Abstract
Background
The Public Dental Service (PDS) in Finland has catered for the overwhelming majority of the young for more than 50 years. They have had examinations, preventive measures and all other necessary treatment free of charge. This study aimed to survey the treatment needs and treatment measures provided for children and adolescents and changes in these during the period 2001–2013.
Methods
Using each person’s unique identifier, data on patients (< 18 years), their oral health (CPI > 2, D + d > 0) and treatment received in the period 2001–2013 were collected retrospectively from municipal databases in five PDS-units covering 320,000 inhabitants. The National Institute for Health and Welfare gave ethical approval. Permission to use local data was received from the Directors in the PDS units. Treatment measures were grouped into 14 categories and patients into three age categories (0–6 years, 7–13 years and 14–17 years). Trend analysis was used to test changes over time.
Results
About 40,000 children and adolescents visited the PDS each year and 2,488,805 treatment measures were provided for them during the entire study period. The proportion of those in need of treatment decreased from 44.4 to 33.2% during the study period. The most common treatment categories were examinations (613,753, 24.7%), orthodontics (499,033, 20.1%), preventive measures (372,473, 15.0%) and restorative treatment (355,325, 14.3%); these made up 74% of all treatment measures. During the study period, statistically highly significant (p < 0.001***) increasing trends were found for examinations, anaesthesia and the total number of treatment measures, and a significant (p < 0.001***) decreasing trend in restorative treatment were found for all the young. More preventive treatment measures were provided for those not in need of treatment compared with those in need of treatment.
Conclusion
Although children’s oral health had improved and restorative treatment provided had decreased, the total number of treatment measures increased. Healthy children received frequent examinations and high numbers of preventive treatment measures. Targeting treatment according to needs was not satisfactory.
Keywords: Registers, Oral health, Treatment needs, Public dental service, Treatment measures
Background
Dental caries still affects a great number of children and adolescents in spite of the range of caries preventive methods available [1]. Well-organized oral health care provision systems are in place, such as in the Nordic countries, that provide the young with regular and basically free dental care regardless their place of residence [2]. In Finland, the public sector has catered for children’s dental care since the 1950s, when the school dental services started. In 1972, the Primary Health Care Act obliged municipalities to provide annual examinations and all necessary preventive and dental care free of charge to all persons below 18 years of age. Generally this is undertaken all over the country in the Public Dental Service (PDS). Since the 1970s, children and adolescents’ oral health has improved greatly in many countries including Finland. The mean DMFT value for 12-year-olds was 6.9 in 1975, 1.2 in 1991 and in 2000 [3] and 0.9 in 2013 [4]. Correspondingly, the proportion of caries-free children was 1% in 1975, 30% in 1991, 38% in 2000 [3] and 56% in 2013 [4]. A similar improvement has been seen in the other Nordic and most Western European countries [5].
Oral health has become more important, dental care more systematic and less invasive and self-care definitely more common. Other factors such as economic progress and life style changes have also played a role. Along with improvement of the oral health of the young in Finland, it was intended that adults be able to use the subsidised services of the PDS. All age restrictions on access were gradually abolished up to 2002 [2]. However, in 2009, a third (36.4%) of all treatment measures in the PDS were still provided for children and adolescents [6]. Health improvement can be expected to change the treatment provided.
Little research has been published [6–9] on the content of children’s dental care in general and especially in a longitudinal perspective. Overall, developing outcome measures for oral healthcare is still just beginning [10].
The aim of this study was to survey treatment needs and treatment measures provided in the Public Dental Service for children and adolescents under 18 years of age and changes in them during a 13-year period from 2001 to 2013.
Methods
Five PDS units in southern Finland using a specific electronic patient registration system (WinHit, In Net OY; www.winhit.fi) were asked to participate in the study. Ethical approval for the study was provided by the National Institute for Health and Welfare (THL 1697284289204448) and permission to use the local data by the directors of health services in each PDS unit in 2001. The number of children and adolescents (< 18 years) in the participating PDS units’ catchment areas was in 2001, 55,103 and in 2013, 60,983 persons [11].
Data on all the young people (< 18 years) who had visited the five PDS units during 2001–2013 were collected retrospectively from each municipal database. For each year, the numbers of all patients who had attended for a dental visit and all treatment measures provided by any professional category (dentists, dental hygienists and dental nurses) were extracted from the databases. Registered data on need for basic periodontal and restorative treatment (CPI > 2, D + d > 0) [12] were also collected.
The patients were grouped into three age categories (0–6 years, 7–13 years and 14–17 years). The items of treatment provided were classified into 13 main treatment areas: clinical examinations including complementary examinations (laboratory tests etc.), preventive care (instruction about oral hygiene, dietary advice, fluoride varnish, fissure sealants etc.), periodontics, restorative care (permanent and temporary fillings, crowns made of filling material), endodontics, treatment of temporomandibular disorders (TMD), orthodontics, prosthetics, anaesthesia (local anaesthesia, sedatives, nitrous oxide), emergency treatment, radiology, oral surgery and other treatment (removal of sutures, local medications, certificates etc).
The R 3.3 environment for statistical computing was used for descriptive and inferential analyses.
To separate possible trends in the volumes of treatment categories from annual fluctuations, the log-volumes of categories were modelled as linear over time, allowing for correlated residuals [13]. A similar model was fitted for the total treatment need over time, and for the agreement of treatment need and preventive treatment provided. Note that a linear model on the log-scale is equivalent to a constant proportional change (in percentages) per year (with random fluctuations, the AR residuals). Overall, the models fitted the data well, except for treatment of temporomandibular disorders and prosthetics with very few available years with known volumes. Statistical significance was tested at the level of p < 0.05.
Results
During 2001–2013, the number of children and adolescents who visited the PDS was around 40,000 each year and fluctuated slightly between a minimum 36,263 (in 2006) and a maximum 40,746 (in 2009), Table 1. The number of patients in the two youngest age groups was stable during the study period and the number of 14–17 year old patients increased slightly from 8270 to 9250 (11.9%; Table 1).
Table 1.
Numbers of the young patients (< 18 years), total and by age group (0–6 years, 7–13 years and 14–17 years) treated in the five PDS units; numbers of those having visited a dentist, dental hygienist and dental nurse and numbers of treatment measures by treatment category provided for them by year and totally during 2001–2013 as well as the change between 2001 and 2013 (%)
| Year | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Sum (%) | Change from 2001 to 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients, all and number in the category | Total number of different individuals in age category during the 13 years. | ||||||||||||||
| All (N) | 39,682 | 39,297 | 40,022 | 36,316 | 37,857 | 36,263 | 38,216 | 36,442 | 40,746 | 36,809 | 40,433 | 37,386 | 39,517 | 118,402 | -0,4 |
| 0–6 year olds(%) | 12,918(33%) | 12,479(32%) | 12,744(33%) | 11,505(33%) | 12,314(33%) | 11,101(31%) | 11,817(31%) | 11,117(31%) | 13,064(33%) | 11,836(32%) | 12,604(31%) | 10,728(29%) | 12,025(30%) | 66,572 | -6,9 |
| 7–13 year olds(%) | 18,494(47%) | 18,488(47%) | 18,734(47%) | 16,994(47%) | 17,307(46%) | 16,940(47%) | 17,234(45%) | 16,519(45%) | 18,603(46%) | 17,231(47%) | 18,350(44%) | 17,922(48%) | 18,242(46%) | 69,835 | -1,4 |
| 14–17 year olds(%) | 8270(21%) | 8330(21%) | 8544(21%) | 7817(22%) | 8236(22%) | 8222(23%) | 9165(24%) | 8806(24%) | 9079(22%) | 7742(21%) | 9479(23%) | 8736(23%) | 9250(23%) | 53,919 | 11,9 |
| Examined(per cent of patients) | Sum | ||||||||||||||
| 0–6 year olds(%) | 11,258(87%) | 11,008(88%) | 11,292(88%) | 9632(84%) | 10,737(87%) | 9698(87%) | 10,692(90%) | 9305(84%) | 10,790(83%) | 9477(80%) | 11,042(87%) | 9092(85%) | 10,246(85%) | 134,269 | −9,0 |
| 7–13 year olds(%) | 14,871(80%) | 14,870(80%) | 15,192(81%) | 13,563(80%) | 13,697(79%) | 13,604(80%) | 13,833(80%) | 12,835(77%) | 14,117(76%) | 11,836(69%) | 13,169(72%) | 12,073(67%) | 12,833(70%) | 176,493 | −13,7 |
| 14–17 year olds(%) | 6694(81%) | 6726(81%) | 6992(82%) | 6137(79%) | 6488(79%) | 6422(78%) | 7373(80%) | 6732(76%) | 7111(78%) | 5088(66%) | 7111(75%) | 5893(67%) | 6396(69%) | 85,163 | −4,5 |
| In need of basic treatment(per cent of the examined) | Sum | ||||||||||||||
| 0–6 year olds(%) | 1281(11%) | 1176(11%) | 1208(11%) | 1069(11%) | 929(9%) | 852(9%) | 718(7%) | 689(8%) | 692(6%) | 430(5%) | 520(5%) | 477(5%) | 430(4%) | 10,471 | −66,4 |
| 7–13 year olds(%) | 8647(58%) | 8382(56%) | 8983(59%) | 796,459%) | 7589(55%) | 6335(47%) | 5733(41%) | 5366(43%) | 5640(40%) | 5466(46%) | 5826(44%) | 5488(46%) | 5884(46%) | 87,303 | −32,0 |
| 14–17 year olds(%) | 4644(69%) | 4562(68%) | 4809(69%) | 4125(67%) | 4424(68%) | 3812(59%) | 4185(57%) | 3481(57%) | 3383(48%) | 2715(53%) | 3765(53%) | 3550(60%) | 3481(54%) | 50,936 | −25,0 |
| Treatment measures | Sum (%) | ||||||||||||||
| All treatment measures | 180,967 | 196,527 | 195,887 | 182,910 | 182,458 | 169,864 | 181,623 | 178,628 | 204,659 | 196,513 | 208,163 | 199,309 | 211,297 | 2,488,805 | 16,8 |
| 0–6 year olds | 35,137(19%) | 35,125(18%) | 35,827(18%) | 32,704(18%) | 31,390(17%) | 28,596(17%) | 32,363(18%) | 31,244(17%) | 37,470(18%) | 34,808(18%) | 34,474(17%) | 30,788(15%) | 35,350(17%) | 435,276(17%) | 0,6 |
| 7–13 year olds | 105,888(59%) | 115,003(59%) | 111,940(57%) | 103,898(57%) | 102,848(56%) | 95,354(56%) | 97,201(54%) | 94,350(553) | 108,471(53%) | 107,138(55%) | 112,350(54%) | 110,470(55%) | 114,977(54%) | 1,379,888(55%) | 8,6 |
| 14–17 year olds | 39,942(22%) | 46,399(24%) | 48,120(25%) | 46,308(25%) | 48,220(26%) | 45,914(27%) | 52,059(29%) | 53,034(30%) | 58,718(29%) | 54,567(28%) | 61,339(29%) | 58,051(29%) | 60,970(29%) | 673,641(27%) | 52,6 |
| Examinations | 45,682(25%) | 45,927(23%) | 47,117(24%) | 42,656(23%) | 43,313(24%) | 43,827(26%) | 48,141(27%) | 46,411(26%) | 52,956(26%) | 45,388(23%) | 52,437(25%) | 47,671(24%) | 52,227(25%) | 613,753(25%) | 14,3 |
| Orthodontics | 37,466(21%) | 42,266(22%) | 40,594(21%) | 40,197(22%) | 40,216(22%) | 35,169(21%) | 32,756(18%) | 31,276(18%) | 36,816(18%) | 40,036(20%) | 37,234(18%) | 41,196(21%) | 43,811(21%) | 499,033(20%) | 16,9 |
| Preventive care | 19,260(11%) | 23,683(12%) | 30,034(15%) | 27,819(15%) | 27,463(15%) | 24,659(15%) | 28,953(16%) | 28,949(16%) | 32,987(16%) | 30,657(16%) | 35,901(17%) | 29,779(15%) | 32,329(15%) | 372,473(15%) | 67,9 |
| Restorative treatment | 39,706(22%) | 38,697(20%) | 31,840(16%) | 27,454(15%) | 26,734(15%) | 24,478(14%) | 27,061(15%) | 26,124(15%) | 25,946(13%) | 24,000(12%) | 23,147(11%) | 20,946(11%) | 19,192(9%) | 355,325(14%) | −51,7 |
| Anaesthesia | 11,773(7%) | 13,479(7%) | 14,497(7%) | 14,450(8%) | 14,308(8%) | 13,416(8%) | 14,995(8%) | 15,224(9%) | 16,974(8%) | 17,972(9%) | 18,042(9%) | 17,458(9%) | 17,386(8%) | 199,974(8%) | 47,7 |
| Radiology | 8176(5%) | 11,199(6%) | 11,525(6%) | 11,259(6%) | 11,651(6%) | 10,643(6%) | 12,262(7%) | 11,781(7%) | 12,708(6%) | 10,987(6%) | 12,542(6%) | 12,456(6%) | 13,988(7%) | 151,177(6%) | 71,1 |
| Other treatment | 1956(1%) | 16,53(1%) | 1389(1%) | 872(< 1%) | 945(1%) | 1839(1%) | 2601(1%) | 3743(2%) | 10,000(5%) | 10,708(5%) | 11,937(6%) | 12,610(6%) | 14,498(7%) | 74,751(3%) | 641,2 |
| Emergency treatment | 3316(2%) | 4896(2%) | 5151(3%) | 5261(3%) | 5418(3%) | 5095(3%) | 4593(3%) | 4927(3%) | 5410(3%) | 5930(3%) | 5953(3%) | 6432(3%) | 6799(3%) | 69,181(3%) | 105,0 |
| Oral surgery | 5207(3%) | 5718(3%) | 5619(3%) | 5802(3%) | 5405(3%) | 4864(3%) | 4852(3%) | 4738(3%) | 4921(2%) | 5246(3%) | 5217(3%) | 5187(3%) | 5153(2%) | 67,929(3%) | −1,0 |
| Periodontics | 6241(3%) | 6548(3%) | 5940(3%) | 5060(3%) | 4911(3%) | 3718(2%) | 2846(2%) | 2861(2%) | 3030(1%) | 2496(1%) | 2806(1%) | 2836(1%) | 3079(1%) | 52,372(2%) | −50,7 |
| Endodontics | 1332(1%) | 1563(1%) | 1707(1%) | 1679(1%) | 1727(1%) | 1809(1%) | 2180(1%) | 2190(1%) | 2503(1%) | 2677(1%) | 2576(1%) | 2425(1%) | 2474(1%) | 26,842(1%) | 85,7 |
| Treatment of TMD disorders | 190(< 1%) | 293(< 1%) | 262(< 1%) | 342(< 1%) | 316(< 1%) | 274(< 1%) | 302(< 1%) | 333(< 1%) | 334(< 1%) | 352(< 1%) | 334(< 1%) | 288(< 1%) | 331(< 1%) | 3951(< 1%) | 74,2 |
| Prosthetics | 662(< 1%) | 605(< 1%) | 212(< 1%) | 59(< 1%) | 51(< 1%) | 73(< 1%) | 81(< 1%) | 71(< 1%) | 74(< 1%) | 64(< 1%) | 37(< 1%) | 25(< 1%) | 30(< 1%) | 2044(< 1%) | − 95,5 |
Altogether 2,488,805 treatment measures were provided for the young during the study period (Table 1). More than half of them (1,379,888; 55.4%) were provided for the 7–13-year-olds, about a third (673,641; 27.1%) for the 14–17- year olds and the rest (435,276; 17.5%) for the 0–6- year olds. During the 13-year study period, the 0–6- year olds had on average 6.5 treatment measures per patient, the 7–13- year olds 19.8 and 14–17- year olds 12.5 treatment measures each, respectively.
Examinations (613,753; 24.7%), orthodontics (499,033; 20.1%), preventive measures (372,473, 15.0%), restorative treatment (355,325; 14.3%) and anaesthesia (199,974; 8.0%) made up 82.0% of all treatment measures during the entire study period. Prosthetics and treatment of TMD disorders were extremely uncommon (Table 1).
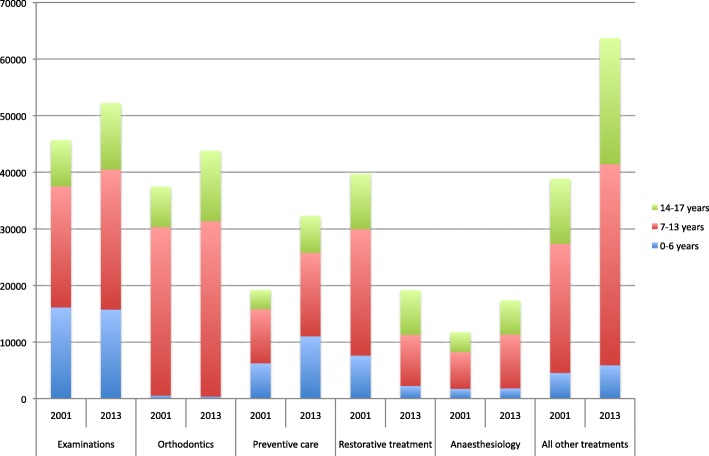
Differences in the most usual treatment categories between the first and last study year are illustrated in Fig. 1. The total number of treatment measures provided increased by 16.8% from 180,967 to 211,297 (Table 1). Examinations increased from 45,927 to 52,227 (14.3%), orthodontics from 37,466 to 43,811 (16.9%), prevention from 19,260 to 32,329 (67.9%), anaesthesia from 11,773 to 17,386 (47.7%) respectively and restorative treatment decreased from 38,697 to 19,192 (− 57.4%; Table 1, Fig. 1).
Fig. 1.
Comparison of numbers of five most common treatment measures (and all other treatments combined) provided for children and adolescents by age group (0–6 years, 7–13 years and 14–17 years) in five PDS units in 2001 and 2013
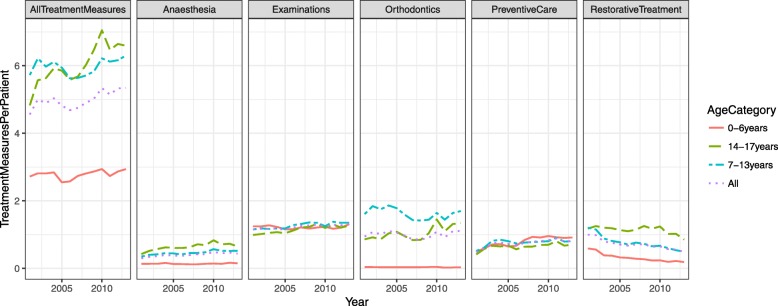
The increasing trends in examinations, anaesthesia and the total number of treatment measures, as well as the decreasing trend in restorative treatment were statistically highly significant (p < 0.001***) for all the young. Accordingly, there was an increasing trend (from 4.5 to 5.2, p = 0.028*) in annual treatment measures per patient (Fig. 2, Table 2). Among the youngest children (0–6 years), the mean number of treatment measures increased slightly (from 2.7 to 2.9, p = 0.031*), among the 7–13 year-olds the increase was also small (from 5.7 to 6.3, p = 0.320 ns). Among the oldest adolescents (14–17 years), the increasing trend was very clear (from 4.8 to 6.6, p = 0.005**).
Fig. 2.
Numbers of the five most usual treatment measures and all treatment measures combined per patient provided for children and adolescents (< 18 years) by age group (0–6 years, 7–13 years and 14–17 years) and totally in five PDS units from 2001 to 2013
Table 2.
Trend analysis on treatment need, on the number of treatment measures per patient in each treatment category provided for all children and adolescents (< 18 years) and separately for the three age categories (0–6 years, 7–13 years and 14–17 years) For the three age categories, only statistically significant treatment categories are presented
| Treatment provided | Age category | mu | sd | t | p |
|---|---|---|---|---|---|
| All treatments and age categories | |||||
| All treatments | All the young | 0.011 | 0.004 | 2.523 | 0.028* |
| All treatments | 0-6 years | 0.005 | 0.005 | 1.085 | 0.031* |
| All treatments | 7-13 years | 0.007 | 0.006 | 1.042 | 0.320 |
| All treatments | 14–17 years | 0.024 | 0.007 | 3.439 | 0.005** |
| Treatment categories and all ages | |||||
| Examinations | All the young | 0.012 | 0.002 | 5.129 | < 0.001*** |
| Orthodontics | All the young | 0.007 | 0.014 | 0.491 | 0.633 |
| Preventive measures | All the young | 0.044 | 0.029 | 1.497 | 0.163 |
| Restorative treatment | All the young | −0.056 | 0.010 | −5.348 | < 0.001*** |
| Anaesthesia | All the young | 0.032 | 0.007 | 4.638 | < 0.001*** |
| Radiology | All the young | 0.045 | 0.029 | 1.561 | 0.147 |
| Other Treatment | All the young | 0.167 | 0.104 | 1.605 | 0.137 |
| Emergencies | All the young | 0.058 | 0.032 | 1.785 | 0.102 |
| Oral surgery | All the young | −0.007 | 0.006 | −1.044 | 0.319 |
| Periodontics | All the young | −0.059 | 0.035 | −1.652 | 0.127 |
| Endodontics | All the young | 0.052 | 0.025 | 2.05 | 0.065 |
| Treatment of TMJ disorders | All the young | 0.030 | 0.017 | 1.812 | 0.097 |
| Prosthetics | All the young | −0.257 | 0.137 | −1.877 | 0.087 |
| For the three age categories only statistically significant treatment categories are presented. | |||||
| Examinations | 7-13 years | 0.015 | 0.003 | 4.246 | 0.001*** |
| Examinations | 14–17 years | 0.022 | 0.005 | 4.612 | < 0.001*** |
| Orthodontics | 14–17 years | 0.035 | 0.015 | 2.411 | 0.035* |
| Restorative treatment | 0-6 years | −0.092 | 0.012 | −7.933 | < 0.001*** |
| Restorative treatment | 7-13 years | −0.072 | 0.015 | −4.742 | < 0.001*** |
| Anaesthesia | 7-13 years | 0.031 | 0.006 | 4.719 | < 0.001*** |
| Emergencies | 7-13 years | 0.030 | 0.008 | 3.836 | 0.003** |
| Emergencies | 14–17 years | 0.070 | 0.019 | 3.673 | 0.004** |
| Periodontics | 0-6 years | −0.142 | 0.036 | −4.001 | 0.002** |
| Endodontics | 0-6 years | 0.024 | 0.010 | 2.555 | 0.027* |
| Endodontics | 14–17 years | 0.069 | 0.015 | 4.608 | < 0.001*** |
| Prosthetics | 14–17 years | −0.149 | 0.047 | −3.15 | 0.009** |
| Treatment need | |||||
| In need of treatment | 0-6 years | −0.092 | 0.010 | −9.021 | < 0.001*** |
| In need of treatment | 7-13 years | −0.031 | 0.019 | −1.623 | 0.133 |
| In need of treatment | 14–17 years | −0.035 | 0.013 | −2.808 | 0.017* |
| Prevention | |||||
| No treatment need | 0-6 years | 0.169 | 0.055 | 3.086 | 0.010* |
| No treatment need | 7-13 years | 0.054 | 0.048 | 1.117 | 0.288 |
| No treatment need | 14–17 years | 0.056 | 0.052 | 1.086 | 0.301 |
| In need of treatment | 0-6 years | −0.113 | 0.051 | −2.231 | 0.047* |
| In need of treatment | 7-13 years | 0.074 | 0.129 | 0.571 | 0.580 |
| In need of treatment | 14–17 years | −0.094 | 0.094 | −1.000 | 0.340 |
mu proportional change (log) per year
sd RMSE of the prop, change
t the t test statistic for H0 of zero mu
p statistical significance
When studying treatment profiles over age categories, in examinations there was an increasing trend in older children (from 1.2 to 1.4, p = 0.001**) for 7–13 year olds and for 14–17 year olds (from 1.0 to 1.3, p < 0.001***) (Table 2, Fig. 2).
Orthodontic treatment was most common among the 7–13 year-olds and 43.8% of them were treated. They had on average 1.5 treatments per year throughout the study period. Among the oldest children about 27.0% of children had had orthodontic treatment and there was an increasing trend from 0.9 to 1.3 treatment measures (p = 0.035*; Fig. 2, Table 2). Orthodontics was uncommon for the youngest children; only 2.9% had had such treatment. During the whole study period, 30.2% of children received orthodontic treatment.
In 2001, preventive treatment was provided for fewer than every second young patient. Among the 0–6 year-olds it almost doubled (p < 0.100 ns), among older age groups the increase was less than double (Fig. 2, Table 2).
There were more preventive treatment measures per patient among those not in need of treatment compared with those in need of treatment in every age category. In addition, among those in need of treatment there was a decreasing trend in mean preventive treatment per patient in the 0–6-year-olds (p = 0.047*) and 13–17-year-olds (p = 0.340 ns; Table 2).
In 2001, there was one restoration for every second child among the 0–6 year-olds and this number had decreased by 69% (p < 0.001***) by 2013. Among older children there was one restoration per patient in 2001 and the decline by 2013 was 61% (p < 0.001**) for 7–13 year olds and 36% (p < 0.320 ns) for 14–17 year olds (Fig. 2, Table 2).
There was one anaesthesia treatment for every tenth 0–6-year-old and one for every second 14–17-year-old. Among the 7–13-year olds there was an increasing trend, from 0.3 to 0.5 treatments (p < 0.001***; Fig. 2, Table 2).
During the study period 2001–2013, the proportion of those in need of basic (caries and periodontal) treatment decreased in all age groups: in the 0–6 year olds from 11 to 4% (p < 0.001***), in the 7–13 year olds from 58 to 46% (p = 0.133 ns) and in the14–17 year olds from 69 to 54% (p = 0.017*; Tables 1 and 2).
Discussion
The main findings in this study were the declining trends in treatment needs and restorative treatment and the increase in the total numbers of treatment measures, especially examinations, anaesthesia and orthodontics in the young (< 18 years). An unexpected finding was that those in need of treatment received less preventive care than those not in need of treatment; the trends diverged in that respect. The fact that more preventive care was provided for those not in need of basic treatment raises noteworthy ethical questions about targeting resources. Are the “at risk” patients being neglected or is restorative treatment still regarded as “the final cure”? In Finland, the recently published evidence-based guidelines for the prevention and management of caries recommend, for caries active children and adolescents, advisory interventions to change unfavourable behaviours, the use of fluoride toothpaste twice a day, fluoride varnish application twice a year, fissure sealants and more specific measures under special circumstances [14]. A recent study of preventive routines in use in children’s and adolescents’ dental care in the PDS in neighbouring Norway showed that clinical practice was not in accordance with the evidence-based guidelines [1]. In Finland, the implementation of the national best practice guidelines depends on how up-to-date the local PDS unit’s strategy is.
“Knowledge translation” is a complex process requiring the leaders of the organisation to introduce the new knowledge and treatment recommendations to the personnel and to make available time and resources to keep up with developments [15]. Unfortunately, this is not everyday practice in dentistry. The trend towards increasing total numbers of treatment measures among the “healthy young” is worrying, especially when politically there has been a desire to improve adults’ access to the PDS. An earlier study showed that the young were five times more likely to be examined in the PDS than adult patients although they were three times less likely to be in need of care [16]. A law enacted in 2011 requires two dental examinations before a child reaches 7 years old and three more examinations before the age of 18 years [17]. The present study recorded more than one examination per patient per year and a trend from 1.2 to 1.3 examinations per patient per year.
The study results show a big (16.9%) increase in orthodontic care provision, which is difficult to explain. There has been no change in the criteria for accessing free of charge orthodontic treatment in the PDS. It is unlikely that bite dysfunctions have increased in the young population but demand probably has increased. In our study, the proportion (30.2%) of children who received orthodontic treatment is in line with reports from the Scandinavian countries [18].
The increase in anaesthesia can be considered to be due to improved pain and fear management. In addition, the treatment is not time consuming [7].
There is little tradition in feasibility evaluation of dental treatment patterns and outcome assessment of dental care [19]. Monitoring of how oral health care functions has focused on economic indicators such as costs and numbers of patients. Local and regional policy-makers, who lack understanding of substance, often have difficulty understanding oral care, so that dentists have had great clinical autonomy [20].
Use of patient management data collected in state-funded dental services or in public and private insurance databases has become a promising method for studying how treatment provided relates to treatment needs and oral health outcomes [21, 22]. In a recent British study, patient management data provided valid accounts of the care without patient recall or selection bias and overall treatment received mirrored treatment needs presented in national epidemiological surveys fairly well [8]. Finland has a long tradition of collecting treatment and performance data in the PDS; these data have however, mainly been used locally, e.g. for paying activity-related remuneration for the dentists and not much for planning of services.
One advantage of this study is that recording of certain oral health indices (treatment needs) and all treatment measures is mandatory in the PDS and, as mentioned, part of each dentist’s salary is based on the treatment measures provided. Thus data from the PDS records have been considered reliable [23]. Further, the data were collected from each unit’s database backup by the same expert using the same script.
A limitation of the study is that the PDS units use many different database systems and produce slightly different data, making it impossible to compare between the units without massive adjustments. Thus, we chose five medium sized or large PDS units in southern Finland using the same patient database system. The total number of Finnish PDS units is 194, most of them are small (< 5000 inhabitants). So, the results of this study can be generalized to medium or large towns in southern Finland. A further limitation of this study is that no information on social background is collected in the PDS register. Also, the information collected on treatment needs and the indicators used were rather crude.
More research is needed on the unexpectedly low use of preventive treatment measures. Also we need more information about the need for and performance of orthodontic care. Almost all the young people in Finland (99%) use the PDS [6]. Throughout the study period, the annual coverage (proportion of the population that attended the PDS) of children and adolescents was high, around 75% [16]. During the study period, the number of dental hygienists doubled (+ 97.9%) and the number of dentists did not change (− 0.0%). When comparing the treatment profile in this study with national data from 2009 it is clear that our figures are in line with national figures and indicate that the selected PDS-units were not outliers among the Finnish PDS units [7]. This study shows that use of routine administrative data collected in the PDS organization can improve transparency of oral health service delivery and offers good tools for leaders and decision makers.
Conclusions
The volume of treatment need and restorative care decreased in all groups of children and adolescents in the study period. Nevertheless, the total number of treatment measures provided increased. The increase was biggest for examinations, anaesthesia and orthodontics. Children not in need of treatment received more preventive care than those in need of treatment. We conclude that treatment need and treatment provided were not in accordance in children’s oral health care; relatively healthy children received a large amount of examinations and preventive treatment measures.
Acknowledgements
We are grateful to the PDS units that offered their data for our study. We would also like to thank Jari Moisanen, Miikka Ristkari and Esko Ristkari from In Net Ltd. (www.winhit.fi) for their valuable help in gathering the material for this study.
Abbreviations
- AR residual
Autoregressive residual
- CPI
Community Periodontal Index
- d
number of decayed decidous teeth
- D
Number of permanent decayed teeth
- DMFT
Number of decayed, missed and filled teeth
- ns
Not significant
- PDS
Public Dental Service
- THL
The National Institute for Health and Welfare (Terveyden ja Hyvinvoinnin Laitos)
- TMD
Temporomandibular disorders
Authors’ contributions
JL and EW planned and designed the study. JL organized the practicalities and the data collection. JL and JS analysed the data. EW helped to interpret the results. JL and EW drafted the manuscript. All authors read and approved the final paper.
Funding
No funding received.
Availability of data and materials
The data that support the findings of this study are available from the National Institute for Health and Welfare (THL) but restrictions apply to the availability of these data, which were used under licence for the current study, and are thus not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the National Institute for Health and Welfare (THL) as well as the participating communities.
Ethics approval and consent to participate
Ethical Committee approval for this study was not necessary according to Finnish law and the obligations of the National Institute for Health and Welfare (THL). This study was considered to be routine work (quality assurance) at THL and the Department’s Director approved the data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Widström E, Tillberg A, Byrkjeflot LI, Skudutyte-Rysstad R. Chair-side preventive interventions in the Public Dental Service in Norway. Br Dent J. 2016;221(4):179–185. doi: 10.1038/sj.bdj.2016.601. [DOI] [PubMed] [Google Scholar]
- 2.Widström E, Agustdóttir H, Byrkjeflot LI, Pälvärinne R, Christensen LB. Systems for provision of oral health care in the Nordic countries. Tandlægebladet. 2015;119:702–711. [Google Scholar]
- 3.Nordblad A, Suominen-Taipale AL, Rasilainen J, Karhunen T. Suun terveydenhuoltoa terveyskeskuksissa 1970- luvulta vuoteen 2000 [Oral Health Care at Health Centres from the 1970s to the year 2000. English summary]. National Research and development Centre for Welfare and Health (stakes), reports 278. Saarijärvi: Gummerus Kirjapaino; 2004. [Google Scholar]
- 4.Kaukonen A-K, Virtanen JI, Nieminen P, Linden J, Widström E. Dental caries development in 12-year-olds in Finland and in the Scandinavian and Baltic countries. Medicina; 2019. In press
- 5.Council of the European Chief Dental Officers (CECDO). Oral Health Database [website]. http://www.cecdo.org. Accessed 15 Nov 2011.
- 6.Widström E, Linden J, Tiira H, Seppälä TT, Ekqvist M. Treatment provided in the public dental Service in Finland in 2009. Community Dent Health. 2015;32:60–64. [PubMed] [Google Scholar]
- 7.Widström E, Linden J. Treatment provided in the public dental service and by private dentists in Finland. Oral Health Dent Manag. 2018;17:1024. [Google Scholar]
- 8.Guiney P, Felicia H, Whelton H, Woods H. Analysis of a payments database reveals trends in dental treatment provision. J Dent Res. 2013;92(7 Suppl):63S–69S. doi: 10.1177/0022034513484327. [DOI] [PubMed] [Google Scholar]
- 9.Holt C. Brugen af og betaling for tandpleje i Danmark, Sverige og Norge. Nor Tannlegeforen Tid. 2013;123:12–18. [Google Scholar]
- 10.Hummel R, Bruers J, van der Galien O, van der Sanden W, van der Hejden G. Outcome measures for oral health based on clinical assessments and claims data: feasibility evaluation in practice. BMC Oral Health. 2017;17:125. doi: 10.1186/s12903-017-0410-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Statistics Finland. Population structure. http://www.stat.fi/til/vaerak/index.html. Accessed 27 Oct 2018.
- 12.World Health Organization . Oral health surveys: basic methods - 5th edition. Geneve: WHO press; 2013. [Google Scholar]
- 13.Chandler R, Scott M. Statistical methods for trend detection and analysis in the environmental sciences. New Jersey: Wiley; 2011. [Google Scholar]
- 14.Suomalaisen Lääkäriseura Duodecimin ja Suomen Hammaslääkäriseura Apollonia ry:n asettama työryhmä. Karies (hallinta). Käypähoito-suositus Finnish Guideline for management of caries, English summary. www.kaypahoito.fi/web/kh/suositukset/suositus?id=hoi50078. Accessed 27 Oct 2018
- 15.Sipilä R, Lommi M-L. Hoitosuositukset eivät muutu hoitokäytännöiksi Itsestään. Treatment recommendations do not automatically translate into treatment practices, English summary. Duodecim. 2014;130:832–839. [PubMed] [Google Scholar]
- 16.Linden J, Josefsson K, Widström E. Frequency of visits and examinations in the public dental Service in Finland – a retrospective analysis, 2001–2013. BMC Oral Health. 2017;17:138. doi: 10.1186/s12903-017-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valtioneuvoston asetus neuvolatoiminnasta, koulu- ja opiskeluterveydenhuollosta sekä lasten ja nuorten ehkäisevästä suun terveydenhuollosta. 6.4.2011/338. (Government regulation of prenatal care, school and student health of children and young people in preventive oral health, In Finnish.). https://www.finlex.fi/fi/laki/alkup/2011/20110338. Accessed 27 Oct 2018.
- 18.Mohlin B, Dømgaard P, Kurol J, Pietilä T. Hälsorisker vid obehandlade malocklusioner (English summary) health hazards caused by malocclusions. Tandläkartidningen. 2007;99(2):40–45. [Google Scholar]
- 19.Skeie M, Klock KS. Scandinavian systems monitoring the oral health in children and adolescents; an evaluation of their quality and utility in the light of modern perspectives of caries management. BMC Oral health. 2014;14:14.43. doi: 10.1186/1472-6831-14-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alestalo P. Management and leadership in the public dental Service in Finland between 2003 and 2011, thesis. Helsinki: University of Helsinki; 2015. [Google Scholar]
- 21.Heller KE, Eklund SA, Burt BA, Briskie DM, Lawrence LM. Using insurance claims and demographic data for surveillance of Children's Oral health. J Public Health Dent. 2004;64(1):5–13. doi: 10.1111/j.1752-7325.2004.tb02719.x. [DOI] [PubMed] [Google Scholar]
- 22.Guiney H, Felicia P, Whelton H, Woods N. Comparing epidemiologically estimated treatment need with treatment provided in two dental schemes in Ireland. BMC Oral Health. 2012;12(31). 10.1186/1472-6831-12-31. [DOI] [PMC free article] [PubMed]
- 23.Hausen H, Kärkkäinen S, Seppä L. Caries data collected from public health records compared with data based on examinations by trained examiners. Caries Res. 2001;35:360–365. doi: 10.1159/000047475. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the National Institute for Health and Welfare (THL) but restrictions apply to the availability of these data, which were used under licence for the current study, and are thus not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the National Institute for Health and Welfare (THL) as well as the participating communities.