Abstract
Background
Polycystic ovarian syndrome (PCOS) is characterised by the clinical signs of oligo‐amenorrhoea, infertility and hirsutism. Conventional treatment of PCOS includes a range of oral pharmacological agents, lifestyle changes and surgical modalities. Beta‐endorphin is present in the follicular fluid of both normal and polycystic ovaries. It was demonstrated that the beta‐endorphin levels in ovarian follicular fluid of otherwise healthy women who were undergoing ovulation were much higher than the levels measured in plasma. Given that acupuncture impacts on beta‐endorphin production, which may affect gonadotropin‐releasing hormone (GnRH) secretion, it is postulated that acupuncture may have a role in ovulation induction via increased beta‐endorphin production effecting GnRH secretion. This is an update of our previous review published in 2016.
Objectives
To assess the effectiveness and safety of acupuncture treatment for oligo/anovulatory women with polycystic ovarian syndrome (PCOS) for both fertility and symptom control.
Search methods
We identified relevant studies from databases including the Gynaecology and Fertility Group Specialised Register, CENTRAL, MEDLINE, Embase, PsycINFO, CNKI, CBM and VIP. We also searched trial registries and reference lists from relevant papers. CENTRAL, MEDLINE, Embase, PsycINFO, CNKI and VIP searches are current to May 2018. CBM database search is to November 2015.
Selection criteria
We included randomised controlled trials (RCTs) that studied the efficacy of acupuncture treatment for oligo/anovulatory women with PCOS. We excluded quasi‐ or pseudo‐RCTs.
Data collection and analysis
Two review authors independently selected the studies, extracted data and assessed risk of bias. We calculated risk ratios (RR), mean difference (MD), standardised mean difference (SMD) and 95% confidence intervals (CIs). Primary outcomes were live birth rate, multiple pregnancy rate and ovulation rate, and secondary outcomes were clinical pregnancy rate, restored regular menstruation period, miscarriage rate and adverse events. We assessed the quality of the evidence using GRADE methods.
Main results
We included eight RCTs with 1546 women. Five RCTs were included in our previous review and three new RCTs were added in this update of the review. They compared true acupuncture versus sham acupuncture (three RCTs), true acupuncture versus relaxation (one RCT), true acupuncture versus clomiphene (one RCT), low‐frequency electroacupuncture versus physical exercise or no intervention (one RCT) and true acupuncture versus Diane‐35 (two RCTs). Studies that compared true acupuncture versus Diane‐35 did not measure fertility outcomes as they were focused on symptom control.
Seven of the studies were at high risk of bias in at least one domain.
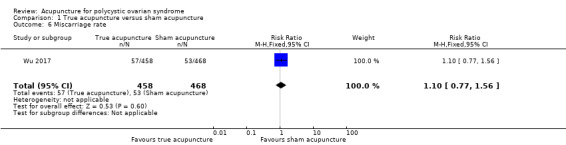
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in live birth (RR 0.97, 95% CI 0.76 to 1.24; 1 RCT, 926 women; low‐quality evidence); multiple pregnancy rate (RR 0.89, 95% CI 0.33 to 2.45; 1 RCT, 926 women; low‐quality evidence); ovulation rate (SMD 0.02, 95% CI –0.15 to 0.19, I2 = 0%; 2 RCTs, 1010 women; low‐quality evidence); clinical pregnancy rate (RR 1.03, 95% CI 0.82 to 1.29; I2 = 0%; 3 RCTs, 1117 women; low‐quality evidence) and miscarriage rate (RR 1.10, 95% CI 0.77 to 1.56; 1 RCT, 926 women; low‐quality evidence).
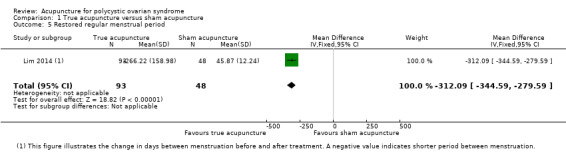
Number of intermenstrual days may have improved in participants receiving true acupuncture compared to sham acupuncture (MD –312.09 days, 95% CI –344.59 to –279.59; 1 RCT, 141 women; low‐quality evidence).
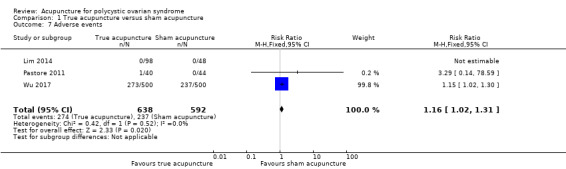
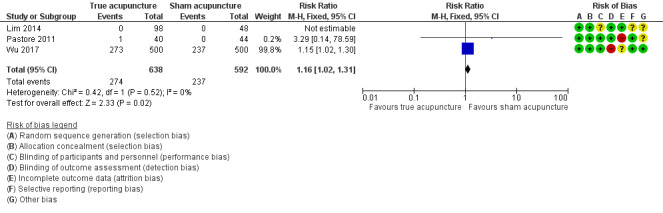
True acupuncture probably worsens adverse events compared to sham acupuncture (RR 1.16, 95% CI 1.02 to 1.31; I2 = 0%; 3 RCTs, 1230 women; moderate‐quality evidence).
No studies reported data on live birth rate and multiple pregnancy rate for the other comparisons: physical exercise or no intervention, relaxation and clomiphene. Studies including Diane‐35 did not measure fertility outcomes.
We were uncertain whether acupuncture improved ovulation rate (measured by ultrasound three months post treatment) compared to relaxation (MD 0.35, 95% CI 0.14 to 0.56; 1 RCT, 28 women; very low‐quality evidence) or Diane‐35 (RR 1.45, 95% CI 0.87 to 2.42; 1 RCT, 58 women; very low‐quality evidence).
Overall evidence ranged from very low quality to moderate quality. The main limitations were failure to report important clinical outcomes and very serious imprecision.
Authors' conclusions
For true acupuncture versus sham acupuncture we cannot exclude clinically relevant differences in live birth rate, multiple pregnancy rate, ovulation rate, clinical pregnancy rate or miscarriage. Number of intermenstrual days may improve in participants receiving true acupuncture compared to sham acupuncture. True acupuncture probably worsens adverse events compared to sham acupuncture.
No studies reported data on live birth rate and multiple pregnancy rate for the other comparisons: physical exercise or no intervention, relaxation and clomiphene. Studies including Diane‐35 did not measure fertility outcomes as the women in these trials did not seek fertility.
We are uncertain whether acupuncture improves ovulation rate (measured by ultrasound three months post treatment) compared to relaxation or Diane‐35. The other comparisons did not report on this outcome.
Adverse events were recorded in the acupuncture group for the comparisons physical exercise or no intervention, clomiphene and Diane‐35. These included dizziness, nausea and subcutaneous haematoma. Evidence was very low quality with very wide CIs and very low event rates.
There are only a limited number of RCTs in this area, limiting our ability to determine effectiveness of acupuncture for PCOS.
Plain language summary
Acupuncture for polycystic ovarian syndrome
Review question
What is the effectiveness and safety of acupuncture treatment for ovulation disorders in women with polycystic ovarian syndrome (PCOS)?
Background
PCOS is where women have multiple cysts (fluid‐filled sacs) on their ovaries (organs that produce eggs) and is characterised by the clinical signs of infrequent or very light menstruation (periods), failure to conceive (become pregnant) and excessive hair growth. Women may or may not have symptoms. The current standard western treatments for women with PCOS are prescription medicines, surgery and lifestyle changes. There has been evidence suggesting acupuncture may influence ovulation (release of the egg) by affecting levels of various hormones. Acupuncture is a Chinese therapy where fine needles are inserted into the skin in certain places. The exact mechanism of how acupuncture works for PCOS is not known and we aimed to explore the use of it for PCOS in this review.
Study characteristics
We searched medical databases for clinical studies where people were randomly put into one of two or more treatment groups including acupuncture treatment for women with PCOS who were infrequently or never ovulating. Acupuncture was compared with pretend acupuncture (sham), no treatment, lifestyle changes (e.g. relaxation) and conventional treatment.
We included eight studies with 1546 women in this review. The studies compared true acupuncture versus sham acupuncture, clomiphene (medicines to induce ovulation), relaxation and Diane‐35 (combined oral contraceptive pill); and low‐frequency electroacupuncture (where small electrical currents are passed through the acupuncture needles) versus physical exercise. We included women who wanted to get pregnant and women who wanted regular ovulation and symptom control as our two main populations of interest.
Key results
Our main interests were live birth rate, multiple pregnancy rate (for women who wanted to get pregnant) and ovulation rate (for women who wanted regular ovulation/symptom control). Due to the very low quality of the evidence and imprecise results, we were uncertain of the effect of acupuncture on live birth rate, multiple pregnancy rate and ovulation rate compared to sham acupuncture. For the same reasons, we were also uncertain of the effect of acupuncture on clinical pregnancy and miscarriage rate. Acupuncture may have improved restoration of regular menstrual periods. Acupuncture probably worsened side effects when compared to sham acupuncture.
No studies reported data on live birth rate and multiple pregnancy rate for the other comparisons: physical exercise or no intervention, relaxation and clomiphene. Studies including Diane‐35 did not measure fertility outcomes as women were only interested in symptom control.
We were uncertain whether acupuncture improved ovulation rate compared to relaxation or Diane‐35 (measured by ultrasound, which uses high‐frequency sound waves to create an image, three months after treatment). The other comparisons did not report on ovulation rate.
Side effects were recorded in the acupuncture group for the comparisons physical exercise or no intervention, clomiphene and Diane‐35. These included dizziness, nausea (feeling sick) and bruising.
The overall evidence was low or very low quality. There is currently insufficient evidence to support the use of acupuncture for treatment of ovulation disorders in women with PCOS.
Quality of the evidence
The evidence ranged from very low to moderate quality, the main limitations were not reporting important clinical results and not enough data.
Summary of findings
Summary of findings for the main comparison. True acupuncture compared to sham acupuncture for polycystic ovarian syndrome.
| True acupuncture compared to sham acupuncture for polycystic ovarian syndrome | |||||
| Patient or population: polycystic ovarian syndrome Setting: outpatient Intervention: true acupuncture Comparison: sham acupuncture | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with sham acupuncture | Risk with true acupuncture | ||||
| Live birth rate | Study population | RR 0.97 (0.76 to 1.24) | 926 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| 224 per 1000 | 218 per 1000 (171 to 278) | ||||
| Multiple pregnancy rate | Study population | RR 0.89 (0.33 to 2.45) | 926 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| 17 per 1000 | 15 per 1000 (6 to 42) | ||||
| Ovulation rate | The mean ovulation rate was 0 | SMD 0.02 higher (0.15 lower to 0.19 higher) | — | 1010 (2 RCTs) | ⊕⊕⊝⊝ Lowc,d |
| Clinical pregnancy rate | Study population | RR 1.03 (0.82 to 1.29) | 1117 (3 RCTs) | ⊕⊕⊝⊝ Lowd,e | |
| 211 per 1000 | 217 per 1000 (173 to 272) | ||||
| Restored regular menstrual period | The mean restored regular menstrual period was 0 | MD 312.09 days lower (344.59 lower to 279.59 lower) | — | 141 (1 RCT) | ⊕⊕⊝⊝ Lowf |
| Miscarriage rate | Study population | RR 1.10 (0.77 to 1.56) | 926 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| 113 per 1000 | 125 per 1000 (87 to 177) | ||||
| Adverse events | Study population | RR 1.16 (1.02 to 1.31) | 1230 (3 RCTs) | ⊕⊕⊕⊝ Moderatee | |
| 400 per 1000 | 464 per 1000 (408 to 524) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio; SMD: standardised mean difference. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded one level for high risk of detection bias in one study. bDowngraded one level for imprecision ‐ single study and confidence intervals compatible with benefit in either arm or no effect. cDowngraded one level for high risk of performance bias in one study. dDowngraded one level for imprecision ‐ confidence intervals compatible with benefit in either arm or no effect. eDowngraded one level for high risk of attrition bias and detection bias in two studies. fDowngraded two levels for imprecision ‐ single study with small sample size.
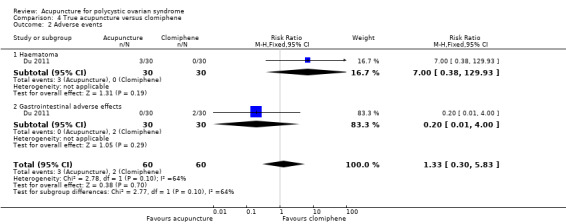
Summary of findings 2. Low‐frequency electroacupuncture compared to physical exercise or no intervention for polycystic ovarian syndrome.
| Low‐frequency electroacupuncture compared to physical exercise or no intervention for polycystic ovarian syndrome | |||||
| Patient or population: polycystic ovarian syndrome Setting: outpatient Intervention: low‐frequency electroacupuncture Comparison: physical exercise or no intervention | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with physical exercise or no intervention | Risk with low‐frequency electroacupuncture | ||||
| Live birth rate | No studies reported on live birth rate | ||||
| Multiple pregnancy rate | No studies reported on multiple pregnancy rate | ||||
| Ovulation rate | No studies reported on ovulation rate | ||||
| Restored regular menstrual period – low‐frequency electroacupuncture vs physical exercise | The mean restored menstruation frequency in the physical exercise group was 0.11 (SD 0.36). | The mean restored menstruation frequency in the low‐frequency electroacupuncture group was 0.33 (SD 0.37). | MD 0.22 higher (0.01 lower to 0.45 higher) | 40 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
| Restored regular menstrual period – low‐frequency electroacupuncture vs no intervention | The mean restored menstruation frequency in the no intervention group was –0.04 (SD 0.07) | The mean restored menstruation frequency in the low‐frequency electroacupuncture group was 0.33 (SD 0.37) | MD 0.37 higher (0.21 higher to 0.53 higher) | 31 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
| Adverse eventsc | Study population | RR 4.46 (0.77 to 25.78) | 201 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| 0 per 1000 | 0 per 1000 (0 to 0) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio; SD: standard deviation. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded two levels for high risk of performance bias and detection bias. bDowngraded two levels for imprecision ‐ single study with small sample size. cFive cases of adverse events were recorded in the low‐frequency electroacupuncture group and no adverse events were reported in the physical exercise or no intervention group.
Summary of findings 3. True acupuncture compared to relaxation for polycystic ovarian syndrome.
| True acupuncture compared to relaxation for polycystic ovarian syndrome | |||||
| Patient or population: polycystic ovarian syndrome Setting: outpatient Intervention: true acupuncture Comparison: relaxation | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with relaxation | Risk with true acupuncture | ||||
| Live birth rate | No studies reported on live birth rate | ||||
| Multiple pregnancy rate | No studies reported on multiple pregnancy rate | ||||
| Ovulation rate | The mean ovulation rate was 0 | MD 0.35 higher (0.14 higher to 0.56 higher) | — | 28 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
| Adverse events | No studies reported on adverse events | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded one level for high risk of performance bias. bDowngraded two levels for imprecision ‐ single study with small sample size.
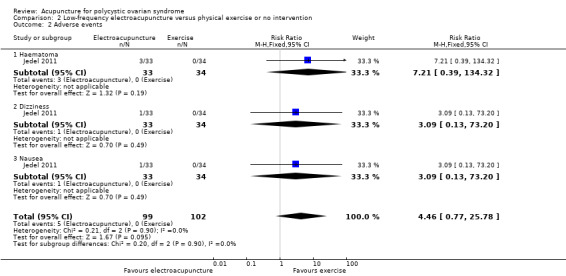
Summary of findings 4. True acupuncture compared to clomiphene for polycystic ovarian syndrome.
| True acupuncture compared to clomiphene for polycystic ovarian syndrome | |||||
| Patient or population: polycystic ovarian syndrome Setting: outpatient Intervention: true acupuncture Comparison: clomiphene | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with clomiphene | Risk with true acupuncture | ||||
| Live birth rate | No studies reported on live birth rate | ||||
| Multiple pregnancy rate | No studies reported on multiple pregnancy rate | ||||
| Ovulation rate | No studies reported on ovulation rate | ||||
| Restored regular menstrual period – restored menstruation at the end of treatment | Study population | RR 1.64 (0.94 to 2.85) | 60 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| 367 per 1000 | 601 per 1000 (345 to 1000) | ||||
| Restored regular menstrual period – restored menstruation 1 month after end of treatment | Study population | RR 1.50 (1.03 to 2.19) | 60 (1 RCT) | ⊕⊝⊝⊝ Very lowa,c | |
| 533 per 1000 | 800 per 1000 (549 to 1000) | ||||
| Adverse events | Study population | RR 1.33 (0.30 to 5.83) | 120 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| 33 per 1000 | 44 per 1000 (10 to 194) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded two levels for high risk of performance bias, detection bias, reporting bias and other bias. bDowngraded two levels for imprecision ‐ single study with small sample size and confidence intervals compatible with benefit in either arm or no effect. cDowngraded two levels for imprecision ‐ single study with small sample size.
Summary of findings 5. True acupuncture compared to Diane‐35 for polycystic ovarian syndrome.
| True acupuncture compared to Diane‐35 for polycystic ovarian syndrome | |||||
| Patient or population: polycystic ovarian syndrome Setting: outpatient Intervention: true acupuncture Comparison: Diane‐35 | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with Diane‐35 | Risk with true acupuncture | ||||
| Live birth rate | For women seeking symptom control, no fertility outcomes were measured. | ||||
| Multiple pregnancy rate | For women seeking symptom control, no fertility outcomes were measured. | ||||
| Ovulation rate | Study population | RR 1.45 (0.87 to 2.42) | 68 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | |
| 394 per 1000 | 571 per 1000 (343 to 953) | ||||
| Adverse events | Study population | RR 0.70 (0.25 to 1.99) | 360 (2 RCTs) | ⊕⊝⊝⊝ Very lowc,d | |
| 29 per 1000 | 20 per 1000 (7 to 57) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded two levels for high risk of performance bias, detection bias, attrition bias and other bias. bDowngraded two levels for imprecision ‐ single study with small sample size and confidence intervals compatible with benefit in either arm or no effect. cDowngraded two levels for high risk of performance bias, detection bias and attrition bias in two studies; additional high risk of other bias in one study. dDowngraded two levels for imprecision ‐ small sample size and confidence intervals compatible with benefit in either arm or no effect.
Background
Description of the condition
Polycystic ovarian syndrome (PCOS) is characterised by the clinical signs of oligo‐amenorrhoea (infrequent or very light menstruation), infertility (failure to conceive) and hirsutism (excessive hair growth). Biochemically, women with PCOS often show signs of hyperandrogenism (excessive production of androgen). They often have anovulatory infertility (failure to conceive due to no ovulation), and metabolic disorders (e.g. diabetes mellitus) (Wild 2000). In addition, PCOS can have substantial implications on a woman's psychological well‐being across the entire lifespan (Teede 2010). PCOS has become a major healthcare issue that deserves an increase in focus, from both clinical and public health perspectives.
Clinically, PCOS is one of the most common endocrine conditions seen in gynaecology and general endocrinology practice (Norman 2004). The diagnostic criteria for PCOS that we applied in this review were based on the Rotterdam Criteria established by the European Society of Human Reproduction and Embryology (ESHRE) and the American Society of Reproductive Medicine (ASRM) consensus in Rotterdam, 2003 (ESHRE/ASRM 2004). Any woman with at least two of the following three criteria were considered to have PCOS: ovulatory dysfunction (oligo‐ or anovulation), hyperandrogenaemia or polycystic ovaries on ultrasound evaluation; after the exclusion of other aetiologies of hyperandrogenism (excessive production of androgens such as androgen‐secreting tumours, hyperprolactinaemia, dysthyroid disease, Cushing's syndrome and congenital adrenal cortical hyperplasia).
In 2012, the prevalence rate of PCOS was between 6% and 10% based on the National Institute of Health criteria and was as high as 15% based on the Rotterdam criteria (Fauser 2012). Limited data are available regarding prevalence of this condition in Australia. One south Australian survey identified that 12% to 18% of women of reproductive age were affected (March 2010). National differences in prevalence rates exist, for example, one study showed a rate of 26% in the UK (Michelmore 1999). Results from these surveys are dependent on the protocol used. If the US criteria that do not consider ovarian morphology were adopted, the prevalence rate ranged from 4.5% to 11.2% from an unselected group of white and black Americans in a population‐based study in Alabama (Knochenhauer 1998). There was a prevalence rate of 9% in Greece (Diamanti‐Kandarakis 1999), and 6.5% in Spain (Asunicón 2000). The highest reported prevalence of PCOS was 52% among South Asian immigrants in the UK, of whom 49.1% had menstrual irregularities (Rodin 1998).
In traditional Chinese medicine, all diseases are classified into different syndromes (e.g. deficiency or excess) according to the person's clinical presentations (signs and symptoms). It is believed that kidney deficiency is the major concern relating to the reproductive function of women with PCOS (Ni 2007; Wang 2008).
Description of the intervention
Body acupuncture and ear acupuncture have been used as treatments for oligo/anovulatory women with PCOS. Body acupuncture involves stimulation of body acupuncture points through body needling using different sized sterile needles; while ear acupuncture involves points on the external ears that are stimulated either by needles or pellets. In randomised controlled trials (RCTs) of acupuncture, sham acupuncture is also known as placebo acupuncture. However, how sham acupuncture should be performed still remains controversial and can be different from study to study. The general principle of administering sham acupuncture is not to stimulate the actual acupuncture point with needles or electrostimulation.
Electroacupuncture is also known as electrostimulation. It is performed using stimulation with electrical impulses of acupuncture needles on selected acupuncture points.
Acupuncture is known to be a safe treatment. Transient adverse effects, such as skin erythema, bruising, bleeding and pain, are uncommon. Reports of significant complications are exceedingly rare. One observational study including more than 200,000 participants who received acupuncture for pain found an adverse event rate of 8.6% (Witt 2009). Another similar study estimated that the serious adverse event rate was between 0 and 1.1 per 10,000 treatments (MacPherson 2001).
Currently the first‐line pharmacological therapy for anovulatory infertility in women with PCOS is the administration of oral selective oestrogen receptor modulator such as clomiphene (Teede 2011). However, up to 40% of affected women show little clinical improvement with clomiphene therapy (Brown 2009). Other agents, such as insulin sensitisers, are used. This is based on the hypothesis that increasing insulin sensitivity reduces serum androgen levels thus improving fertility (Acbay 1996). Evidence suggests that metformin offers some improvement beyond clomiphene therapy (Tang 2012). Women resistant to these therapies can be further trialled on exogenous gonadotrophin preparations (ESHRE 1997). Alternatively, surgical options, such as laparoscopic ovarian drilling, can be explored (Gadir 1990). Women who respond to clomiphene therapy have higher risks of ovarian hyperstimulation syndrome and multiple pregnancy (Farhi 1996). Combined oral contraceptive pills such as Diane‐35 (ethinylestradiol and cyproterone acetate) are also used in women with PCOS to achieve symptom control. Oestrogen increases sex hormone binding globulin (SHBG) while progestin suppress luteinising hormone (LH) levels resulting in decreased production of androgen by the ovaries and decreased bioavailable androgen. This results in improvement in symptoms including hirsutism, acne and menstrual irregularity seen in women with PCOS. Thus, oral contraceptives are recommended as first‐line therapy for hirsutism, acne and menstrual abnormalities in women with PCOS (Legro 2013).
In recent years there has been extensive interest into non‐steroidal aromatase inhibitors such as letrozole. In anovulatory women, aromatase inhibitors downregulate oestrogen biosynthesis and reduce negative feedback to the hypothalamus, which leads to stronger gonadotropin‐releasing hormone (GnRH) pulses (Franik 2018). One Cochrane Review suggested a significant efficacy advantage to clomiphene, despite low to moderate quality of evidence (Franik 2018). Aromatase inhibitors are also free from adverse effects associated with antioestrogenic effects in the endometrium and cervix. Nevertheless, currently, use of such therapy is limited by low quality of supportive evidence.
How the intervention might work
Scientific studies have investigated the acupuncture meridians and the neuroendocrinological aspects of the meridians. Mayer 1977 proposed that acupuncture may stimulate the production of endorphin, an effect antagonised (counteracted) by the narcotic antagonist naloxone, in order to provide an analgesic effect. Ku 2001, Petti 1998, and Ulett 1998 have carried out further research in this area and postulated that beta‐endorphin and various neuropeptides (e.g. protein pro‐opiomelanocortin) within the nervous system may be implicated in producing the effects of acupuncture.
Aleem 1987 identified the presence of beta‐endorphin in the follicular fluid from both normal and polycystic ovaries. Petraglia 1987 demonstrated that the beta‐endorphin levels in ovarian follicular fluid of otherwise healthy women who were undergoing ovulation were much higher than the levels measured in plasma. Studies have shown that acupuncture decreases cortisol concentrations and modulates central and peripheral beta‐endorphin production and secretion, influencing the release of GnRH and gonadotrophin (Stener‐Victorin 2007). Different non‐randomised preliminary observational studies have shown that acupuncture may normalise the production of LH and follicle‐stimulating hormone (FSH) (Aso 1976; Cai 1997; Mo 1993). Chen 1991 considered that electroacupuncture has a role in normalising the hypothalamic‐pituitary ovarian axis, which in turn affects the menstruation cycle pattern. Clinically, the selection of acupuncture points is based on traditional Chinese medicine principles and can be variable.
Gerhard 1992 (in a case series) used ear acupuncture on 45 infertile women with dysfunction of ovulation and compared the treatment group with women receiving conventional medical treatment (e.g. dexamethasone, clomiphene citrate and gonadotropin). They concluded that the rate of return of menstruation was comparatively better in the ear acupuncture group despite no difference between the two groups on pregnancy rates.
Stener‐Victorin 2000 (in a case series) investigated its efficacy on ovulation induction in women with PCOS. Although the sample size was small (24 participants), two‐thirds of the women in the study reported a regular menstruation pattern for up to three months after cessation of the electroacupuncture treatment.
Why it is important to do this review
Women with PCOS seek both fertility and symptom control such as irregular menstrual cycles, amenorrhoea, insulin resistance, polycystic ovaries, androgen disturbance, hirsutism, acne, or a combination of these. Currently the main forms of treatment for women with PCOS are pharmacological‐based therapies such as clomiphene for fertility and the combined oral contraceptive pill for symptoms control (e.g. irregular menstrual cycles). However, pharmacological‐based therapies are also associated with different adverse effects.
Acupuncture is growing in popularity among western countries. Xue 2007 reported that 68.9% of the Australian population are users of complementary and alternative medicine, while 9.2% of the Australian population have used acupuncture according to a national population‐based survey performed in 2005. In the UK, a steady increase over time in the utilisation of acupuncture was reported from 3 million per year in 2001 to about 4 million in 2012 (Hopton 2012; Thomas 2001). In the USA, the number of acupuncture users increased by 50% over the 10‐year period from 2002 to 2012 (Cui 2017).
Previously there was uncertainty regarding the efficacy of acupuncture for oligo/anovulatory women with PCOS due to absence of RCTs and systematic reviews. This present review will contribute to the clinical knowledge in this area by summarising currently available knowledge. From a clinical point of view, the management of PCOS has been an evolving area where current paradigms were continuously challenged with novel modalities. This review aimed to address both women with PCOS who seek fertility and those that seek symptom control. This is an update of a Cochrane Review first published in 2011, which aimed to provide an objective basis for healthcare practitioners to recommend acupuncture treatment for women where complementary therapy may be appropriate.
Objectives
To assess the effectiveness and safety of acupuncture treatment for oligo/anovulatory women with polycystic ovarian syndrome (PCOS) for both fertility and symptom control.
Methods
Criteria for considering studies for this review
Types of studies
RCTs studying the efficacy of acupuncture treatment for oligo/anovulation in women with PCOS. We excluded quasi‐, pseudo‐ or non‐RCTs. We excluded cross‐over trials unless first‐phase data were available.
Types of participants
Women of reproductive age (18 to 44 years) with PCOS and oligo/anovulation. We included both women who sought fertility and those that sought symptom control.
The diagnostic criteria of PCOS applied in this review were based on the ESHRE and ASRM consensus in Rotterdam in 2003 (ESHRE/ASRM 2004). We considered any woman with any two of the three listed criteria as having PCOS. After the exclusion of other aetiologies of hyperandrogenism (such as androgen‐secreting tumour, hyperprolactinaemia, dysthyroid disease, Cushing's syndrome and congenital adrenal cortical hyperplasia), these were the presence of:
oligo or anovulation;
hyperandrogenaemia or
polycystic ovaries.
Ideally the diagnostic criteria for PCOS should have been stated and described in trials selected for this review. If the trials did not use the Rotterdam consensus, the review authors evaluated the diagnostic criteria for each individual study to confirm whether they met the Rotterdam consensus. If the diagnostic criteria were not clearly stated, we contacted the trial authors to obtain clarification. Where clarification was not available, we excluded the trials. Differences in diagnostic criteria may produce variability in the clinical characteristics of the women included and the results obtained. We had planned to consider, document and explore these changes in a sensitivity analysis.
Types of interventions
Acupuncture, including body needling and low‐frequency electroacupuncture, was the main intervention.
Eligible comparators were placebo, no intervention, lifestyle intervention and conventional treatment of PCOS (e.g. clomiphene citrate).
Sham acupuncture is also known as placebo acupuncture and uses techniques that are not intended to stimulate known acupuncture points. Normally it is used for the control group in a RCTs of acupuncture.
We excluded clinical trials using Chinese herbal medicine for the management of PCOS from this review because it is assessed in another Cochrane Review (Zhang 2010). We also excluded clinical trials that included ovarian wedge resection as the control intervention because this method is no longer applied by surgeons since the development of laparoscopic ovarian drilling.
Types of outcome measures
Primary outcomes
Live birth rate (defined as delivery of live foetus after 20 completed weeks of gestation) – for women seeking fertility.
Multiple pregnancy rate (defined as more than one intrauterine pregnancy) – for women seeking fertility.
Ovulation rate (as determined by ultrasound or increased progesterone) – for women seeking symptom control.
Secondary outcomes
Clinical pregnancy rate (defined as evidence of gestational sac or foetal heart motion, confirmed with ultrasound).
Restored regular menstrual period (as defined by study authors, including rate or continuous measurements).
Miscarriage rate (loss of intrauterine pregnancy before 20 completed weeks of gestation).
Adverse events (as defined by study authors).
Search methods for identification of studies
We developed a comprehensive search strategy to identify all RCTs regardless of language or publication status (published, unpublished, in press or in progress).
Electronic searches
We identified relevant studies from:
the Gynaecology and Fertility Group Specialised Register (searched 22 May 2018);
CENTRAL via the Cochrane Central Register of Studies Online (CRSO) (searched 22 May 2018);
Ovid MEDLINE (searched from 1946 to 22 May 2018);
Ovid Embase (searched from 1980 to 22 May 2018);
Ovid PsycINFO (searched from 1806 to 22 May 2018);
Ovid AMED (searched from 1985 to 22 May 2018);
Chinese National Knowledge Infrastructure (CNKI; including the Chinese journal full‐text database (CJFD), China's important Conference Papers Database and China dissertation database) (searched from 2010 to 24 May 2018);
Chinese BioMedical Literature Database (CBM) (searched from 2010 to 21 November 2015);
VIP database for Chinese Technical Periodicals (searched from 2010 to 24 May 2018).
We combined the MEDLINE search with the Cochrane highly sensitive search strategy for identifying randomised trials, which appears in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We combined the Embase search with trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (www.sign.ac.uk/search‐filters.html).
We constructed search strategies by using a combination of subject headings and text words relating to the use of acupuncture for the management of PCOS (Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7; Appendix 8; Appendix 9). All the terms were translated into Chinese for the searches in Chinese databases to be conducted. There was no language restriction in these searches.
We searched trial registers for ongoing and registered trials on 22 May 2018: ClinicalTrials.gov, a service of the US National Institutes of Health (clinicaltrials.gov/ct2/home); the World Health Organization International Trials Registry Platform search portal (www.who.int/trialsearch/Default.aspx); the Australian and New Zealand Clinical Trial Registry (www.anzctr.org.au/Default.aspx) (Appendix 10); and Chinese Clinical Trial Registry (www.chictr.org.cn/).
Searching other resources
We checked the reference lists of relevant trials, reviews and textbooks.
Data collection and analysis
Selection of studies
In this update, two review authors (RN, GZ) performed the searches and retrieved the articles. We retrieved and reviewed all studies that claimed to be randomised and had not already been reviewed as part of earlier versions of this review. We judged trials as adequately randomised if they met the set criteria (Higgins 2011).
Data extraction and management
In this update, two review authors (RN, GZ) independently extracted data using a piloted data extraction form, which included details of methods, participants, interventions and outcomes. All studies were then assessed independently and any dispute was resolved by a third independent review author (HC).
Assessment of risk of bias in included studies
We assessed the methodological quality using the six domains described in Cochrane's tool for assessing risk of bias (Figure 1; Figure 2):
1.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
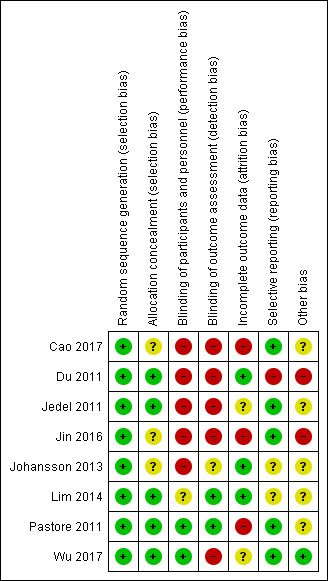
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting;
other sources of bias.
Measures of treatment effect
We used risk ratio (RR) to measure binary outcomes. For continuous outcomes, we used mean difference (MD) if the studies used same measurement scales. If studies used different scales, we used the standardised mean difference (SMD). We calculated 95% confidence intervals (CI) for all outcomes.
Unit of analysis issues
The unit of analysis was the woman for all outcomes.
Dealing with missing data
We analysed the data on an intention‐to‐treat (ITT) basis as far as possible (i.e. including all randomised participants in analysis, in the groups to which they were randomised). Where data were not obtainable, we analysed only the available data.
Assessment of heterogeneity
We assessed heterogeneity using the Chi2 test (with a 10% level of statistical significance). We planned to use the I2 statistic to estimate the total variation across studies, with less than 25% considered as low‐level heterogeneity; 25% to 50% as moderate level and greater than 50% as a high level of heterogeneity (Higgins 2002). In addition, we scanned forest plots visually for evidence of heterogeneity (non‐overlapping CIs). We planned further investigation such as subgroup analysis to be carried out to consider possible causes of any heterogeneity. In addition, we planned to use a random‐effects model if statistical heterogeneity was evident from the formal tests.
Assessment of reporting biases
We planned to assess publication bias using a funnel plot, if there were sufficient studies (at least 10) in one analysis.
Data synthesis
If the studies were sufficiently similar, we combined the data using a fixed‐effect model. Comparisons included in this review were:
true acupuncture versus sham acupuncture;
low‐frequency electroacupuncture versus physical exercise or no intervention;
true acupuncture versus lifestyle intervention (relaxation);
true acupuncture versus conventional treatment (clomiphene);
true acupuncture versus conventional treatment (Diane‐35).
Subgroup analysis and investigation of heterogeneity
If there is a sufficient number of RCTs for inclusion in the review in future updates, we plan to conduct a subgroup analysis to explore sources of heterogeneity. We plan to base subgroups on differences observed, for example, content of acupuncture prescription or clinical differences between participants.
Sensitivity analysis
We planned to conduct sensitivity analyses for the primary outcomes to determine whether the conclusions were robust to arbitrary decisions made regarding the eligibility and analysis. These analyses included consideration of whether the review conclusions would have differed if:
eligibility had been restricted to studies at low risk of bias, defined as studies at low risk of selection bias and not at high risk of bias in any domain;
a fixed‐effect model had been adopted;
alternative imputation strategies had been implemented;
the summary effect measure had been RR rather than odds ratio.
Sensitivity analyses was not conducted for this review due to insufficient number of studies.
Quality of the evidence: 'Summary of findings' table
We presented 'Summary of findings tables' using GRADEpro and Cochrane methods. One table evaluated the overall quality of the body of evidence for the main review outcomes (live birth rate, multiple pregnancy rate, ovulation rate, clinical pregnancy rate, restored regular menstrual period, miscarriage rate and adverse events) for the main review comparison (true acupuncture compared to sham acupuncture).
Additional 'Summary of findings' tables were prepared for the main review outcomes for other important comparisons (low‐frequency electroacupuncture compared to physical exercise or no intervention, true acupuncture compared to relaxation, true acupuncture compared to clomiphene, and true acupuncture compared to Diane‐35). We assessed the quality of the evidence using GRADE criteria: risk of bias, consistency of effect, imprecision, indirectness and publication bias). Two review authors (RN, GZ) independently made judgements about evidence quality (high, moderate, low or very low) and resolved disagreements by discussion. Judgements were justified, documented and incorporated into reporting of results for each outcome. We extracted study data, formatted our comparisons in data tables and prepared 'Summary of findings' tables before writing the results and conclusions of our review.
Results
Description of studies
Results of the search
The initial search combined with the new updated search identified 1263 articles from databases and registers specified in the Methods section. After screening and removal of duplicates, we assessed 44 full‐text articles for eligibility. We excluded other articles on the basis of their titles or abstracts because they did not meet the inclusion criteria. After screening the full text of the selected articles, 13 articles met the inclusion criteria. Five RCTs were included in our previous review (Du 2011; Jedel 2011; Johansson 2013; Lim 2014; Pastore 2011). Three new studies (seven articles) were included in this version of the review (Cao 2017; Jin 2016; Wu 2017). Five articles were publications relating to the same study (Wu 2017). Thus, we included eight RCTs in this review (Figure 3).
3.
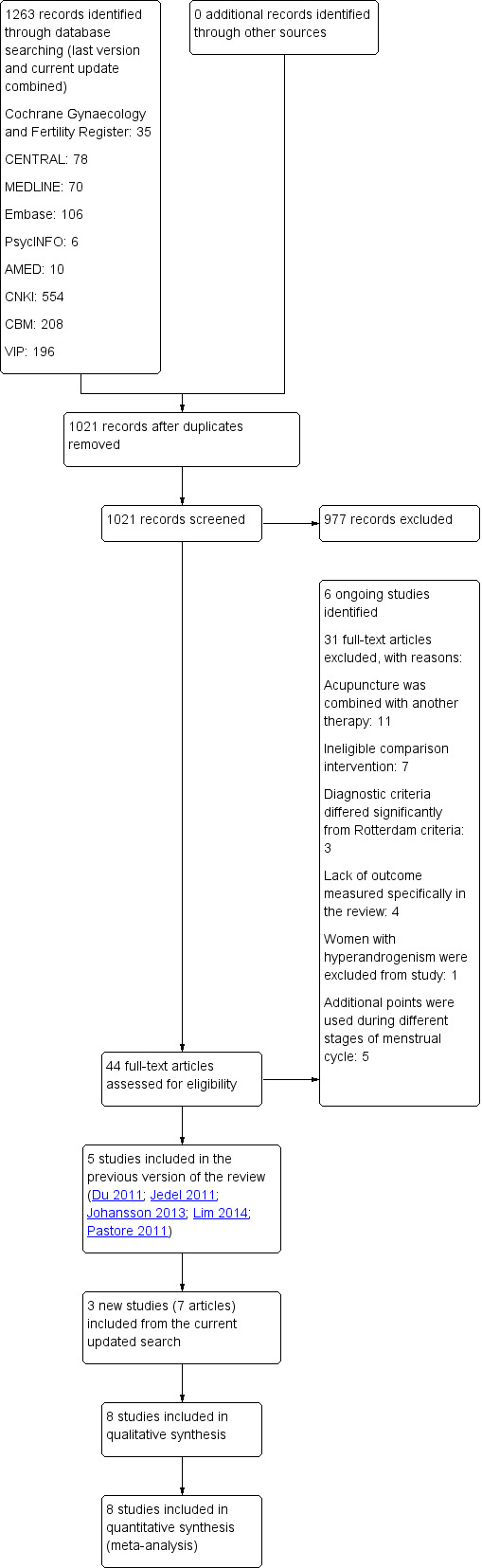
Study flow diagram. PCOS: polycystic ovarian syndrome.
Included studies
See Characteristics of included studies table.
Study design
We included eight RCTs in this review. One multicentre, two‐arm parallel study was conducted in Australia and China (Lim 2014); one single‐centre, three‐arm parallel study was conducted in Sweden (Jedel 2011); one single‐centre, two‐arm parallel study was conducted in the US (Pastore 2011); three single‐centre, two‐arm parallel studies conducted in China (Cao 2017; Du 2011; Jin 2016), one single‐centre, two‐arm parallel trial was conducted in Sweden (Johansson 2013), and one multicentre, 2 × 2 factorial trial was conducted in China (Wu 2017).
Participants
The trials included 1546 women with PCOS. This included 1418 women who were seeking fertility (Du 2011; Jedel 2011; Johansson 2013; Lim 2014; Pastore 2011; Wu 2017), and 128 women who were seeking symptom control (Cao 2017; Jin 2016). Cao 2017 included 56 participants; Du 2011 included 60 participants; Jedel 2011 included 84 participants; Jin 2016 included 72 participants; Johansson 2013 included 32 participants; Lim 2014 included 146 participants; Pastore 2011 included 96 participants; and Wu 2017 included 1000 participants. All participants had a diagnosis of PCOS made on the basis of Rotterdam consensus, which included either ultrasound or presence of oligo‐amenorrhoea and hyperandrogenism, or both. Two studies included additional diagnoses based on Chinese medicine principles (Du 2011; Lim 2014).
The main inclusion criteria were:
ultrasound‐verified polycystic ovaries with 10 or 12 follicles of 2 mm to 9 mm or an ovarian volume of 10 mL in one or both ovaries, or both (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Johansson 2013; Lim 2014; Wu 2017);
presence of oligo‐amenorrhoea and hyperandrogenism (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Lim 2014; Pastore 2011; Wu 2017);
kidney yang deficiency syndrome as per Chinese medicine diagnosis (Lim 2014);
traditional Chinese medicine diagnosis of menstrual irregularity, amenorrhoea and infertility (Du 2011).
The main exclusion criteria were:
any pharmacological treatment including Chinese herbal prescriptions or breastfeeding in period prior to entering study (Cao 2017; Jedel 2011; Jin 2016; Johansson 2013; Lim 2014; Wu 2017);
diabetes mellitus, and endocrine or neoplastic causes of hyperandrogenaemia, including Cushing's syndrome, congenital adrenal hyperplasia and hyperprolactinaemia (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Johansson 2013; Pastore 2011; Wu 2017);
aged below 18 years (Cao 2017; Jin 2016; Lim 2014), or above 35 years (Jin 2016); above 38 years (Johansson 2013); or above 45 years (Cao 2017).
abnormal full blood count, renal or liver function tests (Cao 2017; Jin 2016; Lim 2014);
pregnancy within the past six weeks or within six weeks postabortion or postpartum (Wu 2017).
There were no significant differences between baseline characteristics of all studies (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Johansson 2013; Lim 2014; Pastore 2011; Wu 2017).
Interventions
Five studies compared true acupuncture versus sham acupuncture (Cao 2017; Jin 2016; Johansson 2013; Lim 2014; Pastore 2011; Wu 2017). Jin 2016, Johansson 2013, Pastore 2011, Cao 2017, and Wu 2017 used a combination of manual stimulation and low‐frequency electroacupuncture at specified acupuncture points in the intervention group. Lim 2014 used body needling with manual stimulation only. Two different sets of acupuncture points were used alternately in Johansson 2013 and Wu 2017. In Johansson 2013, participants allocated to the control group received relaxation sessions of equal length with the same therapist. Wu 2017 was a 2 × 2 factorial study that used clomiphene citrate as the second main intervention. Participants were therefore allocated to active acupuncture plus clomiphene, active acupuncture plus placebo, control acupuncture plus clomiphene and control acupuncture plus placebo. Participants who received clomiphene and placebo were pooled in both arms of the meta‐analysis.
One study assessed low‐frequency electroacupuncture and physical exercise (Jedel 2011). Women in the acupuncture intervention group met regularly with researchers to receive treatment and women who received physical exercise only met once with researchers and received weekly telephone calls. There was a third arm to this study of no active intervention where women received telephone information only.
One study compared acupuncture with conventional treatment with clomiphene (Du 2011). In this study, the acupuncture group received three cycles of the monthly acupuncture regimen. The comparison group received clomiphene 50 mg daily for five days. In both groups, treatment was given on the fifth day after beginning of menstruation. In the case of amenorrhoea, progesterone was used to induce withdrawal bleeding before treatment was given in either group.
Two studies compared acupuncture versus Diane‐35 (ethinylestradiol and cyproterone acetate tablets) (Cao 2017; Jin 2016). In Cao 2017, the acupuncture group received continuous twice weekly acupuncture treatment for 12 weeks; while in Jin 2016, the treatments were given three times weekly for three months. The comparison group received three cycles of Diane‐35, one tablet daily for 21 days and a seven‐day break. Both groups received treatment on the fifth day after beginning of menstruation or withdrawal bleeding.
Outcomes
Primary outcomes
Live birth rate
One study reported live birth rates (Wu 2017).
Multiple pregnancy rate
One study reported multiple pregnancy rate (Wu 2017).
Ovulation rate
Five studies reported ovulation rate (Du 2011; Jin 2016; Johansson 2013; Pastore 2011; Wu 2017).
Secondary outcomes
Clinical pregnancy rate
Three studies reported clinical pregnancy rate (Lim 2014; Pastore 2011; Wu 2017). Ascertainment of pregnancy was by participant self‐report in Lim 2014 and Pastore 2011. One trial measured serum human chorionic gonadotropin concentration and confirmed pregnancy with pelvic ultrasound (Wu 2017).
Restored regular menstrual period
Five studies reported restored regular menstrual period (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Lim 2014).
Miscarriage rate
One study reported miscarriage rate (Wu 2017).
Adverse events
Six studies reported adverse events secondary to treatment (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Pastore 2011; Wu 2017). The other studies did not report adverse events (Johansson 2013; Lim 2014).
Excluded studies
We excluded 31 studies after evaluation of the full‐text articles. See Characteristics of excluded studies table.
Risk of bias in included studies
Allocation
Sequence generation
All studies described adequate methods of randomisation (computer generated) and were at low risk of bias (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Johansson 2013; Lim 2014; Pastore 2011; Wu 2017).
Allocation concealment
Johansson 2013, Jin 2016, and Cao 2017 did not describe allocation concealment and were at unclear risk of bias. Du 2011 concealed allocation in opaque envelopes that were distributed sequentially and was at low risk of bias. The other four studies were at low risk of bias as they adequately described method of concealment including use of sealed, opaque envelopes (Lim 2014; Pastore 2011), preprinted barcode labels (Wu 2017), or concealing until interventions were assigned (Jedel 2011).
Blinding
Blinding of participants and personnel (performance bias)
Pastore 2011 reported blinding of the participants and principal investigator (low risk of bias). Wu 2017 reported blinding of participants in the acupuncture arm and blinding of participants and study investigators in the clomiphene and placebo group (low risk of bias).
Lim 2014 reported blinding of participants only (unclear risk of bias).
Cao 2017, Du 2011, Jedel 2011, and Jin 2016 did not report any blinding methods (high risk of bias).
Johansson 2013 did not blind participants or therapists in the study due to the nature of the intervention and the control in the study (high risk of bias).
Blinding of outcome assessment (detection bias)
Cao 2017, Du 2011, Jedel 2011, Jin 2016, and Wu 2017 did not report any blinding methods used (high risk of bias).
Johansson 2013 reported biological outcomes were measured at an independent laboratory and investigators were blinding until statistical analyses; however, it was unclear if investigators were blinded during statistical analyses (unclear risk of bias).
Outcome assessment was completed by statisticians independent to the study in Lim 2014 (low risk of bias).
Pastore 2011 reported blinding of clinical research co‐ordinator and biostatistician (low risk of bias).
Incomplete outcome data
Eleven of 96 women dropped out during the intervention phase in Pastore 2011 with no age, education, body‐mass index (BMI) or race difference between the dropouts and the remainder of the cohort. One woman entered menopausal transition during the trial and was also excluded. The trial did not report number of women lost to follow‐up. There was no ITT analysis (high risk of bias).
Lim 2014 excluded four out of 146 women between enrolment and randomisation phase. There were no dropouts during intervention phase reported. They reported reasons for excluding the women (low risk of bias).
Jedel 2011 reported 10 dropouts between allocation and baseline assessments, 15 between baseline and week 16 and nine between weeks 16 and 32. They conducted an ITT analysis on the 74 participants who went through baseline assessments. They did not report a comparison of baseline characteristics of dropouts and women remaining in the trial (unclear risk of bas).
Johansson 2013 reported five dropouts after randomisation. In the active treatment arm, four women were excluded before baseline assessment and one woman was lost before final assessment. ITT analysis was performed of 12 women from the treatment arm and all 16 women from the control arm. The authors described reasons for dropouts adequately in the published reports (low risk of bias).
Du 2011 reported that all participants completed the study (low risk of bias).
Four women out of 56 dropped out during the intervention phase in Cao 2017, and four out of 72 dropped out during the intervention phase in Jin 2016. The difference between age, BMI or clinical feature of the dropouts and the remainder of the cohort was not performed. There was no ITT analysis (high risk of bias).
Wu 2017 reported four participants who conceived after randomisation and before intervention commenced. These women completed the last visit and were included in the primary analysis. During the intervention phase, 74 participants dropped out from the study. Fifteen participants dropped out from the active acupuncture and clomiphene arm; 14 participants dropped out from the control acupuncture and clomiphene arm; 27 participants dropped out from the active acupuncture and placebo arm and 18 participants dropped out from the control acupuncture and placebo arm. Out of the 14 participants who dropped out from the control acupuncture and clomiphene arm, two were due to intervention adverse effects. Out of the 27 participants who dropped out from the active acupuncture and placebo arm, three were due to intervention adverse effects. There was no ITT analysis. The authors described reasons for dropouts adequately in the published reports (unclear risk of bias).
Selective reporting
Two studies did not report adverse events in their published reports and were at unclear risk of bias (Johansson 2013; Lim 2014). Du 2011 did not report the number of women who had no ovulation during treatment period (high risk of bias). The remaining studies reported all listed outcomes (low risk of bias).
Other potential sources of bias
We identified no other potential sources of bias in four studies (Cao 2017; Jedel 2011; Johansson 2013; Lim 2014; Pastore 2011). Jin 2016 and Du 2011 are both unpublished studies from thesis. We graded them at high risk of bias for possible lack of adequate peer review. Wu 2017 was supported by various government and non‐government grants. One author in the study reported conflict of interest due to grant funding. They reported that funding agencies had no role in the design or conduct of the study (low risk of bias).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
We examined two populations in this review – women seeking fertility (comparisons 1, 2, 3 and 4) and women seeking symptom control (comparison 5 True acupuncture versus conventional treatment Diane‐35).
1 True acupuncture versus sham acupuncture
Three studies compared true acupuncture versus sham acupuncture (Lim 2014; Pastore 2011; Wu 2017).
Primary outcomes
Live birth rate
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in live birth (RR 0.97, 95% CI 0.76 to 1.24; 1 RCT, 926 women; low‐quality evidence; Analysis 1.1; Wu 2017). This means, low‐quality evidence suggested that if 22% of women achieved live birth with sham acupuncture, between 17% and 28% would achieve live birth with true acupuncture.
1.1. Analysis.
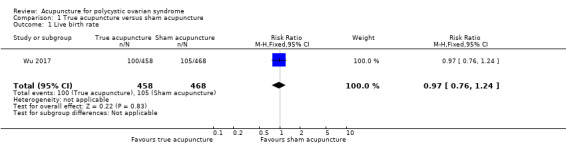
Comparison 1 True acupuncture versus sham acupuncture, Outcome 1 Live birth rate.
Multiple pregnancy rate
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in multiple pregnancy rate (RR 0.89, 95% CI 0.33 to 2.45; 1 RCT, 926 women; low‐quality evidence; Analysis 1.2; Wu 2017). This means, low‐quality evidence suggested that if 2% of women achieved multiple pregnancy with sham acupuncture, between 0.6% and 4% would achieve multiple pregnancy with true acupuncture.
1.2. Analysis.
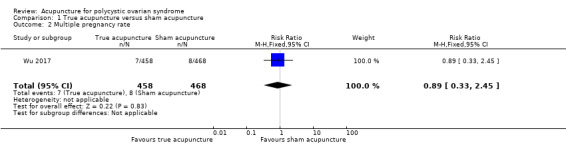
Comparison 1 True acupuncture versus sham acupuncture, Outcome 2 Multiple pregnancy rate.
Ovulation rate
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in ovulation rate (SMD 0.02, 95% CI –0.15 to 0.19; I2 = 0%; 2 RCTs, 1010 women; low‐quality evidence; Analysis 1.3; Figure 4; Pastore 2011; Wu 2017).
1.3. Analysis.
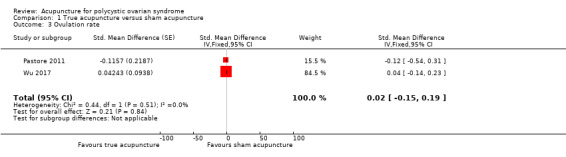
Comparison 1 True acupuncture versus sham acupuncture, Outcome 3 Ovulation rate.
4.
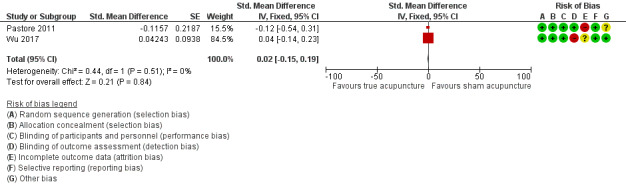
Forest plot of comparison: 1 True acupuncture versus sham acupuncture, outcome: 1.3 Ovulation rate.
Secondary outcomes
Clinical pregnancy rate
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in clinical pregnancy rate (RR 1.03, 95% CI 0.82 to 1.29; I2 = 0%; 3 RCTs, 1117 women; low‐quality evidence; Analysis 1.4; Figure 5; Lim 2014; Pastore 2011; Wu 2017). This means, low‐quality evidence suggested that if 21% of women achieved clinical pregnancy with sham acupuncture, between 17% and 27% would achieve clinical pregnancy with true acupuncture.
1.4. Analysis.
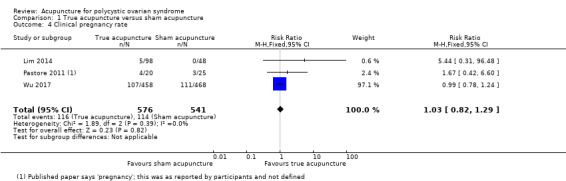
Comparison 1 True acupuncture versus sham acupuncture, Outcome 4 Clinical pregnancy rate.
5.
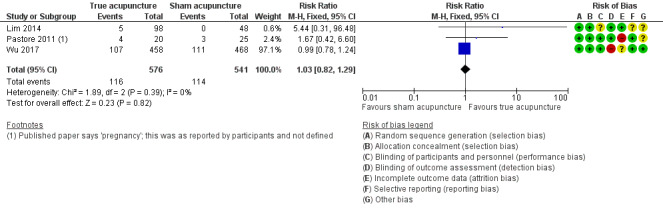
Forest plot of comparison: 1 True acupuncture versus sham acupuncture, outcome: 1.4 Clinical pregnancy rate.
Restored regular menstrual period
Lim 2014 reported difference in intermenstrual days pre and post treatment. Number of intermenstrual days may have improved in participants receiving true acupuncture compared to sham acupuncture (MD –312.09 days, 95% CI –344.59 to –279.59; 1 RCT, 141 women; low‐quality evidence; Analysis 1.5; Lim 2014).
1.5. Analysis.
Comparison 1 True acupuncture versus sham acupuncture, Outcome 5 Restored regular menstrual period.
Miscarriage rate
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in miscarriage rate (RR 1.10, 95% CI 0.77 to 1.56; 1 RCT, 926 women; low‐quality evidence; Analysis 1.6; Wu 2017). This means, low‐quality evidence suggested that if 11% of women had a miscarriage with sham acupuncture, between 9% and 18% would have a miscarriage with true acupuncture.
1.6. Analysis.
Comparison 1 True acupuncture versus sham acupuncture, Outcome 6 Miscarriage rate.
Adverse events
All three studies reported adverse events. True acupuncture probably worsened adverse events compared to sham acupuncture (RR 1.16, 95% CI 1.02 to 1.31; I2 = 0%; 3 RCTs, 1230 women; moderate‐quality evidence; Analysis 1.7; Figure 6; Lim 2014; Pastore 2011; Wu 2017). This means, moderate‐quality evidence suggested that if 40% of women had adverse events with sham acupuncture, between 41% and 52% of women had adverse events with true acupuncture.
1.7. Analysis.
Comparison 1 True acupuncture versus sham acupuncture, Outcome 7 Adverse events.
6.
Forest plot of comparison: 1 True acupuncture versus sham acupuncture, outcome: 1.7 Adverse events.
Pastore 2011 reported one adverse event (back muscle spasm) and Lim 2014 found no adverse events (based on unpublished data). Wu 2017 reported 99 adverse events in 500 women who received true acupuncture compared to 55 adverse events in 500 women who received sham acupuncture before conception. The most common adverse events in the true acupuncture group were bruising and diarrhoea. One participant with liver dysfunction and one participant with fracture of coccyx were reported in the true acupuncture plus Clomiphene group. Among participants who conceived there were 174 adverse events in 159 women in the true acupuncture group compared to 182 adverse events in 161 women in the sham acupuncture group. The most common adverse events in the true acupuncture group were oedema and threatened abortion. In terms of serious adverse effects, there were two participants with ectopic pregnancy, two participants with late abortion, seven participants with preterm labour, eight participants with gestational diabetes, one participant with severe pre‐eclampsia, three participants with placenta previa and one participant with preterm labour.
2 Low‐frequency electroacupuncture versus lifestyle intervention (physical exercise) or no intervention
Jedel 2011 compared low‐frequency electroacupuncture to physical exercise or no intervention.
Primary outcomes
Live birth rate
No studies reported live birth rate.
Multiple pregnancy rate
No studies reported multiple pregnancy rate.
Ovulation rate
No studies reported ovulation rate.
Secondary outcomes
Clinical pregnancy rate
No studies reported pregnancy rate.
Restored regular menstrual period
Jedel 2011 reported difference in menstrual frequency before and after treatment. In this study, one menstruation per month was defined as a menstrual frequency of 1.0. We were uncertain whether low‐frequency electroacupuncture improved menstruation frequency at 32 weeks in women who received low‐frequency electroacupuncture compared to physical exercise (MD 0.22, 95% CI –0.01 to 0.45; 1 RCT, 40 women; very low‐quality evidence). We were uncertain whether low‐frequency electroacupuncture improved menstrual frequency at 32 weeks compared to no intervention (MD 0.37, 95% CI 0.21 to 0.53; 1 RCT, 31 women; very low‐quality evidence; Analysis 2.1).
2.1. Analysis.
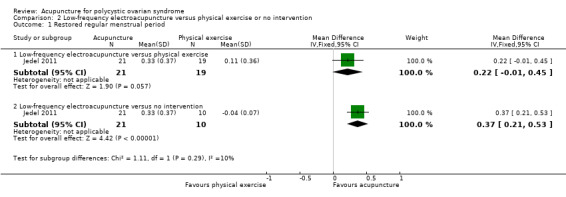
Comparison 2 Low‐frequency electroacupuncture versus physical exercise or no intervention, Outcome 1 Restored regular menstrual period.
Miscarriage rate
No studies reported miscarriage rate.
Adverse events
There were three cases of skin erythema, one case of dizziness and one case of nausea following low‐frequency electroacupuncture. No other short‐term or long‐term adverse events were reported in either physical exercise group or no intervention group (Analysis 2.2).
2.2. Analysis.
Comparison 2 Low‐frequency electroacupuncture versus physical exercise or no intervention, Outcome 2 Adverse events.
3 True acupuncture versus lifestyle intervention (relaxation)
Johansson 2013 compared true acupuncture on a twice weekly regimen to relaxation sessions at the same settings.
Primary outcomes
Live birth rate
No studies reported live birth rate.
Multiple pregnancy rate
No studies reported multiple pregnancy rate.
Ovulation rate
We were uncertain whether true acupuncture improved ovulation frequency (defined as ovulations per month) compared to relaxation (MD 0.35, 95% CI 0.14 to 0.56; 1 RCT, 28 women; very low‐quality evidence; Analysis 3.1).
3.1. Analysis.
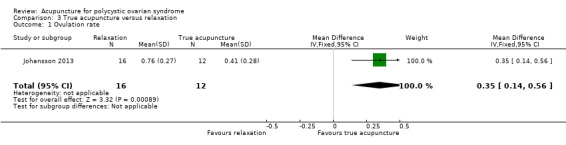
Comparison 3 True acupuncture versus relaxation, Outcome 1 Ovulation rate.
Secondary outcomes
Clinical pregnancy rate
No studies reported pregnancy rate. One participant in Johansson 2013 became pregnant before baseline assessment and she was not included in the ITT analysis.
Restored regular menstrual period
No studies reported restored regular menstrual period.
Miscarriage rate
No studies reported miscarriage rate.
Adverse events
No studies reported adverse events.
4 True acupuncture versus conventional treatment (clomiphene)
Du 2011 compared true acupuncture to conventional treatment (clomiphene).
Primary outcomes
Live birth rate
No studies reported live birth rate.
Multiple pregnancy rate
No studies reported multiple pregnancy rate.
Ovulation rate
No studies reported ovulation rate. Du 2011 reported number of ovulations during treatment. However, we could not calculate ovulation rate because the number of women who had no ovulation was not reported. Du 2011 did not report ovulation during the follow‐up period.
Secondary outcomes
Clinical pregnancy rate
No studies reported pregnancy rate.
Restored regular menstrual period
We were uncertain whether true acupuncture improved restored regular menstrual period compared to clomiphene. Du 2011 reported restoration of menstruation at the end of treatment and one month after the end of treatment. During treatment, 14/30 women from the acupuncture group reported restored menstruation, defined as three normal menstruations during three months. Eleven out of 30 women in the clomiphene group reported restored menstruation at the end of treatment (RR 1.64, 95% CI 0.94 to 2.85; 1 RCT, 60 women; very low‐quality evidence; Analysis 4.1). This means, very low‐quality evidence suggested that if 37% of women achieved restored menstruation at end of treatment with clomiphene, between 34% and 100% would achieve restored menstruation at end of treatment with true acupuncture. At one month after treatment, 24/30 women in the acupuncture group reported normal menstruation while 16/30 women in the clomiphene group reported normal menstruation (RR 1.50, 95% CI 1.03 to 2.19; 1 RCT, 60 women; very low‐quality evidence; Analysis 4.1). This means, very low‐quality evidence suggested that if 53% of women achieved normal menstruation at one after treatment with clomiphene, between 55% and 100% would achieve normal menstruation at one month with true acupuncture.
4.1. Analysis.

Comparison 4 True acupuncture versus clomiphene, Outcome 1 Restored regular menstrual period.
Miscarriage rate
No studies reported miscarriage rate.
Adverse events
Du 2011 reported three cases of mild subcutaneous haematoma in the acupuncture group. There were two cases of minor gastrointestinal adverse effects in the clomiphene group (Analysis 4.2).
4.2. Analysis.
Comparison 4 True acupuncture versus clomiphene, Outcome 2 Adverse events.
5 True acupuncture versus conventional treatment (Diane‐35)
Cao 2017 and Jin 2016 compared acupuncture to Diane‐35. The focus population in this comparison was women seeking symptom control.
Primary outcomes
Live birth rate
For women seeking symptom control, no fertility outcomes were measured.
Multiple pregnancy rate
For women seeking symptom control, no fertility outcomes were measured.
Ovulation rate
We were uncertain whether true acupuncture improved ovulation rate compared to Diane‐35 (RR 1.45, 95% CI 0.87 to 2.42; 1 RCT, 58 women; very low‐quality evidence; Analysis 5.1; Jin 2016). This means, very low‐quality evidence suggested that if 39% of women achieved ovulation with Diane‐35, between 34% and 95% would achieve ovulation with true acupuncture. Ovulation was measured by ultrasound three months after treatment.
5.1. Analysis.

Comparison 5 True acupuncture versus Diane‐35, Outcome 1 Ovulation rate.
Secondary outcomes
Clinical pregnancy rate
For women seeking symptom control, no fertility outcomes were measured. However, Jin 2016 observed that two participants in the acupuncture group reported pregnancy and were subsequently withdrawn from the study.
Restored regular menstrual period
We were uncertain whether true acupuncture restored regular menstrual period compared to Diane‐35.
Quantitative meta‐analysis of data was not possible due to heterogeneity in, and reporting of, outcomes.
We were uncertain whether true acupuncture improved menstrual restoration rate three months after end of treatment compared to Diane‐35 (RR 1.27, 95% CI 0.92 to 1.77; 1 RCT, 68 women; very low‐quality evidence; Jin 2016). This means, very low‐quality evidence suggested that if 61% of women achieved menstrual restoration three months after end of treatment with Diane‐35, between 56% and 107% would achieve menstrual restoration three months after the end of treatment with true acupuncture.
We were uncertain whether true acupuncture improved menstrual frequency within three months before and after treatment compared to Diane‐35 (MD –0.77, 95% CI –1.20 to –0.34; one RCT, 52 women; very low‐quality evidence; Cao 2017).
We were uncertain whether true acupuncture improved menstrual duration within three months before and after treatment compared to Diane‐35 (MD –0.71, 95% CI –3.48 to 2.06; one RCT, 52 women; very low‐quality evidence; Cao 2017).
Miscarriage rate
No studies reported miscarriage rate.
Adverse events
There were one (Jin 2016) and two (Cao 2017) cases of mild subcutaneous haematoma in the true acupuncture group. There were two cases of nausea (Cao 2017), one case of headache (Cao 2017), one case of gastrointestinal upset (Jin 2016), and one case of weight gain (Jin 2016) following Diane‐35 (Analysis 5.2).
5.2. Analysis.
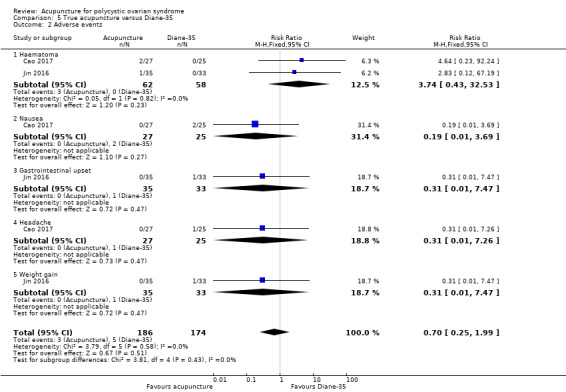
Comparison 5 True acupuncture versus Diane‐35, Outcome 2 Adverse events.
Other analyses
There were too few studies to conduct any of our planned subgroup and sensitivity analyses, or to construct a funnel plot to assess risk of publication bias.
Discussion
Summary of main results
This review assessed the effectiveness and safety of acupuncture treatment for oligo/anovulatory women with PCOS. We found five studies that compared true acupuncture versus sham acupuncture, one study compared low‐frequency electroacupuncture and physical exercise and no intervention, one study compared acupuncture with clomiphene and two studies compared acupuncture and Diane‐35. A total of 1546 women with PCOS were included in this review.
For true acupuncture versus sham acupuncture, we could not exclude clinically relevant differences in live birth, multiple pregnancy rate, ovulation rate, clinical pregnancy rate and miscarriage rate. Number of intermenstrual days may have improved in participants receiving true acupuncture compared to sham acupuncture. True acupuncture probably worsened adverse events compared to sham acupuncture. Quality of evidence ranged from moderate to very low quality.
No studies reported data on live birth rate and multiple pregnancy rate for the other comparisons: physical exercise or no intervention, relaxation and clomiphene. Studies including Diane‐35 did not measure fertility outcomes.
We were uncertain whether acupuncture improved ovulation rate (measured by ultrasound three months post treatment) compared to relaxation or Diane‐35. The other comparisons did not report ovulation rate.
Adverse events were recorded in the acupuncture group for the comparisons physical exercise or no intervention, clomiphene and Diane‐35. These included dizziness, nausea and subcutaneous haematoma. Evidence was very low quality with very wide CIs and very low event rates.
Overall completeness and applicability of evidence
The included studies poorly addressed the primary outcomes of this review, with only one study reporting the primary outcomes live birth rate and multiple pregnancy rate. Five of eight studies addressed the primary outcome ovulation rate; however, there was significant heterogeneity in reporting and measurement of ovulation rate. Moreover, there were insufficient data on adverse events for comparisons other than true acupuncture versus sham acupuncture, to determine the overall safety of acupuncture as a treatment for oligo/anovulation in women with PCOS.
Quality of the evidence
We included only eight RCTs in the present review and most had small sample sizes. Seven of the studies were at high risk of bias in at least one domain (Cao 2017; Du 2011; Jedel 2011; Jin 2016; Johansson 2013; Pastore 2011; Wu 2017). The evidence ranged from very low quality to moderate quality, the main limitations being failure to report important clinical outcomes, and very serious imprecision.
Potential biases in the review process
We did not search any non‐English or non‐Chinese databases, hence studies published in languages other than English or Chinese may not have been identified in the review process. However, there was no exclusion of study that was due to language. There may also have been unpublished data that our searches did not find. In addition, one included study was published by an author (DL) of this review (Lim 2014).
In order to minimise any potential risk of bias during the review process, two review authors (RN, GZ) independently extracted data using a piloted data extraction form. Specifically, the author (DL) of one of the primary studies (Lim 2014) was excluded to extract data from their own study. All studies were then assessed independently and any dispute was resolved by a fifth independent author (HC).
Agreements and disagreements with other studies or reviews
Several systematic reviews have examined acupuncture for PCOS. Jo 2017 conducted a systematic review and meta‐analysis on acupuncture for PCOS which included 27 RCTs comparing acupuncture with sham acupuncture, medication, no treatment or acupuncture combined with medication. The review found similar results to this review, reporting very limited evidence for acupuncture in improving ovulation, menstruation rates and hormonal changes. Qu 2016 included nine RCTs in a systematic review and meta‐analysis which included studies comparing acupuncture with sham acupuncture or acupuncture in addition to other treatment. Unlike this study, the authors found significant improvement in recovery of menstrual cycles and lower BMI and LH levels. However, there was no evidence in improvement of other hormonal parameters. Similar to this study, Qu 2016 found that studies had unclear or high risks of bias in multiple domains and limited quality.
Authors' conclusions
Implications for practice.
For true acupuncture versus sham acupuncture, we cannot exclude clinically relevant differences in live birth rate, multiple pregnancy rate, ovulation rate, clinical pregnancy rate or miscarriage. Number of intermenstrual days may improve in participants receiving true acupuncture compared to sham acupuncture. True acupuncture probably worsens adverse events compared to sham acupuncture.
No studies reported data on live birth rate and multiple pregnancy rate for the other comparisons: physical exercise or no intervention, relaxation and clomiphene. Studies including Diane‐35 did not measure fertility outcomes.
We are uncertain whether acupuncture improves ovulation rate (measured by ultrasound three months post treatment) compared to relaxation or Diane‐35. The other comparisons did not report on this outcome.
There were adverse events in the acupuncture group for the comparisons physical exercise or no intervention, clomiphene and Diane‐35. These included dizziness, nausea and subcutaneous haematoma. Evidence was very low quality with very wide confidence intervals and very low event rates.
There are only a limited number of randomised controlled trials (RCT) in this area, limiting our ability to determine effectiveness of acupuncture for polycystic ovarian syndrome (PCOS).
Implications for research.
Given the lack of evidence for acupuncture for PCOS, further large‐scale, properly designed RCTs are needed to assess the use of acupuncture in the management of PCOS. Women with PCOS meeting standard diagnostic criteria (e.g. Rotterdam consensus) seeking fertility or symptom control should be recruited and an acupuncture regimen involving a set of standard acupuncture points and mode of stimulation should be considered. Controls should also receive a standard regimen of sham acupuncture in order to minimise the potential therapeutic effects of sham acupuncture. Consistent, standard outcome measures including live birth rate should be reported.
What's new
| Date | Event | Description |
|---|---|---|
| 4 July 2019 | Amended | Editing PLS using GRADE terminology |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 8, 2011
| Date | Event | Description |
|---|---|---|
| 24 May 2019 | New search has been performed | Three studies included in this update (Cao 2017; Jin 2016; Wu 2017), and ongoing studies identified (ChiCTR‐IOR‐15007358; ChiCTR1800015738; NCT02653911; ChiCTR1800017304; NCT02647827; NCT02491333). |
| 24 May 2019 | New citation required but conclusions have not changed | The updated review now has included three new studies however conclusions have not changed. |
Acknowledgements
The review authors would like to thank Dr Zhen Zheng from the Royal Melbourne Institute of Technology (RMIT) University for her kind assistance throughout the pre‐title registration period. We wish to acknowledge Dr Wei Chen, Prof A O'Sullivan, Prof Felix Wong, Ke Xu, Charlie CL Xue, Nini Chen and Liu J as authors of previous versions of this review. We also acknowledge Dr Yang Liu from the Institute of History of Chinese Medicine and Medical Literature, China Academy of Chinese Medical Sciences (CACMS) for the assistance of Chinese literature search in the second review update. We would like to thank Jane Marjoribanks, Jane Thomas, Katie Stocking and Gabriela Cooper for their valuable peer review comments.
Appendices
Appendix 1. Cochrane Gynaecology and Fertility Group Specialised Register search strategy
Searched 22 May 2018
PROCITE platform
Keywords CONTAINS "polycystic ovary morphology" or "*Polycystic Ovary Syndrome" or "PCOS" or "Oligo‐amenorrhea" or "oligoamenorrhea" or "oligoanovulatory" or "oligohypomenorrhea" or "amenorrhea" or "amenorrhoea" or "hirsutism" or Title CONTAINS "polycystic ovary morphology" or "*Polycystic Ovary Syndrome" or "PCOS" or "Oligo‐amenorrhea" or "oligoamenorrhea" or "oligoanovulatory" or "oligohypomenorrhea" or "amenorrhea" or "amenorrhoea" or "hirsutism"
AND
Keywords CONTAINS "acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "Tui Na" or Title CONTAINS "acupoint" or "acupressure" or "acupressure‐acupuncture therapy" or "acupuncture" or "electro‐acupuncture" or "electroacupuncture" or "moxibustion" or "Tui Na" (36 hits)
Appendix 2. CENTRAL Register of Studies Online (CRSO) search strategy
Searched 22 May 2018
Web platform
#1 MESH DESCRIPTOR Polycystic Ovary Syndrome EXPLODE ALL TREES 1170
#2 (polycystic ovar*):TI,AB,KY 2370
#3 (PCOS or PCOD):TI,AB,KY 1928
#4 (stein‐leventhal syndrome):TI,AB,KY 3
#5 hirsut*:TI,AB,KY 591
#6 #1 OR #2 OR #3 OR #4 OR #5 2924
#7 MESH DESCRIPTOR Acupuncture Therapy EXPLODE ALL TREES 3825
#8 Acupuncture:TI,AB,KY 10622
#9 electroacupuncture:TI,AB,KY 1518
#10 meridian:TI,AB,KY 528
#11 needling:TI,AB,KY 1353
#12 moxi*:TI,AB,KY 2537
#13 acup*?point*:TI,AB,KY 2
#14 (acup* point*):TI,AB,KY 2197
#15 (shiatsu or tui na):TI,AB,KY 28
#16 shu:TI,AB,KY 258
#17 acupressure:TI,AB,KY 763
#18 (trigger adj3 point*):TI,AB,KY 682
#19 #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 14633
#20 #6 AND #19 74
Appendix 3. MEDLINE search strategy
Searched from 1946 to 22 May 2018
Ovid Platform
1 exp Polycystic Ovary Syndrome/ (12729) 2 polycystic ovar$.tw. (14304) 3 stein‐leventhal syndrome.tw. (561) 4 PCOS.tw. (9242) 5 PCOD.tw. (280) 6 hirsut$.tw. (8470) 7 exp Amenorrhea/ or exp Oligomenorrhea/ or exp Hirsutism/ (13627) 8 oligomenorrh$.tw. (1345) 9 amenorrh$.tw. (13508) 10 or/1‐9 (40945) 11 acupuncture.tw. (19129) 12 exp Acupuncture/ (1501) 13 exp acupuncture therapy/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp acupuncture points/ or exp moxibustion/ (21203) 14 electroacupuncture.tw. (3716) 15 meridian$.tw. (4886) 16 needling.tw. (2398) 17 moxi$.tw. (7063) 18 acup$ point$.tw. (1544) 19 (shiatsu or tui na).tw. (108) 20 shu.tw. (759) 21 acupressure.tw. (894) 22 (trigger adj3 point$).tw. (1905) 23 or/11‐22 (38977) 24 randomized controlled trial.pt. (462119) 25 controlled clinical trial.pt. (92434) 26 randomized.ab. (413162) 27 randomised.ab. (82543) 28 placebo.tw. (194596) 29 clinical trials as topic.sh. (183822) 30 randomly.ab. (291200) 31 trial.ti. (183145) 32 (crossover or cross‐over or cross over).tw. (76588) 33 or/24‐32 (1211060) 34 exp animals/ not humans.sh. (4462498) 35 33 not 34 (1115554) 36 10 and 23 and 35 (75)
Appendix 4. Embase search strategy
Searched from 1980 to 22 May 2018
Ovid Platform
1 exp ovary polycystic disease/ (23430) 2 polycystic ovar$.tw. (19736) 3 stein‐leventhal syndrome.tw. (370) 4 PCOS.tw. (14034) 5 PCOD.tw. (379) 6 hirsut$.tw. (9566) 7 exp "amenorrhea and oligomenorrhea"/ or exp secondary amenorrhea/ or exp amenorrhea/ or exp primary amenorrhea/ (27466) 8 exp oligomenorrhea/ (2823) 9 oligomenorrh$.tw. (1798) 10 amenorrh$.tw. (15759) 11 or/1‐10 (62000) 12 exp acupuncture/ or exp acupressure/ or exp electroacupuncture/ (40601) 13 electroacupuncture.tw. (4439) 14 meridian$.tw. (5663) 15 needling.tw. (3136) 16 moxi$.tw. (9532) 17 acup$ point$.tw. (2359) 18 (shiatsu or tui na).tw. (154) 19 shu.tw. (1578) 20 acupressure.tw. (1187) 21 (trigger adj3 point$).tw. (2894) 22 or/12‐21 (56901) 23 11 and 22 (320) 24 Clinical Trial/ (964217) 25 Randomized Controlled Trial/ (499723) 26 exp randomization/ (78253) 27 Single Blind Procedure/ (31333) 28 Double Blind Procedure/ (147013) 29 Crossover Procedure/ (55360) 30 Placebo/ (311217) 31 Randomi?ed controlled trial$.tw. (181155) 32 Rct.tw. (28426) 33 random allocation.tw. (1779) 34 randomly allocated.tw. (29590) 35 allocated randomly.tw. (2315) 36 (allocated adj2 random).tw. (796) 37 Single blind$.tw. (20811) 38 Double blind$.tw. (181979) 39 ((treble or triple) adj blind$).tw. (775) 40 placebo$.tw. (267842) 41 prospective study/ (448348) 42 or/24‐41 (1902190) 43 case study/ (54421) 44 case report.tw. (353224) 45 abstract report/ or letter/ (1037032) 46 or/43‐45 (1436046) 47 42 not 46 (1854050) 48 23 and 47 (129)
Appendix 5. PsycINFO search strategy
Searched from 1806 to 22 May 2018
Ovid Platform
1 exp endocrine sexual disorders/ (1133) 2 polycystic ovar$.tw. (375) 3 stein‐leventhal syndrome.tw. (2) 4 PCOS.tw. (243) 5 PCOD.tw. (6) 6 hirsut$.tw. (148) 7 exp amenorrhea/ (254) 8 oligomenorrh$.tw. (49) 9 amenorrh$.tw. (827) 10 or/1‐9 (2275) 11 exp acupuncture/ (1340) 12 electroacupuncture.tw. (259) 13 meridian$.tw. (795) 14 needling.tw. (125) 15 moxi$.tw. (60) 16 acup$ point$.tw. (147) 17 acupuncture.tw. (1823) 18 (shiatsu or tui na).tw. (22) 19 shu.tw. (202) 20 acupressure.tw. (160) 21 (trigger adj3 point$).tw. (322) 22 or/11‐21 (3398) 23 10 and 22 (2)
Appendix 6. AMED (Allied and Complementary Medicine) search strategy
Searched from 1985 to 22 May 2018
Ovid Platform
1 exp ovarian disease/ (220) 2 polycystic ovar$.tw. (72) 3 stein‐leventhal syndrome.tw. (1) 4 PCOS.tw. (34) 5 PCOD.tw. (17) 6 hirsut$.tw. (71) 7 exp amenorrhea/ (37) 8 Hirsut$.tw. (71) 9 amenorrh$.tw. (94) 10 oligomenorrh$.tw. (10) 11 or/1‐10 (400) 12 exp acupuncture/ (3302) 13 exp Acupoints/ or exp Electroacupuncture/ or exp Acupuncture therapy/ (7814) 14 acupuncture.tw. (9739) 15 electroacupuncture.tw. (1060) 16 meridian$.tw. (677) 17 needling.tw. (879) 18 moxi$.tw. (646) 19 exp Moxibustion/ (543) 20 acup$ point$.tw. (646) 21 (shiatsu or tui na).tw. (341) 22 shu.tw. (91) 23 acupressure.tw. (395) 24 (trigger adj3 point$).tw. (472) 25 or/12‐24 (11584) 26 11 and 25 (40)
Appendix 7. CNKI search strategy
Searched December 2010 to May 2018
Web platform
1 polycystic ovary syndrome 2 polycystic ovary 3 ovary polycystic disease 4 #1˜#3/or 5 acupuncture 6 electroacupuncture 7 traditional medicine 8 traditional Chinese medicine 9 traditional Chinese medicine combined with western medicine 10 #4˜#9/or 11 random* 12 #3 and #10 and #11
All of the search terms were translated into Chinese terms when we conduct the searches in Chinese databases.
Appendix 8. SinoMed (CBM) search strategy
Searched 2010 to November 2015
Web platform
Title or Keywords or Abstract CONTAINS: "random" AND ("polycystic ovarian syndrome" OR "polycystic ovaries") AND ("needling" OR "acupuncture" OR "electroacupuncture" OR "traditional Chinese medicine" OR "traditional medicine" OR "traditional Chinese medicine combined with western medicine")
All of the search terms were translated into Chinese terms when we conduct the searches in Chinese databases.
Appendix 9. Chinese VIP database search strategy
Searched 2010 to May 2018
Web platform
Keyword and Title CONTAINS "polycystic ovarian syndrome" OR "polycystic ovaries" AND ((Keyword and Title CONTAINS "needling" OR "electroacupuncture" OR "acupuncture" OR "traditional Chinese medicine" OR "traditional medicine" OR "traditional Chinese medicine combined with western medicine") OR (Abstract CONTAINS needling" OR "electroacupuncture" OR "acupuncture" OR "traditional Chinese medicine" OR "traditional medicine" OR "traditional Chinese medicine combined with western medicine")) AND Full text CONTAINS "random"
All of the search terms were translated into Chinese terms when we conduct the searches in Chinese databases.
Appendix 10. Ongoing trials
Ongoing trials were also searched in:
ClinicalTrials.gov
World Health Organization International Trials Registry
Australian and New Zealand Clinical Trial Registry
Data and analyses
Comparison 1. True acupuncture versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Live birth rate | 1 | 926 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.76, 1.24] |
| 2 Multiple pregnancy rate | 1 | 926 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.33, 2.45] |
| 3 Ovulation rate | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.02 [‐0.15, 0.19] | |
| 4 Clinical pregnancy rate | 3 | 1117 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.82, 1.29] |
| 5 Restored regular menstrual period | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐312.09 [‐344.59, ‐279.59] |
| 6 Miscarriage rate | 1 | 926 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.77, 1.56] |
| 7 Adverse events | 3 | 1230 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.02, 1.31] |
Comparison 2. Low‐frequency electroacupuncture versus physical exercise or no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Restored regular menstrual period | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Low‐frequency electroacupuncture versus physical exercise | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐0.01, 0.45] |
| 1.2 Low‐frequency electroacupuncture versus no intervention | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.21, 0.53] |
| 2 Adverse events | 1 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.46 [0.77, 25.78] |
| 2.1 Haematoma | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.21 [0.39, 134.32] |
| 2.2 Dizziness | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.13, 73.20] |
| 2.3 Nausea | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [0.13, 73.20] |
Comparison 3. True acupuncture versus relaxation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ovulation rate | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.35 [0.14, 0.56] |
Comparison 4. True acupuncture versus clomiphene.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Restored regular menstrual period | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Restored menstruation at the end of treatment | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.94, 2.85] |
| 1.2 Restored menstruation 1 month after end of treatment | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [1.03, 2.19] |
| 2 Adverse events | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.30, 5.83] |
| 2.1 Haematoma | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.38, 129.93] |
| 2.2 Gastrointestinal adverse effects | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.00] |
Comparison 5. True acupuncture versus Diane‐35.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ovulation rate | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.87, 2.42] |
| 2 Adverse events | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.25, 1.99] |
| 2.1 Haematoma | 2 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.74 [0.43, 32.53] |
| 2.2 Nausea | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.69] |
| 2.3 Gastrointestinal upset | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.47] |
| 2.4 Headache | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.26] |
| 2.5 Weight gain | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.47] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cao 2017.
| Methods | Method: randomised controlled trial Blinding: nil Intervention: acupuncture Control: Diane‐35 (ethinylestradiol and cyproterone acetate tablets) Time: treatments for 12 continuous weeks. |
|
| Participants | Country: China Number of participants: 56 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Acupuncture
Following were treated bilaterally, Fuke, Huanchao, Tianhuang (Yinlingquan, SP 9), Renhuang (Sanyinjiao, SP 6), Guanyuan (CV 4), Zigong (EX‐CA 1) Diane‐35
|
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised using random number method |
| Allocation concealment (selection bias) | Unclear risk | No concealment described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding described (difficult to blind when using different method) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/56 women dropped out during the intervention phase. The difference between age, BMI or clinical feature of the dropouts and the remainder of the cohort was not performed. There was no ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Unclear risk | No other potential bias identified |
Du 2011.
| Methods | Method: randomised controlled trial Blinding: nil Intervention: acupuncture Control: clomiphene Time: treatment for 3 continuous months or pregnancy. Follow‐up 1 month |
|
| Participants | Country: China Number of participants: 60 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Acupuncture
Clomiphene
|
|
| Outcomes |
|
|
| Notes | Study was from an unpublished thesis for Master's degree at Guangzhou University of Chinese Medicine. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation with PEMS 3.1 software was used to allocate participants at 1:1 ratio into 2 groups. |
| Allocation concealment (selection bias) | Low risk | Computer‐generated sequences were sealed in numbered opaque envelops. Participants were allocated sequentially to envelops. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not described. However, blinding of participants or practitioner was unlikely given nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawal or exclusion after enrolment |
| Selective reporting (reporting bias) | High risk | Number of women with no ovulation during treatment period not reported |
| Other bias | High risk | Reported as a part of thesis, instead of published in a peer‐reviewed journal |
Jedel 2011.
| Methods | Method: randomised controlled clinical trial Blinding: nil Intervention: low‐frequency electroacupuncture, physical exercise Control: no active intervention Time: 12‐week observation period and baseline assessment, 16‐week intervention, 16‐week follow‐up |
|
| Participants | Country: Sweden Number of participants: low‐frequency electroacupuncture: 33; physical exercise: 34; no active intervention: 17 Inclusion criteria
Exclusion criteria
|
|
| Interventions | 3 groups Low‐frequency electroacupuncture
Physical exercise
No active intervention
|
|
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants stratified by age and BMI and randomised using computer‐generated randomisation. |
| Allocation concealment (selection bias) | Low risk | Concealed until interventions assigned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding described. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers and reasons for dropout in all phases were described. No comparison of baseline characteristics of dropouts and those remaining in trial was reported. ITT analysis performed. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported. |
| Other bias | Unclear risk | No other potential bias identified. |
Jin 2016.
| Methods | Method: randomised controlled trial Blinding: nil Intervention: acupuncture Control: Diane‐35 (ethinylestradiol and cyproterone acetate tablets) Time: treatments for 3 months |
|
| Participants | Country: China Number of participants: 72 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Acupuncture
Diane‐35
|
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomised using computer method. |
| Allocation concealment (selection bias) | Unclear risk | No concealment described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding described (difficult to blind when using different method). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding described. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/72 dropped out during the intervention phase. The difference between age, BMI or clinical feature of the dropouts and the remainder of the cohort was not performed. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported. |
| Other bias | High risk | Reported as a part of thesis, instead of published in a peer‐reviewed journal. |
Johansson 2013.
| Methods | Method: randomised controlled trial Blinding: single, investigators blinded until statistical analysis Intervention: acupuncture Control: relaxation Time: 10–13 weeks' intervention. Measurements were taken within 1 week of interventions. |
|
| Participants | Country: Sweden Number of participants: acupuncture: 16; relaxation: 16 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Acupuncture
Attention control (relaxation)
|
|
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants or therapists was not possible because of natures of intervention and control in this study. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Biological outcomes were measured at an independent laboratory. It was unclear what was meant by "investigators were blinded until statistical analyses." There was potential risk from blinding of outcome assessment if blinding was stopped prior to statistical analysis. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts were adequately described. |
| Selective reporting (reporting bias) | Unclear risk | All predetermined outcomes were reported. However, there was no mention of adverse events. |
| Other bias | Unclear risk | No other potential bias identified. |
Lim 2014.
| Methods | Method: randomised controlled trial Blinding: single (participants) Intervention: acupuncture Control: sham acupuncture Time: 7 months |
|
| Participants | Country: Australia and China Number of participants: acupuncture: 98: sham acupuncture: 48 Inclusion criteria
Exclusion criteria
|
|
| Interventions | True acupuncture
Sham body acupuncture
Intervention frequency: weekly for 3 months |
|
| Outcomes | Primary outcome
Secondary outcomes
|
|
| Notes | Live birth was not measured. Clarification from author was sought regarding adverse events. There were no adverse events noted in the study and hence was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation achieved by computer‐generated program. |
| Allocation concealment (selection bias) | Low risk | Presealed identical envelopes used. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Trial described as single blinded, only participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment was done by statisticians who were independent of the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number and reason for dropout between enrolment and allocation were described. No participants dropped out or lost to follow‐up during intervention. |
| Selective reporting (reporting bias) | Unclear risk | All listed outcomes were reported; however, adverse effects were not reported. |
| Other bias | Unclear risk | No other potential bias identified. |
Pastore 2011.
| Methods | Method: randomised controlled trial Blinding: double blind Intervention: acupuncture Control: sham acupuncture Time: 5 months |
|
| Participants | Country: US Number of participants: acupuncture: 46; sham acupuncture: 50 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Time: 12 acupuncture/sham session: twice weekly for the first 4 weeks followed by once weekly for an additional 4 weeks True acupuncture
Sham acupuncture
|
|
| Outcomes | Ovulation rate LH:FSH ratio |
|
| Notes | Authors contacted for data regarding live births (primary outcome) but data not available from authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation achieved by random number generator program. Participants stratified by obese (BMI) and non‐obese. |
| Allocation concealment (selection bias) | Low risk | Consecutive study identifications were assigned to a treatment arm by a graduate student independent of the study. Quote: "These assignments were placed in individual sealed, opaque envelopes labelled with the study identifications." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The trial was described as blinded, parties who were blinded and method of blinding was described. Quote: "The participants, principal investigator, clinical research coordinator, and biostatistician (J.T.P.) were all blind to the intervention arm." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The trial was described as blinded, parties who were blinded and method of blinding was described. Quote: "The participants, principal investigator, clinical research coordinator, and biostatistician (J.T.P.) were all blind to the intervention arm." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number and reason for dropout during intervention described. Number and reason for dropout during 3‐month follow‐up not given. ITT not performed |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported. |
| Other bias | Unclear risk | No other potential bias identified. |
Wu 2017.
| Methods | Method: factorial trial Blinding: acupuncture double blinded to participants and study investigators, known to acupuncturists and data manager at each site; clomiphene and placebo assignments double blinded to participant and study investigators, known to data manager at each site. Intervention: acupuncture, clomiphene Control: control acupuncture and placebo drug |
|
| Participants | Country: China Number of participants: active acupuncture + clomiphene: 250; control acupuncture + clomiphene: 250; active acupuncture + placebo: 250; control acupuncture + placebo: 250 Inclusion criteria
Exclusion criteria
|
|
| Interventions | Participants randomised to 4 arms
Active acupuncture
Control acupuncture
Clomiphene
Placebo
|
|
| Outcomes | Primary outcome
Secondary outcomes
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation stratified within 21 participating sites and defined with a random block size of 4 or 8. Participants were randomly allocated in a ratio of 1:1:1:1 into 1 of 4 intervention groups by an interactive online computer program in a central office. |
| Allocation concealment (selection bias) | Low risk | Medication bottles had preprinted barcode labels and were distributed to sites and assigned to the participants as they were enrolled. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Active and control acupuncture treatments single blinded to participant. Treatments known to acupuncturists and data manager at each site. Clomiphene and placebo assignments double blinded to participants and study investigators. Known to data manager. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not described in the report. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers and reasons for dropout in all phases were described. 4 participants who conceived after randomisation and before intervention commenced. These participants completed the last visit and were included in the primary analysis. During the intervention phase, 74 participants dropped out from the study. 15 participants dropped out from the active acupuncture + clomiphene arm; 14 participants dropped out from the control acupuncture + clomiphene arm; 27 participants dropped out from the active acupuncture + placebo arm and 18 participants dropped out from the control acupuncture + placebo arm. Out of the 14 participants who dropped out from the control acupuncture + clomiphene arm, 2 were due to intervention adverse effects. Out of the 27 participants who dropped out from the active acupuncture + placebo arm, 3 were due to intervention adverse effects. There was no ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported. |
| Other bias | Low risk | Conflict of interest disclosed by 1 author (Legro) who reported serving as consultant to Bayer, Kindex, Euroscreen, Millendo, Takeda, Clarus, Sprou and AstraZeneca; serving as a site investigators and receiving grants from Ferring and AstraZeneca. The study was supported by various government and non‐government grants. Quote: "The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication." |
BMI: body‐mass index; FSH: follicle‐stimulating hormone; ITT: intention to treat; LH: luteinising hormone; PCOS: polycystic ovarian syndrome.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cai 2016 | Additional acupuncture points were used based on traditional Chinese medicine patterns for both electroacupuncture and acupoint catgut‐embedding therapy groups. The frequency for electroacupuncture was not a set value for each participant. |
| Chen 2014 | Acupuncture combined with another therapy. Embedded short suture as additional intervention in acupuncture group. There was also a lack of outcome measurement specified in this review. |
| Chen 2015b | Acupuncture combined with another therapy. Chinese herbal medicine combined with acupuncture, multiple conventional medicine used in control group. |
| Fang 2016 | Lack of outcome measures specified in this review. |
| Hao 2015 | Ineligible comparison intervention. 2 different forms of acupuncture compared. |
| He 2017 | Lack of outcome measures specified in this review. |
| Huang 2016 | Ineligible intervention, both acupuncture and western medicine were used in treatment group. |
| Jiang 2014 | Acupuncture combined with another therapy. Herbal medicine given to all groups apart from clomiphene‐only group. |
| Jiang 2015a | Acupuncture combined with another therapy. Herbal medicine given to all groups except for clomiphene‐only group. |
| Jiang 2015b | Ineligible treatment/comparison either using a combination of Chinese herbal medicine and acupuncture, with or without conventional medicine. |
| Jin 2014 | Lack of outcome measures specified in this review. |
| Kuang 2013 | Acupuncture combined with another therapy. Effects of clomiphene citrate combined with acupuncture as intervention studied. |
| Li 2010 | Lack of outcome measures specified in this review. |
| Li 2011a | Diagnostic criteria used differed significantly from Rotterdam consensus. |
| Li 2011b | Acupuncture combined with another therapy. Controlled ovarian hyperstimulation given as cointervention to both groups. |
| Li 2013 | Diagnostic criteria used were different from Rotterdam consensus. |
| Li 2014 | Acupuncture combined with another therapy. Controlled ovarian hyperstimulation performed on both acupuncture and conventional group. |
| Li 2015 | Ineligible comparison intervention: conventional medicine was used in both groups. |
| Li 2017 | Different points were used for each participant during treatments in 2 types of acupuncture regimen. |
| Liu 2012 | Acupuncture combined with another therapy. Oral contraceptives given to both groups. |
| Liu 2017 | Diagnostic criteria used differed significantly from Rotterdam consensus. It was unclear which type of conventional medicine was used in the control group. Lack of outcome measure specified in this review. |
| Peng 2017 | Ineligible comparator, Electroacupuncture on real points vs manual acupuncture on sham points. |
| Qu 2012 | Women with clinical or biochemical hyperandrogenism excluded from the study. |
| Rashidi 2013 | Ineligible comparison intervention. Acupuncture compared to in vitro fertilisation treatment instead of treatment for polycystic ovarian syndrome. |
| Sun 2010 | Acupuncture combined with another therapy. Controlled ovarian hyperstimulation given to both groups. |
| Wang 2013 | Acupuncture combined with another therapy. |
| Yang 2015 | Not a randomised study. Additional points were used during different stages of menstrual cycle. Multiple drugs were used for the control group. |
| Yang 2017 | Different additional points were used for each participant during treatment of acupuncture. |
| Yu 2013 | Ineligible comparison intervention. Acupuncture compared with electrical acupuncture and herbal medicine. Studies involving herbal medicine excluded because of coexisting review. |
| Zhang 2013 | Acupuncture combined with another therapy. |
| Zhou 2016 | Different additional points were used for each participant during treatment of acupuncture. Multiple type of conventional medicine may be used for patients. Acupuncture treatment duration may be inconsistent due to ultrasound evaluation of ovulation. |
Characteristics of ongoing studies [ordered by study ID]
ChiCTR‐IOR‐15007358.
| Trial name or title | A randomized controlled trial to evaluate the effectiveness of electroacupuncture for polycystic ovary syndrome |
| Methods | Randomised parallel controlled trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Electroacupuncture Clomiphene citrate |
| Outcomes | Ovulation rate, LH, E2, dominant follicle rate The time point of ovulation, mean number of dominant follicle, follicular size before ovulation, pregnancy rate |
| Starting date | 1 January 2015 |
| Contact information | Feng Shuwei. Chengdu University of TCM |
| Notes |
ChiCTR1800015738.
| Trial name or title | Intervention of acupuncture based on metabonomics on key targets of PCOS dampness syndrome |
| Methods | Randomised parallel controlled trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Acupuncture Western medicine Acupuncture + western medicine |
| Outcomes | Biomarkers |
| Starting date | 1 May 2018 |
| Contact information | Xiaoxia Li, Shandong University of Traditional Chinese Medicine |
| Notes |
ChiCTR1800017304.
| Trial name or title | A multicenter, randomized, controlled trial for comparing personalized acupuncture versus standardized acupuncture, versus letrozole, placebo in the treatment of anovulatory women with polycystic ovary syndrome |
| Methods | Randomised, parallel controlled trial |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | 2 different acupuncture regimens Letrozole Placebo |
| Outcomes | Live birth rate, ovulation rate, ongoing pregnancy rate, multiple pregnancy rate, miscarriage rate, hormonal profile, metabolic profile, adverse effect profile |
| Starting date | 1 August 2018 |
| Contact information | Ma Hongxia, the First Affiliated Hospital of Guangzhou Medical University |
| Notes |
NCT02491333.
| Trial name or title | The RCT of acupuncture on PCOS combined with IR |
| Methods | Randomised controlled trial |
| Participants | 342 Chinese women with BMI > 18.5 who satisfy Rotterdam criteria |
| Interventions | True acupuncture Sham acupuncture Metformin Placebo metformin |
| Outcomes | HOMA‐IR, HOMA‐B, AUCglu, menstrual frequency, body composition, metabolic profile, hormonal profile, questionnaires, side effect profile, expectation and credibility of treatment, AUCins, ovulation rate |
| Starting date | August 2015 |
| Contact information | Hongxia Ma, The First Affiliated Hospital of Guangzhou Medical University |
| Notes |
NCT02647827.
| Trial name or title | Acupuncture or metformin for insulin resistance in women with polycystic ovary syndrome: a randomized controlled trial |
| Methods | Randomised controlled trial |
| Participants | 303 Swedish women with BMI 25–40 who satisfy Rotterdam criteria |
| Interventions | Acupuncture Metformin Lifestyle intervention |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | December 2015 |
| Contact information | Elisabet Stener‐Victorin, PhD, Karolinska Institutet |
| Notes | Estimated study completion date: December 2019 |
NCT02653911.
| Trial name or title | Efficacy of acupuncture on menstrual frequency in women with polycystic ovary syndrome: protocol for a randomized, controlled trial |
| Methods | Randomised controlled trial |
| Participants | 172 participants diagnosed with polycystic ovary syndrome |
| Interventions | Electroacupuncture Sham‐acupuncture |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | July 2018 |
| Contact information | Zhou Jing, Department of Acupuncture, Guang'anmen Hospital of China Academy of Chinese Medical Sciences |
| Notes | Estimated study completion date: June 2020 |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; AUCglu: area under the glucose curve; AUCins: area under the insulin curve; BMI: body‐mass index; E2: 17β‐estradiol; FSH: follicle‐stimulating hormone; GnRH: gonadotropin‐releasing hormone; HbA1c: glycated haemoglobin; HOMA‐B: homeostatic model assessment for β‐cell function; HOMA‐IR: homeostatic model assessment for insulin resistance; LH: luteinising hormone; PCOS: polycystic ovarian syndrome; TSH: thyroid‐stimulating hormone.
Differences between protocol and review
Authors: we added Dr Wei Chen and Dr Lisa N Cheng to the authors, as data extractors and review manuscript developers at the 2015 version of this systematic review.
Authors: Dr Wei Chen, Prof A O'Sullivan and Prof Felix Wong stepped down and were replaced by Dr Rachel Ng, Dr Ke Xu and Ms Nini Chen as data extractors and review manuscript developers at the second edition of this systematic review.
Authors: Dr Ke Xu and Ms Nini Chen stepped down and were replaced by Dr George Shengxi Zhang and Dr Hui Chen as data extractors and review manuscript developers at the third edition of this systematic review.
Methods: in the third edition of the systematic review we changed multiple pregnancy from a secondary outcome to a primary outcome.
Methods: we added adverse events as a secondary outcome in the review.
Methods: we added lifestyle intervention as a comparison as per advice of referee.
Methods: we described subgroup analysis in a more concise way, as per advice of referee.
Methods: we changed the definition of the outcome restored regular menstrual period to 'as defined by authors'.
Methods: we were unable to access Chinese BioMedical Literature Database (CBM) for this version of the review and therefore have not been able to update the search for this database
Methods: we changed measurement of dichotomous outcomes from Mantel Haenszel odds ratio to risk ratio.
Methods: we changed the definition of Live birth rate from “Live birth rate per couple (in studies or study subgroups of women seeking a live birth)” to “Live birth rate (defined as delivery of live foetus after 20 completed weeks of gestation) – for women seeking fertility”
Methods: we changed the definition of Clinical pregnancy rate from "Clinical pregnancy rate per woman" to "Clinical pregnancy rate (defined as evidence of gestational sac or foetal heart motion, confirmed with ultrasound)."
Contributions of authors
DL: for the protocol: protocol development and revision; topic conception and methodological aspects; protocol review and final proof. For the systematic review: study selection, methodology, adequacy of treatment, data analysis, interpretation of findings and writing the review.
RN: for the systematic review of the English literature: study selection, methodology, adequacy of treatment, data extraction, data analysis, interpretation of findings and writing the review.
GZ: for the systematic review of the Chinese literature: study selection, methodology, adequacy of treatment, data extraction, data analysis, interpretation of findings and writing the review.
LC: for the protocol: topic conception; protocol final proof. For the systematic review: final proof; provided expert advice on gynaecology for the studies found.
HC: for the systematic review: dispute resolution for study selection, adequacy of treatment and revision, and review of final interpretations of findings and provided expert advice on acupuncture treatment in the studies found.
Sources of support
Internal sources
No sources of support supplied
External sources
-
South Western Sydney Clinical School Scholarship, University of New South Wales, Australia, Australia.
CED Lim received the postgraduate scholarship from South Western Sydney Clinical School, Faculty of Medicine, University of New South Wales (2008‐10) to support the work in this project
Declarations of interest
The primary author of one included study is also the primary author (DL) of this review (Lim 2014). In order to minimise any potential risk of bias during the review process, two review authors (RN, GZ) independently extracted data using a piloted data extraction form. All studies were then assessed independently and any dispute was resolved by a third independent review author (HC).
Edited (no change to conclusions)
References
References to studies included in this review
Cao 2017 {published data only}
- Cao Y, Zhang L, Zhao D, Liu Z. DONG's extraordinary acupoints for the ovarian function of polycystic ovary syndrome: a randomized controlled pilot trial [董氏针灸改善多囊卵巢综合征患者卵巢功能: 随机对照预试验]. Zhongguo Zhenjiu 2017;37(7):710‐14. [DOI] [PubMed] [Google Scholar]
Du 2011 {published data only}
- Du Y. [腹针治疗多囊卵巢综合征排卵障碍的临床研究]. Clinical Observation of Abdominal Acupuncture for Polycystic Ovarian Syndrome with Ovulatory Dysfunction [thesis]. Guangzhou (China): Guangzhou University of Chinese Medicine, 2011. [Google Scholar]
Jedel 2011 {published data only}
- Jedel E, Labrie F, Oden A, Holm G, Nilsson L, Janson PO, et al. Impact of electro‐acupuncture and physical exercise on hyperandrogenism and oligo/amenorrhea in women with polycystic ovary syndrome: a randomized controlled trial. American Journal of Physiology. Endocrinology and Metabolism 2011;300:E37‐45. [DOI] [PubMed] [Google Scholar]
- Stener‐Victorin E, Holm G, Janson PO, Gustafson D, Waern M. Acupuncture and physical exercise for affective symptoms and health‐related quality of life in polycystic ovary syndrome: secondary analysis from a randomized controlled trial. BMC Complementary and Alternative Medicine 2013;13(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jin 2016 {published data only}
- Jin CL. [针刺疏肝调气法治疗多囊卵巢综合征临床研究]. Clinical Study on Treatment of Polycystic Ovary Syndrome with Acupuncture and Shugan Tiaoqi Method [PhD thesis]. Beijing (China): Beijing University of Traditional Chinese Medicine, 2016. [Google Scholar]
Johansson 2013 {published data only}
- Johansson J, Redman L, Veldhuis PP, Sazonova A, Labrie F, Holm G, et al. Acupuncture for ovulation induction in polycystic ovary syndrome: a randomized controlled trial. American Journal of Physiology. Endocrinology and Metabolism 2013;304:E934‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lim 2014 {published and unpublished data}
- Lim CED, Luo X, Zhan X, Wong WS. ACUPCOS: acupuncture & PCOS – a multi‐centre randomised controlled trial. International Journal of Gynecological and Obstetrical Research 2014;2:1‐13. [Google Scholar]
Pastore 2011 {published and unpublished data}
- Pastore LM, Williams CD, Jenkins J, Patrie JT. True and sham acupuncture produced similar frequency of ovulation and improved LH to FSH ratios in women with polycystic ovary syndrome. Journal of Clinical Endocrinology & Metabolism 2011;96:3143‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2017 {published data only}
- Deng Y, Xie L, Wu XK, Ng EH, Victorin ES, Zhang H, et al. Prediction models for ovulation, conception, pregnancy and live birth in infertile women with polycystic ovary syndrome. Human Reproduction 2017;32 Suppl 1:i454‐5. [Google Scholar]
- Wen Y, Ma HL, Wu XK. Acupuncture and clomiphene interventions in PCOS conversely affect the insulin resistance profiles in early pregnancy subjects: a secondary analysis of a randomized controlled trial. Journal of Obstetrics and Gynaecology Research 2017;43 Suppl 1:160‐1. [Google Scholar]
- Wu X, Stener‐Victorin E, Liu J, Wu T, Ng E, Legro RS, et al. Acupuncture and clomiphene for infertility in the polycystic ovary syndrome: a multicentre randomized controlled trial. Fertility and Sterility 2016;106(3 Suppl 3):e375. [DOI] [PubMed] [Google Scholar]
- Wu XK, Stener‐Victorin E, Kuang HY, Ma HL, Gao JS, Xie LZ, et al. Effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome: a randomized clinical trial. Journal of the American Medical Association 2017;317(24):2502‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L, Qiao X. Acupuncture is not as effective as infertility treatment in women with PCOS. Evidence‐Based Medicine 2017;22(6):229‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Cai 2016 {published data only}
- Cai X, Li Y, Wang J, Cao J. Clinical observation of electro‐acupuncture and acupoint catgut‐embedding therapy in the treatment of obese polycystic ovary syndrome [电针及穴位埋线治疗肥胖型多囊卵巢综合征的临床观察]. Guangming Journal of Chinese Medicine 2016;31(4):538‐41. [Google Scholar]
Chen 2014 {published data only}
- Chen R, Wang C, Yan QY. Observation on therapeutic effect of polycystic ovary syndrome of damp‐phlegm constitution treated with embedding therapy on back‐shu points and front‐mu points combined with needle‐pricking therapy on Sifeng (EX‐UE 10) [Chinese]. Zhongguo Zhen Jiu 2014;34(4):355‐8. [PubMed] [Google Scholar]
Chen 2015b {published data only}
- Chen M, Zhang H, Zhang YC. Clinical observation of acupuncture plus medication for obesity‐type polycystic ovary syndrome [针刺配合药物干预肥胖型多囊卵巢综合征临床观察]. Shanghai Journal of Acupuncture and Moxibustion 2015;4:310‐3. [Google Scholar]
Fang 2016 {published data only}
- Fang Q, Zou P, Li K. Effect of acupuncture induced ovulation on follicular development and reproductive hormones in patients with polycystic ovary syndrome [针刺促排卵对多囊卵巢综合征患者卵泡发育及生殖激素的影响]. Beijing Journal of Traditional Chinese Medicine 2016;35(3):198‐201. [Google Scholar]
Hao 2015 {published data only}
- Hao C, Zhang T, Qi J, Ji L. Acupuncture at Zhibian (BL 54) through Shuidao (ST 28) for polycystic ovary syndrome [Chinese]. Zhongguo Zhen Jiu 2015;35(5):461‐4. [PubMed] [Google Scholar]
He 2017 {published data only}
- He X, Pan Z, Huang J. Clinical effect of acupuncture treatment of polycystic ovary syndrome guided by TCM syndrome [中医辩证指导的针刺疗法治疗多囊卵巢综合征的临床研究]. Medical Innovation of China 2017;14(22):66‐8. [Google Scholar]
Huang 2016 {published data only}
- Huang L. [通元针法治疗多囊卵巢综合征合并不孕的临床疗效观察]. Observation of acupuncture treatment of Tongyuan Polycystic ovary syndrome with infertility [Master's thesis]. Guangzhou (China): Guangzhou University of Chinese Medicine, 2016. [Google Scholar]
Jiang 2014 {published data only}
- Jiang DS, Wu XQ, Zhang YC. Effects of warm needling combined with zhangmo decoction on endometrial receptivity in patient with ovulation induction [Chinese]. Zhongguo Zhen Jiu 2014;34(2):130‐4. [PubMed] [Google Scholar]
Jiang 2015a {published data only}
- Jiang D, Zhang Y, Wu X, Wu S. Infertility in polycystic ovary syndrome treated with acupuncture and clomiphene: a randomized controlled trial [Chinese]. Zhongguo Zhen Jiu 2015;35(2):114‐8. [PubMed] [Google Scholar]
Jiang 2015b {published data only}
- Jiang D, Zhang Y, Wu X, Wu S. Clinical study on infertility due to polycystic ovary syndrome of kidney deficiency and blood stasis type treated with integrated Chinese and western medicine [中西医结合治疗肾虚血瘀型多囊卵巢综合征性不孕症的临床研究]. Liaoning Journal of Traditional Chinese Medicine 2015;42(4):803‐5. [Google Scholar]
Jin 2014 {published data only}
- Jin CL, Wei LX, Zhao JP, Wu ZC. Efficacy comparison between electroacupuncture and Dyne‐35 in treatment of polycystic ovary syndrome [Chinese]. Zhongguo Zhen Jiu 2014;34(12):1174‐8. [PubMed] [Google Scholar]
Kuang 2013 {published data only}
- Kuang H, Li Y, Wu X, Hou L, Wu T, Liu J, et al. Acupuncture and clomiphene citrate for live birth in polycystic ovary syndrome: study design of a randomized controlled trial. Evidence‐based Complementary and Alternative Medicine : ECAM 2013;2013:527303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2010 {published data only}
- Li B, Han J. Clinical observation of acupuncture plus medicine in the treatment of polycystic ovarian syndrome [针药结合治疗多囊卵巢综合征临床观察]. Journal of Clinical Acupuncture and Moxibustion 2010;26(1):20‐1. [Google Scholar]
Li 2011a {published data only}
- Li C, Zhang S. Clinical observation of acupuncture for polycystic ovarian syndrome in 30 cases [针刺治疗多囊卵巢综合征30例临床观察]. Beijing Journal of Traditional Chinese Medicine 2011;30(2):128‐30. [Google Scholar]
Li 2011b {published data only}
- Li Y. [电针对IVF‐ET周期的PCOS患者卵泡液LIF和卵细胞质量的临床研究]. Clinical Study of Electroacupuncture for Leukemia Inhibitory Factor of Follicular Fluid and Quality of Oocytes in the Treatment of Polycystic Ovarian Syndrome with In Vitro Fertilization and Embryo Transfer [thesis]. Jinan City, China: Shandong University of Traditional Chinese Medicine, 2011. [Google Scholar]
Li 2013 {published data only}
- Li N. Efficacy and safety evaluation of acupuncture combined with auricular point sticking therapy in the treatment of polycystic ovary syndrome [Chinese]. Zhongguo Zhen Jiu 2013;33(11):961‐4. [PubMed] [Google Scholar]
Li 2014 {published data only}
- Li J, Cui W, Sun W, Wen J. Effect of electroacupuncture on egg quality and tumor necrosis factor‐alpha of patients with polycystic ovarian syndrome. World Journal of Acupuncture 2014; Vol. 24, issue 3:9‐15.
Li 2015 {published data only}
- Li S. Metformin and auxiliary acupuncture in the treatment of obese women infertility with polycystic ovary syndrome for 75 cases [针灸辅助二甲双胍治疗肥胖型多囊卵巢综合征不孕症75例]. Chinese Medicine Modern Distance Education of China 2015;13(6):78‐9. [Google Scholar]
Li 2017 {published data only}
- Li N, Zhang N. Therapeutic effect of midnight‐midday ebb flow theory on the treatment of ovulation disorders in women with polycystic ovary syndrome [子午流注开穴法治疗多囊卵巢综合征排卵障碍的疗效观察]. Beijing Journal of Traditional Chinese Medicine 2017;36(1):74‐6. [Google Scholar]
Liu 2012 {published data only}
- Liu Y, Liu X, Li X, Liang R. Clinical study of acupuncture and acupoint injection combined intrauterine insemination for polycystic ovarian syndrome with infertility [针刺及封闭穴位联合宫腔内人工授精治疗PCOS不孕症的临床研究]. Journal of Chengdu Medical College 2012;7(2z):3. [Google Scholar]
Liu 2017 {published data only}
- Liu S, Jia N, Cai S, Lu X, Li H. A comparative study on monitoring clinical effects of acupuncture on polycystic ovary syndrome by ultrasound [超声监测针灸治疗后多囊卵巢综合症患者疗效的对比研究]. Clinical Journal of Chinese Medicine 2017;9(5):116‐8. [Google Scholar]
Peng 2017 {published data only}
- Peng Y, Cong J, Hu N, Chang H, Lu N, Yang X. Acupuncture with resolving phlegm therapy in the treatment of polycystic ovary syndrome: evaluation of clinical efficacy [针刺化痰法对多囊卵巢综合征的临床疗效评价]. Journal of Clinical Acupuncture and Moxibustion 2017;33(2):5‐8. [Google Scholar]
Qu 2012 {published data only}
- Qu H. [腹针治疗肾虚血瘀型多囊卵巢综合征排卵障碍的临床研究]. Clinical Observation of Abdominal Acupuncture for Polycystic Ovarian Syndrome with Ovulatory Dysfunction in Kidney Deficiency and Blood Stasis Pattern [thesis]. Guangzhou, China: Guangzhou University of Chinese Medicine, 2012. [Google Scholar]
Rashidi 2013 {published data only}
- Rashidi BH, Tehrani ES, Hamedani NA, Pirzadeh L. Effects of acupuncture on the outcome of in vitro fertilisation and intracytoplasmic sperm injection in women with polycystic ovarian syndrome. Acupuncture in Medicine 2013;31(2):151‐6. [DOI] [PubMed] [Google Scholar]
Sun 2010 {published data only}
- Sun W, Cui W, Li J. Study of effect mechanism of electroacupuncture for polycystic ovarian syndrome in kidney deficiency pattern [电针干预对肾虚型PCOS患者影响机制的研究]. Chinese Journal of Birth Health & Heredity 2010;18(1):105‐7. [Google Scholar]
Wang 2013 {published data only}
- Wang H, Gu Z. Clinical observation of acupuncture plus medicine for polycystic ovarian syndrome with infertility [针药结合治疗多囊卵巢性不孕症临床观察]. Journal of Hubei University of Chinese Medicine 2013;15(6):57‐8. [Google Scholar]
Yang 2015 {published data only}
- Yang J, Xu J, Liu Y, Huang J. Clinical investigation on the effect of acupuncture‐induced artificial menstrual cycle on polycystic ovary syndrome related follicular dysplasia [针灸人工周期疗法治疗多囊卵巢综合征卵泡发育不良的临床研究]. Lishizhen Medicine and Materia Medica Research 2015;26(12):2954‐5. [Google Scholar]
Yang 2017 {published data only}
- Yang D, Zhao M, Tan J. Effect of polycystic ovary syndrome treated with the periodic therapy of acupuncture [针刺调周法治疗多囊卵巢综合征的临床疗效分析]. Zhongguo Zhenjiu 2017;37(8):825‐9. [DOI] [PubMed] [Google Scholar]
Yu 2013 {published data only}
- Yu L, Liao Y, Wu H, Zhao J, Wu L, Shi Y, et al. Effects of electroacupuncture and Chinese kidney‐nourishing medicine on polycystic ovary syndrome in obese patients. Journal of Traditional Chinese Medicine 2013;33(3):287‐93. [DOI] [PubMed] [Google Scholar]
Zhang 2013 {published data only}
- Zhang H. Acupuncture plus medicine for polycystic ovarian syndrome in 30 cases [针刺配合西药治疗多囊卵巢综合征30例]. China's Naturopathy 2013;21(11):60‐1. [Google Scholar]
Zhou 2016 {published data only}
- Zhou Y, Wu J, Lin W, Pi M, Chen P, Yang Z. The "regulating conception‐governor vessel" acupuncture method for infertility of polycystic ovarian syndrome [调任通督针刺法”治疗多囊卵巢综合征不孕症的临床疗效观察]. Zhongguo ZhenJiu 2016;36(12):1237‐40. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ChiCTR1800015738 {published data only}
- ChiCTR1800015738. Intervention of acupuncture based on metabonomics on key targets of PCOS dampness syndrome [基于代谢组学的针刺对PCOS痰湿证关键靶点的干预研究]. www.chictr.org.cn/showprojen.aspx?proj=26694 (first received 18 April 2018).
ChiCTR1800017304 {published data only}
- ChiCTR1800017304. A multicenter, randomized, controlled trial for comparing personalized acupuncture versus standardized acupuncture, versus letrozole, placebo in the treatment of anovulatory women with polycystic ovary syndrome [个性化针灸、标准化针灸、来曲唑和安慰剂对多囊卵巢综合症无排卵妇女活产率影响:多中心随机试验]. www.chictr.org.cn/showprojen.aspx?proj=28407 (first received 23 July 2018).
ChiCTR‐IOR‐15007358 {published data only}
- ChiCTR‐IOR‐15007358. A randomized controlled trial to evaluate the effectiveness of electroacupuncture for polycystic ovary syndrome [针刺治疗多囊卵巢综合症的随机对照研究]. www.chictr.org.cn/showproj.aspx?proj=12273 (first received 26 October 2015).
NCT02491333 {published data only}
- NCT02491333. The effect of acupuncture on insulin sensitivity of women with polycystic ovary syndrome and insulin resistance: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT02491333 (first received 8 July 2015).
NCT02647827 {published data only}
- NCT02647827. Acupuncture or metformin for insulin resistance in women with polycystic ovary syndrome: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT02647827 (first received 6 January 2016).
NCT02653911 {published data only}
- NCT02653911. Efficacy of acupuncture on menstrual frequency in women with polycystic ovary syndrome: protocol for a randomized, controlled trial. clinicaltrials.gov/ct2/show/NCT02653911 (first received 13 January 2016).
Additional references
Acbay 1996
- Acbay O, Gundogdu S. Can metformin reduce insulin resistance in polycystic ovary syndrome?. Fertility and Sterility 1996;65(5):946‐9. [PubMed] [Google Scholar]
Aleem 1987
- Aleem FA, Eltabbakh GH, Omar RA, Couthren AL. Ovarian follicular fluid beta‐endorphin levels in normal and polycystic ovaries. American Journal of Obstetrics and Gynecology 1987;156:1197‐200. [DOI] [PubMed] [Google Scholar]
Aso 1976
- Aso T, Motohashi T, Murata M, Nishimura T, Kakizaki K. The influence of acupuncture stimulation on plasma levels of LH, FSH, progesterone and estradiol in normally ovulating women. American Journal of Chinese Medicine 1976;4:391‐401. [DOI] [PubMed] [Google Scholar]
Asunicón 2000
- Asunción M, Calvo RM, San Millán JL, Sancho J, Avila S, Escobar‐Morreale HF. A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women in Spain. Journal of Clinical Endocrinology and Metabolism 2000;85:243‐8. [DOI] [PubMed] [Google Scholar]
Brown 2009
- Brown J, Farquhar C, Beck J, Boothroyd C, Hughes E. Clomiphene and anti‐oestrogens for ovulation induction in PCOS. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD002249.pub4] [DOI] [PubMed] [Google Scholar]
Cai 1997
- Cai X. Substitution of acupuncture for human chorionic gonadotropin in ovulation induction. Journal of Traditional Chinese Medicine 1997;17:19‐21. [PubMed] [Google Scholar]
Chen 1991
- Chen BY, Yu J. Relationship between blood radioimmunoreactive beta‐endorphin and hand skin temperature during the electro‐acupuncture induction of ovulation. Acupuncture & Electro‐therapeutics Research 1991;16:1‐5. [DOI] [PubMed] [Google Scholar]
Cui 2017
- Cui J, Wang S, Ren J. Zhang J, Jing J. Use of acupuncture in the USA: Changes over a decade (2002–2012). Acupuncture in Medicine 2017;35(3):200‐7. [DOI] [PubMed] [Google Scholar]
Diamanti‐Kandarakis 1999
- Diamanti‐Kandarakis E, Kouli CR, Bergiele AT, Filandra FA, Tsianateli TC, Spina GG, et al. A survey of the polycystic ovary syndrome in Greek island of Lesbos: hormonal and metabolic profile. Journal of Clinical Endocrinology and Metabolism 1999;84:4006‐11. [DOI] [PubMed] [Google Scholar]
ESHRE 1997
- European Society of Human Reproduction and Embryology Capri Workshop. Female infertility: treatment options for complicated cases. Human Reproduction 1997;12:1191‐6. [PubMed] [Google Scholar]
ESHRE/ASRM 2004
- The Rotterdam European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long term health risks related to polycystic ovary syndrome (PCOS). Human Reproduction 2004;19(1):41‐7. [DOI] [PubMed] [Google Scholar]
Farhi 1996
- Farhi J, West C, Patel A, Jacobs HS. Treatment of anovulatory infertility: the problem of multiple pregnancy. Human Reproduction 1996;11:429‐34. [DOI] [PubMed] [Google Scholar]
Fauser 2012
- Fauser B, Tarlatzis B, Reber R, Legro R, Balen A, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM‐Sponsored 3rd PCOS Consensus Workshop Group. Fertility and Sterility 2012;97(1):28‐38. [DOI] [PubMed] [Google Scholar]
Franik 2018
- Franik S, Eltrop SM, Kremer JA, Kiesel L, Farquhar C. Aromatase inhibitors (letrozole) for subfertile women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews 2018, Issue 5. [DOI: 10.1002/14651858.CD010287.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gadir 1990
- Gadir AA, Mowafi RS, Alnaser HM, Alrashid AH, Shaw RW. Ovarian electrocautery versus hMG and pure FSH therapy in the treatment of patients with polycystic ovarian disease. Clinical Endocrinology 1990;33:585‐92. [DOI] [PubMed] [Google Scholar]
Gerhard 1992
- Gerhard I, Postneek F. Auricular acupuncture in the treatment of female infertility. Gynecological Endocrinology 1992;6:171‐81. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a metaanalysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hopton 2012
- Hopton AK, Curnoe S, Kanaan M, Macpherson H. Acupuncture in practice: mapping the providers, the patients and the settings in a national cross‐sectional survey. BMJ Open 2012;2(1):e000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jo 2017
- Jo J, Lee YJ, Lee HS. Acupuncture for polycystic ovarian syndrome: a systematic review and meta‐analysis. Medicine 2017;96(23):e7066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Knochenhauer 1998
- Knochenhauer ES, Key TJ, Kashar‐Miller M, Waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the south eastern United States: a prospective study. Journal of Clinical Endocrinology and Metabolism 1998;83:3078‐82. [DOI] [PubMed] [Google Scholar]
Ku 2001
- Ku Y, Chang Y. Beta‐endorphin and GABA‐mediated depressor effect of specific electroacupuncture surpasses pressor response of emotional circuit. Peptides 2001;22:1465‐70. [DOI] [PubMed] [Google Scholar]
Legro 2013
- Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Paquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society Clinical Practice guideline. Journal of Clinical Endocrinology & Metabolism 2013;98(12):4565‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacPherson 2001
- MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ 2001;323:486‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
March 2010
- March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Human Reproduction 2010;25:544‐51. [DOI] [PubMed] [Google Scholar]
Mayer 1977
- Mayer DJ, Price DD, Rafil A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Research 1977;121:368‐72. [DOI] [PubMed] [Google Scholar]
Michelmore 1999
- Michelmore KF, Balen AH, Dunger DB, Vessey MP. Polycystic ovaries and associated clinical and biochemical features in young women. Clinical Endocrinology 1999;51:779‐86. [DOI] [PubMed] [Google Scholar]
Mo 1993
- Mo X, Li D, Pu Y, Xi G, Le X, Fu Z. Clinical studies on the mechanism of acupuncture stimulation of ovulation. Journal of Traditional Chinese Medicine 1993;13:115‐9. [PubMed] [Google Scholar]
Ni 2007
- Ni HY, Gong J. Research progress on Chinese herbal medicine in treating PCOS. Liaoning Journal of Traditional Chinese Medicine 2007;34(1):123‐4. [Google Scholar]
Norman 2004
- Norman RJ, Wu R, Stankiewicz MT. Polycystic ovary syndrome. Medical Journal of Australia 2004;180(3):132‐7. [DOI] [PubMed] [Google Scholar]
Petraglia 1987
- Petraglia F, DiMeo G, Storchi R, Segre A, Facchinette F, Szalay S. Proopiomelanocortin‐related peptides and methionine enkephalin in human follicular fluid: changes during the menstrual cycle. American Journal of Obstetrics and Gynecology 1987;157:142‐6. [DOI] [PubMed] [Google Scholar]
Petti 1998
- Petti F, Bangrazi A, Liguori A, Reale G, Ippoliti F. Effects of acupuncture on immune response related to opioid‐like peptides. Journal of Traditional Chinese Medicine 1998;18:55‐63. [PubMed] [Google Scholar]
Qu 2016
- Qu F, Wu Y, Hu XY, Barry J, Zhou J, Wang FF, et al. The effects of acupuncture on polycystic ovary syndrome: a systematic review and meta‐analysis. European Journal of Integrative Medicine 2016;8(1):12‐8. [Google Scholar]
Rodin 1998
- Rodin DA, Bano G, Bland JM, Taylor K, Nussey SS. Polycystic ovaries and associated metabolic abnormalities in Indian subcontinent Asian women. Clinical Endocrinology 1998;49:91‐9. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 2000
- Stener‐Victorin E, Waldenstrom U, Tagnfors U, Lundeberg T, Lundstedt G, Janson PO. Effects of electro‐acupuncture on anovulation in women with polycystic ovary syndrome. Acta Obstetricia et Gynecologica Scandinavica 2000;79:180‐8. [PubMed] [Google Scholar]
Stener‐Victorin 2007
- Stener‐Victorin E, Jedel E, Manneras L. Acupuncture in polycystic ovary syndrome: current experimental and clinical evidence. Journal of Neuroendocrinology 2007;20(3):290‐8. [DOI] [PubMed] [Google Scholar]
Tang 2012
- Tang T, Lord JM, Norman RJ, Yasmin E, Balen AH. Insulin‐sensitising drugs (metformin, rosiglitazone, pioglitazone, D‐chiro‐inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD003053.pub5] [DOI] [PubMed] [Google Scholar]
Teede 2010
- Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Medicine 2010;8:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teede 2011
- Teede HJ, Misso ML, Deeks AA, Moran LJ, Stuckey BG, Wong JL, et al. Assessment and management of polycystic ovary syndrome: summary of an evidence‐based guideline. Medical Journal of Australia 2011;195:S65‐112. [DOI] [PubMed] [Google Scholar]
Thomas 2001
- Thomas KJ, Nicholl JP, Coleman P. Use and expenditure on complementary medicine in England: a population based survey. Complementary Therapies in Medicine 2001;9:2‐11. [DOI] [PubMed] [Google Scholar]
Ulett 1998
- Ulett GA, Han S, Han JS. Electroacupuncture: mechanisms and clinical application. Biological Psychiatry 1998;44:129‐38. [DOI] [PubMed] [Google Scholar]
Wang 2008
- Wang BQ, Ling M. Research development of Chinese herbal medicine for PCOS. Shandong Journal of Traditional Chinese Medicine 2008;27(2):138‐40. [Google Scholar]
Wild 2000
- Wild S, Pierpoint T, Jacobs H, McKeigue P. Long‐term consequences of polycystic ovary syndrome: results of a 31 year follow‐up study. Human Fertility 2000;3(2):101‐5. [DOI] [PubMed] [Google Scholar]
Witt 2009
- Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forschende Komplementärmedizin/Research in Complementary Medicine 2009;16:91‐7. [DOI] [PubMed] [Google Scholar]
Xue 2007
- Xue CC, Zhang AL, Lin V, Costa C, Story D. Complementary and alternative medicine use in Australia: a national population‐based survey. Journal of Alternative and Complementary Medicine 2007;13(6):643‐50. [DOI] [PubMed] [Google Scholar]
Zhang 2010
- Zhang J, Li T, Zhou L, Tang L, Xu L, Wu T, et al. Chinese herbal medicine for subfertile women with polycystic ovarian syndrome. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD007535.pub2] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Lim 2016
- Lim CE, Ng RW, Xu K, Cheng NC, Xue CC, Liu JP, Chen N. Acupuncture for polycystic ovarian syndrome. Cochrane Database of Systematic Reviews 2016, Issue 5. [DOI: 10.1002/14651858.CD007689.pub3] [DOI] [PubMed] [Google Scholar]


