Abstract
Background:
The morphometric characteristics of the anterior cruciate ligament (ACL) and the femoral intercondylar notch within which it resides have been implicated as risk factors for injuries to this important stabilizer of the knee. Prior research has produced equivocal results with differing methodologies, and consequently, it is unclear how these characteristics affect the injury risk in male and female patients.
Hypothesis:
The morphometric characteristics of the ACL and femoral intercondylar notch are individually and independently associated with the risk of suffering a noncontact ACL injury, and these relationships are different in male and female patients.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Magnetic resonance imaging scans of the bilateral knees were obtained on 88 case-control pairs (27 male, 61 female) matched for age, sex, and participation on the same sports team. Patients had suffered a grade III, first-time, noncontact ACL tear. The femoral notch width at 4 locations, the thickness of the bony ridge at the anteromedial outlet of the femoral notch, the femoral notch volume, ACL volume, and ACL cross-sectional area were measured.
Results:
Multivariate analysis of combined data from male and female patients revealed that decreased ACL volume (odds ratio [OR], 0.829), decreased femoral notch width (OR, 0.700), and increased bony ridge thickness at the anteromedial outlet of the femoral notch (OR, 1.614) were significant independent predictors of an ACL injury. Separate analyses of male and female patients indicated that the femoral notch ridge may be more strongly associated with a risk in female patients, while ACL volume is more strongly associated with a risk in male patients. However, statistical analysis performed with an adjustment for body weight strengthened the association between ACL volume and the risk of injuries in female patients.
Conclusion:
Morphometric features of both the ACL and femoral notch combine to influence the risk of suffering a noncontact ACL injury. When included together in a multivariate model that adjusts for body weight, the effects of the morphometric measurements are similar in male and female patients. If body weight is not taken into consideration, ACL volume is not associated with a risk in female patients.
Keywords: ACL, femoral intercondylar notch, knee anatomy
Injuries to the anterior cruciate ligament (ACL) of the knee are common and debilitating; however, the combination of risk factors that predispose patients to this injury is unknown. It is estimated that there are 100,000 to 200,000 ACL injuries per year in the United States.26,35 Both intrinsic and extrinsic factors have been investigated as potential risk factors for ACL tears. Intrinsic factors that have been studied include variations in knee anatomy such as ACL size, shape of the tibial plateau, and morphometry of the femoral intercondylar notch.32 It is unclear what significance a narrow notch has with regard to ACL injuries. It is possible that a small notch is an indication of a small ACL, which is more susceptible to injuries.9,10 It has also been theorized that a narrow notch produces mechanical impingement of the ACL, which results in a shear force that could act to tear the ligament during high-risk movements or where repetitive contact between the ligament and bone reduces the structural properties of the ligament over time.30
Various imaging techniques have been employed to characterize the morphometry of the femoral notch and its relationship to the risk of an ACL injury. Numerous studies have examined plain radiographs of the femoral notch to determine whether stenosis of the notch is a risk factor. Results of these studies have been equivocal, with several showing an inverse relationship between the femoral notch width and the risk of suffering an ACL tear21,22,25,28,29,33,34 and others showing no relationship.18,20,23,24,27 These divergent findings may be explained, at least in part, by differences in study designs, methodologies, or inaccurate measurements. For example, Anderson et al3 found that the various methods for plane film radiographic measurement of the femoral notch are inaccurate when compared with direct measurement in cadaveric specimens. Many of the femoral notch width studies used the notch width index (NWI), described by Souryal et al,34 to account for changes in the notch width that occur with increasing patient size. However, the NWI assumes that both the notch width and femoral bicondylar width increase with increasing height. This assumption has been questioned by studies showing that the femoral notch width does not increase with an increase in height, and therefore, the NWI may not provide good standardization.8,28
More recent studies have used magnetic resonance imaging (MRI)- and computed tomography-based techniques to characterize the femoral notch and ACL geometry in 3 dimensions in an effort to determine their relationship to the risk of ACL injuries. Using these comprehensive measurement techniques, several studies have reported significant differences in either notch widths or NWIs between patients with and without ACL injuries,5,11,14,19,30 while other studies have found no significant difference in the notch width or NWI between such groups.1,2,15,18 Two studies have measured notch volumes in ACL-injured patients and found that they were either not different30 or paradoxically larger38 than those of control participants. There is evidence that the presence of a bony ridge on the anteromedial aspect of the femoral notch is a potential risk factor for a noncontact ACL injury.14 Researchers have also investigated whether ACL size and/or volume are related to the injury risk, and this has revealed that ACL-injured patients had significantly smaller ACL volumes than control participants.11 It has consistently been shown that women have smaller ACLs, medial femoral condyles, lateral femoral condyles, and bicondylar widths than men.4,7,37 This may partially account for 2.4 to 9.5 times the increased risk of ACL injuries in women compared with men.17 Lastly, there is evidence that the femoral notch size is correlated with the size of the ACL.9,10 In addition to different measurement and imaging techniques, conflicting results may be caused by a number of factors, including the use of control participants who differ from injured patients in their athletic activities, risk exposure, levels of play, and playing conditions.
Despite previous research, it remains unclear how the morphometry of the ACL and femoral notch influence the risk of ACL injuries. One study derived a multivariate statistical model using stepwise logistic regression, which showed that the width of the posterior outlet of the notch and thickness of the bony ridge at the anteromedial outlet of the notch were significant independent predictors of injuries; however, the geometric properties of the ACL were not included in that model.14 To our knowledge, the current study is the first to examine the combined effects of ACL volume, femoral notch width, femoral notch volume, and thickness of the bony ridge at the anteromedial outlet of the femoral notch on the risk of suffering an ACL injury.
The objective of the current study was to measure the morphometry of the femoral intercondylar notch (width, volume, and thickness of the bony ridge at the anterome-dial outlet of the notch) and the ACL (volume and crosssectional area) in patients who suffered their first noncontact ACL injury and matched control participants to determine the individual and independent effects of those variables on the risk of suffering a noncontact ACL injury. We hypothesized that a decrease in ACL size (evaluated as volume and cross-sectional area) and a reduction in the region within which it resides (evaluated as intercondylar femoral notch width, femoral notch volume, and increased thickness of the bony ridge at the anteromedial outlet of the femoral notch) are individually and independently associated with the risk of suffering noncontact ACL injuries and that this relationship is different for male and female patients. This information is important to identify who is at increased risk for suffering an injury so that an intervention can be targeted to them and will serve as the supporting motivation for future clinical research.
MATERIALS AND METHODS
This report is based on an analysis of MRI data that were obtained as part of a larger prospective cohort study with a nested case-control analysis designed to develop a comprehensive multivariate risk model for noncontact ACL injuries.6,16,31 The larger study used a design that selected 3 matched control participants for each ACL-injured patient; however, the costs associated with MRI acquisition only permitted the selection of 1 control participant per ACL-injured patient for the current report. The 4-year study began in the fall 2008 sports season and involved athletes from 36 institutions (28 high schools and 8 colleges). Those responsible for providing medical care to the sports teams located at these institutions, such as licensed athletic trainers and physicians, identified and approached athletes about participation when an ACL injury was suspected. To be included, the ACL-injured patients and matched control participants were those in organized athletics. Patients injured while participating in their sport had to have suffered their first ACL injury (to either limb) that was confirmed by arthroscopic visualization at the time of surgery. A noncontact ACL injury was defined as an event occurring with no direct contact to the ACL-injured knee from another athlete, the ground, or other object. This was determined by the person responsible for medical care at the institution where the injury occurred and was confirmed by the injured patient. Injured patients were matched to control participants who were selected from the same team and were the same sex and age. The Committee on Human Research of the Medical Sciences Review Board at our institution approved this study. All participants and/or their legal guardians provided signed informed consent before participation.
MRI Protocol and Segmentation
The ACL-injured patients and control participants underwent bilateral MRI scans that were obtained as previously described6 using the same Phillips Achieva 3.0-T MRI scanner system equipped with an 8-channel SENSE knee coil (Phillips Medical Systems, Best, the Netherlands) at our institution’s research MRI facility. Patients were positioned supine in the scanner with the legs extended. The MRI scans obtained included sagittal T1-weighted 3-dimensional (3D) fast field echo (FFE) (resolution, 0.3 × 0.3 mm; slice thickness, 1.2 mm) and sagittal 3D proton density-weighted sequences (resolution, 0.4 × 0.4 mm; slice thickness, 0.7 mm). DICOM images were viewed and digitized using Osirix Software (Pixmeo v 3.6.1, open source, http://www.osirix-viewer.com). Manual segmentation was completed using a Cintiq 21UK digitizing tablet (Wacom Technology Corp, Vancouver, Washington, USA). Sagittal 3D T1-weighted FFE scans were used for measurements of the femoral notch volume and ACL volume. Coronal oblique scans were created using multiplanar reconstruction (MPR) on the proton density-weighted sequences by orienting the long axis parallel to the anterior border of the ACL, which were used for all measurements of the notch width and thickness of the bony ridge at the anteromedial outlet of the femoral notch. Similarly, an axial oblique plane oriented transverse to the ACL was aligned using MPR to calculate its cross-sectional area (Figure 1).
Figure 1.

Sagittal proton density-weighted scan through the midplane of the anterior cruciate ligament (ACL) showing the orientation of the coronal oblique plane (COB) parallel to the anterior border of the ACL and the orientation of the axial oblique plane (AOB) oriented transverse to the ACL.
Femoral Notch Measurements
A reference line (RL in Figure 2) was created as a tangent to the posterior subchondral aspects of both femoral condyles as previously described by Staeubli et al.36 All femoral notch widths were measured parallel to this reference line. The femoral notch width was measured at 4 levels in the coronal oblique plane: at the notch inlet (NW_I) posteriorly, at the notch outlet (NW_O) anteriorly, at the anterior attachment of the ACL to the lateral femoral condyle (NW_AA), and at the middle of the ACL attachment (NW_MA) (Figure 2). A femoral NWI was calculated for each notch width by dividing the notch width by the bicondylar width. The bony ridge on the anteromedial aspect of the medial femoral condyle was measured on consecutive slices in the coronal oblique plane (Figure 3). For each slice, a line was fit to the medial femoral notch wall using a least-squares approach (Figure 3). The ridge thickness was then calculated as the sum of 2 distances from the best-fit line, and these included the maximum point of the ridge extrusion and the first intrusion of the notch wall into the notch. This was done for each consecutive slice, and the maximum ridge thickness was used in the analyses. Femoral notch volume measurements were performed using a method similar to that described by Charlton et al.8 Axial 3D T1-weighted FFE scans were used, with the borders of the notch defined as follows: The most distal slice included was the last slice where there was continuity between the femoral condyles (Figure 4). The most proximal slice was the first slice with both femoral condyles clearly visible. The area of the notch was measured on each slice along the border of the notch, stopping posteriorly at the border of the articular cartilage (Figure 4). The volumes were then calculated by summating the areas of each slice and multiplying by the slice thickness (0.3 mm).
Figure 2.
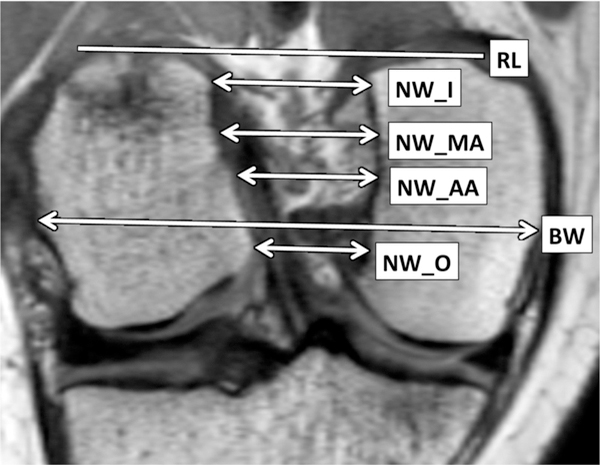
Coronal oblique proton density-weighted scan showing various measurements of the notch width. All widths were measured in the same orientation as the reference line (RL). BW, bicondylar width; NW_AA, notch width at the anterior attachment of the anterior cruciate ligament (ACL); NW_I, notch width at the inlet; NW_MA, notch width at the midattachment point of the ACL; NW_O, notch width at the outlet.
Figure 3.
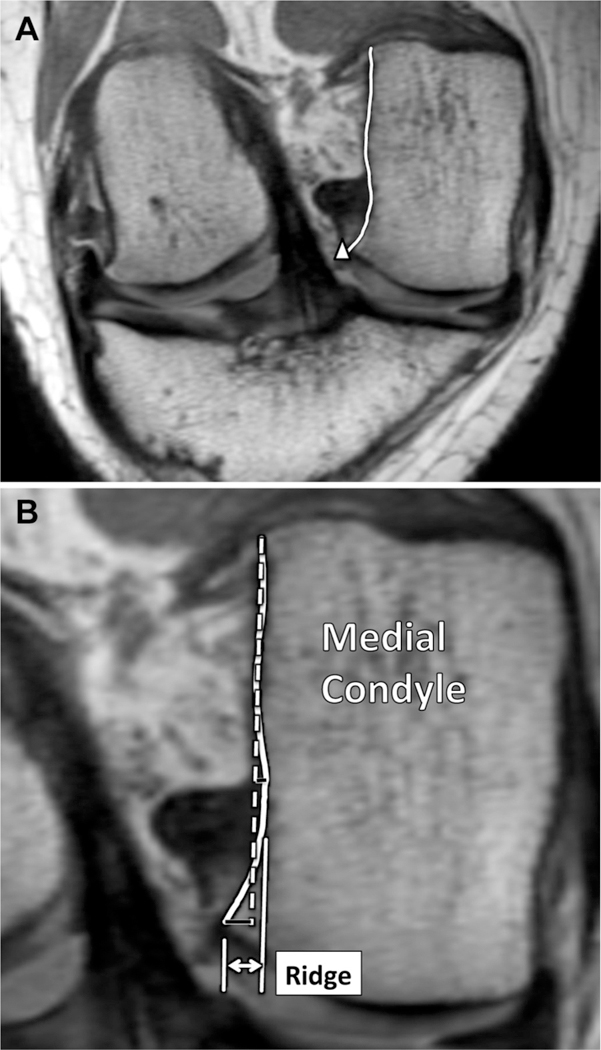
Notch ridge thickness: (A) In the coronal plane oblique to the anterior cruciate ligament, the contour of the medial wall is segmented (white line), starting with the most posterior portion and ending with the ridge peak (white triangle). (B) Best-fit line (dashed line) fit to the segmented notch wall (black squares). The notch ridge thickness is calculated as the sum of the perpendicular distance from the best-fit line to the peak of the ridge and the perpendicular distance from the best-fit line to the first intrusion of the notch wall (black lines). The notch ridge thickness was calculated on a series of coronal oblique slices, and the maximum ridge was used for analyses.
Figure 4.
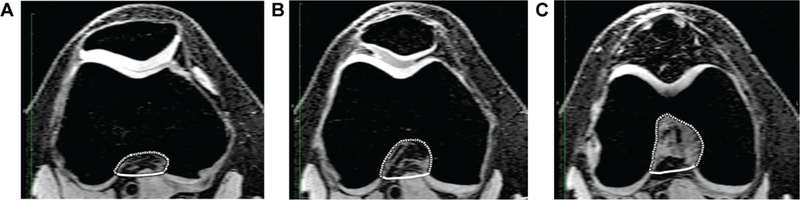
Axial T1-weighted 3-dimensional fast field echo scans showing the notch volume method. (A) The first slice chosen where both condyles are visible. (B) Slice in the middle. (C) Last slice included, where there is still continuity between the condyles.
ACL Measurements
Volumetric measurements of the ACL were obtained from sagittal T1-weighted scans by manual segmentation of the ACL, using a technique that was previously described to be reliable and accurate30 (Figure 5). The volume was calculated as the sum of the outlined areas multiplied by the slice thickness (1.2 mm). Using the coronal oblique plane, a point that was one third of the total length of the ACL from its attachment to the tibia was identified and marked. Then, in the axial oblique plane oriented to give a transverse view of the ACL, its circumference was segmented and the cross-sectional area calculated (Figure 6).
Figure 5.
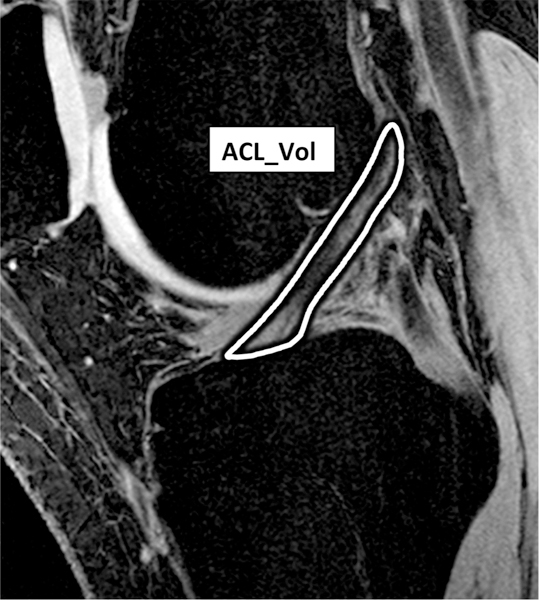
Anterior cruciate ligament outline (white line) in the sagittal plane for calculation of the volume.
Figure 6.
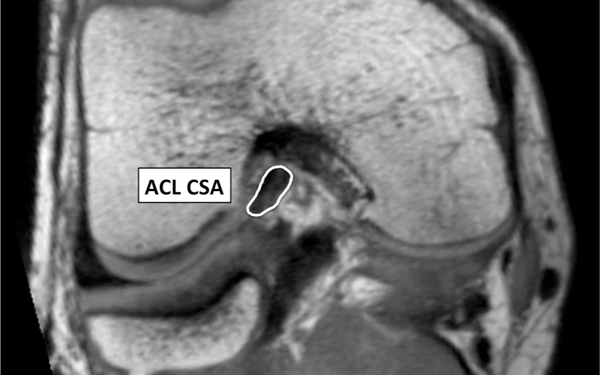
Axial oblique proton density–weighted scan depicting the cross-sectional area (CSA) at a transverse slice of the anterior cruciate ligament at a location one third of its overall length from the tibial insertion site.
Interexaminer and Intraexaminer Reliability
Reliability of the measurements was established using variance component analysis to estimate the variability between examiners, within examiners, and between participants. Intraclass correlation coefficients (ICCs) were then calculated using the approach described by Ellaszlw et al12 for assessing interobserver and intraobserver reliability. A random subset of knees (1 per patient) were measured at 2 different time points by 2 examiners, who were blinded to the identity of the patient, to assess reproducibility of the femoral notch and ACL measurements (see Appendix Figure A1, available in the online version of this article at http://ajsm.sagepub.com/supplemental). The ICCs for intrarater reliability ranged between 0.885 and 0.974 for the femoral notch measurements, ranged between 0.898 and 0.920 for the ACL measurements, and was 0.841 for the thickness of the bony ridge at the anteromedial outlet of the femoral notch measurement (Appendix Table A1, available online). Interrater ICCs were slightly lower, particularly for the ACL geometry measurements, but each of the measurements reported in this article was taken by the same person (Appendix Table A1).
Statistical Analysis
Most measurements of ACL and femoral notch morphometry were dependent on the patient having an intact ACL. Because the injured leg of our injured patients was ACL deficient, the contralateral uninjured leg was used. To support the use of the uninjured leg of the ACL-injured patients as a surrogate for the injured leg before the injury event, symmetry was established by investigating side-to-side differences in control participants using paired t tests.
The initial step was to use the ACL and femoral notch morphometry measurements of the uninjured knee of the ACL-injured patients and the corresponding knee of the matched controls in univariate conditional logistic regression analyses to assess their associations with the risk of suffering a noncontact ACL injury. The next step was to perform multivariate conditional logistic regression analysis to determine the independent effects of the ACL and femoral notch morphometry measurements (the primary study hypothesis). Because the notch width measurements made at the 4 locations are highly correlated, only 1 was used together with the notch ridge as measures of femoral notch geometry in the multivariate model. Both notch width at the outlet (NW_O) and anterior attachment of the ACL (NW_AA) had equally strong univariate associations with the risk of ACL injuries, but anterior attachment of the ACL (NW_AA) was selected for inclusion in the model because it retained a stronger association with the risk after adjusting for the femoral notch ridge. Similarly, ACL volume was included rather than cross-sectional area as a measure of ACL geometry because the 2 measures were correlated and ACL volume had a stronger association with the injury risk. Additional multivariate analyses were performed with height, weight, or body mass index (BMI) included as explanatory variables to determine if body size influenced the effects of the morpho-metric measurements on the injury risk. All statistical analyses were performed on female and male data separately as well as for male and female patients combined. A value of P < .05 was chosen as the level of significance.
RESULTS
There were 176 patients included in the study (88 patients who suffered a first noncontact ACL injury and 88 matched controls). There were 122 female patients (61 case-control pairs) and 54 male patients (27 case-control pairs). The demographics of the group, the sports in which they participated, and the time interval between the noncontact ACL injury and acquisition of the MRI scan have been published.6
Side-to-Side Comparisons of the Knees of Control Participants
There were no statistically significant side-to-side differences (injured vs uninjured knees as defined by the corresponding leg of the matched injured patient) in the control participants for all the measurements of ACL and femoral notch geometry (Appendix Table A2, available online). This supported the use of measurements obtained from the uninjured knee of the ACL-injured patients as surrogate measurements for the injured knee before the ACL disruption. We therefore tested our primary hypothesis using the uninjured side of the ACL-injured patients and the corresponding knee of the control participants by conditional logistic regression analyses. Descriptive statistics for the various measurements of the uninjured knee of ACL-injured patients and the corresponding leg of control participants in all groups are presented in Table 1.
TABLE 1.
Descriptive Statistics of Patientsa
| Variable | Female Patients | Male Patients | All Patients |
|---|---|---|---|
| NW_I, mm | |||
| Cases | 21.5 ± 2.2 | 24.6 ± 2.6 | 22.5 ± 2.7 |
| Controls | 22.4 ± 2.3 | 25.5 ± 3.4 | 23.4 ± 3.0 |
| NW_AA, mm | |||
| Cases | 18.0 ± 1.9 | 19.4 ± 2.1 | 18.4 ± 2.1 |
| Controls | 19.1 ± 1.9 | 21.1 ± 2.5 | 19.7 ± 2.3 |
| NW_MA, mm | |||
| Cases | 19.5 ± 2.2 | 21.0 ± 2.3 | 20.0 ± 2.3 |
| Controls | 20.2 ± 2.1 | 22.2 ± 2.9 | 20.8 ± 2.5 |
| NW_O, mm | |||
| Cases | 14.6 ± 2.5 | 16.4 ± 2.7 | 15.1 ± 2.6 |
| Controls | 16.1 ± 2.0 | 18.0 ± 2.4 | 16.7 ± 2.3 |
| N_Vol, mm3 | |||
| Cases | 6091.0 ± 1061.0 | 7782.0 ± 1524.0 | 6609.0 ± 1444.0 |
| Controls | 6466.0 ± 1178.0 | 8835.0 ± 1599.0 | 7193.0 ± 1711.0 |
| Ridge, mm | |||
| Cases | 3.7 ± 1.1 | 3.7 ± 1.5 | 3.7 ± 1.2 |
| Controls | 3.3 ± 0.9 | 3.7 ± 1.3 | 3.4 ± 1.1 |
| ACL_Vol, mm3 | |||
| Cases | 992.0 ± 230.0 | 1140.0 ± 344.0 | 1037.0 ± 277.0 |
| Controls | 1072.0 ± 249.0 | 1386.0 ± 363.0 | 1169.0 ± 321.0 |
| ACL_CSA, cm2 | |||
| Cases | 0.37 ± 0.11 | 0.40 ± 0.12 | 0.38 ± 0.11 |
| Controls | 0.39 ± 0.11 | 0.47 ± 0.11 | 0.41 ± 0.11 |
Data are reported as mean ± standard deviation for cases (n = 88) and matched controls (n = 88). ACL_CSA, anterior cruciate ligament (ACL) cross-sectional area; ACL_Vol, ACL volume; N_Vol, femoral notch volume; NW_AA, notch width at the anterior attachment of the ACL to the lateral femoral condyle; NW_I, notch width at the inlet; NW_MA, notch width at the middle of the ACL attachment; NW_O, notch width at the outlet; Ridge, bony ridge at the anteromedial outlet of the femoral notch.
Associations of Femoral Notch and ACL Geometry With the Risk of ACL Injuries
Univariate Analysis.
Univariate analysis of data obtained from the female patients as a group revealed that each of the femoral notch width measurements (NW_I, NW_AA, NW_MA, and NW_O) and the thickness of the bony ridge at the anteromedial outlet of the femoral notch (Ridge) were significantly associated with the risk of an ACL injury (Table 2). Univariate analysis of data from male patients as a group demonstrated that the femoral notch width measurements at both the anterior point of the ACL attachment and the anterior outlet of the ACL (NW_AA and NW_O, respectively) and both the volume and cross-sectional area of the ACL (ACL_Vol and ACL_CSA, respectively) were significantly associated with the risk of an ACL injury (Table 2). Odds ratios (ORs) for all of the femoral notch width measurements except notch width at the middle of the ACL attachment (NW_MA) indicated somewhat weaker associations with the risk of ACL injuries in male patients compared with female patients (Table 2). As a consequence of this and the smaller sample size, the ORs for the notch width measures were not as statistically significant in the male patients as in the female patients. In contrast, diminished femoral notch volume, ACL volume, and ACL cross-sectional area were significantly associated with an increased risk of ACL injuries in male patients but not in female patients (Table 2). The most notable dissimilarity in the ORs for male and female patients was observed for thickness of the bony ridge at the anteromedial outlet of the femoral notch. In female patients, an increase in thickness was significantly associated with an increase in the risk of ACL injuries (OR, 1.658), but there was no indication of such an association in male patients (OR, 0.972).
TABLE 2.
Univariate Logistic Regression for Female, Male, and Combined Data Comparing Uninjured Limbs of Cases to Corresponding Limbs of Controlsa
| Variable | Female Patients | Male Patients | All Patients |
|---|---|---|---|
| NW_I, mm | 0.845 (0.714–0.999)b | 0.918 (0.77S-1.090) | 0.878 (0.777–0.992)b |
| NW_AA, mm | 0.693 (0.544–0.883)c | 0.745 (0.566–0.979)b | 0.714 (0.595–0.857)c |
| NW_MA, mm | 0.817 (0.670–0.996)b | 0.812 (0.628–1.051) | 0.815 (0.697–0.954)b |
| NW_O, mm | 0.692 (0.557–0.859)c | 0.722 (0.528–0.986)b | 0.701 (0.587–0.838)c |
| N_Vol,d mm3 | 0.968 (0.935–1.003) | 0.943 (0.892–0.996)b | 0.960 (0.932–0.987)b |
| Ridge, mm | 1.658 (1.100–2.500)b | 0.972 (0.662–1.427) | 1.273 (0.969–1.672) |
| ACL_Vol,d mm3 | 0.850 (0.719–1.005) | 0.767 (0.610–0.964)b | 0.817 (0.717–0.931)c |
| ACL_CSA, cm2 | 0.973 (0.936–1.011) | 0.942 (0.890–0.998)b | 0.962 (0.932–0.993)b |
Data are reported as odds ratios (ORs) with corresponding 95% confidence intervals. ACL_CSA, anterior cruciate ligament (ACL) cross-sectional area; ACL_Vol, ACL volume; N_Vol, femoral notch volume; NW_AA, notch width at the anterior attachment of the ACL to the lateral femoral condyle; NW_I, notch width at the inlet; NW_MA, notch width at the middle of the ACL attachment; NW_O, notch width at the outlet; Ridge, bony ridge at the anteromedial outlet of the femoral notch.
P < .05.
P < .01.
OR calculated per 100 mm3.
When data from both male and female patients were considered as a combined group with univariate analysis, both femoral notch morphometry (NW_AA, NW_I, NW_MA, NW_O, and N_Vol) and ACL morphometry (ACL_Vol and ACL_CSA) were significantly associated with the risk of an ACL injury (all P < .05) (Table 2). A decrease in these measurements was associated with an increase in the risk of suffering an ACL injury. The only measurement not significantly related to the risk of suffering an ACL injury in the combined analysis was thickness of the bony ridge at the anteromedial outlet of the femoral notch.
For each of the notch width measurements, index ratios were calculated similarly to the previously described NWI by dividing the measurement by the bicondylar width of the femur.34 The use of these index ratios, however, did not strengthen any of the associations with the risk of ACL injuries that were observed using the unstandardized measurements.
Multivariate Analysis.
Multivariate analysis of the data obtained from the female patients demonstrated that the decreased femoral notch width at the anterior attachment of the ACL (NW_AA) (OR, 0.695; P = .005) and increased thickness of the bony ridge at the anteromedial outlet of the femoral notch (OR, 1.774; P = .017) were significant independent predictors of ACL injuries when included in a multivariate conditional logistic regression model with ACL volume (Table 3); ACL volume was not a significant predictor in the model for female patients.
TABLE 3.
Multivariate Conditional Logistic Regression for Analysis of Injury Risk, Unadjusted and Adjusted for Body Weighta
| Variable | Unit Change | Unadjusted Model | Model Adjusted for Body Weight | ||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | ||
| Female data only | |||||||
| NW_AA, mm | 1 mm | 0.695 | 0.540–0.894 | .005 | 0.629 | 0.469–0.843 | .002 |
| ACL_Vol, mm3 | 100 mm3 | 0.895 | 0.739–1.084 | .256 | 0.793 | 0.634–0.991 | .041 |
| Ridge, mm | 1 mm | 1.774 | 1.110–2.835 | .017 | 1.686 | 1.025–2.776 | .040 |
| Weight, kg | 1 kg | 1.088 | 1.020–1.161 | .011 | |||
| Male data only | |||||||
| NW_AA, mm | 1 mm | 0.699 | 0.494–0.990 | .044 | 0.722 | 0.495–1.053 | .091 |
| ACL_Vol, mm3 | 100 mm3 | 0.736 | 0.547–0.990 | .043 | 0.715 | 0.509–1.004 | .053 |
| Ridge, mm | 1 mm | 1.555 | 0.864–2.799 | .141 | 1.506 | 0.825–2.746 | .182 |
| Weight, kg | 1 kg | 1.015 | 0.946–1.088 | .681 | |||
| Combined data | |||||||
| NW_AA, mm | 1 mm | 0.700 | 0.574–0.854 | .0004 | 0.694 | 0.557–0.864 | .001 |
| ACL_Vol, mm3 | 100 mm3 | 0.829 | 0.713–0.965 | .015 | 0.772 | 0.647–0.921 | .004 |
| Ridge, mm | 1 mm | 1.614 | 1.146–2.272 | .006 | 1.556 | 1.093–2.216 | .014 |
| Weight, kg | 1 kg | 1.053 | 1.005–1.103 | .029 | |||
Data in bold represent statistically significant observations. ACL_Vol, anterior cruciate ligament (ACL) volume; NW_AA, notch width at the anterior attachment of the ACL to the lateral femoral condyle; OR, multivariate odds ratio for increase in unit change; Ridge, bony ridge at the anteromedial outlet of the femoral notch.
Multivariate analysis of the data obtained from the male patients indicated that the femoral notch width at the anterior attachment of the ACL (NW_AA) (OR, 0.699; P = .044) and the volume of the ACL (OR, 0.736; P = .043) were significant independent predictors of ACL injuries (Table 3). Notch ridge was not a statistically significant independent predictor of the risk for male patients (P = .141), but its OR of 1.555 was considerably larger than that in the univariate analysis and was more similar to the OR observed for female patients.
Multivariate conditional logistic regression analysis of the combined male and female data indicated that decreased femoral notch width at the anterior attachment of the ACL (NW_AA) (OR, 0.700; P = .0004), decreased ACL volume (OR, 0.829; P = .015), and increased thickness of the bony ridge at the anteromedial outlet of the femoral notch (OR, 1.614; P = .006) were significant independent predictors of an increased risk of ACL injuries when included together in a regression model (Table 3).
Adjustment for Body Size.
All regression analyses were repeated with height, weight, and BMI included as covari-ates. None of these measures of body size had a substantial effect on the associations between the morphometric measures and the risk of ACL injuries, but the largest effects were observed for weight, and only those are reported here. When each femoral notch and ACL geometry measurement was included in a model with weight, the results were generally very similar to those observed in the unadjusted univariate analyses. For female patients, however, the weight-adjusted ORs for femoral notch volume (OR, 0.946), ACL volume (OR, 0.760), and ACL cross-sectional area (OR, 0.947) were very similar to those observed for male patients and were significantly associated with the risk of ACL injuries.
When weight was added to the multivariate models, it only had a notable effect on the relationship between ACL volume and injury risk in the models fitted to the combined male and female data and data from female patients (Table 3). In female patients, the OR for ACL volume was 0.793 (P = .041) after adjusting for weight compared with 0.895 (P = .256) in the unadjusted model. As a consequence, the relationship between ACL volume and the risk of an ACL injury was also strengthened when weight was added to the multivariate model fitted to the combined data from male and female patients.
DISCUSSION
Multivariate analysis of the data from the female patients as a group, when adjusted for body weight, demonstrated that ACL volume, femoral intercondylar notch width, and thickness of the bony ridge at the anteromedial outlet of the femoral notch were significant independent predictors of ACL injuries. This finding was similar to that of the combined group analysis and suggests that a female patient with a smaller ACL volume is more susceptible to injuries than female patients of similar weights with larger ACL volumes and that the risk of injuries is increased with a decreased femoral notch size that is produced by the combination of a decreased femoral notch width and increased thickness of the bony ridge at the anteromedial outlet of the femoral notch. Multivariate analysis of the data from the male patients as a group revealed that ACL volume and femoral notch width were independently associated with ACL injuries. A decrease in each was associated with an increased risk of injuries; however, thickness of the bony ridge at the anteromedial outlet of the femoral notch was not associated with injuries for male patients. These findings provide support for our hypothesis that the morphometry of the ACL and the femoral notch within which it resides act individually and independently to influence the risk of suffering a noncontact ACL injury. While there were similarities in the relationship between ACL and femoral notch geometry and the risk of noncontact ACL injuries between male and female patients, there were differences. For example, the femoral notch ridge was more strongly associated with a risk in female patients, while ACL volume was more strongly associated with a risk in male patients. However, statistical analysis performed with an adjustment for body weight strengthened the association between ACL volume and the risk of injuries in female patients. For both sexes, it is unclear how ACL size is influenced by the bony structures that surround it during growth and development. It may be that a small femoral notch produces a small ACL, which creates a reduction in its structural properties and in turn predisposes the ligament to an increased risk of disruptions.30 Another mechanism that has been described is that a decrease in the femoral notch size produces bony impingement against a small ACL, which predisposes the ligament to an increased risk of failure.30 It may be that these 2 mechanisms act synergistically.
When considering the pooled data from the male and female patients, the multivariate analyses performed with and without adjusting for body weight demonstrated that a decrease in the ACL volume and femoral intercondylar notch width combined with an increase in the thickness of the bony ridge at the anteromedial outlet of the femoral notch have substantial influences on the risk of suffering a noncontact ACL injury. For example, the analysis without adjusting for body weight indicated that there is a 42.9% increase in the risk of ACL tears for a 1-mm decrease in the width of the femoral notch, a 20.6% increase in the risk of a tear for every 100-mm3 decrease in ACL volume (equivalent to one third the volume of a dime), and a 61.4% increase in the risk for every 1-mm increase in the thickness of the bony ridge at the anteromedial outlet of the femoral notch. Consequently, when considering the pooled data from male and female patients, a person who differs by these amounts in relation to the mean values of their peers on all 3 variables has 2.78 times the risk of suffering an ACL disruption (1.429 × 1.206 × 1.614 = 2.78). These variables affected the injury risk independently, and this finding suggests that the development of screening tools to determine who is at an increased risk of suffering an ACL disruption so that intervention programs can be targeted to them should include an assessment of both ACL and femoral notch morphometry. The analysis with an adjustment for body weight produced very similar associations with the risk of ACL injuries; in this case, a person who differed by the previously mentioned amounts in relation to the mean values of their peers on all 3 variables has 2.9 times the risk of an ACL tear.
The results from this study are in agreement with those of previous studies that have shown femoral notch stenosis as a risk factor for injuries.5,11,14,19,30 Everhart et al14 recently found significantly smaller notch widths at both the “anterior outlet” and “posterior outlet” in ACL-injured patients compared with controls. These measurements are comparable with our measurements, termed the notch width at the anterior outlet and posterior inlet (NW_O and NW_I, respectively). Our results support the conclusion that each notch width is an important femoral notch dimension in terms of its role as a risk factor for an ACL injury. The univariate analysis showed that the thickness of the bony ridge at the anteromedial outlet of the femoral notch was not a significant risk factor for the combined male and female data but that it was significant when considering the female patients as a group. This is in contrast with the Everhart et al14 study, which found significance in the pooled data and in male patients but not female patients. A subsequent cadaveric study by Everhart et al,13 however, showed more significant notch stenosis due to ridging in female patients compared with male patients. Our study confirmed their result of increased thickness of the bony ridge at the anteromedial outlet of the femoral notch as a significant predictor in the multivariate model of the pooled male and female data and when considering female patients alone. The stronger association between notch ridge thickness and the risk of suffering an ACL injury found in female patients may support the finding that notch stenosis occurs more frequently in female patients.
Other findings of the current study indicated that the total femoral notch volume and femoral notch width are significant risk factors for noncontact ACL injuries. Univariate analysis of the pooled male and female data revealed that a smaller femoral notch volume was associated with a significantly increased risk of ACL injuries. Although this finding was as hypothesized, it was in contrast with the previous literature that either failed to show a difference30 or paradoxically found larger femoral notch volumes38 in ACL-injured patients compared with controls. Aside from our finding regarding a decreased notch width at the outlet (NW_O), the only other notch width measurement that was significantly associated with the injury risk for the pooled male and female data as well as for male and female patients as separate groups was at the anterior attachment of the ACL (NW_AA). Bush et al (unpublished data, 2012) used the same 4 width measurements as our study and found that the notch width at the anterior attachment of the ACL (NW_AA) was most strongly correlated with peak ACL strain values.
An important aspect of our study design was that the control participants were randomly selected from a cohort of patients who had similar exposures with no ACL injury before or at the time the case patient was injured: This approach produced ORs from the nested case-control analysis that were similar to the relative risk estimates that would have been obtained from a complete analysis of all cohort members. Consequently, we were able to create a large sample size of patients who suffered noncontact ACL injuries and select sex-, age-, and activity-matched controls. It may seem obvious that participation in sports is a definitive risk factor for ACL injuries; however, many studies use healthy age-matched controls who do not participate in the same activity that produced the ACL injury or those who required an MRI scan for a knee-related concern that did not involve the ACL. Our study prospectively identified athletes suffering an ACL injury and paired them with control participants who were on the same sports team as the injured patients and therefore had similar environmental and athletic exposures. This study design allowed us to more directly assess how factors intrinsic to the ACL and bony structures of the knee that surround it affect the injury risk. We also found that controlling for femoral bicondylar width (a surrogate for femur size) did not change the significance of the results. This finding suggests that features of the knee joint that most influence the risk of ACL injuries include the geometric properties of the ACL and bony intercondylar notch of the femur.
The patients in this study were part of a larger prognostic investigation of the risk factors for an ACL injury. These included measures of body size (patient height, weight, and BMI) as independent predictors of ACL injuries, and consequently, we did not match cases and controls based on these variables. To explore whether body size had an effect on the associations between the morpho-metric measures obtained in the current study and the risk of ACL injuries, we repeated all regression analyses with height, weight, and BMI included as covariates. None of these measures of body size had a substantial effect on the associations between the morphometric measures and the risk of ACL injuries. The largest effect was observed for weight in which the relationship between ACL volume and the risk of an ACL injury was strengthened after adjusting for body weight in the models fitted to the female data and the combined male and female data.
The results of our study have several significant therapeutic implications. They provide a rationale for future clinical studies to determine if femoral notchplasty can reduce the risk of reinjuries and motivate studies that are designed to determine if we can use imaging studies to predict ACL injuries to the contralateral limb. In addition, the findings from this study can help to identify those at an increased risk for ACL injuries so that interventions such as neuromuscular control and strength training programs can be targeted to them. The findings from our study also serve as motivation for future studies to determine why family history of an ACL injury and joint geometry are associated with an increased risk of severe knee ligament injuries. If these are to be explored using a genome-wide association study to identify an underlying genetic mechanism that predisposes patients to suffering this injury, then the findings from our study would support focusing on markers that are associated with the development and formation of the ACL and femoral notch.
A potential limitation associated with this study was that the contralateral knee of the ACL-injured patients was measured, and these data were used as surrogate measures to represent the ACL-injured knee before the injury. This was evaluated by comparing the side-to-side differences of the measurements in control participants, and this revealed that there were no differences. Previous studies have also used the same approach and demonstrated side-to-side symmetry of knee morphometry.30
In summary, this study focused on the ACL and the structures that surround it and through multivariate analysis demonstrated that ACL volume, the size of the femoral intercondylar notch, and thickness of the bony ridge at the anteromedial outlet of the femoral notch are significant predictors of ACL injuries among female patients. Also, ACL volume and femoral notch width were associated with ACL injuries for male patients. Future studies should attempt to expand on multivariate models with other factors such as the tibial plateau shape and geometry of the meniscus, cartilage, and tibial spines.
Supplementary Material
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by National Institutes of Health grant R01AR05421 and Department of Energy grant SC 0001753.
Footnotes
For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav
REFERENCES
- 1.Al-Saeed O, Brown M, Athyal R, Sheikh M. Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):678–682. [DOI] [PubMed] [Google Scholar]
- 2.Alizadeh A, Kiavash V. Mean intercondylar notch width index in cases with and without anterior cruciate ligament tears. Iran J Radiol. 2008;5(4):205–208. [Google Scholar]
- 3.Anderson AF, Anderson CN, Gorman TM, Cross MB, Spindler KP. Radiographic measurements of the intercondylar notch: are they accurate? Arthroscopy. 2007;23(3):261–268, 268.e1–268.e2. [DOI] [PubMed] [Google Scholar]
- 4.Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29(1):58–66. [DOI] [PubMed] [Google Scholar]
- 5.Anderson AF, Lipscomb AB, Liudahl KJ, Addlestone RB. Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15(6):547–552. [DOI] [PubMed] [Google Scholar]
- 6.Beynnon BD, Hall J, Sturnick DR, et al. An increase of the posteriorinferior directed slope of the lateral tibial plateau subchondral bone is associated with an increased risk of suffering a non-contact ACL injury: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(5):1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandrashekar N, Slauterbeck J, Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med. 2005;33(10):1492–1498. [DOI] [PubMed] [Google Scholar]
- 8.Charlton WP, St John TA, Ciccotti MG, Harrison N, Schweitzer M. Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med. 2002;30(3):329–333. [DOI] [PubMed] [Google Scholar]
- 9.Davis TJ, Shelbourne KD, Klootwyk TE. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1999;7(4):209–214. [DOI] [PubMed] [Google Scholar]
- 10.Dienst M, Schneider G, Altmeyer K, et al. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127(4):253–260. [DOI] [PubMed] [Google Scholar]
- 11.Domzalski M, Grzelak P, Gabos P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop. 2010;34(5):703–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellaszlw M, Young SL, Woodbury MG, Fryday-Field K. Statisitical methodology for the concurrent assessment of interrater and intrarater reliability: using goniometric measurements as an example. Phys Ther. 1994;74:777–788. [DOI] [PubMed] [Google Scholar]
- 13.Everhart JS, Flanigan DC, Chaudhari AM. Anteromedial ridging of the femoral intercondylar notch: an anatomic study of 170 archival skeletal specimens. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):80–87. [DOI] [PubMed] [Google Scholar]
- 14.Everhart JS, Flanigan DC, Simon RA, Chaudhari AM. Association of noncontact anterior cruciate ligament injury with presence and thickness of a bony ridge on the anteromedial aspect of the femoral intercondylar notch. Am J Sports Med. 2010;38(8):1667–1673. [DOI] [PubMed] [Google Scholar]
- 15.Fung DT, Hendrix RW, Koh JL, Zhang LQ. ACL impingement prediction based on MRI scans of individual knees. Clin Orthop Relat Res. 2007;460:210–218. [DOI] [PubMed] [Google Scholar]
- 16.Goetschius J, Smith HC, Vacek PM, et al. Application of a clinic-based algorithm as a tool to identify female athletes at risk for anterior cruciate ligament injury: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2012;40(9):1978–1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gwinn DE, Wilckens JH, McDevitt ER, Ross G, Kao TC. The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28(1):98–102. [DOI] [PubMed] [Google Scholar]
- 18.Herzog RJ, Silliman JF, Hutton K, Rodkey WG, Steadman JR. Measurements of the intercondylar notch by plain film radiography and magnetic resonance imaging. Am J Sports Med. 1994;22(2):204–210. [DOI] [PubMed] [Google Scholar]
- 19.Hoteya K, Kato Y, Motojima S, et al. Association between intercondylar notch narrowing and bilateral anterior cruciate ligament injuries in athletes. Arch Orthop Trauma Surg. 2011;131(3):371–376. [DOI] [PubMed] [Google Scholar]
- 20.Houseworth SW, Mauro VJ, Mellon BA, Kieffer DA. The intercondylar notch in acute tears of the anterior cruciate ligament: a computer graphics study. Am J Sports Med. 1987;15(3):221–224. [DOI] [PubMed] [Google Scholar]
- 21.Ireland ML, Ballantyne BT, Little K, McClay IS. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):200–205. [DOI] [PubMed] [Google Scholar]
- 22.Kocher MS, Mandiga R, Klingele K, Bley L, Micheli LJ. Anterior cruciate ligament injury versus tibial spine fracture in the skeletally immature knee: a comparison of skeletal maturation and notch width index. J Pediatr Orthop. 2004;24(2):185–188. [PubMed] [Google Scholar]
- 23.LaPrade RF, Burnett QM 2nd. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1994;22(2):198–202, discussion 203. [DOI] [PubMed] [Google Scholar]
- 24.Lombardo S, Sethi PM, Starkey C. Intercondylar notch stenosis is not a risk factor for anterior cruciate ligament tears in professional male basketball players: an 11-year prospective study. Am J Sports Med. 2005;33(1):29–34. [DOI] [PubMed] [Google Scholar]
- 25.Lund-Hanssen H, Gannon J, Engebretsen L, Holen KJ, Anda S, Vat-ten L. Intercondylar notch width and the risk for anterior cruciate ligament rupture: a case-control study in 46 female handball players. Acta Orthop Scand. 1994;65(5):529–532. [DOI] [PubMed] [Google Scholar]
- 26.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 27.Schickendantz MS, Weiker GG. The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. Am J Sports Med. 1993;21(1):110–113. [DOI] [PubMed] [Google Scholar]
- 28.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears: a prospective study. Am J Sports Med. 1998;26(3):402–408. [DOI] [PubMed] [Google Scholar]
- 29.Shelbourne KD, Facibene WA, Hunt JJ. Radiographic and intraoperative intercondylar notch width measurements in men and women with unilateral and bilateral anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):229–233. [DOI] [PubMed] [Google Scholar]
- 30.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40(3):521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature. Part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Souryal TO. The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. Am J Sports Med. 1993;21(6):898. [DOI] [PubMed] [Google Scholar]
- 34.Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am J Sports Med. 1988;16(5):449–454. [DOI] [PubMed] [Google Scholar]
- 35.Spindler KP, Wright RW. Clinical practice: anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Staeubli HU, Adam O, Becker W, Burgkart R. Anterior cruciate ligament and intercondylar notch in the coronal oblique plane: anatomy complemented by magnetic resonance imaging in cruciate ligament-intact knees. Arthroscopy. 1999;15(4):349–359. [DOI] [PubMed] [Google Scholar]
- 37.van Diek FM, Wolf MR, Murawski CD, van Eck CF, Fu FH. Knee morphology and risk factors for developing an anterior cruciate ligament rupture: an MRI comparison between ACL-ruptured and noninjured knees. Knee Surg Sports Traumatol Arthrosc. 2014;22(5): 987–994. [DOI] [PubMed] [Google Scholar]
- 38.van Eck CF, Kopf S, van Dijk CN, Fu FH, Tashman S. Comparison of 3-dimensional notch volume between subjects with and subjects without anterior cruciate ligament rupture. Arthroscopy. 2011;27(9):1235–1241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


