Abstract
The ultimate trauma management system should allow the completion of all time‐consuming life‐saving procedures in one trauma resuscitation room. In 2011, the Hybrid Emergency Room System (HERS) was developed in Japan as a novel trauma care system that allows clinicians to perform all life‐saving procedures for severely injured patients, including whole‐body computed tomography examination, damage control surgery, and transcatheter arterial embolization by interventional radiology, on the same table in the same room without transferring the patient. Since then, the number of HERS installations has rapidly increased around Japan. To promote further innovation and dissemination of this new and creative concept of trauma management, the Japanese Association for Hybrid Emergency Room System was launched on June 21, 2018. In this article, the concept, history, and current evidence behind this new trauma workflow system are summarized. This is the first review to show the next direction of trauma care using HERS.
Keywords: Computed tomography, interventional radiology, patient care management, severe trauma, surgery
Introduction
Many major urban trauma centers have elected to install a computed tomography (CT) scanner, operating room, and angiography room just next to their emergency rooms.1, 2, 3, 4 Although this concept substantially diminishes delays resulting from transferring patients to CT scanners and undertaking bleeding control procedures, the ultimate trauma management system should allow all of the necessary time‐consuming life‐saving procedures to be carried out in one trauma resuscitation room. Here, the concept, history, and current evidence behind a novel trauma workflow system, the Hybrid Emergency Room System (HERS), are summarized. To encourage further innovation and dissemination of HERS, the Japanese Association for Hybrid Emergency Room System was created on June 21, 2018 in Kyoto, Japan.
What is HERS?
Trauma is a surgical disease, and all life‐threatening hemorrhagic events have traditionally been controlled through surgery. In the cutting‐edge trauma care system, however, non‐operative management of trauma through interventional radiology (IR) procedures has become an important focus of interest, even in the care of hemodynamically unstable patients.5 To better exploit the trauma care system, precise diagnosis and comprehension of injury mechanisms are essential. Identification of the exact point of bleeding by contrast‐enhanced CT has expanded the indications and strengthened the effectiveness of IR.6, 7 Therefore, rapid access to both a CT scanner and IR procedures are key components in the further development and innovation of trauma care.
In August 2011, Osaka General Medical Center (Osaka, Japan) implemented a new trauma workflow concept comprising a sliding CT scanner system with IR features that allows all emergency therapeutic interventions to be carried out without relocating the patient to different departments (Fig. 1). Such a concept can facilitate definitive interventions more quickly in comparison with a conventional trauma care protocol.8 The room and trauma system was named the “Hybrid Emergency Room System”.
Figure 1.

Hybrid Emergency Room System. All life‐saving procedures including airway management, computed tomography (CT) examination, emergency surgery, and interventional radiology (IR) can be carried out promptly and safely on the same table without transferring the patient to different departments.
Generally, the term “hybrid” refers to something that is a mixture of two very different things. In HERS terminology, the combination of ‘‘examinations’’ and ‘‘treatments’’ in the same space results in a novel “hybrid” concept of acute medicine and trauma care. This novel system allows the performance of all life‐saving procedures, including whole‐body CT examination, damage control surgery, and transcatheter arterial embolization by IR, in severely injured patients on the same table without ever having to transfer them to other departments (Fig. 2). Although many institutions have already installed an angio‐CT suite or a hybrid operating room, the trauma strategy of temporarily using these existing rooms as a trauma resuscitation space is insufficient in fulfilling the original HERS concept. The principal concept of HERS consists of a special angio‐CT suite designated exclusively for the management of possibly critical patients combined with a well‐trained team specializing in undertaking trauma resuscitation in a single room.
Figure 2.
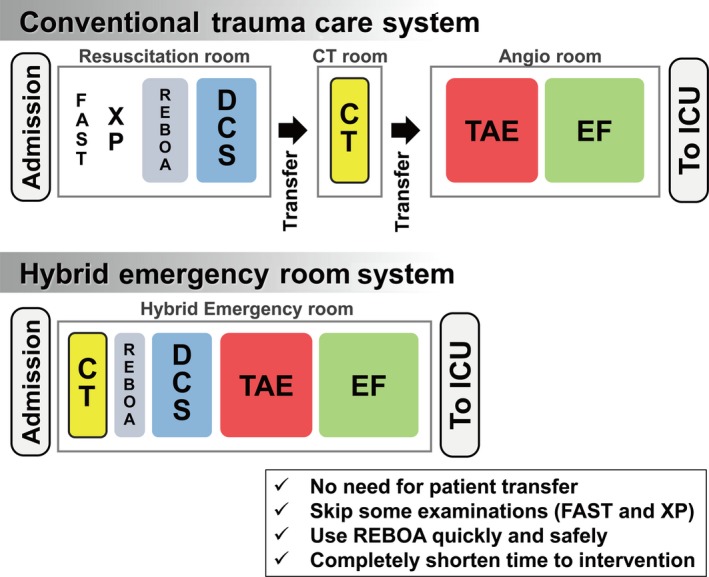
Conceptual diagram of trauma workflow in the conventional trauma care system versus that in the Hybrid Emergency Room System. Sample trauma flow of a patient suffering, as an example, a pelvic fracture with severe bleeding and shock. CT, computed tomography; DCS, damage control surgery; EF, external fixation; FAST, focused assessment with sonography for trauma; ICU, intensive care unit; REBOA, resuscitative endovascular balloon occlusion of the aorta; TAE, transarterial embolization; XP, X‐ray photography.
Rapid spread of HERS around Japan
After the first HERS installation in July 2011, the number of HERS installations has rapidly increased around Japan (Table 1). To improve the workflow of trauma care, several studies previously tried to show the effectiveness on work‐up time1, 2, 3, 4 and survival benefit9, 10 of integrating CT into the trauma resuscitation room. In HERS, the central concept of carrying out not only diagnostic procedures but also definitive trauma intervention all in one resuscitation room is thought to be a breakthrough in trauma care. Due to the numerous reports on HERS, many level I trauma centers in Japan are becoming interested in and enthusiastic about HERS installation in their own institutions.
Table 1.
Installation and spread of the hybrid emergency room system (HERS) in Japan
| Institution | HERS model | Angio‐CT system | Space occupied by HERS† | Installation year of HERS | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | ||||
| Osaka General Medical Center | Single‐room | CX TSX‐101A; INFX‐8000C; Canon Medical Systems | 91.5 m2 (53.9 m2) | Aug | → | → | → | → | → | → | → |
| Tokyo Metropolitan Bokutoh Hospital | Single‐room | CXL TSX‐101A; INFX‐8000C; Canon Medical Systems | 79.2 m2 (47.6 m2) | July | → | → | → | → | |||
| Yonemori Hospital | Single‐room | Definition AS+; Siemens Healthcare. Xper FD20; Philips | 95.2 m2 (85.1 m2) | Sept | → | → | → | → | |||
| Jichi Medical University Saitama Medical Center | Single‐room | PRIME TSX‐303A; INFX‐8000C; Canon Medical Systems | 81.8 m2 (53.0 m2) | Apr | → | → | |||||
| Hyogo Emergency Medical Center | Single‐room | PRIME TSX‐303A; INFX‐8000C; Canon Medical Systems | 72.9 m2 (45.5 m2) | Mar | → | ||||||
| Teikyo University Hospital | Single‐room | ONE TSX‐301C; INFX‐8000C; Canon Medical Systems | 73.6 m2 (51.8 m2) | July | → | ||||||
| Kansai Medical University General Medical Center | Dual‐room | PRIME TSX‐303A; INFX‐8000C; Canon Medical Systems | 92.3 m2 (68.8 m2) | July | → | ||||||
| Shimane University Hospital | Single‐room | PRIME TSX‐303A; INFX‐8000H; Canon Medical Systems | 109.0 m2 (82.0 m2) | Aug | → | ||||||
| Saiseikai Yokohamashi Tobu Hospital | Dual‐room | PRIME TSX‐303A; INFX‐8000C; Canon Medical Systems | 109.6 m2 (79.2 m2) | Oct | → | ||||||
| Tohoku University Hospital | Single‐room | Definition AS+; ARTIS pheno; Siemens Healthcare | 123.6 m2 (110.4 m2) | May | |||||||
The arrows in the table means the HERS are working.
Area of the total space occupied by HERS with the actual medical treatment space in parentheses.
The barriers to the new installation of HERS are adequate space and funding. The area of the existing HERS installations varies between hospitals, as shown in Table 1. To establish a HERS, space for a machinery room and control room for the equipment used in CT/IR are required in addition to that for actual medical treatment. Most of the institutions have decided to install their HERS at a time when significant renovations of the hospital or emergency department are undertaken. However, if a sufficient area already exists for HERS installation and approximately $0.5–2 million in funding is available, a hospital trauma team might consider the installation of a new HERS in their emergency department. To date, 11 HERS have been installed (10 in Japan and 1 in Korea), and the spread of HERS is expected to accelerate over the next several years.
Available clinical evidence regarding HERS
The effects of interventions carried out in the HERS room on 696 patients with severe trauma (Injury Severity Score ≥16) were previously reported in a single‐center, historical, controlled study.11 The HERS was found to be significantly associated with decreased mortality (adjusted odds ratio [aOR], 0.50; 95% confidence interval [CI], 0.29–0.85; P = 0.011) and reduced deaths from exsanguination (aOR, 0.17; 95% CI, 0.06–0.47; P = 0.001). The times to the initiation of CT and emergency bleeding control procedures were both shorter in the HERS group versus the conventionally treated group (11 [8–16] versus 26 [21–32] min; P < 0.0001 and 47 [37–57] versus 68 [51–85] min; P < 0.0001, respectively). This was the first report to show the effectiveness on clinical outcomes of the innovation of trauma workflow provided by the installation of HERS in the trauma resuscitation room.
The same dataset from a single center was also used to assess the effectiveness of the HERS on functional outcomes in patients with severe traumatic brain injury (TBI).12 The timely treatment of severe TBI is essential to limit secondary damage to the brain, thus, the concept of HERS could also be suitable for the treatment of severe TBI. As a primary end‐point, an unfavorable outcome at 6 months post‐injury as evaluated by the Glasgow Outcome Scale – Extended was significantly reduced after the HERS installation (aOR, 0.42; 95% CI, 0.18–0.93; P = 0.036). The strength of HERS in the trauma care setting might not be limited only to hemorrhagic patients at risk of death from exsanguination who undergo emergency bleeding control procedures; severe TBI patients with impending herniation can also benefit from the HERS thanks to the capacity to rapidly undertake intracranial surgery and deliver immediate neurocritical care.
Future directions
In the historical controlled study undertaken at Osaka General Medical Center, patient outcomes did not immediately improve after HERS installation. In fact, the restricted cubic spline curve revealed that the estimated mortality rose temporarily during the first year after the HERS installation and then dropped below the baseline mortality value.11 These results suggested that specialized team‐based learning focused specifically on working within the HERS is absolutely essential to best utilize the HERS in trauma care. The complete trauma team consists of trauma surgeons, emergency physicians, radiologists, anesthesiologists, nurses, radiological technologists, and other paramedical staff. To specifically address the needs of the specialized trauma team needed for HERS, the Japanese Association for Hybrid Emergency Room System was recently established. The primary objectives of the association are to standardize trauma management protocols specialized for HERS, to educate and improve the sophistication of the trauma teams, and to combat all trauma deaths.
The development not only of well‐trained trauma teams as mentioned above but also the next‐generation HERS itself is expected to be quite remarkable. One of the major limitations of the original HERS is that the room can be occupied by one severely injured patient for a prolonged period due to the performance of several time‐consuming emergency procedures. To overcome this issue, Kansai Medical University General Medical Center installed the first so‐called “second‐generation HERS” in July 2017.13 This second‐generation HERS implemented a dual‐room angio‐CT system to increase patient throughput. These two rooms are separated by a moveable door, and the sliding CT scanner can move between these two rooms as needed. The dual‐room HERS has enabled both the treatment of two severely injured patients simultaneously and the use of CT scanning or IR for another inpatient or outpatient using the second room next to the primary HERS room already in use.
Looking forward, the Japanese Association for Hybrid Emergency Room System will continue to innovate and disseminate HERS as a new and creative concept in trauma management.
Disclosure
Approval of the research protocol: N/A.
Informed consent: N/A.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Conflict of interest: None declared.
Appendix I.
Founding Members of the Japanese Association for Hybrid Emergency Room System
Kazuma Yamakawa, Satoshi Fujimi, and Atsushi Watanabe (Osaka General Medical Center, Osaka); Kazuhiro Sugiyama (Tokyo Metropolitan Bokutoh Hospital, Tokyo); Michiaki Hata (Yonemori Hospital, Kagoshima); Takashi Moriya (Saitama Medical Center Jichi Medical University, Saitama); Shigenari Matsuyama (Hyogo Emergency Medical Center, Hyogo); Takashi Fujita (Teikyo University School of Medicine, Tokyo); Yasushi Nakamori (Kansai Medical University General Medical Center, Osaka); Hiroaki Watanabe (Shimane University Faculty of Medicine, Shimane); Tomohiro Funabiki (Saiseikai Yokohamashi Tobu Hospital, Kanagawa); Shigeki Kushimoto (Tohoku University Graduate School of Medicine, Miyagi); Junichi Matsumoto (St. Marianna University School of Medicine, Kanagawa); Isao Ukai (Hyogo Prefectural Nishinomiya Hospital, Hyogo); and Takahiro Kinoshita (Osaka University Graduate School of Medicine, Osaka).
Funding information
No funding information provided.
[Correction added on 17 May 2019, after first online publication: The author names and corresponding affiliations have been changed to “The founding members of the Japanese Association for Hybrid Emergency Room System”.]
References
- 1. Weninger P, Mauritz W, Fridrich P et al Emergency room management of patients with blunt major trauma: evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J. Trauma 2007; 62: 584–91. [DOI] [PubMed] [Google Scholar]
- 2. Hilbert P, zur Nieden K, Hofmann GO, Hoeller I, Koch R, Stuttmann R. New aspects in the emergency room management of critically injured patients: a multi‐slice CT‐oriented care algorithm. Injury 2007;38:552–8. [DOI] [PubMed] [Google Scholar]
- 3. Fung Kon Jin PH, Goslings JC, Ponsen KJ, van Kuijk C, Hoogerwerf N, Luitse JS. Assessment of a new trauma workflow concept implementing a sliding CT scanner in the trauma room: the effect on workup times. J. Trauma 2008;64:1320–6. [DOI] [PubMed] [Google Scholar]
- 4. Lee KL, Graham CA, Lam JM, Yeung JH, Ahuja AT, Rainer TH. Impact on trauma patient management of installing a computed tomography scanner in the emergency department. Injury 2009; 40: 873–5. [DOI] [PubMed] [Google Scholar]
- 5. Hughes J, Scrimshire A, Steinberg L et al Interventional Radiology service provision and practice for the management of traumatic splenic injury across the Regional Trauma Networks of England. Injury 2017; 48: 1031–4. [DOI] [PubMed] [Google Scholar]
- 6. Misselbeck TS, Teicher EJ, Cipolle MD et al Hepatic angioembolization in trauma patients: indications and complications. J. Trauma 2009; 67: 769–73. [DOI] [PubMed] [Google Scholar]
- 7. Juern JS, Milia D, Codner P et al Clinical significance of computed tomography contrast extravasation in blunt trauma patients with a pelvic fracture. J. Trauma Acute Care Surg. 2017; 82: 138–40. [DOI] [PubMed] [Google Scholar]
- 8. Wada D, Nakamori Y, Yamakawa K, Fujimi S. First clinical experience with IVR‐CT system in the emergency room: positive impact on trauma workflow. Scand J. Trauma Resusc. Emerg. Med. 2012; 20: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saltzherr TP, Bakker FC, Beenen LF, Dijkgraaf MG, Reitsma JB, Goslings JC, REACT Study Group . Randomized clinical trial comparing the effect of computed tomography in the trauma room versus the radiology department on injury outcomes. Br. J. Surg. 2012;99(Suppl 1):105–13. [DOI] [PubMed] [Google Scholar]
- 10. Huber‐Wagner S, Mand C, Ruchholtz S et al Effect of the localisation of the CT scanner during trauma resuscitation on survival – a retrospective, multi‐centre study. Injury 2014; 45(Suppl 3): S76–82. [DOI] [PubMed] [Google Scholar]
- 11. Kinoshita T, Yamakawa K, Matsuda H et al The survival benefit of a novel trauma workflow that includes immediate whole‐body computed tomography, surgery, and interventional radiology, all in one trauma resuscitation room: A retrospective historical control study. Ann. Surg. 2019; 269: 370–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kinoshita T, Hayashi M, Yamakawa K et al Effect of the Hybrid Emergency Room System on functional outcome in patients with severe traumatic brain injury. World Neurosurg. 2018; 118: e792–9. [DOI] [PubMed] [Google Scholar]
- 13. Wada D, Nakamori Y, Kanayama S et al First installation of a dual‐room IVR‐CT system in the emergency room. Scand J. Trauma Resusc. Emerg. Med. 2018; 26: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]


