 MFMs and 201 REIs. The majority of REI and MFM providers agreed with upper limit BMI cutoffs (72.5% vs 68.2%, p = 0.29), but REIs were twice as likely to support lower limit BMI restrictions compared to MFMs (56.2% vs 28.4%, p < 0.0001). Those who supported upper BMI restrictions were more likely to be female and report existing institutional BMI cutoffs. The majority of respondents (99.3%) believed that an official statement to guide clinicians should be issued by a national professional organization.
Conclusions
Although practice patterns widely vary, the majority of REIs and MFMs believe that there should be a BMI cutoff above which women should not be offered immediate fertility treatment. Furthermore, there is a reported need for a written statement by a national professional organization to guide clinical practice and to ensure that OB/GYN subspecialists are providing consistent, fair, and safe recommendations to infertile women at the extremes of BMI.
Keywords: Body mass index (BMI), Fertility treatment
Introduction
Obesity is now considered a global public health crisis and is correlated with a dramatic increase in chronic disease, associated health care costs, and mortality [1, 2]. The Centers for Disease Control estimate that over one-third of reproductive-age women were obese in the USA between 2011 and 2014 [3]. Body mass index (BMI), calculated as weight in kilograms divided by meters squared, is an internationally employed measure used to define obesity. In pregnancy, women who are overweight (preconception BMI ≥ 25.0 and < 29.9) or obese (preconception BMI ≥ 30.0) experience higher rates of pregnancy complications, including miscarriage, gestational diabetes, hypertensive disorders, preeclampsia, preterm delivery, congenital anomalies, labor complications, and Cesarean delivery [4–8]. Conversely, underweight women (preconception BMI ≤ 18.5) may be at increased risk for preterm birth [9].
Extremes of BMI have also been associated with decreased natural fecundity and increased rates of infertility. Possible etiologies in both under- and overweight women include oligo- or anovulation, changes in endometrial receptivity, and diminished oocyte quality or competence [10–13]. Infertility is considered a disease [14], and medically necessary treatments may include treatments ranging from oral ovulation induction agents to in vitro fertilization (IVF). However, when using assisted reproductive technologies (ART), overweight or obese women may demonstrate lower pregnancy rates, lower live birth rates, and higher miscarriage rates following IVF, intracytoplasmic sperm injection (ICSI), or frozen embryo thaw/transfer cycles [15–18]. Obesity has also been associated with increased odds of IVF cycle cancellation and reduction in number of oocytes retrieved [19, 20]. Meanwhile, underweight women who conceive using ART are at increased risk of miscarriage, preterm birth, and low birth weight [16, 21].
Acknowledging that patients with infertility often require medical treatment, while recognizing that the extremes of maternal BMI may decrease success rates of fertility interventions and increase maternal–fetal morbidity, many providers within the USA and internationally have established BMI cutoffs for fertility treatment [22–24]. However, individual practice patterns vary, cutoffs may be arbitrary, rather than evidence-based, and national or international standardized practice guidelines do not exist. Furthermore, the opinions of women’s health subspecialists, including fertility specialists and high-risk obstetricians, may be vastly different. The objective of our study was to gather information on existing BMI cutoffs in fertility practices, and to explore the opinions of both reproductive endocrinology and infertility (REI) and maternal–fetal medicine (MFM) physicians regarding the necessity and appropriateness of these restrictions. In addition, we sought to compare characteristics of respondents who agreed with, versus those who disagreed with, BMI cutoffs for offering fertility treatment.
Materials and methods
An anonymous survey was distributed to members of the Society for Reproductive Endocrinology and Infertility (SREI) and the Society of Maternal Fetal Medicine (SMFM). The survey included questions about respondent demographics, geographic location, knowledge of existing institutional or clinic BMI policies, and personal opinions on BMI cutoffs for fertility treatment. Participants were also invited to provide anonymous, free-text comments.
In univariate analyses, distributions of categorical variables were compared using a chi-squared test or Fisher’s exact test. Distributions of continuous variables were compared using a t test allowing for unequal variances. A logistic regression model was used to determine the associations between age, sex, race, geographic region, specialty, and degree, with a respondent’s training in weight loss counseling, existing clinic or departmental BMI cutoffs for fertility treatment, and personal opinions on BMI restrictions. Respondents who had missing data for any of these variables were excluded from this model. Statistical inference on the odds ratio was based on the Wald statistic, computed from the regression slope parameter and its standard error. A 95% confidence interval was computed using the approximate normal distribution for logistic regression parameter estimates. This study was deemed exempt by the University of Michigan Institutional Review Board (HUM00059601).
Results
Respondents included 398 MFM and 201 REI providers, representing a response rate of 23% by SMFM members and 20% by SREI members. Survey respondents had a mean age of 49.4 years, and the majority of respondents identified as non-Hispanic white (80.5%). Additional demographic information is provided in Table 1.
Table 1.
Characteristics of survey respondents
| Overall (N = 607) | Agree with upper BMI restrictions (N = 410) | Disagree with upper BMI restrictions (N = 183) | Maternal–fetal medicine (N = 398) | Reproductive endocrinology and infertility (N = 201) | p value* | ||
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | p value* | N (%) | N (%) | ||
| Age (years) | |||||||
| 30–35 | 62 (10.6) | 44 (11.2) | 18 (9.9) | 0.66 | 33 (8.4) | 27 (14.8) | 0.06 |
| 36–49 | 210 (35.8) | 143 (36.5) | 61 (33.7) | 146 (37.0) | 63 (34.4) | ||
| 50+ | 314 (53.6) | 205 (52.3) | 102 (56.4) | 216 (54.7) | 93 (50.8) | ||
| No response | 21 | 18 | 2 | 3 | 18 | ||
| Sex | |||||||
| Male | 318 (52.7) | 201 (49.3) | 110 (60.4) | 0.01 | 202 (51.0) | 112 (56.0) | 0.25 |
| Female | 286 (47.4) | 207 (50.7) | 72 (39.6) | 194 (49.0) | 88 (44.0) | ||
| No response | 3 | 2 | 1 | 2 | 1 | ||
| Race/ethnicity | |||||||
| Non-Hispanic white | 450 (80.5) | 304 (80.9) | 136 (79.5) | 0.34 | 292 (80.2) | 152 (80.4) | 0.05 |
| Non-Hispanic black | 27 (4.8) | 16 (4.3) | 11 (6.4) | 22 (6.0) | 5 (2.7) | ||
| Hispanic | 26 (4.7) | 19 (5.1) | 6 (3.5) | 14 (3.9) | 12 (6.4) | ||
| Asian | 51 (9.1) | 32 (8.5) | 18 (10.5) | 35 (9.6) | 16 (8.5) | ||
| Other | 5 (0.9) | 5 (1.3) | 0 (0) | 1 (0.3) | 4 (2.1) | ||
| No response | 48 | 34 | 12 | 34 | 12 | ||
| Region | |||||||
| USA, Northeast | 162 (27.7) | 115 (29.1) | 46 (25.7) | 0.67 | 111 (28.4) | 49 (26.3) | <0.001 |
| USA, Southeast | 119 (20.3) | 78 (19.8) | 36 (20.1) | 68 (17.4) | 50 (26.9) | ||
| USA, Midwest | 131 (22.4) | 89 (22.5) | 39 (21.8) | 93 (23.8) | 33 (17.7) | ||
| USA, Southwest | 41 (7.0) | 30 (7.6) | 11 (6.2) | 31 (7.9) | 10 (5.4) | ||
| USA, West | 116 (19.8) | 72 (18.2) | 43 (24.0) | 87 (22.3) | 29 (15.6) | ||
| USA, no region specified | 7 (1.2) | 6 (1.5) | 1 (0.6) | 0 (0) | 7 (3.8) | ||
| Outside USA | 9 (1.5) | 5 (1.3) | 3 (1.7) | 1 (0.3) | 8 (4.3) | ||
| No response | 22 | 15 | 4 | 7 | 15 | ||
| Training in weight loss counseling | |||||||
| Yes, I have received formal training | 109 (18.5) | 79 (19.7) | 30 (16.6) | 0.17 | 69 (17.7) | 39 (20.4) | 0.40 |
| No, but I have acquired the knowledge elsewhere | 371 (62.9) | 257 (63.9) | 110 (60.8) | 244 (62.4) | 122 (63.9) | ||
| No, I could not provide adequate counseling | 110 (18.6) | 66 (16.4) | 41 (22.7) | 78 (20.0) | 30 (15.7) | ||
| No response | 17 | 8 | 2 | 7 | 10 | ||
Abbreviations: body mass index (BMI)
*p values were computed using a chi-square test or Fisher’s exact test (when > 20% of cells had expected counts < 5 and at least one cell had expected count < 1) for categorical comparisons and t test allowing for unequal variances for comparisons of means
Among all respondents, 23.9% practiced in a clinic or department with reported BMI restrictions for specific fertility treatments, while 33.8% were unaware if such restrictions existed (Table 2). For those practices or departments with existing BMI guidelines, the mean upper limit reported for offering IVF was a BMI of 40.8 kg/m2 (SD 5.0). For treatments other than IVF, including injectable or oral superovulation or ovulation induction medications, the mean upper limit reported was a BMI of 42.1 kg/m2 (SD 6.3) (Table 2).
Table 2.
Reported upper BMI restrictions for fertility treatment
| Overall (N = 607) | Agree with upper BMI cutoff (N = 410) | Disagree with upper BMI cutoff (N = 183) | Maternal–fetal medicine (N = 398) | Reproductive endocrinology and infertility (N = 201) | p value* | ||
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | p value* | N (%) | N (%) | ||
| Does your department have a BMI cutoff for fertility treatment? | |||||||
| Yes | 73 (14.0) | 69 (19.4) | 4 (2.5) | < 0.001 | 18 (24.7) | 55 (28.1) | < 0.001 |
| Yes, for some treatment | 52 (9.9) | 39 (11.0) | 13 (8.0) | 2 (0.6) | 50 (25.5) | ||
| No | 221 (42.3) | 131 (36.9) | 87 (53.4) | 132 (41.1) | 87 (44.4) | ||
| Do not know | 177 (33.8) | 116 (32.7) | 59 (36.2) | 169 (52.7) | 4 (2.0) | ||
| Not applicable | 75 (12.5) | 54 (13.2) | 18 (9.9) | 72 (18.3) | 0 (0) | ||
| No response | 9 | 1 | 2 | 5 | 5 | ||
| What is your BMI cutoff for IVF? | |||||||
| Mean (SD) | 40.8 (5.0) | 40.8 (4.8) | 40.9 (6.3) | 0.98 | 41.1 (6.5) | 40.8 (4.8) | 0.84 |
| 30–34 | 5 (4.5) | 5 (5.2) | 0 (0) | 0.19 | 1 (6.3) | 4 (4.2) | 0.98 |
| 35–39 | 16 (14.3) | 11 (11.3) | 5 (33.3) | 2 (12.5) | 14 (14.6) | ||
| 40–44 | 69 (61.6) | 61 (62.9) | 8 (53.3) | 10 (62.5) | 59 (61.5) | ||
| 45–49 | 9 (8.0) | 9 (9.3) | 0 (0) | 1 (6.3) | 8 (8.3) | ||
| 50+ | 13 (11.6) | 11 (11.3) | 2 (13.3) | 2 (12.5) | 11 (11.5) | ||
| No response | 13 | 11 | 2 | 4 | 9 | ||
| What is your BMI cutoff for non-IVF fertility treatment? | |||||||
| Mean (SD) | 42.1 (6.3) | 41.9 (5.9) | 45.0 (13.2) | 0.73 | 40.9 (6.9) | 42.5 (6.1) | 0.47 |
| 30–34 | 3 (5.2) | 3 (5.5) | 0 (0) | 0.67 | 1 (7.1) | 2 (4.6) | 0.40 |
| 35–39 | 9 (15.5) | 8 (14.6) | 1 (33.3) | 2 (14.3) | 7 (15.9) | ||
| 40–44 | 27 (46.6) | 26 (47.3) | 1 (33.3) | 9 (64.3) | 18 (40.9) | ||
| 45–49 | 7 (12.1) | 7 (12.7) | 0 (0) | 0 (0) | 7 (15.9) | ||
| 50+ | 12 (20.7) | 11 (20.0) | 1 (33.3) | 2 (14.3) | 10 (22.7) | ||
| No response | 67 | 53 | 14 | 6 | 61 | ||
BMI body mass index, IVF in vitro fertilization
*p values were computed using a chi-square test or Fisher’s exact test (when > 20% of cells had expected counts < 5 and at least one cell had expected count < 1) for categorical comparisons and t test allowing for unequal variances for comparisons of means
Among REI providers, 72.5% believed that there should be a BMI above which patients should not be offered fertility treatment. Similarly, 68.2% of MFM specialists agreed with this statement (Table 3). When broken down by specific fertility treatment, REIs were less likely than MFMs to support upper BMI restrictions for injectable and oral medications; however, the vast majority of REIs and MFMs agreed that there should be an upper limit BMI cutoff for women pursuing IVF (Table 3).
Table 3.
Opinions on upper BMI restrictions for fertility treatment
| Overall | Maternal–fetal medicine | Reproductive endocrinology and infertility | p value* | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| There should be a BMI above which patients should not be offered fertility treatment. | 410/593 (69.1) |
266/390 (68.2) |
142/196 (72.5) |
0.29 |
| There should be an upper limit BMI cutoff for IVF. |
402/410 (98.0) |
261/266 (98.1) |
138/142 (97.2) |
0.74 |
| If yes, what is your proposed BMI cutoff? | ||||
| Mean (SD) | 40.1 (5.7) | 40.1 (6.1) | 40.0 (4.8) | 0.77 |
| 25–29 | 3 (0.8) | 2 (0.8) | 1 (0.8) | 0.17 |
| 30–34 | 32 (8.3) | 25 (9.9) | 7 (5.2) | |
| 35–39 | 84 (21.7) | 50 (19.8) | 33 (24.6) | |
| 40–44 | 184 (47.4) | 119 (47.2) | 65 (48.5) | |
| 45–49 | 38 (9.8) | 21 (8.3) | 17 (12.7) | |
| 50+ | 47 (12.1) | 35 (13.9) | 11 (8.2) | |
| No response | 16 | 11 | 5 | |
| There should be an upper limit BMI cutoff for injectable medications. | 368/410 (89.8) |
252/266 (94.7) |
113/142 (79.6) |
< 0.001 |
| If yes, what is your proposed BMI cutoff? | ||||
| Mean (SD) | 40.2 (5.9) | 40.1 (6.1) | 40.5 (5.5) | 0.54 |
| 25–29 | 3 (0.8) | 2 (0.8) | 1 (0.9) | 0.51 |
| 30–34 | 31 (8.7) | 24 (9.8) | 7 (6.3) | |
| 35–39 | 77 (21.6) | 49 (20.1) | 27 (24.3) | |
| 40–44 | 162 (45.4) | 116 (47.5) | 46 (41.4) | |
| 45–49 | 33 (9.2) | 19 (7.8) | 14 (12.6) | |
| 50+ | 51 (14.3) | 34 (13.9) | 16 (14.4) | |
| No response | 14 | 10 | 4 | |
| There should be an upper limit BMI cutoff for oral medications. | 327/410 (79.8) |
233/266 (87.6) |
91/142 (64.1) |
< 0.001 |
| If yes, what is your proposed BMI cutoff? | ||||
| Mean (SD) | 40.0 (6.0) | 40.1 (6.2) | 40.0 (5.6) | 0.85 |
| 25–29 | 3 (1.0) | 2 (0.9) | 1 (1.2) | 0.95 |
| 30–34 | 30 (9.5) | 23 (10.1) | 7 (8.1) | |
| 35–39 | 70 (22.2) | 47 (20.7) | 22 (25.6) | |
| 40–44 | 142 (45.1) | 105 (46.3) | 37 (43.0) | |
| 45–49 | 24 (7.6) | 17 (7.5) | 7 (8.1) | |
| 50+ | 46 (14.6) | 33 (14.5) | 12 (14.0) | |
| No response | 15 | 9 | 6 | |
| Which organization should establish BMI cutoffs for fertility treatment, if an official statement were to be issued? | ||||
| American Society for Reproductive Medicine | 337 (82.2) | 216 (81.2) | 121 (85.2) | 0.31 |
| Society for Maternal-Fetal Medicine | 178 (43.4) | 128 (48.1) | 49 (34.5) | 0.008 |
| American College of Obstetricians and Gynecologists | 239 (58.3) | 164 (61.7) | 73 (51.4) | 0.046 |
| Other | 5 (1.2) | 0 (0) | 5 (3.5) | 0.005 |
| No statement should be made | 3 (0.7) | 0 (0) | 3 (2.1) | 0.04 |
*p values were computed using a chi-square test or Fisher’s exact test (when > 20% of cells had expected counts < 5 and at least one cell had expected count < 1) for categorical comparisons and t test allowing for unequal variances for comparisons of means
Among all respondents, 41.9% believed that delaying immediate fertility treatment in women above certain BMI cutoffs would stigmatize overweight or obese patients, and 42.3% expressed concern that BMI restrictions would prevent timely treatment in women of advanced reproductive age. These views were more frequently shared by providers who disagreed with upper BMI cutoffs, versus those who supported them (Fig. 1). REI physicians more frequently believed that older infertile women who are overweight or obese should be offered immediate fertility treatment, so as not to compromise an abbreviated reproductive timeline (Fig. 1). The majority of respondents (81.5% of MFMs and 70.5% of REIs) recommended preconception MFM consultation for overweight or obese women, and agreed that morbidly obese infertile women should be offered consultation for bariatric surgery prior to attempting pregnancy (86.4% of MFMs and 80.5% of REIs) (Fig. 1). Most respondents (99.3%) also agreed that infertility providers should recommend weight loss to their overweight and obese patients seeking conception. Although 63.9% of REI providers reported knowledge and experience in weight loss counseling, only 20.4% reported receiving formal training in this regard.
Fig. 1.
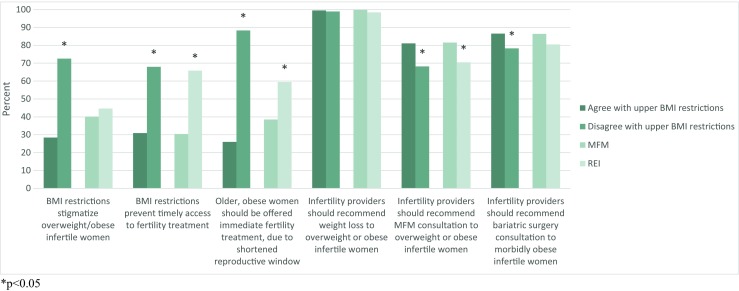
Opinions on upper BMI restrictions for fertility treatment. *p < 0.05
In logistic regression, providers who agreed with upper BMI limits were more likely to be female, work in a department with existing BMI restrictions, recommend preconception MFM consultation for overweight or obese women, and disagree with the sentiments that weight restrictions stigmatize patients and prevent timely access to fertility care (Table 4).
Table 4.
Characteristics associated with support of upper BMI restrictions (N = 426 respondents)
| Odds ratio (95% CI)* | |
|---|---|
| Female sex | 2.32 (1.16–4.66) |
| Existing departmental BMI restrictions | |
| Yes | 5.37 (2.18–13.3) |
| No | 1.00 (reference) |
| Do not know | 0.95 (0.42–2.14) |
| Opinions | |
| Weight restrictions on fertility treatment do not stigmatize overweight and obese women. | 3.10 (1.58–6.08) |
| I am not concerned that BMI restrictions would limit timely access to fertility treatment. | 2.53 (1.17–5.49) |
| Older overweight and obese women should not be allowed fertility treatment, even if they lose the “reproductive window.” | 31.5 (14.4–69.0) |
| Providers should recommend preconception MFM consultation to infertile women who are overweight or obese. | 2.99 (1.39–6.43) |
BMI body mass index, MFM maternal–fetal medicine
*Logistic regression model included age, sex, race, region, specialty (MGM, REI, other), degree (MPH, PhD, MS, MBA, other), training in weight loss counseling, existing departmental BMI restrictions, and opinions on BMI restrictions
At the opposite BMI extreme, only 37.6% of respondents agreed that there should be a BMI below which patients should not be offered fertility treatment (Table 5). Of these respondents, lower BMI limits were supported for women undergoing IVF (95.4%), injectable medications (94.1%), and oral agents (88.1%). The mean proposed lower limit for all treatments was BMI of 17.3 (SD 1.6). Approximately twice as many REI specialists supported lower BMI restrictions compared to MFM providers (56.2% vs 28.4%, p < 0.0001).
Table 5.
Opinions on lower BMI restrictions for fertility treatment
| Overall | Maternal–fetal medicine | Reproductive endocrinology and infertility | p value* | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| There should be a BMI below which patients should not be offered fertility treatment. | 219/583 (37.6) |
108/381 (28.4) |
109/194 (56.2) |
< 0.0001 |
| There should be a lower limit BMI cutoff for IVF. | 209/219 (95.4) |
104/108 (96.3) |
103/109 (94.5) |
0.75 |
| If yes, what is your proposed cutoff? | ||||
| Mean (SD) | 17.3 (1.6) | 17.4 (1.8) | 17.3 (1.4) | 0.47 |
| 12–15 | 28 (14.1) | 19 (19.6) | 9 (8.8) | < 0.001 |
| 16–17 | 66 (32.8) | 20 (20.6) | 46 (45.1) | |
| 18–22 | 104 (52.5) | 58 (59.8) | 47 (46.1) | |
| No response | 11 | 7 | 4 | |
| There should be a lower limit BMI cutoff for injectable medications. | 206/219 (94.1) |
104/108 (96.3) |
99/109 (90.8) |
0.17 |
| If yes, what is your proposed cutoff? | ||||
| Mean (SD) | 17.3 (1.6) | 17.5 (1.8) | 17.2 (1.4) | 0.35 |
| 12–15 | 28 (14.3) | 18 (18.6) | 8 (8.0) | < 0.001 |
| 16–17 | 64 (32.7) | 20 (20.6) | 44 (45.4) | |
| 18–22 | 104 (53.1) | 59 (60.8) | 43 (45.4) | |
| No response | 10 | 7 | 4 | |
| There should be a lower limit BMI cutoff for oral medications. | 193/219 (88.1) | 97/108 (89.8) | 93/109 (85.3) | 0.32 |
| If yes, what is your proposed cutoff? | ||||
| Mean (SD) | 17.3 (1.6) | 17.4 (1.8) | 17.2 (1.4) | 0.55 |
| 12–15 | 26 (14.1) | 18 (19.8) | 6 (6.7) | < 0.001 |
| 16–17 | 64 (34.8) | 20 (22.0) | 44 (49.4) | |
| 18–22 | 94 (51.1) | 53 (58.2) | 39 (43.8) | |
| No response | 9 | 6 | 4 |
*p values were computed using a chi-square test or Fisher’s exact test (when > 20% of cells had expected counts < 5 and at least one cell had expected count < 1) for categorical comparisons and t test allowing for unequal variances for comparisons of means
The vast majority of respondents (99.3%) believed that an official statement or guideline on BMI cutoffs should be issued by a national professional organization. The American Society for Reproductive Medicine (ASRM), the American College of Obstetrics and Gynecology (ACOG), and the Society for Maternal Fetal Medicine (SMFM) were supported by respondents to be the most appropriate organizations to do so (82.2%, 58.3%, and 43.4%, respectively).
Discussion
In our national survey of REI and MFM providers, our findings demonstrate that there is a wide difference of opinion as to whether fertility treatments should be offered to infertile women at the extremes of BMI. While the majority of REI and MFM respondents agree with upper BMI cutoffs for initiation of fertility treatment, particularly IVF, only 24% of respondents reported existing BMI policies within their clinic or department. Our findings also demonstrate a need for a data-driven, formal statement on BMI guidelines issued by a professional OB/GYN organization such as ASRM, ACOG, or SMFM, due to the vast variation in practice patterns. Furthermore, despite an overwhelming consensus that patients should be counseled on weight loss, only a minority of respondents reported ever receiving formal training in this regard.
Our results are consistent with results from similar survey studies. In a survey of Canadian IVF directors, the median upper BMI limit for allowing IVF was 38 (interquartile range 35 to 40) [22]. Meanwhile, in the USA, a survey of IVF clinics in the Society for Assisted Reproductive Technology database demonstrated that the upper BMI cutoffs for fertility treatments range from 35 to 50 [23]. In that survey, reasons cited for having BMI restrictions in place for obese women included anesthesia safety concerns during oocyte retrieval, concern for lower IVF success rates, adverse pregnancy outcomes, and technical difficulties with speculum and ultrasound visualization during treatment monitoring [23]. Unlike these prior studies, our survey was distributed to both REI and MFM providers, two subspecialty groups who may be involved in the preconception care of overweight or obese women. Furthermore, our survey also inquired about respondents’ views on underweight women, and fertility interventions other than IVF, including oral or injectable ovulation agents.
The argument in support of BMI restrictions
In our analyses, we explored the opinions of those who supported, versus those who did not support, BMI restrictions in the setting of fertility treatment. In general, those who supported upper limit BMI cutoffs were less likely to believe that BMI restrictions stigmatized, or delayed access to fertility care, for obese women. Respondents who supported BMI restrictions were also more likely to be female, and less likely to believe that obese, older women should be offered immediate fertility treatment due to a shortened reproductive timeline. By inviting respondents to include free-text comments, the following sentiments were anonymously shared:
“It is fairly well established that obesity is associated with decreased pregnancy rates and is a major contributor to pregnancy complications... I believe that national guidelines set by the ASRM for BMI, similar to that for [number] of embryos to transfer at IVF, will support physicians in impressing upon patients the importance of losing weight before initiating active fertility treatment. I also believe that REIs require more training in metabolism, and fertility programs need to offer appropriate referrals for genuine weight loss management to match the needs of these patients.”
“Infertility treatment is an elective service. Although informed consent and patient autonomy are hallmarks of proper patient care, provision of an elective treatment to women at the extremes of BMI greatly increases potential harm to both the patient and the future offspring that may be conceived.”
“The only specialty that has a chance to have an impact on the obesity epidemic is OB-GYN. Pre-pregnancy weight, weight gain during pregnancy, and gestational diabetes all contribute to obesity in their offspring and probably have epigenetic consequences for generations to come.”
The argument against BMI restrictions
In our analyses, respondents who disagreed with upper BMI cutoffs were more likely to believe that these restrictions would stigmatize and delay access to care for obese women. They were also more likely to believe that older, obese women should receive immediate fertility treatment. The following written comments were anonymously provided by survey respondents who disagreed with BMI restrictions:
“It does not make sense to impose limits based on BMI, when there are no mandatory policies on [elective single embryo transfer], age, or other medical illnesses that are known to be associated with increased perinatal or neonatal morbidity.”
“It is patently paternalistic to suggest that women should not be able to control their own reproductive choices. Give good counseling about the risks, support weight loss in the overall plan, and let patients be adults and make informed choices.”
“It is discriminatory to penalize obese women by refusing treatment.”
“In general, we strongly advise weight loss before treatment. However, we have never been able to establish an evidence-based [BMI] cut-off. I favor individualized decisions rather than strict guidelines.”
The withholding of fertility treatment from certain medical populations, such as those with HIV, cancer, or other potentially life-threatening diseases, has been deemed inappropriate and unethical [25]. However, guidelines do not exist about the ethical implications of withholding immediate fertility treatment from patients at the extremes of BMI. Obese patients may experience bias and stigma from their health care providers at baseline, which may lead to avoidance of seeking care, mistrust in the patient–provider relationship, and poorer quality of life [26]. Importantly, the prevalence of obesity varies by race and economic status, with higher obesity rates in non-Hispanic whites, non-Hispanic blacks, Hispanics, and those of lower socioeconomic status [6, 27]. BMI restrictions in the setting of fertility treatment may indirectly discriminate against specific socioeconomic or racial populations. There is already evidence to suggest that minority populations seek fertility care less often [28, 29] and BMI may be a contributing factor to these disparities in access to care. Indeed, the issue of withholding fertility treatment due to patient BMI is a controversial one, particularly in light of a recent randomized controlled trial which found that delaying fertility interventions to allow for lifestyle interventions, compared to immediate fertility treatment, did not result in higher live birth rates of healthy singleton pregnancies [30].
The strengths of our study include a nationally representative sample of fertility specialists and high-risk obstetricians. Because both groups of these subspecialists have the opportunity to provide care for women during the preconception and prenatal periods, involving both REI and MFM specialists is a unique aspect of our survey study. For this same reason, not including general obstetrician/gynecologists is a limitation. Clinical practice type was also not assessed in the survey, and the particular distribution of clinicians practicing in academic, community-based, and private settings may have impacted our results. Another limitation is that a validated survey was not used in our study. However, to our knowledge, ours is the first study to explore the opinions and practice patterns of subspecialty OB/GYNs on a national level.
In conclusion, practice patterns are inconsistent among OB/GYN subspecialists in regard to BMI restrictions and fertility treatments. Differences in opinion between REI and MFM providers suggest different priorities and experiences in patient care. Importantly, there is a need for written consensus guidelines by women’s health leaders. Fertility specialists and high-risk obstetricians should work together to provide consistent, reasonable, and fair patient recommendations to balance the tenets of patient autonomy with primum non nocere.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. Centers for Disease Control and Prevention (CDC). CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005-2013. MMWR Suppl. 2014;63:3–27. [PubMed] [Google Scholar]
- 2.Kent S, Fusco F, Gray A, Jebb SA, Cairns BJ, Mihaylova B. Body mass index and healthcare costs: a systematic literature review of individual participant data studies. Obes Rev. 2017;18:869–879. doi: 10.1111/obr.12560. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;1–8. [PubMed]
- 4.Persson M, Cnattingius S, Villamor E, Söderling J, Pasternak B, Stephansson O, et al. Risk of major congenital malformations in relation to maternal overweight and obesity severity: cohort study of 1.2 million singletons. BMJ. 2017;357:j2563. doi: 10.1136/bmj.j2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torloni MR, Betrán AP, Daher S, Widmer M, Dolan SM, Menon R, Bergel E, Allen T, Merialdi M. Maternal BMI and preterm birth: a systematic review of the literature with meta-analysis. J Matern Fetal Neonatal Med. 2009;22:957–970. doi: 10.3109/14767050903042561. [DOI] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists ACOG Committee opinion no. 549: obesity in pregnancy. Obstet Gynecol. 2013;121:213–217. doi: 10.1097/01.AOG.0000425667.10377.60. [DOI] [PubMed] [Google Scholar]
- 7.Scott-Pillai R, Spence D, Cardwell CR, Hunter A, Holmes VA. The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004-2011. BJOG. 2013;120:932–939. doi: 10.1111/1471-0528.12193. [DOI] [PubMed] [Google Scholar]
- 8.Joy S, Istwan N, Rhea D, Desch C, Stanziano G. The impact of maternal obesity on the incidence of adverse pregnancy outcomes in high-risk term pregnancies. Am J Perinatol. 2009;26:345–349. doi: 10.1055/s-0028-1110084. [DOI] [PubMed] [Google Scholar]
- 9.Lynch AM, Hart JE, Agwu OC, Fisher BM, West NA, Gibbs RS. Association of extremes of prepregnancy BMI with the clinical presentations of preterm birth. Am J Obstet Gynecol. 2014;210:428.e1–428.e9. doi: 10.1016/j.ajog.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Mahutte N, Kamga-Ngande C, Sharma A, Sylvestre C. Obesity and reproduction. J Obstet Gynaecol Can. 2018;40:950–966. doi: 10.1016/j.jogc.2018.04.030. [DOI] [PubMed] [Google Scholar]
- 11.Brewer CJ, Balen AH. The adverse effects of obesity on conception and implantation. Reproduction. 2010;140:347–364. doi: 10.1530/REP-09-0568. [DOI] [PubMed] [Google Scholar]
- 12.Kominiarek MA, Jungheim ES, Hoeger KM, Rogers AM, Kahan S, Kim JJ. American Society for Metabolic and Bariatric Surgery position statement on the impact of obesity and obesity treatment on fertility and fertility therapy endorsed by the American College of Obstetricians and Gynecologists and the Obesity Society. Surg Obes Relat Dis. 2017;13:750–757. doi: 10.1016/j.soard.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Davies MJ. Evidence for effects of weight on reproduction in women. Reprod BioMed Online. 2006;12:552–561. doi: 10.1016/S1472-6483(10)61180-7. [DOI] [PubMed] [Google Scholar]
- 14.Practice Committee of the American Society for Reproductive Medicine Definitions of infertility and recurrent pregnancy loss. Fertil Steril. 2008;89:1603. doi: 10.1016/j.fertnstert.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Provost MP, Acharya KS, Acharya CR, Yeh JS, Steward RG, Eaton JL, Goldfarb JM, Muasher SJ. Pregnancy outcomes decline with increasing body mass index: analysis of 239,127 fresh autologous in vitro fertilization cycles from the 2008-2010 Society for Assisted Reproductive Technology registry. Fertil Steril. 2016;105:663–669. doi: 10.1016/j.fertnstert.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Kawwass JF, Kulkarni AD, Hipp HS, Crawford S, Kissin DM, Jamieson DJ. Extremities of body mass index and their association with pregnancy outcomes in women undergoing in vitro fertilization in the United States. Fertil Steril. 2016;106:1742–1750. doi: 10.1016/j.fertnstert.2016.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rittenberg V, Seshadri S, Sunkara SK, Sobaleva S, Oteng-Ntim E, El-Toukhy T. Effect of body mass index on IVF treatment outcome: an updated systematic review and meta-analysis. Reprod BioMed Online. 2011;23:421–439. doi: 10.1016/j.rbmo.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Sarais V, Pagliardini L, Rebonato G, Papaleo E, Candiani M, Viganò P. A comprehensive analysis of body mass index effect on in vitro fertilization outcomes. Nutrients. 2016;8:109. doi: 10.3390/nu8030109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacKenna A, Schwarze JE, Crosby JA, Zegers-Hochschild F. Outcome of assisted reproductive technology in overweight and obese women. JBRA Assist Reprod. 2017;21:79–83. doi: 10.5935/1518-0557.20170020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luke B, Brown MB, Missmer SA, Bukulmez O, Leach R, Stern JE, Society for Assisted Reproductive Technology writing group The effect of increasing obesity on the response to and outcome of assisted reproductive technology: a national study. Fertil Steril. 2011;96:820–825. doi: 10.1016/j.fertnstert.2011.07.1100. [DOI] [PubMed] [Google Scholar]
- 21.Veleva Z, Tiitinen A, Vilska S, Hydén-Granskog C, Tomás C, Martikainen H, et al. High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod. 2008;23:878–884. doi: 10.1093/humrep/den017. [DOI] [PubMed] [Google Scholar]
- 22.Dayan N, Spitzer K, Laskin CA. A focus on maternal health before assisted reproduction: results from a pilot survey of Canadian IVF medical directors. J Obstet Gynaecol Can. 2015;37:648–655. doi: 10.1016/S1701-2163(15)30204-8. [DOI] [PubMed] [Google Scholar]
- 23.Kaye L, Sueldo C, Engmann L, Nulsen J, Benadiva C. Survey assessing obesity policies for assisted reproductive technology in the United States. Fertil Steril. 2016;105:703–706.e2. doi: 10.1016/j.fertnstert.2015.11.035. [DOI] [PubMed] [Google Scholar]
- 24.Zachariah M, Fleming R, Acharya U. Management of obese women in assisted conception units: a UK survey. Hum Fertil. 2006;9:101–105. doi: 10.1080/14647270500475214. [DOI] [PubMed] [Google Scholar]
- 25.Practice Committee of American Society for Reproductive Medicine Recommendations for reducing the risk of viral transmission during fertility treatment with the use of autologous gametes: a committee opinion. Fertil Steril. 2013;99:340–346. doi: 10.1016/j.fertnstert.2012.08.028. [DOI] [PubMed] [Google Scholar]
- 26.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–326. doi: 10.1111/obr.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7:130–138. doi: 10.1007/s13679-018-0301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ethics Committee of the American Society for Reproductive Medicine Disparities in access to effective treatment for infertility in the United States: an Ethics Committee opinion. Fertil Steril. 2015;104:1104–1110. doi: 10.1016/j.fertnstert.2015.07.1139. [DOI] [PubMed] [Google Scholar]
- 29.Quinn M, Fujimoto V. Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril. 2016;105:1119–1123. doi: 10.1016/j.fertnstert.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Mutsaerts MAQ, van Oers AM, Groen H, Burggraaff JM, Kuchenbecker WKH, Perquin DAM, Koks CAM, van Golde R, Kaaijk EM, Schierbeek JM, Oosterhuis GJE, Broekmans FJ, Bemelmans WJE, Lambalk CB, Verberg MFG, van der Veen F, Klijn NF, Mercelina PEAM, van Kasteren YM, Nap AW, Brinkhuis EA, Vogel NEA, Mulder RJAB, Gondrie ETCM, de Bruin JP, Sikkema JM, de Greef MHG, ter Bogt NCW, Land JA, Mol BWJ, Hoek A. Randomized trial of a lifestyle program in obese infertile women. N Engl J Med. 2016;374:1942–1953. doi: 10.1056/NEJMoa1505297. [DOI] [PubMed] [Google Scholar]


