
INTRODUCTION
The present article describes the course of history of spinal surgery in Japan from the pioneering period to the progressive era (1911–2017), and the history of progression surrounding the establishment of the Neurospinal Society of Japan (1986) to present-day developments.
The essential features of this article comprise the following five papers: “The history of spinal surgery in the field of neurosurgery of Japan” by Dr. Satoru Kadoya [1]; “Advancements in spinal surgery” [2]; “The history of spinal surgery in Japan: from the pioneering period to the progressive era” [3]; “The history of spinal surgery in Japan (part 2): the latter half of the progressive era (2000–2017)” [4] by the author (Hiroshi Abe); and “The history of Japanese spinal surgery and problems to be solved expeditiously” by Dr. Junya Hanakita [5].
THE PIONEERING PERIOD (1911–1959)
The surgical removal of a spinal cord tumor (C6 neurinoma) performed by Hayari Miyake in 1911 was the first procedure on record in the field of spinal surgery in Japan (Fig. 1) [6,7]. The patient was a 30-year-old woman who developed tetraplegia and abasia over consequent 5 years. Miyake diagnosed a tumor located in the cervical C5 and C6 regions on the basis of the patient’s history and neurological symptoms. Surgery was performed in the lateral position with chloroform–ether combination anesthesia. A walnut-sized elliptical tumor was removed, and the surgery was completed upon closing the dura mater with sutures [8]. The patient experienced liquorrhea up to postoperative day 15; however, the surgical wound healed, and the patient gained the ability to walk after approximately 1.5 months. Seiichiro Sato, the surgical assistant, reported in detail the difficulties experienced during the postoperative management of this case [8].
Fig. 1.
Hayari Miyake
Around the same period, Hayazo Ito reported 6 cases of laminectomy. In 1949, Masaru Kuru reported cordotomy for treating pain. In 1950, Kenji Tanaka reported “cervical spinal cord surgery” performed in the lateral position, and in 1952, Dennosuke Jinnai reported three cases of spinal cord tumors [1].
EARLY STAGE (1960–1979)
Mitsuo Tsuru (Fig. 2) presented the surgical outcomes of 38 cases of cervical spondylosis in 1960 and 1962 [9,10]. All procedures were posterior decompression (laminectomy). Tsuru was trained in neurosurgery for 6 years in the USA, where he was the first Japanese physician to obtain a board-certified neurosurgeon from the American Board of Neurosurgery. He subsequently returned to Japan in 1957. From 1958, he commenced neurosurgical practice at Hokkaido University Hospital. Brain diseases and spinal diseases were treated equally at Hokkaido University, where both the number of patients and surgeries were approximately the same for the brain and spine.
Fig. 2.
Mituso Tsuru
In 1962, Kenzo Yada (Fig. 3) reported 40 cases of early decompression for spinal cord injury [11]. Yada was also trained in the USA and became the third Japanese physician to obtain a board-certified neurosurgeon from the American Board of Neurosurgery, after which he returned to Japan in 1960. Yada graduated from Keio University and, rather than returning to his original school to work, he joined Hokkaido University, where Tsuru, who he had met in the USA, was working. Yada proactively devoted himself to surgery for spinal disease.
Fig. 3.

Kenzo Yada
In 1964, Chikao Nagashima (Fig. 4), who had been trained in the Department of Neurosurgery University of Tokyo, studied spinal surgery outside of Japan under Dr. Scoville and reported his experience of four cases of Scoville surgery (laminectomy+facetectomy) [12] upon returning to Japan.
Fig. 4.

Chikao Nagashima
These 3 individuals, Mitsuo Tsuru, Kenzo Yada, and Chikao Nagashima, presented surgery for various types of spinal diseases each year up to the late 1960s and were a driving force for spinal surgery in the early stage in Japan.
While spinal surgery–related papers began to be presented at the Annual Meeting of the Japan Neurological Society from this period onward, less than 10 presentations had been made in each Meeting by 1964 [5].
A spinal surgery–related topic was first selected as the symposium in 1967 with the title of “whiplash injury.” In 1968, “whiplash injury” was selected again. Subsequently, the topics, “spinal surgery” in 1971, and “cervical spine and spinal cord surgery” in 1973 were selected [1]. Thereafter, rapid increases were noted in the number of presentations on spinal surgery–related subjects in both the symposia and general sessions of the Annual Meeting of Japan Neurological Society.
During this period, the Japan Medical Society of Paraplegia (later named the Japan Medical Society of Spinal Cord Lesions) contributed to the development of spinal surgery in Japan. The society held their first scientific meeting in 1960. Initially, the society consisted of orthopedic surgeons and urologists, and the presentations were mostly related to spine and spinal cord injury, subsequent sequelae, and rehabilitation. Thereafter, neurosurgeons were added, and in 1960, Mitsuo Tsuru served as the president of the 15th Annual Meeting of Paraplegia. Subsequently, neurosurgeons actively took part, and Kenzo Yada served as the president of the 18th Meeting (1983), succeeded by Hiroshi Abe in the 24th Meeting (1989), Satoru Kadoya in the 30th Meeting (1995), Hiroshi Nakagawa in the 38th Meeting (2003), Yoshinobu Iwasaki in the 43rd Meeting (2008), Junya Hanakita in the 47th Meeting (2012), and Masakazu Takayasu in the 53rd Meeting (2018) (Table 1).
Table 1.
Japan Medical Society of spinal cord lesion
| Year | President | Specialty | Place | |
|---|---|---|---|---|
| 1st | 1966 | Tamikazu Tenji | Orthopedics | Beppu |
| 2nd | 1967 | Torao Iwahara | Orthopedics | Tokyo |
| 15th | 1980 | Mitsuo Tsuru | Neurosurgery | Sapporo |
| 18th | 1983 | Kenzo Yada | Neurosurgery | Yokohama |
| 24th | 1989 | Hiroshi Abe | Neurosurgery | Sapporo |
| 30th | 1995 | Satoshi Kadoya | Neurosurgery | Kanazawa |
| 38th | 2003 | Hiroshi Nakagawa | Neurosurgery | Aichi |
| 43rd | 2008 | Yoshinobu Iwasaki | Neurosurgery | Sapporo |
| 47th | 2012 | Junya Hanakita | Neurosurgery | Shizuoka |
| 53rd | 2018 | Masakazu Takayasu | Neurosurgery | Nagoya |
When Tsuru first started participating in this society in the 1960s, upon announcing early decompression for spinal cord injury caused by vertebral fracture and dislocation, Torao Iwahara (Department of Orthopedic Surgery, Keio University) remarked that “an injured spinal cord looks like a banana that has been stepped on, and that even if decompression is performed quickly, it will not change the possibility of recovery.” Later, Tsuru confided into me that he was very resentful of this comment.
In 2002, the name of the society was changed to the “Japan Medical Society of Spinal Cord Lesion” during the 37th Meeting. Presently, as medical departments that participate in the society, the department of rehabilitation, and neurology have been added. President of this society also have now come to be selected from the above departments.
PROGRESSIVE ERA (1980–2017)
From 1980 to 2001, the Spinal Cord Symposium, which was held 22 times, greatly contributed to the development of spinal surgery in Japan. The members of founders comprised a total of 10 individuals who were selected from the departments of neurosurgery, orthopedic surgery, neurology, and neuroradiology (Table 2).
Table 2.
The theme and chairman of spine and spinal cord symposium
| Year | Theme | Chairman | |
|---|---|---|---|
| 1st | 1980 | Anomaly of Craniocervical Junction | Mitsuo Tsuru |
| 2nd | 1981 | Cervical Spondylotic Myelopathy | Shunichi Inoue |
| 3rd | 1982 | Neuroradiology of Spinal Cord | Toru Mannen |
| 4th | 1983 | Syringomyelia | Kenzo Yada |
| 5th | 1984 | Incomplete lesion of Spinal Cord by Trauma and chronic compression | Keiro Ono |
| 6th | 1985 | Approach to spastic paraplegia | Tsutomu Yanagi |
| 7th | 1986 | Ossification and calcification of Spinal ligament | Chikao Nagashima |
| 8th | 1987 | Pain due to Spinal Cord | Takaaki Igata |
| 9th | 1988 | Image Diagnosis of Diseases of the Spinal Cord | Naoki Kobayashi |
| 10th | 1989 | Deformity of the Spine | Hisao Ikeda |
| 11th | 1990 | Syringomyelia | Satoshi Kadoya |
| 12th | 1991 | Electric Diagnosis of Spinal Cord | Takahide Kurokawa |
| 13th | 1992 | Image Diagnosis of Spinal Cord | Kazuo Miyasaka |
| 14th | 1993 | Cervial Spondylosis | Kiyoharu Inoue |
| 15th | 1994 | Vascular Diseases of Spinal Cord | Masamichi Tomonaga |
| 16th | 1995 | Spinal Arachnoiditis | Eizo Yoshizawa |
| 17th | 1996 | Spinal Disraphism | Tadayuki Maehara |
| 18th | 1997 | HTLV-1 Associated Myelopathy | Eisaku Ohama |
| 19th | 1998 | Diagnosis and Therapy of Spinal Cord Tumor | Hiroshi Abe |
| 20th | 1999 | Traumatic Spinal Cord Injury | Shinya Kawai |
| 21th | 2000 | Image Diagnosis of Diseases of Spinal Cord | Shinichi Suga |
| 22nd | 2001 | Spine 2001 –Prospect for Future– | Hiroshi Abe, Takaaki Igata |
The theme of the first Spinal Cord Symposium was Anomalies of the craniovertebral junction (CVJ) and was held in Tokyo, with Mitsuo Tsuru serving as the president. The venue was filled with enthusiastic individuals who exchanged arguments during heated discussions. Thereafter, the succeeding Spinal Cord Symposium that was held in Tokyo once a year with different themes. The themes and presidents from the 1st to the 22nd Spinal Cord Symposium are presented in Table 2. The final Symposium was held in 2001; it was hosted by 2 people, Hiroshi Abe and Takaaki Igata; had a theme of “Spine 2001—future prospects—”; and ended on a successful note.
In 1986, the Japanese Society of Spinal Surgery, which became the Neurospinal Society of Japan in 2016, was finally established by Japanese neurosurgeons. Shuro Nishimura (Fig. 5) and Akira Hakuba dedicated themselves to the foundation of the meeting, and the secretariat was established in the Department of Neurosurgery, Osaka City University, to which they belonged. Table 3 presents the 11 members of founders at the time of the inauguration. The first meeting was held in Tokyo in 1986, with Kenzo Yada serving as the president. The meeting was held for only one day; furthermore, the venue was very crowded since it was a single site. The symposium addressed “cervical spondy-losis” for 3 hours in the morning. For the afternoon sessions, only selected 24 papers out of the submitted 51 abstracts were presented. The subject titles and presenters in the symposium are listed in Table 4. Heated discussions were held regarding the choice of the anterior and posterior approaches, or the indication of anterior surgery without bone graft as the surgical procedure for cervical spondylosis. All presenters were debaters who could not be stopped once they started talking, and Hiroshi Abe, who was the symposium chairman, had difficulty closing the symposium [13]. The Society had been officially recognized as the study group since 1986. In 1998, at the time of the 13th meeting, the study group became the society. The successive presidents and venues from the 1st to the 33rd Meeting are presented in Table 5. At the 33rd Meeting of the Neurospinal Society of Japan (2018, Nara), the number of presentations had increased to a total of 450 papers, including 7 symposia with 39 papers, 178 oral presentations, 216 poster presentations, special lectures, educational lectures, luncheon seminars, afternoon seminars, hands-on seminars, and so on.
Fig. 5.
Shuro Nishimura
Table 3.
Proposers of the Japanese Society of Spinal Surgery 1986
| Hiroshi Abe |
| Akira Hakuba |
| Satoshi Kadoya |
| Kazuo Kinoshita |
| Tsunemaro Koyama |
| Satoshi Matsumoto |
| Chikao Nagashima |
| Hiroshi Nakagawa |
| Masamichi Tomonaga |
| Kenzo Yada |
| Hiroshi Yamada |
Table 4.
Symposium “cervical spondylosis”
| Subject | Specker | |
|---|---|---|
| 1st | Mechanism of neurological symptoms | Shigekuni Tachibana |
| 2nd | Anterolateral approach to cervial spondylosis –results of 310 cases– | Akira Hakuba |
| 3rd | Cervical spondylosis –surgical methods– | Satoshi Kadoya |
| 4th | Microsurgical anterior approach to cervical disc disease with narrow canal | Hiroshi Nakagawa |
| 5th | Bilateral medial facetectomy and laminectomy | Chikao Nagashima |
| 6th | Surgical indication of cervical disc disease | Yoshinobu Iwasaki |
Table 5.
Neurospinal Society of Japan
| Year | Successive presidents | Place | |
|---|---|---|---|
| 1st | 1986 | Kenzo Yada | Tokyo |
| 2nd | 1987 | Chikao Nagashima | Tokyo |
| 3rd | 1988 | Masamichi Tomonaga | Fukuoka |
| 4th | 1989 | Kazuo Kinoshita | Miyazaki |
| 5th | 1990 | Satoshi Matsumoto | Kobe |
| 6th | 1991 | Satoshi Kadoya | Kanazawa |
| 7th | 1992 | Hiroshi Abe | Sapporo |
| 8th | 1993 | Akira Hakuba | Osaka |
| 9th | 1994 | Shiro Waga | Tsu |
| 10th | 1995 | Haruhiko Kikuchi | Kyoto |
| 11th | 1996 | Hiroshi Nakagawa | Nagoya |
| 12th | 1997 | Akinori Kondo | Osaka |
| 13th | 1998 | Tsunemaro Koyama | Otsu |
| 14th | 1999 | Hiroshi Takahashi | Tokyo |
| 15th | 2000 | Norihiko Tamaki | Kobe |
| 16th | 2001 | Isao Yamamoto | Yokohama |
| 17th | 2002 | Junya Hanakita | Shizuoka |
| 18th | 2003 | Toshiaki Abe | Tokyo |
| 19th | 2004 | Norihiko Kubota | Fukui |
| 20th | 2005 | Yoshinobu Iwasaki | Sapporo |
| 21st | 2006 | Hideaki Iizuka | Kanazawa |
| 22nd | 2007 | Kim Phyo | Omiya |
| 23rd | 2008 | Teiji Tominaga | Matsushima |
| 24th | 2009 | Asakazu Goya | Miyazaki |
| 25th | 2010 | Masakazu Takayasu | Nagoya |
| 26th | 2011 | Shigekuni Tachibana | Numatsu |
| 27th | 2012 | Masanori Ito | Urayasu |
| 28th | 2013 | Motoi Shoda | Nagoya |
| 29th | 2014 | Junichi Mizuno | Tokyo |
| 30th | 2015 | Kazutoshi Hida | Sapporo |
| 31st | 2016 | Satoru Tani | Tokyo |
| 32nd | 2017 | Kenji Ohata | Osaka |
| 33rd | 2018 | Hiroyuki Nakase | Nara |
| 34th | 2019 | Izumi Koyanagi | Sapporo |
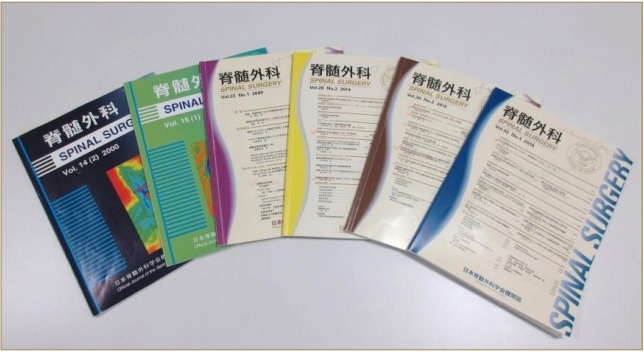
Volume one of Spinal Surgery was published in 1987, as the official journal of the society (Fig. 6). The first chief editor was Akira Hakuba, who held the position for 10 years until volume 10 (1997). The second chief editor was Hiroshi Abe, who held the position from volumes 11 to 14 (1997–2000). The third chief editor was Hiroshi Nakagawa from volumes 15 to 21 (2001–2007); the fourth chief editor was Toshiaki Abe from volumes 22 to 24 (2008–2010); the fifth chief editor was Phyo Kim from volumes 25 to 29 (2011–2015); the sixth chief editor was Masakazu Takayasu from volumes 30 to 32 (2016–2018); and the seventh chief editor was Makoto Taniguchi from volume 33 onwards (2019 to present) (Table 6) (Fig. 7).
Fig. 6.
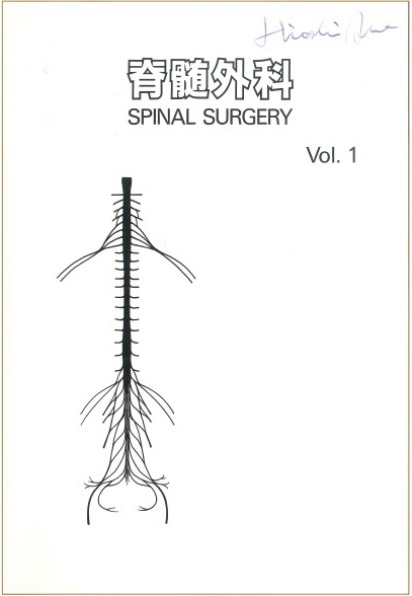
Spinal Surgery Vol.1, 1987.
Table 6.
Chief editors of “spinal surgery”
| Editor | Volume | Year |
|---|---|---|
| Akira Hakuba | 1–10 | 1987–1997 |
| Hiroshi Abe | 11–14 | 1997–2000 |
| Hiroshi Nakagawa | 15–21 | 2001–2007 |
| Toshiaki Abe | 22–24 | 2008–2010 |
| Phyo Kim | 25–29 | 2011–2015 |
| Masakazu Takayasu | 30–32 | 2016–2018 |
| Makoto Taniguchi | 33– | 2019– |
Fig. 7.
Spinal Surgery Vol. 11-33, 1997-2019.
In 2005, the Japanese Society of Spinal Surgery decided to change the organizing committee system to the board of directors. In 2006, Hiroshi Nakagawa was elected as the first chief director, and 23 directors were selected. In 2008, Junya Hanakita was elected as the second chief director, and, in 2013, Phyo Kim was elected as the third chief director, who still holds the position. As of 2018, there were 29 directors.
The English name of the society was the Japanese Society of Spinal Surgery (JSSS) from 1986 to 2016. In 2016, the name was changed to the Neurospinal Society of Japan. In 2002, the Board certification system was established in the JSSS. In 2003, 29 board certified spinal surgery instructors and 12 training facilities were approved. In 2005, 170 were approved as certified spinal surgeon. In 2018, the numbers had increased to 127 certified instructors and 486 certified surgeons (now 1,281 in total members).
In 2009, the Japanese Medical Specialty Board requested the creation of a new board system for spinal surgeon, which comprised neurosurgeons and orthopedic surgeons. In 2016, as a result of repeated discussions among the representative neurosurgeons and orthopedic surgeons, a system was put into action and started a combined board certification system of spinal surgeon in 2017.
LEADERS WHO CONTRIBUTED TO THE DEVELOPMENT OF SPINAL SURGERY IN JAPAN
This section describes the leaders and pioneers in Japan who contributed to the development of spinal surgery from the 1960s to the late 1990s.
1. Mitsuo Tsuru (Fig. 8)
Fig. 8.

Mitsuo Tsuru
Tsuru studied neurosurgery in Boston and was the first Japanese to obtain a board-certified neurosurgeon in the USA. In the 1960s, he was a driving force for spinal surgery in Japan, achieving successful surgical treatment for several spinal diseases, including cervical spondylosis, spinal cord trauma, and spinal cord tumors. Thereafter, neurosurgeons had been performing spinal surgery routinely as a common practice. Moreover, he made the pioneering orthopedic surgeons recognize the efforts of the neurosurgeons in spinal surgery.
On the outside, Tsuru often appeared as a cheerful American gentleman. However, he provided tough instructions to residents, and in the operating theater, his thunderous voice echoed to the other far distant operating theaters.
2. Kenzo Yada (Fig. 9)
Fig. 9.

Kenzo Yada, Mitsuo Tsuru, Hiroshi Abe (from left).
Yada also studied neurosurgery in Boston, where he acquired a board-certified neurosurgeon in the USA before returning to Japan. At the Hokkaido University Hospital, he performed surgeries for all kinds of spinal diseases and achieved excellent outcomes especially in the early reduction and decompression of spinal cord injury [11], posterior decompressions for cervical ossification of the posterior longitudinal ligament (OPLL) [14], thoracic OPLL and spinal cord tumor.
Yada was a good English speaker with clear voice, and held assertive arguments equally with Tsuru. From his freshman years, Hiroshi Abe received guidance from Yada. Yada’s tough guidance was not similar to Tsuru’s use of a loud voice, but what he said was accurate and well-reasoned, against which Hiroshi Abe had no chance to argue.
3. Chikao Nagashima (Fig. 10)
Fig. 10.
Chikao Nagashima
Together with Tsuru and Yada, Nagashima was a driving force for spinal surgery in Japan from the 1960s to the 1970s. He proposed and achieved excellent results with laminectomy+facetectomy [15] for cervical spondylosis [12] and cervical OPLL. He also reported on posterior fixation for atlantoaxial dislocation and surgery for vertebral insufficiency caused by cervical spondylosis. Nagashima was good at drawing and always printed his intraoperative sketches in his articles.
4. Satoshi Matsumoto (Fig. 11)
Fig. 11.
Satoshi Matsumoto
Satoshi Matsumoto was the first pediatric neurosurgeon who was devoted to the establishment of pediatric neurosurgery in Japan. In the field of spinal surgery, his achievements for spina bifida have been outstanding [16]. In particular, he proposed his opinion that tethered cord syndrome and low conus should be clearly distinguished from each other [17]. Following retirement from Kobe University, he founded the Japan Spina Bifida and Hydrocephalus Foundation, which is a public service corporation, to help elucidating the cause and advancements in treatment methods for spina bifida. Matsumoto was a warmhearted gentleman who also had a stubborn side and would never bend his theory.
5. Haruhiko Kikuchi (Fig. 12)
Fig. 12.
Haruhiko Kikuchi
Kikuchi spent several years learning microsurgery under Professor Yasargil; he introduced microsurgery to Japan in the late 1960s and popularized it. He was an authority on microscopic surgery. In surgeries for cervical aneurysm and cerebral arteriovenous malformation (AVM), he was second to none. In the field of spinal surgery, he reported his experience of 11 cases of spinal AVM treated for the first time in Japan [18].
While Hiroshi Abe was working at Hokkaido University, he invited Kikuchi to perform surgeries at Hokkaido University Hospital for several times. Kikuchi’s surgery was rapid, skillful, had no unnecessary maneuvers, and the intraoperative silence was, by far, the best. He was an unperturbable samurai warrior.
6. Satoru Kadoya (Fig. 13)
Fig. 13.

Satoru Kadoya
Kadoya spent several years engaged in research on spinal cord injury at Cleveland Clinic and, upon returning to Japan, he helped popularize spinal surgery in Japan, where he achieved many accomplishments. In 1985, Kadoya first reported the Smith-Robinson procedure by microsurgery in Japan [19]. Furthermore, he proposed a grading and scoring system for the neurologic symptoms in cervical spondylosis [20], and he proactively engaged in efforts and achieved many accomplishments for lumbar diseases [21]. Kadoya had a warm personality; however, with his theory at the core, he was calm and confident.
7. Akira Hakuba (Fig. 14)
Fig. 14.
Akira Hakuba
Hakuba received training as a resident for several years under Professor Malis. Upon acquiring a boardcertified neurosurgeon in USA, he returned to Japan, where he achieved many accomplishments in skull base surgery and spinal surgery. Hakuba reported excellent results with his original transuncodiscal approach for cervical spondylosis [22]. He also reported the transoral approach [23] and expansive suboccipital cranioplasty for syringomyelia [24]. Hakuba was also an excellent English speaker and was high-spirited at scientific meetings, where he poured out sharp questions and remarks.
8. Tsunemaro Koyama (Fig. 15)
Fig. 15.
Tsunemaro Koyama
Koyama studied spinal surgery under the guidance of Professor Kraynbuel before he returned to Japan, where he achieved many accomplishments on spinal surgery. Koyama reported the effectiveness of the postero-lateral pia mater incision for intramedullary spinal cord tumors, depending on the localization of the tumor [25]. Furthermore, as a spinal surgeon, he achieved many accomplishments in the field of surgery for lumbar disease, asserting that both cervical disease and lumbar disease should be firmly addressed [26]. He reported the use of hydroxyapatite in cervical spondylosis [27]. On the basis of his experience in many cases of cervical and lumbar diseases, Koyama’s calm remarks carried weight and were understood by all.
9. Hiroshi Nakagawa (Fig. 16)
Fig. 16.

Hiroshi Nakagawa
Nakagawa was trained as a resident for several years in Boston and New York under Professor Malis. Upon acquiring a board-certified neurosurgeon in the USA, he returned to Japan. Prior to studying abroad, Nakagawa received tough guidance and training under Tsuru, similar to how Hiroshi Abe was trained, at the same Department of Neurosurgery, Hokkaido University. After returning to Japan, Nakagawa assumed a new post as an associate professor at Aichi Medical University, where he worked to promote spinal surgery. He achieved many accomplishments, including anterior surgery without bone graft for cervical spondylosis and disc [28], anterior decompression and fusion of cervical OPLL [29], and instrument surgery for spinal disease [30]. He continued active spinal surgery practice after retirement from Aichi Medical University. At present, he performs surgeries on several cases per week and instructs young physicians.
MAJOR POINTS IN THE HISTORY OF SPINAL SURGERY FOR SPINAL CORD DISEASE IN JAPAN
1. Cervical spondylosis (Table 7)
Table 7.
Cervical spondylosis, disc
| Year | Posterior approach |
Anterior approach |
||
|---|---|---|---|---|
| Author | Method | Author | Method | |
| 1960 | Tsuru | Laminectomy | ||
| 1963 | Tsuru | Cloward method | ||
| 1968 | Nagashima | Laminectomy | ||
| Microsurgery | ||||
| 1976 | Kirita | Laminectomy | Hakuba | Trans-unco-discal approach |
| 1978 | Hattori | Laminoplasty | ||
| 1979 | Hirabayashi | Laminoplasty | Kadoya | Smith-Robinson method |
| 1980 | Nakagawa | Without bone graft | ||
| 1982 | Kurokawa | Laminoplasty | Iwasaki | Smith-Robinson method |
| 1985 | Koyama | Hydoroxyapatite | ||
| 1988 | Koyama | Laminoplastymicrosurgery | ||
| 1992 | Isu | Williams-Isu method | ||
| 1995 | Kawai | Laminoplasty | ||
| Microsurgery | ||||
| 1998 | Hanakita | Bilateral open-door laminoplasty | Kim | Hydoroxyapatite |
| 1999 | Nakagawa | Titanium cage | ||
| 2000 | Shiokawa·Hanakita | Bilateral open-door laminoplasty | Kubo | Titanium cage |
| 2000 | Hida | Titanium cage | ||
| 2000 | Hoshimaru | Hydoroxyapatite | ||
| 2001 | Goto·Ohata | Bilateral open-door laminoplasty | Nishimura | Hydoroxyapatite |
| 2002 | Takayasu | Bilateral open-door laminoplasty | Kuribayashi | Hydoroxyapatite |
| 2003 | Harada | Hydoroxyapatite | ||
| 2004 | Koyanagi | Titanium cage | ||
| 2006 | Yuki | Titanium cage | ||
| 2007 | Kim | Spinolaminoplasty | Mizuno | Titanium cage |
| 2008 | Horikoshi | Titanium cage | ||
| 2009 | Imamura | Titanium cage | ||
| 2009 | Yasumoto | Titanium cage | ||
| 2012 | Takayasu | Titanium cage | ||
Surgery for cervical spondylosis began in 1958 at Hokkaido University Hospital after Tsuru returned to Japan from his study in the USA. At that time, the only procedure that was being performed was posterior decompression (laminectomy). Although this improved spinal cord symptoms, root injury frequently occurred due to excessive posterior movement of the spinal cord. As a means to solve this problem, Scoville [31] reported a method of combining facetectomy with laminectomy to open the intervertebral foramen by a posterior approach. Using his own cases, Nagashima introduced Scoville’s method to Japan in 1964 [12].
Kirita reported the use of extensive simultaneous laminectomy to decompress the spinal cord in one manipulation (i.e., the double open-door method), to avoid spinal cord injury caused by decompression of the lamina one by one [32]. This revolutionary method gained widespread popularity.
In the latter half of the 1970s, various types of laminoplasty were reported by orthopedic surgeons. In the field of neurosurgery, Koyama provided the first publication [33]. In time, laminoplasty gained widespread popularity for its advantages over laminectomy, in terms of maintaining postoperative cervical spine alignment and the avoidance of swan neck. Thereafter, various laminoplasty procedures were published, including spinolaminoplasty [34,35], bilateral open-door laminoplasty [36-38], and open-door laminoplasty [39]. For most laminoplasty procedures, fixation is performed using devices such as a ceramic spacer and a miniplate.
On the contrary, the anterior approach to the cervical spine, reported by Cloward [40] in 1950, gained widespread popularity as a revolutionary method in the 1960s. Tsuru introduced the original Cloward method to Japan in 1963 [41]. In 1976, Hakuba [22] reported excellent results using the transuncodiscal anterior approach by microscopic surgery. Kadoya et al. [42] also reported excellent results with the Smith-Robinson method by microscopic surgery. From this point onward, the anterior approach by microsurgery has gained widespread popularity and dramatically improved outcomes. In 1992, Nakagawa et al. [28] reported an anterior procedure without bone graft. In 1986, Iwasaki et al. [43] reported the Smith-Robinson method.
In 1986, Koyama and Handa [27] reported an experience of using hydroxyapatite to prevent complications, such as iliac bone pain associated with bone graft harvesting for anterior fixation. Likewise, Kim et al. [44] and Hoshimaru and Koyama [45] reported their experiences with the use of hydroxyapatite.
In 1992, Isu et al. [46] reported the Williams-Isu method of using a part of the vertebral body as another method to prevent iliac bone problems. In this method, the wide operative field enabled removal of large bone spurs and herniated discs.
In 1999, Nakagawa et al. [47] reported an experience of using a titanium cage as artificial bone. In 2000, Kubo et al. [48] and Hida et al. [49] reported similar experiences with the use of a titanium cage. Thereafter, reports of the use of a titanium cage suddenly increased. The use of a cylindrical cage was reported by Koyanagi [50] and Imamura et al. [51], whereas the use of a box-shaped cage was reported by Takayasu [52], Yasumoto et al. [53], and Yuki et al. [54] The experience of using both types of cage was reported by Mizuno and Sano [55] and Horikoshi et al. [56]; the latter reported that the box-shaped cage resulted in less postoperative subsidence [57].
For cervical spondylosis, the choice of the anterior approach and posterior decompression had been a point of discussion for a long time [58]. Although posterior decompression had been considered suitable for cervical spondylosis that affects multiple intervertebral spaces with a narrow canal, the author believes that the anterior approach by microsurgery should be performed for all other cases of cervical spondylosis (70%–80%).
2. Cervical OPLL (Table 8)
Table 8.
Cervical ossification of the posterior longitudinal ligament
| Year | Posterior decompression |
Anterior decompression |
||
|---|---|---|---|---|
| Author | Method | Author | Method | |
| 1972 | Nagashima | Laminectomy | ||
| 1976 | Kirita | Laminectomy | Sako | Corpectomy |
| 1976 | Yamaura | Corpectomy | ||
| 1977 | Manabe | Corpectomy | ||
| 1977 | Kamikozuru | Corpectomy | ||
| 1978 | Kataoka | Laminoplasty | Watanabe | Corpectomy |
| 1979 | Hirabayashi | Laminoplasty | ||
| Microsurgery | ||||
| 1980 | Abe | Corpectomy | ||
| 1982 | Kurokawa | Laminoplasty | ||
| 1984 | Kawai | Laminoplasty | ||
| 1987 | Kojima | Corpectomy | ||
| 1994 | Obara | Anterolateral vertebrotomy | ||
| 1995 | Nagashima | Laminoplasty | ||
| 1996 | Nakagawa | Corpectomy | ||
| 1997 | Igarashi · Koyama | Laminoplasty | Mizuno·Nakagawa | Corpectomy |
| 1997 | Morimoto | Laminoplasty | Hida·Abe | Corpectomy |
| 1977 | Kojima·Waga | Corpectomy | ||
| 1999 | Takayasu | Anterolateral vertebrotomy | ||
| 2001 | Nishiura | Anterolateral vertebrectomy | ||
As in cervical spondylosis, posterior decompression for cervical OPLL gained popularity in the late 1960s. Procedures such as laminectomy+facetectomy by Nagashima [15] and extensive simultaneous laminectomy by Kirita [32,57] were performed.
From the 1970s, orthopedic surgeons started to perform various types of laminoplasty. In neurosurgical practice, Nagashima and Yoshizawa [59], Igarashi et al. [60], and Morimoto [61] also published reports on laminoplasty.
On the contrary, anterior decompression and fusion for cervical OPLL is an ideal way of extracting lesions (i.e., ossified ligaments) by an anterior approach; this had been attempted and reported successively by orthopedic surgeons, including Sakoh [62] and Yamaura [63] in 1976, Manabe and Nomura [64] and Kamikozuru et al. [65] in 1977, and Watanabe et al. [66] in 1978. However, the surgical procedures used by all these pioneers was macroscopically performed and included many problems, such as surgical complications and a large volume of blood loss. The outcome was not concluded to be good.
In Europe and the USA, reports on anterior decompression for cervical OPLL included 20 cases by Harsh et al. [67] in 1987 and 18 cases by Herkowitz in 1988 [68]. Notably, the Japanese pioneers had performed anterior decompression 10 years earlier than their Western counterparts. I would like to express my respect for the bravery of the Japanese pioneers who resolutely challenged the difficult anterior decompression. Considering that anterior decompression by microsurgery may reduce complications, the author carefully and cautiously attempted anterior decompression by microsurgery for a small OPLL, and the results were surprisingly good [69].
In 1981, I reported the results of 12 cases of anterior decompression and fusion for cervical OPLL to the Journal of Neurosurgery [70]. This was the first worldwide report on anterior decompression and fusion for cervical OPLL by microsurgery. The subsequent responses were great, and from the orthopedic surgeons in New York and from the neurosurgeons in Hawaii and Korea, many patients with cervical OPLL were referred to Hokkaido University Hospital [71]. Thereafter, anterior decompression by microsurgery was reported by Kojima et al. [72] in 1987 and by Nakagawa and Mizuno [29] in 1989 and was eventually popularized as a refined procedure that improved outcomes. In 1997, Mizuno et al. [73] performed anterior decompression on 121 patients and reported that the postoperative outcomes for myelopathy were excellent and good in 89% of the patients. In the same year, Hida et al. [74] performed anterior decompression on 132 patients and reported excellent and good outcomes for the upper limbs in 94% of the patients and for the lower limbs in 97% of the patients. Kojima et al. [75] reported that, among 64 patients, anterior decompression had excellent outcomes in 80% of the patients prior to 1993 and in 100 % of the patients from 1993 to 1997.
In these reports, all vertebral body defects were reconstructed with autologous iliac bone. From the late 1990s onwards, artificial bones, such as mesh cage or distractable vertebral body substitute, had been used for avoiding troubles associated with iliac bone harvesting. Moreover, the method of vertebral body decompression by vertebrectomy from an anterolateral approach, rather than from a midline approach, was reported by Ohara et al. [76], Takayasu et al. [77], and Nishiura et al. [78] In some cases, with decompression alone, fixation was not necessarily required; therefore, the procedure is less invasive, compared with midline decompression.
As for cervical spondylosis, the choice between anterior and posterior decompression for cervical OPLL remains controversial. However, the author believes that when the continuity of the OPLL is long (i.e., exceeding three vertebral bodies and four intervertebral spaces) and when there is no localized prominence, posterior decompression should be performed; for other instances, anterior or anterolateral decompression should be indicated.
3. Spinal AVMs (Table 9)
Table 9.
Spinal arteriovenous malformation
| Year | Author | Author (Japanese) |
|---|---|---|
| 19,671,971 | Di Chiro | |
| 19,701,971 | Djindjian | |
| Microsurgery | ||
| 19,701,971 | Yasargil | |
| 1975 | Pia | |
| 1976 | Kikuchi | |
| 19,761,982 | Karasawa · Kikuchi | |
| 1979 | Malis | |
| 1982 | Saito | |
| 19,831,988 | Oldfield | |
| 1986 | Heros | |
| 19,921,999 | Berenstein | |
| 19,931,980 | Merland, Mourier | |
| 1994 | Barrow | |
| 1995 | Goto | |
| 1997 | Bao | Miyasaka |
| 1998 | Miyamoto | |
| 1998 | Ogata · Goto | |
| 1999 | Hida· Abe | |
| 2002 | Spetzler | Miyamoto |
| 2003 | Lasjaunias | Hida |
| 2013 | Matsumaru |
The treatment of spinal AVM has progressed rapidly since the disease stage classification was elucidated by neuroradiologists Di Chiro et al. [79] and Djindjian [80].
In the 1970s, surgical treatment was reported by the pioneers Yasargil [81], Pia [82], and Malis [83]. In Japan, the first study was reported by Kikuchi on 11 patients [18]. This led to the popularization of the concept of and treatment for spinal AVM. Kikuchi [18,84] described the surgical procedures including the feeder artery processing, nidus removal and processing of the draining vein. He reported that clipping and coagulation of the feeder artery alone or incomplete partial removal of nidus were entirely useless. In 1982, Saito [85] also reported the treatment outcomes of 12 patients with spinal AVM and noted that in the perimedullary type of disease, the draining vein does not need to be removed after feeder artery processing and nidus extraction.
In the 1990s, excellent outcomes for endovascular embolization were reported by neuroradiologists Goto [86] and Miyasaka [87]. Reports by Miyamoto et al. [88,89] in 1998 and Hida et al. [90] in 1999 indicated that a combination of embolization and surgery enabled more finely tuned treatment and improved these outcomes.
Thereafter, Mourier et al. [91] in 1993, Spetzler et al. [92] in 2002, and Lasjaunias [93] in 2003 each proposed a classification system for spinal AVM. In recent years, conditions with a nidus had been called AVM, whereas those that simply affected the vessel route without a nidus had been called arteriovenous fistula (AVF) [94].
In recent years, considerable advancements have been made in the field of endovascular treatment [94,95]. Matsumaru et al. [94] reported 31 patients with AVF that were primarily treated with embolization. He reported that additional surgery led to good therapeutic outcomes in patients with incomplete embolization.
From a surgical standpoint, Hida et al. [96] prioritized embolization for dural and epidural AVF as the first line treatment, but additional surgery was performed when the embolization was incomplete. For perimedullary AVF, surgical AV shunt obliteration has been considered the first line treatment because of the presence of collateral arteries in the pia mater. For intramedullary AVM, embolization and stereotaxic radiation were performed [97-99].
The treatment for spinal AVM has progressed remarkably, and the most satisfactory results had been achieved for the dural and perimedullary types. Accumulation of results obtained from endovascular treatment and stereotaxic radiation for the intramedullary type is anticipated.
4. Intramedullary spinal cord tumor (Table 10)
Table 10.
Intramedullary spinal cord tumors
| Year | Author | Case | Author (Japanese) | Case | Histology |
|---|---|---|---|---|---|
| 1907 | von Eiselberg | 1 | |||
| 1913 | von Eiselberg | 13 | |||
| 1967 | Greenwood | 10 | |||
| 1967 | Guidetti | 71 | |||
| Microsurgery | |||||
| 1976 | Yasargil | 12 | |||
| 1978 | Malis | 86 | |||
| 1979 | Stein | 13 | |||
| 1982 | F. Epstein | 19 | |||
| 1986 | Abe | 10 | |||
| 1988 | Stein | 100 | |||
| 1991 | Brotchi | 65 | |||
| 1992 | F. Epstein | 25 | |||
| 1994 | Sonntag | 54 | |||
| 1996 | Brotchi | 171 | |||
| 1997 | Koyama | 25 | Ependymoma | ||
| 1999 | Koyanagi· Abe | 105 | |||
| 1999 | Ohata | 18 | Ependymoma | ||
| 1999 | Hoshimaru · Koyama | 36 | Ependymoma | ||
| 2003 | Nishikawa · Ohata | 69 | |||
| 2005 | Yamamoto | 18 | Hemangioblastoma | ||
| 2005 | Tani | 9 | Hemangioblastoma | ||
| 2014 | Goya | 76 | |||
| 2015 | Takami · Ohata | 24 | Ependymoma | ||
| 2015 | Seki | 33 | Astrocytoma | ||
Surgery for intramedullary spinal cord tumor was reported about one hundred years ago with 1 case reported by von Eiselsberg et al. [100] Thereafter, a large number of cases have been reported, including 13 cases by von Eiselsberg et al. [100] in 1913, 10 cases by Greenwood [101] in 1967, and 71 cases by Guidetti [102] in 1967.
Upon entering the era of microscopic surgery, reports on the dramatic improvement in outcomes were published by Yasargil and De Preux [103] in 1975, Malis [104] in 1978, and Stein [105] in 1979. In 1986 in Japan, Hiroshi Abe [106] was the first to report 10 patients treated by microsurgery. In 1987, Stein reported 100 cases in the Congress of Neurological Surgeons (CNS) in USA. At that time, Hiroshi Abe attended the CNS and, upon hearing Stein’s lecture, was overwhelmed by the excellent intraoperative photographs. He learned a great deal regarding the procedure of tumor removal by midline approach, while ensuring loose tension on the left and right sides of the pia mater with the use of a small thread. Later, in 1996, Brotchi and Fischer [107] reported 171 cases. In Japan, 25 cases of ependymoma were subsequently reported by Fujita and Koyama [25]. Koyama claimed that the incision of the spinal pia mater does not necessarily require a midline approach, but he emphasized that depending on the location of the tumor, an incision of the pia mater can be performed by the postero-lateral approach or from directly above the tumor [108].
In 1999, Koyanagi et al. [109] finally reported their accumulated experience on 105 cases in Japan. In that report, Koyanagi et al. [109] reported that 42 of 105 patients were ependymoma and 97% of them underwent total and subtotal extirpation; their findings showed excellent and good results in 24 patients (57%), with no exacerbation of long-term prognosis. Hoshimaru reported 36 cases of spinal ependymoma. In his report, 34 of them underwent total excision and 14 cases (39%) showed symptomatic improvement [110]. On the basis of the results in 17 cases of total removal out of 18 ependymoma cases, Ohata et al. [111] asserted that total extirpation should be performed for ependymoma whenever possible, while paying due care to avoid injury to the dorsal column. In 2003, Nishikawa et al. [112] reported that 25 of 69 patients with intramedullary tumors were ependymoma and that 24 of them underwent total excision, and 10 (40%) of them demonstrated symptomatic improvement. For ependymoma surgery. Takami et al. [113,114] noted that the tumor margin should be carefully dissected and removed en bloc; Hiroshi Abe completely agreed with this concept [115].
Goya [116], Yamamoto et al. [117], and Tani et al. [118] published reports on hemangioblastoma; in all cases, total extirpation was almost 100% and showed good postoperative outcomes.
Seki et al. [119] reported on 33 patients with astrocytoma. Total or subtotal extirpation of low-grade astrocytoma was achieved in 65%, with a 5-year survival rate of 62%. For high-grade astrocytoma, 90% underwent partial extirpation. A 5-year survival rate of grade III astrocytoma was 63%, while that of grade IV was 0%.
5. Syringomyelia (Table 11)
Table 11.
Syringomyelia with Chiari malformation
| Year | Author | Method |
|---|---|---|
| 1988 | Isu· Iwasaki | Syringo–Subarachnoid shunt |
| 1989 | Hakuba | Gardner’s opposterior fossa decompression |
| 1989 | Toshiaki Abe | Gardner’s opposterior fossa decompression |
| 1990 | Yamaura | Foramen magnum decompression |
| 1990 | Isu | Outer membrane decompression |
| 1995 | Hida | Syringo–Subarachnoid shunt |
| 1997 | Sakamoto · Hakuba | Expansive suboccipital cranioplasty |
| 2004 | Kubota · Yamaura | Foramen magnum decompression |
The theory of Gardner for the mechanism of syringomyelia with Chiari malformation has been well known [120]. In 1969, Williams [121] supported Gardner’s theory, which stated that cerebrospinal fluid circulation disturbance at the foramen magnum causes a difference between the intracranial and spinal cavity pressures, resulting in cerebrospinal fluid influx into the central canal via the obex from the fourth ventricle and the formation of a syrinx within the spinal cord.
On the contrary, Ball and Dayan [122] in 1972 and Aboulker [123] in 1979 explained that disturbance of cerebrospinal fluid circulation increases intravenous pressure, which consequently increases the spinal subarachnoid pressure and forces the cerebrospinal fluid into the spinal cord parenchyma via the Virchow-Robin space. But, this theory did not gain much support, and most people at that time supported the hydrodynamic theory of Gardner.
However, the advent of magnetic resonance imaging (MRI) clarified that the fourth ventricle and syrinx were not connected and completely negated the hydrodynamic theory [124,125]. In 1998, Abe et al. [126] reported that in 87 patients with syrinx, a communication between the fourth ventricle and syrinx could not be confirmed on the MRI findings and by observation during surgery. Furthermore, on the basis of the examination of autopsy cases, Ohama et al. [127] found that the central canal was patent in few cases and asserted that the syrinx initially formed from the posterior root entry zone extending to the dorsal horn.
Previously, the mainstream treatment for syringomyelia was posterior fossa decompression. Batzdorf [128] in 1988 and Milhorat et al. [129] in 1992 also supported the effectiveness of posterior fossa decompression. In Japan, posterior fossa decompression was reported by Hakuba et al. [130] and Abe et al. [131] in 1990. In the same year, Yamaura et al. [132] proposed that posterior fossa decompression should be named foramen magnum decompression to emphasize the importance of decompression of the foramen magnum. This was a revolutionary proposal, to which many people agreed, and, from that time onward, the procedure had been commonly referred to as foramen magnum decompression in Japan. The surgical technique for this foramen magnum decompression gradually changed and evolved over time; The expansive duraplasty using artificial dura substitute without incision of the arachnoid membrane has been more popular. In 1993, Isu et al. [133] reported outer membrane decompression method in which sectioning was only the outer membrane of the dura mater and not opening the inner layer. In 1999, Sakamoto et al. [24] reported the outcomes of expansive suboccipital cranioplasty. In 2004, Kubota et al. [134] performed foramen magnum decompression on 56 patients and reported a reduction in the syrinx in 90% of cases.
On the contrary, collapsing the syrinx can be achieved in a more minimally invasive manner. Syringoperitoneal shunt or syringo–subarachnoid shunt was reported by Phillips and Kindt [135] in 1981, Tator et al. [136] in 1982, Babaro et al. [137] in 1984, and Padovani et al. [138] in 1989. All these reports indicated good outcomes. In 1988, Isu et al. [139] reported a minimally invasive method of using a shunt tube that he invented; the procedure is completed with dural and arachnoid incision of less than 1.0 cm, through which shunting procedures are performed in a small fenestration by hemi-semi laminectomy. This procedure drastically reduced complications of shunt surgery. In 1995, Hida et al. [140] reported good outcomes using the same method.
Foramen magnum decompression may become the first choice of surgical procedure for syringomyelia with Chiari malformation. However, I believe that shunt surgery should be considered for the case with small degrees of Chiari malformation and large size of syrinx that needs quick reduction of the syringomyelia because of urgent symptoms such as pain [141].
6. Spina Bifida (Table 12)
Table 12.
Spina bifida
| Year | Author | Method |
|---|---|---|
| 1978 | Keizo Sakamoto | Spina bifida occulta |
| 1979 | Kaneko | Spina bifida cystica |
| 1983 | Yamada | Meningomyelocele |
| 1985 | Oi | Spina bifida newborn |
| 1985 | Kiyoshi Sato | Intraspinal lipoma |
| 1988 | Oi · Matsumoto | Tethered cord syndrome |
| 1997 | Koyanagi | Lumbar lipoma |
| 1997 | Matsumoto | Tethered cord syndrome |
| 2002 | Arai | Spina bifida occulta |
| 2002 | Arai | Lumbar lipoma |
| 2008 | Koyanagi | Conus lipoma |
Since 1950, the emergent surgical treatment for open spina bifida or spina bifida with cyst rupture at birth had been performed for neonates in Japan. As for spina bifida occulta, the first report was published by Sakamoto et al. [142] in 1978. On the basis of his experience on 35 patients with spina bifida occulta that postoperative improvement was difficult after onset of neurological symptoms, Sakamoto suggested the necessity of early surgery during infancy. In 1979, Kaneko et al. [143] reported the bipedicle flaps method using hints obtained from plastic surgery as a surgical procedure for preventing postoperative liquorrhea. In 1983, Yamada et al. [144] examined the postoperative functional plasticity in 47 infant patients with myelomeningocele and reported poor prognosis in intelligence among those with hydrocephalus and Chiari malformation, and in neurological symptoms among those with meningocele at a high level. In 1985, based on his experience on 37 patients with spina bifida who underwent surgery during the neonatal phase, Oi et al. [145] suggested that the treatment of spina bifida requires a team of several medical departments and paramedical staff.
In 1985, Sato et al. [146] examined the metrizamide myelography findings of lumbosacral congenital spinal lipoma, which he classified into 4 types, and reported that the surgical manipulations performed varied according to difference of types; he asserted that preventive surgery should be carefully performed for asymptomatic lipoma. In 1988, Oi and Matsumoto [147] clarified the confusing theories on the historical background, definitions, and pathophysiology of tethered cord syndrome. Over time, the advent of MRI enabled clarification of the concept of the tethered cord, as well as the diagnostic details for lipoma in the spinal canal; the need to release the tethered cord in the early phase was emphasized, leading to the promotion of early surgery [148,149].
Koyanagi et al. [150,151] performed surgery on 34 patients with tethered cord with occult spinal dysraphism, which prevented the subsequent progression of symptoms in 81% of these patients. However, the preoperative symptoms only improved in 35% of the patients, he asserted that untethering should be performed quickly once tethered cord syndrome is diagnosed.
However, in 1997, Matsumoto [17] reported a paradigm shift in treatment policy for spina bifida. Even with advanced surgical procedures available and improvement in management in the perioperative period, he insisted that prophylactic surgery should be carefully determined for asymptomatic cases. Furthermore, Matsumoto [17] emphasized that tethered cord should be strictly distinguished from low conus.
In 2002, Arai et al. [152] reported good outcomes in 120 patients with lumbar spinal lipoma on whom he performed surgery. As the frequency of symptoms increased with age, he concluded that prophylactic untethering surgery was useful. On the contrary, when the disease was classified into five types, the combined type presented a complex structure and pathophysiology, making surgery difficult, and surgery for asymptomatic patients should, therefore, be carefully determined [153]. In 2008, based on an analysis of the relationship between the morphology of conus lipomas and the appearance of symptoms in 58 patients, Koyanagi et al. [154] reported that early loss of motor function is caused by massive lipomas located at the lumbar spine level, and that patients with lipomas confined to the sacrum had early bladder disturbance. Koyanagi et al. [154] asserted that when clear mechanical stress on the spinal cord is confirmed by imaging, early prophylactic surgery is a suitable treatment.
In conclusion, regarding the indication of prophylactic surgery for occult spinal dysraphism, untethering should be performed as early as possible when the tethering is confirmed by imaging and neurological symptoms. For disease presenting a complex structure on image findings and asymptomatic, surgery should be carefully determined.
7. Transoral Approach for Lesions of the CVJ (Table 13)
Table 13.
Transoral approach to the craniocervical junction
| Year | Born anomaly, atlantoaxial dislocation | Tumor | Aneurysm |
|---|---|---|---|
| 1966 | Sano | ||
| 1976 | Abe | Hashi | |
| 1978 | Saito | ||
| 1978 | Yamaura | ||
| 1983 | Abe | Hayakawa | |
| 1985 | Hakuba | Abe | Abe |
| 1985 | Chono · Abe | ||
| 1989 | Koshu· Abe | Hayakawa · Yamada | |
| 1990 | Kohno | ||
| 1991 | Akino· Abe | ||
| 1994 | Nakagawa | ||
| 1995 | Takahashi | ||
| 1998 | Mori · Takayasu | ||
| 2001 | Imamura | ||
| 2006 | Takayasu | Takayasu | |
| 2013 | Takayasu | ||
| 2016 | Takayasu | Takayasu |
Lesions of the CVJ are approached via various routes; however, this paper makes reference to the anterior (transoral) approach. Lesions include bone deformity, atlantoaxial dislocation, trauma, tumor, and vertebrobasilar aneurysm.
1) Approach to bone deformities
Transoral approach to the bone anomaly was first reported by Scoville and Sharman [155] in 1951. Subsequently, following reports by Fang et al. [156] in 1962, and Greenberg et al. [157] in 1968, this approach gradually gained popularity. Thereafter, large case series were reported by Spetzler et al. [158] in 1979, Menezes et al. [159] in 1980, and Crockard et al. [160] in 1986, which led to the establishment of the surgical procedure, and the intensification of its application for tumors and aneurysms.
In Japan, Hiroshi Abe (the author) [161,162] was the first to report the transoral approach for bone deformity in 1976 and 1983. Thereafter, the author presented his experiences on 16 cases using the transoral approach at the Annual Meeting of American Association of Neurological Surgeons in 1989. During that meeting Menezes spoke of his experience with nearly 200 cases. However, Menezes and Crockard performed additional posterior fusion after removing bone deformity such as the odontoid process from anterior side, without performing anterior fusion. Hiroshi Abe’s favorite theory was that after performing anterior decompression in patients without C1–2 instability, anterior fusion using autologous bone between C1 and C2, or between the foramen magnum and C2 was sufficient and posterior fixation was unnecessary. Therefore, the author always discussed on this point with Menezes and Crockard.
Several reports on transoral approach appeared in the literature over time in Japan—Hakuba [23] in 1985, Koshu et al. [163] in 1986, Kohno et al. [164] in 1990. In 1994, Nakagawa et al. [165] performed one-stage surgery simultaneously with posterior fixation. In 1995, Takahashi et al. [166] reported the transoral approach for 19 patients with atlantoaxial dislocation. In 1991, Akino et al. [167] reported 30 cases of the transoral approach. In the 2000s, Takayasu et al. [168] reported his experience with 13 patients. Furthermore, Takayasu [169] in 2013, published his experience with 29 cases of not only bone deformity but also other CVJ lesions, and systematized this approach by describing indication and surgical details.
2) Transoral approach for tumors
Menezes and VanGilder [170] reported numerous cases of the transoral approach for treating tumors. In 1985, Chono et al. [171] reported 1 case of meningioma, and in 2006, 3 cases of chordoma [172]. In 1998, 1 case each of chordoma and osteoblastoma was reported by Miyagi et al. [173] and Mori et al. [174] respectively, and in 2001, Imamura et al. [175] reported 1 case of meningioma. In 2006, Takayasu et al. [168] reported his experience of 6 tumor cases.
However, recent advances in surgical approaches and techniques have enabled the resection of many of tumors located anterior to the foramen-magnum-C1–2 region without the transoral approach. In this regard, tumorectomy by transoral approach is considered to be limited to chordoma and bone tumors such as osteoblastoma accompanied with bone destruction [176,177].
3) Transoral approach for cerebral aneurysm
In 1966, for the first time, Sano et al. [178] performed surgery to treat an aneurysm using the transoral approach. Subsequently, others reported this surgery—Hashi et al. [179] in 1976, Yamaura et al. [180] in 1979, Saito et al. [181] in 1980, Hayakawa et al. [182] in 1981, Abe et al. [183] in 1985, and Hayakawa et al. [184] in 1989. At that time, Japan led the world in the transoral approach for cerebral aneurysm. Nevertheless, advances in endovascular surgery, surgical approaches, and techniques led to the gradual phasing out of the transoral approach for aneurysms.
A historical narrative of the transoral approach for various lesion types has been provided above. As of today, it may be emphasized that the transoral approach is indicated for bone deformity lesions, chordoma, and bone tumors. In particular, the transoral approach is well indicated for patients with marked anterior compression of the medulla and upper cervical cord in whom symptom recovery cannot be expected by posterior decompression. In recent years, mastery of surgical techniques using advanced operative instruments and tools (fibrin glue) ensures the safety of the procedure [169,185,186]. Thus, the transoral approach should probably be used more frequently for various lesions.
8. Spine and Spinal Cord Injury (Table 14)
Table 14.
Spinal cord injury
| Year | Author | Method |
|---|---|---|
| 1963 | Yada · Tsuru | Decompression for acute spinal and injury |
| 1968 | Tsuru | Whiplash injury |
| 1986 | Kadoya | Cervical cord injury |
| 1990 | Nakamura · Kadoya | Acute cervical cord injury |
| 1992 | Yamamoto · Nakagawa | Magnetic resonance (MR) image of spinal cord injury |
| 1995 | Takahashi · Koyanagi | MR image of acute cervical cord injury |
| 1998 | Morota · Nakagawa | Spinal cord injury in children |
| 2000 | Nakagawa · Mizuno | Instrumentation and navigation of cervical cord injury |
| 2000 | Koyanagi | Spinal cord injury without bone injury |
| 2003 | Anzai | Spinal cord injury without bone injury |
| 2003 | Hirano | Spinal cord injury without bone injury |
| 2014 | Suzuki | Treatment and management of acute spinal cord injury |
| 2017 | Suzuki | Treatment of acute spinal cord injury |
In Japan, spine and spinal cord injury has since long been treated by the departments of surgery and orthopedic surgery. The department of neurosurgery commenced treatment in 1958, when Tsuru started medical practice at the Hokkaido University Hospital after completing his training in the USA. After Yada joined Hokkaido University in 1960, the institution was essentially dedicated to activities involving the treatment of spinal cord injury. In 1963, Yada and Tsuru [187] proactively performed early decompression for 27 patients with cervical cord injury, and reported a marked improvement in three cases. Yada’s indications for surgery included the following: (1) when patients present spinal cord symptoms immediately after injury, and have complete or incomplete block on Queckenstedt’s test; (2) when the level of spinal cord symptoms is ascending, and/or the symptoms progressively deteriorate; (3) when persistent spinal cord compression caused by fracture and dislocation is revealed on X-ray; and (4) in the event of an open wound with liquor leakage.
Circa 1963, “whiplash injury” created a furor worldwide. Tsuru [188] calmly stated that “this injury primarily affects supporting tissues such as neck muscles and ligaments, with little serious injury to the spinal cord and nerves.” Several years later, whiplash injury turned out to be just as Tsuru indicated, and the commotion died down.
In the 1970s, Kadoya proactively engaged in the treatment of spinal cord injury, after research work in Cleveland, USA. Kadoya and Nakamura [189] adopted the philosophy that spinal cord decompression does not necessary require early intervention, and that reduction of the dislocation should be attempted first. However, if reduction cannot be achieved, and when spinal cord compression caused by bone fragments within the spinal canal and intervertebral discs is observed, then surgery should be performed. In 1990, Nakamura and Kadoya [190] reported, based on his experience of 88 patients with cervical spinal cord injury, that recovery of symptoms was dependent on the degree of neurological symptoms varies between 24 and 72 hours after injury, and that significant recovery of symptoms was observed in patients with a score of 3.5 or more on the Yale spinal scale.
From the 1990s through to 2000, Nakagawa also proactively engaged in acute spinal cord injury on returning to Japan after receiving training in Boston and New York in the USA. Diagnosis of spinal cord injury by imaging studies enabled detailed observation of the vertebral bone injuries by computed tomography (CT), and the advent of MRI enabled the differentiation of the status of injured spinal cords. In 1992, Yamamoto et al. [191] reported poor prognosis in patients exhibiting extensive intramedullary high signal intensity on T2-weighted imaging; however, the recovery of symptoms was possible in patients with a localized hyperintense area. In 1995 and in 1999, Takahashi et al. [192,193] also emphasized the benefits of MRI for spinal cord injury.
The treatment of acute spine and spinal cord injury also dramatically improved with developments in instrumentation and navigation. In 2000, Nakagawa et al. [194] reported the use of spinal instrumentation in 63 patients with cervical spine and spinal cord injury, and achieved strong internal fixation with instrumentation. According to this report, in many patients, early ambulation with early rehabilitation was possible, which resulted in early discharge and return to social work. In 1998, Morota and Nakagawa [195] reported that for pediatric patients with spinal cord injury younger than 10 years, conservative treatment was effective in many of them and surgical treatment should be carefully determined. In 2000, Koyanagi et al. [196] reported 42 patients with cervical cord injury that was not accompanied by bone injury. More than 90% of these patients exhibited cervical spondylosis, cervical OPLL and developmental spinal canal stenosis, while MRI revealed 93% with spinal cord compression. Of the 37 patients (88%) who underwent surgery, 32 patients (76%) showed an improvement according to the Frankel grade. In 2003, Anzai et al. [197] conducted laminoplasty in 30 out of 69 cervical cord injury patients without bone injury, and reported that the surgery group exhibited more improvement compared to the conservative treatment group. In the same year, Hirano et al. [198] performed laminoplasty on 11 cervical cord injury patients without bone injury, and reported improvement in all patients. In Japan, approximately half of all patients with traumatic cervical cord injury present cervical cord injury without bone injury, and, therefore, determining a treatment plan for these patients is a major concern; however, a more aggressive approach to treatment is likely to be adopted going forward.
In 2017, Suzuki et al. [199] reported the results of 316 patients with spinal cord injury who underwent acute phase surgery during a 20-year period from 1993 to 2013. It was revealed, from this study, that an improvement of one grade or more was observed in 48% of patients with American Spinal Injury Association (ASIA) category A complete injury, and 1 patient showed an improvement to ASIA-D. Among 262 patients with ASIA B to D injury, 84% of the patients reportedly showed an improvement of 1 grade or more. These were surprisingly excellent results. All patients underwent surgery for decompression and/or fixation within 48 hours of injury. Surgery was indicated for confirmed compressive lesions consistent with symptoms, or responsible lesion with instability. In 2012, Fehlings et al. [200] recommended early surgery within 8–24 hours of injury on the basis of collaborative research results of the North American spinal cord injury centers. In 2015, Jug et al. [201] reported that outcomes of patients who underwent surgery within 8 hours of injury were significantly better than those who underwent surgery within 24 hours. The treatment policy by Suzuki [202] had been proposed prior to the reports by Fehlings and Jug, and it can thus be said that a proactive approach and efforts in building a collaborative team medicine by Suzuki [202] are admirable.
9. Lumbar Canal Stenosis (Table 15)
Table 15.
Lumbar canal stenosis
| Year | Authior | Method | Author | Less invasive method |
|---|---|---|---|---|
| 1994 | Koyama | The concept of lumbar canal stenosis | ||
| 1995 | Kadoya | Lumbar canal stenosis –pathogenesis and treatment– | ||
| 1995 | Hanakita · Mizuno | 257 Cases of lumbar canal stenosis | ||
| 1996 | Yamada | Unilateral partial laminectomy with bilateral decompression | ||
| 1997 | Kadoya | Spinal canal stenosis –cervical and lum- bar– | ||
| 1997 | Koyama | Surgical treatment for canal stenosis and lumbar disc hernia | ||
| 1998 | Sato · Kadoya | Limited decompression for lumbar canal stenosis | Harada | Unilateral partial laminectomy with bilateral decompression |
| 1998 | Hanakita· Suwa | Localized decompression for lumbar canal stenosis | Suwa·Hanakita | Unilateral partial laminectomy with bilateral decompression |
| 2003 | Inoue | Unilateral partial laminectomy with bilateral decompression | ||
| 2003 | Iwatsuki | Unilateral partial laminectomy with bilateral decompression | ||
| 2004 | Hanakita | Pathogenesis and surgery of lumbar spondylosis | ||
| 2006 | Yada | Unilateral partial laminectomy with bilateral decompression | ||
| 2007 | Hanakita | Complications in 3486 cases of spine surgery | ||
| 2007 | Sugawara · Isu | Decompression for lumbar spondylosis and spondylolisthesis | ||
| 2007 | Sugawara · Isu | Decompression for lumbar stenosis with spondylolisthesis | ||
| 2009 | Kino·Hanakita | Unilateral partial laminectomy with bilateral decompression | ||
| 2011 | Shoda | Instrumentation for lumbar spine | Sasaki | Unilateral partial laminectomy with bilateral decompression |
| 2012 | Sugawara · Isu | Decompression for lumbar stenosis with spondylolisthesis | ||
| 2012 | Hara | Posterior fusion for lumbar degenerative disease | ||
| 2015 | Shoda | Lumbar interbody fusion for lumbar spondylolisthesis | ||
| 2015 | Mizuno | Evolution of lumbar fusion |
In Japan, orthopedic surgeons have long worked on lumbar spine disease with enthusiasm. In the 1930s, neurosurgeons also performed surgery for lumbar disc hernia throughout Japan. Naturally, all surgeons were performed macroscopically. In neurosurgery, Satoru Kadoya and Tsunemaro Koyama were the first to embark upon lumbar spine disease treatment. Space limitations limit our discussion only to lumbar spine degenerative disease (excluding herniated disc).
Kadoya engaged in the treatment of both cervical spine and lumbar spine disease in the 1970s upon returning to Japan after studying abroad, and accomplished groundbreaking results [203]. In 1994, Sato et al. [204,205] reported the outcomes of microscopic posterior decompression of lumbar canal stenosis for 47 patients, and 103 patients in 1998. Favorable outcomes were reported for all procedures, with an improvement rate of 90%. Following decompression, Kadoya [203] noted that fixation was necessary only when total facetectomy was performed and when significant instability is present, but not otherwise.
Upon returning to Japan after learning spinal surgery under the guidance of professor Krayenbuel in Switzerland, Koyama received further guidance in spinal surgery by Akinori Kondo. Koyama [206] strictly indicated that the diagnosis of lumbar canal stenosis should be based on the criteria defined by Verbiest, according to the antero-posterior diameter measurements of the spinal canal. Koyama published educational articles based on his experience of lumbar canal stenosis, pathophysiology, surgical procedures, and related procedures for lumbar herniated disc, and provided guidelines for many neurosurgeons to engage in spinal surgery [26,207].
Hanakita et al. [208] also began learning spinal cord surgery from Akinori Kondo and in 1995, made a presentation on his experience of already treating 257 patients with lumbar canal stenosis and related pathophysiology and surgical methods. Hanakita [209] gradually adopted a minimally invasive surgical approach, excluded patients with facet joint hypertrophy and obtuse-angled lamina, and recommended decompression by unilateral approach. Hanakita and Suwa [210] performed posterior fixation for slip distance of more than 10 mm, and slip angle more than 15 degrees. In 2007, Hanakita [211] reported on postoperative complications in his spinal cord and spine surgical experience of 3,486 patients, leaving a legacy for subsequent generations of neurosurgeons.
The contributions by Kadoya, Koyama, and Hanakita to lumbar spine disease deserve close attention, as these are truly great achievements that paved the way for neurosurgeons, who could previously only perform cervical spine surgery, to engage in spine and spinal cord surgery of the whole spine, including the thoracic spine and lumbar spine.
The question of whether or not to perform fixation in addition to posterior decompression remains controversial. Shoda et al. [212] performed fixation for slip distance of more than 3 mm or 5%, or in the event of posterior opening of more than 5 degrees. Mizuno et al. [213] performed fixation when deformity correction was required due to severe slipping or scoliosis, and when postoperative instability increased due to decompression. Hara et al. [214] performed fixation in the event of posterior opening more than 5 degrees on flexion, and antero-posterior slipping more than 10% on dynamic radiography, or in the event of lateral slipping of more than 10%. Complications that can occur in the event of such fixation include bone fracture affecting the pedicle or bony end plate during instrument placement, dural injury, nerve injury, blood vessel damage, infection, and the adjacent level disorder [213,215].
Fixation methods include posterior lumbar interbody fusion using a cage, or transforaminal lumbar interbody fusion wherein a cage is inserted via the intervertebral foramen following facetectomy, with the method combining percutaneous pedicle screw and cortical bone trajectory, the details of which are omitted due to the space limitations of this paper.
On the contrary, since 2007, Sugawara et al. [216-218] reported the results of follow-up observation without fusion whenever possible for lumbar canal stenosis accompanied by spondylolisthesis. In 2012, results of 31 patients who underwent the procedure were reported, which revealed no significant difference; the rate of improvement in lumbar pain was 67% for patients without preoperative instability, and 53% for patients with preoperative instability. Similarly, reports indicating that good outcomes with decompression only were not uncommon [219-221]; He recommended performing decompression alone as the primary surgery. The question of whether or not to combine decompression and fixation remains a topic for debate; however, when combined with fixation, it is imperative to minimize complications as much as possible.
For posterior decompression of the lumbar spine, fenestration had been performed by partial laminectomy; however in recent years, bilateral decompression by unilateral approach has been frequently used. This approach gained sudden popularity after reports by Wiltse and Spencer [222] in 1988, Poletti [223] in 1995 and Yamada et al. [224] in 1995 who published the first report on 35 patients in Japan. Subsequently, Harada and Harada [225] reported on 60 patients, 35 patients by Suwa et al. [226] in 1998, 28 patients by Inoue et al. [227], 30 patients by Iwatsuki et al. [228] in 2003, 22 patients by Okuda et al. [229] in 2006, 60 patients by Kino et al. [230] in 2009, and of 19 patients by Sasaki et al. [231] in 2011. More than 90% of patients in all the reports showed improvement in symptoms. This bilateral decompression method by unilateral approach carries the risk of insufficient decompression of the contralateral side, and dura mater damage if performed by an inexperienced surgeon; however, if performed by an expert, the technique is a good, minimally invasive method.
DOCTORS WHO PROMOTED THE DEVELOPMENT OF SPINAL SURGERY IN JAPAN
Doctors who played an active role from the latter half of the 1990s to the present day in the early 2000s, and even to this day, are presented.
1. Junya Hanakita (Fig. 17)
Fig. 17.
Junya Hanakita
Hanakita’s contributions involving performing surgery on several thousand patients with lumbar spine disease, including lumbar canal stenosis and lumbar herniated disc, are second to none. He has published extensively on lumbar degenerative disease, which was a major achievement that paved the way for neurosurgeons to treat lumbar spine disease. Hanakita [232] reported his experience of 21 patients who underwent surgery to remove ossified lesions by anterolateral thoracotomy approach for thoracic OPLL, and was a pioneer who took on the challenge of difficult surgeries. His trustworthy report of complications in 3,846 cases in spinal surgery should be mandatorily read by those aspiring to perform spinal surgery. Hanakita served as the second chief director of the Neurospinal Society of Japan from 2008 to 2012 and also contributed to the establishment of the Board certification system of spinal surgeon. Despite his warm personality, he delivered harsh remarks at society meetings. He is passionate about mountain climbing and golf.
2. Yoshinobu Iwasaki (Fig. 18)
Fig. 18.
Yoshinobu Iwasaki
Iwasaki performed experimental study on spinal cord injury in dogs. Then he contributed to the research in the pathophysiology and mechanisms of the symptoms of cervical spondylosis. He reported the phenomenon of intramedullary penetration of contrast medium on CT myelography in patients with cervical spondylosis, to the Journal of Neurosurgery [233]. He achieved favorable outcomes for intramedullary tumors. He contributed to the establishment of the Board certification system of spinal surgeon. He was earnest, enjoyed debating, gardening and visiting hot springs with his family, and was devoted to his family.
3. Shigekuni Tachibana (Fig. 19)
Fig. 19.

Shigekuni Tachibana
Tachibana achieved results in experimental and clinical research in surgery for spinal cord injury in the acute stage, and was a proponent of early surgery [234,235]. He had unique theories in his research on the onset mechanism of flexion myelopathy [236], onset of spinal cord syrinx and the mechanism underlying syrinx enlargement. His greatest achievement was his efforts in peripheral nerve surgery. He accomplished great works in the diagnosis and surgical treatment of entrapment neuropathies, such as carpal tunnel, cubital tunnel, and tarsal tunnel syndromes [237]. He was earnest and directed sharp questions to presenters at society meetings. However, he is essentially a Tokyo boy with a gentle demeanor who loved fishing and sailboats.
4. Toyohiko Isu (Fig. 20)
Fig. 20.

Toyohiko Isu
From his training days as a resident, Isu steadily published numerous articles and was a man of ideas, who ruminated about spinal cord disease pathophysiology and surgical methods. He conceived the “Williams-Isu method” [238] which did not use the iliac bone, but utilized part of the vertebral body intraoperatively in anterior fusion for cervical spondylosis. He also devised a unique shunt tube (Sapporo shunt) for use in syrinx-subarachnoid shunting of syringomyelia [139]. In foramen magnum decompression, he devised a surgical method of opening only the outer layer of the dura without sectioning whole dura mater [133]. In recent years, he achieved several accomplishments in peripheral nerve surgery, publishing 12 books, as well as many articles [239], and was in great demand for delivering lectures. Isu enjoyed walking, and was always thinking about something as he went on walks.
5. Hideaki Iizuka (Fig. 21)
Fig. 21.
Hideaki Iizuka
Iizuka performed experimental study on spinal cord injury under Professor Young in New York, and presented his research results to the Journal of Neurosurgery [240,241]. After returning to Japan, he diagnosed and treated several acute stage spine and spinal cord injury cases. He particularly studied fixation for unstable upper cervical lesions in upper cervical injury [242]. In recent years, he has recommended minimally invasive surgery for various types of lumbar degenerative lesions [243]. Iizuka has a soft demeanor; however, once he has his mind made up, he performs his tasks with strong determination and will.
6. Phyo Kim (Fig. 22)
Fig. 22.
Phyo Kim
Kim received training as a resident and student of Professor Sundt at the Mayo Clinic from 1984 to 1990, and after acquiring a Ph.D., he returned to Japan. In the field of spinal surgery, Kim has abundant experience using hydroxyapatite [44] and reported various techniques for laminoplasty. Recently, he proposed a surgical approach that takes into account myoarchitecture when performing laminoplasty. Since 2013, he serves as the third chief director of the Neurospinal Society of Japan. He discussed with the orthopedic surgeons and led to the creation of a common system of board certification system of spinal surgeon. He helped to found Neurospine, a joint official English journal of spinal surgery in Japan, Korea, and Taiwan, which was established in March 2018. Kim is a warm gentleman who converses in English as a native speaker and keeps in shape by cycling and skiing.
7. Masakazu Takayasu (Fig. 23)
Fig. 23.

Masakazu Takayasu
Takayasu is a man of ideas, who devised and developed various surgical procedures and surgical instruments for spinal surgery. He reported the anterolateral approach for cervical OPLL [77], and various fixations for lesions of the CVJ [244]. He achieved many surgeries with the anterior and posterior approach to CVJ [168,169]. In particular, his rich experience with the transoral approach in 50 patients has not been surpassed. In recent years, he has focused on minimally invasive surgeries, and also devises techniques and develops surgical instruments. He is proficient in English and keeps in shape by playing tennis and swimming.
8. Junichi Mizuno (Fig. 24)
Fig. 24.

Junichi Mizuno
Mizuno studied spinal surgery at Emory University in the USA. In Japan, he received guidance in spinal surgery by Hiroshi Nakagawa. Surgery for ossification of the spinal column ligament, and the pathology of compressive spinal cord lesion are considered his lifework. He has achieved accomplishments in cervical spondylosis, cervical OPLL and instrumentation surgery [245-247]. In recent years, he is working to popularize minimally invasive surgery using an endoscope and microscope. Mizuno is internationally active as a member of the ASIA SPINE, Asia Pacific Cervical Spine, and World Federation of Neurosurgical Societies spinal committees. He loves scuba diving and tennis.
9. Kazutoshi Hida (Fig. 25)
Fig. 25.

Kazutoshi Hida
Hida was trained by Hiroshi Abe and Yoshinobu Iwasaki. He has rich experience in anterior fusion of cervical spondylosis [248], anterior decompression and fusion of cervical OPLL [74], syringo-subarachnoid shunting and foramen magnum decompression for syringomyelia [140], and surgery for intramedullary tumor [249]. In particular, he proposed treatment methods for different types of spinal AVM, and achieved excellent results by developing a surgical technique for perimedullary AVF using intraoperative Digital subtraction angiography and Indocyanine green angiography [90]. He leads Japan in spinal AVM, largely due to his work. He is a board-certified spinal surgery instructor, and since 2009, he serves as chairman of the board certification system for spinal surgeons of the Neurospinal Society of Japan. He is proficient in English. He likes playing tennis, taking smash hits that go far over the net. He is impulsive and hot-blooded when he gets carried away.
10. Izumi Koyanagi (Fig. 26)
Fig. 26.

Izumi Koyanagi
Koyanagi was a classmate with Hida at Hokkaido University School of Medicine and also received training under Hiroshi Abe and Yoshinobu Iwasaki. His accomplishments are in the areas of surgery of spinal cord injury in the acute stage [196,250], early surgery of occult spinal dysraphism [151,251], surgery of intramedullary tumor [109], and research in the mechanisms of syringomyelia. While studying abroad at the University of Toronto in Canada (under Prof. Tator), his photographs of spinal cord microvasculatures in experimental spinal cord injury were used twice on the cover of Neurosurgery (the bulletin of the CNS) [252,253]. Fehlings, a star scientist at the University of Toronto, was Koyanagi’s colleague in Tator’s Laboratory. He serves as the chair of the academic committee of the Neurospinal Society of Japan. Koyanagi has a bright personality and is constantly smiling. He is a good singer and will not let the microphone go at banquets and end-of-year parties. His cheerfulness laughs away any difficult matter.
CONCLUSIONS
In this paper, I reviewed and described advances in spinal surgery in Japan from the pioneering period to the progressive era (1911–2017). Recent developments in spinal surgery in Japan include several amazing advancements. I hope that in the future, progress in this field will advance from the late developmental stage to the maturity, and that the younger generation will be actively involved in this process. I hope that this paper will be of use when reflecting upon the achievements of our predecessors.
Footnotes
The authors have nothing to disclose.
REFERENCES
- 1.Kadoya S. A historical review of the spine and spinal cord surgery in neurological surgery of Japan. Spinal Surg. 1999;13:1–14. Japanese. [Google Scholar]
- 2.Abe H. Progress of spinal surgery. In: Fukui H, editor. The history of neurosurgery. Tokyo: Igakushoin; 2003. pp. 55–74. Japanese. [Google Scholar]
- 3.Abe H. The dawn and development of spinal surgery in Japan. Spinal Surg. 2016;30:5–19. Japanese. [Google Scholar]
- 4.Abe H. The history of spinal surgery in Japan. Spinal Surg. 2018;32:251–69. Japanese. [Google Scholar]
- 5.Hanakita J. History of Japanese spinal neurosurgery and problems to be solved expeditiously. Spinal Surg. 2011;25:9–13. Japanese. [Google Scholar]
- 6.Kitamura K. Miyake Hayari. Clin Neurosci. 1999;17:116. Japanese. [Google Scholar]
- 7.Nagahiro S. The first surgeon who succeeded to remove brain and spinal cord tumors. Jpn J Neurosurg. 2015;24:189–91. Japanese. [Google Scholar]
- 8.Sato S. Surgery of spinal cord tumor-a case report- Tokyo Med J. 1912;26:1–27. Japanese. [Google Scholar]
- 9.Takeda T, Tsuru M, Kashiwaba T. Cervical spondylosis. In: The 19th Congress of Japan Neurosurgical Society; Sapporo, Japan. 1960. Japanese. [Google Scholar]
- 10.Tsuru M, Takeda T, Yada K. Clinical disc syndrome-its neurological manifestation and the effects of various treatment. In: The 1st Asian and Australasian Congress of Neurological Surgery; Tokyo, Japan. 1962. Japanese. [Google Scholar]
- 11.Yada K, Tsuru M, Takamura H. Surgery for acute spinal cord injury. In: The 24th Congress of Japanese Clinical Surgery; Mie, Japan. 1962. Japanese. [Google Scholar]
- 12.Nagashima C. Surgical treatment of cervical spondylosis-Scoville method-. In: The 23rd Congress of the Japan Neurosurgical Society; Morioka, Japan. 1964. Japanese. [Google Scholar]
- 13.Tachibana S, Hakuba A, Kadoya S, et al. Symposium “cervical spondylosis”. Spinal Surg. 1987;1:2–53. Japanese. [Google Scholar]
- 14.Yada K, Sato M, Tsuru M. Cervical radiculo-myelopathy due to calcified posterior longitudinal ligament. In: The 3rd Congress of Asian-Australasian Society of Neurological Surgons; Tokyo, Japan. 1971. Japanese. [Google Scholar]
- 15.Nagashima C. Cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg. 1972;37:653–60. doi: 10.3171/jns.1972.37.6.0653. [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto S, Sato K. Spina bifida. Tokyo: Springer; 1999. [Google Scholar]
- 17.Matsumoto S. Spina bifida-change of treatment and tethered cord syndrome. Spinal Surg. 1997;11:99–110. Japanese. [Google Scholar]
- 18.Kikuchi H. Surgery of spinal AVM. Operation. 1976;30:303–6. Japanese. [Google Scholar]
- 19.Kadoya S, Nakamura T, Kwak R, et al. Anterior osteophytectomy for cervical spondylotic myelopathy in developmentally narrow canal. J Neurosurg. 1985;63:845–50. doi: 10.3171/jns.1985.63.6.0845. [DOI] [PubMed] [Google Scholar]
- 20.Kadoya S. Grading and scoring system for neurological function in degenerative cervical spine disease--Neurosurgical Cervical Spine Scale. Neurol Med Chir (Tokyo) 1992;32:40–1. doi: 10.2176/nmc.32.40. [DOI] [PubMed] [Google Scholar]
- 21.Kadoya S. Lumber spondylosis-pathogenesis and therapy. Jpn J Neurosurg. 1995;4:98–103. Japanese. [Google Scholar]
- 22.Hakuba A. Trans-unco-discal approach. A combined anterior and lateral approach to cervical discs. J Neurosurg. 1976;45:284–91. doi: 10.3171/jns.1976.45.3.0284. [DOI] [PubMed] [Google Scholar]
- 23.Hakuba A. Anterior transoral approach to atlanto-axial dislocation. Neurosurgeons. 1985;4:231–6. Japanese. [Google Scholar]
- 24.Sakamoto H, Nishikawa M, Hakuba A, et al. Expansive suboccipital cranioplasty for the treatment of syringomyelia associated with Chiari malformation. Acta Neurochir (Wien) 1999;141:949–60. doi: 10.1007/s007010050401. [DOI] [PubMed] [Google Scholar]
- 25.Fujita K, Koyama T. Long term prognosis of 25 cases of spinal ependymomas by total removal. Spine Spinal Cord. 1997;10:153–8. Japanese. [Google Scholar]
- 26.Koyama T. Surgery of lumbar cervical stenosis and lumbar disc hernia. Spinal Surg. 1997;11:111–6. Japanese. [Google Scholar]
- 27.Koyama T, Handa J. Porous hydroxyapatite ceramics for use in neurosurgical practice. Surg Neurol. 1986;25:71–3. doi: 10.1016/0090-3019(86)90118-7. [DOI] [PubMed] [Google Scholar]
- 28.Nakagawa H, Yamamoto H, Mizuno J. Microdiscectomy and osteophytectomy without bone graft to cervical spondylosis and disc hernia. Spinal Surg. 1997;6:33–9. Japanese. [Google Scholar]
- 29.Nakagawa H, Mizuno J. Pathophysiology and surgical treatment of ossification of the posterior longitudinal ligament of cervical spine. Neurol Surg. 1996;24:205–10. Japanese. [PubMed] [Google Scholar]
- 30.Nakagawa H. Surgical instrumentation for the cervical spine. Spinal Surg. 1997;11:13–22. Japanese. [Google Scholar]
- 31.Scoville WB. Cervical spondylosis treated by bilateral facetectomy and laminectomy. J Neurosurg. 1961;18:423–8. doi: 10.3171/jns.1961.18.4.0423. [DOI] [PubMed] [Google Scholar]
- 32.Kirita Y. Posterior decompression for cervical spondylosis-wide laminectomy- Orthop Mook. 1979;6:216–30. Japanese. [Google Scholar]
- 33.Koyama T. Osteoplastic laminotomy. Spine Spinal Cord. 1983;1:235–43. Japanese. [Google Scholar]
- 34.Kim P, Murata H, Kurokawa R, et al. Myoarchitectonic spinolaminoplasty: efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine. 2007;7:293–304. doi: 10.3171/SPI-07/09/293. [DOI] [PubMed] [Google Scholar]
- 35.Nishikawa S, Kim Y, Masamura K, et al. Surgical results of anterior fusion and laminoplasty for cervical spine. Spinal Surg. 2012;26:221–6. Japanese. [Google Scholar]
- 36.Shiokawa K, Hanakita J, Suwa H, et al. Laminoplasty by titanium miniplate. Spinal Surg. 2000;14:111–6. Japanese. [Google Scholar]
- 37.Goto T, Ohata K, Matsusaka Y, et al. En bloc laminoplasty by ceramic spacer and miniplate. Spinal Surg. 2001;15:23–8. Japanese. [Google Scholar]
- 38.Takayasu M, Takagi T, Nishizawa T, et al. Bilateral opendoor cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg. 2002;96(1 Suppl):22–8. doi: 10.3171/spi.2002.96.1.0022. [DOI] [PubMed] [Google Scholar]
- 39.Hoshimaru M. Device for minimum invasive laminoplasty. Jpn J Neurosurg. 2007;16:625–30. Japanese. [Google Scholar]
- 40.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–17. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 41.Tsuru M, Takada T, Yada K. Anterior approach for cervical disc disease. In: The 22nd Congress of Japan Neurosurgical Society; Osaka, Japan. 1963. Japanese. [Google Scholar]
- 42.Kadoya S, Nakamura B, Emori T. Microsurgical anterior approach to cervical spondylosis. Operation. 1979;33:1275–8. Japanese. [Google Scholar]
- 43.Iwasaki Y, Isu T, Abe H. Operative methods for cervical disc disease. Neurol Med Chir (Tokyo) 1986;26:857–62. doi: 10.2176/nmc.26.857. [DOI] [PubMed] [Google Scholar]
- 44.Kim P, Wakai S, Matsuo S, et al. Bisegmental cervical interbody fusion using hydroxyapatite implants: surgical results and long-term observation in 70 cases. J Neurosurg. 1998;88:21–7. doi: 10.3171/jns.1998.88.1.0021. [DOI] [PubMed] [Google Scholar]
- 45.Hoshimaru M, Koyama T. Long term results of cervical anterior fusion with apaceram. Spine Spinal Cord. 2000;13:27–32. Japanese. [Google Scholar]
- 46.Isu T, Kamada K, Yamauchi T, et al. New device of cervical anterior fusion using bone graft from vertebral bodies. Neurol Surg. 1992;20:1055–61. Japanese. [PubMed] [Google Scholar]
- 47.Nakagawa H, Mizuno J, Cho K. Minimum invasive surgery in anterior approach for cervical disc disease. Jpn J Neurosurg. 1999;8:189–93. Japanese. [Google Scholar]
- 48.Kubo K, Nakagawa H, Kuroki M. Cervical interbody cage fusion. Spine Spinal Cord. 2000;13:39–45. Japanese. [Google Scholar]
- 49.Hida K, Iwasaki Y, Abe H. Experience of titanium cage for cervical spondylosis. Spine Spinal Cord. 2000;13:47–50. Japanese. [Google Scholar]
- 50.Koyanagi I. Standard of spine and spinal cord surgery. Spinal Surg. 2004;18:231–9. Japanese. [Google Scholar]
- 51.Imamura H, Aida T, Kato M. Anterior approach for three degenerated intervertebral-spaces in cervical spondylosis. Spinal Surg. 2009;23:204–10. Japanese. [Google Scholar]
- 52.Takayasu M. Choice of surgical methods in anterior approach for cervical spondylosis. Jpn J Neurosurg. 2012;21:864–72. Japanese. [Google Scholar]
- 53.Yasumoto Y, Abe Y, Tsutsumi S, et al. Cervical anterior fusion for aged patients. Spinal Surg. 2009;23:36–41. Japanese. [Google Scholar]
- 54.Yuki M, Hirashita K, Goda T, et al. Postoperative X-ray findings of cervical anterior fusion by box type of titanium cage. Spinal Surg. 2006;20:233–40. Japanese. [Google Scholar]
- 55.Mizuno J, Sano H. Instrumentation of cervical anterior approach. Jpn J Neurosurg. 2007;16:611–7. Japanese. [Google Scholar]
- 56.Horikoshi T, Uchida M, Watanabe S, et al. Factors of postoperative sinking of cages after cervical anterior fusion. Spinal Surg. 2008;22:17–22. Japanese. [Google Scholar]
- 57.Kirita Y, Miyazaki K, Hayashi T, et al. Wide laminectomy to cervical OPLL. Operation. 1976;30:287–302. Japanese. [Google Scholar]
- 58.Sugawara T. Cervical anterior approach or posterior approach? Jpn J Neurosurg. 2014;23:462–7. Japanese. [Google Scholar]
- 59.Nagashima C, Yoshizawa H. Postoperative results of myelopathy due to cervical OPLL. Spinal Surg. 1995;9:1–10. Japanese. [Google Scholar]
- 60.Igarashi M, Ikai Y, Yoshida N, et al. Surgery of cervical OPLL. Spinal Surg. 1997;11:53–60. Japanese. [Google Scholar]
- 61.Morimoto T. Expanding laminoplasty to cervical OPLL. Spinal Surg. 1997;11:81–6. Japanese. [Google Scholar]
- 62.Sakoh T. Anterior decompression to cervical OPLL. Operation. 1976;30:281–5. Japanese. [Google Scholar]
- 63.Yamaura I. Surgery to cervical OPLL-anterior decompression- Orthopedics. 1976;27:87–95. Japanese. [Google Scholar]
- 64.Manabe M, Nomura S. Anterior decompression to cervical OPLL. Neurol Surg. 1977;5:1253–9. Japanese. [PubMed] [Google Scholar]
- 65.Kamikozuru M, Yamaura I, Fujii K. Anterior decompression to multi-level cervical OPLL. Clin Orthop. 1977;12:416–24. Japanese. [Google Scholar]
- 66.Watanabe T, Inoue S, Tsuji T, et al. Anterior decompression to cervical OPLL. Operation. 1978;32:59–67. Japanese. [Google Scholar]
- 67.Harsh GR 4th, Sypert GW, Weinstein PR, et al. Cervical spine stenosis secondary to ossification of the posterior longitudinal ligament. J Neurosurg. 1987;67:349–57. doi: 10.3171/jns.1987.67.3.0349. [DOI] [PubMed] [Google Scholar]
- 68.Herkowitz HN. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. Spine (Phila Pa 1976) 1988;13:774–80. doi: 10.1097/00007632-198807000-00011. [DOI] [PubMed] [Google Scholar]
- 69.Abe H, Ito T, Iwasaki Y, et al. Anterior decompression for ossification of the posterior longitudinal ligament of the cervical spine (author’s transl) Neurol Med Chir (Tokyo) 1980;20:1183–96. doi: 10.2176/nmc.20.1183. [DOI] [PubMed] [Google Scholar]
- 70.Abe H, Tsuru M, Ito T, et al. Anterior decompression for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg. 1981;55:108–16. doi: 10.3171/jns.1981.55.1.0108. [DOI] [PubMed] [Google Scholar]
- 71.Abe H, Hida K. OPLL of the cervical spine. In: Tindall GT, Cooper PR, Barrow DL, editors. Practice of neurosurgery. Baltimore: Williams & Williams; 1996. pp. 2451–60. [Google Scholar]
- 72.Kojima T, Waga S, Kubo Y, et al. Anterior cervical vertebrectomy and interbody fusion for multi-level spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery. 1989;24:864–72. doi: 10.1227/00006123-198906000-00012. [DOI] [PubMed] [Google Scholar]
- 73.Mizuno J, Nakagawa H, Isobe M. Result of anterior decompression for cervical OPLL. Spinal Surg. 1997;11:39–46. Japanese. [Google Scholar]
- 74.Hida K, Iwasaki Y, Koyanagi I, et al. Surgical treatment for cervical OPLL-Indication of anterior decompression and posterior decompression- Spinal Surg. 1997;11:27–32. Japanese. [Google Scholar]
- 75.Kojima S, Waga S, Kubo K, et al. Anterior decompression for myelopathy due to cervical OPLL. Spinal Surg. 1997;11:33–8. Japanese. [Google Scholar]
- 76.Obara S, Monma F, Ohyama T, et al. Antero-lateral partial vertebrectomy. Spinal Surg. 1994;8:125–30. Japanese. [Google Scholar]
- 77.Takayasu M, Hara M, Takagi T, et al. Osteoplastic anterolateral vertebrectomy without fusion for multilevel cervical ossification of the posterior longitudinal ligament. Neurosurgery. 1994;45:500–7. doi: 10.1097/00006123-199909000-00018. [DOI] [PubMed] [Google Scholar]
- 78.Nishiura T, Nishida A, Handa A, et al. Anterolateral vertebrectomy. Spinal Surg. 2001;15:7–14. [Google Scholar]
- 79.Di Chiro G, Doppman JL, Ommaya AK, et al. Radiology of spinal cord arteriovenous malformation. Prog Neurol Surg. 1971;4:329–54. [Google Scholar]
- 80.Djindjian R. Embolization of angiomas of the spinal cord. Surg Neurol. 1975;4:411–20. [PubMed] [Google Scholar]
- 81.Yasargil MG. Diagnosis and treatment of spinal cord arteriovenous malformations. Prog Neurol Surg. 1971;4:355–428. [Google Scholar]
- 82.Pia HW. Treatment of spinal angiomas. In: Honda H, editor. Microneurosurgery. Tokyo: Igaku Shoin; 1975. pp. 127–36. [Google Scholar]
- 83.Malis LI. Microsurgery for spinal cord arteriovenous malformations. Clin Neurosurg. 1979;26:543–55. doi: 10.1093/neurosurgery/26.cn_suppl_1.543. [DOI] [PubMed] [Google Scholar]
- 84.Karasawa J, Kikuchi H, Kose S. Surgery for spinal AVM. Neurol Med Chir. 1976;16:127–43. Japanese. [Google Scholar]
- 85.Saito I. Surgical technique of spinal angioma. Neurol Surg. 1982;10:197–701. Japanese. [PubMed] [Google Scholar]
- 86.Goto K. Microanatomy of spinal vessels and endovascular approach for spinal vascular anomaly. In: Nakagawa H, editor. Neurosurgical anatomy for microsurgery. Tokyo: Saimed Pub; 1995. pp. 107–18. Japanese. [Google Scholar]
- 87.Miyasaka K. Embolization for spinal AVM. Igaku Ayumi. 1986;149:623–5. Japanese. [Google Scholar]
- 88.Miyamoto T. Classification and symptoms of spinal AVM. Spine Spinal Cord. 1998;11:1040–3. Japanese. [Google Scholar]
- 89.Miyamoto T, Kataoka T. Spinal AVM. Neurol Surg. 2002;30:143–53. Japanese. [PubMed] [Google Scholar]
- 90.Hida K, Iwasaki Y, Goto K, et al. Results of the surgical treatment of perimedullary arteriovenous fistulas with special reference to embolization. J Neurosurg. 1999;90(2 Suppl):198–205. doi: 10.3171/spi.1999.90.2.0198. [DOI] [PubMed] [Google Scholar]
- 91.Mourier KL, Gobin YP, George B, et al. Intradural perimedullary arteriovenous fistulae: results of surgical and endovascular treatment in a series of 35 cases. Neurosurgery. 1993;32:885–91. doi: 10.1227/00006123-199306000-00001. [DOI] [PubMed] [Google Scholar]
- 92.Spetzler RF, Detwiler PW, Riina HA, et al. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96(2 Suppl):145–56. doi: 10.3171/spi.2002.96.2.0145. [DOI] [PubMed] [Google Scholar]
- 93.Lasjaunias P. Spinal cord vascular lesions. J Neurosurg. 2003;98(1 Suppl):117–9. doi: 10.3171/spi.2003.98.1.0117. [DOI] [PubMed] [Google Scholar]
- 94.Matsumaru Y, Hara T, Matsumura A. Spinal AV shunt. Jpn J Neurosurg. 2013;22:44–51. Japanese. [Google Scholar]
- 95.Ogata N, Goto K. Endovascular surgery for spinal AVM. Spinal Surg. 1998;12:103–10. Japanese. [Google Scholar]
- 96.Hida K, Asano T, Aoyama T, et al. Combined treatment for spinal AVM. Jpn J Neurosurg. 2011;20:20–8. Japanese. [Google Scholar]
- 97.Hida K, Shirato H, Isu T, et al. Focal fractionated radiotherapy for intramedullary spinal arteriovenous malformations: 10-year experience. J Neurosurg. 2003;99(1 Suppl):34–8. doi: 10.3171/spi.2003.99.1.0034. [DOI] [PubMed] [Google Scholar]
- 98.Onodera T, Nishikawa N, Shirato H, et al. Stereotaxic radiation therapy for intramedullary spinal AVM. Spine Spinal Cord. 2011;24:289–93. Japanese. [Google Scholar]
- 99.Ishii K, Imai H, Takai K, et al. Stereotaxic radiotherapy for spinal vascular malformation. Spinal Surg. 2012;26:327–31. Japanese. [Google Scholar]
- 100.von Eiselsberg AF, Ranzi R. Über die chirurgische Behandlung der Hirn-und Rückenmarkstumoren. Arch Klin Chir. 1913;102:309–468. [Google Scholar]
- 101.Greenwood J., Jr Surgical removal of intramedullary tumors. J Neurosurg. 1967;26:276–83. doi: 10.3171/jns.1967.26.2.0276. [DOI] [PubMed] [Google Scholar]
- 102.Guidetti B. Intramedullary tumours of the spinal cord. Acta Neurochir (Wien) 1967;17:7–23. doi: 10.1007/BF01670413. [DOI] [PubMed] [Google Scholar]
- 103.Yasargil MG, De Preux J. Microsurgical experiments in 12 cases of intramedullary hemangioblastomas. Neurochirurgie. 1975;21:425–34. [PubMed] [Google Scholar]
- 104.Malis LI. Intramedullary spinal cord tumors. Clin Neurosurg. 1978;25:512–39. doi: 10.1093/neurosurgery/25.cn_suppl_1.512. [DOI] [PubMed] [Google Scholar]
- 105.Stein BM. Surgery of intramedullary spinal cord tumors. Clin Neurosurg. 1979;26:529–42. doi: 10.1093/neurosurgery/26.cn_suppl_1.529. [DOI] [PubMed] [Google Scholar]
- 106.Abe H, Iwasaki Y, Isu T. Surgery of intramedullary spinal cord tumors. Neurosurgeon. 1986;5:263–76. Japanese. [Google Scholar]
- 107.Brotchi J, Fischer G. Intramedullary spinal cord tumors-Results. In: Fischer G, Brotchi J, editors. Intramedullary spinal cord tumors. Stuttgart: Thieme; 1996. pp. 85–90. [Google Scholar]
- 108.Koyama T. Surgery of intramedullary spinal cord tumors (2) Nichidoku-Iho. 1999;44:542–54. Japanese. [Google Scholar]
- 109.Koyanagi I, Abe H, Iwasaki Y. Surgery of intramedullary spinal cord tumors. Nichidoku-Iho. 1999;44:530–41. Japanese. [Google Scholar]
- 110.Hoshimaru M, Koyama T, Hashimoto N, et al. Results of microsurgical treatment for intramedullary spinal cord ependymomas: analysis of 36 cases. Neurosurgery. 1999;44:264–9. doi: 10.1097/00006123-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 111.Ohata K, Takami T, Gotou T, et al. Surgical outcome of intramedullary spinal cord ependymoma. Acta Neurochir (Wien) 1999;141:341–6. doi: 10.1007/s007010050309. [DOI] [PubMed] [Google Scholar]
- 112.Nishikawa S, Ohata K, Nishio A, et al. Long term results of treatment for intramedullary spinal cord tumors. Spinal Surg. 2003;17:89–98. Japanese. [Google Scholar]
- 113.Takami T, Naito K, Yamagata T, et al. Surgical management of spinal intramedullary tumors: radical and safe strategy for benign tumors. Neurol Med Chir (Tokyo) 2015;55:317–27. doi: 10.2176/nmc.ra.2014-0344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Takami T, Naito K, Yamaga T, et al. Surgery of intramedullary spinal cord tumors. Jpn J Neurosurg. 2017;26:333–40. Japanese. [Google Scholar]
- 115.Abe H. Intramedullary spinal cord tumors. in neurosurgical field. In: Ochiai N, editor. Recent technique in border area. Tokyo: Medical View; 2001. pp. 41–9. Japanese. [Google Scholar]
- 116.Goya T. Removal of intramedullary spinal cord tumors. Spinal Surg. 2014;26:5–10. Japanese. [Google Scholar]
- 117.Yamamoto I, Kanno H, Sakamoto K, et al. Surgery of spinal hemangioblastomas. Spinal Surg. 2005;19:307–14. Japanese. [Google Scholar]
- 118.Tani S, Abe H, Isojima A, et al. Surgical treatment of spinal hemangioblastomas. Spinal Surg. 2005;19:39–45. Japanese. [Google Scholar]
- 119.Seki T, Hida K, Iwasaki Y, et al. Results of treatment for spinal astrocytomas. Spinal Surg. 2015;29:326–9. Japanese. [Google Scholar]
- 120.Gardner WJ, Angel J. The mechanism of syringomyelia and its surgical correction. Clin Neurosurg. 1958;6:131–40. doi: 10.1093/neurosurgery/6.cn_suppl_1.131. [DOI] [PubMed] [Google Scholar]
- 121.Williams B. The distending force in the production of communicating syringomyelia. Lancet. 1969;26:189–93. doi: 10.1016/s0140-6736(69)91427-5. [DOI] [PubMed] [Google Scholar]
- 122.Ball MJ, Dayan AD. Pathogenesis of syringomyelia. Lancet. 1972;2:799–801. doi: 10.1016/s0140-6736(72)92152-6. [DOI] [PubMed] [Google Scholar]
- 123.Aboulker J. La syringomyelia et les liquids intrarachidiens. Neurochirurgie. 1979;25(Suppl 1):1–144. [Google Scholar]
- 124.Pojunas K, Williams AL, Daniels DL, et al. Syringomyelia and hydromyelia: magnetic resonance evaluation. Radiology. 1984;153:679–83. doi: 10.1148/radiology.153.3.6494463. [DOI] [PubMed] [Google Scholar]
- 125.Sherman JL, Barkovich AJ, Citrin Charkes MC. The MR appearance of syringomyelia: new observations. AJNR. 1986;7:985–95. doi: 10.2214/ajr.148.2.381. [DOI] [PubMed] [Google Scholar]
- 126.Abe T, Isojima A, Nagashima H, et al. Role of central canal in pathogenesis of syringomyelia. Spine Spinal Cord. 1998;11:733–8. Japanese. [Google Scholar]
- 127.Ohhama E, Kitayama M, Mihara E, et al. Spinal central canal of syringomyelia-Investigation of cadaver. Spine Spinal Cord. 1998;11:739–44. Japanese. [Google Scholar]
- 128.Batzdorf U. Chiari I malformation with syringomyelia. Evaluation of surgical therapy by magnetic resonance imaging. J Neurosurg. 1988;68:726–30. doi: 10.3171/jns.1988.68.5.0726. [DOI] [PubMed] [Google Scholar]
- 129.Milhorat TH, Johnson WD, Miller JI, et al. Surgical treatment of syringomyelia based on magnetic resonance imaging criteria. Neurosurgery. 1992;31:231–44. doi: 10.1227/00006123-199208000-00008. [DOI] [PubMed] [Google Scholar]
- 130.Hakuba A, Tokunoh N, Nishimura S. Surgical treatment for syringomyelia with Chiari malformation. Spinal Surg. 1990;4:69–76. Japanese. [Google Scholar]
- 131.Abe T, Tashibu K, Ogami N. Gardner’s operation for syringomyelia. Spinal Surg. 1990;4:61–7. Japanese. [Google Scholar]
- 132.Yamaura A, Arai T, Ohtsuka Y. Surgery for syringomyelia-proposal of foramen magnum decompressionv. Spinal Surg. 1990;4:53–60. Japanese. [Google Scholar]
- 133.Isu T, Sasaki H, Takamura H, et al. Foramen magnum decompression with removal of the outer layer of the dura as treatment for syringomyelia occurring with Chiari I malformation. Neurosurgery. 1993;33:845–9. [PubMed] [Google Scholar]
- 134.Kubota M, Yamauchi T, Saeki N, et al. Foramen magnum decompression for syringomyelia with chiari-malformation. Spinal Surg. 2004;18:81–6. Japanese. [Google Scholar]
- 135.Phillips TW, Kindt GW. Syringoperitoneal shunt for syringomyelia: a preliminary report. Surg Neurol. 1981;16:462–6. doi: 10.1016/0090-3019(81)90248-2. [DOI] [PubMed] [Google Scholar]
- 136.Tator CH, Meguro K, Rowed DW. Favorable results with syringosubarachnoid shunts for treatment of syringomyelia. J Neurosurg. 1982;56:517–23. doi: 10.3171/jns.1982.56.4.0517. [DOI] [PubMed] [Google Scholar]
- 137.Barbaro NM, Wilson CB, Gutin PH, et al. Surgical treatment of syringomyelia. Favorable results with syringoperitoneal shunting. J Neurosurg. 1984;61:531–8. doi: 10.3171/jns.1984.61.3.0531. [DOI] [PubMed] [Google Scholar]
- 138.Padovani R, Cavallo M, Gaist G. Surgical treatment of syringomyelia: favorable results with syringosubarachnoid shunting. Surg Neurol. 1989;32:173–80. doi: 10.1016/0090-3019(89)90175-4. [DOI] [PubMed] [Google Scholar]
- 139.Isu T, Iwasaki Y, Abe H. Surgical technique of syringosubarachnoid shunt for syringomyelia. Operation. 1988;42:951–6. [Google Scholar]
- 140.Hida K, Iwasaki Y, Koyanagi I, et al. Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery. 1995;37:673–8. doi: 10.1227/00006123-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 141.Abe H. Syringomyelia. Clin Neurosci. 1995;20:1428–9. Japanese. [Google Scholar]
- 142.Sakamoto K, Kobayashi N, Sato N. Spina bifida occulta. Nerv Syst Child. 1978;3:187–96. Japanese. [Google Scholar]
- 143.Kaneko S, Abe H, Sasaki M, et al. Surgical results of spina bifida cystica-Bipedicle flaps method- Nerv Syst Child. 1979;4:251–8. Japanese. [Google Scholar]
- 144.Yamada H, Tanaka H, Nakamura S, et al. Prognosis and functional plasticity. Nerv Syst Child. 1983;8:263–70. Japanese. [Google Scholar]
- 145.Oi S, Ohshio T, Furukawa M, et al. Treatment for spina bifida. Pediatr Surg. 1985;17:343–9. [Google Scholar]
- 146.Sato K, Shimoji T, Sumie H, et al. Surgically confirmed myelographic classification of congenital intraspinal lipoma in the lumbosacral region. Childs Nerv Syst. 1985;1:3–11. doi: 10.1007/BF00706723. [DOI] [PubMed] [Google Scholar]
- 147.Oi S, Matsumoto S. Tethered cord syndrome. Neurosurgeons. 1988;7:117–32. [Google Scholar]
- 148.Hoffman HJ, Hendrick EB, Humphreys RP. The tethered spinal cord: its protean manifestations, diagnosis and surgical correction. Childs Brain. 1976;2:145–55. doi: 10.1159/000119610. [DOI] [PubMed] [Google Scholar]
- 149.McLone DG, Mutluer S, Naidich TP. Lipomeningoceles of the conus medullaris. In: Raimordi AJ, editor. Concepts in pediatric neurosurgery. Basel: Karger; 1983. pp. 170–7. [Google Scholar]
- 150.Koyanagi I, Iwasaki Y, Hida K, et al. Tethered cord syndrome with lumbar lipoma. Spine Spinal Cord. 1997;10:683–8. Japanese. [Google Scholar]
- 151.Koyanagi I, Iwasaki Y, Hida K, et al. Surgical treatment supposed natural history of the tethered cord with occult spinal dysraphism. Childs Nerv Syst. 1997;13:268–74. doi: 10.1007/s003810050081. [DOI] [PubMed] [Google Scholar]
- 152.Arai H, Miyajima M, Yada O. Significance of preventive surgery for spina bifida occulta. In: Report of research for diagnosis, therapy and prevention for spina bifida occulta. Tokyo: Ministry of Health and Welfare; 2002. pp. 27–34. Japanese. [Google Scholar]
- 153.Arai H. Diagnosis and treatment of lumbosacral lipoma. Spine Spinal Cord. 2002;15:849–55. Japanese. [Google Scholar]
- 154.Koyanagi I, Hida K, Iwasaki Y, et al. Radiological findings and clinical course of conus lipoma: implications for surgical treatment. Neurosurgery. 2008;63:546–51. doi: 10.1227/01.NEU.0000324727.61036.23. [DOI] [PubMed] [Google Scholar]
- 155.Scoville WB, Sharman IJ. Platybasia, report of ten cases with comments on familial tendency, a special diagnostic sign and end results of operation. Ann Surg. 1951;133:469–502. doi: 10.1097/00000658-195104000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fang HSY, Ong GB. Direct anterior approach to the upper cervical spine. J Bone Joint Surg. 1962;44:1588–604. [Google Scholar]
- 157.Greenberg AD, Scoville WB, Davey LM. Transoral decompression of atlanto-axial dislocation due to odontoid hypoplasia. Report of two cases. J Neurosurg. 1968;28:266–9. doi: 10.3171/jns.1968.28.3.0266. [DOI] [PubMed] [Google Scholar]
- 158.Spetzler RF, Selman WR, Nash CL, Jr, et al. Transoral microsurgical odontoid resection and spinal cord monitoring. Spine (Phila Pa 1976) 1979;4:506–10. doi: 10.1097/00007632-197911000-00009. [DOI] [PubMed] [Google Scholar]
- 159.Menezes AH, VanGilder JC, Graf CJ, et al. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53:444–55. doi: 10.3171/jns.1980.53.4.0444. [DOI] [PubMed] [Google Scholar]
- 160.Crockard HA, Pozo JL, Ransford AO, et al. Transoral decompression and posterior fusion for rheumatoid atlantoaxial subluxation. J Bone Joint Surg Br. 1986;68:350–6. doi: 10.1302/0301-620X.68B3.3733795. [DOI] [PubMed] [Google Scholar]
- 161.Abe H, Tsuru M, Mitsumori K, et al. Atlanto-axial dislocation, Instability index and indication for surgery. Neurol Surg. 1976;4:57–72. Japanese. [PubMed] [Google Scholar]
- 162.Abe H, Tsuru M, Iwasaki Y. Anterior fixation for anomaly of craniovertebral junction. in Research of generation and prevention for abnormality of spine and spinal cord. Tokyo: Ministry of Health and Welfare; 1983. pp. 58–65. Japanese. [Google Scholar]
- 163.Kohshu K, Muraishi K, Sonobe M, et al. Transoral approach to atlanto-axial dislocation-a case report- Spinal Surg. 1989;3:89–93. Japanese. [Google Scholar]
- 164.Kohno K, Sakaki S, Shiraishi T, et al. Successful treatment of adult Arnold-Chiari malformation associated with basilar impression and syringomyelia by the transoral anterior approach. Surg Neurol. 1990;33:284–7. doi: 10.1016/0090-3019(90)90050-y. [DOI] [PubMed] [Google Scholar]
- 165.Nakagawa H, Yamada H, Yamamoto H, et al. One-stage surgery for congenital atlanto-axial dislocation. Spinal Surg. 1994;8:99–104. Japanese. [Google Scholar]
- 166.Takahashi T, Suzaki N, Sawamura S. Anterior decompression and posterior fixation to diseases of craniovertebral junction. Spine Spinal Cord. 1995;8:601–9. Japanese. [Google Scholar]
- 167.Akino M, Abe H, Hida K, et al. Surgical treatment for diseases of craniovertebral junction. Spinal Surg. 1997;11:123–8. Japanese. [Google Scholar]
- 168.Takayasu M, Yasuda M, Joukou M, et al. Minimal invasive transoral approach to odontoid process. Spinal Surg. 2006;20:149–56. Japanese. [Google Scholar]
- 169.Takayasu M. Surgical strategy of craniovertebral junction. Jpn J Neurosurg. 2013;22:427–34. Japanese. [Google Scholar]
- 170.Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69:895–903. doi: 10.3171/jns.1988.69.6.0895. [DOI] [PubMed] [Google Scholar]
- 171.Chono Y, Abe H, Iwasaki Y. Total removal of a foramen magnum meningioma-a case report- Neurol Surg. 1985;13:109–14. Japanese. [PubMed] [Google Scholar]
- 172.Abe H, Ishii N, Sakuma S. Transoral approach to tumors of foramen magnum. In: Tabuchi, editor. Surgery of brain tumor. Tokyo: MC Medica Pub; 2006. pp. 260–9. Japanese. [Google Scholar]
- 173.Miyagi A, Maeda H, Sugawara T. Advantage of endoscope and neuronavigator to removal for clivus chordoma. Neurol Surg. 1998;26:169–75. Japanese. [PubMed] [Google Scholar]
- 174.Mori Y, Takayasu M, Saito K, et al. Benign osteoblastoma of the odontoid process of the axis: a case report. Surg Neurol. 1998;49:274–7. doi: 10.1016/s0090-3019(97)00190-0. [DOI] [PubMed] [Google Scholar]
- 175.Imamura J, Ikeyama Y, Tsutida E, et al. Transoral transclival approach for intradural lesions using a protective bone baffle to block cerebrospinal fluid pulse energy--two case reports. Neurol Med Chir (Tokyo) 2001;41:222–6. doi: 10.2176/nmc.41.222. [DOI] [PubMed] [Google Scholar]
- 176.Abe H. Surgery for tumors around foramen magnum. Neurol Surg. 1983;11:353–8. [PubMed] [Google Scholar]
- 177.Abe H. Surgery for foramen magnum tumors. Spine Spinal Cord. 1989;2:219–28. Japanese. [Google Scholar]
- 178.Sano K, Jinpo M, Saito I. Tanspharyngeal approach to an aneurysm of the basilar artery-a case report- Brain and Nerve. 1966;18:1197–203. Japanese. [PubMed] [Google Scholar]
- 179.Hashi K, Hakuba A, Ikuno H. Transoral transclival approach to the basilar aneurysm. Neurol Surg. 1976;4:183–9. Japanese. [PubMed] [Google Scholar]
- 180.Yamaura A, Makino H, Isobe K, et al. Repair of cerebrospinal fluid fistula following transoral transclival approach to a basilar aneurysm. Technical note. J Neurosurg. 1979;50:834–8. doi: 10.3171/jns.1979.50.6.0834. [DOI] [PubMed] [Google Scholar]
- 181.Saito I, Takahashi H, Joshita H, et al. Clipping of vertebrobasilar aneurysms by the transoral transclival approach. Neurol Med Chir (Tokyo) 1980;20:753–8. doi: 10.2176/nmc.20.753. [DOI] [PubMed] [Google Scholar]
- 182.Hayakawa T, Kamikawa K, Ohnishi T, et al. Transoral transclival approach to aneurysms of the basilar artery - experience with three cases (author’s transl) Neurol Med Chir (Tokyo) 1981;21:477–84. doi: 10.2176/nmc.21.477. [DOI] [PubMed] [Google Scholar]
- 183.Abe H, Miyamachi K, Takikawa S. Transoral approach to the vertebro-basilar aneurysms. In the Abstract of the 44th Annual Meeting of Japan Neurological Surgery; 1985. p. 264. Japanese. [Google Scholar]
- 184.Hayakawa T, Yamada K, Yoshimine T, et al. Transoral transclival approach to the vertebrobasial aneurysms. Neurol Surg. 17:609–14. Japanese. [PubMed] [Google Scholar]
- 185.Takayasu M. Present and future of surgery for craniovertebral junction. Jpn J Neurosurg. 1989;15:609–14. Japanese. [Google Scholar]
- 186.Takayasu M. Surgery of craniovertebral junction-choice and point of surgical method- Jpn J Neurosurg. 2016;25:737–45. Japanese. [Google Scholar]
- 187.Yada K, Tsuru M. Surgical treatment for spinal cord injury-decompression for acute spinal cord injury- Saigai Igaku. 1963;6:131–6. Japanese. [Google Scholar]
- 188.Tsuru M. “Whip lash injury”-neurosurgical treatment- Clin Orthop. 1968;3:315–23. Japanese. [Google Scholar]
- 189.Kadoya S, Nakamura T. Choice and trimming of treatment for cervical spine and spinal cord injury. Orthop Surg Traumatol. 1986;29:15–22. Japanese. [Google Scholar]
- 190.Nakamura T, Kadoya S. Treatment of acute cervical spine and spinal cord injury. Japan Med Soc Spinal Cord Lesion. 1990;3:18–9. Japanese. [Google Scholar]
- 191.Yamamoto H, Nakagawa H, Yamada T, et al. MRI finding of spine and spinal cord injury. Prog CT. 1992;14:155–60. Japanese. [Google Scholar]
- 192.Takahashi I, Koyanagi I, Hida K, et al. MRI finding of acute cervical cord injury. Neurotraumatology. 1995;18:205–9. Japanese. [Google Scholar]
- 193.Takahashi I, Kitahara T, Endo M, et al. Treatment of acute cervical cord injury-Multiple trauma and complications- Spine Spinal Cord. 1999;12:371–6. Japanese. [Google Scholar]
- 194.Nakagawa H, Mizuno J, Cho K. Surgery for cervical spine and spinal cord injury-Spinal instrumentation and navigation- Nichidoku-Iho. 2000;45:317–26. Japanese. [Google Scholar]
- 195.Morota N, Nakagawa H. Treatment for spine and spinal cord injury in childhood. Nerv Syst Child. 1998;23:314–22. Japanese. [Google Scholar]
- 196.Koyanagi I, Iwasaki Y, Hida K, et al. Acute cervical cord injury without fracture or dislocation of the spinal column. J Neurosurg. 2000;93(1 Suppl):15–20. doi: 10.3171/spi.2000.93.1.0015. [DOI] [PubMed] [Google Scholar]
- 197.Anzai K, Imoo M, Horita T, et al. Cervical laminoplasty for cervical cord injury without fractures or dislocations of the cervical column. Spinal Surg. 2003;17:7–14. Japanese. [Google Scholar]
- 198.Hirano H, Ito Y, Sugawara T, et al. Surgical treatment for cervical cord injury without fractures or dislocations of the cervical column. Spinal Surg. 2003;17:15–22. Japanese. [Google Scholar]
- 199.Suzuki S, Inoue T, Murakami K, et al. Acute treatment for spinal cord injury. Jpn J Neurosurg. 2017;26:200–7. Japanese. [Google Scholar]
- 200.Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) PLoS One. 2012;7:e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Jug M, Kejžar N, Vesel M, et al. Neurological Recovery after Traumatic Cervical Spinal Cord Injury Is Superior if Surgical Decompression and Instrumented Fusion Are Performed within 8 Hours versus 8 to 24 Hours after Injury: A Single Center Experience. J Neurotrauma. 2015;32:1385–92. doi: 10.1089/neu.2014.3767. [DOI] [PubMed] [Google Scholar]
- 202.Suzuki S. Acute treatment and management of spinal cord injury. Neurol Surg. 2014;42:777–93. Japanese. [Google Scholar]
- 203.Kadoya S. Cervical and lumbar spondylosis. Spinal Surg. 1997;11:1–12. Japanese. [Google Scholar]
- 204.Sato H, Kadoya S. Surgery for lumbar canal stenosis. Spine Spinal Cord. 1994;7:685–9. Japanese. [Google Scholar]
- 205.Sato H, Umemori T, Yamamoto N, et al. Long term results of limited decompression for lumbar canal stenosis. Spinal Surg. 1998;12:187–94. Japanese. [Google Scholar]
- 206.Koyama T. Concept of spinal canal stenosis. Spine Spinal Cord. 1994;9:659–64. Japanese. [Google Scholar]
- 207.Koyama T, Fujisawa H. Lumbar disc hernia. Jpn J Neurosurg. 1995;4:104–10. Japanese. [Google Scholar]
- 208.Hanakita J, Mizuno J, Suwa H, et al. Experience of 257 cases of lumbar canal stenosis. Spinal Surg. 1995;9:95–102. Japanese. [Google Scholar]
- 209.Hanakita J. Pathogenesis and surgery of lumbar spondylosis-minimal invasive surgery- Jpn J Neurosurg. 2004;13:183–9. Japanese. [Google Scholar]
- 210.Hanakita J, Suwa H. Posterior decompression and posterolateral fusion for lumbar degenerative diseases. Spinal Surg. 1998;12:111–22. Japanese. [Google Scholar]
- 211.Hanakita J. Compications in 3,486 cases of spine and spinal cord surgery by single operator. Jpn J Neurosurg. 2007;16:632–43. Japanese. [Google Scholar]
- 212.Shoda M, Kuno S, Inoue T, et al. Lumbar instrumentation-pedicle screw and posterior lumbar interbody fusion- Spinal Surg. 2011;25:130–4. Japanese. [Google Scholar]
- 213.Mizuno M, Kuraishi K, Suzuki H. Change and evolution of lumbar fusion. Neurol Surg. 2017;45:759–69. doi: 10.11477/mf.1436203589. Japanese. [DOI] [PubMed] [Google Scholar]
- 214.Hara M, Nishimura Y, Takemoto M, et al. Posterior fusion for lumbar degenerative diseases-mini open TLIF- Jpn J Neurosurg. 2012;21:118–27. Japanese. [Google Scholar]
- 215.Shoda M, Yoshida K, Yamamoto Y. Pedicle screw and posterior lumbar interbody fusion for lumbar spondylolisthesis. Spinal Surg. 2015;29:5–9. Japanese. [Google Scholar]
- 216.Sugawara J, Isu T, Kim K, et al. Posterior decompression for lumbar spondylosis-spondylolisthesis. Spinal Surg. 2007;21:137–44. Japanese. [Google Scholar]
- 217.Sugawara J, Isu T, Kim K, et al. Surgical results of posterior decompression for lumbar canal stenosis with lumbar spondylolisthesis. Spinal Surg. 2009;23:225–30. Japanese. [Google Scholar]
- 218.Sugawara J, Isu T, Kim K, et al. Posterior decompression for lumbar canal stenosis with lumbar spondylolisthesis. Jpn J Neurosurg. 2012;21:111–7. Japanese. [Google Scholar]
- 219.Baba I, Yamazaki A. Long term results of non-fusion for degenerative spondylolisthesis. J Joint Surg. 2001;20:736–45. Japanese. [Google Scholar]
- 220.Nishimura Y, Tsuneoka T, Hara H, et al. Lumbar pain by decompression for lumbar degenerated spondylolisthesis. Clin Orthop. 2001;36:825–8. Japanese. [Google Scholar]
- 221.Nishizawa T, Chiba K, Nakamura M, et al. Long term results of posterior decompression for lumbar spondylolisthesis-postoperative instability by laminectomy and minimal laminotomy- Clini Orthop. 2003;38:493–99. Japanese. [Google Scholar]
- 222.Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976) 1988;13:696–706. [PubMed] [Google Scholar]
- 223.Poletti CE. Central lumbar stenosis caused by ligamentum flavum: unilateral laminotomy for bilateral ligamentectomy: preliminary report of two cases. Neurosurgery. 1995;37:343–7. doi: 10.1227/00006123-199508000-00025. [DOI] [PubMed] [Google Scholar]
- 224.Yamada H, Yamamoto H, Nakajima M. Unilateral laminotomy for lumbar canal stenosis. Spinal Surg. 1996;9:110–5. Japanese. [Google Scholar]
- 225.Harada N, Harada T. Unilateral approach with bilateral decompression for lumbar canal stenosis. Spinal Surg. 1998;12:33–40. Japanese. [Google Scholar]
- 226.Suwa H, Hanakita J, Morimoto M, et al. Unilateral approach with bilateral ligamentectomy for lumbar canal stenosis. Spinal Surg. 1998;12:177–86. Japanese. [Google Scholar]
- 227.Inoue Y, Nishi H, Shimizu Y, et al. Microscopic ligamentectomy for central lumbar canal stenosis-unilateral approach- Spinal Surg. 2003;17:131–8. Japanese. [Google Scholar]
- 228.Iwatsuki K, Yoshimine T, Kato A, et al. Unilateral laminotomy and bilateral partial facetectomy for lumbar canal stenosis. Spinal Surg. 2003;17:125–30. Japanese. [Google Scholar]
- 229.Okuda O, Sato K, Arai H, et al. Surgical results of lumbar canal stenosis. Geriatr Neurosurg. 2006;18:77–82. Japanese. [Google Scholar]
- 230.Kino T, Hanakita J, Takahashi T, et al. Unilateral approach with bilateral yellow ligamentectomy for lumbar canal stenosis. Spinal Surg. 2009;23:183–8. Japanese. [Google Scholar]
- 231.Sasaki M, Aoki M, Fujiwara M, et al. Anatomy of bilateral lumbar canal decompression by unilateral approach for lumbar canal stenosis. Spinal Surg. 2011;25:203–8. Japanese. [Google Scholar]
- 232.Hanakita J. Surgery for OPLL of thoracic spine-Removal of OPLL by microscopic anterolateral approach- Spinal Surg. 2013;27:106–13. Japanese. [Google Scholar]
- 233.Iwasaki Y, Abe H, Isu T, et al. CT myelography with intramedullary enhancement in cervical spondylosis. J Neurosurg. 1985;63:363–6. doi: 10.3171/jns.1985.63.3.0363. [DOI] [PubMed] [Google Scholar]
- 234.Tachibana S, Okada K, Ohwada T, et al. Surgical treatment for acute spinal cord injury-Effect of posterior longitudinal myelotomy- Neurol Surg. 1984;12:183–8. Japanese. [PubMed] [Google Scholar]
- 235.Tachibana S. Experimental study of spinal cord injury by hyperextension of cervical spine. EEG EMG. 1986;14:114–21. Japanese. [Google Scholar]
- 236.Tachibana S, Kitahara Y, Iida H, et al. Spinal cord intramedullary pressure. A possible factor in syrinx growth. Spine (Phila Pa 1976) 1994;19:2174–8. [PubMed] [Google Scholar]
- 237.Tachibana S. Surgical treatment for neuropathy by nerve entrapment. Clin Neurol. 2012;52:840–3. doi: 10.5692/clinicalneurol.52.840. Japanese. [DOI] [PubMed] [Google Scholar]
- 238.Isu T, Kamada K, Kobayashi N, et al. The surgical technique of anterior cervical fusion using bone grafts obtained from cervical vertebral bodies. J Neurosurg. 1994;80:16–9. doi: 10.3171/jns.1994.80.1.0016. [DOI] [PubMed] [Google Scholar]
- 239.Isu T, Kim K, Morimoto D, et al. Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain. Neurospine. 2018;15:25–32. doi: 10.14245/ns.1836024.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Iizuka H, Yamamoto T, Iwasaki Y, et al. Experimental spinal cord injury: quantitation of axonal damage by automated image analysis. J Neurosurg. 1986;64:304–8. doi: 10.3171/jns.1986.64.2.0304. [DOI] [PubMed] [Google Scholar]
- 241.Iizuka H, Yamamoto H, Iwasaki Y, et al. Evolution of tissue damage in compressive spinal cord injury in rats. J Neurosurg. 1987;66:595–603. doi: 10.3171/jns.1987.66.4.0595. [DOI] [PubMed] [Google Scholar]
- 242.Iizuka H, Kadoya S. Spine-spinal cord injury-upper cervical spine- In: Tsubokawa T, Takakura K, Kikuchi H, editors. New neurosurgery. Tokyo: Asakura-shoten; 1996. pp. 896–907. Japanese. [Google Scholar]
- 243.Iizuka H, Iida T, Sato H. Posterior approach to lumbar spine. In: Date I, Morita A, Kikuta K, editors. Surgical approach for young neurosurgeons. Tokyo: Medical View; 2015. pp. 160–72. [Google Scholar]
- 244.Takayasu M, Aoyama M, Joko M, et al. Surgical Intervention for Instability of the Craniovertebral Junction. Neurol Med Chir (Tokyo) 2016;56:465–75. doi: 10.2176/nmc.ra.2015-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Mizuno J, Nakagawa H, Inoue T, et al. Clinicopathological study of “snake-eye appearance” in compressive myelopathy of the cervical spinal cord. J Neurosurg. 2003;99(2 Suppl):162–8. doi: 10.3171/spi.2003.99.2.0162. [DOI] [PubMed] [Google Scholar]
- 246.Mizuno J, Nakagawa H, Matsuo N, et al. Dural ossification associated with cervical ossification of the posterior longitudinal ligament: frequency of dural ossification and comparison of neuroimaging modalities in ability to identify the disease. J Neurosurg Spine. 2005;2:425–30. doi: 10.3171/spi.2005.2.4.0425. [DOI] [PubMed] [Google Scholar]
- 247.Mizuno J, Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6(6 Suppl):282S–288S. doi: 10.1016/j.spinee.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 248.Hida K, Iwasaki Y, Yano S, et al. Long-term follow-up results in patients with cervical disk disease treated by cervical anterior fusion using titanium cage implants. Neurol Med Chir (Tokyo) 2008;48:440–6. doi: 10.2176/nmc.48.440. [DOI] [PubMed] [Google Scholar]
- 249.Hida K, Iwasaki Y, Seki T, et al. two-stage operation for resection of spinal cord astrocytomas: technical case report of three cases. Neurosurgery. 2006;58(4 Suppl 2):ONS–E373. doi: 10.1227/01.NEU.0000208965.41531.A3. [DOI] [PubMed] [Google Scholar]
- 250.Koyanagi I, Iwasaki Y, Hida K, et al. Acute cervical cord injury associated with ossification of the posterior longitudinal ligament. Neurosurgery. 2003;53:887–91. doi: 10.1227/01.neu.0000083590.84053.cc. [DOI] [PubMed] [Google Scholar]
- 251.Koyanagi I, Iwasaki Y, Hida K, et al. Factors in neurological deterioration and role of surgical treatment in lumbosacral spinal lipoma. Childs Nerv Syst. 2000;16:143–9. doi: 10.1007/s003810050481. [DOI] [PubMed] [Google Scholar]
- 252.Koyanagi I, Tator CH, Theriault E. Silicone rubber microangiography of acute spinal cord injury in the rat. Neurosurgery. 1993;32:260–8. doi: 10.1227/00006123-199302000-00015. [DOI] [PubMed] [Google Scholar]
- 253.Koyanagi I, Tator CH, Lea PJ. Three-dimensional analysis of the vascular system in the rat spinal cord with scanning electron microscopy of vascular corrosion casts. Part 2: Acute spinal cord injury. Neurosurgery. 1993;33:285–91. [PubMed] [Google Scholar]


