Abstract
Background:
Among reproductive-aged women, exposure to interpersonal trauma is associated with genitourinary symptoms. Little is known about the relationship between these exposures and the genitourinary health of older women, who tend to experience different and more prevalent genitourinary symptoms due to menopause and aging.
Objectives:
In this study, we examined relationships between common types of interpersonal trauma and aging-related genitourinary dysfunction among older women.
Study Design:
We analyzed data from the National Social Life, Health, and Aging Project, a national area probability sample of older community-dwelling adults born between 1920–1947. We used cross-sectional data from home-based study visits conducted in 2005–2006 to examine interpersonal violence exposures (any lifetime sexual assault, past-year emotional and physical abuse), and past-year genitourinary symptoms (urinary incontinence, other urinary problems, and vaginal pain/lubrication problems with sexual intercourse) among women participants. Multivariable logistic regression models were used to relate interpersonal violence and genitourinary symptoms, adjusting for age, race/ethnicity, body mass index, education, marital status, parity, hormone therapy, depressive and anxiety symptoms, and self-reported health. In exploratory models, we further adjusted for vaginal maturation, a tissue-specific marker of aging-related urogenital atrophy obtained from vaginal self-swabs.
Results:
In this national sample of 1,551 older women (mean age 69 ± 2 years), 9% reported sexual assault, 23% reported emotional abuse, and <1% reported physical abuse. Urinary incontinence and other urinary problems were reported by 42% and 17%, respectively, and 42% of sexually active women (n=527) reported vaginal symptoms with intercourse. In multivariable regression analyses adjusted for age, race/ethnicity, education, marital status, parity, hormone therapy, anxiety, depressive symptoms, and self-reported health, women with any lifetime history of sexual assault had 2.5 times the odds (95% CI 1.0–6.3) of vaginal symptoms, while women who reported past-year emotional abuse had higher odds of urinary incontinence (OR 1.7, 95% CI 1.2–2.4) and other urinary problems (OR 1.8, 95% CI 1.2–2.8). Among women who provided vaginal self-swabs (n=869), adjustment for vaginal maturation attenuated associations with other urinary problems (OR 1.6, 95% CI .9–2.6) and vaginal symptoms (OR 2.2, 95% CI 0.8–5.8).
Conclusion:
Sexual assault and emotional abuse may play a role in the development or experience of aging-related genitourinary dysfunction in older women. Clinicians caring for older women should recognize the prevalence and importance of traumatic exposures in health related to menopause and aging.
Keywords: Emotional abuse, genitourinary, sexual assault, sexual dysfunction, urinary incontinence
Introduction
An estimated one in four women will experience physical, emotional, or sexual abuse in their lifetimes. These interpersonal trauma exposures are related to increased risk for mental health and medical comorbidities. Research and clinical attention has historically focused on younger women, and less is known about the prevalence of interpersonal trauma in older women, or the potential impact of these experiences on aging-related health.1,2 However, a growing body of evidence indicates that older women not only remain at risk for these exposures, but that the effect of interpersonal trauma may be even more pronounced on their physical health outcomes.3,4
Common physical health concerns among older women include chronic and progressive genitourinary symptoms affecting daily functioning and interpersonal relationships.5 The prevalence of these symptoms, including urinary incontinence, other urinary complaints, and vaginal symptoms related to sexual function, increases with aging. Although risk is primarily attributed to aging-related biological changes, medical comorbidities, and vulvovaginal atrophy secondary to estrogen loss, significant variation in the development and presentation of these symptoms remains unexplained. Among younger women, increased risk for different but related genitourinary symptoms are associated with interpersonal trauma6,7 and other psychosocial risk factors.8 The relationship between these exposures and symptoms has not been examined among older women, for whom interpersonal trauma is an under-recognized risk factor that may impact a broad range of aging-related health concerns and shape genitourinary aging.
In this study, we examined associations between interpersonal trauma and genitourinary dysfunction in a nationally representative sample of older women. We hypothesized that interpersonal trauma would be associated with increased risk for urinary and vaginal symptoms, independent of other known demographic, psychosocial, and clinical risk factors.
Materials and Methods
Study Population
We used data from the first wave of the National Social Life, Health, and Aging Project (NSHAP), a nationally representative probability sample of community-dwelling adults born between 1920 and 1947.9 Details about study design and sampling have been described elsewhere.10 . Between July 2005-March 2006, in-person home-based interviews were conducted with 1,550 women (75.5% overall-weighted response rate). The institutional review boards of the University of Chicago and NORC approved the protocol; all participants provided informed consent.
Interpersonal Trauma Exposures
Interpersonal trauma exposures were assessed by trained interviewers using structured questionnaire items similar to those used in screening protocols11 and other observational studies.3 Any lifetime sexual assault was assessed using the question, “Thinking about your entire life so far, has anyone ever made you have sex by using force or threatening to harm you or someone close to you?” Past-year physical abuse was assessed using the question, “Is there anyone who hits, kicks, slaps, pushes or throws things at you?” Past-year emotional abuse was categorized by a positive response to questions, “Is there anyone who is too controlling over your daily decisions and life?” and/or “Is there anyone who insults you or puts you down?”. Social relationships with perpetrators were not specified in these questionnaires, and could include any person that the respondent had interacted with in the previous year. All items were dichotomized to indicate the presence or absence of the exposure.
Genitourinary outcomes
Urinary symptoms.
The presence and frequency of urinary symptoms were assessed using structured-item questions previously used in epidemiologic studies of older women.12,13 Women were asked, “In the past 12 months, have you had difficulty controlling your bladder, including leaking small amounts of urine, leaking when you cough or sneeze, or not being able to make it to the bathroom on time?” to assess urinary incontinence and “In the past 12 months, have you had other problems with urinating, such as incomplete emptying, a weak urinary stream, straining to begin urination, or difficulty in postponing urination?” to assess other urinary problems. Those who reported symptoms in the past 12 months were asked to categorize the frequency of their symptoms as every day or a few times a week, month, or year. Urinary symptoms that occurred at least “a few times a month” were considered clinically significant, consistent with thresholds in previous studies of similar populations.14–16
Vaginal symptoms affecting sexual activity.
All women who reported partnered, voluntary sexual activity within the past year were asked if there was a period of several months or more that they experienced: a) pain during intercourse, and b) vaginal lubrication difficulty during intercourse. Women were considered to have clinically significant vaginal symptoms if they endorsed pain and/or lubrication difficulty.
Vaginal Maturation
Vaginal epithelial cytology samples from 1,028 (66%) participants were collected from vaginal self-swab specimens. Details about the collection protocol17 and the evaluation of samples18 have been described elsewhere, and the reliability of self-swab sampling has been previously validated.19 Following standard protocols, samples were used to assess the proportion of parabasal, intermediate, or superficial vaginal epithelial cells. Consistent with other observational and interventional studies of urogenital aging,20–22 findings were then used to calculate the vaginal maturation value, a standardized tissue-based marker of vaginal atrophy.18 A lower maturation value may signify genitourinary syndrome of menopause, a common chronic and progressive condition characterized by vulvovaginal, urinary, and/or sexual symptoms related to estrogen loss and vulvovaginal atrophy.5
Covariates
Sociodemographic and health-related covariates were self-reported. Age (continuous) was calculated from interview date and date of birth. Race/ethnicity, education, self-reported health (excellent, very good, good, fair, poor), menopausal hormone therapy use, marital status (married/living with a partner vs. all other responses), and parity (0, 1, 2+ live births) were obtained with interviewer-administered questions. Depressive symptoms were assessed with an interviewer-administered Center for Epidemiologic Studies Depression Scale (CES-D; range=0–60)23 and anxiety symptoms with the Generalized Anxiety Disorder-7 Item scale (GAD-7, range=0–21),24 analyzed as continuous scores.
Statistical Analyses
Characteristics of the sample were examined using weighted descriptive statistics to account for differential probabilities of selection and response rates.10 Differences in three main outcomes: 1) urinary incontinence, 2) other urinary problems, and 3) vaginal pain/lubrication difficulty were examined with logistic regression models in Mplus 8.025. Data for urinary symptoms were available in the full sample, while vaginal symptoms were only assessed in women who reported past-year partnered sexual activity. We employed the full information maximum likelihood method,26,27 which has been shown to produce greater accuracy in model estimations by adjusting for the uncertainty caused by missing data.28,29 Primary analyses were performed using unadjusted models followed by fully adjusted multivariable models. All adjusted models controlled for age, race/ethnicity, education, BMI, marital status, parity, hormone therapy, depressive symptoms, anxiety symptoms, and self-reported health. In exploratory analyses, fully adjusted multivariable models were repeated in a subsample restricted to women who had provided vaginal self-swab specimens, with vaginal maturation included as an additional covariate.
Sampling weights were used to ensure correct calculation of the point estimates. As recommended by NSHAP, we used weight accounting for non-response by age and race.30 Stratification and clustering statements were used to calculate standard errors along with the corresponding tests of statistical significance.
Results
Characteristics of the sample
The primary analytic sample included 1551 women (mean age 68.5, SD 0.23) who provided self-report data on interpersonal trauma and genitourinary symptoms. Participants were primarily non-Latina white (80.5%), married or living with a partner (57.8%), and multiparous (85.3%). Over 69% reported their health as “good” or better, and clinically significant depressive symptoms were reported by only 6% of participants.
Interpersonal trauma exposures
Any lifetime sexual assault was reported by 9.0% of participants, while 22.5% reported past-year emotional abuse (Table 1). Past-year physical abuse was reported by 5 women (<1%), and not included in subsequent analyses due to insufficient power. Over 20% of women in the sample did not provide information about sexual assault. Analyses of key variable differences between groups suggest that non-response to this item was more common among African American and non-partnered women. The prevalence of any lifetime sexual assault and past-year emotional abuse declined with age (Figure 1).
Table 1.
Baseline characteristics of study participants (n=1,551)
| Characteristic | n | weighted n (weighted %) |
|---|---|---|
| Past-year emotional abuse | 329 | 329.1 (22.5) |
| Any lifetime sexual assault | 99 | 113.0 (9.0) |
| Urinary incontinencea | 599 | 606.7 (41.9) |
| Other urinary problemsa | 229 | 231.4 (16.6) |
| Vaginal symptomsb | 221 | 261.5 (42.1) |
| Agec | ||
| 57–65 | 555 | 689.0 (44.5) |
| 66–75 | 538 | 504.9 (32.6) |
| 76–85 | 458 | 354.6 (22.9) |
| Race/ethnicity | ||
| Non-Latina White | 1079 | 124.1 (80.5) |
| Black or African American | 285 | 167.1 (10.8) |
| Latina or Hispanic | 151 | 103.4 (6.7) |
| Married/living with a partner | 762 | 895.5 (57.8) |
| Education | ||
| High school or less | 831 | 768.3 (49.6) |
| College+ | 720 | 780.2 (50.4) |
| Hormone therapy | 160 | 189.6 (12.4) |
| Parity | ||
| Nulliparous | 34 | 29.2 (2.1) |
| Primiparous | 175 | 179.8 (12.6) |
| Multiparous | 1221 | 1217.0 (85.3) |
| Self-reported health | ||
| Excellent | 174 | 199.3 (6.5) |
| Very good | 441 | 483.3 (31.3) |
| Good | 496 | 486.2 (31.5) |
| Fair | 313 | 273.5 (20.8) |
| Poor | 119 | 100.6 (6.5) |
| Depressive symptoms (CES-D ≥16)c | 99 | 25 (4.2) |
| Anxiety symptoms (GAD-7 ≥8)c | 235 | 72 (13.5) |
| Vaginal estrogenization (maturation mean ± SD)d | 869 | 46.6 (0.8) |
Assessed in full sample (n=1551); in analyses, variables dichotomized to ≥ a few times a month vs. else.
Limited to participants who report being sexually active within the past year (n=527).
Continuous variable used in analyses.
Limited to participants who provided adequate vaginal cytology sample (n=869).
Figure 1. Prevalence of interpersonal trauma exposures by age.
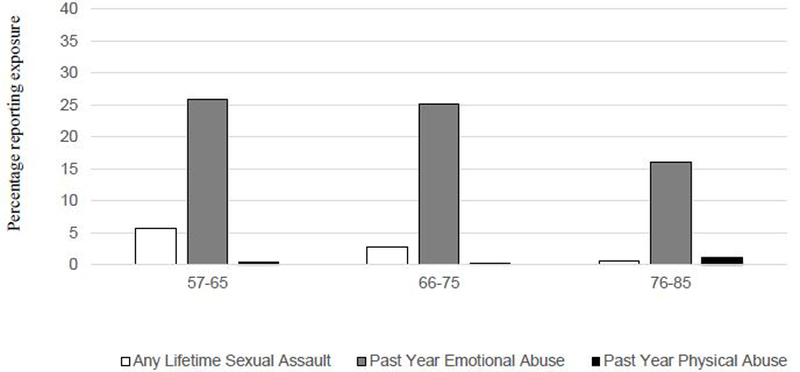
Chi-square tests of trend indicate that reported sexual assault and emotional abuse, but not physical abuse, declined with age (p<.01, p<.001, p=.92, respectively).
Genitourinary symptoms
In the full sample, 41.9% reported urinary incontinence, and 16.6% reported other urinary problems. Among participants who reported partnered sexual activity (n=527), 42.1% reported pain with intercourse or lubrication difficulty affecting sexual function (Table 1). All genitourinary symptoms were more common with increased age.
Vaginal maturation
Vaginal self-swab specimens were provided by 1,028 participants, with 869 specimens determined adequate for further analysis. As previously reported, participants who did not provide vaginal swab specimens were older, less likely to have graduated from high school, and less likely to report hormone therapy use or frequent sexual activity in the previous year.18 Participants who did not provide specimens were also more likely to report lifetime sexual violence exposure, but there were no differences in past-year emotional abuse. Genitourinary symptom reporting was similar in both groups.18 The mean vaginal maturation value was 46.6 (SD .8) (Table 1); 43% had a maturation value less than 50, a commonly used threshold for distinguishing clinically significant vaginal atrophy.
Interpersonal trauma and urinary symptoms
In the full primary analytic sample (n=1551), any lifetime sexual assault was not associated with urinary symptoms in minimally or fully adjusted models. In contrast, past-year emotional abuse was associated with both urinary incontinence (OR 1.7, 95% CI 1.2–2.4) and other urinary problems (OR 1.8, 95% CI 1.2–2.8) (Table 2).
Table 2.
Associations between interpersonal maltreatment and genitourinary symptoms (n=1551)
|
Any lifetime sexual assault OR (95% CI) |
Past-year emotional abuse OR (95% CI) |
|
|---|---|---|
| Urinary incontinence (n=1551) | 1.0 (.6−1.6) | 1.7 (1.2−2.4)** |
| Other urinary problems (n=1551) | 0.8 (.4−1.3) | 1.8 (1.2−2.8)** |
| Vaginal symptoms (n=527)† | 2.5 (1.0−6.3)* | 1.6 (1.0−2.6) |
p<.05
p<.01
Full information maximum likelihood models, adjusted for age, race/ethnicity, BMI, education, marital status, parity, hormone therapy, depressive symptoms, anxiety symptoms, and self-reported health.
Vaginal symptoms only assessed among women who reported partnered sexual activity in the previous 12 months.
In sensitivity analyses, a similar but attenuated pattern of results was seen in the subsample limited to women who provided vaginal swab specimens (n=869), both with and without additional adjustment for vaginal maturation. Past-year emotional abuse remained significantly associated with urinary incontinence (OR 1.5, 95% CI 1.0–2.4), but not other urinary problems (OR 1.6, .9–2.6) (Table 3).
Table 3.
Associations between interpersonal maltreatment and genitourinary symptoms (subsample limited to women with vaginal cytology data, n=869)
|
Any lifetime sexual assault OR (95% CI) |
Past-year emotional abuse OR (95% CI) |
|
|---|---|---|
| Urinary incontinence (n=869) | 1.6 (.9−2.6) | 1.6 (1.1−2.4)* |
| Other urinary problems (n=869) | 0.6 (.3−1.0) | 1.6 (.9−2.6) |
| Vaginal symptoms (n=306)† | 2.0 (.7−5.9) | 1.7 (.9−3.3) |
p<.05
Full information maximum likelihood models, adjusted for age, race/ethnicity, BMI, education, marital status, parity, hormone therapy, depressive symptoms, anxiety symptoms, self-reported health, and vaginal maturation.
Vaginal symptoms only assessed among women who reported partnered sexual activity in the previous 12 months.
Interpersonal trauma and vaginal symptoms
Among sexually active women (n=527), any lifetime sexual assault was associated with vaginal pain with intercourse/lubrication difficulty in fully adjusted models (OR 2.5, 95% CI 1.0–6.3). Past-year emotional abuse was not significantly associated with vaginal symptoms (Table 2).
In exploratory analyses, a similar pattern of results was seen among women who provided vaginal swab specimens and reported sexual activity in the previous year (n=306), both with and without additional adjustment for vaginal maturation. The association between any lifetime sexual assault and vaginal symptoms was similar but no longer significant (OR 2.0, 95% CI .7–5.9); no association was seen between past-year emotional abuse and vaginal symptoms (Table 3). Vaginal maturation was not related to vaginal symptoms (data not shown).
Comment
We examined associations between interpersonal trauma and genitourinary symptoms in a nationally representative sample of older, community-dwelling women. While few women reported physical abuse in the past year, at least one in five women reported past-year emotional abuse, and almost one in ten reported any lifetime history of sexual assault. Accounting for known risk factors, any lifetime history of sexual assault was associated with more than two-fold increased odds of vaginal symptoms affecting sexual function, while past-year emotional abuse was associated with over 70% increased odds of urinary incontinence and other urinary symptoms.
This study adds to a growing body of evidence demonstrating that older women remain at risk for interpersonal trauma, affecting mortality and declining physical functioning.3 A recent review of the existing literature suggests that the risk for emotional abuse remains stable across the lifespan, while recent physical abuse may be less common among older women.4 Our research is consistent with these findings, with nearly a quarter of older women reporting recent emotionally abusive experiences, while physical abuse was rarely reported. Despite the prevalence of emotional abuse among older women in this and other studies, emotional abuse tends to receive less attention in clinical settings and research endeavors than physical and sexual abuse. However, our findings suggest that this common and often under-recognized exposure has independent effects on genitourinary symptoms that may negatively impact quality of life and daily functioning.
These findings advance our knowledge of the health-related impact of trauma among older women, identifying novel associations between trauma and common genitourinary symptoms. The specific links we observed between emotional abuse and urinary symptoms, as well as between sexual assault and vaginal symptoms related to sexual function, are consistent with some past research focused on reproductive-aged women. Increased risk for vaginal symptoms and associated sexual dysfunction has been observed among reproductive-aged women who report a history of childhood and/or adulthood sexual assault.31–33 Similarly, studies of women in younger age groups have shown an association between emotional intimate partner violence and self-reported urinary incontinence and general genitourinary symptoms.34,35 However, past studies have also demonstrated a relationship between sexual assault and lower urinary tract symptoms in reproductive-aged women,6,34,36–38 which was not seen in our study.
Differences between findings in the current study and the previous literature may be due to the different etiology and expression of genitourinary symptoms in older women, and/or differences in the timing of sexual assault experiences occurring in older versus younger women. Urinary symptoms are more common among older women, with increased risk related in part to the cumulative effects of childbirth, chronic medical conditions such as diabetes and cardiovascular disease, declining physical function, and atrophic changes related to estrogen loss. Given these risk factors related to menopause and aging, interpersonal trauma may not play as unique role in the pathophysiology of these symptoms in older women as they do in younger women. Additionally, the relationship between sexual assault and genitourinary outcomes may change over time. Sexual assault was only assessed as an exposure that had occurred at any point in a participant’s lifetime, and it was not possible to account for time elapsed since this experience.
The observed relationships between trauma and genitourinary symptoms may be due to behavioral and/or biological pathways, which cannot be fully determined from this assessment. However, our findings indicate that the effects of interpersonal trauma on genitourinary dysfunction appear to be independent of sociodemographic differences as well as differences in general self-reported health and mood symptoms. Further, our findings do not indicate that associations between interpersonal trauma exposures and genitourinary symptoms are primarily mediated by tissue-specific markers of urogenital atrophy. After adjustment for vaginal maturation, a marker of vaginal cellular atrophy related to estrogen loss, we still observed a strong relationship between emotional abuse and urinary incontinence and a non-significant but related pattern between emotional abuse and other urinary problems, suggesting that the relationship between trauma and genitourinary dysfunction is largely or entirely mediated by other mechanisms. Although the relationship between sexual assault and vaginal symptoms was attenuated to non-significance in equivalent models, the pattern of results remained the same. The loss of statistical significance may have been due to reduced power and selection bias in this constrained subsample, which was limited to a fraction of the larger sample who both remained sexually active and provided cytology specimens. Women who reported any lifetime sexual violence were also less likely to provide specimens, which may have contributed to underestimated risk in this subsample. These findings do not negate a role of vaginal maturation in genitourinary dysfunction. However, this exploratory analysis suggests that for many women, the subjective experience of genitourinary symptoms is related to psychosocial factors, and not dependent on tissue-specific evidence of atrophy.
These findings should be interpreted in light of several limitations. Information about vaginal symptoms was only assessed among women who reported partnered sexual activity in the previous year, precluding examination of these relationships among women who are no longer sexually active. Women who remain sexually active well into their 70s, 80s, and 90s may be a unique population with limited generalizability, as partnered sexual activity reflects a level of health as well as availability of partners. The urinary symptom measures in this study have not undergone psychometric validation against voiding diaries, although they have previously been used to demonstrate associations with other health-related outcomes in older women.12,13 Only 66% of participants provided vaginal self-swabs, limiting our ability to interpret exploratory analyses that included vaginal maturation in this subsample. Differences in vaginal maturation may be expected in those who did not provide self-swabs, who tended to be older, less likely to use hormone therapy, and less likely to be sexually active. Information about the use of lubricants and/or vaginal estrogen therapy, which may affect vaginal symptom presentation and vaginal cytology, was not available. The duration of interpersonal trauma exposures, as well as the relationship of the perpetrator(s) to the participants, cannot be determined in this data. Emotional and physical abuse assessment was limited to past-year exposures, while no specificity of timing was available for history of sexual assault. The items used to define emotional abuse are dependent on subjective interpretations of interpersonal experiences, which may not accurately reflect abusive behaviors. Some women chose not to respond to these questions, particularly those related to sexual assault; although we used statistical approaches to account for missing data, this may reflect the sensitive nature of these disclosures, especially as they were assessed in home-based interviews where partners, family members, and potential perpetrators may have been present.
This study also has a number of strengths, including a large, nationally representative sample of community-dwelling older women, a population that is understudied in relation to trauma as well as sexual health. We accounted for a wide array of demographic, psychosocial, and clinical factors, thus minimizing the likelihood that observed associations were caused by confounding. The study also includes the characterization of multiple aspects of common and disruptive aging-related genitourinary symptoms, assessed with both self-report measures and tissue-specific markers of vulvovaginal atrophy.
Conclusion
Our findings from a national cohort of older women indicate that sexual assault and emotional abuse may play a role in the development and experience of aging-related genitourinary complaints in older women, independent of demographic or clinical factors. Although these exposures are not typically considered in the clinical care of older women, our research suggests that they are both prevalent and important in shaping the experience of genitourinary aging for older women. These findings highlight the importance of additional research to clarify the role of different types of interpersonal trauma exposures in women’s health across the lifespan. They also call attention to the need for greater recognition of the prevalence and importance of traumatic exposures by clinicians caring for older women, and the expanded use of both routine screening for traumatic exposures and trauma-informed care approaches for symptoms related to menopause and aging.
Implications and Contributions:
A. Why was this study conducted?
To examine relationships between interpersonal trauma exposures and the genitourinary health of older women
B. What are the key findings?
Any lifetime sexual assault and past-year emotional abuse were common in this large, national sample of older women.
Emotional abuse was associated with urinary symptoms, while sexual assault was associated with vaginal symptoms related to sexual dysfunction.
Associations were independent of demographic and clinical risk factors, and only mildly attenuated in exploratory analyses including tissue-specific markers of vaginal atrophy.
C. What does this study add to what is already known?
This research adds to the limited literature examining the prevalence and health-related impact of trauma in older adults, providing new evidence to suggest that clinicians caring for older women should expand use of trauma-informed care approaches for symptoms related to menopause and aging.
Acknowledgments
Funding sources/roles of funding sources: The initial study design, methods, subject recruitment, and data collection for NSHAP was funded by the National Institutes of Health, including the National Institute on Aging, the Office of Women’s Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research (R01AG021487), and conducted by the non-partisan and objective research organization NORC at the University of Chicago. The sponsor was not involved in the analysis or preparation of this manuscript. This research was supported in part by the VA Advanced Fellowship Program in Women’s Health at the San Francisco VA Health Care System (CJG).
Footnotes
Conflict of Interest Disclosures: Dr. Gibson received travel support from NORC at the University of Chicago to present the initial study concept and design for this manuscript at the 2016 NSHAP Data Users’ Conference. Dr. Lisha and Dr. Walter have no conflicts of interest to report. Dr. Huang has received research grants from Pfizer Inc. and Astellas through the University of California San Francisco to conduct research unrelated to this manuscript.
Related presentations: An abstract from this research was presented at the Society for General Internal Medicine 2018 Annual Meeting, Denver, CO, April 11–14, 2018.
Publisher's Disclaimer: Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs.
Condensation of the paper: Interpersonal trauma was associated with aging-related genitourinary complaints among 1,551 older women, independent of demographic or clinical factors, and only mildly attenuated by tissue-specific markers of vaginal atrophy.
References
- 1.Tracy EE, Speakman E. Intimate partner violence: not just a concern of the reproductive ages. Menopause 2012;19(1):3–5. [DOI] [PubMed] [Google Scholar]
- 2.Karakurt G, Silver KE. Emotional abuse in intimate relationships: the role of gender and age. Violence Vict 2013;28(5):804–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cannell MB, Weitlauf JC, Garcia L, Andresen EM, Margolis KL, Manini TM. Cross-sectional and longitudinal risk of physical impairment in a cohort of postmenopausal women who experience physical and verbal abuse. BMC Womens Health 2015;15:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knight L, Hester M. Domestic violence and mental health in older adults. Int Rev Psychiatry 2016;28(5):464–474. [DOI] [PubMed] [Google Scholar]
- 5.Gandhi J, Chen A, Dagur G, et al. Genitourinary syndrome of menopause: evaluation, sequelae, and management. Am J Obstet Gynecol 2016. [DOI] [PubMed]
- 6.Bradley CS, Nygaard IE, Mengeling MA, et al. Urinary incontinence, depression and posttraumatic stress disorder in women veterans. Am J Obstet Gynecol 2012;206(6):502 e501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yehuda R, Lehrner A, Rosenbaum TY. PTSD and Sexual Dysfunction in Men and Women. J Sex Med 2015;12(5):1107–1119. [DOI] [PubMed] [Google Scholar]
- 8.Cohen BE, Maguen S, Bertenthal D, Shi Y, Jacoby V, Seal KH. Reproductive and other health outcomes in Iraq and Afghanistan women veterans using VA health care: association with mental health diagnoses. Womens Health Issues 2012;22(5):e461–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waite LJ, Laumann EO, Levinson W, Lindau ST, O’Muircheartaigh CA National Social Life, Health, and Aging Project (NSHAP): Wave 1 Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2014. [Google Scholar]
- 10.O’Muircheartaigh C, Eckman S, Smith S. Statistical design and estimation for the national social life, health, and aging project. J Gerontol B Psychol Sci Soc Sci 2009;64 Suppl 1:i12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain N, Sprague S, Madden K, Hussain FN, Pindiprolu B, Bhandari M. A comparison of the types of screening tool administration methods used for the detection of intimate partner violence: a systematic review and meta-analysis. Trauma Violence Abuse 2015;16(1):60–69. [DOI] [PubMed] [Google Scholar]
- 12.Yip SO, Dick MA, McPencow AM, Martin DK, Ciarleglio MM, Erekson EA. The association between urinary and fecal incontinence and social isolation in older women. Am J Obstet Gynecol 2013;208(2):146 e141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erekson EA, Ciarleglio MM, Hanissian PD, Strohbehn K, Bynum JP, Fried TR. Functional disability and compromised mobility among older women with urinary incontinence. Female Pelvic Med Reconstr Surg 2015;21(3):170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waetjen LE, Xing G, Johnson WO, Melnikow J, Gold EB, Study of Women’s Health Across the N. Factors associated with seeking treatment for urinary incontinence during the menopausal transition. Obstet Gynecol 2015;125(5):1071–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suskind AM, Cawthon PM, Nakagawa S, et al. Urinary Incontinence in Older Women: The Role of Body Composition and Muscle Strength: From the Health, Aging, and Body Composition Study. J Am Geriatr Soc 2017;65(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Townsend MK, Curhan GC, Resnick NM, Grodstein F. The incidence of urinary incontinence across Asian, black, and white women in the United States. Am J Obstet Gynecol 2010;202(4):378 e371–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindau ST, Hoffmann JN, Lundeen K, Jaszczak A, McClintock MK, Jordan JA. Vaginal self-swab specimen collection in a home-based survey of older women: methods and applications. J Gerontol B Psychol Sci Soc Sci 2009;64 Suppl 1:i106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindau ST, Dude A, Gavrilova N, Hoffmann JN, Schumm LP, McClintock MK. Prevalence and correlates of vaginal estrogenization in postmenopausal women in the United States. Menopause 2017;24(5):536–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hess R, Austin RM, Dillon S, Chang CC, Ness RB. Vaginal maturation index self-sample collection in mid-life women: acceptability and correlation with physician-collected samples. Menopause 2008;15(4 Pt 1):726–729. [DOI] [PubMed] [Google Scholar]
- 20.Simon J, Nachtigall L, Gut R, Lang E, Archer DF, Utian W. Effective treatment of vaginal atrophy with an ultra-low-dose estradiol vaginal tablet. Obstet Gynecol 2008;112(5):1053–1060. [DOI] [PubMed] [Google Scholar]
- 21.Carmignani LO, Pedro AO, Montemor EB, Arias VA, Costa-Paiva LH, Pinto-Neto AM. Effects of a soy-based dietary supplement compared with low-dose hormone therapy on the urogenital system: a randomized, double-blind, controlled clinical trial. Menopause 2015;22(7):741–749. [DOI] [PubMed] [Google Scholar]
- 22.Davila GW, Singh A, Karapanagiotou I, et al. Are women with urogenital atrophy symptomatic? Am J Obstet Gynecol 2003;188(2):382–388. [DOI] [PubMed] [Google Scholar]
- 23.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement 1977(1):385–401.
- 24.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 25.Muthén L, Muthén B. MPlus User’s guide Fifth edition Muthén & Muthén; 2007. [Google Scholar]
- 26.Little RJA, Rubin DB. Statistical analysis with missing data 1987.
- 27.Rubin DB. Inference and missing data. Biometrika 1976;63(3):581. [Google Scholar]
- 28.Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods 2001;6(4):330–351. [PubMed] [Google Scholar]
- 29.McArdle JJ, Hamagami F. Modeling incomplete longitudinal and cross-sectional data using latent growth structural models. Experimental Aging Research 1992. [DOI] [PubMed]
- 30.O’Muircheartaigh C, English N, Pedlow S, Kwok PK. Sample design, sample augmentation, and estimation for Wave 2 of the NSHAP. J Gerontol B Psychol Sci Soc Sci 2014;69 Suppl 2:S15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Golding JM, Wilsnack SC, Learman LA. Prevalence of sexual assault history among women with common gynecologic symptoms. Am J Obstet Gynecol 1998;179(4):1013–1019. [DOI] [PubMed] [Google Scholar]
- 32.Campbell R, Wasco SM. Understanding rape and sexual assault: 20 years of progress and future directions. J Interpers Violence 2005;20(1):127–131. [DOI] [PubMed] [Google Scholar]
- 33.Meana M, Binik YM, Khalife S, Cohen D. Psychosocial correlates of pain attributions in women with dyspareunia. Psychosomatics 1999;40(6):497–502. [DOI] [PubMed] [Google Scholar]
- 34.Link CL, Lutfey KE, Steers WD, McKinlay JB. Is abuse causally related to urologic symptoms? Results from the Boston Area Community Health (BACH) Survey. Eur Urol 2007;52(2):397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson JK, John R, Humera A, Kukreja S, Found M, Lindow SW. The prevalence of emotional abuse in gynaecology patients and its association with gynaecological symptoms. Eur J Obstet Gynecol Reprod Biol 2007;133(1):95–99. [DOI] [PubMed] [Google Scholar]
- 36.Bradley CS, Nygaard IE, Hillis SL, Torner JC, Sadler AG. Longitudinal associations between mental health conditions and overactive bladder in women veterans. Am J Obstet Gynecol 2017;217(4):430 e431–430 e438. [DOI] [PubMed] [Google Scholar]
- 37.Bradley CS, Nygaard IE, Torner JC, Hillis SL, Johnson S, Sadler AG. Overactive bladder and mental health symptoms in recently deployed female veterans. J Urol 2014;191(5):1327–1332. [DOI] [PubMed] [Google Scholar]
- 38.Klausner AP, Ibanez D, King AB, et al. The influence of psychiatric comorbidities and sexual trauma on lower urinary tract symptoms in female veterans. J Urol 2009;182(6):2785–2790. [DOI] [PubMed] [Google Scholar]


