Key Points
Question
Are the obstruction patterns during drug-induced sleep endoscopy similar to those found during natural sleep endoscopy?
Findings
In this cohort study of 26 patients with snoring or obstructive sleep apnea, the upper-airway obstruction patterns showed a good agreement rate between drug-induced sleep endoscopy (performed with sedative drugs) and natural sleep endoscopy.
Meaning
Findings for drug-induced sleep endoscopy were similar to those for natural sleep endoscopy, suggesting that drug-induced sleep endoscopy may be a reliable test.
Abstract
Importance
Drug-induced sleep endoscopy (DISE) has been suggested to be a valuable technique for identifying the obstruction site associated with sleep-disordered breathing. However, the reliability of DISE findings is controversial because the procedure uses sedative drugs, which may have implications for the obstruction patterns observed on DISE.
Objective
To compare the obstruction patterns during DISE with the obstruction patterns during natural sleep endoscopy (NSE).
Design, Setting, and Participants
This prospective cohort study was conducted between June 2013 and May 2018 in Kyungpook National University Chilgok Hospital in Daegu, South Korea. All analysis took place from June 1 to July 31, 2018. Participants had an obstructive sleep apnea diagnosis, were older than 18 years, and had an apnea hypopnea index higher than 5 on type I polysomnography. The patients initially enrolled were excluded from the study for not reaching adequate sleep depth and waking up during insertion of the nasopharyngoscope.
Intervention
Patients underwent DISE using midazolam and NSE without sedatives on 2 different days.
Main Outcomes and Measures
Obstruction findings were observed only in the same range (65-75) of the bispectral index on both days. Obstruction findings were classified according to the VOTE (velum, oropharynx lateral wall, tongue base, and epiglottis) classification. The extent of agreement between DISE and NSE findings was evaluated using Cohen weighted κ value.
Results
The study included 26 patients with snoring or obstructive sleep apnea (mean [SD] age, 44.7 [10.3] years; predominantly male [22 (85%)]). The mean (SD) apnea hypopnea index was 41.9 (17.2) and the lowest mean (SD) oxygen saturation was 79.8% (12.2%). The degree of agreement in upper-airway obstruction between DISE and NSE was 76.9% (Cohen weighted κ = 0.42; 95% CI, 0.02-0.83) in the velum, 88.5% (Cohen weighted κ = 0.84; 95% CI, 0.67-1.01) in the oropharynx lateral wall, 69.2% (Cohen weighted κ = 0.66; 95% CI, 0.46-0.86) in the tongue base, and 92.3% (Cohen weighted κ = 0.67; 95% CI, 0.24-1.11) in the epiglottis. Agreement of configuration of the velum was 88.5% (Cohen weighted κ = 0.50; 95% CI, −0.03 to 1.03) and the epiglottis was 92.3% (Cohen weighted κ = 0.67; 95% CI, 0.24-1.11).
Conclusions and Relevance
Obstruction patterns of the upper airway appeared to be in agreement between DISE and NSE, suggesting that DISE may be a reliable test; future studies of multiple positions and sleep stages with larger sample sizes may confirm these results.
This cohort study evaluates findings from drug-induced vs natural sleep tests for adults with sleep-disordered breathing, including degrees and types of upper-airway collapse.
Introduction
Use of drug-induced sleep endoscopy (DISE) for the evaluation of the upper airway has increased in patients with snoring or obstructive sleep apnea (OSA).1,2 This evaluation in awake patients may be insufficient for examining upper-airway collapse during sleep.3 Because DISE is performed while the patient is asleep, it is potentially a more reliable method compared with examinations while the patient is awake, such as cephalometry, Muller maneuver, computed tomography, magnetic resonance imaging, and tonsil or palatal grading.
Borowiecki et al4 introduced sleep endoscopy during natural sleep without the use of sedative drugs in 1978; however, it was not feasible in routine practice. In 1991, Croft and Pringle5 reported airway assessments of sedated patients with OSA, and since then, DISE, which can be performed routinely, has become more popular and widely used for evaluating upper-airway obstruction.6 However, some controversy surrounds the type and dose of sedative drug,7,8,9,10 the best classification to describe the findings,11 the interrater and intrarater reliability of DISE findings,12,13 and the differences in obstruction patterns between drug-induced sleep and natural sleep.14,15 Many previous studies have attempted to address the controversies associated with the choice of sedative drug (midazolam vs propofol vs midazolam plus propofol),9,10,16 the best classification system for the findings (NOHL classification [nose, oropharynx, hypopharynx, and larynx] or VOTE [velum, oropharynx, tongue base, and epiglottis] classification),11 and the interrater and intrarater reliability of DISE findings.12,13 However, to our knowledge, thus far no study has investigated the reliability of DISE findings in terms of their agreement with natural sleep endoscopy (NSE) findings. Therefore, in this study, we compared the obstruction patterns observed during DISE with those observed during NSE in patients with OSA.
Methods
Between June 2013 and May 2018, patients with an OSA diagnosis were prospectively included in this study conducted in Kyungpook National University Chilgok Hospital in Daegu, South Korea. The inclusion criteria were as follows: (1) older than 18 years, (2) apnea-hypopnea index (AHI) higher than 5 on type I polysomnography, and (3) consent to participate in the study. Polysomnographic parameters were defined by the American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events, as follows: apnea as 90% or greater drop in respiratory flow for 10 seconds or more, and hypopnea as 30% or greater drop in respiratory flow for 10 seconds or more with 3% or greater oxygen desaturation or arousal. Patients whose general condition was a contraindication of the use of midazolam were excluded. The study protocol was approved by the Kyungpook National University Chilgok Hospital Institutional Review Board. Written informed consent was obtained from all participants.
Participants underwent 2 separate sleep endoscopy examinations on different days (ie, DISE with midazolam, and NSE without sedatives). Obstruction findings were observed only in the same range (65-75) of the bispectral index on both days.
NSE and DISE Procedures
Natural sleep endoscopy was performed in the hospital room at night by an experienced otolaryngologist (S.J.H.). The nasal mucosa was topically anesthetized and shrunk with gauze soaked in 4% lidocaine and 0.1% epinephrine just before the patient went to sleep. Bispectral index was used to monitor the depth of sleep. The examination was started at the onset of snoring or apnea and performed for 20 minutes (if possible). A nasopharyngoscope (VNL1130; KayPENTAX Inc) was inserted through the wider nasal cavity at the onset of sleep-disordered breathing. For a direct comparison with DISE, obstruction findings were examined only when patients were in the supine position.
Drug-induced sleep endoscopy was performed in the outpatient clinic by the same otolaryngologist who performed the NSE. The nasal mucosa was topically anesthetized and shrunk with gauze soaked with 4% lidocaine and 0.1% epinephrine. After sufficient nasal anesthesia level had been reached, the patient was placed in the supine position and peripheral oxygen saturation was monitored using a pulse oximeter. Bispectral index was used to monitor the depth of sleep. Midazolam at a dose of 0.05 mg/kg was administered intravenously to induce sleep, and the depth of sleep was maintained in the same range as during the NSE. When the depth-of-sleep target was not achieved, 1 mg of midazolam was added every 5 minutes. Up to 9 mg of additional midazolam was administered under careful monitoring. A nasopharyngoscope was inserted through the wider nasal cavity at the onset of sleep-disordered breathing.
The degrees and types of upper-airway collapse at each site during both natural sleep and drug-induced sleep were assessed using the VOTE classification.17 The obstruction sites of the upper airway in the VOTE classification are as follows: velum (V), oropharynx lateral walls (O), tongue base (T), and epiglottis (E). The degree of obstruction is graded as follows: 0 (no obstruction—no vibration), 1 (partial obstruction—vibration), 2 (complete obstruction—collapse), and X (not visualized). The type of collapse is classified as anteroposterior, lateral, or concentric in the velum, although the type of collapse can show only a lateral pattern in the oropharynx lateral wall and only the anteroposterior pattern at the tongue base. The pattern in the epiglottis can be classified as anteroposterior or lateral.11
To assess the reliability of DISE findings, we compared the grades of upper-airway obstruction for the velum, oropharynx lateral wall, tongue base, and epiglottis of DISE with those of NSE. The patterns of upper-airway obstruction in the velum and epiglottis of both DISE and NSE were also compared. Because some otolaryngologists consider sites of obstruction grades 1 and 2 as a treatment target, we compared sites requiring treatment (obstruction grades 1 and 2) with those not requiring treatment (obstruction grade 0). In addition, because some otolaryngologists consider only sites of obstruction grade 2 as a treatment target, we compared sites requiring treatment (obstruction grade 2) with those not requiring treatment (obstruction grades 0 and 1).
Statistical Analysis
Statistical analyses were performed with MedCalc, version 12.7.4 (MedCalc Software). Continuous variables were presented as the mean with SD. Fisher exact test and an unpaired, 2-tailed t test were used to compare differences in sex, age, body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), and AHI between included and excluded patients. Two-sided P < .05 was considered statistically significant. To evaluate the agreement between DISE and NSE findings of upper-airway obstruction, we used Cohen weighted κ according to the following rating scheme: less than 0.20, poor agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, good agreement; and greater than 0.81, very good agreement.
Results
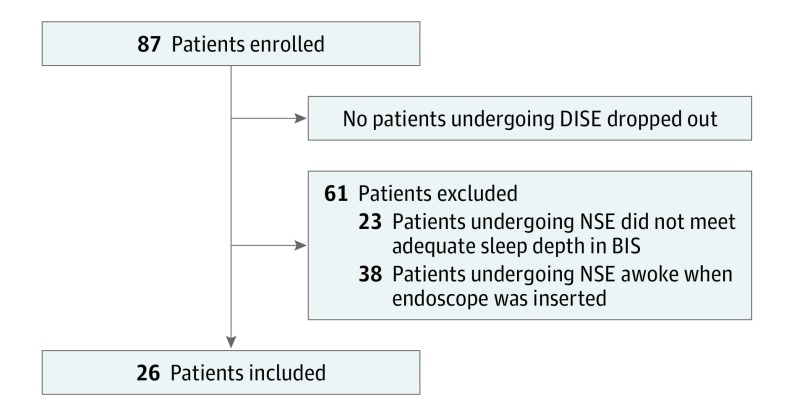
A total of 87 patients were enrolled in this study. Of these, 61 patients (70%) were excluded: 23 did not achieve adequate depth of sleep and 38 woke up during insertion of the nasopharyngoscope (Figure). The final sample comprised 26 patients with snoring or OSA, with a mean (SD) age of 44.7 (10.3) years and who were predominantly male (22 [85%]).
Figure. Flowchart of the Study Protocol.
BIS indicates bispectral index; DISE, drug-induced sleep endoscopy; and NSE, natural sleep endoscopy.
The mean (SD) BMI was 26.8 (4.4), and the mean (SD) AHI was 41.9 (17.2). The mean (SD) AHI during rapid-eye movement sleep was 44.6 (15.4) and non-rapid eye movement sleep was 41.3 (18.7). The lowest mean (SD) oxygen saturation was 79.8% (12.2%), and the mean (SD) duration of oxygen saturation below 90% was 34.3 (46.2) minutes. The mean (SD) Epworth Sleepiness Scale score was 8.9 (4.6). The mean (SD) Friedman tonsil grade was 1.4 (0.8), palatal or tongue position was 2.7 (0.5), and stage was 2.6 (0.7) (Table 1). A statistically significant difference was found in the mean (SD) examination duration between DISE and NSE (22.4 [2.4] minutes vs 3.5 [2.1] minutes; P < .001). No statistically significant differences between included and excluded patients were observed in sex (male and female: 22 and 4 vs 54 and 7; P = .73), mean (SD) age (44.7 [10.3] years vs 43.1 [11.2] years; P = .79), mean (SD) BMI (26.8 [4.4] vs 27.1 [4.0] ; P = .51), and mean (SD) AHI (41.9 [17.2] vs 39.2 [16.4]; P = .53).
Table 1. Characteristics of Study Participants.
| Variable | Mean (SD) [Range] |
|---|---|
| Sex, No. (%) | |
| Male | 22 (85) |
| Female | 4 (15) |
| Age, y | 44.7 (10.3) [26-63] |
| BMI | 26.8 (4.4) [20.7-36.7] |
| AHI, events/h | 41.9 (17.2) [15.2-78.1] |
| REM-AHI, events/h | 44.6 (15.4) [9.5-73.2] |
| NREM-AHI, events/h | 41.3 (18.7) [11.4-81.3] |
| Nadir of SpO2, % | 79.8 (12.2) [41.0-95.0] |
| Duration of SpO2 < 90%, min | 34.3 (46.2) [0-160.1] |
| ESS score | 8.9 (4.6) [3-18] |
| Friedman tonsil grade | 1.4 (0.8) [0-3] |
| Friedman palatal or tongue position | 2.7 (0.5) [1-3] |
| Friedman stage | 2.6 (0.7) [1-3] |
Abbreviations: AHI, apnea-hypopnea index; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ESS, Epworth Sleepiness Scale; NREM-AHI, AHI during non-rapid eye movement; REM-AHI, AHI during rapid-eye movement; SpO2, peripheral capillary oxygen saturation.
Agreement Between DISE and NSE Findings
A comparison of the grade of upper-airway obstruction between DISE and NSE is shown in Table 2. The degree of obstruction was slightly higher during DISE than during NSE at all obstruction sites. The grades of airway obstruction for the velum and tongue base showed relatively lower agreement (76.9% and 69.2%) and Cohen weighted κ values (0.42 [95% CI, 0.02-0.83] and 0.66 [95% CI, 0.46-0.86]) compared with those for the oropharynx lateral wall (88.5%; Cohen weighted κ = 0.84 [95% CI, 0.67-1.01]) and epiglottis (92.3%; Cohen weighted κ = 0.67 [95% CI, 0.24-1.11]).
Table 2. Comparison of Upper-Airway Obstruction Grade Between Drug-Induced Sleep Endoscopy and Natural Sleep Endoscopy.
| Obstruction Site | Grade | Agreement, % | Cohen Weighted κ (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| DISE | NSE | |||||||
| 0 | 1 | 2 | 0 | 1 | 2 | |||
| Velum | 0 | 3 | 23 | 2 | 5 | 19 | 76.9 | 0.42 (0.02-0.83) |
| Oropharynx lateral wall | 16 | 6 | 4 | 19 | 3 | 4 | 88.5 | 0.84 (0.67-1.01) |
| Tongue base | 11 | 7 | 8 | 15 | 6 | 5 | 69.2 | 0.66 (0.46-0.86) |
| Epiglottis | 21 | 1 | 4 | 23 | 1 | 2 | 92.3 | 0.67 (0.24-1.11) |
Abbreviations: DISE, drug-induced sleep endoscopy; NSE, natural sleep endoscopy.
Circular obstruction in the velum was observed more frequently during DISE than during NSE, but the agreement was very high (88.5%; Cohen weighted κ = 0.50; 95% CI, −0.03 to 1.03) (Table 3). The findings for the epiglottis also showed high agreement (92.3%) and good Cohen weighted κ value (0.67 [95% CI, 0.24-1.11]).
Table 3. Comparison of Upper-Airway Obstruction Pattern Between Drug-Induced Sleep Endoscopy and Natural Sleep Endoscopy.
| Obstruction Site | Pattern, No. | Agreement, % | Cohen Weighted κ (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| DISE | NSE | |||||||
| AP | Lat | Circ | AP | Lat | Circ | |||
| Velum | 2 | 2 | 22 | 2 | 2 | 19 | 88.5 | 0.50 (−0.03 to 1.03) |
| Epiglottis | 4 | 1 | 0 | 2 | 1 | 0 | 92.3 | 0.67 (0.24 to 1.11) |
Abbreviations: AP, antero-posterior; Circ, circular; DISE, drug-induced sleep endoscopy; Lat, lateral; NSE, natural sleep endoscopy.
When sites of obstruction grades 1 and 2 were considered, DISE showed more sites requiring treatment compared with NSE (Table 4). However, all sites showed good agreement between DISE and NSE (degree of agreement >85%; Cohen weighted κ >0.60). When sites of obstruction grade 2 were considered, DISE also showed more sites requiring treatment compared with NSE (Table 4). However, agreement between DISE and NSE was moderate in the velum (degree of agreement = 84.6%; Cohen weighted κ = 0.52 [95% CI, 0.09-0.95) and was good in other sites (degree of agreement >85%; Cohen weighted κ >0.60).
Table 4. Comparison of Obstruction Sites Requiring Treatment Between Drug-Induced Sleep Endoscopy and Natural Sleep Endoscopy.
| Obstruction Site | Obstruction Grade 0 vs Grade 1, 2 | Obstruction Grade 0, 1 vs Grade 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DISE | NSE | Agreement, % | Cohen Weighted κ (95% CI) | DISE | NSE | Agreement, % | Cohen Weighted κ (95% CI) | |||||
| Obstruction Grade 0 | Obstruction Grades 1, 2 | Obstruction Grade 0 | Obstruction Grades 1, 2 | Obstruction Grades 0, 1 | Obstruction Grade 2 | Obstruction Grades 0, 1 | Obstruction Grade 2 | |||||
| Velum | 0 | 26 | 2 | 24 | 92.3 | NA | 3 | 23 | 7 | 19 | 84.6 | 0.52 (0.09-095) |
| Oropharynx lateral wall | 16 | 10 | 19 | 7 | 88.5 | 0.74 (0.47-1.02) | 22 | 4 | 22 | 4 | 92.3 | 0.70 (0.31-1.10) |
| Tongue base | 11 | 15 | 15 | 11 | 84.6 | 0.69 (0.43-0.97) | 18 | 8 | 21 | 5 | 88.5 | 0.70 (0.38-1.02) |
| Epiglottis | 21 | 5 | 23 | 3 | 92.3 | 0.71 (0.32-1.10) | 22 | 4 | 24 | 2 | 92.3 | 0.63 (0.13-1.12) |
Abbreviations: DISE, drug-induced sleep endoscopy; NSE, natural sleep endoscopy.
Discussion
Carrasco-Llatas et al7 compared the obstruction findings between DISE performed using midazolam and DISE performed using propofol and found good agreement between the 2 procedures. Yoon et al18 performed similar comparisons between propofol and dexmedetomidine hydrochloride and also observed excellent agreement. Therefore, reports suggest that the type of sedative used does not affect DISE findings considerably.
Because DISE findings are assessed subjectively by clinicians, the results could show intraexaminer variability. A study by Kerizian et al12 showed that DISE had moderate to substantial interrater reliability. Carrasco-Llatas et al19 also reported moderate interrater agreement for DISE. Together, these results indicate that, although DISE involves subjective assessments of the findings, DISE results are not unreliable. In terms of reproducibility, Rodriquez-Bruno et al13 evaluated the reproducibility of DISE and demonstrated good test-retest reliability.
These results suggest that the reliability of DISE is not affected by the use of a variety of drugs and subjective assessments. Furthermore, DISE has good reproducibility. However, it has an inherent shortcoming in that sedative drugs are essential to perform DISE, which may affect the obstruction pattern of the upper airway. The respiratory parameters of OSA, especially in AHI and oxygen saturation, have been shown to be similar between drug-induced sleep and natural sleep. However, sleep architecture (especially, the rapid-eye movement stage) is substantially different between the 2 kinds of sleep,20,21 which may affect the upper-airway obstruction pattern observed during DISE.
In this study, we compared the obstruction patterns during DISE with those during NSE. To our knowledge, this study is the first to investigate the obstruction pattern aspect of DISE. We found that the obstruction patterns of the upper airway showed moderate to good agreement between DISE and NSE. However, the degree of obstruction was slightly higher for DISE than NSE. This finding may be associated with muscle relaxation from midazolam; however, the difference in the duration of the 2 examinations may also have played a role. We performed DISE examination for at least 20 minutes, a sufficient period, but we could not perform NSE for more than 20 minutes because of wakefulness of the patient during the examination. Because DISE shows time-dependent changes in the obstruction pattern,1 the difference in examination duration may have affected the results. Especially for the velum and tongue base, the results showed relatively low concordance between NSE and DISE. Therefore, attention should be paid to the interpretation of the DISE results of these sites. In contrast, DISE and NSE showed high concordance rates (>80%) when compared with the sites in which treatment was needed or not needed. Considering that DISE is an important method for identifying the obstruction sites requiring treatment, it seems to be a reliable test, especially given that it has a very high agreement with NSE, from a clinical point of view.
When the distribution of value deviates from the category, the κ value decreases because the expected agreement (Pe) increases in the calculation formula of κ: κ = (Po – Pe) / (1 – Pe), in which Po is the observed agreement; this occurrence is the κ paradox.22 Although the κ value was low in the velum and epiglottis, which showed deviated distribution (most patients showed grade 2 and circular obstruction in the velum and no obstruction in the epiglottis) owing to the κ paradox, the agreement rate was high in all sites of the upper airway.
Limitations
The main limitation of this study is the small sample size. More patients could not be included owing to the wakefulness of patients during endoscopy and low depth of sleep when the scope was inserted in the nose during NSE. In addition, although body position and obesity could affect the findings of sleep endoscopy,23 only obstruction findings in the supine position were examined and few (23%) obese patients (BMI >30) were included in this study. Moreover, although bispectral index was used to compare findings in the identical depth of sleep, it does not show sleep stages. Therefore, future studies that include multiple positions and sleep stages with larger sample sizes are warranted to confirm this study’s results.
Conclusions
Although sedative drugs are used during DISE, the upper-airway obstruction patterns show a good concordance rate between DISE and NSE. Because the results indicate that DISE findings are similar to those of NSE, DISE seems to be a reliable test.
References
- 1.Heo SJ, Park CM, Kim JS. Time-dependent changes in the obstruction pattern during drug-induced sleep endoscopy. Am J Otolaryngol. 2014;35(1):42-47. doi: 10.1016/j.amjoto.2013.08.017 [DOI] [PubMed] [Google Scholar]
- 2.Lee JS, Heo SJ, Kim JS, Ahn D, Sohn JH, Kim H. Relationship between the severity of laryngopharyngeal reflux and sleep apnea: using drug-induced sleep endoscopy (DISE). Eur Arch Otorhinolaryngol. 2018;275(1):219-224. doi: 10.1007/s00405-017-4812-4 [DOI] [PubMed] [Google Scholar]
- 3.Trudo FJ, Gefter WB, Welch KC, Gupta KB, Maislin G, Schwab RJ. State-related changes in upper airway caliber and surrounding soft-tissue structures in normal subjects. Am J Respir Crit Care Med. 1998;158(4):1259-1270. doi: 10.1164/ajrccm.158.4.9712063 [DOI] [PubMed] [Google Scholar]
- 4.Borowiecki B, Pollak CP, Weitzman ED, Rakoff S, Imperato J. Fibro-optic study of pharyngeal airway during sleep in patients with hypersomnia obstructive sleep-apnea syndrome. Laryngoscope. 1978;88(8 Pt 1):1310-1313. [DOI] [PubMed] [Google Scholar]
- 5.Croft CB, Pringle M. Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci. 1991;16(5):504-509. doi: 10.1111/j.1365-2273.1991.tb01050.x [DOI] [PubMed] [Google Scholar]
- 6.De Vito A, Agnoletti V, Berrettini S, et al. Drug-induced sleep endoscopy: conventional versus target controlled infusion techniques–a randomized controlled study. Eur Arch Otorhinolaryngol. 2011;268(3):457-462. doi: 10.1007/s00405-010-1376-y [DOI] [PubMed] [Google Scholar]
- 7.Carrasco Llatas M, Agostini Porras G, Cuesta González MT, et al. Drug-induced sleep endoscopy: a two drug comparison and simultaneous polysomnography. Eur Arch Otorhinolaryngol. 2014;271(1):181-187. doi: 10.1007/s00405-013-2548-3 [DOI] [PubMed] [Google Scholar]
- 8.Capasso R, Rosa T, Tsou DY, et al. Variable findings for drug-induced sleep endoscopy in obstructive sleep apnea with propofol versus dexmedetomidine. Otolaryngol Head Neck Surg. 2016;154(4):765-770. doi: 10.1177/0194599815625972 [DOI] [PubMed] [Google Scholar]
- 9.Cho JS, Soh S, Kim EJ, et al. Comparison of three sedation regimens for drug-induced sleep endoscopy. Sleep Breath. 2015;19(2):711-717. doi: 10.1007/s11325-015-1127-9 [DOI] [PubMed] [Google Scholar]
- 10.Viana A, Zhao C, Rosa T, et al. The effect of sedating agents on drug-induced sleep endoscopy findings. Laryngoscope. 2019;129(2):506-513. doi: 10.1002/lary.27298 [DOI] [PubMed] [Google Scholar]
- 11.da Cunha Viana A Jr, Mendes DL, de Andrade Lemes LN, Thuler LC, Neves DD, de Araújo-Melo MH. Drug-induced sleep endoscopy in the obstructive sleep apnea: comparison between NOHL and VOTE classifications. Eur Arch Otorhinolaryngol. 2017;274(2):627-635. doi: 10.1007/s00405-016-4081-7 [DOI] [PubMed] [Google Scholar]
- 12.Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN. Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg. 2010;136(4):393-397. doi: 10.1001/archoto.2010.26 [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ. Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg. 2009;140(5):646-651. doi: 10.1016/j.otohns.2009.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo SK, Kwon SB, Moon JS, Lee SH, Lee HB, Lee SJ. Comparison of snoring sounds between natural and drug-induced sleep recorded using a smartphone. Auris Nasus Larynx. 2018;45(4):777-782. doi: 10.1016/j.anl.2017.09.005 [DOI] [PubMed] [Google Scholar]
- 15.Certal VF, Pratas R, Guimarães L, et al. Awake examination versus DISE for surgical decision making in patients with OSA: a systematic review. Laryngoscope. 2016;126(3):768-774. doi: 10.1002/lary.25722 [DOI] [PubMed] [Google Scholar]
- 16.Virk JS, Kotecha B. Sneezing during drug-induced sedation endoscopy. Sleep Breath. 2014;18(3):451-452. doi: 10.1007/s11325-014-1007-8 [DOI] [PubMed] [Google Scholar]
- 17.Kezirian EJ, Hohenhorst W, de Vries N. Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol. 2011;268(8):1233-1236. doi: 10.1007/s00405-011-1633-8 [DOI] [PubMed] [Google Scholar]
- 18.Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS. A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope. 2016;126(3):763-767. doi: 10.1002/lary.25801 [DOI] [PubMed] [Google Scholar]
- 19.Carrasco-Llatas M, Zerpa-Zerpa V, Dalmau-Galofre J. Reliability of drug-induced sedation endoscopy: interobserver agreement. Sleep Breath. 2017;21(1):173-179. doi: 10.1007/s11325-016-1426-9 [DOI] [PubMed] [Google Scholar]
- 20.Sadaoka T, Kakitsuba N, Fujiwara Y, Kanai R, Takahashi H. The value of sleep nasendoscopy in the evaluation of patients with suspected sleep-related breathing disorders. Clin Otolaryngol Allied Sci. 1996;21(6):485-489. doi: 10.1111/j.1365-2273.1996.tb01095.x [DOI] [PubMed] [Google Scholar]
- 21.Rabelo FA, Braga A, Küpper DS, et al. Propofol-induced sleep: polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol Head Neck Surg. 2010;142(2):218-224. doi: 10.1016/j.otohns.2009.11.002 [DOI] [PubMed] [Google Scholar]
- 22.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543-549. doi: 10.1016/0895-4356(90)90158-L [DOI] [PubMed] [Google Scholar]
- 23.Yalamanchili R, Mack WJ, Kezirian EJ. Drug-induced sleep endoscopy findings in supine vs nonsupine body positions in positional and nonpositional obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2018;145(2):159-165. doi: 10.1001/jamaoto.2018.3692 [DOI] [PMC free article] [PubMed] [Google Scholar]