Abstract
Background:
High tibial osteotomy (HTO) is increasingly used in young and physically active patients with knee osteoarthritis. These patients have high expectations, including return to sport (RTS). By retaining native knee structures, a return to highly knee-demanding activities seems possible. However, evidence on patient-related outcomes, including RTS, is sparse. Also, time to RTS has never been described. Furthermore, prognostic factors for RTS after HTO have never been investigated. These data may further justify HTO as a surgical alternative to knee arthroplasty.
Purpose:
To investigate the extent and timing of RTS after HTO in the largest cohort investigated for RTS to date and to identify prognostic factors for successful RTS.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Consecutive patients with HTO, operated on between 2012 and 2015, received a questionnaire. First, pre- and postoperative sports participation questions were asked. Also, time to RTS, sports level and frequency, impact level, the presymptomatic and postoperative Tegner activity score (1-10; higher is more active), and the postoperative Lysholm score (0-100; higher is better) were collected. Finally, prognostic factors for RTS were analyzed using a logistic regression model. Covariates were selected based on univariate analysis and a directed acyclic graph.
Results:
We included 340 eligible patients of whom 294 sufficiently completed the questionnaire. The mean follow-up was 3.7 years (± 1.0 years). Out of 256 patients participating in sports preoperatively, 210 patients (82%) returned to sport postoperatively, of whom 158 (75%) returned within 6 months. We observed a shift to participation in lower-impact activities, although 44% of reported sports activities at final follow-up were intermediate- or high-impact sports. The median Tegner score decreased from 5.0 (interquartile range [IQR], 4.0-6.0) presymptomatically to 4.0 (IQR, 3.0-4.0) at follow-up (P < .001). The mean Lysholm score at follow-up was 68 (SD, ± 22). No significant differences were found between patients with varus or valgus osteoarthritis. The strongest prognostic factor for RTS was continued sports participation in the year before surgery (odds ratio, 2.81; 95% CI, 1.37-5.76).
Conclusion:
More than 8 of 10 patients returned to sport after HTO. Continued preoperative sports participation was associated with a successful RTS. Future studies need to identify additional prognostic factors.
Keywords: high tibial osteotomy (HTO), medial opening wedge, lateral closing wedge, de-rotation osteotomy, return to sport, participation, prognosis, directed acyclic graph
A growing number of patients less than 60 years of age suffer from debilitating knee osteoarthritis (OA), due to the obesity epidemic and prolonged participation in high-impact sports and work activities.6,32 Clinicians refer to these patients as falling into a “treatment gap,”14,17 since knee arthroplasty (KA) at a young age is considered undesirable by patients as well as clinicians.23 In the search for treatment alternatives to KA in young and active patients, use of high tibial osteotomy (HTO) has regained considerable interest in recent years.3,27
It is known that younger patients with OA have significantly higher expectations from their knee surgery, including a return to high-impact sports and work activities.14,36 However, participation in such activities after KA results in a 3- to 5-fold increased risk of revision surgery.23 In contrast, HTO retains native knee structures, thus eliminating the risk of prosthesis wear. Furthermore, retention of the natural joint surfaces and ligaments offers the potential for more normal kinematic function.27 Previous studies have shown that HTO compared favorably with KA in terms of postoperative range of motion5 and knee kinematics.30 Consequently, a successful return to highly knee-demanding activities, including sports, may be expected.
Yet, specific studies on the possibility of obtaining such ambitious goals remain sparse. Recent systematic reviews found that 85% of patients can return to sport (RTS) after HTO.7,13 However, the included studies mainly reported on small patient cohorts and showed several methodological flaws. Hence, a lack of robust evidence from large HTO cohorts on relevant patient outcomes, including RTS, still exists.8,34 Additionally, prognostic factors for a successful RTS have never been described. Identifying such factors could improve preoperative counseling and shared decision making, which is essential in obtaining satisfying results in the challenging young knee OA population.20
Therefore, the aim of the present study was to investigate the extent and timing of RTS after HTO in the largest cohort to date and to identify prognostic factors for a successful RTS. We hypothesized that HTO, by retaining native knee structures and providing more natural knee kinematics, would allow for high rates of RTS.
Methods
Study Design and Patient Selection
We performed a monocenter cross-sectional study in consecutive patients with HTO operated on between 2012 and 2015. HTOs were identified based on the surgical code in the database of electronic patient records. Eligibility criteria included age between 18 and 70 years at follow-up, good understanding of the Dutch language, and sufficient ability to complete the questionnaire. Patients who had been treated with HTO bilaterally were asked to complete the questionnaire for the most recent operation. We excluded patients who were operated on for other indications than OA. An online questionnaire was developed using an electronic data management system (Castor EDC, www.castoredc.com). Eligible patients received an invitation by email between May and July 2017, followed by a maximum of 2 telephone reminders. Institutional review board approval was obtained from the local medical ethical review board (reference no. W17_382 #17.448). All patients provided written informed consent.
Patient Characteristics
Patients’ age, body mass index (BMI) (kg/m2), and education level were obtained. Also, patients were asked if they had experienced postoperative complications and whether the same leg had been operated on again after HTO, for example, revision surgery or KA. The American Society of Anesthesiologists classification, degree of correction, and additional information on possible revision surgery and hardware removal were collected from the electronic medical record.
Surgical Technique and Rehabilitation
Surgery was performed by 1 of 3 dedicated knee osteotomy surgeons (one of whom was R.J.v.H.). The HTO frontal plane and transverse plane techniques have been described in previous publications.3,31 Figure 1 illustrates both HTO types that were performed. For varus malalignment, patients underwent a biplanar medial opening wedge HTO. For valgus malalignment, patients underwent a biplanar medial closing wedge HTO. Before surgery, detailed planning was performed for each patient. Degrees of correction in the frontal and sagittal plane were converted to millimeters of wedge to be created or resected, as measured on the calibrated radiographs. In the operating room, calipers and rulers were used to define the wedge in the bone with K-wires (DePuy Synthes) under fluoroscopic guidance. Plate fixation in all patients was performed with angular stable plates (TomoFix; Synthes GmbH). Postoperatively, physical therapy–guided immediate range of motion exercises and muscle strengthening was started. All patients were restricted to partial weightbearing for 6 weeks. Thromboembolic prophylaxis, that is, 40 mg enoxoparin, was prescribed once daily for 6 weeks. After 6 weeks, knee radiographs were obtained to verify bone healing and stability of fixation. Full weightbearing was allowed thereafter, provided that bone healing and stability of fixation were sufficient. At 3 months postoperatively, knee radiographs and, if deemed necessary, full-length standing radiographs were obtained to verify bone healing and the correction of deformity, respectively.
Figure 1.
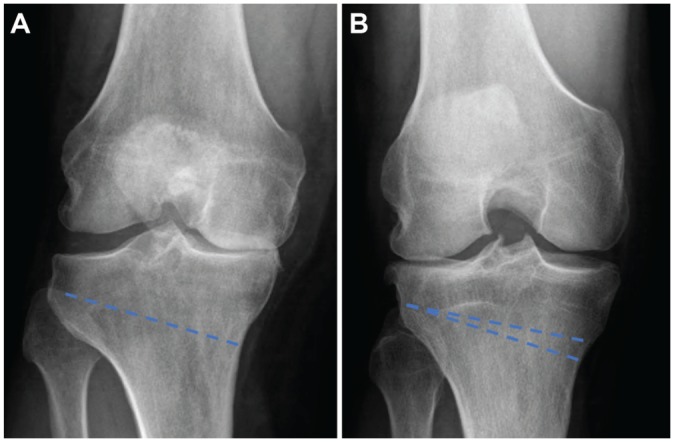
Preoperative anteroposterior radiographs of high tibial osteotomies (HTOs) with projected osteotomy cuts (striped lines). (A) Right knee before opening wedge HTO. (B) Right knee before medial closing wedge HTO.
Sport Outcome Measures
The primary outcome measure was the percentage of patients that returned to sport postoperatively. Secondary outcome measures included the timing of RTS and the frequency, duration, and type of performed sports activities pre- and postoperatively. The validated Tegner activity scale (0-10; higher is more physically active) and Lysholm score (0-100; higher is better function) were collected.9 Since no validated questionnaire exists to assess RTS in patients with knee osteotomy, we adapted the sports questionnaire described by Naal et al,18 which has been used in several studies investigating RTS after knee surgery, including knee osteotomy.10,22 A detailed description of the questionnaire can be found in a previous publication.12 The first question was whether patients had participated in 1 or more sports in their lifetime. If this was not the case, all subsequent sports questions were automatically skipped. Preoperative sports participation was defined as both presymptomatically, that is, before the onset of restricting knee symptoms, and 1 year preoperatively. Postoperative sports participation was defined as 1 year postoperatively and at final follow-up. For each time point, the highest level of participation (recreative, competitive, professional) was asked. Next, sports frequency (0-7 times per week), duration (hours per week), and timing of RTS (weeks) were asked. To assess the level of impact, sports activities were rated as low, intermediate, or high impact according to the classification by Vail et al.29 Finally, patients were asked to rate their sports ability at follow-up, compared with the best sports ability in their lifetime (much worse, worse, unchanged, improved, much improved).
Statistical Analysis
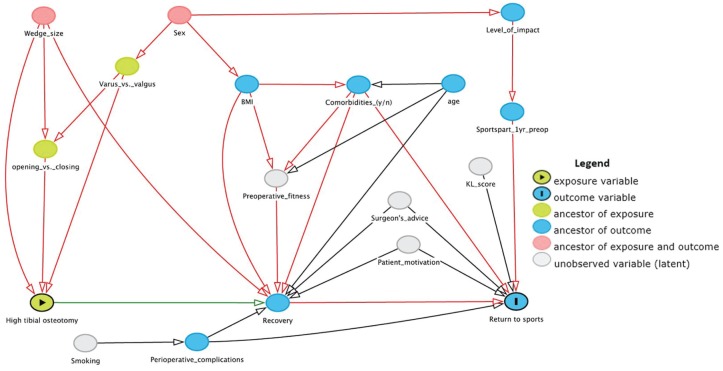
Patient data and pre- and postoperative sports participation were analyzed using descriptive statistics. RTS percentage was calculated by selecting patients who participated in 1 or more sports presymptomatically, preoperatively, or both, and calculating the percentage of these patients performing 1 or more sports 1 year postoperatively, at final follow-up, or both. Also, timing of RTS and frequency and duration of sports participation were analyzed using descriptive statistics. Primary analyses were performed for the total group. Next, subgroup analyses on RTS were performed for the varus and valgus OA subgroups. To investigate prognostic factors for RTS, a logistic regression model was used. First, univariate analysis was performed to assess baseline differences between patients who did RTS and patients who did not RTS. Next, variable selection was based on a causal path diagram that was created using the directed acyclic graph (DAG) approach.26 Covariates were selected based on recent literature on HTO,13 known prognostic factors for functional outcome in patients with KA,6,35 and hypothesized relationships. With the DAG approach, an a priori model of the postulated relationships between the exposure (HTO), outcome variable of interest (RTS), and covariates is established.26 This leads to theoretically and expert-based adjustment and the most parsimonious model being chosen, without the risk of overadjustment and associated reduction of statistical power that could occur otherwise. In the DAG (Figure 2), arrows represent direct causal effects of 1 factor on another. For example, smoking increases the risk of perioperative complications, which in turn negatively influences recovery and thereby RTS. Based on the assumptions described in the diagram, the adjustment set required to estimate the effect of covariates on RTS after HTO included the variables BMI, wedge size, and sports participation 1 year preoperatively. By adjusting for these factors, the effect of all the described covariates in Figure 2 on RTS was investigated. The DAG was created using DAGitty version 2.3.28 A P value <.05 was considered significant. Odds ratios (ORs) and 95% CIs were calculated. All statistical analyses were performed with SPSS for Windows (version 24.0; IBM Corp).
Figure 2.
Directed acyclic graph representing the causal assumptions used for covariate selection.
Results
Participants
Out of 482 consecutive HTOs that were identified in the electronic patient database, 340 HTO patients were deemed eligible for participation (Figure 3). At a mean follow-up of 3.7 years (± 1.0 years), all 340 patients responded, of whom 301 patients completed the questionnaire and 294 could be included in the final analysis. The indication for surgery was unicompartmental OA and varus (n = 235) or valgus (n = 59) knee alignment caused by a tibial deformity. In 1 patient with varus OA, a lateral opening wedge HTO was performed because of laxity of the lateral collateral ligaments. Baseline characteristics are presented in Table 1.
Figure 3.
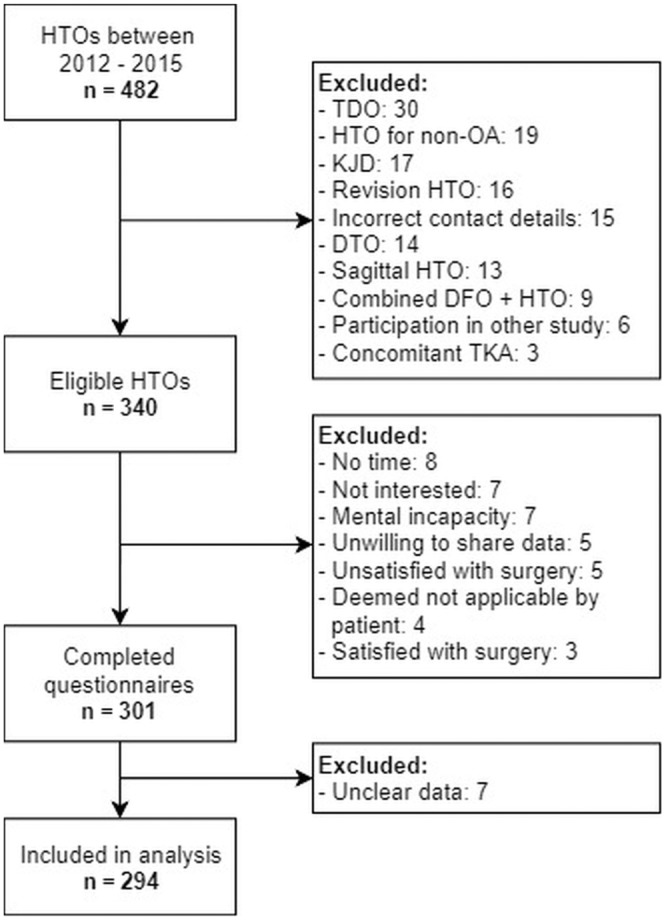
Inclusion flow diagram. DFO, distal femoral osteotomy; DTO, distal tibial osteotomy; HTO, high tibial osteotomy; KJD, knee joint distraction; OA, osteoarthritis; TDO, tibial de-rotation osteotomy; TKA, total knee arthroplasty.
Table 1.
Baseline Characteristics of the Total Group and Varus and Valgus Osteoarthritis Subgroups a
| Outcome Measure | Total Group (N = 294) | Varus OA Group (n = 235) | Valgus OA Group (n = 59) |
|---|---|---|---|
| Mean age at surgery, y (SD) | 50.3 (9.2) | 51.1 (8.9) | 47.1 (9.7) |
| Mean follow-up, y (SD) | 3.7 (1.0) | 3.8 (1.0) | 3.5 (1.0) |
| Sex, female (%) | 120 (41) | 73 (31) | 47 (80) |
| Mean BMI, kg/m2 (SD) | 27.5 (4.4) | 27.5 (4.5) | 27.5 (4.2) |
| Side, right (%) | 151 (51) | 115 (49) | 36 (61) |
| ASA classification, n (%) | |||
| I | 171 (58) | 137 (58) | 34 (58) |
| II | 122 (41) | 97 (41) | 25 (42) |
| III | 1 (1) | 1 (1) | — |
| Osteotomy type, n (%) | |||
| Medial owHTO | 235 (80) | 235 (100) | — |
| Medial cwHTO | 58 (20) | — | 58 (98) |
| Lateral owHTO | 1 (1) | — | 1 (2) |
| Wedge size, mm (SD) | |||
| Medial owHTO | 10.0 (3.0) | 10.0 (3.0) | — |
| Medial cwHTO | 6.7 (2.1) | — | 6.7 (2.1) |
| Lateral cwHTO | — | — b | |
| Revision surgery, yes (%) | 20 (7) | 13 (6) | 7 (12) |
| Revision osteotomy | 2 | 2 | — |
| Non-union | 3 | 3 | — |
| TKA | 11 | 5 | 6 |
| Arthroscopic debridement | 2 | 2 | — |
| Meniscectomy | 1 | 1 | — |
| MUA | 1 | — | 1 |
| Hardware removal, yes (%) | 153 (52) | 114 (49) | 38 (64) |
| Timing of hardware removal, y (SD) | 1.1 (0.6) | 1.3 (0.6) | 0.8 (0.4) |
ASA, American Society of Anesthesiologists; BMI, body mass index; cw, closing wedge; HTO, high tibial osteotomy; MUA, manipulation under anesthesia; OA, osteoarthritis; ow, opening wedge; TKA, total knee arthroplasty; —, no data available.
Wedge size not reported in the patient’s file.
Tegner and Lysholm Scores
Patients reported that their median Tegner score decreased from 5.0 (interquartile range [IQR], 4.0-6.0) presymptomatically to 4.0 (IQR, 3.0-4.0) at follow-up (P < .001). The mean Lysholm score at follow-up was 68 (± 22). In total, 38% of patients reported a Lysholm score of <65 points (poor), 29% a score of 65-83 (fair), 25% a score of 84-94 (good), and 8% a score of >94 (excellent).
Return to Sport
Out of 256 patients participating in 1 or more sports preoperatively, 210 (82%) returned to sport postoperatively. In the varus OA group, 206 patients participated in 1 or more sports preoperatively, of whom 168 patients (82%) could RTS, compared with 42 out of 50 patients (84%) in the valgus OA group (not significant). For the 210 patients who returned to sport, time to RTS was ≤6 months in 158 patients (75%) and 193 patients (92%) returned within 1 year. Figure 4 presents the level of sports participation of the total group at the 4 time points (presymptomatically, 1 year preoperatively, 1 year postoperatively, at final follow-up). Table 2 presents the results for sports frequency in terms of times per week and hours per week and the type of performed sports activities (low, intermediate, and high impact). On average, patients performed 5.8 sports activities per patient presymptomatically, of which 34% were low-impact, 37% were intermediate-impact, and 29% were high-impact activities. This number decreased to 3.3 activities per patient 1 year preoperatively (49% low, 35% intermediate, and 16% high impact) and 3.1 activities per patient 1 year postoperatively (56% low, 34% intermediate, and 10% high impact). At follow-up, patients performed an average of 3.7 activities per patient (56% low, 34% intermediate, and 10% high impact). The participation in all mentioned sports activities at the 4 time points can be found in Appendix Table A1 (available in the online version of this article). Sports ability at final follow-up compared with the best lifetime sports ability was worse or much worse in 173 patients (68%), unchanged in 38 patients (15%), and improved or much improved in 44 patients (17%).
Figure 4.
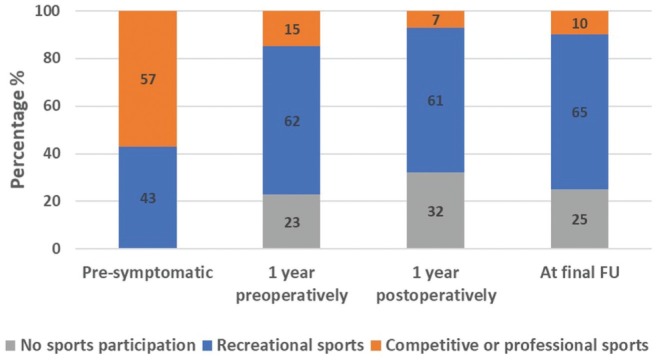
Reported level of sports participation at 4 time points. Patients who participated in 1 or more sports presymptomatically (n = 256) were selected. Their sports participation at 1 year preoperatively, 1 year postoperatively, and final follow-up is presented as the proportion performing “no sports,”“recreational sports,” and “competitive or professional sports.” FU, follow-up.
Table 2.
Sports Frequency and Hours, Level of Impact, and Time to RTS at the 4 Time Points a
| Presymptomatically, n (%) | 1 Year Preoperatively, n (%) | 1 Year Postoperatively, n (%) | At Final Follow-up, n (%) | |
|---|---|---|---|---|
| Sports frequency, times/week | ||||
| No participation | — | 54 (21) | 73 (29) | 63 (24) |
| ≤1 | 37 (14) | 71 (28) | 66 (26) | 58 (23) |
| 2 | 69 (27) | 69 (27) | 65 (25) | 61 (24) |
| 3 | 69 (27) | 38 (15) | 25 (10) | 43 (17) |
| ≥4 | 79 (32) | 24 (9) | 27 (10) | 31 (12) |
| Sports participation, h/week | ||||
| No participation | — | 48 (19) | 70 (27) | 61 (24) |
| 0-2 | 54 (21) | 98 (39) | 100 (39) | 70 (28) |
| 3-4 | 80 (32) | 67 (26) | 49 (19) | 74 (29) |
| 5-6 | 51 (20) | 20 (8) | 17 (7) | 24 (9) |
| >6 | 69 (27) | 19 (8) | 19 (8) | 25 (10) |
| Level of impact | ||||
| Low | 514 (34) | 314 (49) | 306 (56) | 395 (56) |
| Intermediate | 554 (37) | 225 (35) | 184 (34) | 242 (34) |
| High | 427 (29) | 105 (16) | 54 (10) | 74 (10) |
| Total sports | 1495 (—) | 644 (—) | 544 (—) | 711 (—) |
| Time to RTS, week | ||||
| 0-12 | — | — | — | 47 (24) |
| 13-15 | — | — | — | 45 (23) |
| 16-18 | — | — | — | 24 (12) |
| 19-22 | — | — | — | 12 (6) |
| 23-25 | — | — | — | 19 (10) |
| 26-52 | — | — | — | 32 (16) |
| >52 | 16 (8) | |||
In cases with inconsistent answers, data were coded as missing. Thus, not all the numbers add up to 256 patients and percentages for level of participation and frequency may vary slightly. RTS, return to sport; —, no data available.
Prognostic Factors for RTS
On the basis of the DAG (Figure 2) and our univariate analysis (Table 3), the following variables were included in the logistic regression analysis: preoperative BMI, wedge size, and sports participation in the year before surgery (Table 4). The logistic regression model was statistically significant (P < .05), explained 8% (Nagelkerke R2) of the variance in RTS, and correctly classified 81% of cases. The OR for RTS was significantly higher for patients who reported participation in 1 or more sports in the year before surgery compared with those who did not (OR, 2.81; 95% CI, 1.37-5.76). BMI and wedge size were not significantly associated with RTS.
Table 3.
Univariate Analysis of Factors Associated With RTS (Yes vs No) After HTO a
| Outcome Measure | RTS (n = 210) | No RTS (n = 46) | P Value |
|---|---|---|---|
| Mean age at surgery, y (SD) | 50.4 (9.2) | 48.7 (8.2) | .25 b |
| Mean follow-up, y (SD) | 3.7 (1.0) | 3.6 (1.1) | .27 b |
| Female sex, n (%) | 81 (39) | 20 (43) | .54 c |
| Mean BMI, kg/m2 (SD) | 27.1 (3.8) | 28.5 (4.1) | .04 b |
| Side, right (%) | 106 (50) | 24 (52) | .84 c |
| ASA classification, n (%) | |||
| I | 131 (62) | 23 (50) | .25 c |
| II | 78 (37) | 23 (50) | |
| III | 1 (1) | — | |
| Indication, n (%) | |||
| Varus OA | 168 (80) | 38 (83) | .69 c |
| Valgus OA | 42 (20) | 8 (17) | |
| Wedge size, mm (SD) | 9.2 (3.2) | 9.7 (3.3) | .39 b |
| Level of impact 1 year preoperatively, n (%) | |||
| Low | 43 (25) | 14 (47) | .04 c |
| Intermediate | 64 (38) | 6 (20) | |
| High | 62 (37) | 10 (33) | |
| Sports participation 1 year preoperatively, n (%) | |||
| Yes | 169 (80) | 28 (61) | <.01 c |
| No | 41 (20) | 18 (39) | |
Boldface type indicates statistical significance at P < .10. ASA, American Society of Anesthesiologists; BMI, body mass index; HTO, high tibial osteotomy; OA, osteoarthritis; RTS, return to sport; —, no data available.
Independent samples t test.
Chi-square test or Fisher exact test in cases with <5 expected counts.
Table 4.
Logistic Regression Model Analyzing the Effect of BMI, Wedge Size, and Preoperative Sports Participation on the Odds for RTS After HTO a
| Predictors for RTS | Reference | OR | 95% CI |
|---|---|---|---|
| BMI, kg/m2 | — | 0.94 | 0.86-1.02 |
| Wedge size, mm | — | 0.97 | 0.87-1.08 |
| Sports participation 1 year preoperatively (yes/no) | No | 2.81 | 1.37-5.76 |
—, no reference category for continuous variables in the model; BMI, body mass index; HTO, high tibial osteotomy; OR, odds ratio; RTS, return to sport.
Discussion
The most important finding of the present study, in the largest reported HTO cohort analyzed for RTS to date, was that 210 of 256 patients (82%) returned to sport after HTO. Furthermore, 158 (75%) of these patients returned within 6 months and 193 (92%) returned within 1 year. There was no difference in RTS between patients undergoing HTO for varus or valgus OA. Last, continued sports participation in the year before surgery was significantly associated with higher RTS.
In recent years, consideration has increased for patients’ wish to participate in high-impact activities after knee surgery, including knee osteotomy.14 Early studies reported RTS percentages after HTO of less than 50%.16 Improvements in surgical techniques and the introduction of angular stable plate fixation resulted in higher RTS rates (60%-100%) in more recent studies.1,22 Our RTS percentage of 82% is slightly lower than the percentages reported in 2 recent systematic reviews.7,13 However, the RTS percentage is highly influenced by the definition of preoperative sports participation, that is, presymptomatic or preoperative participation.13 Furthermore, several studies described RTS as postoperative sports participation rather than true RTS, namely postoperative sports participation of patients who also participated in sports preoperatively. For the present study, both presymptomatic and preoperative sports participation were asked, and only patients who participated in sports preoperatively were included in the RTS analysis. Consequently, our approach likely resulted in a more reliable RTS estimate compared with previous research.
Additionally, this is the first study investigating time to RTS after HTO. A majority of 75% of patients returned within 6 months. In comparison, 71% of patients returned within 6 months after distal femoral osteotomy (DFO).12 In total, KA median time to RTS was 13 weeks compared with 12 weeks in unicompartmental KA.35 Thus, time to RTS was longer after knee osteotomy compared with KA. This may be explained by slower bone healing and the need for plate removal in many patients, resulting in extended rehabilitation protocols after knee osteotomy. Regarding level of impact, 44% of reported sports activities were intermediate- or high-impact sports after HTO in our cohort. After DFO, this percentage was 45%.12 In contrast, participation in intermediate- and high-impact sports was only 11% after total KA and 23% after unicompartmental KA.35 These findings appear to confirm our hypothesis that, by retaining native knee structures, knee osteotomy allows for more frequent participation in high-impact activities compared with KA.
To further improve patient selection in HTO, identification of predictors for a successful clinical outcome is essential. Our univariate analysis showed no difference in preoperative high-impact sports participation between the patients who did and did not RTS. This was an unexpected outcome, since participation in high-impact activities has been shown to decrease markedly after knee osteotomy, KA, and knee cartilage regeneration procedures.13,21,35 Since obesity is considered a contraindication for HTO (Rand JA, Neyret P. Unpublished data. Presented at ISAKOS Meeting on the Management of Osteoarthritis of the Knee Before Total Knee Arthroplasty, Hollywood, FL, 2005), an association between BMI and RTS was not expected. While BMI was associated with RTS in our univariate analysis, our regression model did not show an association between BMI and RTS. This latter finding is in line with previous studies, which found no association between BMI and RTS.22,25 Based on our DAG, wedge size was included in the regression model, but it was not associated with RTS. However, after HTO using angular stable plate fixation, early full weightbearing is possible.4,15 Consequently, the use of angular stable fixation in our study may have eliminated the negative effect of increased wedge size on RTS. Last, continued sports participation in the year before surgery was the strongest prognostic factor for RTS. Interestingly, in patients with knee and hip arthroplasty, preoperative regular participation in physical activity also was the strongest predictor of physical activity 3 years postoperatively.19 A possible explanation is patient motivation, which is undoubtedly high in cases of continued sports participation despite debilitating knee OA. Likewise, high patient motivation was associated with improved postoperative activity levels in 139 French HTO patients.1 Thus, we may assume that patient motivation plays an important role. Therefore, the importance of motivation to RTS should be discussed with the patient and actively supported before HTO.
While the eligibility criteria for HTO and unicompartmental KA vary11 (Rand JA, Neyret P. Unpublished data. Presented at ISAKOS Meeting on the Management of Osteoarthritis of the Knee Before Total Knee Arthroplasty, Hollywood, FL, 2005), recent meta-analyses have directly compared functional outcomes between these treatment options.5,24 Both studies concluded that HTO results in better range of motion, while unicompartmental KA showed better pain relief and fewer complications. Knee function scores and the proportion of patients that acquired a good or excellent surgical result did not differ between HTO and unicompartmental KA. Unfortunately, none of the included studies directly compared sports participation. The authors concluded that HTO may be the preferred surgical option in patients with high activity requirements, where a superior range of motion is essential and the risk of polyethylene wear after unicompartmental KA would be highest.5,24
Regarding clinical relevance, our data hopefully improve preoperative decision making, since many patients wish to know whether and when they can return to high-demanding sports activities. Furthermore, establishing realistic expectations concerning RTS before surgery may prevent postoperative dissatisfaction.2,20 Additionally, our study is the first to include a regression analysis investigating factors associated with RTS after HTO. The presented DAG may serve as a theoretical framework to guide future variable selection when investigating prognostic factors for sports participation after HTO. In this way, counseling of younger patients with knee OA, eligible for HTO, can be further improved.
A limitation of the present study is its cross-sectional design, which increases the risk of recall bias. Also, we performed a monocenter study in a high-volume knee osteotomy clinic, which might limit the external validity of our findings. Future studies addressing these limitations are needed to confirm modern-day HTO as a worthwhile treatment option for young patients with “old knees” in terms of functional outcomes.8 An important next step is the development of national registries. In the United Kingdom, the UK Knee Osteotomy Registry, including both surgical and patient-reported outcome measures, was launched in 2014.8 Also, the Australian Knee Osteotomy Registry is currently being developed.33 These registries, as well as future prospective studies, will hopefully fill the void in literature regarding patient-relevant outcomes after knee osteotomy.
Conclusion
In conclusion, more than 8 out of 10 patients RTS after HTO, of which the majority return within 6 months. A shift from participation in intermediate- and high-impact sports to low- and intermediate-impact sports can be expected. Sustained sports participation in the year before surgery is a prognostic factor for RTS after HTO. These findings support further justification of HTO as a surgical alternative to KA in young and active patients with knee OA.
Supplemental Material
Supplemental material, DS_10.1177_0363546519849476 for Prognostic Factors for Return to Sport After High Tibial Osteotomy: A Directed Acyclic Graph Approach by Alexander Hoorntje, P. Paul F.M. Kuijer, Berbke T. van Ginneken, Koen L.M. Koenraadt, Rutger C.I. van Geenen, Gino M.M.J. Kerkhoffs and Ronald J. van Heerwaarden in The American Journal of Sports Medicine
Acknowledgments
The authors thank Elise Bonvie-Van Lammeren for her assistance with data collection.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.C.I.v.G. is a paid consultant for Zimmer Biomet. R.J.v.H. has received fees for organizing an educational program from Clockwork Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E. Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc. 2013;21(1):64-73. [DOI] [PubMed] [Google Scholar]
- 2. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brinkman J-M, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, Heerwaarden RJ van. Osteotomies around the knee. J Bone Joint Surg Br. 2008;90(12):1548-1557. [DOI] [PubMed] [Google Scholar]
- 4. Brinkman JM, Luites JW, Wymenga AB, van Heerwaarden RJ. Early full weight bearing is safe in open-wedge high tibial osteotomy. Acta Orthop. 2010;81(2):193-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cao ZW, Mai XJ, Wang J, Feng EH, Huang YM. Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: a systematic review and meta-analysis. J Arthroplasty. 2018;33(3):952-959. [DOI] [PubMed] [Google Scholar]
- 6. Cooper C, Snow S, McAlindon T, Kellingray S, Stuart B, Dieppe P. Risk factors for incidence and progression of radiographic knee osteoarthritis. Arthritis Rheum. 2000;43(5):995-1000. [DOI] [PubMed] [Google Scholar]
- 7. Ekhtiari S, Haldane CE, De Sa D, Simunovic N, Musahl V, Ayeni OR. Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am. 2016;98(18):1568-1577. [DOI] [PubMed] [Google Scholar]
- 8. Elson DW, Dawson M, Wilson C, Risebury M, Wilson A. The UK Knee Osteotomy Registry (UKKOR). Knee. 2015;22(1):1-3. [DOI] [PubMed] [Google Scholar]
- 9. Eshuis R, Lentjes GW, Tegner Y, Wolterbeek N, Veen MR. Dutch translation and cross-cultural adaptation of the Lysholm score and Tegner activity scale for patients with anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2016;46(11):976-983. [DOI] [PubMed] [Google Scholar]
- 10. Faschingbauer M, Nelitz M, Urlaub S, Reichel H, Dornacher D. Return to work and sporting activities after high tibial osteotomy. Int Orthop. 2015;39(8):1527-1534. [DOI] [PubMed] [Google Scholar]
- 11. Hamilton TW, Pandit HG, Jenkins C, Mellon SJ, Dodd CAF, Murray DW. Evidence-based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. J Arthroplasty. 2017;32(6):1779-1785. [DOI] [PubMed] [Google Scholar]
- 12. Hoorntje A, van Ginneken BT, Kuijer PPFM, et al. Eight respectively nine out of ten patients return to sport and work after distal femoral osteotomy [published online October 22, 2018]. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-018-5206-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoorntje A, Witjes S, Kuijer PPFM, et al. High rates of return to sports activities and work after osteotomies around the knee: a systematic review and meta-analysis. Sports Med. 2017;47(11):1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khan M, Adili A, Winemaker M, Bhandari M. Management of osteoarthritis of the knee in younger patients. Can Med Assoc J. 2018;190(3):e72-e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lansdaal JR, Mouton T, Wascher DC, et al. Early weight bearing versus delayed weight bearing in medial opening wedge high tibial osteotomy: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2016;25(12):3670-3678. [DOI] [PubMed] [Google Scholar]
- 16. Lerat J, Moyen B, Garin C, Besse J, Brunet-Guedj E. Anterior laxity and medial arthritis in varus knee. Reconstruction of the anterior cruciate ligament associated with a high tibial osteotomy. J Orthop Surg. 1993;7(3):333-342. [PubMed] [Google Scholar]
- 17. London NJ, Miller LE, Block JE. Clinical and economic consequences of the treatment gap in knee osteoarthritis management. Med Hypotheses. 2011;76(6):887-892. [DOI] [PubMed] [Google Scholar]
- 18. Naal FD, Fischer M, Preuss A, et al. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688-1695. [DOI] [PubMed] [Google Scholar]
- 19. Naylor JM, Pocovi N, Descallar J, Mills KA. Participation in regular physical activity after total knee or hip arthroplasty for osteoarthritis: prevalence, associated factors, and type. Arthritis Care Res (Hoboken). 2019;71(2):207-217. [DOI] [PubMed] [Google Scholar]
- 20. Neuprez A, Delcour J-P, Fatemi F, et al. Patients’ expectations impact their satisfaction following total hip or knee arthroplasty. PLoS One. 2016;11(12):e0167911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pestka JM, Feucht MJ, Porichis S, Bode G, Südkamp NP, Niemeyer P. Return to sports activity and work after autologous chondrocyte implantation of the knee: which factors influence outcomes? Am J Sports Med. 2016;44(2):370-377. [DOI] [PubMed] [Google Scholar]
- 22. Salzmann GM, Ahrens P, Naal FD, et al. Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sport Med. 2009;37(2):312-318. [DOI] [PubMed] [Google Scholar]
- 23. Santaguida PL, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428-436. [PMC free article] [PubMed] [Google Scholar]
- 24. Santoso MB, Wu L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res. 2017;12(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saragaglia D, Rouchy RC, Krayan A, Refaie R. Return to sports after valgus osteotomy of the knee joint in patients with medial unicompartmental osteoarthritis. Int Orthop. 2014;38(10):2109-2114. [DOI] [PubMed] [Google Scholar]
- 26. Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith JO, Wilson AJ, Thomas NP. Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):3-22. [DOI] [PubMed] [Google Scholar]
- 28. Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package “dagitty.” Int J Epidemiol. 2016;45(6):1887-1894. [DOI] [PubMed] [Google Scholar]
- 29. Vail T, Mallon W, Liebelt R. Athletic activities after joint arthroplasty. Sports Med Arthrosc. 1996;4:298-305. [Google Scholar]
- 30. van Egmond N, Stolwijk N, van Heerwaarden R, van Kampen A, Keijsers NLW. Gait analysis before and after corrective osteotomy in patients with knee osteoarthritis and a valgus deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2904-2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Heerwaarden RJ, Van der Haven I, Kooijman MAP, Wymenga AB. Derotation osteotomy for correction of congenital rotational lower limb deformities in adolescents and adults. Surg Tech Orthop Traumatol. 2003;55(10):575-585. [Google Scholar]
- 32. Verbeek J, Mischke C, Robinson R, et al. Occupational exposure to knee loading and the risk of osteoarthritis of the knee: a systematic review and a dose-response meta-analysis. Saf Health Work. 2017;8(2):130-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vertullo C. Feasibility of an Australian Knee Osteotomy Registry. Orthop J Sports Med. 2016;4(suppl 2):2325967116S00033. [Google Scholar]
- 34. Webb M, Dewan V, Elson D. Functional results following high tibial osteotomy: a review of the literature. Eur J Orthop Surg Traumatol. 2018;28(4):555-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Witjes S, Gouttebarge V, Kuijer PPFM, van Geenen RCI, Poolman RW, Kerkhoffs GMMJ. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46(2):1-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Witjes S, van Geenen RC, Koenraadt KL, et al. Expectations of younger patients concerning activities after knee arthroplasty: are we asking the right questions? Qual Life Res. 2017;26(2):403-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_0363546519849476 for Prognostic Factors for Return to Sport After High Tibial Osteotomy: A Directed Acyclic Graph Approach by Alexander Hoorntje, P. Paul F.M. Kuijer, Berbke T. van Ginneken, Koen L.M. Koenraadt, Rutger C.I. van Geenen, Gino M.M.J. Kerkhoffs and Ronald J. van Heerwaarden in The American Journal of Sports Medicine