This quasi-experimental study investigates whether the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) was associated with improved perinatal and birth outcomes among recipients in California.
Key Points
Question
Did revisions to the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food package in October 2009, which increased access to whole grains, fruits, vegetables, and low-fat milk, result in improvements in maternal or infant health?
Findings
In this quasi-experimental study of 2 897 537 infants, the revised WIC food package was associated with reduced maternal preeclampsia and gestational weight gain as well as improvements in infant gestational age and birth weight.
Meaning
This evaluation of a major US public health program suggests that improving women’s nutrition may be an important target of clinical interventions and health policy.
Abstract
Importance
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves more than one-quarter of pregnant and postpartum women. In October 2009, the WIC food package underwent revisions to improve nutritional content. No studies have investigated the downstream effects of this revision on maternal and infant health.
Objective
To investigate whether the revised WIC food package improved perinatal and birth outcomes among recipients.
Design, Setting, and Participants
We conducted a quasi-experimental difference-in-differences analysis, comparing WIC recipients (the treatment group) before and after the package revisions while accounting for temporal trends among nonrecipients (the control group). Multivariable linear regressions were adjusted for sociodemographic covariates. This study was conducted using linked birth certificate and hospital discharge data from California from January 2007 to December 2012. Analysis began July 2018.
Exposures
Whether pregnant women received the revised WIC package, which included more whole grains, fruit, vegetables, and low-fat milk.
Main Outcomes and Measures
Measures of maternal and infant health, including maternal preeclampsia, gestational diabetes, and gestational weight gain as well as infant gestational age, birth weight, and hospitalizations.
Results
The sample included 2 897 537 infants born to 2 441 658 mothers. WIC recipients were more likely to be Hispanic, less educated, of greater parity, and younger than nonrecipients. The revised WIC food package was associated with reductions in maternal preeclampsia (−0.6% points; 95% CI, −0.8 to −0.4) and more than recommended gestational weight gain (−3.2% points; 95% CI, −3.6 to −2.7), increased likelihood of as recommended (2.3% points; 95% CI, 1.8 to 2.8) and less than recommended (0.9% points; 95% CI, 0.5 to 1.2) gestational weight gain, and longer gestational age (0.2 weeks; 95% CI, 0.001 to 0.034). Among infants, an increased likelihood of birth weight that was appropriate for gestational age was observed (0.9% points; 95% CI, 0.5 to 1.3). Although birth weight itself was reduced (−0.009 SDs; 95% CI, −0.016 to −0.001), this was accompanied by reductions in small for gestational age (−0.4% points; 95% CI, −0.7 to −0.1), large for gestational age (−0.5% points; 95% CI, −0.8 to −0.2), and low-birth-weight infants (−0.2% points; 95% CI, −0.4 to −0.004), suggesting that the revised food package improved distributions of birth weight.
Conclusions and Relevance
The revised WIC food package, intended to improve women’s nutrition during pregnancy, was associated with beneficial impacts on maternal and child health. This suggests that WIC policy may be an important lever to reduce health disparities among high-risk women and children at a critical juncture in the life course.
Introduction
Maternal nutrition is an important determinant of fetal development.1 Evidence points to the long-term effects of fetal programming on children’s health,2,3 likely due to changes in fetal hormones, metabolism, and other physiologic processes.4 This transmission of disadvantage during pregnancy may explain the intergenerational persistence of health disparities in the United States.5 Researchers have called for additional studies to identify policies and interventions targeting maternal nutrition to reduce the long-term adverse effects among children.2
One of the main US programs focused on nutrition among vulnerable families is the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). WIC is a federal program for low-income pregnant and postpartum women and children younger than 5 years that provides nutritional support, nutrition education, breastfeeding support, and referrals to health and social services.6 More than a quarter of pregnant and postpartum women receive WIC,7 highlighting its potential to reduce disparities in perinatal and later-life health. The introduction of WIC in the mid-1970s resulted in higher birth weights, particularly for less-educated mothers,8 with similar findings in more recent years.9,10
In October 2009, the US Department of Agriculture implemented major revisions to the standard WIC food package after criticism that it had been essentially unchanged for more than 30 years.11 The revised food package was intended to be more nutritious, thereby addressing obesity and chronic disease.11 It included more whole grains, fruits, vegetables, and low-fat milk.11 The revised food package increased household expenditures on whole grains and decreased purchasing of refined grains and whole milk among WIC recipients,12,13,14,15,16 and it led to improvements in maternal and child nutrition.17,18 Little is known regarding the downstream effects of these changes in maternal nutrition on perinatal outcomes. Evaluating public policies is critical, as a handful of prior studies have found that related safety net programs may have unintended negative consequences.19,20 Also, WIC benefits may be redirected to other household members,21 such that changes in purchasing may not translate into improvements in maternal and infant health.
The present study examined the association between the revised WIC food package and perinatal outcomes, using data from more than 2 million births in California. Leveraging a quasi-experimental difference-in-differences (DID) design, we compared pre-post policy changes among WIC recipients with pre-post changes in a control group of nonrecipients to estimate the associations of program revisions with outcomes. Because prior work has shown racial/ethnic disparities in counseling received by WIC recipients and in nutritional and breastfeeding practices prior to the implementation of the revised food package,22,23,24 we also conducted subgroup analyses by race/ethnicity. At a time when federal funding for WIC is increasingly challenged,25 evidence on the intergenerational impacts of WIC may help inform policy making and other clinical and community-level interventions targeting maternal nutrition.
Methods
Data
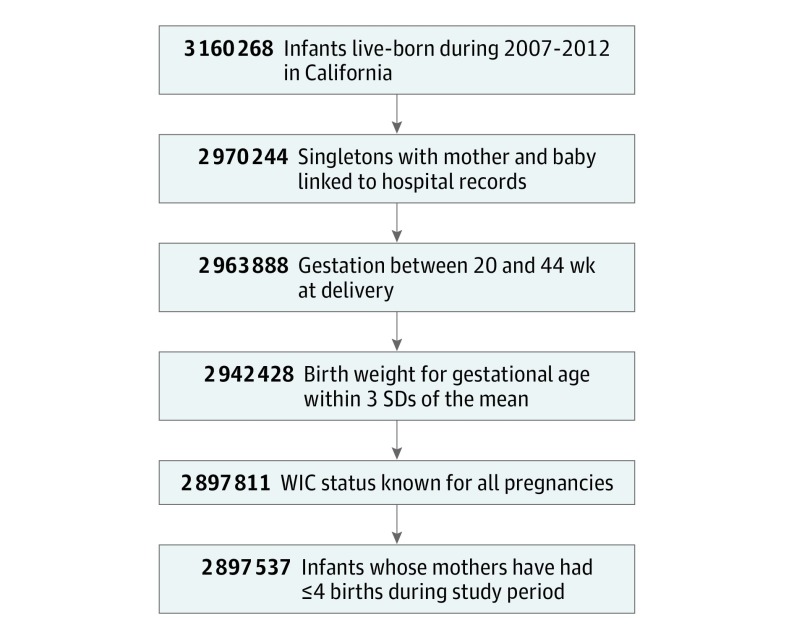
This study used data from January 2007 to December 2012 from the California Office of State Health Planning and Development database. The database contains linked birth certificates and hospital discharge records for mothers and infants from 1 year before birth to 1 year after birth. We included California singleton infants live-born from 2007 to 2012 with a gestational age of 20 to 44 weeks at delivery (Figure and eMethods in the Supplement). The study was approved by the Committee for the Protection of Human Subjects within the Health and Human Services Agency of California (protocol #12-09-0702l). Informed consent was waived by the institutional review board because this study used administrative birth certificate data. Analysis began in July 2018.
Figure. Sample Selection of Infants in Study.
Data set was constructed using linked birth certificate, death certificate, and hospital discharge data from the California Office of State Health Planning and Development. WIC indicates Special Supplemental Nutrition Program for Women, Infants, and Children.
Variables
Exposure
Beginning in 2007, California birth certificates included a question indicating whether the mother received WIC benefits during the current pregnancy. Among WIC recipients, we considered a woman to have received the revised WIC food package if her pregnancy occurred after the October 2009 revisions. Women whose pregnancies included October 2009 were classified as having received the revised package if they gave birth in February 2010 or later (ie, at least half the pregnancy occurred after the package revisions).
Outcomes
We selected maternal and infant outcomes that could be affected by the mother’s receipt of the revised food package. Maternal outcomes included whether the mother was diagnosed as having preeclampsia or gestational diabetes. We also calculated whether the mother gained less weight, more weight, or was within recommended gestational weight gain (GWG) according to guidelines from the Institute of Medicine (now the National Academy of Medicine).26 These categories were determined based on height, prepregnancy weight, and delivery weight.
Infant outcomes included a z score for birth weight (mean [SD], 0 [1]), weeks of gestation at delivery, and binary variables representing whether the infant was preterm (ie, born before 37 weeks’ gestation); was appropriate for gestational age (AGA), small for gestational age (SGA), large for gestational age (LGA), had low birth weight (LBW, <2500 g) or very LBW (<1500 g); had a longer than expected hospital admission at birth (>2 days for vaginal delivery, >4 days for cesarean delivery); or was readmitted to the hospital within 1 year after birth.
Covariates
Covariates included sociodemographic variables on the birth certificate. We adjusted models for mother’s education, age, race/ethnicity, and parity and infant’s sex and year of birth.
Analysis
We first tabulated sample characteristics among WIC recipients and nonrecipients who gave birth before and after implementation of the revised food package. We then estimated the associations of the revised food package with outcomes using DID analysis. Difference-in-differences design is a quasi-experimental technique for examining the association of policy changes with outcomes while accounting for secular trends.27,28 We took advantage of the fact that revisions to WIC food packages occurred in October 2009 and that this policy change was unlikely to be associated with mother or infant characteristics. This created a natural experiment in that a mother who gave birth in February 2010 or later was exposed to the revised food package for at least half of her pregnancy, while a mother who gave birth before February 2010 was exposed to the revised WIC food package for less than half of her pregnancy or not at all. We thus compared WIC recipients who gave birth on or after February 2010 with those who gave birth before February 2010. To factor out possible secular trends in outcomes over time, DID analysis “differences out” pre-post changes observed among individuals who did not receive WIC.
One underlying assumption is that pre-post differences in outcomes would have been similar between WIC recipients and nonrecipients in the absence of the revised package. While this counterfactual scenario fundamentally cannot be tested, we assessed whether trends in the outcomes during the prerevision period were parallel for WIC recipients and nonrecipients (eMethods, eFigure 1, and eFigure 2 in the Supplement). We also assessed whether the pre-post changes in observed covariates were similar among WIC recipients and nonrecipients to rule out differential compositional changes over time.
Practically speaking, DID analysis involved the implementation of multivariable linear regressions, including an interaction term between WIC status and an indicator for whether the birth occurred before or after the revised food package was implemented. These analyses adjusted for covariates listed above, and additional sensitivity tests included controls for month of birth. The eMethods and eTable 1 in the Supplement include additional details and equations. All tests were 2-tailed, and P values less than .05 were considered to be statistically significant.
Secondary Analyses
First, we conducted subgroup analyses to test for heterogeneity in the response to the WIC revisions by race/ethnicity. To do so, we carried out stratified analyses to produce estimates for each racial/ethnic group, as well as regressions including an interaction term between race/ethnicity and the primary exposure variable to determine whether differences by race/ethnicity were statistically significantly different from one another. Second, because birth certificates do not include information on timing or duration of WIC receipt during pregnancy, we excluded women whose pregnancies included October 2009 to avoid misclassification (n = 383 483).
Results
Sample Characteristics
The final sample included 2 897 537 infants born to 2 441 658 mothers. Overall, 68.1% of WIC recipients were Hispanic, compared 26.0% of nonrecipients. In addition, 25.2% of WIC recipients had more than a high school education, compared with about 72.9% of nonrecipients. WIC recipients were also more likely to be of greater parity and younger than nonrecipients (Table 1). Maternal health was similar for WIC recipients and nonrecipients, although the health of WIC recipients’ infants was worse for several outcomes (Table 2). This included a lower birth weight z score (−0.002 vs 0.05), a higher proportion with SGA birth weight (8.9% vs 8.0%), longer than expected admission at birth (11.1% vs 9.6%), and more readmission in the first year of life (11.1% vs 8.7%).
Table 1. Sample Sociodemographic Characteristics by WIC Receipt and Birthdate Relative to Implementation of Revised WIC Food Packagea.
| Characteristic | WIC, No. (%) | No WIC, No. (%) | ||
|---|---|---|---|---|
| Born Before Revision (n = 821 878) | Born After Revision (n = 747 167) | Born Before Revision (n = 716 675) | Born After Revision (n = 611 817) | |
| Mother | ||||
| Race/ethnicity | ||||
| White | 92 081 (11.2) | 94 983 (12.7) | 303 368 (42.3) | 264 405 (43.2) |
| Black | 53 654 (6.5) | 51 753 (6.9) | 28 162 (3.9) | 21 396 (3.5) |
| Hispanic | 577 860 (70.3) | 490 965 (65.7) | 195 834 (27.3) | 149 426 (24.4) |
| Asian | 45 315 (5.5) | 45 662 (6.1) | 141 048 (19.7) | 129 011 (21.1) |
| Other | 52 968 (6.4) | 63 804 (8.5) | 48 263 (6.7) | 47 579 (7.8) |
| Amount of education, y | ||||
| <12 | 350 035 (44.0) | 261 292 (36.3) | 51 479 (7.4) | 30 198 (5.2) |
| 12 | 263 671 (33.1) | 245 910 (34.1) | 135 537 (19.6) | 93 264 (15.9) |
| >12 | 182 332 (22.9) | 213 115 (29.6) | 505 145 (73.0) | 463 251 (79.0) |
| Parity status | ||||
| Nulliparous | 303 105 (36.9) | 270 634 (36.2) | 311 340 (43.5) | 270 142 (44.2) |
| Parity 1-2 | 234 149 (28.5) | 214 519 (28.7) | 245 384 (34.3) | 213 938 (35.0) |
| Parity ≥3 | 284 331 (34.6) | 261 861 (35.1) | 159 550 (22.3) | 127 520 (20.9) |
| Age at delivery, mean (SD), y | 26.0 (6.2) | 26.5 (6.2) | 30.4 (5.7) | 30.9 (5.4) |
| Infant | ||||
| Male | 420 471 (51.2) | 381 270 (51.0) | 368 263 (51.4) | 314 794 (51.5) |
| Birth year | ||||
| 2007 | 266 209 (32.4) | 0 | 246 736 (34.4) | 0 |
| 2008 | 270 293 (32.9) | 0 | 233 129 (32.5) | 0 |
| 2009 | 263 982 (32.1) | 0 | 219 774 (30.7) | 0 |
| 2010 | 21 394 (2.6) | 237 462 (31.8) | 17 036 (2.4) | 194 921 (31.9) |
| 2011 | 0 | 255 601 (34.2) | 0 | 207 879 (34.0) |
| 2012 | 0 | 254 104 (34.0) | 0 | 209 017 (34.2) |
Abbreviation: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
N = 2 897 537. Sample includes singleton infants who were live-born in California from 2007 to 2012, with gestational age between 20 and 44 weeks at delivery. Data set was constructed using linked birth certificate, death certificate, and hospital discharge data from the California Office of State Health Planning and Development. For women whose pregnancies included October 2009, we classified them as having been exposed if they gave birth in February 2010 or later (ie, at least half of their pregnancy occurred after the package was revised).
Table 2. Sample Health Characteristics by WIC Receipt and Birthdate Relative to Implementation of Revised WIC Food Packagea.
| Characteristic | WIC, No. (%) | No WIC, No. (%) | ||
|---|---|---|---|---|
| Born Before Revision (n = 821 878) | Born After Revision (n = 747 167) | Born Before Revision (n = 716 675) | Born After Revision (n = 611 817) | |
| Mother | ||||
| Preeclampsia | 28 393 (3.5) | 28 203 (3.8) | 21 983 (3.1) | 20 661 (3.4) |
| Gestational diabetes | 61 955 (7.6) | 67 369 (9.1) | 55 608 (7.8) | 56 505 (9.3) |
| Gestational weight gainb | ||||
| <Recommended | 161 587 (21.9) | 155 717 (22.1) | 118 001 (17.9) | 104 195 (18.1) |
| >Recommended | 303 682 (41.1) | 284 257 (40.3) | 284 898 (43.2) | 242 375 (42.2) |
| Within recommendation | 272 908 (37.0) | 265 827 (37.7) | 257 326 (39) | 227 729 (39.7) |
| Infant | ||||
| Birth weight, mean (SD), z score | 0.006 (0.95) | −0.01 (1.0) | 0.06 (0.9) | 0.04 (0.9) |
| Gestational age at birth, mean (SD), wk | 38.7 (1.8) | 38.7 (1.8) | 38.7 (1.9) | 38.8 (1.8) |
| Born <37 wk gestation | 59 160 (7.2) | 51 374 (6.9) | 51 291 (7.2) | 41 168 (6.7) |
| Birth weight categories | ||||
| AGA | 670 668 (81.7) | 611 740 (81.9) | 586 784 (81.9) | 503 261 (82.3) |
| SGA | 72 911 (8.9) | 67 256 (9.0) | 56 717 (7.9) | 49 388 (8.1) |
| LGA | 77 544 (9.4) | 67 695 (9.1) | 72 551 (10.1) | 58 781 (9.6) |
| LBW | 41 875 (5.1) | 38 493 (5.2) | 35 586 (5.0) | 30 067 (4.9) |
| Very LBW | 6014 (0.7) | 5735 (0.8) | 5817 (0.8) | 4830 (0.8) |
| Lengthy admission at birth | 90 518 (11.0) | 83 361 (11.2) | 69 746 (9.7) | 58 416 (9.6) |
| Admitted in year after birth | 94 328 (11.5) | 81 230 (10.9) | 64 891 (9.1) | 50 737 (8.3) |
Abbreviations: AGA, appropriate for gestational age; LBW, low birth weight; LGA, large for gestational age; SGA, small for gestational age; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Sample includes California singleton infants who were live-born from 2007 to 2012, with gestational age between 20 and 44 weeks at delivery. Data set was constructed using linked birth certificate, death certificate, and hospital discharge data from the California Office of State Health Planning and Development. For women whose pregnancies included October 2009, we classified them as having been exposed if they gave birth in February 2010 or later (ie, at least half of their pregnancy occurred after the package was revised).
Gestational weight gain categories are based on recommendations of the Institute of Medicine.
Difference-in-Differences Model Assumptions
All outcomes except preterm birth and gestational diabetes demonstrated roughly parallel trends during the prerevision period (eFigure 1 in the Supplement). The changes in key covariates between the prerevision and postrevision periods among WIC recipients were similar to pre-post changes among nonrecipients (Table 1), which supports the assumptions underlying the DID models.
Revised WIC Package and Maternal Health
The revised food package was associated with reduced likelihood of preeclampsia (−0.6% points; 95% CI, −0.8 to −0.4), reduced likelihood of more-than-recommended GWG (−3.2% points; 95% CI, −3.6 to −2.7), increased likelihood of less-than-recommended GWG (0.9% points; 95% CI, 0.5 to 1.2), and increased likelihood of within-recommended GWG (2.3% points; 95% CI, 1.8 to 2.8) (Table 3). We were unable to rule out the null hypothesis that there was no association with gestational diabetes. In the sensitivity analyses in which we excluded mothers whose pregnancies included October 2009, results were similar to the primary analyses (eTable 2 in the Supplement).
Table 3. Association of Revised WIC Food Package With Maternal and Infant Healtha.
| Characteristic | Association of Revised WIC Package (95% CI) |
|---|---|
| Mother | |
| Preeclampsia | −0.60 (−0.76 to −0.43) |
| Gestational diabetes | −0.035 (−0.25 to 0.18) |
| Gestational weight gainb | |
| <Recommended | 0.86 (0.47 to 1.3) |
| >Recommended | −3.2 (−3.6 to −2.7) |
| Within recommended | 2.3 (2.3 to 2.8) |
| Infant | |
| Birth weight, z score | −0.009 (−0.016 to −0.001) |
| Gestational age at birth, wk | 0.018 (0.001 to 0.034) |
| Born <37 wk gestation | 0.17 (−0.075 to 0.42) |
| Birth weight categories | |
| AGA | 0.94 (0.55 to 1.3) |
| SGA | −0.42 (−0.69 to −0.15) |
| LGA | −0.52 (−0.81 to −0.23) |
| LBW | −0.21 (−0.42 to −0.004) |
| Very LBW | −0.079 (−0.16 to 0.005) |
| Longer than expected infant admission at birth | −0.001 (−0.31 to 0.31) |
| Infant readmitted in first year after birth | −0.056 (−0.39 to 0.27) |
Abbreviations: AGA, appropriate for gestational age; LBW, low birth weight; LGA, large for gestational age; SGA, small for gestational age; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Values above represent the coefficients on the interaction term between WIC receipt and mother giving birth in February 2010 or later. Coefficients for binary outcomes were multiplied by 100 and therefore represent a change in percentage points. Analyses involved multivariable linear models (ie, linear probability models for binary outcomes) with maternal fixed effects and robust standard errors clustered by mother. Covariates included mother’s race/ethnicity, education, age, and parity and infant’s sex and year of birth.
Gestational weight gain categories are based on recommendations of the Institute of Medicine.
Revised WIC Package and Infant Health
Infants of WIC recipients exposed to the revised food package had longer mean gestational age at birth (0.2 weeks; 95% CI, 0.001 to 0.034) and reduced birth weight z score (−0.009 SDs; 95% CI, −0.016 to −0.001) (Table 3). They were also more likely to be AGA (0.9% points; 95% CI, 0.5 to 1.3) and less likely to be SGA (−0.4% points; 95% CI, −0.7 to −0.1) and LGA (−0.5% points; 95% CI, −0.8 to −0.2) or have LBW (−0.2% points; 95% CI, −0.4 to −0.004). We were unable to rule out the null hypothesis that there was no association with preterm birth, very LBW, length of admission at birth, or readmissions in the first year of life. When excluding mothers whose pregnancy included October 2009, results were similar to the primary analysis, except that differences for gestational age and birth weight were no longer statistically significant at P < .05 (eTable 2 in the Supplement).
Differences by Race/Ethnicity
There were racial/ethnic differences in the estimated associations of the revised WIC food package with maternal health (Table 4). Black women, Hispanic women, Asian women, and women of other races had reduced gestational diabetes, while white women did not. The increase in less-than-recommended GWG was less pronounced among Hispanic, Asian, and other women compared with white women, and the reduction in more-than-recommended GWG was less pronounced among Hispanic and Asian women.
Table 4. Association of Revised WIC Food Package With Maternal and Infant Health by Racea.
| Variable | Association of Revised WIC Package (95% CI) | ||||
|---|---|---|---|---|---|
| Whiteb | Black | Hispanic | Asian | Other | |
| Mother | |||||
| Preeclampsia | −0.31 (−0.64 to 0.017) | 0.16 (−0.74 to 1.1) | −0.55 (−0.84 to −0.26) | −0.33 (−0.74 to 0.081) | 0.039 (−0.78 to 0.86) |
| Gestational diabetes | 0.71 (0.27 to 1.1) | −1.1 (−2.0 to −0.24)c | −0.31 (−0.70 to 0.083)c | −1.1 (−1.9 to −0.22)c | −0.43 (−1.5 to 0.66)c |
| Gestational weight gaind | |||||
| <Recommended | 2.0 (1.2 to 2.8) | 1.7 (−0.17 to 3.5) | 1.0 (0.35 to 1.7)c | 1.3 (−0.095 to 2.7)c | 0.16 (−1.6 to 1.9)c |
| >Recommended | −4.2 (−5.2 to −3.2) | −5.5 (−7.7 to −3.3) | −1.8 (−2.7 to −1.0)c | −2.2 (−3.7 to −0.80)c | −3.2 (−5.6 to −0.90) |
| Within recommended | 2.2 (1.2 to 3.3) | 3.8 (1.4 to 6.2) | 0.80 (−0.13 to 1.7) | 0.93 (−0.86 to 2.7) | 3.1 (0.50 to 5.6) |
| Infant | |||||
| Birth weight, z score | −0.030 (−0.046 to −0.013) | −0.051 (−0.086 to −0.016) | −0.0029 (−0.016 to 0.011)c | −0.0030 (−0.026 to 0.020)c | 0.016 (−0.022 to 0.055)c |
| Gestational age at birth, wk | −0.036 (−0.069 to −0.0020) | −0.045 (−0.14 to 0.052) | 0.048 (0.019 to 0.078)c | 0.021 (−0.030 to 0.071)c | −0.026 (−0.11 to 0.057) |
| Born <37 wk gestation | 0.77 (0.26 to 1.3) | 0.17 (−1.1 to 1.5) | −0.23 (−0.67 to 0.21)c | −0.0017 (−0.80 to 0.80)c | 0.084 (−1.2 to 1.4) |
| Birth weight categories | |||||
| AGA | 1.0 (0.17 to 1.8) | −0.46 (−2.3 to 1.4) | 1.1 (0.43 to 1.8) | −0.52 (−1.7 to 0.70)c | 0.59 (−1.4 to 2.6) |
| SGA | −0.020 (−0.55 to 0.51) | 0.40 (−1.1 to 1.8) | −0.58 (−1.0 to −0.13) | 0.18 (−0.82 to 1.2) | −1.3 (−2.5 to 0.027) |
| LGA | −0.98 (−1.6 to −0.33) | 0.067 (−1.1 to 1.2)c | −0.53 (−1.1 to −0.0077) | 0.34 (−0.36 to 1.0)c | 0.66 (−0.87 to 2.2)c |
| LBW | 0.20 (−0.20 to 0.61) | 0.15 (−1.1 to 1.4) | −0.26 (−0.62 to 0.097) | 0.070 (−0.66 to 0.80) | −0.51 (−1.5 to 0.51) |
| Very LBW | −0.073 (−0.24 to 0.089) | 0.59 (−0.033 to 1.2)c | 0.021 (−0.13 to 0.17) | −0.048 (−0.30 to 0.21) | −0.18 (−0.60 to 0.24) |
| Longer than expected infant admission at birth | 0.35 (−0.30 to 0.99) | 0.33 (−1.2 to 1.9) | −0.38 (−0.91 to 0.15) | 0.072 (−0.94 to 1.1) | −0.53 (−2.1 to 1.0) |
| Infant readmitted in first year after birth | −0.083 (−0.78 to 0.61) | −1.4 (−2.9 to 0.066) | −0.30 (−0.87 to 0.27) | 0.32 (−0.75 to 1.4) | −1.0 (−2.6 to 0.62) |
Abbreviations: AGA, appropriate for gestational age; LBW, low birth weight; LGA, large for gestational age; SGA, small for gestational age; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Values above represent the coefficients on the interaction term between WIC receipt and mother giving birth in February 2010 or later in regressions that were stratified by race/ethnicity. Coefficients for binary outcomes were multiplied by 100 and therefore represent a change in percentage points. Analyses involved multivariable linear models (ie, linear probability models for binary outcomes) with maternal fixed effects and robust standard errors clustered by mother. Covariates included mother’s education, age, and parity and infant’s sex and year of birth.
Reference group.
P < .05 indicates that a given estimate is statistically significantly different from the estimate for white women in regressions that included an interaction term for race/ethnicity.
Gestational weight gain categories are based on recommendations of the Institute of Medicine.
For infant health, reduced birth weight was less pronounced among Hispanic and Asian women compared with white women, and birth weight increased among other women. Hispanic and Asian women were also more likely to have higher gestational age at delivery and reduced likelihood of preterm birth than white women in response to the revised WIC food package. Asian women had lower likelihood of having an AGA infant, while black, Asian, and other women had increased likelihood of having an LGA infant. Black women were more likely to have a very LBW infant compared with white women.
Discussion
In this study, we estimated the associations of the 2009 revised WIC food package with perinatal outcomes. We used quasi-experimental DID analysis in a large diverse sample of California births. The revised WIC food package was intended to improve maternal nutrition by providing more whole grains, fruits, vegetables, and low-fat milk. We found improvements in a number of outcomes, including maternal preeclampsia and weight gain, gestational age, and appropriate birth weight for gestational age.
While previous studies have found beneficial associations of the revised WIC food package with household food expenditures and maternal dietary quality,12,13,14,15,16,17 this is the first study to our knowledge to examine downstream health benefits during the perinatal period. In several cases, the magnitude of the findings represents a clinically meaningful change, which is likely to have a substantial impact at the population level.29 For example, we found a reduction in preeclampsia of 0.6% points, which represents a 17% reduction from a base of 3.5%. Nutritional factors such as low fiber and high lipid intake have been implicated as risk factors for preeclampsia, perhaps because they trigger inflammatory responses and endothelial dysfunction.30 However, most of these studies have involved correlational analyses that are unable to account for confounding by unobserved characteristics that may differ for women who eat different amounts of these foods. Our study provides quasi-experimental evidence suggesting this association may be causal and that policies to improve maternal nutrition may be an effective strategy to prevent preeclampsia.
Similarly, we found reductions in maternal GWG among WIC recipients after the implementation of the revised food package. More than 40% of women in this sample gained more weight than recommended, and the revised food package resulted in a reduction of 3.2% points, or 7.8% compared with the control group. This could be explained by the substitution of low-fat milk for whole milk or the provision of whole-grain instead of white bread, which has a higher glycemic index.31 Because excessive GWG has been correlated with increased obesity and chronic disease later in life for mothers and children32,33 and because low-income children are at high risk of severe obesity,34 future studies should examine whether the revised WIC food package had effects on long-term health.
For infant health outcomes, effect sizes were more modest perhaps because these represent outcomes further downstream from the primary intervention. Given the sample size, it is unlikely that analyses were underpowered. Nevertheless, while these may not be clinically meaningful changes for an individual patient, some represent meaningful changes in disease distribution at the population level.29 For example, we found that the revised food package was associated with longer gestation (roughly 1% of an SD). While there was also evidence of reduced birth weight, we found accompanying reductions in SGA, LGA, and LBW babies—about 4% to 5% lower than baseline levels—suggesting that the reduction in birth weight might be explained by fewer LGA and more AGA infants rather than an increase in SGA infants. Alternatively, it may be due to in utero fetal selection, in that high-risk fetuses may be more likely to be born owing to better nutrition.35 Moreover, the change in birth weight represented reduction in the z score of 0.009, which may not be meaningful in a sample this large. As expected, the reduction in LBW (0.2% points) was smaller than the reduction that was documented among WIC recipients when the program was first introduced (1.4% points)8 perhaps because the package revisions represent only an incremental change over and above the availability of the package itself. We were unable to rule out the null hypothesis that there was no association with infant hospitalizations, possibly because of the rarity of this outcome or because it is driven by factors other than nutrition. Nevertheless, these findings suggest improved maternal nutrition translated into improvements in newborn outcomes.
We were also unable to rule out the null hypothesis that there was no association of the revised WIC food package with gestational diabetes and preterm birth. Of note, these were the 2 outcomes for which the parallel trends assumption was not met, so the results for these outcomes should be interpreted cautiously. Prior work suggests that maternal nutrition is an important determinant of gestational diabetes,36 but it may be that the revised food package did not reduce the consumption of other products like sugar-sweetened beverages that may be more important culprits than refined grains, or that the origins of gestational diabetes lie in the preconception period. Similarly, prior work suggests that maternal psychosocial stressors and biomedical factors are important determinants of preterm birth.37 While prior work has found that WIC receipt is associated with reduced preterm birth,38 it may be that revisions to the food package did not provide any additional benefit.
There were inconsistent racial/ethnic differences in the association of the revised food package with maternal and infant health. Black women, Hispanic women, Asian women, and women of other races were less likely to develop gestational diabetes, although this result should be interpreted cautiously because this outcome failed the parallel trends test. Hispanic and Asian women were less likely than white women to experience reduced GWG. These women were also more likely to have heavier infants of greater gestational age. The burden of adverse birth outcomes and infant mortality is born disproportionately by black women,39,40 and our study suggests that differences in the associations of the revised WIC food package with outcomes do not explain these findings. Future studies should attempt to further illuminate and address these inequities. For example, prior work has found that WIC counselors offer disparate counseling to white and black women22 and that Hispanic women are more likely than black women to reside in close proximity to WIC-approved stores,41 concerning for structural racism embedded in the clinical and community contexts.42,43
Limitations
This study has several limitations. First, linked birth certificate and hospital discharge data were only available through 2012; future studies should attempt to replicate these analyses when more recent data become available from state agencies. Second, our study was conducted in California, and results may not generalize to other states; while the WIC food package is intended to be standard nationwide, the foods available in local stores may differ and the characteristics of pregnant women in California may differ from those in other states. Also, we did not have information on the timing of WIC enrollment during pregnancy, as this information is not provided on birth certificates. Finally, DID analysis relies on the assumption that there were no other exposures that may differentially influence outcomes between the treatment and control groups over the course of the study period. The Great Recession of 2008 to 2009 may represent such a confounder. While we were not able to test this counterfactual scenario, prior work has found that adverse health effects of the recession accrued disproportionately to individuals of lower socioeconomic status,44 which is the opposite of our findings and therefore unlikely to explain our results.
Conclusions
In conclusion, we found that revisions to improve the nutritional content of the WIC food package in October 2009 were associated with improvements in maternal and infant health at the population level, with inconsistent differences by race/ethnicity. More than a quarter of pregnant and postpartum women in the United States receive WIC, making it among the largest safety net programs for vulnerable families. These findings should be incorporated into future cost-benefit analyses of WIC.45 The results suggest that social policy may be an important lever to reduce health disparities, and it strengthens the evidence for improving maternal nutrition during pregnancy.
eMethods.
eTable 1. Effect of revised WIC food package on maternal and infant health outcomes, including control variables for month and year of birth
eTable 2. Effect of revised WIC food package on maternal and infant health outcomes, excluding pregnancies that included October 2009
eFigure 1. Graphical evaluation of parallel trends assumption
eFigure 2. Graphical evaluation of parallel trends assumption in low-education sample
References
- 1.Barker DJP. Maternal nutrition, fetal nutrition, and disease in later life. Nutrition. 1997;13(9):807-813. doi: 10.1016/S0899-9007(97)00193-7 [DOI] [PubMed] [Google Scholar]
- 2.Wu G, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. J Nutr. 2004;134(9):2169-2172. doi: 10.1093/jn/134.9.2169 [DOI] [PubMed] [Google Scholar]
- 3.Painter RC, Roseboom TJ, Bleker OP. Prenatal exposure to the Dutch famine and disease in later life: an overview. Reprod Toxicol. 2005;20(3):345-352. doi: 10.1016/j.reprotox.2005.04.005 [DOI] [PubMed] [Google Scholar]
- 4.Barker DJP, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341(8850):938-941. doi: 10.1016/0140-6736(93)91224-A [DOI] [PubMed] [Google Scholar]
- 5.Aizer A, Currie J. The intergenerational transmission of inequality: maternal disadvantage and health at birth. Science. 2014;344(6186):856-861. doi: 10.1126/science.1251872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bitler MP, Currie J, Scholz JK. WIC eligibility and participation. J Hum Resour. 2003;38:1139-1179. doi: 10.2307/3558984 [DOI] [Google Scholar]
- 7.Oliveira V, Frazao E. The WIC Program: Background, Trends, and Economic Issues, 2015 Edition. Economic Information Bulletin no. 134. Washington, DC: United States Department of Agriculture, Economic Research Service; 2015. [Google Scholar]
- 8.Hoynes H, Page M, Stevens AH. Can targeted transfers improve birth outcomes?: evidence from the introduction of the WIC program. J Public Econ. 2011;95(7-8):813-827. doi: 10.1016/j.jpubeco.2010.12.006 [DOI] [Google Scholar]
- 9.Bitler MP, Currie J. Does WIC work? the effects of WIC on pregnancy and birth outcomes. J Policy Anal Manage. 2005;24(1):73-91. doi: 10.1002/pam.20070 [DOI] [PubMed] [Google Scholar]
- 10.Kowaleski-Jones L, Duncan GJ. Effects of participation in the WIC program on birthweight: evidence from the National Longitudinal Survey of Youth: Special Supplemental Nutrition Program for Women, Infants, and Children. Am J Public Health. 2002;92(5):799-804. doi: 10.2105/AJPH.92.5.799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute of Medicine WIC Food Packages: Time for a Change. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 12.Oh M, Jensen HH, Rahkovsky I. Did revisions to the WIC program affect household expenditures on whole grains? Appl Econ Perspect Policy. 2016;38(4):578-598. doi: 10.1093/aepp/ppw020 [DOI] [Google Scholar]
- 13.Andreyeva T, Luedicke J. Federal food package revisions: effects on purchases of whole-grain products. Am J Prev Med. 2013;45(4):422-429. doi: 10.1016/j.amepre.2013.05.009 [DOI] [PubMed] [Google Scholar]
- 14.Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages on access to healthy foods. J Acad Nutr Diet. 2012;112(6):850-858. doi: 10.1016/j.jand.2012.02.019 [DOI] [PubMed] [Google Scholar]
- 15.Andreyeva T, Tripp AS. The healthfulness of food and beverage purchases after the federal food package revisions: the case of two New England states. Prev Med. 2016;91:204-210. doi: 10.1016/j.ypmed.2016.08.018 [DOI] [PubMed] [Google Scholar]
- 16.Ng SW, Hollingsworth BA, Busey EA, Wandell JL, Miles DR, Poti JM. Federal nutrition program revisions impact low-income households’ food purchases. Am J Prev Med. 2018;54(3):403-412. doi: 10.1016/j.amepre.2017.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamad R, Batra A, Karasek D, et al. . The impact of the revised WIC food package on maternal nutrition during pregnancy and postpartum [published online May 16, 2019]. Am J Epidemiol. 2019;kwz098. doi: 10.1093/aje/kwz098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tester JM, Leung CW, Crawford PB. Revised WIC food package and children’s diet quality. Pediatrics. 2016;137(5):e20153557. doi: 10.1542/peds.2015-3557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamad R, Collin DF, Rehkopf DH. Estimating the short-term effects of the earned income tax credit on child health. Am J Epidemiol. 2018;187(12):2633-2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haider SJ, Jacknowitz A, Schoeni RF. Welfare work requirements and child well-being: evidence from the effects on breast-feeding. Demography. 2003;40(3):479-497. doi: 10.1353/dem.2003.0023 [DOI] [PubMed] [Google Scholar]
- 21.Robinson C. The gendered health benefits of WIC participation. J Econ Insight. 2018;44(1):21-43. [Google Scholar]
- 22.Beal AC, Kuhlthau K, Perrin JM. Breastfeeding advice given to African American and white women by physicians and WIC counselors. Public Health Rep. 2003;118(4):368-376. doi: 10.1016/S0033-3549(04)50264-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurley KM, Black MM, Papas MA, Quigg AM. Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low-income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Matern Child Nutr. 2008;4(2):95-105. doi: 10.1111/j.1740-8709.2007.00105.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kong A, Odoms-Young AM, Schiffer LA, et al. . Racial/ethnic differences in dietary intake among WIC families prior to food package revisions. J Nutr Educ Behav. 2013;45(1):39-46. doi: 10.1016/j.jneb.2012.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National WIC Association. Weekly WIC policy update. https://www.nwica.org/blog/weekly-wic-policy-update-107#.XNw9gRRKhhE. Published March 26, 2018. Accessed May 15, 2019.
- 26.Institute of Medicine Nutrition During Pregnancy: Part I, Weight Gain: Part II, Nutrient Supplements. Washington, DC; 1990. [Google Scholar]
- 27.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. doi: 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- 28.Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health. 2017;38:351-370. doi: 10.1146/annurev-publhealth-031816-044208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR; Clinical Significance Consensus Meeting Group . Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371-383. doi: 10.4065/77.4.371 [DOI] [PubMed] [Google Scholar]
- 30.Xu H, Shatenstein B, Luo Z-C, Wei S, Fraser W. Role of nutrition in the risk of preeclampsia. Nutr Rev. 2009;67(11):639-657. doi: 10.1111/j.1753-4887.2009.00249.x [DOI] [PubMed] [Google Scholar]
- 31.Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287(18):2414-2423. doi: 10.1001/jama.287.18.2414 [DOI] [PubMed] [Google Scholar]
- 32.Sridhar SB, Darbinian J, Ehrlich SF, et al. . Maternal gestational weight gain and offspring risk for childhood overweight or obesity. Am J Obstet Gynecol. 2014;211(3):259.e1-259.e8. doi: 10.1016/j.ajog.2014.02.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen AK, Chaffee BW, Rehkopf DH, Coyle JR, Abrams B. Excessive gestational weight gain over multiple pregnancies and the prevalence of obesity at age 40. Int J Obes (Lond). 2014;38(5):714-718. doi: 10.1038/ijo.2013.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan L, Park S, Slayton R, Goodman AB, Blanck HM. Trends in severe obesity among children aged 2 to 4 years enrolled in special supplemental nutrition program for women, infants, and children from 2000 to 2014. JAMA Pediatr. 2018;172(3):232-238. doi: 10.1001/jamapediatrics.2017.4301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baird DD. The gestational timing of pregnancy loss: adaptive strategy? Am J Hum Biol. 2009;21(6):725-727. doi: 10.1002/ajhb.20935 [DOI] [PubMed] [Google Scholar]
- 36.Silva-Zolezzi I, Samuel TM, Spieldenner J. Maternal nutrition: opportunities in the prevention of gestational diabetes. Nutr Rev. 2017;75(suppl 1)(suppl 1):32-50. doi: 10.1093/nutrit/nuw033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth. 2015;28(3):179-193. doi: 10.1016/j.wombi.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 38.Fingar KR, Lob SH, Dove MS, Gradziel P, Curtis MP. Reassessing the association between WIC and birth outcomes using a fetuses-at-risk approach. Matern Child Health J. 2017;21(4):825-835. doi: 10.1007/s10995-016-2176-9 [DOI] [PubMed] [Google Scholar]
- 39.Rossen LM, Khan D, Schoendorf KC. Mapping geographic variation in infant mortality and related black-white disparities in the US. Epidemiology. 2016;27(5):690-696. doi: 10.1097/EDE.0000000000000509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nuru-Jeter A, Dominguez TP, Hammond WP, et al. . “It’s the skin you’re in”: African-American women talk about their experiences of racism: an exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2009;13(1):29-39. doi: 10.1007/s10995-008-0357-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hillier A, McLaughlin J, Cannuscio CC, Chilton M, Krasny S, Karpyn A. The impact of WIC food package changes on access to healthful food in 2 low-income urban neighborhoods. J Nutr Educ Behav. 2012;44(3):210-216. doi: 10.1016/j.jneb.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 42.Odoms-Young A, Bruce MA. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Health. 2018;41(suppl 2):S3-S6. doi: 10.1097/FCH.0000000000000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small-for-gestational-age birth. Am J Public Health. 2015;105(8):1681-1688. doi: 10.2105/AJPH.2015.302613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Margerison-Zilko C, Goldman-Mellor S, Falconi A, Downing J. Health impacts of the great recession: a critical review. Curr Epidemiol Rep. 2016;3(1):81-91. doi: 10.1007/s40471-016-0068-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nianogo RA, Wang MC, Basurto-Davila R, et al. . Economic evaluation of California prenatal participation in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) to prevent preterm birth. Prev Med. 2019;124:42-49. doi: 10.1016/j.ypmed.2019.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Effect of revised WIC food package on maternal and infant health outcomes, including control variables for month and year of birth
eTable 2. Effect of revised WIC food package on maternal and infant health outcomes, excluding pregnancies that included October 2009
eFigure 1. Graphical evaluation of parallel trends assumption
eFigure 2. Graphical evaluation of parallel trends assumption in low-education sample