Key Points
Question
How many children with medical needs are at risk of losing Medicaid and Children’s Health Insurance Program and Supplemental Nutrition Assistance Program because of the proposed public charge rule change?
Findings
This cross-sectional study found that 8.3 million children who are enrolled in Medicaid and Children’s Health Insurance Program or Supplemental Nutrition Assistance Program, of whom 5.5 million have specific medical need, are at risk of losing health and nutrition benefits. Between 0.8 and 1.9 million children with medical needs could be disenrolled from these benefits.
Meaning
The proposed public charge rule would likely cause millions of children to lose health and nutrition benefits, including many children with specific medical needs that, if left untreated, may contribute to child deaths and future disability.
Abstract
Importance
In October 2018, the Trump administration published a proposed rule change that would increase the chance of an immigrant being deemed a “public charge” and thereby denied legal permanent residency or entry to the United States. The proposed changes are expected to cause many immigrant parents to disenroll their families from safety-net programs, in large part because of fear and confusion about the rule, even among families to whom the rule does not technically apply.
Objective
To simulate the potential harms of the rule change by estimating the number, medical conditions, and care needs of children who are at risk of losing their current benefits, including Medicaid and Children’s Health Insurance Program (CHIP) and Supplemental Nutrition Assistance Program (SNAP).
Design, Setting, and Participants
A cross-sectional study used nationally representative data from 4007 children 17 years of age or younger who participated in the 2015 Medical Expenditure Panel Survey to assess their potential risk of losing benefits because they live with a noncitizen adult. Statistical analysis was conducted from January 3 to April 8, 2019.
Main Outcomes and Measures
The number of children at risk of losing benefits; the number of children with medical need, defined as having a potentially serious medical diagnosis; being disabled (or functionally limited); or having received any specific treatment in the past year. The numbers of children who would be disenrolled under likely disenrollment scenarios drawn from research on immigrants before and after the 1996 welfare reform were estimated.
Results
A total of 8.3 million children who are currently enrolled in Medicaid and CHIP or receiving SNAP benefits are potentially at risk of disenrollment, of whom 5.5 million have specific medical needs, including 615 842 children with asthma, 53 728 children with epilepsy, 3658 children with cancer, and 583 700 children with disabilities or functional limitations. Nonetheless, among the population potentially at risk of disenrollment, medical need was less common than among other children receiving Medicaid and CHIP or SNAP (64.5%; 95% CI, 61.5%-67.4%; vs 76.0%; 95% CI, 73.9%-78.4%; P < .001). The proposed rule is likely to cause parents to disenroll between 0.8 million and 1.9 million children with specific medical needs from health and nutrition benefits.
Conclusions and Relevance
The proposed public charge rule would likely cause millions of children to lose health and nutrition benefits, including many with specific medical needs that, if left untreated, may contribute to child deaths and future disability.
This cross-sectional study simulates the number, medical conditions, and care needs of children who are at risk of losing their current benefits, including Medicaid and Children’s Health Insurance Program and Supplemental Nutrition Assistance Program, after a proposed US federal rule change.
Introduction
When an immigrant applies for entry into the United States or for permanent resident status (ie, a Lawful Permanent Resident Card, commonly known as a “green card”), immigration officials decide if the immigrant is, or will become, a public charge (ie, someone likely to become dependent on public benefits). Such persons are denied permission to enter or reenter the country or become permanent residents. Under a longstanding policy, an immigrant who has used cash assistance or is institutionalized in a government-funded facility may be deemed to be a public charge. Previously, receipt of other government benefits was not considered in assessing an immigrant’s public charge status. In October 2018, the Trump administration published a proposed rule change that is a significant departure from the prior policy and increases the chance of an immigrant being denied legal permanent residency or entry to the United States.1
The proposed rule instructs immigration officials to consider a broadened array of public benefits—including (nonemergency) Medicaid, Supplemental Nutrition Assistance Program (SNAP), Medicare Part D low-income subsidies, and housing assistance such as Section 8 housing vouchers—along with other factors when making public charge determinations. In response to the proposed changes, many immigrant parents are expected to disenroll themselves and their children from safety-net benefits programs. Although no changes to the rule have taken effect thus far, reports indicate that disenrollment is already occurring.2,3,4 A major contributor to disenrollment is the so-called chilling effect: fear and confusion about the rule, even among immigrant families to which the rule does not technically apply.5
More than 260 000 public comments have been submitted to the Department of Homeland Security on the proposed rule.1 Under federal law, the Department of Homeland Security must review and respond to these comments prior to publishing the final rule. It is unclear how long this process will take or when the final rule will be published. If the final rule closely resembles the proposed rule, millions of children may be disenrolled from Medicaid and Children’s Health Insurance Program (CHIP).5 In addition, many children will face other new barriers to health care because family members are likely to disenroll from benefits such as housing assistance and SNAP.
We analyzed nationally representative data to assess the number of children who are at risk of losing health and nutrition benefits, and those children’s specific medical needs. We also present 3 disenrollment scenarios to illustrate how the rule changes could affect children.
Methods
Data Source
We analyzed the 2015 Medical Expenditure Panel Survey (MEPS), a national household survey administered by the Agency for Healthcare Research and Quality that provides information on health care needs, use, expenditures, and medical conditions. We linked the MEPS to the National Health Interview Survey (from which the MEPS sample is drawn) to determine citizenship and nativity of MEPS respondents. We then linked the MEPS household files with the MEPS medical conditions file to identify medical diagnoses. The MEPS inquires about lifetime (ever) diagnosis for select priority conditions (such as cancer, diabetes, asthma, and attention-deficit/hyperactivity disorder) and about current-year diagnosis for other conditions. The 2015 MEPS sample included 35 427 respondents, of whom 9615 were children 17 years of age or younger. The institutional review board at Cambridge Health Alliance designated this study exempt from review because it analyzed publicly available deidentified data.
Definitions
We considered children to be at risk of losing benefits if they lived with at least 1 noncitizen adult. We defined medical need as having a medical diagnosis or disability or receiving a specific treatment. Medical diagnoses included asthma; attention-deficit/hyperactivity disorder; influenza; respiratory conditions (other than asthma, influenza, allergic rhinitis, or viral upper respiratory tract infections); gastrointestinal conditions; ear infections; diabetes; musculoskeletal and rheumatologic conditions; epilepsy; mental health conditions; ear, nose, throat, mouth, and sensory conditions; cancer; congenital abnormalities or developmental disorders; and/or circulatory disorders. Potentially life-threatening illnesses were defined as influenza, diabetes, epilepsy, and cancer. Disability included functional limitation, walking with an assistive device, or disability due to a mental health condition (Columbia Impairment Scale score ≥15).6 In addition, we considered all newborns (who require immunizations and screenings) to have medical need, as well as children of any ages who were prescribed medications; received therapy (physical, occupational, or speech) or counseling; were pregnant; saw a specialist; had any illness, injury, or condition “that required care right away”; and/or required any care, test, or treatment.
We defined children receiving benefits as those who were insured by Medicaid and CHIP or resided in a household reporting receipt of SNAP for 1 or more household members. We included CHIP beneficiaries because many states use blended funding for Medicaid and CHIP, and enrollees may not know which program is funding their health coverage. We included estimates for all children enrolled in Medicaid and CHIP (regardless of family SNAP enrollment) (eTable 1 and 2 in the Supplement).
Statistical Analysis
Statistical analysis was conducted from January 3 to April 8, 2019. We used χ2 tests to compare the difference between children at risk of benefit loss and those not at risk. All analyses used person-level weights supplied by the Agency for Healthcare Research and Quality that allow extrapolation to national estimates, and appropriate procedures to account for the complex sampling design. P < .05 was considered significant.
Disenrollment Estimates
For estimates of potential changes in coverage owing to public charge policies, as others have done,5,7 we modeled several scenarios using different disenrollment rates. We drew on previous research on the chilling effect of the 1996 welfare reform, which included changes to Medicaid eligibility based on immigration status.8,9 These scenarios illustrate the likely outcome if the draft proposed rule were to take effect. Our principal estimate assumes a 25% disenrollment rate among at-risk children, based on a study that included children who remained technically eligible for benefits after the welfare reform changes.9 Given the uncertainty about the actual outcome, we also examined the outcome if the disenrollment rate was 10 percentage points lower or higher (ie, 15% or 35%).
Results
A total of 8.3 million children are at risk of losing Medicaid and CHIP and/or household nutrition assistance, of whom 5.5 million had specific medical needs (Table 1). Children at risk of losing benefits were less likely to have medical need than other children receiving benefits (64.5%; 95% CI, 61.5%-67.4%; vs 76.0%; 95% CI, 73.9%-78.4%; P < .001).
Table 1. Demographic Characteristics of Children With Medical Need at Risk of Losing Current Medicaid and CHIP and/or SNAP Benefits Because of Proposed Public Charge Rule Change.
| Characteristic | Children at Risk (n = 1338) | Children Not at Risk (n = 2669) | P Value | ||||
|---|---|---|---|---|---|---|---|
| Unweighted, No. | Weighted, No. | Weighted, % (95% CI) | Unweighted, No. | Weighted, No. | Weighted, % (95% CI) | ||
| Total children receiving benefits | 2118 | 8 319 236 | 25.1 (21.7-28.6) | 3553 | 24 791 754 | 74.9 (73.8-78.2) | NA |
| Children with medical need receiving benefits | 1338 | 5 459 910 | 64.5 (61.5-67.4) | 2669 | 19 639 492 | 76.0 (73.9-78.4) | <.001 |
| Age, y | |||||||
| 0-5 | 493 | 2 251 070 | 41.2 (37.4-45.1) | 901 | 7 163 855 | 36.5 (33.7-39.2) | .07 |
| 6-12 | 552 | 2 044 533 | 37.4 (34.1-40.8) | 1101 | 7 637 381 | 38.9 (36.6-41.2) | |
| 13-17 | 293 | 1 164 306 | 21.3 (18.5-24.1) | 667 | 4 838 256 | 24.6 (22.0-27.2) | |
| Sex | |||||||
| Male | 726 | 2 958 078 | 54.2 (50.2-58.2) | 1418 | 10 034 636 | 51.1 (48.6-53.6) | .22 |
| Female | 612 | 2 501 831 | 45.8 (41.8-49.8) | 1251 | 9 604 856 | 48.9 (46.4-51.4) | |
| Income (% FPL) | |||||||
| 0-249 | 1247 | 4 824 768 | 88.4 (85.3-91.4) | 2356 | 16 083 244 | 81.5 (78.7-85.1) | .01 |
| 250-399 | 62 | 404 855 | 7.4 (5.1-9.7) | 231 | 2 237 462 | 11.4 (9.0-13.8) | |
| ≥400 | 29 | 230 286 | 4.2 (2.2-6.3) | 82 | 1 318 787 | 6.7 (4.6-8.9) | |
| Race/ethnicity | |||||||
| Hispanic | 1140 | 4 354 899 | 79.8 (74.4-85.1) | 819 | 3 901 136 | 19.9 (16.8-22.9) | <.001 |
| White non-Hispanic | 42 | 256 842 | 4.7 (1.8-7.6) | 687 | 8 836 487 | 45.0 (40.6-49.3) | |
| Black, non-Hispanic | 66 | 398 730 | 7.3 (3.8-10.8) | 919 | 4 641 910 | 23.6 (20.1-27.2) | |
| Asian | 75 | 367 692 | 6.7 (4.1-9.3) | 42 | 276 902 | 1.4 (0.7-2.2) | |
| Other | 15 | 81 747 | 1.5 (0.3-2.7) | 202 | 1 983 057 | 10.1 (6.7-13.5) | |
| Immigration statusa | |||||||
| Citizen | 1067 | 4 060 354 | 91.3 (88.4-94.1) | 2176 | 15 357 858 | 99.9 (99.9-100.0) | <.001 |
| Noncitizen | 72 | 387 471 | 8.1 (5.3-10.9) | 2 | 7956 | 0.05 (0.0-0.14) | |
Abbreviations: CHIP, Children’s Health Insurance Program; FPL, federal poverty level; NA, not applicable; SNAP, Supplemental Nutrition Assistance Program.
Among children in the study sample for whom we could attain citizenship information.
Most at-risk children with medical need were US citizens (91.3%; 95% CI, 88.4%-94.1%), while all other children receiving benefits were US citizens (99.9%; 95% CI, 99.9%-100.0%; P < .001) (Table 1). Compared with other children with medical need who received health or nutrition benefits, those at risk of losing benefits were more likely to be Hispanic (79.8%; 95% CI, 74.4%-85.1%; vs 19.9%; 95% CI, 16.8%-22.9%; P < .001) and to have family incomes less than 250% of the federal poverty level (88.4%; 95% CI, 85.3%-91.4%; vs 81.5%; 95% CI, 78.7%-85.1%; P = .01).
Medical Conditions and Specific Medical Care Needs of Children at Risk of Losing Benefits
Children at risk of losing benefits included 1.3 million with at least 1 potentially life-threatening condition (including 676 284 with influenza; 615 842 with asthma; and 53 728 with epilepsy) (Table 2). In addition, the at-risk group included 618 302 newborns (all of whom need evaluation and immunizations), 1.1 million children who saw specialists, and 946 272 who were prescribed medications. Children at risk of losing benefits who needed medical care were less likely than other children receiving benefits to be disabled (10.7%; 95% CI, 8.7%-12.7%; vs 21.1%; 95% CI, 18.6%-23.6%; P < .001).
Table 2. Medical Conditions and Care Needs of Children With Medical Need at Risk of Losing Medicaid and CHIP and/or SNAP Benefits Because of Proposed Public Charge Rules.
| Characteristic | Children at Risk (n = 1338) | Children Not at Risk (n = 2669) | P Value | ||||
|---|---|---|---|---|---|---|---|
| Unweighted, No. | Weighted, No. | Weighted, % (95% CI) | Unweighted, No. | Weighted, No. | Weighted, % (95% CI) | ||
| Total children with medical need | 1338 | 5 459 910 | 64.6 (61.6-67.6) | 2669 | 19 639 492 | 76.1 (73.9-78.4) | <.001 |
| Received a diagnosis of a medical condition | 1015 | 4 210 990 | 77.1 (74.0-80.3) | 2099 | 15 580 094 | 79.3 (77.4-81.3) | .22 |
| Asthmaa | 156 | 615 842 | 11.3 (9.0-13.5) | 630 | 3 649 827 | 18.6 (16.4-20.8) | <.001 |
| Attention-deficit/hyperactivity disorder | 79 | 316 742 | 6.1 (4.4-7.8) | 475 | 3 649 437 | 19.5 (17.5-21.5) | <.001 |
| Other respiratory conditionb | 372 | 1 527 559 | 32.1 (27.5-36.8) | 577 | 4 702 131 | 27.3 (24.1-30.4) | .08 |
| Influenzaa | 156 | 676 284 | 14.2 (10.6-17.9) | 216 | 1 680 507 | 9.7 (7.6-11.9) | .03 |
| Gastrointestinal | 192 | 861 032 | 18.1 (15.0-22.0) | 374 | 3 133 796 | 18.2 (15.2-21.1) | .98 |
| Ear infection | 128 | 582 300 | 12.3 (9.1-15.4) | 277 | 2 469 257 | 14.3 (11.7-17.0) | .36 |
| Musculoskeletal and rheumatologic | 113 | 436 838 | 9.2 (7.4-11.0) | 239 | 1 875 581 | 10.9 (9.4-12.3) | .19 |
| Epilepsya | 13 | 53 728 | 1.1 (0.5-1.8) | 31 | 227 936 | 1.3 (0.7-1.9) | .68 |
| Mental health | 18 | 79 791 | 1.7 (0.6-2.8) | 101 | 845 757 | 4.9 (3.6-6.2) | .001 |
| Ear, nose, throat, mouth, and sensory | 210 | 845 990 | 17.8 (14.3-21.3) | 376 | 3 026 506 | 17.5 (15.3-19.8) | .90 |
| Congenital abnormality or developmental disorder | 39 | 141 670 | 3.0 (2.0-4.0) | 73 | 633 483 | 3.7 (2.5-4.6) | .38 |
| Genitourinary | 34 | 161 915 | 3.4 (2.0-4.8) | 58 | 467 888 | 2.7 (2.0-3.4) | .33 |
| Circulatory disorder | 18 | 61 414 | 1.3 (0.6-2.0) | 42 | 314 332 | 1.8 (1.1-2.5) | .30 |
| Other | 53 | 216 515 | 4.6 (2.8-6.3) | 140 | 1 078 385 | 6.3 (4.9-7.6) | .13 |
| Disabled | 583 700 | 10.7 (8.7-12.7) | 4 147 036 | 21.1 (18.6-23.6) | <.001 | ||
| Functionally impaired, including walking limitations or using assistive device | 69 | 321 666 | 6.1 (4.4-7.8) | 283 | 2 088 850 | 10.9 (8.9-13.0) | <.001 |
| Disabled due to mental health condition | 90 | 347 302 | 10.2 (7.8-12.7) | 358 | 2 802 084 | 21.4 (18.7-24.0) | <.001 |
| Needed specific treatment | 893 | 3 711 854 | 68.0 (64.2-71.7) | 2011 | 15 512 498 | 80.0 (76.7-81.3) | <.001 |
| All newborns | 122 | 618 302 | 11.3 (9.0-13.7) | 225 | 1 887 868 | 9.6 (8.1-11.2) | .20 |
| Needed care for illness or injury | 399 | 1 791 142 | 40.0 (35.4-44.6) | 1064 | 9 010 125 | 53.7 (49.6-57.9) | <.001 |
| Any care, test, or treatment | 340 | 1 337 519 | 25.2 (22.1-28.3) | 783 | 6 147 204 | 32.0 (29.3-34.7) | .001 |
| Specialist | 258 | 1 120 273 | 21.1 (18.2-24.1) | 573 | 4 636 462 | 24.2 (21.4-27.0) | .13 |
| Prescribed medication | 223 | 946 272 | 17.8 (14.8-20.9) | 797 | 5 984 076 | 31.3 (28.7-33.8) | <.001 |
| Therapy (physical, speech, or occupational) | 129 | 554 294 | 10.5 (8.2-12.7) | 352 | 2 622 838 | 13.7 (11.9-15.4) | .03 |
| Counseling | 98 | 402 916 | 7.6 (5.4-9.8) | 405 | 3 093 847 | 16.1 (14.0-18.2) | <.001 |
Abbreviations: CHIP, Children’s Health Insurance Program; SNAP, Supplemental Nutrition Assistance Program.
Asthma, influenza, epilepsy, cancer, and diabetes are considered life-threatening conditions.
Excluding allergic rhinitis, viral upper respiratory tract infections, and influenza.
Estimates of Number Likely to Disenroll Under Disenrollment Scenarios
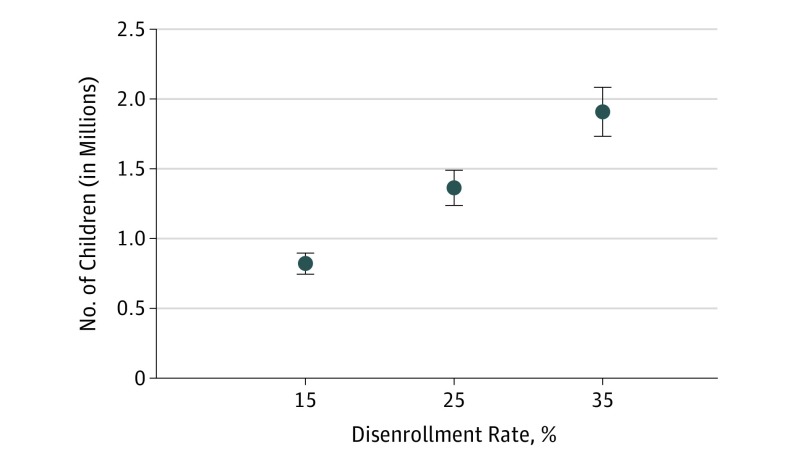
A total of 1.4 million children would be disenrolled from Medicaid and CHIP and/or family benefits if 25% of at-risk individuals disenroll from benefits (Figure). In the sensitivity analysis assuming a disenrollment rate of 15%, 0.8 million children with medical needs would be disenrolled from benefits; assuming a disenrollment rate of 35%, 1.9 million children with medical needs would be disenrolled from benefits.
Figure. Estimates of Children With Medical Need Who Would Lose Current Benefits Under Disenrollment Scenarios as a Result of the Proposed Public Charge Rule.
Error bars indicate 95% CIs.
Discussion
In this study, we estimate projected harms if the proposed public charge rules were to be implemented. Consistent with prior research,10 we estimate that millions of children in need of medical care are at risk of losing benefits owing to the proposed changes to the public charge rules.
These losses would likely contribute to child deaths and future disability. Parents will face difficult choices on whether to remain enrolled in vital benefits, or risk being denied a green card, reentry into the United States, or the ability to sponsor other family members seeking to immigrate to the United States. Denial of green-card status for parents could lead to family separation or relocation of children (most of whom are US citizens) to their parents’ country of origin, where adequate medical care may not be available. If parents disenroll from SNAP or housing assistance, their children’s risk of food insecurity, malnutrition, poverty, and homelessness is likely to rise, which may well increase health care costs in the long run, and reduce self-sufficiency in adulthood.11,12,13,14,15 Although the loss of benefits is harmful to all children, it seems likely to be particularly deleterious for children with specific medical needs.
Limitations
Our study has several limitations. We were unable to estimate the number of children in households receiving housing assistance or Medicare part D low-income subsidies, and hence underestimate the population at risk. We considered only children who live with noncitizen adults to be at risk of losing coverage. Because of widespread fear and confusion, some immigrant families in which all members are citizens might also disenroll from benefits.16 Similarly, our estimates of the number who may disenroll are based on scenarios from welfare reform that denied federal benefits to some immigrants but did not impose specific sanctions; because the proposed public charge rule explicitly threatens families’ immigration status, disenrollment rates might be higher than we estimate.
Conclusions
Most children who lose Medicaid and CHIP become uninsured.5 Without coverage, they are likely to forego or delay needed care,17 and some, such as children with epilepsy18,19 or asthma,20 as well as newborns who require immunizations,21,22,23 are likely to incur higher long-term health care costs. In addition, undertreatment of illness increases school absenteeism and parental work absence, which, in the case of asthma, led to a loss of parental productivity of $719.1 million in 1996 alone.20
However, our main concerns are not economic but ethical. We believe that denial of needed health care and nutrition to anyone, but particularly to children, violates human rights.24 We call on the medical community to speak out against this unjust and unethical proposal to change the public charge rule.
eTable 1. Demographic Characteristics of Children With “Medical Need” at Risk of Losing Medicaid/CHIP Benefits Due to Proposed Public Charge Rules
eTable 2. Medical Conditions and Care Needs of Children With “Medical Need” at Risk of Losing Medicaid/CHIP
References
- 1.Department of Homeland Security Proposed rule: Inadmissibility on Public Charge Grounds. CIS No. 2499–10; DHS Docket No. USCIS–2010–0012. Federal Register https://www.federalregister.gov/documents/2018/10/10/2018-21106/inadmissibility-on-public-charge-grounds. Published October 10, 2018. Accessed May 22, 2019.
- 2.Lopez A. Fear of deportation or green card denial deters some parents from getting kids care. https://www.npr.org/sections/health-shots/2019/01/26/686325494/fear-of-deportation-or-green-card-denial-deters-some-parents-from-getting-kids-c. Published January 26, 2019. Accessed January 31, 2019.
- 3.Evich HB. Immigrants, fearing Trump crackdown, drop out of nutrition programs. https://www.politico.com/story/2018/09/03/immigrants-nutrition-food-trump-crackdown-806292. Updated September 4, 2018. Accessed January 31, 2019.
- 4.Blitzer J. Trump’s public-charge rule is a one-two punch against immigrants and public assistance. The New Yorker https://www.newyorker.com/news/dispatch/trumps-public-charge-rule-is-a-one-two-punch-against-immigrants-and-public-assistance. Published September 28, 2018. Accessed January 31, 2019.
- 5.Artiga S, Damico A, Garfield R; Henry J. Kaiser Family Foundation. Potential effects of public charge changes on health coverage for citizen children. http://files.kff.org/attachment/Issue-Brief-Potential-Effects-of-Public-Charge-Changes-on-Health-Coverage-for-Citizen-Children. Published May 2018. Accessed January 31, 2019.
- 6.Bird HR, Andrews H, Schwab-Stone M, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. Int J Methods Psychiatr Res. 1996;6(4):-. doi: [DOI] [Google Scholar]
- 7.Ponce N, Lucia L, Shimada T; UCLA Center for Health Policy Research. How proposed changes to the ‘public charge’ rule will affect health, hunger and the economy in California. http://healthpolicy.ucla.edu/newsroom/Documents/2018/public-charge-seminar-slides-nov2018.pdf. Updated November 29, 2018. Accessed April 9, 2019.
- 8.Kandula NR, Grogan CM, Rathouz PJ, Lauderdale DS. The unintended impact of welfare reform on the Medicaid enrollment of eligible immigrants. Health Serv Res. 2004;39(5):1509-1526. doi: 10.1111/j.1475-6773.2004.00301.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaushal N, Kaestner R. Welfare reform and health insurance of immigrants. Health Serv Res. 2005;40(3):697-721. doi: 10.1111/j.1475-6773.2005.00381.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zallman L, Finnegan KE, Himmelstein D, Woolhandler S; California Health Care Foundation. Changing public charge immigration rules: the potential impact on children who need care. https://www.chcf.org/wp-content/uploads/2018/10/ChangingPublicChargeImmigrationRules.pdf. Published October 2018. Accessed January 31, 2019.
- 11.Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental Nutrition Assistance Program (SNAP) participation and health care expenditures among low-income adults. JAMA Intern Med. 2017;177(11):1642-1649. doi: 10.1001/jamainternmed.2017.4841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Food and Nutrition Service, US Department of Agriculture The savings in Medicaid costs for newborns and their mothers from prenatal participation in the WIC program. https://www.fns.usda.gov/wic/savings-medicaid-costs-newborns-and-their-mothers-resulting-prenatal-participation-wic-program. Accessed January 31, 2019.
- 13.Poblacion A, Bovell-Ammon A, Sheward R, et al. Stable homes make healthy families. Children’s HealthWatch What If? series. http://childrenshealthwatch.org/wp-content/uploads/CHW-Stable-Homes-2-pager-web.pdf. Published July 2017. Accessed January 31, 2019.
- 14.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65-72. doi: 10.1542/peds.2006-3717 [DOI] [PubMed] [Google Scholar]
- 15.Sonik RA. Massachusetts inpatient Medicaid cost response to increased Supplemental Nutrition Assistance Program benefits. Am J Public Health. 2016;106(3):443-448. doi: 10.2105/AJPH.2015.302990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Batalova J, Fix M, Greenberg M Chilling effects: the expected public charge rule and its impact on legal immigrant families' public benefits use. Migration Policy Institute website. https://www.migrationpolicy.org/research/chilling-effects-expected-public-charge-rule-impact-legal-immigrant-families. Accessed January 31, 2019.
- 17.Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027-1037. doi: 10.1542/peds.2012-0668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kortland LM, Knake S, Rosenow F, Strzelczyk A. Cost of status epilepticus: a systematic review. Seizure. 2015;24:17-20. doi: 10.1016/j.seizure.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 19.Hillman J, Lehtimäki K, Peltola J, Liimatainen S. Clinical significance of treatment delay in status epilepticus. Int J Emerg Med. 2013;6(1):6. doi: 10.1186/1865-1380-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang LY, Zhong Y, Wheeler L. Direct and indirect costs of asthma in school-age children. Prev Chronic Dis. 2005;2(1):A11. [PMC free article] [PubMed] [Google Scholar]
- 21.Bolin K, Forsgren L. The cost effectiveness of newer epilepsy treatments: a review of the literature on partial-onset seizures. Pharmacoeconomics. 2012;30(10):903-923. doi: 10.2165/11597110-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 22.Sullivan SD, Weiss KB, Lynn H, et al. ; National Cooperative Inner-City Asthma Study (NCICAS) Investigators . The cost-effectiveness of an inner-city asthma intervention for children. J Allergy Clin Immunol. 2002;110(4):576-581. doi: 10.1067/mai.2002.128009 [DOI] [PubMed] [Google Scholar]
- 23.Whitney CG, Zhou F, Singleton J, Schuchat A; Centers for Disease Control and Prevention (CDC) . Benefits from immunization during the vaccines for children program era—United States, 1994-2013. MMWR Morb Mortal Wkly Rep. 2014;63(16):352-355. [PMC free article] [PubMed] [Google Scholar]
- 24.De Schutter O. Report of the Special Rapporteur on the right to food. https://www.ohchr.org/EN/HRBodies/HRC/RegularSessions/Session25/Documents/A_HRC_25_57_ENG.DOC. Published January 24, 2014. Accessed April 4, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Demographic Characteristics of Children With “Medical Need” at Risk of Losing Medicaid/CHIP Benefits Due to Proposed Public Charge Rules
eTable 2. Medical Conditions and Care Needs of Children With “Medical Need” at Risk of Losing Medicaid/CHIP