Abstract
Purpose
To investigate the relationship between serum/follicular fluid fetuin-B levels and fertilization outcomes in conventional IVF cycles.
Methods
A prospective cohort study of conventional IVF treatments including 78 cycles with low fertilization rates (two pronuclei [2PN] rate < 30%; LF group) and 104 cycles performed during the same period with 2PN rate > 70% (high fertilization group, HF). To calculate the required sample size, a two-sample t test power analysis was applied to data from our pilot study, using PASS 11.0 software. Fetuin-B was measured using a commercial sandwich enzyme-linked immunosorbent assay.
Results
Serum fetuin-B and follicular fluid fetuin-B were positively correlated (r = 0.703, P < 0.001). Compared to the HF group, the LF group had significantly lower levels of fetuin-B, both in serum (5.81 ± 1.53 vs. 7.19 ± 1.42, P < 0.001) and follicular fluid (5.06 ± 1.29 vs. 6.16 ± 1.52, P < 0.001). The serum fetuin-B level from cycles with polypronuclear (PPN) zygotes was significantly lower when compared to cycles without PPN zygotes (6.82 ± 1.65 vs. 6.10 ± 1.43, P = 0.006). However, serum fetuin-B level was not correlated with preimplantation embryo development or clinical pregnancy.
Conclusion
Serum fetuin-B level is correlated with fertilization rate in conventional IVF and it may be used as a predictive marker of fertilization in IVF treatment.
Keywords: Fetuin-B, Fertilization rate, Follicular fluid, Conventional IVF
Introduction
Currently, IVF fertilization rates approach 70–80% [1] owing to the improvements in ovarian stimulation, culture media, and laboratory facilities. However, total fertilization failure or very low fertilization still occurs in 5–10% of in vitro fertilization (IVF) cycles [2]. Fertilization failure is an extremely stressful experience for couples undergoing IVF cycles, as well as for embryologists. To avoid fertilization failure, unnecessarily intracytoplasmic sperm injection (ICSI) treatments have been carried out, which may be associated with increased genetic (especially epigenetic) risks in offspring [3, 4].
Although sperm abnormalities may cause fertilization failure, inherent qualities of the oocytes are also crucial for successful fertilization [1]. Before successful fertilization, spermatozoa need to bind and penetrate the zona pellucida (ZP), a glycoprotein matrix surrounding the mammalian oocyte. The human ZP contains four zona proteins (ZP1–ZP4), and ZP2 is particularly important in gamete recognition and binding [5]. Upon fertilization, cortical granules are released from the mammalian oocytes, triggering structural changes in the ZP that lead to ZP hardening (ZPH) and blockade of further sperm entry [6]. A previous study showed that ZPH is mediated by the metalloprotease ovastacin, which is released from cortical granules of the oocyte and cleaves ZP2 to the fragmented ZP2f, leading to ZPH [7]. However, small amounts of cortical granules are also released prior to fertilization during oocyte meiotic maturation [8, 9]. Premature ZPH usually occurs during oocyte in vitro maturation (IVM) leading to a decreased fertilization rate [9, 10]. In vivo, fetuin-B, a liver-derived plasma protein present in follicular fluid, prevents premature ZPH by inhibiting ovastacin, thus keeping the oocyte fertilizable [6, 11].
Fetuin-B is a member of the cystatin superfamily of protease inhibitors [12]. It has diverse pathophysiological functions relating to nonalcoholic fatty liver disease, diabetes [13], acute myocardial infarction [14], and coronary artery disease [15]. It has been shown that female Fetub−/−mice are completely and permanently infertile [11], and downregulation of serum fetuin-B by antisense oligonucleotides leads to transient infertility in female mice [16]. As the fetuin-B gene is well-conserved between mammals, with 61% sequence homology in mice, rats, and humans [17], fetuin-B may also play an important role in human fertilization. High fetuin-B levels in serum and follicular fluid have been associated with fertilization success in IVF [18]. However, this finding was from a pilot study with a small sample size.
In this study, we aimed to further explore the relationship between fetuin-B levels and fertilization rates in IVF cycles. The associations of fetuin-B levels with oocyte maturation, embryo development, clinical pregnancy, and live birth were also investigated.
Materials and methods
Study subjects
This was a prospective cohort study on low fertilization cycles of conventional IVF treatments in the Women’s Hospital, Zhejiang University School of Medicine, between June 2016 and October 2017. The study was approved by the Medical Ethics Committee of the Women’s Hospital, Zhejiang University School of Medicine, and informed consent was obtained from all participants. Seventy-eight IVF cycles with low fertilization rates (two pronuclei [2PN] rate < 30%) were included in the study (LF group) and 104 IVF cycles performed during the same period with 2PN rate > 70% (high fertilization group, HF) were recruited as controls. All of the 182 couples were treated with conventional insemination.
The exclusion criteria were male factor infertility, unexplained infertility, patients with genetic disorders, female age > 38, poor ovarian reserves (follicle-stimulating hormone level > 12 mIU/mL or antral follicle count < 5), and poor ovarian response (< 3 oocytes retrieved).
ART program
Ovarian stimulation was performed using a standard regimen as we have described previously [19]. Oocytes were transvaginally retrieved under ultrasound guidance 36 h after triggering ovulation. Retrieved oocyte-cumulus complexes (COCs) were cultured in a supplemented G-IVF medium (Vitrolife, Sweden) at 37 °C in an incubator with 6% CO2. Semen samples were collected by masturbation after 3 to 7 days of sexual abstinence. After the liquefaction of semen at room temperature, semen analysis was performed according to World Health Organization (WHO) guidelines [20]. The semen samples of the patients were treated with a two-layer density gradient centrifugation using Isolate (Irvine Scientific, USA) followed by the swim up technique. COCs were inseminated with 100,000–500,000 progressive motile spermatozoa/ml 3–5 h after oocyte aspiration. Sixteen to 20 h after insemination, the zygotes were checked for 2PN and polar bodies to assess fertilization. Normally fertilized 2PN zygotes were transferred into fresh drops of G-1 medium (Vitrolife, Sweden). An early cleavage check was done at 26 ± 1 h and a D3 embryo assessment was performed at 68 ± 1 h after insemination. A good-quality embryo was defined as follows: 6–10 cells, < 25% fragmentation, and equally sized mononucleated blastomeres. Embryo transfer was performed for all the patients on day 3 with the best 1–2 embryos.
Clinical pregnancy was defined as a positive plasma β-hCG concentration and by the ultrasound detection of a fetal heartbeat after 5 weeks. Implantation rate was defined as the number of gestation sacs on ultrasound as a percentage of the embryos transferred. Early pregnancy loss includes anembryonic gestation and embryonic or fetal death, inevitable abortion, and incomplete abortion [21]. Live birth was defined as a birth in which one or more fetuses were live-born.
Serum and follicular fluid sampling, ELISA experiment
We obtained the sample of serum and follicular fluid on the day of oocyte pickup. Follicular fluid was collected from the first large follicle with a diameter ≥ 18 mm in size and from which an oocyte was retrieved. Samples contaminated with blood were excluded. Blood and follicular fluid samples were centrifuged for 10 min at 3000 rpm and stored at − 80 °C for subsequent analysis.
Fetuin-B was assayed using a commercial sandwich enzyme-linked immunosorbent assay (ELISA) (Human Fetuin B ELISA Kit, RayBiotech, USA), following the manufacturer’s protocol.
Study size calculation
To calculate the required sample size, a two-sample t test power analysis was applied to the data from our pilot study including 26 LF cycles and 44 HF cycles using PASS 11.0 software. Results suggested that 50 samples for each group were enough.
Statistical analysis
Statistical analysis was performed with the Statistical Package for Social Sciences for Windows software package version 22.0 (SPSS, Chicago, IL, USA). Data were described as mean ± SD and compared using t test or Mann–Whitney U test. Chi-square tests or Fisher’s exact test was used to compare embryo transfer outcome rates. Pearson correlation was used to analyze the linear relationship between two variables. P < 0.05 was considered to be statistically significant.
Results
Demographics and IVF cycle characteristics
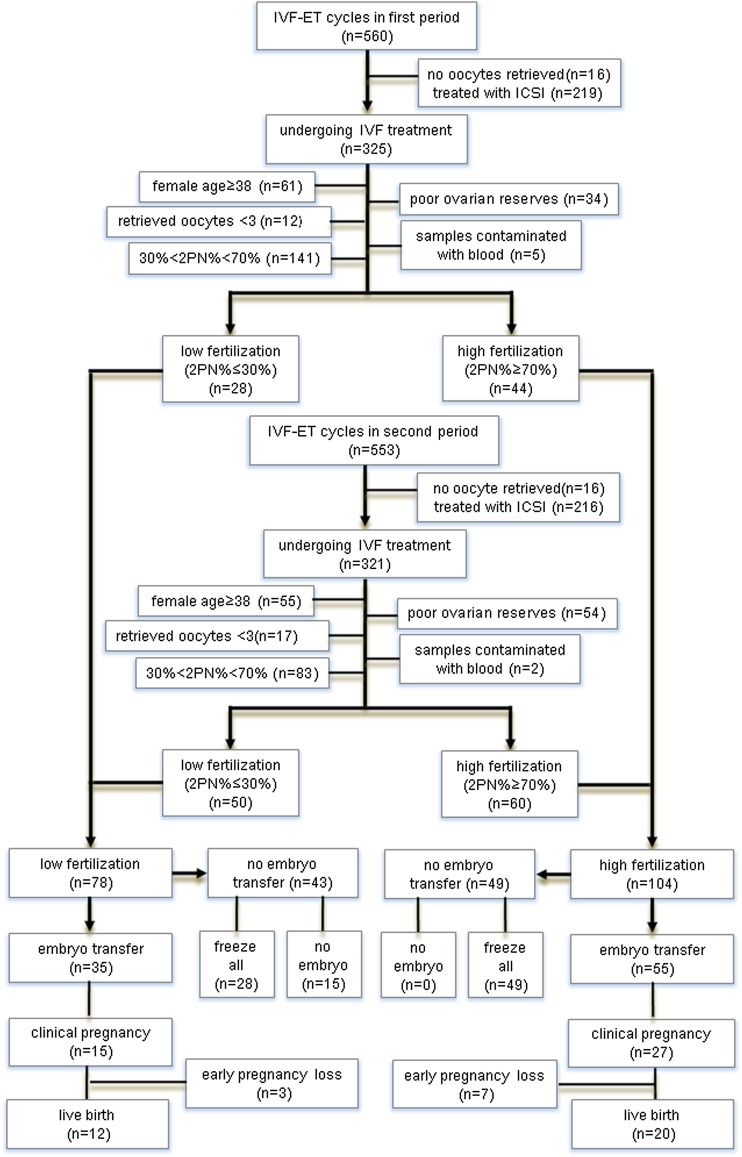
Out of the 646 IVF cycles performed during the study period, 78 cycles were included in LF group and 104 cycles were included in HF group (Fig. 1). No difference was found between the two groups in age, BMI, and basal hormone profiles. The number of retrieved oocytes was similar in both groups (P > 0.05). The patients’ clinical characteristics are summarized in Table 1.
Fig. 1.
Flowchart of patient selection process and IVF treatment
Table 1.
Clinical characteristics of patients in LF and HF groups
| LF group N = 78 | HF group N = 104 | P value | |
|---|---|---|---|
| Age, mean ± SD | 31.43 ± 4.36 | 31.16 ± 3.94 | 0.660 |
| BMI (kg/m2), mean ± SD | 22.65 ± 2.82 | 22.02 ± 2.98 | 0.145 |
| Infertility duration (years), mean ± SD | 4.05 ± 3.22 | 3.96 ± 2.85 | 0.832 |
| No of retrieved oocytes, mean (SD) | 12.59 ± 6.68 | 12.93 ± 5.42 | 0.703 |
| No of MII oocytes, mean (SD) | 10.97 ± 6.35 | 12.45 ± 5.47 | 0.045 |
| E2 on hCG trigger day (pmol/L), mean ± SD | 14,874 ± 9133 | 14,282 ± 8686 | 0.657 |
| Basal FSH (IU/L), mean ± SD | 6.73 ± 1.87 | 6.72 ± 1.79 | 0.638 |
| Basal E2 (pmol/L), mean ± SD | 118.18 ± 71.69 | 116.99 ± 62.32 | 0.398 |
| Basal LH (IU/L)), mean ± SD | 4.98 ± 2.21 | 5.41 ± 2.87 | 0.258 |
| Primary cause of infertility, N (%) | |||
| Tubal | 58 (74.4%) | 68 (65.4%) | 0.194 |
| Endometriosis | 7 (9.0%) | 15 (14.4%) | 0.264 |
| Uterine factor | 5 (6.4%) | 10 (9.6%) | 0.437 |
| Anovulatory | 8 (10.3%) | 11 (10.6%) | 0.944 |
italics: significant result
Fetuin-B levels were correlated with fertilization rates in IVF cycles
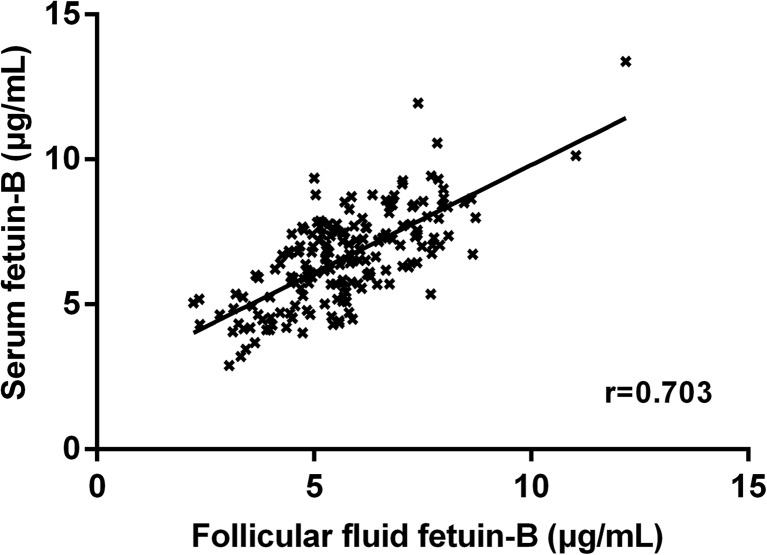
We investigated the relationship between fetuin-B levels in follicular fluid and in serum and found that follicular fluid fetuin-B levels were positively correlated with serum fetuin-B levels (r = 0.703, P < 0.001; Fig. 2).
Fig. 2.
Correlation between fetuin-B levels in serum and follicular fluid. r = 0.703, P < 0.001
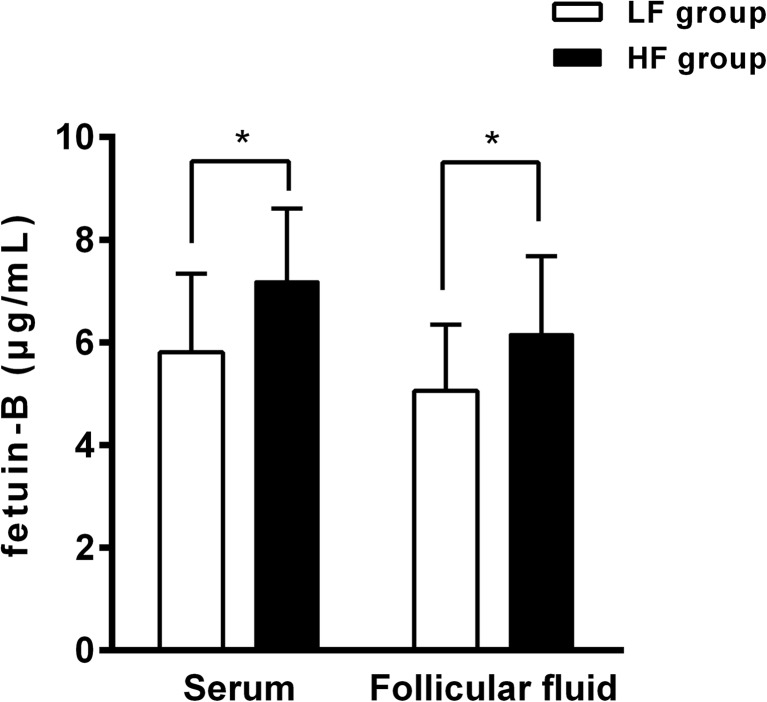
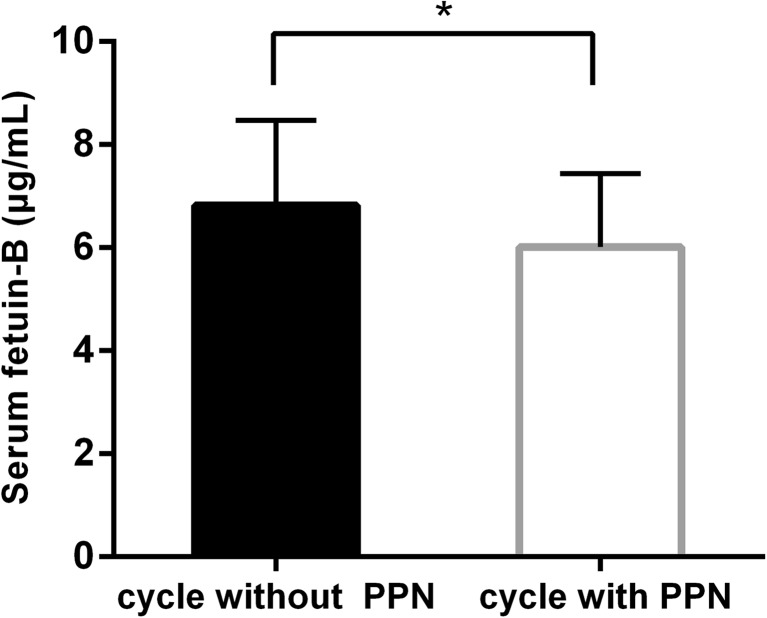
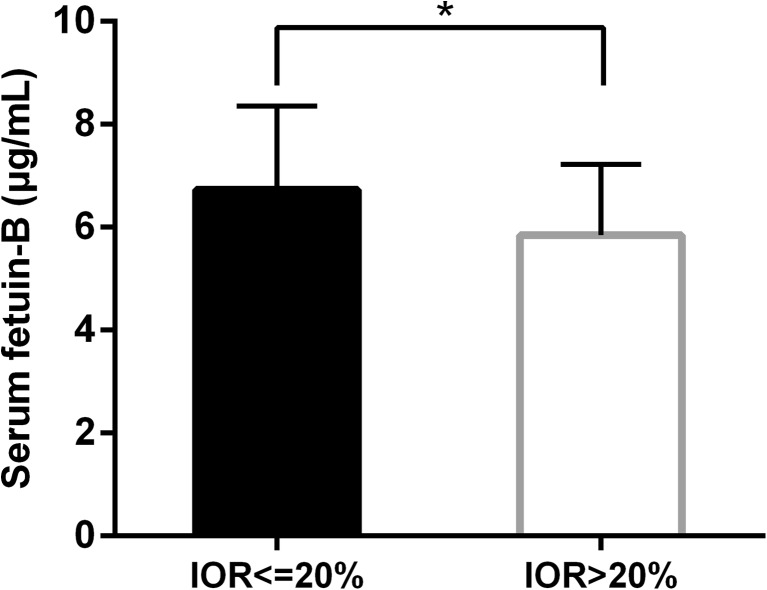
Compared with the HF group, the LF group had significantly lower levels of fetuin-B both in serum (5.81 ± 1.53 vs 7.19 ± 1.42, P < 0.001) and follicular fluid (5.06 ± 1.29 vs 6.16 ± 1.52, P < 0.001; Fig. 3), suggesting a correlation between fetuin-B level and normal fertilization (2PN) rate in IVF. We further investigated the relationship between fetuin B level and abnormal fertilization and found that the serum fetuin-B levels from cycles with polypronuclear (PPN) zygotes were significantly lower when compared to cycles without PPN zygotes (6.82 ± 1.65 vs. 6.10 ± 1.43, P = 0.006; Fig. 4).
Fig. 3.
Serum and follicular fluid fetuin-B levels in LF and HF groups. LF: low fertilization (2PN rate < 30%). HF: high fertilization (2PN rate > 70%).*P < 0.05
Fig. 4.
Serum fetuin- B levels in cycles with or without PPN zygotes. PPN: polypronuclear.*P < 0.05
Fetuin-B levels and oocyte maturation rate
As oocyte nuclear and cytoplasmic maturation are the prerequisites for successful fertilization, we investigated whether fetuin-B level was associated with oocyte maturation rate. Our results showed that the serum fetuin-B levels from cycles with high maturation rates (immature oocyte rate ≤ 20%) were significantly higher than those from cycles with low maturation rate, i.e., immature oocyte rate > 20% (6.73 ± 1.62 vs. 5.85 ± 1.37, P = 0.005; Fig. 5). Moreover, the maturation rate of retrieved oocytes in the HF group was significantly higher than that of the oocytes in the LF group (Table 2).
Fig. 5.
The relationship between serum fetuin-B levels and immature oocyte rate in IVF cycles. IOR: Immature oocyte rate.*P < 0.05
Table 2.
IVF outcomes of LF and HF group
| LF group | HF group | P value | |
|---|---|---|---|
| MII oocyte rate, (% per retrieved oocyte) | 87.2% (856/982) | 98.6% (1326/1345 | 0.000 |
| Good-quality embryo rate, (% per 2PN) | 57.8% (96/166) | 52.6% (593/1127) | 0.209 |
| Canceled cycles, N | 15 | 0 | – |
| Clinical pregnancy rate (% per transfer cycle) | 42.9% (15/35) | 49.1% (27/55) | 0.563 |
| Early pregnancy loss, (% per transfer cycle) | 20.0% (3/35) | 25.9% (7/55) | 0.666 |
| Live birth, (% per transfer cycle) | 34.3% (12/35) | 36.4% (20/55) | 0.841 |
| Implantation, (% per transferred embryo) | 35.7% (20/56) | 38.2% (34/89) | 0.763 |
Fetuin-B levels and IVF outcomes
Although serum fetuin-B levels were associated with fertilization in IVF cycles, we did not find any relationship between fetuin-B levels and preimplantation embryo development, which was assessed by early cleavage and D3 good-embryo rate (Table 3). In the LF group, 15 cycles were canceled due to fertilization failure or lack of embryo transfer. Fresh embryo transfer was performed in 35 cycles of LF group and 55 cycles of HF group, resulting in 15 clinical pregnancies/12 live births in LF group and 27 clinical pregnancies/20 live births in HF group, respectively. Patients who achieved clinical pregnancy or live birth showed similar serum fetuin-B levels to patients who failed to get pregnant or have a live birth (Table 3). And there were no differences in the rates of good-quality embryo, clinical pregnancy, implantation, and live birth between LF and HF groups (Table 2).
Table 3.
The relationship between serum fetuin-B levels and embryo development/pregnancy outcomes
| N | Fetuin-B (mean ± SD) | P | |
|---|---|---|---|
| Early cleavage | |||
| Yes | 49 | 6.84 ± 1.30 | 0.425 |
| No | 38 | 6.57 ± 1.61 | |
| Good quality embryos on D3 | |||
| > 60% | 75 | 6.43 ± 1.45 | 0.196 |
| < 60% | 92 | 6.75 ± 1.69 | |
| Clinical pregnancy | |||
| Yes | 42 | 6.63 ± 1.25 | 0.099 |
| No | 48 | 6.70 ± 1.66 | |
| Early pregnancy loss | |||
| Yes | 10 | 6.79 ± 1.32 | 0.631 |
| No | 32 | 6.58 ± 1.24 | |
| Live birth | |||
| Yes | 32 | 6.58 ± 1.24 | 0.126 |
| No | 58 | 6.71 ± 1.59 | |
Discussion
In follicles, fetuin-B, a liver-derived plasma protein, keeps the oocyte fertilizable by inhibiting ovastacin, a protease known to trigger ZPH [11]. A pilot study suggested that serum fetuin-B increased during IVF cycles in which at least one oocyte was fertilized (n = 15) while fertilization failure showed no increase in serum fetuin-B (n = 6) [18]. In the current study, we further investigated the relationship between fetuin-B and fertilization outcomes in a larger IVF population and demonstrated a significant correlation between fetuin-B and 2PN rate.
Based on our results showing that fetuin-B helps to achieve normal fertilization in conventional IVF, we give the hypothesis that fetuin-B probably prevents ZPH by inhibiting ovastacin, leading to successful fertilization. Moreover, we found that fetuin-B levels were also associated with PPN rate. As most PPN zygotes derived from conventional IVF are polyspermic [22], low fetuin-B levels in IVF may also be associated with other ZP functional defects leading to polyspermy, in addition to premature ZP hardening.
We also found a negative association between serum fetuin-B levels and immature oocyte rates in IVF. Although serum fetuin-B was unaffected by the menstrual cycle and its associated hormonal changes, very high estradiol levels were associated with increased serum fetuin-B in IVF patients undergoing ovarian stimulation [18]. In a natural cycle, stable fetuin-B levels in serum and follicular fluid are sufficient to keep oocytes fertilizable as only one follicle will be developed in 1 cycle. In contrast, during IVF treatment multiple follicles are developed after ovarian stimulation. Fetuin-B expression will be stimulated by high endogenous estradiol [18] to keep multiple oocytes fertilizable. It is well-known that an increase in serum estradiol concentration is indicative of follicular development and is the most important index of oocyte maturation. We suppose that in IVF cycles with a high immature rate, relatively low fetuin-B levels may be insufficient to inhibit ovastacin in multiple follicles, leading to fertilization failure of some oocytes. Our results suggest that low fetuin-B levels may be related to low oocyte maturation. Oocyte maturation includes not only nuclear maturation characterized by germinal vesicle breakdown and extrusion of the first polar body but also ZP gene mRNA expression [23] and reprogramming of the oocyte cytoplasm [24]. Oocyte maturation is the prerequisite for successful fertilization. Deficiency of oocyte maturity, fetuin-B-related ZPH, and fertilization failure are related to each other.
We found that serum fetuin-B was correlated with follicular fluid fetuin-B, which is consistent with previous studies. These data suggest that fetuin-B can diffuse from the blood into the follicles and that serum fetuin-B may be used as a predictive marker of fertilization outcome in conventional IVF cycles. To avoid fertilization failure, ICSI is frequently used. However, compared with conventional IVF, ICSI is more invasive because it involves physical disruption of the cell membrane of the oocyte and introduction of extraneous material into the oocyte. It has been suggested that ICSI-conceived children may have an increased risk of autism and intellectual impairment [3]. A study based on nearly 60,000 singleton deliveries showed that the human secondary sex ratio after ICSI decreased to 50%, whereas IVF has a male-biased sex ratio of 52.2% [25]. In recent years, it has been noticed that children born through ICSI may have a higher risk of epigenetic disruption, including Angelman syndrome, Beckwith–Wiedemann syndrome, and Silver–Russell syndrome [4]. The investigation of fertilization markers, such as fetuin-B, may help to reduce the overuse of ICSI. An animal study demonstrated that supplementation of IVM media with recombinant mouse fetuin-B increased the fertilization rate [26]. Thus, adding recombinant fetuin-B to human maturation media may also help to keep the ZP penetrable and increase the fertilization rate.
Although our study demonstrated the correlation between serum fetuin-B level and fertilization rate in IVF cycles, the results are preliminary. Further investigation of the relationship between fetuin-B levels and oocyte quality, estradiol, and ovarian stimulation may extend our findings. Well-designed, larger studies should be performed before fetuin-B can be used as an index of fertilization in IVF.
In conclusion, our study shows that serum fetuin-B level is correlated with fertilization rate in conventional IVF and it may be used as a predictive marker of fertilization in IVF treatment.
Funding information
This study was supported by National Natural Science Foundation of China (Grant Nos. 81771585 and 81370761) and Department of Health of Zhejiang Province (CN) (Grant No. 2017198128).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Swain JE, Pool TB. ART failure: oocyte contributions to unsuccessful fertilization. Hum Reprod Update. 2008;14:431–446. doi: 10.1093/humupd/dmn025. [DOI] [PubMed] [Google Scholar]
- 2.Krog M, Prior M, Carlsen E, Loft A, Forman J, Pinborg A, Andersen AN. Fertilization failure after IVF in 304 couples--a case-control study on predictors and long-term prognosis. Eur J Obstet Gynecol Reprod Biol. 2015;184:32–37. doi: 10.1016/j.ejogrb.2014.10.037. [DOI] [PubMed] [Google Scholar]
- 3.Catford SR, McLachlan RI, O'Bryan MK, et al. Long-term follow-up of intra-cytoplasmic sperm injection-conceived offspring compared with in vitro fertilization-conceived offspring: a systematic review of health outcomes beyond the neonatal period. Andrology. 2017;5:610–621. doi: 10.1111/andr.12369. [DOI] [PubMed] [Google Scholar]
- 4.Jiang Z, Wang Y, Lin J, Xu J, Ding G, Huang H. Genetic and epigenetic risks of assisted reproduction. Best Pract Res Clin Obstet Gynaecol. 2017;44:90–104. doi: 10.1016/j.bpobgyn.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Avella MA, Baibakov B, Dean J. A single domain of the ZP2 zona pellucida protein mediates gamete recognition in mice and humans. J Cell Biol. 2014;205:801–809. doi: 10.1083/jcb.201404025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stocker W, Karmilin K, Hildebrand A, et al. Mammalian gamete fusion depends on the inhibition of ovastacin by fetuin-B. Biol Chem. 2014;395:1195–1199. doi: 10.1515/hsz-2014-0189. [DOI] [PubMed] [Google Scholar]
- 7.Burkart AD, Xiong B, Baibakov B, Jiménez-Movilla M, Dean J. Ovastacin, a cortical granule protease, cleaves ZP2 in the zona pellucida to prevent polyspermy. J Cell Biol. 2012;197:37–44. doi: 10.1083/jcb.201112094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ducibella T, Anderson E, Albertini DF, Aalberg J, Rangarajan S. Quantitative studies of changes in cortical granule number and distribution in the mouse oocyte during meiotic maturation. Dev Biol. 1988;130:184–197. doi: 10.1016/0012-1606(88)90425-3. [DOI] [PubMed] [Google Scholar]
- 9.Ducibella T, Kurasawa S, Rangarajan S, Kopf GS, Schultz RM. Precocious loss of cortical granules during mouse oocyte meiotic maturation and correlation with an egg-induced modification of the zona pellucida. Dev Biol. 1990;137:46–55. doi: 10.1016/0012-1606(90)90006-5. [DOI] [PubMed] [Google Scholar]
- 10.Schiewe MC, Araujo E, Jr, Asch RH, Balmaceda JP. Enzymatic characterization of zona pellucida hardening in human eggs and embryos. J Assist Reprod Genet. 1995;12:2–7. doi: 10.1007/BF02214120. [DOI] [PubMed] [Google Scholar]
- 11.Dietzel E, Wessling J, Floehr J, Schäfer C, Ensslen S, Denecke B, Rösing B, Neulen J, Veitinger T, Spehr M, Tropartz T, Tolba R, Renné T, Egert A, Schorle H, Gottenbusch Y, Hildebrand A, Yiallouros I, Stöcker W, Weiskirchen R, Jahnen-Dechent W. Fetuin-B, a liver-derived plasma protein is essential for fertilization. Dev Cell. 2013;25:106–112. doi: 10.1016/j.devcel.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Lee C, Bongcam-Rudloff E, Sollner C, et al. Type 3 cystatins; fetuins, kininogen and histidine-rich glycoprotein. Front Biosci (Landmark Ed) 2009;Volume(14):2911–2922. doi: 10.2741/3422. [DOI] [PubMed] [Google Scholar]
- 13.Li Z, Lin M, Liu C, Wang D, Shi X, Chen Z, Liu Y, Yang S, Li X. Fetuin-B links nonalcoholic fatty liver disease to type 2 diabetes via inducing insulin resistance: association and path analyses. Cytokine. 2018;108:145–150. doi: 10.1016/j.cyto.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Jung SH, Won KJ, Lee KP, Kim HJ, Seo EH, Lee HM, Park ES, Lee SH, Kim B. The serum protein fetuin-B is involved in the development of acute myocardial infarction. Clin Sci (Lond) 2015;129:27–38. doi: 10.1042/CS20140462. [DOI] [PubMed] [Google Scholar]
- 15.Zhu K, Wang Y, Shu P, Zhou Q, Zhu J, Zhou W, du C, Xu C, Liu X, Tang L. Increased serum levels of fetuin B in patients with coronary artery disease. Endocrine. 2017;58:97–105. doi: 10.1007/s12020-017-1387-1. [DOI] [PubMed] [Google Scholar]
- 16.Floehr J, Dietzel E, Schmitz C, Chappell A, Jahnen-Dechent W. Down-regulation of the liver-derived plasma protein fetuin-B mediates reversible female infertility. Mol Hum Reprod. 2017;23:34–44. doi: 10.1093/molehr/gaw068. [DOI] [PubMed] [Google Scholar]
- 17.Olivier E, Soury E, Ruminy P, et al. Fetuin-B, a second member of the fetuin family in mammals. Biochem J. 2000;350(Pt 2):589–597. doi: 10.1042/bj3500589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Floehr J, Dietzel E, Neulen J, Rösing B, Weissenborn U, Jahnen-Dechent W. Association of high fetuin-B concentrations in serum with fertilization rate in IVF: a cross-sectional pilot study. Hum Reprod. 2016;31:630–637. doi: 10.1093/humrep/dev340. [DOI] [PubMed] [Google Scholar]
- 19.Ye Y, Qian Y, Xu C, Jin F. Meiotic segregation analysis of embryos from reciprocal translocation carriers in PGD cycles. Reprod BioMed Online. 2012;24:83–90. doi: 10.1016/j.rbmo.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . WHO Laboratory manual for the examination and processing of human semen. 5. Geneva: World Health Organization; 2010. [Google Scholar]
- 21.Schreiber CA, Creinin MD, Atrio J, Sonalkar S, Ratcliffe SJ, Barnhart KT. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161–2170. doi: 10.1056/NEJMoa1715726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kai Y, Iwata K, Iba Y, Mio Y. Diagnosis of abnormal human fertilization status based on pronuclear origin and/or centrosome number. J Assist Reprod Genet. 2015;32:1589–1595. doi: 10.1007/s10815-015-0568-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Canosa S, Adriaenssens T, Coucke W, Dalmasso P, Revelli A, Benedetto C, Smitz J. Zona pellucida gene mRNA expression in human oocytes is related to oocyte maturity, zona inner layer retardance and fertilization competence. Mol Hum Reprod. 2017;23:292–303. doi: 10.1093/molehr/gax008. [DOI] [PubMed] [Google Scholar]
- 24.Eppig JJ. Coordination of nuclear and cytoplasmic oocyte maturation in eutherian mammals. Reprod Fertil Dev. 1996;8:485–489. doi: 10.1071/RD9960485. [DOI] [PubMed] [Google Scholar]
- 25.Cirkel C, Konig IR, Schultze-Mosgau A, et al. The use of intracytoplasmic sperm injection is associated with a shift in the secondary sex ratio. Reprod BioMed Online. 2018;37:703–708. doi: 10.1016/j.rbmo.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Dietzel E, Floehr J, Van de Leur E, et al. Recombinant fetuin-B protein maintains high fertilization rate in cumulus cell-free mouse oocytes. Mol Hum Reprod. 2017;23:25–33. doi: 10.1093/molehr/gaw067. [DOI] [PubMed] [Google Scholar]