Abstract
Background:
Orthopaedic surgery is a male-dominated specialty associated with many stereotypes, despite the increased representation of females compared to 30 years ago. Numerous studies have examined medical student and resident perceptions regarding females in orthopaedic surgery to explain the disparity, but there are few studies that analyze whether patients have a gender preference in their orthopaedic surgeon. Our study sought to determine whether patients have a preference for the gender of their orthopaedic surgeon, and what traits in orthopaedic surgeons are important to their patients.
Methods:
A total of 191 new patients seen in the emergency department and orthopaedic urgent care clinic were administered a 22-question survey regarding preferences in their orthopaedic provider. Patients were asked questions regarding preferred gender of their provider, as well as preferences in characteristics exhibited.
Results:
The majority of patients did not have a preference for the gender of their orthopaedist (83.9%); however, 14.5% of patients preferred a female surgeon and 1.6% of patients preferred a male surgeon. Female patients had a preference for the same gender compared to male patients and preferred females (p=0.04). Of the patients that had a preference, 90% preferred a female provider. There were trends towards preference for gender that varied depending on subspecialty. There was a statistically insignificant trend towards preference for male providers in total joint replacements and spine surgery, and conversely a preference for female providers in hand surgery and pediatric orthopaedics. 48.6% of patients cited the single most important trait to be board certification, followed by years in practice (27.1%), then reputation or prestige (16.7%). Over one-third of patients found physical appearance, gender, racial background and age to be important traits.
Conclusions:
The majority of patients did not have a preference for the gender of their orthopaedic surgeon. 16.1% of patients had a preference, and the majority of these patients preferred female surgeons. Preferences for a specific gender were seen that varied based on the subspecialty. Efforts at increasing gender diversity in orthopaedics should continue to be a major goal.
Level of Evidence: III
Keywords: gender, patient preferences, female orthopaedic surgeons, women in surgery
Introduction
Orthopaedic surgery is a male-dominated specialty, despite the increasing number of females entering medical school. In 2010, the total number of female medical students was 47.8%.1 Despite this, the percentage of full time women faculty in orthopaedics in that same year was 15%.1 Blakemore in 2003 found that 0.6% of all female residents chose orthopaedics as a specialty, a percentage that has not changed in the past two decades despite the increase in female representation that is seen in other fields of medicine and surgical subspecialties.2 In 2003, orthopaedics had the lowest percentage of female representation compared to all other surgical specialties except thoracic surgery.2 Recent data from the 2017-2018 National GME Census report that orthopaedics has the lowest number of women with only 15.4% female residents, compared to all other surgical subspecialties.3 General surgery residencies are comprised of 40% women, while other traditionally male-dominated specialties such as otolaryngology, urology, thoracic surgery, and neurosurgery have higher female representation than seen in orthopaedics (35.9%, 25.6%, 24.3%, 17.8%, respectively).3 Van Heest found that from 2004-2009 there was only a 1% increase in the number of female medical students going into orthopaedics.4 Numerous studies have examined medical student and resident perceptions regarding females in orthopaedic surgery as an explanation for the decreased female representation.2,5–7 Rohde et al. questioned female orthopaedic residents and members of the Ruth Jackson Orthopaedic Society who cited factors such as physical strength and perceived lack of work-life balance as deterrents for females entering the field.8 Hill et al. further investigated barriers to females entering orthopaedics and cited acceptance by senior faculty as a barrier.1 Despite these findings, there are few studies that analyze whether acceptance by patients play a role in the lack of female representation and whether patients have a gender preference in their orthopaedic surgeon.
Current literature demonstrates that female physicians add important elements to the doctor- patient relationships. Bertakis et al. found that female physicians displayed different approaches to medicine; for example, taking a greater interest in learning about patients’ feelings and arriving to mutual decision-making.9 These practice styles have been described as “female traits.”9 Additionally, female primary care physicians have been identified to have more empathy, spend more time with patients and display more sensitivity than their male counterparts.10,11 Patients have been shown to often have a specific gender preference for their primary healthcare or obstetrics providers.11-13 However, little research exists regarding patient gender preference in their orthopaedist or the traits displayed by a female orthopaedic surgeon. The purpose of this study is to determine whether patients have a preference for the gender of their orthopaedic surgeon, and what traits are important to patients in their orthopaedic surgeon. We hypothesized that patients would not have a preference of the gender of their orthopaedic surgeon, but would prefer a surgeon who displays traits commonly associated with female providers.
Methods
At a single university healthcare system, 191 new patients seen consecutively in the Emergency Department and orthopaedic urgent care for outpatient orthopaedic complaints over a course of six months were administered a 22-question survey regarding their preferences for follow-up with an orthopaedic provider. This was an institutional review board approved study.
New patients were defined as patients who presented to the Emergency Department and orthopaedic urgent care for care provided by a resident or a midlevel provider, as this represented a population of patients who were not a current patient of an orthopaedic surgeon. Patients were excluded if they were under the age of 18 years old, non-English speaking, or an established orthopaedic patient to minimize bias from an ongoing relationship with an orthopaedic provider. Only patients who were to be discharged from the Emergency Department that day were administered the survey. Questions were asked regarding the preferred gender of their provider, as well as preferences in traits exhibited by their provider (Figure 1). Surveys were administered by both a male and female trained administer.
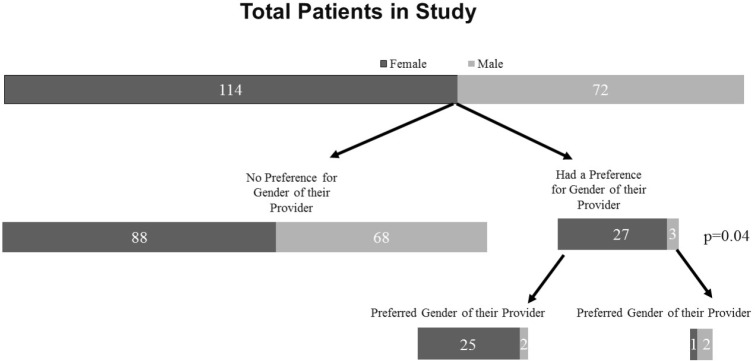
Figure 1.
Survey questions regarding preferences for trait of provider.
Surveys were anonymously given and returned to the provider in a sealed envelope to minimize social desirability bias. There was a 100% response rate; however, of the 191 surveys completed, 49.2% were incomplete, in that a minimum single question or demographic inquiry was left unanswered. Incomplete questions were denoted as “no answer given” and included for analysis of remaining answered questions. Questions were asked regarding nine traits in an orthopaedic surgeon and respondents were asked to rank them in order of importance from “most important” to “least important.” We designated traits with the number “1” assigned to them to receive a ranking of “most important;” “2” received a ranking of “second most important;” “3” received a ranking of “very important;” “4” received a ranking of “important;” “5” received a ranking of “somewhat important;” “6” received a ranking of “less important;” “7” was designated “not very important;” “8” was designated “not important;” and “9” received a ranking of “least important.”
Overall, 191 patients responded to the survey. 61.3% were female and 38.7% were male. Mean age of the patient was 52.7 years [range 18-90 years of age, SD 16.97]. Ethnicities identified included 75.5% Caucasian, 15.2% Black or African American, 6% Hispanic or Latino, 2.2% Asian, Native Hawaiian or Pacific Islander, 0.5% American Indian, Native American or Alaska Native, and 1.6% identified as “Other.” 37.6% of patients reported more than a 4-year college degree (Table 1). Emotional health was represented with 41.4% of patients reporting “excellent,” 36% of patients reporting “very good” (Table 1). 59.2% of patients were married or had a partner (Table 1).
Table 1.
Demographics of Patient Population
| n (%) | Missing data points | |
|---|---|---|
| Gender | 2 | |
| Male | 72 (38.7) | |
| Female | 114 (61.3) | |
| Age | 52.7 years (mean) | 37 |
| 18-90 years range | ||
| Ethnicity | 7 | |
| White or Caucasian | 139 (75.5) | |
| Black or African American | 28 (15.2) | |
| Hispanic or Latino | 11 (6.0) | |
| Asian, Native Hawaiian or Pacific Islander | 4 (2.2) | |
| American Indian or Native American or Alaska Native | 1 (0.5) | |
| Other | 3 (1.6) | |
| Education | 5 | |
| 8th grade or less | 4 (2.2) | |
| Some high school, but did not graduate | 14 (7.5) | |
| High school graduate or GED | 26 (14) | |
| Some college or 2-year degree | 34 (18.3) | |
| 4-year college graduate | 38 (20.4) | |
| More than 4-year college degree | 70 (37.6) | |
| Emotional health | 5 | |
| Excellent | 77 (41.4) | |
| Very good | 67 (36.0) | |
| Good | 26 (14.0) | |
| Fair | 14 (7.5) | |
| Poor | 2 (1.1) | |
| Marital status | 7 | |
| Single | 43 (23.4) | |
| Partner/married | 109 (59.2) | |
| Separated/divorced | 21 (11.4) | |
| Widowed | 11 (6.0) | |
| Other | 0 |
A two-way contingency table was used to explore the association between participants’ preference on various survey questions and their demographic backgrounds (gender, education level, ethnicity, marital status, and emotional status). The significance of association was determined by Pearson’s chi-squared test and Fisher’s t-test. For the analysis of association between participant’s age and their preference, the linear regression model was used, where age was regressed on their preference on individual survey questions. The t-test was carried out to test whether such associations are significant. Data analyses were conducted by R (version 3.3.0). Significance was set at p<0.05.
Results
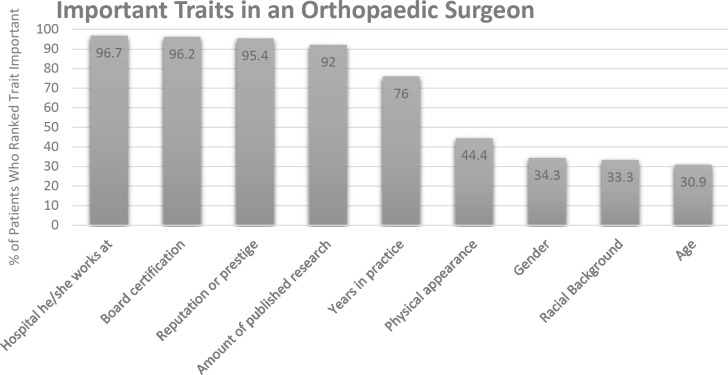
When directly asked whether patients preferred a male or female surgeon, 83.9% of patients had no preference. However, 14.5% of patients preferred a female surgeon and 1.6% of patients preferred a male surgeon. Female patients had a preference for a similar gender compared to male patients (p=0.04). Of the patients that preferred a female surgeon, 89.2% of respondents were female (Figure 2). Additional analysis was performed to stratify for age, ethnicity, emotional health, and education, and there was not a statistically significant difference seen in regard to preference.
Figure 2.
Patient preferences for gender of orthopaedic provider. Flowchart illustrating patient gender preferences of questionnaire respondents. A majority of respondents had no gender preference for their orthopaedic provider; however, when respondents preferred a provider of a specific gender, the respondents were more likely to be female and more likely to prefer a female provider.
Overall, 33.5% of patients reported that they had been treated by a female orthopaedic provider in the past. There was no statistically significant difference in patients who had been treated by a female orthopaedic provider in regards to their preference for a specific gender of their orthopaedist. 88% of patients had no preference in the gender of their orthopaedist after being treated by a female provider. However, 10.2% of patients preferred a female orthopaedist after being treated by a female orthopaedist, compared to 1.7% of these patients who preferred a male orthopaedist (p=0.32).
Patients were asked questions regarding their preferred gender of their orthopaedist depending on the type of subspecialty care they required. Overall, females tended to have more of a preference for the gender of their subspecialty orthopaedist compared to males. The majority of patients reported that they did not have a preference for their provider, but there were trends towards a preference for male or female provider depending on the subspecialty (Table 2). For example, when asked about the preference for the gender of their joint replacement surgeon, of the patients that did have a preference, twice as many preferred a male surgeon (6.6% vs 2.8%, respectively; p=0.24). Of the patients that had a preference, 94% were female. Conversely, when asked about the preferred gender of their hand surgeon, the majority of patients had no preference. However, of the patients that did have a preference, patients preferred female surgeons at a rate almost three times that of male surgeons, although this difference approached statistical significance (6.2% versus 2.2%, respectively, p=0.08). 86.7% of patients who had a preference were female.
Table 2.
Gender Preferences Based on Subspecialty
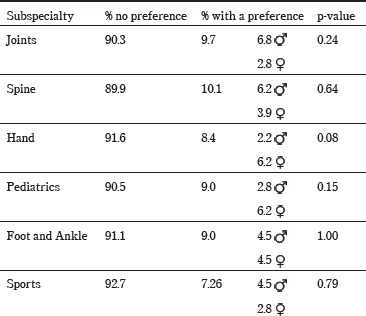 |
Questions were asked regarding preferences for specific traits in their orthopaedic surgeon. When asked whether patients prefer an orthopaedic surgeon who is more athletic versus an orthopaedic surgeon who expressed interest in patients’ feeling and emotions, female patients valued emotional insight more than athleticism (p=0.007). Male patients valued the ability to relate to athletes (p=0.007). While male patients desired the ability to understand and relate to sports, physical strength of the orthopaedist was not found to be an important factor for either gender. Male and female patients preferred a physician who displays sympathy and is able to relate to patients’ problems versus a physician who demonstrates physical strength, although this preference was not statistically significant (p=0.24). There was no significant difference seen between males and females in their desire for an orthopaedist who directs patients to the decision that he or she thinks is best versus an orthopaedist who supports patient-centered decision making (p=0.73).
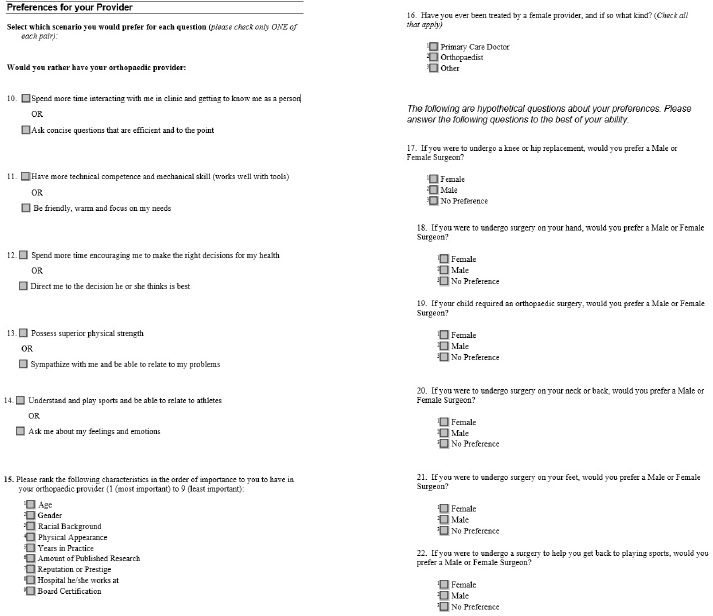
Questions were asked regarding the importance of specific traits desired in an orthopaedic surgeon. When asked the single most important trait, 48.6% of patients cited board certification, followed by years in practice (27.1%), followed by reputation or prestige (16.7%). Over 90 percent of patients reported that the hospital the provider worked at, board certification, reputation of provider, as well as amount of published research were all considered “important” traits (Figure 3). 44.4% of patients ranked physical appearance to be important. 34.3% of patients found gender to be important, while racial background and age were found by 33.3% and 30.9% of patients, respectively, to be important traits (Figure 3).
Figure 3.
Important Traits in an Orthopaedic Surgeon. This chart illustrates the percentage of patients that rated the listed traits as “important” (“most important,” “second most important,” “very important,” “important,” or “somewhat important”). The majority of respondents rated modifiable traits such as hospital affiliation, board certification, reputation, and published research as “important.” While non-modifiable traits like gender, racial background, and age were rated “important” less often, they were still rated “important” by about one-third of respondents.
Discussion
There is compelling evidence for the need to increase diversity in medicine, as communication, patient satisfaction and access to care for the underserved can be improved by gender and ethnic diversity.14-16 Bertakis found that patients of female primary care physicians are more satisfied than those treated by a male physician, even after accounting for patient characteristics and physician practice style.9 Furthermore, gender concordance has been shown to have an effect on communication style. Relationships between female patients and female providers have been shown to have a longer encounter length as well as a perceived more equal contribution to conversation.10,11 Encounters with male-male dyads tend to be the shortest, with more domination of dialogue by the male physician.10,11 Additionally, female concordant visits have been shown to have more positive statements and emotional exchange.10,11 Female physicians have been suggested to participate in more patient-centered communication and have demonstrated to spend more time counseling and teaching preventive behaviors when compared to their male counterparts.9-11 Thus, female orthopaedic surgeons may have different attributes to contribute to each patient encounter, and the lack of female representation in orthopaedics is a cause for concern.
Our results show that the majority of patients do not have preferences for the gender of their orthopaedic provider, as 83.6% of patients when asked directly reported that they had “no preference.” This data suggests that patient preference is unlikely to contribute to the gender disparity in orthopaedics. However, when patients did cite a preference, females were requested more frequently than males, and more commonly by female patients (p=0.04). These results are in accordance with the literature that demonstrates females tend to have more of a preference for the gender of their physician compared to male patients.17,18 Huis In’t Veld et al. studied female patients seeking a plastic surgeon and found that the majority did not have a preference for the gender of their surgeon.19 However, similar to our study, of the patients that did have a preference, females were preferred over males.19 There is evidence that suggests that patients are more comfortable with providers of their same gender. Plunkett et al. found that in obstetrics and gynecology, female physicians were preferred 52.8% of the time compared to 9.6% who preferred male physicians.20 This finding is echoed across fields where intimate interactions are routine.17 When asked reasons for desiring a female physician, patients who had preferences found it easier to talk with female physicians versus male. Likewise, patients who preferred male physicians found it more comfortable to speak with male physicians.17
Interestingly, despite the overall lack of preference for gender of an orthopaedic surgeon, differences in gender preferences according to subspecialty were observed. For total joint replacements and spine surgery, male orthopaedists were preferred over females at double the rate. This preference was displayed by females; however, it was not statistically significant. Abhighari et al. investigated patient gender preferences and found a trend towards preference of male orthopaedists compared to females, although this was found to be statistically insignificant and was not evaluated by subspecialty.21 Questions arise whether this preference is from the current lack of female representation in these specialties, or from perceived stereotypes that may exist regarding need for physical strength and stature. Cannada recently reviewed the number of female fellowship applicants for hip, knee and tumor fellowships and found only 6% of these fellowship applicants are female. Likewise, only 3% of spine applicants are female.22 This lack of gender representation begs the question of whether there is female disinterest in the particular specialty or other factors such as lack of female mentors in these fields that may prevent increasing female representation. Conversely, of patients that had a gender preference, female physicians were preferred in hand surgery and pediatric orthopaedic surgery, although these trends were not statistically significant (p=0.08, p=0.15, respectively). Hand surgery and pediatric orthopaedics have a larger female representation, which may explain the preference seen. Cannada found that the highest number of female fellowship applicants was seen in pediatrics, at 25 percent.22 Bae cited the number of female hand surgeon trainees at 20 percent, although this is comprised of plastic and general surgery applicants in addition to orthopaedic surgery.14 Thus, the higher female representation in pediatrics and hand surgery may suggest increased level of exposure and comfort experienced by patients, as well as female mentors available for trainees.
Our study additionally sought to answer questions of whether patients have preferences for certain traits other than gender. There was no significant difference seen between males and females in their desire for an orthopaedist who employs more patient-centered decision making strategies compared to an orthopaedist who favors surgeon-centered decision making (p=1.00). We aimed to determine whether stereotypes that may exist about orthopaedics, including physical strength and athleticism, were important to patients. Traits more readily desired by both male and female patients included the ability of the orthopaedist to sympathize and provide empathy to the patients’ problems as opposed to possessing physical strength, although this difference was not significant (p=0.24). However, there was a statistically significant difference seen in female patients’ preference for an orthopaedic surgeon who inquires about patient feelings and emotions versus athleticism and ability to relate to athletes (p=0.007). This suggests that there are preferences for various traits exhibited by the orthopaedist that may vary according to patient gender. Additionally, questions were asked regarding traits considered to be of importance to patients (Figure 3). Traits related to experience such as years in practice, reputation or prestige, hospital affiliation, and board certification were widely considered to be important factors. However, personal, non-modifiable factors unrelated to competency or experience such as racial background, physical appearance, gender, and age were listed as an important trait in over a third of patients. This preference argues for the ongoing need for recruitment of orthopaedic trainees of not only diverse gender, but racial background and age, as well. Orthopaedics has been found to lag behind in racial diversity from medical school to orthopaedic residency, when compared to general surgery and other nonsurgical specialties.23 Day et al. found that Asians, Hispanic and Latinos, and African-Americans submit fewer applications for orthopaedic surgery residency compared to Whites, which is troubling due to the trajectory of fewer minorities entering orthopaedics.23 This lack of representation of minorities may impact patient preference from lack of exposure to a diverse group of orthopaedists as well as desire of minority groups for orthopaedists of similar ethnic background and physical appearance. Thus, diversity in gender, age and racial background in orthopaedics can help to address these needs of different patient populations. Improving cultural competency in orthopaedists can be a starting point to achieve this goal. Further studies on racial diversity in orthopaedics may be helpful to further delineate successful strategies for recruitment of orthopaedists of diverse genders as well as racial backgrounds.
Limitations of our study include our sample population, as it was comprised largely of female, Caucasian patients with a greater than 4-year-college education level who sought care in an urgent care or Emergency Department setting. There may be differences in preferences seen in patients of different demographic characteristics. This study demographic is similar to an academic outpatient orthopaedic clinic.24 However, we believe that there would still be preferences seen in our study that are reflective of the gender and ethnic status of the patient, as there is a positive association between physician-patient gender and ethnic/racial concordance.10,16,17 Additionally, our surveys were conducted regardless of patient diagnosis and actual need for surgery. There may be differences in patient preferences in patients who presented with a surgical vs nonsurgical problem that we were unable to detect. However, we believe that patients who sought care in an urgent care or Emergency Department setting were more likely to perceive a need for surgery or acute care than patients who presented for elective outpatient evaluation. Additionally, a formal power analysis was not performed, which could suggest that our nonsignificant findings may have been underpowered. Lastly, our surveys were anonymous, yet 49% of our surveys were incomplete, which may be due to patients’ fear of having their answers revealed. We believe that this may suggest that the preferences seen in our study are an underestimation, as patients may have displayed a Hawthorne effect and chose a more socially acceptable answer that may not be in accordance with their true preferences.
Conclusions
Orthopaedic surgery continues to lag behind other surgical subspecialties in female representation. Our results demonstrate that the majority of patients do not have a preference for the gender of their provider; thus, patient acceptance of female orthopaedic surgeons should not be a factor in this disparity. Bucknall et al. attempted to discover medical student attitudes towards orthopaedics and found that only 24% of female medical students would consider orthopaedic surgery careers.6 Reasons cited included disinterest and male domination.6 Furthermore, medical students who go into orthopaedics tend to report their medical school experiences as the primary influences of their career decision.25 Thus, exposure to orthopaedics early in medical school, with female resident and faculty role models, may help to correct this gender disparity. Lastly, our study shows that there may still be an element of bias in patient perceptions towards orthopaedic surgeons seen in certain subspecialties. Thus, efforts at increasing the number of female orthopaedists should be a major goal that starts at the recruitment level of qualified female medical students, as well as the fostering of female role models.
Acknowledgements
We thank Timothy Ashworth, MD for assistance with data collection.
References
- 1.Hill J.F, Yule A, Zurakowski D, Day C.S. Residents’ perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013;95(19):e1441–6. doi: 10.2106/JBJS.L.00666. [DOI] [PubMed] [Google Scholar]
- 2.Blakemore L.C, Hall J.M, Biermann J.S. Women in surgical residency training programs. J Bone Joint Surg Am. 2003;85(12):2477–80. doi: 10.2106/00004623-200312000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Brotherton SE, Etzel SI. Graduate Medical Education. JAMA. 2018;320(10):1051–1070. doi: 10.1001/jama.2018.10650. [DOI] [PubMed] [Google Scholar]
- 4.Van Heest Ae, Fishman F, Agel J. A 5-Year Update on the uneven distribution of women in orthopaedic surgery resident training programs in the United States. J Bone Joint Surg Am. 2016;98(15):e64. doi: 10.2106/JBJS.15.00962. [DOI] [PubMed] [Google Scholar]
- 5.Biermann JS. Women in orthopedic surgery residencies in the United States. Acad Med. 1998;73(6):708–9. doi: 10.1097/00001888-199806000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Bucknall V, Pynsent P.B. Sex And The Orthopaedic Surgeon; A Survey Of Patient, Medical Student And Male Orthopaedic Surgeon Attitudes Towards Female Orthopaedic Surgeons. Surgeon. 2009;7(2):89–95. doi: 10.1016/s1479-666x(09)80023-1. [DOI] [PubMed] [Google Scholar]
- 7.Templeton K, Wood VJ, Haynes R. Women and Minorities in Orthopaedic Residency Programs. J Am Acad Orthop Surg. 2007;15(suppl_1):S37–41. doi: 10.5435/00124635-200700001-00010. [DOI] [PubMed] [Google Scholar]
- 8.Rohde RS, Wolf JM, Adams JE. Where are the Women in Orthopaedic Surgery? Clin Orthop Relat Res. 2016;474:1950–1956. doi: 10.1007/s11999-016-4827-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertakis KD. The influence of gender on the doctor-patient interaction. Patient Educ Couns. 2009;76(3):356–60. doi: 10.1016/j.pec.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 10.Roter D.L, Hall J.A. Why Physician Gender Matters in Shaping the Physician-Patient Relationship. J Womens Health. 1998;7(9):1093–1097. doi: 10.1089/jwh.1998.7.1093. [DOI] [PubMed] [Google Scholar]
- 11.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 12.Meeuwesen L, Schaap C, Van der Staak C. Verbal analysis of doctor-patient communication. Soc Sci Med. 1991;32(10):1143–1150. doi: 10.1016/0277-9536(91)90091-p. [DOI] [PubMed] [Google Scholar]
- 13.Janssen S.M, Lagro-Janssen A.L.M. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: A systematic review. Patient Educ Couns. 2012;89(2):221–6. doi: 10.1016/j.pec.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 14.Bae GH, Lee AW, Park DJ, Mainwa K, Zurakowski D ASSH Diversity Committee. Day CS. Ethnic and gender diversity in hand surgery trainees. J Hand Surg Am. 2015;40(4):790–7. doi: 10.1016/j.jhsa.2014.10.065. [DOI] [PubMed] [Google Scholar]
- 15.Simon MA. Racial, ethnic, and gender diversity and the resident operative experience. How can the Academic Orthopaedic Society shape the future of orthopaedic surgery? Clin Orthop Relat Res. 1999;360:253–9.13. [PubMed] [Google Scholar]
- 16.Reede JY. A Recurring Theme: The Need For Minority Physicians. Health Aff (Millwood) 2003;22(4):91–93. doi: 10.1377/hlthaff.22.4.91. [DOI] [PubMed] [Google Scholar]
- 17.Kerssens J.J, Bensing J.M, Andela M.G. Patient preference for genders of health professionals. Soc Sci Med. 1997;44(10):1531–1540. doi: 10.1016/s0277-9536(96)00272-9. [DOI] [PubMed] [Google Scholar]
- 18.Bensing J, Van den Brink-Muinen A, De Bakker D. Gender Differences in Practice Style: A Dutch Study of General Practitioners. Medical Care. 1993;31(3):219–229. doi: 10.1097/00005650-199303000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Huis In ‘t Veld,Eva A EA. The Impact of a Plastic Surgeon’s Gender on Patient Choice. Aesthetic surgery journal. 2016. p. sjw180. [DOI] [PMC free article] [PubMed]
- 20.Plunkett B.a, Kohli P, Milad M.P. The importance of physician gender in the selection of an obstetrician or a gynecologist. Am J Obstet Gynecol. 2002;186(5):926–928. doi: 10.1067/mob.2002.123401. [DOI] [PubMed] [Google Scholar]
- 21.Abghari M.S, Takemoto R, Sadiq A, Karia R, Phillips D, Egol K.A. Patient Perceptions and Preferences When Choosing an Orthopaedic Surgeon. Iowa Orthopaedic Journal. 2014;34:204–208. [PMC free article] [PubMed] [Google Scholar]
- 22.Cannada L.K. Women in Orthopaedic Fellowships: What Is Their Match Rate, and What Specialties Do They Choose? Clin Orthop Relat Res. 2016;474:1957. doi: 10.1007/s11999-016-4829-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92(13):2328–35. doi: 10.2106/JBJS.I.01482. [DOI] [PubMed] [Google Scholar]
- 24.Abtahi AM, Presson AP, Zhang C, Saltzman CL, Tyser AR. Association Between Orthopaedic Outpatient Satisfaction and Non-Modifiable Patient Factors. J Bone Joint Surg Am. 2015;97(13):1041–8. doi: 10.2106/JBJS.N.00950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson AL, Sharma J, Chinchilli VM, Emery SE, McCollister Evarts C, Floyd MW, Kaeding CC, Lavelle WF, Marsh JL, Pellegrini VD, Van Heest AE, Black KP. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94(11):e78. doi: 10.2106/JBJS.K.00826. [DOI] [PubMed] [Google Scholar]